Abstract
There is limited understanding of the molecular pathogenesis of thymic epithelial tumors challenging the development of targeted therapies. These tumors exhibit chromosomal copy number alterations that increase in frequency and complexity with increasing aggressiveness of the histological subtype. They show low somatic mutation loads and recurrent mutations have been identified in a very limited number of genes, most commonly GTF2I. High-throughput studies have identified significant genomic and epigenomic differences among the different histological subtypes of thymomas, paving the way for a better understanding of tumorigenesis and progression. This chapter provides a concise overview of molecular genetic alterations of potential clinical significance.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
12.1 Introduction
Integrated genomic analyses of thymic epithelial tumors (TETs) demonstrate significant genetic and molecular heterogeneity among the different histological subtypes [1]. Type A, type AB thymomas, type B thymomas, and thymic carcinomas segregate into distinct genetic/molecular entities on multiplatform omics studies with differences in the loci and frequency of their chromosomal copy number alterations, recurrent gene mutations, miRNA profiles, and, more recently, DNA methylation patterns. Gene fusions and expression of viral/bacterial antigens have not been identified in these tumors [1]. Overall, there is limited understanding of the molecular pathogenesis of thymic epithelial tumors and successful targeted therapies are yet to be discovered. In this chapter, we highlight select molecular genetic features of diagnostic, prognostic, or potential therapeutic significance in TETs.
12.2 Recurrent Gene Mutations in Thymic Epithelial Tumors
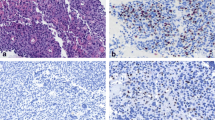
Thymic epithelial tumors harbor one of the lowest rates of somatic mutations among adulthood onset cancers with estimated tumor mutation burden of approximately 0.48 mutations per mega base [1]. Whole genome sequencing studies have identified recurrent mutations in a very limited number of genes (Fig. 12.1), the most frequent being the General Transcription Factor 2I (GTF2I) gene, point mutations of which occur in ~39% of all TETs [1]. Recurrent mutations of genes involved in the EGFR signaling pathway such as RAS family, PIK3CA, AKT, EGFR, and TP53, also occur, albeit at much lower frequencies [1].
12.2.1 GTF2I (General Transcription Factor 2I) Mutations
-
GTF2I is localized on chromosomal region 7q11.23 and encodes for members of the transcription factor IIi, a group of ubiquitously expressed proteins involved in diverse signaling pathways.
-
Mutations are most frequent in type A (82–100%) and type AB (70–74%) thymomas, less common in type B thymomas (20–30%) and thymic carcinoma (7–8%) [1, 2].
-
Characterized by a missense mutation in exon 15 at a single codon (L424H) resulting from T>A nucleotide substitution (Fig. 12.2) [3].
-
Highly specific for thymic epithelial tumors; rare GTF2I mutations described in tumors other than thymomas involve other codons [1].
-
GTF2I mutant tumors show higher expression of genes involved in cell morphogenesis, receptor tyrosine kinases, retinoic acid receptors, neuronal processes, and WNT and SHH signaling pathways [1].
-
GTF2I mutation status not associated with myasthenia gravis [1].
-
Within individual histological subtypes, GTF2I mutant tumors show better outcomes as compared to those wild type [4].
12.2.2 RAS Mutations
-
Activating mutations in HRAS (codon 12, 13, 117), NRAS (codon 61), or KRAS are the second most prevalent gene mutations in TETs [1].
-
HRAS mutations reported predominantly in type A thymomas [1, 5, 6].
-
KRAS and NRAS mutations described in type B2 thymomas and thymic carcinomas [2].
12.2.3 TP53 Mutations
-
Rare, mainly reported in thymic carcinomas and some type B thymomas [1, 2, 5].
-
All mutations are pathogenic loss of function mutations.
12.2.4 KIT Mutations
-
Very rare, detected exclusively in thymic carcinomas (~7% incidence).
-
Reported KIT mutations include V560 deletion in exon 11, H697Y mutation in exon 14, L576P mutation in exon 11, and D820E mutation in exon 17, of which all except the last predict sensitivity to tyrosine kinase inhibition [7].
-
KIT mutations do not correlate with KIT protein overexpression which is seen in more than 75% of thymic carcinomas [8].
12.2.5 Others
-
EGFR mutations are consistently absent in thymomas and very rarely described in thymic carcinomas [5] despite frequent EGFR protein overexpression and EGFR gene amplification [8]; thymic epithelial tumors generally do not respond to EGFR tyrosine kinase inhibitors [8].
-
Mutations in other genes involved in EGFR signaling, namely, AKT1 and PIK3CA, have been reported in type B3 thymomas and thymic carcinomas [5].
-
Rare example of a thymic carcinoma with microsatellite instability due to MLH1 somatic mutation and high tumor mutation burden has been reported [1].
12.3 Chromosome Copy Number Alterations
Copy number gains and losses of multiple chromosomal regions are well described in thymic epithelial tumors with the frequency and complexity of the alterations increasing with the aggressiveness of the histological type (Fig. 12.1). The biological significance of a majority of these alterations is, however, yet to be determined.
12.3.1 6q25.2-25.3 Loss of Heterozygosity
-
Observed in most types of thymomas including thymic carcinomas.
-
FOXC1, a gene encoding for a transcription factor involved in normal thymus development, is located at this locus and is implicated as a tumor suppressor in the development of thymic epithelial tumors.
