Abstract
Postural inaccuracies in persistent dental tasks indicated an upsurge in the prevalence of musculoskeletal disorders in dentists. The study assessed the angle parameters related to the bodily movement of upper arm (UA), lower arm (LA), wrist (W), neck (N), and trunk (T) using self-developed markerless Kinect V2 system and conventional imaging technique. Ten dentists were monitored with both techniques while performing real-time dental procedure. The agreement between the techniques was assessed using Bland–Altman at 95% bias, Pearson and concordance correlation coefficients (r1 and r2), mean difference, and percentage error. For conclusive agreement analysis, contingency coefficient (C), proportion agreement index (Po), Cohen’s kappa (k), and Mann–Whitney at 95% confidence interval were evaluated. Data from both techniques possessed strong correlations (r1 and r2 > 0.90). Cohen’s kappa (0.67) at standard Landis and Koch scale showed good agreement in RULA data. Postural analysis of slow-motion tasks like dentistry using Kinect V2 system proved as unobtrusive and efficient. This may be used by dentists to have periodic postural check.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Despite all measures taken worldwide for improvement of work environments, leading economies are facing consequences of occupational hazards. According to American Working Conditions Survey [1] and European Working Conditions Survey [2], 40.5% and 44% of workers were exposed to tiring postures, respectively, whereas 75% and 62% of workers were susceptible to repetitive arm and hand motions. All MSDs instigated or induced by work performances are concluded as WMSDs [3]. WMSDs are a serious global concern and prevalent among both developing and developed nations. In developing nations, compromising work environments have led to an alarming rise in WMSDs [4, 5].
Various studies documented in the literature worldwide have reported a high incidence of MSDs among the dental practitioners [6,7,8,9,10,11,12,13,14]. The dental profession demands precision, good visual acuity, psychomotor skills, depth perception, manual dexterity, and concentration accompanied with narrow work area (oral cavity of the patient), resulting in inflexible awkward postures for a longer duration during dental task [14, 15]. Even adoption of an optimal sitting posture, due to the little movement of joints static contraction, is there in more than 50% of body muscles. Static posture behavior makes dentists prone to MSDs like tendinitis, tenosynovitis, synovitis, and bursitis [15, 16]. Lower back problems are prevalent among dentists worldwide accompanied by problems in neck, shoulders, hand, and wrist; more than one-third required medical treatment for MSDs [17,18,19].
Movement- and posture-related data of worker is prerequisite to evaluate the vulnerability to risk factors for MSDs with the subsequent aim of ergonomic intervention [20]. Subjected to variation in the mensuration method, varieties of tools are available and are categorized as (1) self reporting, (2) direct measurements, and (3) observational [21, 22]. Mostly self-administered questionnaires, checklists, interviews, and rating scales were used in various studies investigating the prevalence of WMSDs in dentists [10, 12, 13, 23,24,25,26,27,28,29,30] and usually lead to biased results [31, 32]. Delfa et al. and Blanc et al. have used direct methods to analyze postural and biomechanical data in dentistry by making use of wearable sensors like goniometers, EMG electrodes, or markers for motion capturing in simulated dental environments [33, 34]. In actual dental work, direct methods may be difficult to implement as wearable devices usually cause discomfort and affect postural activity. The mass adoption of direct methods becomes inappropriate due to intrusive, expensive, and time-consuming nature of sensors involved [35, 36]. Also, the high contrast stickers used in marker technology may fall off during actual work [37, 38]. In dental ergonomics area, studies have been done using ergonomic evaluation by observational methods like RULA and REBA. These methods involve the judgment of bodily angles using images and video frames and thus require expert opinion for correct estimation of angles [39].
