Abstract
Coronary computed tomography angiography (CCTA) is widely used as a noninvasive cardiovascular imaging modality that allows visualization of both calcified and noncalcified atherosclerotic plaques and exclusion of coronary luminal stenoses with high diagnostic performance. However, high (>400) coronary artery calcium score (CACS) may increase the false-positive rate and decease diagnostic accuracy due to beam-hardening artifacts resulting from heavily calcified plaques. For patients with high CACS cannot be reliably evaluated with CCTA and invasive coronary angiography (ICA) is frequently recommended in routine clinical practice. Recently, dual-energy CT (DECT) has been introduced to reduce beam-hardening artifacts and improve the diagnostic performance of CCTA in patients with severe coronary calcification. In this chapter, we will investigate the implication of CACS and further discuss the application of DECT in patients with CACS.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
4.1 Case of High Calcium Score (>400) Coronary Artery
4.1.1 History
A 52-year-old male patient felt sudden chest pain in the night, which travels to the left arm, shortness of breath, sweating, nausea, and vomiting 2 months ago. After taking medicine, his symptoms relieved. For further diagnosis, this patient came to our hospital and made a reservation for a cardiac CT examination due to suspected myocardial infarction.
4.1.1.1 Physical Examination
-
Blood pressure: 103/73 mmHg
-
Breathing rate: 15/min
-
Heart rate: 67 bpm
4.1.1.2 Electrocardiograph
Reversed T wave, ST segment elevation.
4.1.1.3 Laboratory
Serum myocardial enzyme spectrum showed negative results.
4.1.2 Imaging Examination
4.1.2.1 CT Images
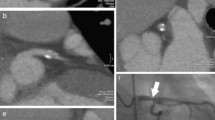
CCTA image was obtained from DECT to evaluate plaque and coronary lumen (Figs. 4.1 and 4.2)
4.1.2.2 Conventional Coronary Angiography (Fig. 4.3)
4.1.3 Imaging Findings and Diagnosis
The CCTA image results showed multiple mixed plaque in LAD, in which severe stenosis in the proximal and middle segment and moderate stenosis in the distal segment. There were multiple mixed plaques in the proximal–middle segments of LCX leading to severe stenosis. Mild-moderate stenosis exists in the middle segment resulting from multiple mixed plaques of RCA. High monoenergetic imaging from DECT can decrease effectively calcified blooming artifact. The invasive coronary angiography images confirmed multiple stenosis in three coronary arteries.
4.1.4 Management
-
Coronary artery bypass grafting operation
-
Conventional medical therapy for coronary artery disease (CAD)
4.2 Discussion
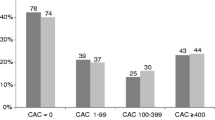
Coronary artery calcium (CAC) is a highly specific feature of coronary atherosclerosis in CAD. The prevalence of CAC continues to increase with growing age, and men have higher calcium levels than women [1]. In addition, patients with high risk factors, such as diabetes mellitus, dyslipidemia, and hypertension, are more susceptible to CAC. The calcium score proposed by Agatston et al. remains the most widely accepted technique for predicting major adverse cardiovascular events and it is determined by the product of the total size and density of the calcified plaque deposited in the coronary artery tree [2]. Standardized categories for CACS include scores of 0 with the absence of calcified plaque, 1 to 10 with minimal plaque, 11 to 100 with mild plaque, 101 to 400 with moderate plaque, and >400 with severe plaque. And CACS >400 indicates significant prognostic implications in specific patient groups [3]. Other techniques for the measurement of coronary artery calcium are volume score and mass score [4].
Intravascular ultrasound (IVUS) has high diagnostic performance in identifying and characterizing plaque composition [5]. According to the range of calcified lesion detected by IVUS, CAC is divided into four classes: Class I with 0°–90° calcification, Class II with 91°–180° calcification, Class III with181°–270° calcification, and Class IV >270° calcification [3].
Optical coherence tomography (OCT) is also an intravascular imaging modality that enables providing cross-sectional images of tissue and has high sensitivity and specificity to identify atherosclerotic plaques [6]. Moreover, optical coherence tomography can be used to assess the thickness and volume of calcified plaque.
4.3 Current Technical Status and Applications of CT
DECT is a novel technology that allows the acquisition of two different datasets from two different X-ray spectra energies. Current techniques for DECT are divided into source-based and detector-based technique [7]. Source-based DECT includes dual-source scanner (two X-ray source–detector systems), rapid kVp switching scanner (a single X-ray source–detector system), dual-spin scanner (a single X-ray source and a single detector layer), and twin-beam scanner (X-ray beam is split into two energy spectra by pre-filtration). Detector-based DECT includes dual-layer detector and photon counting scanner. These techniques not only provide new clinical application for cardiac CT, but also overcome some disadvantages which exist in conventional CT.
Virtual monoenergetic imaging (VMI) generated from DECT reconstruction is analogous to imaging with a monoenergetic beam at single kiloelectron voltage (keV). Although calcium blooming artifact from coronary calcified plaque can lead to overestimate lumen stenosis at conventional CT, it is reduced at DECT by using high monoenergetic imaging. There are some evidences that calcium blooming effectively decreases at higher monoenergetic levels [8, 9]. Moreover, the use of monochromatic reconstructions improved the overall accuracy of coronary stenosis assessment using ICA as a standard of reference [10].
