Abstract
Colorectal cancer (CRC) is one of the most frequent malignancies, causing human deaths in large numbers around the world. It can be prevented by using chemotherapeutic drugs; however, the available drugs have shown systemic toxicity and drug resistance, which makes the treatment a challenging issue. The use of flavonoid-rich sources may effectively reduce the risk of colorectal cancer. Orientin, a C-glycosyl flavonoid exists in diverse medicinal flora, such as Aspalathus linearis, Ocimum tenuiflorum, Passiflora, and Phyllostachys species, and it has been shown to have beneficiary effects in treating cancers, cardiovascular diseases, and neurodegenerative disorders. Recent preclinical validation studies on orientin have evidently shown its anti-carcinogenic effect against human colorectal adenocarcinoma cells and carcinogen-induced CRC albino Wistar rat models. Orientin reinstates the antioxidants to put forth their scavenging mechanism and limits the activation of phase 1 enzymes. Orientin induces mitochondrial intrinsic apoptosis in CRC cells, and thereby actively interrupt cell proliferation and inflammatory signaling pathways without disturbing the normal tissue. Research reports have reported the attenuating effects of orientin on aberrant crypt foci progression in cancer-bearing animal, and it results in a significant suppression of pre-neoplasia to malignant neoplasia transformation. Orientin also suppresses NF-κB and the associated inflammatory cytokines, and thereby ameliorates inducible nitric oxide synthase and cyclooxygenase-2 expression in 1,2-dimethylhydrazine rat models. Thus, this chapter emphasizes the therapeutic effects of flavonoids with a special focus on orientin against CRC. Also, it summarizes our understandings about the molecular mechanisms behind orientin-mediated cancer prevention.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1.1 Introduction
Chemoprevention involves the inhibition or delay in the development of neoplasia by interrupting the instigation of neoplasia as well as transformation before malignancy. Colorectal cancer is probably a preventable cancer. The chemoprevention of colorectal cancer (CRC) has been the spotlight of research for three decades, which intends to thwart or delay the commencement of cancer through the deterioration or anticipation of colonic adenomas (Ricciardiello et al. 2016). Chemotherapy is highly recommended for colorectal cancer patients as palliative and adjuvant chemotherapy. It also depends on the tumor staging of CRC. Adjuvant chemotherapy is optional for patients under the stage III and in some cases for stage II patients with a chance of recurrence after the surgery. Palliative chemotherapy is optional for the stage IV patients, when the cancerous cells spread from the colon to other organs and tissues that are even far apart. 5-Fluorouracil, irinotecan, capecitabine, oxaliplatin, tipiracil, and trifluridine are some of the common chemotherapeutic agents that are used against CRC (Idrees and Tejani 2019; Akhtar and Swamy 2018).
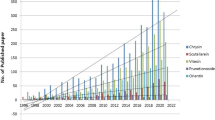
A huge number of chemopreventive agents demonstrated promising results in preclinical models; however clinical trials have succumbed to contradictory outcomes. The detrimental effects of some of the clinically proven antitumor compounds boost up death cases and accentuate a vital need for novel and nontoxic chemopreventive agents (Youns and Hegazy 2017; Bhatia and Nair 2018; Roy et al. 2018). Many known natural compounds are notorious to exert significant inhibitory action against aberrant signaling pathways involved in carcinogenesis. Furthermore, the natural compounds can be obtainable readily. They are cost-effective and harmless with both protective and health-giving potential against cancers (Arivalagan et al. 2015; Bhatia and Nair 2018). The compounds of natural origin, such as dietary agents, have been of immense interest due to the development of novel and innovative therapeutic agents for cancer (Karthi et al. 2016; Tuorkey 2016; Roy et al. 2018). In this regard, medicinal plants have an immense potential of providing natural agents, i.e., secondary metabolites that are effective in treating several types of cancers. Among plant-derived metabolites, flavonoids are found to have several medicinal importance (Chang et al. 2018; Anwar et al. 2019; Jain et al. 2019). Flavonoids like umbelliferone, luteolin, orientin, and eriodictyol have been shown to have considerable antiproliferative activities against cancerous cells. Reports have shown the attenuating effects of orientin on aberrant crypt foci (ACF) progression in cancer-bearing animal, and it results in a significant suppression of pre-neoplasia to malignant neoplasia transformation (Muthu et al. 2016; Mariyappan et al. 2017; Thangaraj et al. 2018). Orientin has also been shown to suppress NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) and the associated inflammatory cytokines and thereby ameliorates inducible nitric oxide synthase and cyclooxygenase-2 expression in 1,2-dimethylhydrazine rat models (Hamiza et al. 2012a, b; Thangaraj et al. 2018). Thus, this chapter emphasizes the therapeutic effects of flavonoids with a special focus on orientin against CRC. Also, it summarizes our understandings about the molecular mechanisms behind orientin-mediated cancer prevention.