To rule out the drawbacks of above methods, elbow, shoulder, and wrist joint data from a field survey of videos during shoulder abduction in 2D was automatically picked up by using a graphic algorithm which controlled error within 12° [40]. However, to obtain body joint data in 3D, in 2013, skeletal tracking system using Kinect V1 was integrated into the RULA method for 3D motion analysis [41], DHM Jack tool, and Task Analysis toolkit module [42]. Choppin et al., discussed the accuracy of Kinect, the maximum error, proportional error, median RMSE, and systematic bias were reported as 58.2°, 1.15°, 12.6°, and 4.38°, respectively, using IPIsoft algorithm and 63.1°, 1.19°, 13.8°, and 3.16°, respectively, using NITE algorithm [43]. Kinect sensors being fully automatic, cheap, portable, non-intrusive, markerless and high frame rate technology justifies its robust applications and studies, covering health care, robotics, physical therapy, performing arts, natural user interface, virtual reality, fall detection, and 3D reconstruction [44]. K2RULA a semi-automatic software was developed which is capable of detecting awkward postures in real time using Kinect V2 [45]. Kinect V2 according to its specifications and studies conducted outperformed Kinect V1 being able to detect 25 body joints, robust to both natural or unnatural light sources and more accurate to human body skeletal tracking [46, 47]. A marker-based study using Kinect V2 as a computational tool was conducted by Weidemann et al.; upper body joint angle inclinations were highly accurate(deviation less than 7.2°) with lower accuracy in neck angle (−31° ± 9.1°) and upper body rotation across a longitudinal axis (24.0° ± 3.5°) [48]. The real-time feedback was developed by Chika Edith Mgbemena et al. which can inform the workers to change the instantaneous awkward sitting posture [49]. Yusuf et al. had captured static (lateral hand lift) and dynamic (lower arm) movement using Kinect V2 sensor, with the respective error rate of 2% and 5% [50]. The above studies establish the possibility of Kinect V2’s use in real-time application tasks and a promising tool for postural analysis.
Dental practitioners all over the world being susceptible to WMSDs need to assess their postures while working. During long-duration dental tasks, it becomes difficult to analyze the posture of the dentist and the presence of ergonomist cannot be avoided. The real-time postural evaluation of dentists, which may eliminate the need of ergonomists is a serious challenge till date. Also, ISO standard 1128-3:2007(E) can be considered as the basis to establish the workplace environment. The steady system for any workstation can be developed using depth sensors which can monitor body joint angles of a worker for an early check of exposure to WMSDs. The current study aims at examining the use of Microsoft Kinect V2 sensor in capturing the real-time postural data in dental practitioners during their practice hours. The study focuses on (1) examining the body joint angle data of dentist acquired by Kinect V2 while doing the actual dental task and its comparison with the data collected through conventional imaging technique. (2) Calculation and comparison of final RULA score from body joint data collected from both Kinect V2 sensor and imaging techniques.
Dental practitioners all over the world being susceptible to WMSDs need to assess their postures while working. During long-duration dental tasks, it becomes difficult to analyze the posture of the dentist and the presence of ergonomist cannot be avoided. The real-time postural evaluation of dentists, which may eliminate the need of ergonomists is a serious challenge till date. Also, ISO standard 1128-3:2007(E) can be considered as the basis to establish the workplace environment. The steady system for any workstation can be developed using depth sensors which can monitor body joint angles of a worker for an early check of exposure to WMSDs. The current study aims at examining the use of Microsoft Kinect V2 sensor in capturing the real-time postural data in dental practitioners during their practice hours. The study focuses on (1) examining the body joint angle data of dentist acquired by Kinect V2 while doing the actual dental task and its comparison with the data collected through conventional imaging technique. (2) Calculation and comparison of final RULA score from body joint data collected from both Kinect V2 sensor and imaging techniques.
2 Methods
2.1 Subjects
Dental practitioners and hygienists were enlisted from the regional dental institute. Subjects having any prior history of WMSDs, injuries in hands, wrists, arms, neck, back, and shoulder were excluded from the study. Ethical permission for the study was taken from Panjab University’s Ethics Committee. Ten professional dental workers (6 males and 4 females) and their patients voluntarily signed the written informed consent form for participation in study, with the disclosure for needful use of procedural photographs concealing their facial identity. To maintain the consistency of data, all the participants were checked for their dominant hand as the right hand and dental scaling with manual tools as the performing job. Participants were explained the study protocol and purpose in advance. The subjects had mean age, height, and weight of 29 ± 4 years, 162 cm, and 67 ± 9 kgs, respectively. All the dentists performed the sitting dental job for more than 15 h a week.
2.2 System Overview
The automatic data capturing software was developed using Microsoft Kinect V2 for windows, PC with windows 8.1,64 bit,8 gbRAM, Intel core i5 processor @2.2GHz. The C# (.NET framework) and Microsoft Kinect for windows SDK2.0 were used as the programming platform to capture 3D depth image and skeletal joint coordinate data. High-quality videography still camera (SONY, HDR-XR550) was used to capture image streams simultaneously while capturing depth image data. The sampling frequency of both Kinect V2 and still camera was 30 fps.