Calcium subtraction imaging can be obtained at conventional CT, but this technique will increase image misregistration risk and radiation dose [11]. In contrast, DECT has the ability to differentiate intravascular calcium from iodine contrast medium based on its material decomposition during image acquisition. Consequently, virtual calcium subtracted images derived from DECT were generated using dedicated subtraction algorithms. The study of De Santis D et al. demonstrated a prototype calcium subtraction algorithm from DECT that can improve coronary lumen assessment and increase diagnostic confidence in patients with heavy calcified coronary artery [12].
Virtual non-contrast (VNC) imaging is characterized by iodine elimination from CT angiographic imaging. Compared with true non-contrast imaging, VNC imaging can be obtained at one acquisition and thereby reduce radiation dose. Moreover, this technique can be used to differentiate contrast medium and other non-iodine material, such as calcified plaque and mental implanted material. VNC imaging can be used for CACS analysis. CACS from VNC imaging has excellent correlations compared with those from true non-contrast imaging [13, 14].
DECT provides multiple possibilities for calcified plaque analysis by different reconstruction algorithms, which are beneficial to disease diagnosis and clinical management.
4.4 Key Points
-
CACS is a reliable technique for cardiac events risk evaluation.
-
High keV monoenergetic imaging can decrease calcium blooming artifact.
-
Calcium subtraction imaging and VNC imaging can reduce radiation dose.
References
McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the multi-ethnic study of atherosclerosis (MESA). Circulation. 2006;113(1):30–7. https://doi.org/10.1161/circulationaha.105.580696.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–32. https://doi.org/10.1016/0735-1097(90)90282-t.
Liu W, Zhang Y, Yu CM, Ji QW, Cai M, Zhao YX, et al. Current understanding of coronary artery calcification. J Geriatr Cardiol. 2015;12(6):668–75. https://doi.org/10.11909/j.issn.1671-5411.2015.06.012.
Alluri K, Joshi PH, Henry TS, Blumenthal RS, Nasir K, Blaha MJ. Scoring of coronary artery calcium scans: history, assumptions, current limitations, and future directions. Atherosclerosis. 2015;239(1):109–17. https://doi.org/10.1016/j.atherosclerosis.2014.12.040.
Nair A, Kuban BD, Tuzcu EM, Schoenhagen P, Nissen SE, Vince DG. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002;106(17):2200–6. https://doi.org/10.1161/01.cir.0000035654.18341.5e.
Yabushita H, Bouma BE, Houser SL, Aretz HT, Jang IK, Schlendorf KH, et al. Characterization of human atherosclerosis by optical coherence tomography. Circulation. 2002;106(13):1640–5. https://doi.org/10.1161/01.cir.0000029927.92825.f6.
Kalisz K, Halliburton S, Abbara S, Leipsic JA, Albrecht MH, Schoepf UJ, et al. Update on cardiovascular applications of multienergy CT. Radiographics. 2017;37(7):1955–74. https://doi.org/10.1148/rg.2017170100.
Van Hedent S, Hokamp NG, Kessner R, Gilkeson R, Ros PR, Gupta A. Effect of virtual monoenergetic images from spectral detector computed tomography on coronary calcium blooming. J Comput Assist Tomogr. 2018;42(6):912–8. https://doi.org/10.1097/RCT.0000000000000811.
Yu L, Leng S, McCollough CH. Dual-energy CT-based monochromatic imaging. AJR Am J Roentgenol. 2012;199(5 Suppl):S9–s15. https://doi.org/10.2214/ajr.12.9121.
Stehli J, Clerc OF, Fuchs TA, Possner M, Gräni C, Benz DC, et al. Impact of monochromatic coronary computed tomography angiography from single-source dual-energy CT on coronary stenosis quantification. J Cardiovasc Comput Tomogr. 2016;10(2):135–40. https://doi.org/10.1016/j.jcct.2015.12.008.
De Santis D, Eid M, De Cecco CN, Jacobs BE, Albrecht MH, Varga-Szemes A, et al. Dual-energy computed tomography in cardiothoracic vascular imaging. Radiol Clin N Am. 2018;56(4):521–34. https://doi.org/10.1016/j.rcl.2018.03.010.
De Santis D, Jin KN, Schoepf UJ, Grant KL, De Cecco CN, Nance JW, et al. Heavily calcified coronary arteries: advanced calcium subtraction improves luminal visualization and diagnostic confidence in dual-energy coronary computed tomography angiography. Investig Radiol. 2018;53(2):103–9. https://doi.org/10.1097/rli.0000000000000416.
Song I, Yi JG, Park JH, Kim SM, Lee KS, Chung MJ. Virtual non-contrast CT using dual-energy spectral CT: feasibility of coronary artery calcium scoring. Korean J Radiol. 2016;17(3):321–9. https://doi.org/10.3348/kjr.2016.17.3.321.
Schwarz F, Nance JW, Ruzsics B, Bastarrika G, Sterzik A, Schoepf UJ. Quantification of coronary artery calcium on the basis of dual-energy coronary CT angiography. Radiology. 2012;264(3):700–7. https://doi.org/10.1148/radiol.12112455.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Liu, P., Wang, Y., Jin, Zy. (2020). Dual-Energy Evaluation of High Calcium Score (>400) Coronary Artery. In: Jin, Zy., Lu, B., Wang, Y. (eds) Cardiac CT. Springer, Singapore. https://doi.org/10.1007/978-981-15-5305-9_4
Download citation
DOI: https://doi.org/10.1007/978-981-15-5305-9_4
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-5304-2
Online ISBN: 978-981-15-5305-9
eBook Packages: MedicineMedicine (R0)