Abstract
Microbes exhibit a strong association with human beings by colonizing different parts of the body. These microbes can be either beneficial or harmful. Pathogenic microbes are known to cause serious infections in humans and in other multicellular organisms which disturb the host physiology. These pathogenic microbes have intrinsic traits which contribute to their survival under hostile conditions, evasion of host immune responses and resistance to various therapeutic agents which in turn confers them with near invincibility. Therefore, exploration of novel agents which could specifically target and kill microbes is very much on the demand. Interestingly, one such agent could be microbes themselves. Utilizing microbial components and/or microbial whole cells either to target pathogens directly or at modulating the biological fitness of the host including boosting host immune responses. In this chapter, we discuss these various modes by which microbes and their products could be employed in combating microbial infections, eventually to improve healthcare.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Diverse microbial communities establish an intimate association with the human body. This complex mixture of microbial communities encompasses high density of bacteria along with archaea, fungi, protozoa and viruses (Sommer and Bäckhed 2013). This human-microbiome interaction begins in the early stages of birth and lasts throughout life (Sommer and Bäckhed 2013). Also, upon environmental exposure microbes colonize in different parts of human body, including skin, oral cavity, gastrointestinal tract and vaginal sites (Dethlefsen et al. 2007).
Gastrointestinal tract of human harbours 10–100 trillion microbes that belong to Firmicutes and Bacteroidetes phyla (Turnbaugh et al. 2007). Gut microbes play a central role in protecting the body by contributing to intestinal homeostasis, metabolism and host immunity (Sommer and Bäckhed 2013). These gut microbes also protect the host from pathogenic microorganisms (Hooper and Macpherson 2010). It is important to note that health and disease conditions are critically driven by the balance between beneficial and pathogenic bacterial populations in addition to the host responses. Perturbations in the gut microbial community by pathogens or other factors result in dysbiosis that is associated with high risk of celiac disease, gastric cancer, autism, obesity, anorexia and Crohn’s disease (Clemente et al. 2012). Broad-spectrum antibiotics kill commensal bacteria and thus collapse the microbial community structure in the body. Overuse of antibiotics for any microbial infection not only leads to the development of antibiotic resistant microbes but also hampers the gastrointestinal microbial homeostasis which in turn becomes an etiological factor for obesity, diabetes, asthma (O’Toole and Gautam 2018). It is estimated that death toll caused by antibiotic resistance microbes will escalate to 10 million in 2050 (De Kraker et al. 2016). Therefore, there is an urgent need to substitute the present intervention strategies for efficient control of infection-borne diseases. Employing commensal microbes or probiotics or molecules derived from them in controlling diseases or infection could be an attractive strategy. Further, the recent developments in genetic engineering such as CRISPR-Cas9 systems seem to offer promise for designing improved antimicrobials. In this chapter, we summarize how microbes could be used as direct tools to tackle pathogenic microbes or as indirect tools to modulate the host responses to mitigate pathogenesis.
2 Faecal Microbial Transplantation (FMT)
As mentioned earlier, gut microbial dysbiosis contributes to the development of different disorders. Faecal microbial transplantation (FMT) is one of the approaches that is being tried as an intervention strategy to restore the microbial balance. Clinical studies using FMT to restore microbial diversity for treating Clostridium difficile-associated colitis have been proven successful (Borody et al. 2003; De Leon et al. 2013). Human intestine has a complex microbial diversity in which most of the bacterial population has not been unveiled. In fact, composition of the microbial population in healthy donors varies from individual to individual. Therefore, it is imperative to design microbial therapy employing bacterial population with proven beneficial effects to precise out treatment (Skelly et al. 2019). Once native microbiota or probiotics arrive the destination in the host body, with the newly achieved balance, an array of mechanisms are executed by the bacteria, which could impact the pathogens by direct or indirect mechanisms (Pickard et al. 2017). Delivering of microbes through FMT effectively eliminate harmful microbes by competing for nutrients and producing antimicrobial molecules (bacteriocins).