2.3 Experimental Design
2.3.1 Data Collection
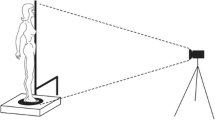
The postural data was collected from a typical dental workstation which included modern Pelton and Crane chair arrangement. The current study involved manual dental scaling task, and for achieving the current objective of capturing better body joint data (with least occlusion), the adjustment with hanging ultrasound cleaning appliance and nozzles were kept at a distant position from Kinect’s proximity. No other modification was made for the current study in dental hospital’s workstation. Dentists performed the dental cleaning task in both standing and sitting postures as per their preference. The dentists who performed the job while sitting used dental stool with backrest. The Kinect sensor was placed radially in between standard 8–9’o clock position of dental chair setup at a distance of 3.5 m from chair center and at a 1.2 m height from the ground using a tripod. The tilt angle of Kinect was kept zero as the optical axis of the sensor was parallel to the ground. The high-quality videography camera was placed at the nearest possible proximity of Kinect sensor at approximately the same position and direction. The digital clock was kept within the camera frame in a fashion that it does not disturb the dentist. To avoid the inessential body skeleton tracking of a patient’s body, the patient was asked to lie on the dental chair before the Kinect is switched on because Kinect sensor considers patient and dental chair as merged bodies or unity is unable to generate automated patient’s virtual skeleton. Dentists were instructed to stand still for once in front of Kinect for 3–4 s just before initiating the scaling task to allow Kinect to detect human body joint coordinates. The data was collected continuously for 5 min, while each dentist performed real-time dental scaling task, sitting between standard 9–11’o clock dental chair position as illustrated in Fig. 1. Both Kinect and videography camera were simultaneously initiated, and more accurate data synchronization was obtained by using digital and stop watches. The flowchart shows the procedure followed in the present study in Fig. 2. The typical RGB image perspective while recording data for the study from the Kinect and videography camera orientation is shown in Fig. 3.
2.3.2 Data Processing and Analysis
The body skeletal information is transformed into a large set of features which were fed into a software program created in Visual Studio. The recorded coordinate joint data was used to create vectors, and subsequent computation was done to calculate final angle values. C# program computed the five prime body angles(dependent variables) present at the right shoulder, right elbow, right wrist, neck, and trunk joints and were represented as angles related to UA, LA, W, N, and T (shown in Fig. 1) (Table 1).
The angle values corresponding to thirty relevant image frames from each cycle of dental scaling work were extracted. RULA method was applied for all the right side physiological features for both Kinect and image readings. Relevant values from both Kinect and conventional readings were considered after removing outlier values.
Following hypothesis were selected to assess the agreement between the results of Kinect and conventional imaging technique. Hypothesis 1: Kinect V2 data values are in agreement with data collected with the conventional method. Hypothesis 2: Final RULA score calculated using Kinect V2 data is in agreement with the RULA score calculated using conventional techniques.
To evaluate agreement among Kinect and conventional imaging technique, Bland–Altman mean difference (bias) and 95% limit of agreement(LoA) defined as bias ±1.96SD were plotted. Mean, mean difference, and standard deviation(SD) of mean difference values from both techniques related to each body angle parameter were recorded. To assess the strength of association among angle parameters recorded using both Kinect and conventional imaging techniques, Pearson correlation coefficient (r1) was evaluated and corresponding p-values were assessed to know the probability of occurrence of results. Also, to evaluate the level of agreement or disagreement among angle parameters recorded using both techniques, concordance correlation coefficients (r2) were evaluated. Percentage errors (PE) were evaluated to assess the percentage of differences between angle values for all body joints derived from both techniques.
For more concrete and conclusive agreement analysis between two sets of calculated RULA values(Kinect and imaging), nonparametric statistical tests were performed. Differences in medians of RULA scores between two techniques were assessed using Mann–Whitney U test at 95% confidence interval to test the null hypothesis: No significant difference exists in the RULA values between Kinect and imaging technique. To assess the strength of association among both systems based on final RULA scores, contingency coefficient (C) was evaluated using two-dimensional contingency tables. Proportion agreement index (PO) was calculated to check the proportion of cases for which RULA scores for both techniques agree. For the sample to sample inter-rater agreement, Cohen’s kappa coefficient (k) [51] was calculated as a quality index, using ordinal RULA scores for both recording techniques.