-
Tumors with reduced m-RNA and protein expression levels of FOXC1 associate with poor prognosis [9].
12.3.2 CDKN2A/B Alterations
12.4 Epigenomic Alterations
-
Many miRNAs have been found to be differentially expressed in various histological subtypes of thymic epithelial tumors [11].
-
A large microRNA cluster on chr19q13.42 activating the PI3K pathway has been identified as the transcriptional hallmark of type A and AB thymomas and is a potential actionable target [12].
-
Altered expression levels of specific miRNAs have been correlated with tumor pathogenesis and prognosis in TETs [8, 13, 14].
-
Recent studies have identified significant differences in the DNA methylation patterns among normal thymus, type A thymoma, type B thymoma, and thymic carcinoma with diagnostic and prognostic connotations [15, 16].
References
Radovich M, Pickering CR, Felau I, Ha G, Zhang H, et al. The integrated genomic landscape of thymic epithelial tumors. Cancer Cell. 2018;33:244–58.
Strobel P, Marx A, Badve S, Chan JKC, Chen G, Detterbeck F, et al. Thymomas Type A thymoma, including atypical variant. In: Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG, editors. WHO classification of tumours of lung, pleura, thymus and heart. 4th ed. Lyon: IARC; 2015. p. 187–92.
Petrini I, Meltzer PS, Kim IK, Lucchi M, Park KS, Fontanini G, et al. A specific missense mutation in GTF2I occurs at high frequency in thymic epithelial tumors. Nat Genet. 2014;46:844–9.
Feng Y, Lei Y, Wu X, Huang Y, Rao H, Zhang Y, Wang F. GTF2I mutation frequently occurs in more indolent thymic epithelial tumors and predicts better prognosis. Lung Cancer. 2017;110:48–52.
Sakane T, Murase T, Okuda K, Saida K, Masaki A, Yamada T, et al. A mutation analysis of the EGFR pathway genes, RAS, EGFR, PIK3CA, AKT1, and BRAF, and TP53 gene in thymic carcinoma and thymoma type A/B3. Histopathology. 2019 Jun 10;75(5):755–66. https://doi.org/10.1111/his.13936.
Enkner F, Pichlhöfer B, Zaharie AT, Krunic M, Holper TM, Janik S, et al. Molecular profiling of thymoma and thymic carcinoma: genetic differences and potential novel therapeutic targets. Pathol Oncol Res. 2017;23:551–64.
Girard N, Shen R, Guo T, Zakowski MF, Heguy A, Riely GJ, et al. Comprehensive genomic analysis reveals clinically relevant molecular distinctions between thymic carcinomas and thymomas. Clin Cancer Res. 2009;15:6790–9.
Rajan A, Girard N, Marx A. State of the art of genetic alterations in thymic epithelial tumors. J Thorac Oncol. 2014;9:S131–6.
Petrini I, Wang Y, Zucali PA, Lee HS, Pham T, Voeller D, Meltzer PS, Giaccone G. Copy number aberrations of genes regulating normal thymus development in thymic epithelial tumors. Clin Cancer Res. 2013;19:1960–71.
Aesif SW, Aubry MC, Yi ES, Kloft-Nelson SM, Jenkins SM, Spears GM, Greipp PT, Sukov WR, Roden AC. Loss of p16(INK4A) expression and homozygous CDKN2A deletion are associated with worse outcome and younger age in thymic carcinomas. J Thorac Oncol. 2017;12:860–71.
Ganci F, Vico C, Korita E, Sacconi A, Gallo E, Mori F, et al. MicroRNA expression profiling of thymic epithelial tumors. Lung Cancer. 2014;85:197–204.
Radovich M, Solzak JP, Hancock BA, Conces ML, Atale R, Porter RF, et al. A large microRNA cluster on chromosome 19 is a transcriptional hallmark of WHO type A and AB thymomas. Br J Cancer. 2016;114:477–84.
Bellissimo T, Ganci F, Gallo E, Sacconi A, Tito C, De Angelis L, et al. Thymic epithelial tumors phenotype relies on miR-145-5p epigenetic regulation. Mol Cancer. 2017;16:88. https://doi.org/10.1186/s12943-017-0655-2.
Wei J, Liu Z, Wu K, Yang D, He Y, Chen GG, Zhang J, Lin J. Identification of prognostic and subtype-specific potential miRNAs in thymoma. Epigenomics. 2017;9:647–57.
Bi Y, Meng Y, Niu Y, Li S, Liu H, He J, et al. Genome-wide DNA methylation profile of thymomas and potential epigenetic regulation of thymoma subtypes. Oncol Rep. 2019;41:2762–74.
Li S, Yuan Y, Xiao H, Dai J, Ye Y, Zhang Q, et al. Discovery and validation of DNA methylation markers for overall survival prognosis in patients with thymic epithelial tumors. Clin Epigenet. 2019;11:38. https://doi.org/10.1186/s13148-019-0619-z.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Nambirajan, A., Singh, V., Jain, D. (2020). Molecular Pathology of Thymic Epithelial Tumors. In: Jain, D., Bishop, J.A., Wick, M.R. (eds) Atlas of Thymic Pathology. Springer, Singapore. https://doi.org/10.1007/978-981-15-3164-4_12
Download citation
DOI: https://doi.org/10.1007/978-981-15-3164-4_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-3163-7
Online ISBN: 978-981-15-3164-4
eBook Packages: MedicineMedicine (R0)