3 Effects of Beneficial Microbes Against Pathogens
3.1 Direct Effects Against Pathogens
-
In a polymicrobial community, commensal microbes compete with other microbes for niche and nutrients. Bacteria produce antibacterial molecules called bacteriocins, that are varied in structure and chemical modification, could be used as on alternate to treat antibiotic-resistant bacteria (Cotter et al. 2013). This proteinaceous bacteriocins kill the target organisms by affecting cell membrane or cell wall integrity or by modulating metabolic pathways (Hols et al. 2019). Bacteriocins are classified into class I, class II, class III and class IV based on physiochemical properties (Ahmed et al. 2017). Commensal bacteria are known to produce novel types of antibacterial molecules (Donia and Fischbach 2015) which in turn provides several clinical advantages. Donia et al. (2014) discovered 3118 biosynthetic gene clusters from the human microbial genomes, and they showed that genes encoding antibacterial molecules are found throughout the genomes and metagenomes of human microbiota. This gives an idea that commensal microbiome could be a treasure to explore novel therapeutic molecules. Rigorous studies on the natural products of commensal bacteria are being expedited due to the novel and versatile nature (Table.19.1). Recently, it was found that commensal bacteria can produce a novel class of antibiotics in which 7α-dehydroxylating bacteria utilize tryptophan as a precursor to produce 1-acetyl-β-carboline and turbomycin A antibiotics that inhibit the growth of C. difficile in the presence of secondary bile acid deoxycholic acid (Kang et al. 2019). Thus, antimicrobials of commensal bacteria seem to play a vital role in colonization resistance.
Bacteria compete with other microbes either by producing antibacterial molecules in the extracellular milieu or by delivering effector proteins into the competitors in a contact-dependent manner using type VI secretory system (T6SS) (Benz and Meinhart 2014). It is increasingly becoming apparent that T6SS is also crucially involved in the inter-bacterial competition and host-microbes interaction (Jani and Cotter 2010). Bacteria cause a detrimental effects on their competitor by delivering effector proteins such as peptidoglycan-degrading enzymes (viz. amidase/glycosidase), membrane-attacking enzymes (viz. phospholipase) and nucleic-acid-degrading enzymes (viz. DNase) through T6SS (Russell et al. 2014a). Previously, it was believed that only pathogenic microbes are attributed to have such specialized T6SS system to deliver toxic proteins. A recent study postulates that even Bacteroidetes, the most prevalent of the gut microbes, might also utilize T6SS to exhibit colonization resistance and to maintain the community structure of the commensal microbes (Russell et al. 2014b).
-
Well-known mechanisms by which commensal microbes eliminate the invading pathogens are by limiting the space and nutrients. Commensal bacteria sequester nutrients that are needed for the growth of pathogenic microorganisms, which consequently affect the growth and efficacy of the colonization of the pathogens (Kamada et al. 2013). For instance, commensal E. coli acquires the amino acid proline efficiently and impedes the growth of shiga toxin-producing E. coli O157:H7 that is well known as a food-borne pathogen (Momose et al. 2008). Maltby et al. (2013) have demonstrated that commensal E. coli HS and E. coli Nissle 1917 utilize the available sugars and restrict the access to the nutrients for pathogenic E.coli O157: H7, thereby they exhibit colonization resistance. Likewise, probiotic E.coli Nissle inhibits the colonization of Salmonella Typhimurium by acquiring iron and creates nutrient-limited conditions which ultimately impact the growth of the pathogen (Deriu et al. 2013). Similarly, commensal Mucispirillum schaedleri competes with Salmonella enterica serovar Typhimurium possibly for nitrate and formate, thereby obstructing pathogen invasion and virulence gene expression (Herp et al. 2019). Commensal-derived indole can inhibit the epithelial cell attachment of Salmonella Typhimurium (Kohli et al. 2018) and Candida albicans (Oh et al. 2012). Commensal Enterobacteriaceae and Clostridia create epithelial hypoxia by consuming available oxygen which in turn inhibit the growth of the enteric Salmonella enterica serovar Enteritidis (Litvak et al. 2019).
-
Bacteria communicate with each other through signalling molecules in order to regulate gene expression upon population density, termed as quorum sensing (QS) (Waters and Bassler 2005). Gram-positive bacteria utilize pheromone-like signalling peptides as a QS signalling molecules, whereas Gram-negative bacteria produce acyl homoserine lactones. Though QS signals are species or genus specific, autoinducer-2 (AI-2) is recognized as an interspecies communicating signal that is being produced, detected and responded across the bacterial kingdom (Bassler 2002). Pathogenic bacteria employ QS mechanism for the production of virulence factors. Many reports evidently have shown that intestinal commensal bacteria produce AI-2 molecules (Lukáš et al. 2008; Thompson et al. 2015). Hsiao et al. (2014) have shown that AI-2 of commensal Ruminococcus obeum plays an imperative role in attenuating the virulence factors of V. cholera. Recent evidence suggests that probiotic Lactobacillus sakei NR28 exhibits quorum quenching activity against enterohaemorrhagic E. coli O157:H7 by inhibiting AI-2 activity and virulence factors (Park et al. 2014). Since most of the intestinal pathogens utilize AI-2 to regulate virulence genes expression, it widens the opportunity to utilize quorum quenching compounds for therapeutic interventions. Indeed, analogues of the QS signals, competitively binding with respective receptors of the pathogen, can be manipulated to attenuate the virulence factors of the pathogens (Boopathi et al. 2017). Paharik et al. (2017) have demonstrated that autoinducing peptide (AIP) from commensal Staphylococcus caprae competitively bind with the receptors of Staphylococcus aureus which in turn reduces pathogen burden and intradermal infection. It was found that AIP of S. caprae binds with AgrC, a ligand-binding receptor protein S. aureus, which in turn affects the capability of S. aureus to defend the host immune system.