3 Results
Table 2 summarizes the values of mean (±SD), Bland–Altman mean difference with 95% limits of agreement, percentage errors, Pearson correlation coefficient, and concordance correlation coefficient from body joint angle data using Kinect and imaging techniques.
The graphs in Fig. 4a–e illustrates the scatter plots of each respective body joint angles data using Kinect–conventional methods (the differences along the vertical axis against the mean values along the horizontal axis). Mean difference or bias and 95% LoA values are represented as horizontal lines on each graph. Bland–Altman test indicated that the data points were evenly and closely distributed across the horizontal bias line. In most of the body angles, more than 95% of the method difference values were spotted within the defined LoA range except in W, which showed the less agreement between the methods in calculating W data. Also, comparatively higher bias value (systematic error = −2.84) recorded in the case of W indicated the systematic difference in results produced by the two methods. Wide LoA in W plot suggested the possible inaccuracy of results with one of the technique. Overestimation of joint angle values was recorded with Kinect in the case of W; observation of the graph suggested the higher existence of data points above the bias line. In case of LA proportional bias was observed, as Kinect underestimated the LA angle values when mean angle values were low and vice versa.
Body angle data (for LA, UA, W, N and T) from Kinect and imaging techniques resulted in optimally high Pearson’s (r1(298) ≥ 0.90, p < 0.001) and concordance correlation coefficients (r2(298) ≥ 0.90), indicating the significant positive correlation between both techniques.
For LA, correlation coefficients had highest values (r1(298) = 0.997, p < 0.001) and (r2(298) = 0.995) with lowest PE (3%) and mean difference (0.225°) values, inferring more association and lower differences among Kinect and imaging technique, therefore indicating the closeness in values obtained from both techniques.
For UA and N, correlation coefficient values were optimally higher (r1(298) = 0.991, p < 0.001), (r2(298) = 0.0.990) and (r1(298) = 0.951, p < 0.001), (r2(298) = 0.948) with relatively higher PE values (10.75% and 11.85%), showing Kinect data values have a good association with conventional values but with more error differences in the values.
The concrete agreement analysis between two sets of calculated RULA values (Kinect and imaging) is summarized in Table 3. The results of the Mann–Whitney test conducted came out to be statistically non-significant (z = −1.893, p > 0.05). Therefore, Mann–Whitney U test results directed to accept the null hypothesis, inferring the similarity in the RULA scores from both techniques. The value of contingency coefficient (C = 0.757) shows the existence of fairly high association among the two RULA score groups. Proportion agreement index (Po = 0.74) indicated that 74% of the total RULA values from both techniques had an agreement. Consistency among RULA values from both Kinect and imaging technique was assessed by calculating Cohen’s kappa index, k = 0.67 (p < 0.0.001), 95% CI (0.504, 0.848). The value of the kappa index was evaluated on Landis and Koch’s scale resulting in “good” agreement among both the techniques. The above results concluded the validity of Hypothesis 2: Final RULA score calculated using Kinect V2 is in agreement with the RULA score calculated using conventional techniques.
The cross-validation of results obtained from Kinect V2 and conventional technique pointed out that the values derived from Kinect V2 were close to those derived using conventional techniques.
4 Discussion
In this section, the results reported in the current study are discussed and bring light to some limitations.
4.1 Main Contributions
The present study aimed at better understanding the body kinematics of dentist while doing the dental procedure and examining the feasibility of Kinect V2 in real-time postural analysis for slow-motion tasks. To the author’s knowledge, this investigation was the first effort to use Kinect as a markerless technique to assess the dental practice ergonomically. In the current study, considerable validity of recorded spatial parameters was observed between the values of joint angle data from markerless and imaging technique.
There lies an anomaly in accuracy of data collection using imaging method while capturing orientations which require depth information (like in W) in 2D. Also, the overestimation of W angle joint data in Bland–Altman plots suggested the possible problem in the accuracy of one of the techniques. The presence of occlusions while capturing the wrist data in certain postures using Kinect might also be the responsible factor for inaccuracies. During the dental procedure, it was observed that 90% of the time hand palm was dorsiflexed which made it cumbersome to capture joint data associated with W accurately. In general, considering joint angle data except for W, no over- or underestimation of data points was observed. This may be supported by the fact that the optical axis of the Kinect sensor was kept parallel to the ground. This is in contrast with the study where overestimated body angle data was obtained [52], which may be due to the adjustment of the Kinect’s tilt angle to capture the body joint skeleton. Non-homogeneity of Kinect data in measurement error within measurement volume was reported in a separate study backing up the fact that measurement errors along with all the three coordinate axis of the Kinect may be responsible for the results with proportional error [53].
As noticed, the values of correlation coefficients for body joint angle data from Kinect and imaging technique ranged on the higher side (near to value 1) unlike the study by other authors where values of correlation coefficients ranged from 0.04 to 0.77 (Pfister et al. [54]). This may be due to the less dynamic nature of dental work procedure if compared with the highly dynamic tasks which involve walking and jogging.
In the present study, the PE values for N and UA ranged on the higher side (10.75–11.85%). Apart from recorded flexion and extension movements in N and UA, the co-existence of other anatomical movements (lateral flexion or torsion in neck and abduction or adduction in the upper arm) in certain postures may be responsible for large deviation of Kinect values from the imaging values.
The Kinect method has proved its potential for the precise spatial data recording of non-static tasks. In the current study, spatial joint angle parameters involving slow-motion dynamic dental task had an overall PE (2.45–11.85%) comparable with an overall PE (4.02–7.73%) from spatial gait parameters in another study [55], which involved the walking trials by backpack carrying school children. Conventional imaging technique was considered as the gold standard for both the current study and the study involving walking trials.
The value of the contingency coefficient (C) in the current study is lesser than the value obtained in an investigation by other authors (Manghisi et al. [45]); the plausible influential factor may be the real-time data collection in the present case study. The authors of the current study suspected the presence of occluded data while doing real-time ergonomic assessment as the deterministic aspect for resulted good agreement level (and not excellent agreement) value of Cohen’s kappa at standard Landis and Koch scale.
It appeared from the results of the current study that Kinect V2 may be considered for its use in detecting optimally correct body angles at least in less dynamically active but dexterity demanding dental procedure tasks. Further, the body angles may provide information about awkward postures in real time, and in the long run, it may be useful to prevent MSDs in dentists. The current study illuminates the idea of developing real-time posture correction feedback system, is operationally compliant with the dentists use, and may reduce the need of ergonomics expert in the routine
postural assessment. In dental studies, ergonomic aspects related to dentistry are taught theoretically in coursework, but currently there is no assessment tool to examine the postural correctness in amateur dentists like students and interns. Therefore, a warning-cum-posture assessment system may be developed to be served as a teaching aid in dental colleges, with the aim of forging young dentists habitual to recommended working postures.
4.2 Limitations
Due to methodological standardization and some acceptable shortcomings of Kinect device, results in the current study were constrained. The study was conducted in the controlled lightening environment where no other human or any extra object intervention was allowed in between the Kinect and the dentist him/herself which may have avoided further occlusions in the data. Further dentists and patients were made to follow the protocol of the study so as to be able to capture the data in a standardized format which may be difficult to follow while routine dental procedures. Without disturbing the code of conduct of dentists, the readings were taken while dentists were in their normal daily wear and laboratory coats, which may have recorded some errors in angle calculation as Kinect scans whole body surface for joint positioning. The role of working positions and isometric spinal loads in determining spine kinematics was not taken into consideration. The data recorded in the current study did not contain any overhead or extremely awkward dentist’s postures, so appropriate prevalidation of Kinect is necessary for such data collection.
5 Conclusion
In this paper, the study related to the use of Kinect V2 sensor in detecting postural data in the actual dental procedure and the variation in its results from conventional imaging methods were discussed. Considering dental work postural variation as non-frequent and non-quick, the proposed system seemed to be an effective option in the case of slow-motion real-time task assessment. Kinect data collection and assessment appeared to be quick and easier than conventional methods. Despite the reported limitations, the results of the present study are promising enough to validate the Kinect method as a viable option for ergonomic evaluation of dental workstations. Hence, keeping a check on the postural inaccuracies in dentists during work using the user-friendly and contemporary Kinect device, the long-term effect on the biomechanical aspects can be restrained.