3.2 Indirect Effects Against Pathogens
In addition to the direct mechanisms, commensal microbes restrict the colonization of pathogens by indirect mechanisms: (1) stimulate the production of antimicrobial peptides of the host, (2) obstruct the translocation of pathogen into epithelial cells by restoring the function of tight junction and (3) enhance innate and adaptive immune system.
In addition to the direct mechanisms, commensal microbes restrict the colonization of pathogens by indirect mechanisms, in which commensal bacteria stimulate the production of antimicrobial peptides of the host, obstruct the translocation of pathogen into epithelial cells by restoring the function of tight junction and enhance innate and adaptive immune system.
Clostridium difficile is a Gram-positive anaerobic spore-forming bacterium which causes severe diarrhoea in the patients who had antibiotic treatments. Commensal microbiota converts the taurocholate (primary bile salt) into deoxycholate (secondary bile salt) using 7α-dehydroxylase. These secondary bile salts inhibit the germination of C. difficile spores (Buffie et al. 2015), whereas primary bile salts promote spore germination of C. difficile (Sorg and Sonenshein, 2008). It implies that the balance between primary and secondary bile salts determine the colonization of C. difficile.
3.2.1 Immunomodulatory Effects
Regulation of immune homeostasis is important to restrict colonization of pathogens. Commensal microbes enhance host immune responses by regulating the functions of macrophages, neutrophils and T cells. Following are the examples of commensal microbes mediated immune modulatory effects against pathogens:
-
Intestinal epithelial cells produce antimicrobial peptides that control intestinal homeostasis. Bifidobacterium breve NCC2950 induces the expression of antimicrobial peptide RegIIIγ, a peptidoglycan-binding C-type lectin that inhibit Gram-positive bacteria (Natividad et al. 2013).
-
Butyrate plays a key role in triggering the antimicrobial activity of the macrophages by modulating the metabolism, in which reduced mTOR kinase activity and increased LC3-mediated host defence lead to resistance against enteropathogens (Schulthess et al. 2019). Commensal-derived butyrate controls the growth of Salmonella enterica serovar Typhimurium by inducing the expression of antimicrobial calprotectin, ROS and autophagosome formation in macrophages (Schulthess et al. 2019).
-
Uptake of molecules occurs in the gastrointestinal tract through the intestinal barrier, in which tight-junction components play a key role in the transport of ions and small molecules (Vancamelbeke and Vermeire 2017). Toxins such as TcdA and TCdB of C. difficile disrupt the connection between zonula occludens-1 and actin filaments, which consequently increase the paracellular permeability (Nusrat et al. 2001). Commensal-derived butyrate diminishes intestinal inflammation and promotes intestinal barrier function in C. difficile-infected mice by activating transcription factor HIF-1 in intestinal epithelial cells, which in turn decreases the epithelial permeability and translocation of the pathogen, thereby giving protection against C. difficile toxin-induced colitis (Fachi et al. 2019).
-
Epithelial layer is covered with mucus layer that physically acts as a barrier hindering the microorganisms from accessing the cell directly (Cornick et al. 2015). Glycoproteins such as mucins are differentially expressed in the mucus layer. Pathogens such as C. difficile decrease the production of MUC2, which is an important component of the mucus layer whereas Bifidobacterium and E. coli protect the host by triggering the production of mucins (Libertucci and Young 2019).