References
Maestas, N., Mullen, K. J., Powell, D., Wachter, T. V., & Wenger, J. B. (2015). Working conditions in The United States: Results of 2015 American working conditions. United States.
Eurofound. (2016). Sixth European working conditions survey—Overview report. Luxembourg: Publications Office of the European Union.
Luttmann, A., Jäger, M., Griefahn, B., Caffier, G., Liebers, F., & Steinberg, U. (2003). Protecting workers health series No. 5. Preventing Musculoskeletal Disorders in Workplace. Retrieved from https://www.who.int/occupational_health/publications/en/oehmsd3.pdf.
Kumar, M. W., Kumar, R. A., Gnanaraj, D. (2012). RULA analysis of workers assembly workstation. Humanizing work and work environment. Ergo: Safety for All, pp. 290–295.
Jafry, T., & O’Neill, D. H. (2000). The application of ergonomics in rural development: A review. Applied Ergonomics, 31, 263–268.
Puriene, A., Janulyte, A., Musteikyte, M., & Bendinskaite, R. (2007). General health of dentists. Literature review. Stomatologija, Baltic Dental and Maxillofacial Journal, 9, 10–20.
Gandavad, A., Ramsay, J. R. E., & Burke, F. J. T. (2007). Assessment of dental student posture in two seating conditions using RULA methodology—A Pilot Study. British Dental Journal, 203, 601–605.
Chaikumarn, M. (2005). Differences in dentists’ working postures when adopting proprioceptive derivation vs. conventional concept. International Journal of Occupational Safety and Ergonomics (JOSE), 11, 441–449.
Leggat, P. A., Kedjarune, U., & Smith, D. R. (2007). Occupational health problems in modern dentistry: A review. Industrial Health, 611–621.
Garcia, P., Pinelli, C., Derceli, J., & Campos, J. (2015). Musculoskeletal disorders in upper limbs in dental students: Exposure level to risk factors. Brazilian Journal of Oral Sciences, 11(2), 148–153.
Gupta, S. (2011). Ergonomic applications to dental practice. Indian Journal of Dental Research, 22, 816–822.
Newell, T. M., Kumar, S. (2004). Prevalence of musculoskeletal disorders among orthodontists in Alberta. International Journal of Industrial Ergonomics, 33(2), 99–107.
Pargali, N., & Jowkar, N. (2010). Prevalence of musculoskeletal pain among dentists in Shiraz, Southern Iran. International Journal of Occupational and Environmental Medicine, 1(2), 69–74.
Finsen, L., Christensen, H., & Bakke, M. (1998). Musculoskeletal disorders among dentists and variation in dental work. Applied Ergonomics, 29(2), 119–125.
Durgha, K. (2014). Sakthi, Occupational hazards and its impact on quality of life of dentists. IOSR Journal of Dental and Medical Sciences, 13(7), 53–56.
Carvalho, M. V., Cavalcanti, F. I., Miranda, H. F., Soriano, E. (2006). Partial rupture of supraspinous tendon in a dentist: A case report. FIEP Bulletin, 76–131.
Doorn, J. W. (1995). Low back disability among self-employed dentists, veterinarians, physicians and physicaltherapists in The Netherlands. Acta Orthopaedica Scandinavica, 263, 1–64.
Ylipää, V., Arnetz, B., & Preber, H. (1999). Predictors of good general health, well-being, and musculoskeletal disorders in Swedish dental hygienists. Acta Odontologica Scandinavica, 57, 277–282.
Dong, H., Loomer, P., Barr, A. (2007). The effect of tool handle shape on hand muscle load and pinch force in a simulated dental scaling task. Applied Ergonomics, 38, 525–531.
Viera, E. R., Kumar, S. (2004). Working Postures: a literature review. Journal of Occupational Rehabilitation, 14(2),143–159.
David, G. C. (2005). Ergonomic methods for assessing exposure to risk factors for work-related musculoskeletal disorders. Occupational Medicine, 55(3), 190–199.
Li, G., & Buckle, P. (1999). Current techniques for assessing physical exposure to workrelated musculoskeletal risks, with emphasis on posture-based methods. Ergonomics, 42(5), 674–694.