3.2.2 Effect on Distal Organs
Recent studies have highlighted that gut microbiota do cross-talk with distantly located organs such as brain, liver, lung, bone and heart (Feng et al. 2018). Perturbations in the structure of the gut microbial community and function, caused by diet, stress or diseased condition, lead to dysbiosis that facilitates microbial-derived products to get into the circulatory system (Jacobs et al. 2017). Plethora of evidences have highlighted the protective role of gut microbiota from pulmonary diseases. For instance, the gut of the germ-free mice colonized with probiotic Bifidobacterium longum 51A protects the host from pulmonary infection by reducing the load of Klebsiella pneumoniae (Vieira et al. 2016). Similarly, commensal microbiota-administered mice have shown resistance against Streptococcus pneumoniae (Schuijt et al. 2016) and Escherichia coli K1 (Deshmukh et al. 2014). Additionally, certain bacteria also produce enzymes such as glycosidases, β-glucuronidase, azoreductases and nitroreductases that can transform procarcinogenic molecules into active carcinogens. Probiotic Bifidobacterium adolescentis SPM0212 can inhibit the functions of harmful faecal enzyme and colon cancer cell line proliferation (Kim et al. 2008).
4 Emerging Therapeutics Approaches
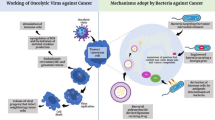
4.1 Phage Therapy
Phage therapy is the direct administration of bacteriophages into the patients in order to target a particular bacterial infection. The mode of using bacteriophages in therapy began way back in the year 1919, but the discovery of antibiotics as a potent therapeutic agent stalled the advancements of phage therapy (Altamirano and Barr 2019). However, with the rampant increase in emergence of antibiotic resistant strains, phage therapy has again gained limelight. Phages are non-living biological entities which consist of a protein capsid which encloses its nucleic acid. The strain-specific receptors help the phages determine its host to which they inject their nucleic acid, which then manipulates the bacterial machinery to produce more phage particles and eventually lyse and destroy the host cells (Lin et al. 2017). The presence of highly strain-specific receptors in the phage is one of the most important features in phage therapy.
Technological improvements have made way for the development of phage cocktails which precisely act upon an array of pathogens (Altamirano and Barr 2019). Engineering the phages to express biofilm-degrading enzymes, such as EPS depolymerase (Hughes et al. 1998) and Dispersin B (Lu and Collins 2007), has shown to help the phages to seep into the biofilm matrix and act on biofilm-based bacterial infections. Similarly bacteriophages are also engineered to overexpress endolysins which degrade the peptidoglycan layer of species-specific bacteria (Borysowski et al. 2006; Gervasi et al. 2014).
The combined use of recombinant phages with antibiotics has been experimentally shown to enhance the killing of resistant bacteria by many folds (Lu and Collins 2009). Human trials employing phage therapy conducted on clinically significant diseases like shigellosis, cholera, typhoid, chronic otitis and MDR S. aureus-induced diabetic foot ulcer have shown great success (Lin et al. 2017). Multiple studies have shown that phages do not disrupt host metabolism and microbiota and do not activate the host immune system (Chan et al. 2013). The development of phage cocktail which precisely act upon an array of pathogens has broadened phage therapy against various bacterial infections. In a recent report, a cocktail of three phages was used to completely treat a patient suffering from cystic fibrosis with disseminated Mycobacterium abscessus infection (Dedrick et al. 2019). As of date, few bacteriophages have been approved for clinical usage, while in the next few years one can witness a surge in phage-mediated therapies (Ghosh et al. 2019).
4.2 Predatory Bacteria
Bdellovibrio bacteriovorus and Micavibrio aeruginosavorus are two Gram-negative bacteria belonging to the phylum proteobacteria. These two species are gaining interest for their abilities to combat antimicrobial resistant Gram-negative bacteria (Dashiff et al. 2011) (Kadouri et al. 2013). Species Bdellovibrio attach, invade and lyse other Gram-negative bacteria, while the Micavibrio species attach, feed itself externally and divide without entering the prey bacteria. Interestingly both the predatory bacteria have shown their potential to prey on ESKAPE pathogens (Enterobacter genus, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Escherichia coli) which are a threat to human health (Negus et al. 2017). Studies have shown that predatory bacteria do not induce pro-inflammatory response in human macrophage cell lines and epithelial cell lines and show no cytotoxic response (Gupta et al. 2016; Monnappa et al. 2016). In addition, the bacteria were found to show a modest increase in the levels of pro-inflammatory cytokines in mouse upon infection through intranasal and intravenous routes. Thus, predatory bacteria could be used as an ideal biological agent to fight drug-resistant bacterial infections (Negus et al. 2017).
4.3 Fighting Pathogens Through Engineered Bacteria
Several bacterial species have been engineered to overexpress protein(s) which in turn can aid in killing or inhibiting other microbes. A potent anti-HIV protein CV-N which is originally synthesized by Nostoc ellipsosporum was made to overexpress in a commensal L. jensenii (Bolmstedt et al. 2001). The engineered L. jensenii which colonizes and forms biofilms in the vaginal mucosa was found to continuously secrete CV-N and prevent HIV transmission in macaques (Lagenaur et al. 2011). L. jensenii engineered to overexpress and deliver RANTES and C1C5 RANTES has also been proposed to be an ideal system to block HIV-1 infection (Secchi et al. 2009).
The empty envelopes of Gram-negative bacteria also called as ghosts have been found to activate broad range of cell types in innate and adaptive immunity. Different types of antigens when loaded into the cytoplasmic lumen and periplasmic space of the ghosts have demonstrated the ability of ghosts as a vaccine candidate and also as an adjuvant. The potential of bacterial ghosts as vaccines and as potential adjuvants against various diseases is reviewed elsewhere (Lubitz et al. 2009; Hajam et al. 2017).
5 Conclusion
Surging evidence suggest that microbes could be efficiently put to use as therapeutic agents to control infectious diseases. Strong evidence about the gut-living commensal bacteria governing the fate of microbial infections at different parts of the body accelerate the hope for designing better therapeutic interventions using microbial agents. Further, genetically modified beneficial microbes could be used for targeted delivery of specific molecules to tackle pathogens. Applying the principle of quorum-sensing inhibition as a therapeutic intervention is also a promising strategy to attenuate pathogenesis of the antibiotic-resistant bacteria. Thus, we surmise that microbes are endowed with potentials and hence could be explored for precision medicine for infection.
References
Ahmad V, Khan MS, Jamal QMS, Alzohairy MA, Al Karaawi MA, Siddiqui MU (2017) Antimicrobial potential of bacteriocins: in therapy, agriculture and food preservation. Int J Antimicrob Agents 49(1):1–11
Altamirano FLG, Barr JJ (2019) Phage therapy in the postantibiotic era. Clin Microbiol Rev 32(2):e00066–e00018
Bassler BL (2002) Small talk: cell-to-cell communication in bacteria. Cell 109(4):421–424
Benz J, Meinhart A (2014) Antibacterial effector/immunity systems: it’s just the tip of the iceberg. Curr Opin Microbiol 17:1–10
Birri DJ, Brede DA, Nes IF (2012) Salivaricin D, a novel intrinsically trypsin-resistant antibiotic from Streptococcus salivarius 5M6c isolated from a healthy infant. Appl Environ Microbiol 78(2):402–410
Bolmstedt AJ, O’Keefe BR, Shenoy SR, McMahon JB, Boyd MR (2001) Cyanovirin-N defines a new class of antiviral agent targeting N-linked, high-mannose glycans in an oligosaccharide-specific manner. Mol Pharmacol 59(5):949–954
Boopathi S, Vashisth R, Manoharan P, Kandasamy R, Sivakumar N (2017) Stigmatellin Y–an anti-biofilm compound from Bacillus subtilis BR4 possibly interferes in PQS–PqsR mediated quorum sensing system in Pseudomonas aeruginosa. Bioorg Med Chem Lett 27(10):2113–2118
Borody TJ, Warren EF, Leis S, Surace R, Ashman O (2003) Treatment of ulcerative colitis using fecal bacteriotherapy. J Clin Gastroenterol 37(1):42–47
Borysowski J, Weber-Dąbrowska B, Górski A (2006) Bacteriophage endolysins as a novel class of antibacterial agents. Exp Biol Med 231(4):366–377
Buffie CG, Bucci V, Stein RR, McKenney PT, Ling L, Gobourne A et al (2015) Precision microbiome reconstitution restores bile acid mediated resistance to Clostridium difficile. Nature 517(7533):205
Chan BK, Abedon ST, Loc-Carrillo C (2013) Phage cocktails and the future of phage therapy. Future Microbiol 8(6):769–783
Clemente JC, Ursell LK, Parfrey LW, Knight R (2012) The impact of the gut microbiota on human health: an integrative view. Cell 148(6):1258–1270