Aljanakh, M., Shaikh, S., Siddiqui, A. A., Mansour, M. A., & Hassane, S. S. (2015). Prevalence of musculoskeletal disorders among dentists in the Ha’il Region of Saudi Arabia. Annals of Saudi Medicine, 35(6), 456–461.
Decharat, S., Phethuayluk, P., Maneelok, S. (2016). Prevalence of musculoskeletal symptoms among Dental health workers, Southern Thailand. Advances in Preventive Medicine, 5494821.
Muralidharan, D., Fareed, N., Shanthi, M. (2013). Musculoskeletal disorders among dental practitioners: does it affect practice? Epidemiology Research International, 716897(2013).
Kalappa, S., & Raghavendra, S. (2017). A study on the influence of ergonomics on the prevalence of chronic pain disorders among dentists. International Surgery Journal, 4(12), 3873–3878.
Atri, M., & Nagraj, A. (2014). Identifying musculoskeletal disorders amongst dentists—The need for the hour. International Journal of Medical Science and Public Health, 3, 730–734.
Moodley, R., & Naidoo, S. (20015). The prevalence of musculoskeletal disorders among dentists in KwaZulu-Natal. South African Dental Journal, 70(3), 98–103.
Mendegeri, V., Ramdurg, P., Kambale, S., & Gajapurad. (2014). Prevalence of musculoskeletal disorders among dentists: A Pilot study. Indian Journal of Dental Sciences, 5(6), 16–20.
Moosavia, S., Desaia, R., Hallaj, S., Sundaramb, K. K., & Hegdec, V. S. (2015). Ergonomic analysis to study the intensity of MSDs among practicing Indian dentists. In Procedia Manufacturing 3, 6th International Conference on Applied Human Factors and Ergonomics (AHFE 2015) and the Affiliated Conferences (Vol. 5, No. 6, pp. 5419–5426).
Burdorf, A., & Laan, J. (1991). Comparison of methods for the assessment of postural load on the back. Scandinavian Journal of Work, Environment & Health, 17, 425–429.
Wiktorin, C., Karlqvist, L., & Winkel, J. (1993). Validity of self-reports exposures to work postures and manual material handling. Scandinavian Journal of Work, Environment & Health, 19, 208–214.
Delfa, N. J. L., Grondin, D. E., Cox, J., Potvin, J. R., & Howarth, S. J. (2017). The biomechanical demands of manual scaling on the shoulders & neck of dental hygienists. Ergonomics, 60(1), 127–137.
Blanc, D., Farre, P., & Hamel, O. (2014). Variability of musculoskeletal Strain on dentists: An Electromyographic and goniometric study. International Journal of Occupational Safety and Ergonomics, 20(2), 295–307.
Kowalski, K., Rhodes, R., Naylor, P.-J., Tuokko, H., & MacDonald, S. (2012). Direct and indirect measurement of physical activity in older adults: A systematic review of literature. International Journal of Behavioral Nutrition and Physical Activity, 9(1), 148.
Xu, X., Gorry, M. R. W., Chou, L., Lin, J., & Chang, C. (2015). Accuracy of Microsoft Kinect for measuring gait parameters during treadmill walking. Gait Posture, 42,145–151.
Bhagwat, S., Hegde, S., & Mandke, L. (2015). Prevalence of musculoskeletal disorders among Indian dentists: A pilot survey with assessment by rapid entire body assessment. World Journal of Dentistry, 6(1), 39–44.
Kriangkrai, R., Sirimala, N., Nathamtong, S., Wintsch, S., Choden, K., & Taechasubamorn, P. (2016). Self-reported prevalence and risk factors of musculoskeletal pain in Thai dental students. International Dental Journal of Students Research, 4(3), 116–122.
McAtamney, L., & Corlett, E. N. (1993). RULA: A survey methods for the investigation of work-related upper limb disorders. Applied Ergonomics, 24(2), 91–99.
Bruno, J. L., Li, Z., Trudeau, M., Raina, S. M., & Dennerlein, J. T. (2012). A single video camera postural assessment system to measure rotation of the shoulder during computer use. Journal of Applied Biomechanics, 28, 343–348.
Haggag, H., Hossny, M., Nahavandi, S., & Creighton, D. (2013). Real time ergonomic assessment for assembly operations using kinect. In: Computer Modelling Simulation (UKSim),UKSim 15th International Conference (pp. 495–500).