Cohen LJ, Han S, Huang YH, Brady SF (2017) Identification of the colicin V bacteriocin gene cluster by functional screening of a human microbiome metagenomic library. ACS infect Dis 4(1):27–32
Cornick S, Tawiah A, Chadee K (2015) Roles and regulation of the mucus barrier in the gut. Tissue Barriers 3(1–2):e982426
Cotter PD, Ross RP, Hill C (2013) Bacteriocins—a viable alternative to antibiotics? Nat Rev Microbiol 11(2):95
Dashiff A, Junka RA, Libera M, Kadouri DE (2011) Predation of human pathogens by the predatory bacteria Micavibrio aeruginosavorus and Bdellovibrio bacteriovorus. J Appl Microbiol 110(2):431–444
De Kraker ME, Stewardson AJ, Harbarth S (2016) Will 10 million people die a year due to antimicrobial resistance by 2050? PLoS Med 13(11):e1002184
De Leon LM, Watson JB, Kelly CR (2013) Transient flare of ulcerative colitis after fecal microbiota transplantation for recurrent Clostridium difficile infection. Clin Gastroenterol Hepatol 11(8):1036–1038
Dedrick RM, Guerrero-Bustamante CA, Garlena RA, Russell DA, Ford K, Harris K et al (2019) Engineered bacteriophages for treatment of a patient with a disseminated drug-resistant Mycobacterium abscessus. Nat Med 25(5):730
Deriu E, Liu JZ, Pezeshki M, Edwards RA, Ochoa RJ, Contreras H et al (2013) Probiotic bacteria reduce Salmonella typhimurium intestinal colonization by competing for iron. Cell Host Microbe 14(1):26–37
Deshmukh HS, Liu Y, Menkiti OR, Mei J, Dai N, O’leary CE et al (2014) The microbiota regulates neutrophil homeostasis and host resistance to Escherichia coli K1 sepsis in neonatal mice. Nat Med 20(5):524
Dethlefsen L, McFall-Ngai M, Relman DA (2007) An ecological and evolutionary perspective on human–microbe mutualism and disease. Nature 449(7164):811
Donia MS, Fischbach MA (2015) Small molecules from the human microbiota. Science 349(6246):1254766
Donia MS, Cimermancic P, Schulze CJ, Brown LCW, Martin J, Mitreva M et al (2014) A systematic analysis of biosynthetic gene clusters in the human microbiome reveals a common family of antibiotics. Cell 158(6):1402–1414
Fachi JL, de Souza Felipe J, Pral LP, da Silva BK, Corrêa RO, de Andrade MCP et al (2019) Butyrate protects mice from Clostridium difficile-induced colitis through an HIF-1-dependent mechanism. Cell Rep 27(3):750–761
Feng Q, Chen WD, Wang YD (2018) Gut microbiota: an integral moderator in health and disease. Front Microbiol 9:151
Gervasi T, Horn N, Wegmann U, Dugo G, Narbad A, Mayer MJ (2014) Expression and delivery of an endolysin to combat Clostridium perfringens. Appl Microbiol Biotechnol 98(6):2495–2505
Ghosh C, Sarkar P, Issa R, Haldar J (2019) Alternatives to conventional antibiotics in the era of antimicrobial resistance. Trends Microbiol 27:323
Gupta S, Tang C, Tran M, Kadouri DE (2016) Effect of predatory bacteria on human cell lines. PLoS One 11(8):e0161242
Hajam IA, Dar PA, Won G, Lee JH (2017) Bacterial ghosts as adjuvants: mechanisms and potential. Vet Res 48(1):37
Herp S, Brugiroux S, Garzetti D, Ring D, Jochum LM, Beutler M et al (2019) Mucispirillum schaedleri antagonizes Salmonella virulence to protect mice against colitis. Cell Host Microbe 25(5):681–694
Hols P, Ledesma-García L, Gabant P, Mignolet J (2019) Mobilization of microbiota commensals and their bacteriocins for therapeutics. Trends Microbiol 27:690. https://doi.org/10.1016/j.tim.2019.03.007
Hooper LV, Macpherson AJ (2010) Immune adaptations that maintain homeostasis with the intestinal microbiota. Nat Rev Immunol 10(3):159
Hsiao A, Ahmed AS, Subramanian S, Griffin NW, Drewry LL, Petri WA et al (2014) Members of the human gut microbiota involved in recovery from Vibrio cholerae infection. Nature 515(7527):423
Hughes KA, Sutherland IW, Jones MV (1998) Biofilm susceptibility to bacteriophage attack: the role of phage-borne polysaccharide depolymerase. Microbiology 144(11):3039–3047
Hyink O, Wescombe PA, Upton M, Ragland N, Burton JP, Tagg JR (2007) Salivaricin A2 and the novel lantibiotic salivaricin B are encoded at adjacent loci on a 190-kilobase transmissible megaplasmid in the oral probiotic strain Streptococcus salivarius K12. Appl Environ Microbiol 73(4):1107–1113