Siemens. (2013). Jack and process simulate human. http://www.plm.automation.siemens.com/en_gb/products/tecnomatix/manufacturing-simulation/humanergonomics/jack.shtml.
Choppin, S., Lane, B., & Wheat, J. (2014). The accuracy of the Microsoft Kinect in joint angle measurement. Sports Technology, 7(1–2), 98–105.
Lun, R., & Wenbig, Z. (2015). A survey of applications and human motion recognition with Microsoft Kinect. Electrical Engineering & Computer Science Faculty Publications, 408.
Manghisi, V. M., Uva, A. E., Fiorentino, M., Bevilacqua, V., Trotta, G. F., & Monno, G. (2017). Real time RULA assessment using Kinect v2 sensor 2017. Applied Ergonomics, 65, 481–491.
Wang, Q., Kurillo, G., Ofli, F., & Bajcsy, R. (2015). Evaluation of pose tracking accuracy in the first and second generation of Microsoft Kinect. In Health-Care Informatics (ICHI, 2015 International Conference) (pp. 380–389). IEEE.
Zennaro, S., Munaro, M., Milani, S., Zanuttigh, P., Bernardi, A., Ghidoni, S., & Menegatti, E. (2015). Performance evaluation of 1st and 2nd generation Kinect for multimedia applications. In Multimedia Expo (ICME), 2015 IEEE International Conference (pp. 1–6). IEEE.
Wiedemann, L., Planinc, R., Nemec, I., & Kampel, M. (2015). Performance evaluation of joint angles obtained by KinectV2. In: Technologies Active-Assisted Living (TechAAL), IET International Conference (pp. 380–389). IET.
Mgbemena, C. E., Oyekan, J., Hutabarat, W., Xu, Y., & Tiwari, A. (2017). Design and implementation of ergonomic risk assessment feedback system for improved work posture assessment. Theoretical Issues in Ergonomics Science, 19(4), 431–455.
Yusuf, K. M. S. T., Nazri, A. F. A., Mustapha, G., & Mahmud, J. (2015). Analysis of static and dynamic motion accuracy for Kinect-virtual Sensei system. Journal of Engineering and Applied Sciences, 10(17), 7328–7335.
Fleis, J. L., Levin, B., & Paik, M. C. (2004). The measurement of interrater agreement. In Statistical methods rates proportions (pp. 598–626). Wiley. Retrieved from https://onlinelibrary.wiley.com/doi/abs/10.1002/0471445428.ch18.
Bhatia, V., Kalra, P., & Randhawa, J. S. (2010). Upper body postural analysis in sitting workplace environment using Microsoft Kinect V2 Sensor. In Proceedings of ICoRD 2019 Volume 2. Research into Design for a Connected World (pp. 575–586).
Dutta, T. (2012). Evaluation of the Kinect sensor for 3-D kinematic measurement in the workplace. Applied Ergonomics, 43, 645–649.
Pfister, A., West, A. M., Bronner, S., & Noah, J. A. (2014). Comparative abilities of Microsoft Kinect and Vicon 3D motion capture for gait analysis. Journal of Medical Engineering & Technology, 38, 274–280.
Gupta, I., Kalra, P., & Iqbal, R. (2017). Gait parameters in school going children using a marker-less approach. Current Science, 111(10), 1668–1675.
Acknowledgements
This study was funded by Centre of Excellence in Industrial & Product Design, Punjab Engineering College, Chandigarh, India, under National Project Implementation Unit scheme with grant number AC/TEQIP-III/MHRD/2017. The authors wish to thank the dental practitioners who volunteered and participated in the study.
Declaration of Interest Statement
The authors have no conflict of interest regarding the publication of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper
Bhatia, V., Randhawa, J.S., Jain, A., Grover, V. (2021). Comparative Analysis of Imaging and Novel Markerless Approach for Measurement of Postural Parameters in Dental Seating Tasks. In: Prakash, C., Krolczyk, G., Singh, S., Pramanik, A. (eds) Advances in Metrology and Measurement of Engineering Surfaces . Lecture Notes in Mechanical Engineering. Springer, Singapore. https://doi.org/10.1007/978-981-15-5151-2_24
Download citation
DOI: https://doi.org/10.1007/978-981-15-5151-2_24
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-5150-5
Online ISBN: 978-981-15-5151-2
eBook Packages: EngineeringEngineering (R0)