Jacobs MC, Haak BW, Hugenholtz F, Wiersinga WJ (2017) Gut microbiota and host defense in critical illness. Curr Opin Crit Care 23(4):257–263
Jani AJ, Cotter PA (2010) Type VI secretion: not just for pathogenesis anymore. Cell Host Microbe 8(1):2–6
Kadouri DE, To K, Shanks RM, Doi Y (2013) Predatory bacteria: a potential ally against multidrug-resistant Gram-negative pathogens. PLoS One 8(5):e63397
Kamada N, Chen GY, Inohara N, Núñez G (2013) Control of pathogens and pathobionts by the gut microbiota. Nat Immunol 14(7):685
Kang JD, Myers CJ, Harris SC, Kakiyama G, Lee IK, Yun BS et al (2019) Bile acid 7α-dehydroxylating gut bacteria secrete antibiotics that inhibit Clostridium difficile: role of secondary bile acids. Cell Chem Biol 26(1):27–34
Kim Y, Lee D, Kim D, Cho J, Yang J, Chung M et al (2008) Inhibition of proliferation in colon cancer cell lines and harmful enzyme activity of colon bacteria by Bifidobacterium adolescentis SPM0212. Arch Pharm Res 31(4):468
Kohli N, Crisp Z, Riordan R, Li M, Alaniz RC, Jayaraman A (2018) The microbiota metabolite indole inhibits Salmonella virulence: involvement of the PhoPQ two-component system. PLoS One 13(1):e0190613
Lagenaur LA, Sanders-Beer BE, Brichacek B, Pal R, Liu X, Liu Y et al (2011) Prevention of vaginal SHIV transmission in macaques by a live recombinant Lactobacillus. Mucosal Immunol 4(6):648
Libertucci J, Young VB (2019) The role of the microbiota in infectious diseases. Nat Microbiol 4(1):35
Lin DM, Koskella B, Lin HC (2017) Phage therapy: an alternative to antibiotics in the age of multi-drug resistance. World J Gastrointest Pharmacol Ther 8(3):162
Litvak Y, Mon KK, Nguyen H, Chanthavixay G, Liou M, Velazquez EM et al (2019) Commensal Enterobacteriaceae protect against Salmonella colonization through oxygen competition. Cell Host Microbe 25(1):128–139
Lu TK, Collins JJ (2007) Dispersing biofilms with engineered enzymatic bacteriophage. Proc Natl Acad Sci 104(27):11197–11202
Lu TK, Collins JJ (2009) Engineered bacteriophage targeting gene networks as adjuvants for antibiotic therapy. Proc Natl Acad Sci 106(12):4629–4634
Lubitz P, Mayr UB, Lubitz W (2009) Applications of bacterial ghosts in biomedicine, Pharmaceutical biotechnology. Springer, New York, pp 159–170
Lukáš F, Gorenc G, Kopečný J (2008) Detection of possible AI-2-mediated quorum sensing system in commensal intestinal bacteria. Folia Microbiol 53(3):221–224
Maltby R, Leatham-Jensen MP, Gibson T, Cohen PS, Conway T (2013) Nutritional basis for colonization resistance by human commensal Escherichia coli strains HS and Nissle 1917 against E. coli O157: H7 in the mouse intestine. PloS one 8(1):e53957
Momose Y, Hirayama K, Itoh K (2008) Competition for proline between indigenous Escherichia coli and E. coli O157: H7 in gnotobiotic mice associated with infant intestinal microbiota and its contribution to the colonization resistance against E. coli O157: H7. Antonie Van Leeuwenhoek 94(2):165–171
Monnappa AK, Bari W, Choi SY, Mitchell RJ (2016) Investigating the responses of human epithelial cells to predatory bacteria. Sci Rep 6:33485
Natividad JM, Hayes CL, Motta JP, Jury J, Galipeau HJ, Philip V et al (2013) Differential induction of antimicrobial REGIII by the intestinal microbiota and Bifidobacterium breve NCC2950. Appl Environ Microbiol 79(24):7745–7754
Negus D, Moore C, Baker M, Raghunathan D, Tyson J, Sockett RE (2017) Predator versus pathogen: how does predatory Bdellovibrio bacteriovorus interface with the challenges of killing gram-negative pathogens in a host setting? Annu Rev Microbiol 71:441–457
Nusrat A, von Eichel-Streiber C, Turner JR, Verkade P, Madara JL, Parkos CA (2001) Clostridium difficile toxins disrupt epithelial barrier function by altering membrane microdomain localization of tight junction proteins. Infect Immun 69(3):1329–1336
Oh S, Go GW, Mylonakis E, Kim Y (2012) The bacterial signalling molecule indole attenuates the virulence of the fungal pathogen Candida albicans. J Appl Microbiol 113(3):622–628
O’Toole RF, Gautam SS (2018) The host microbiome and impact of tuberculosis chemotherapy. Tuberculosis 113:26–29
Paharik AE, Parlet CP, Chung N, Todd DA, Rodriguez EI, Van Dyke MJ et al (2017) Coagulase-negative staphylococcal strain prevents Staphylococcus aureus colonization and skin infection by blocking quorum sensing. Cell Host Microbe 22(6):746–756
Park H, Yeo S, Ji Y, Lee J, Yang J, Park S et al (2014) Autoinducer-2 associated inhibition by Lactobacillus sakei NR28 reduces virulence of enterohaemorrhagic Escherichia coli O157: H7. Food Control 45:62–69
Pickard JM, Zeng MY, Caruso R, Núñez G (2017) Gut microbiota: role in pathogen colonization, immune responses, and inflammatory disease. Immunol Rev 279(1):70–89
Pujol A, Crost EH, Simon G, Barbe V, Vallenet D, Gomez A, Fons M (2011) Characterization and distribution of the gene cluster encoding RumC, an anti-Clostridium perfringens bacteriocin produced in the gut. FEMS Microbiol Ecol 78(2):405–415
Russell AB, Peterson SB, Mougous JD (2014a) Type VI secretion system effectors: poisons with a purpose. Nat Rev Microbiol 12(2):137
Russell AB, Wexler AG, Harding BN, Whitney JC, Bohn AJ, Goo YA et al (2014b) A type VI secretion-related pathway in Bacteroidetes mediates interbacterial antagonism. Cell Host Microbe 16(2):227–236
Salomon RA, Farías RN (1992) Microcin 25, a novel antimicrobial peptide produced by Escherichia coli. J Bacteriol 174(22):7428–7435
Schuijt TJ, Lankelma JM, Scicluna BP, de Sousa e Melo F, Roelofs JJ, de Boer JD et al (2016) The gut microbiota plays a protective role in the host defence against pneumococcal pneumonia. Gut 65(4):575–583
Schulthess J, Pandey S, Capitani M, Rue-Albrecht KC, Arnold I, Franchini F et al (2019) The short chain fatty acid butyrate imprints an antimicrobial program in macrophages. Immunity 50(2):432–445
Secchi M, Xu Q, Lusso P, Vangelista L (2009) The superior folding of a RANTES analogue expressed in lactobacilli as compared to mammalian cells reveals a promising system to screen new RANTES mutants. Protein Expr Purif 68(1):34–41
Skelly AN, Sato Y, Kearney S, Honda K (2019) Mining the microbiota for microbial and metabolite-based immunotherapies. Nat Rev Immunol 19:1
Sommer F, Bäckhed F (2013) The gut microbiota—masters of host development and physiology. Nat Rev Microbiol 11(4):227
Sorg JA, Sonenshein AL (2008) Bile salts and glycine as co germinants for Clostridium difficile spores. J Bacteriol 190(7):2505–2512
Thompson JA, Oliveira RA, Djukovic A, Ubeda C, Xavier KB (2015) Manipulation of the quorum sensing signal AI-2 affects the antibiotic-treated gut microbiota. Cell Rep 10(11):1861–1871
Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI (2007) The human microbiome project. Nature 449(7164):804
Vancamelbeke M, Vermeire S (2017) The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol 11(9):821–834
Vieira AT, Rocha VM, Tavares L, Garcia CC, Teixeira MM, Oliveira SC et al (2016) Control of Klebsiella pneumoniae pulmonary infection and immunomodulation by oral treatment with the commensal probiotic Bifidobacterium longum 51A. Microbes Infect 18(3):180–189
Waters CM, Bassler BL (2005) Quorum sensing: cell-to-cell communication in bacteria. Annu Rev Cell Dev Biol 21:319–346
Zipperer A, Konnerth MC, Laux C, Berscheid A, Janek D, Weidenmaier C et al (2016) Human commensals producing a novel antibiotic impair pathogen colonization. Nature 535(7613):511
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Seenivasan, B., Prakash, C.M., Janakiraman, V. (2020). Fighting Microbes with Microbes. In: Sharma, S., Sharma, N., Sharma, M. (eds) Microbial Diversity, Interventions and Scope. Springer, Singapore. https://doi.org/10.1007/978-981-15-4099-8_19
Download citation
DOI: https://doi.org/10.1007/978-981-15-4099-8_19
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-4098-1
Online ISBN: 978-981-15-4099-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)