1.2 Flavonoid’s Role in Cancer Prevention
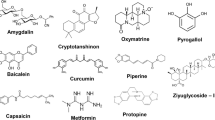
Flavonoids possess the potential of regulating multiple carcinogenic processes, such as apoptosis, angiogenesis, tumor differentiation, and cell proliferation. The flavonoid-induced alterations in kinase activity have a strong relationship with apoptosis, tumor cell proliferation, and invasion. Some of the dietary flavonoids have displayed in vivo antitumor activity and repress inflammation, proliferation, vascularization, and metastasis (Kumar and Pandey 2013; Panche et al. 2016; Tungmunnithum et al. 2018). Epidemiological studies on colon cancer proposed that some flavonoids that prevent colon cancer may enhance therapeutic efficiency by regulating colon tumor cell proliferation and survival signaling pathways (Zamora-Ros et al. 2015; Thangaraj et al. 2018). Flavonoids block several steps in carcinogenesis, namely tumor cell transformation, invasion, and metastasis (Chahar et al. 2011). A positive correlation exists between a flavonoid-rich diet and lowers the risks of colon cancer. Several flavonoids, such as umbelliferone, luteolin, and eriodictyol have been shown to exhibit superior inhibitory activities against colorectal cancer cells (Manju and Nalini 2010; Muthu et al. 2016; Mariyappan et al. 2017). Naturally available flavonoids most commonly exist as O- or C-glycosides. C-Glycosylflavones are the major class of flavonoids, which imparts the dark-yellow color to flowers of Leguminosae family members. C-Glycosides are well known for their diverse pharmacological potentials, including antioxidant, antiinflammatory, antimicrobial, and antitumor activities.
1.3 About Orientin
1.3.1 Chemistry
The IUPAC name of orientin is 2-(3,4-dihydroxyphenyl)-5,7-dihydroxy-8-[(2S,3R,4R,5S,6R)-3,4,5-trihydroxy-6-(hydroxymethyl)oxan-2-yl]chromen-4-one. Orientin is a water-soluble C-glycosyl flavonoid with the molecular formula C21H20O11, and its molecular weight is 448.38 g/mol. In general, C-glycosyl flavonoids possess C6–C3–C6 flavone skeleton, in which two aromatic rings are attached by three carbons cyclized with oxygen, having one to several glucoside units. Orientin has a 15-carbon skeleton, consisting of two phenyl rings (A and B); in specific O-phenolic hydroxyl group at 3′ of B ring and a heterocyclic ring exemption of a C-glycosides linked to glucose of the A ring (An et al. 2015). It comprises phenol groups alongside one ketone group and two ether groups. It is the 8-C glucoside of luteolin, substituted by a β-D-glucopyranosyl moiety at position 8.
1.3.2 Natural Occurrence
Several medicinal plants are the source of orientin. Some of the most widely explored medicinal plants for orientin include Ocimum sanctum (holy basil) (Devi et al. 2004), Aspalathus linearis (rooibos tea) (Koeppen et al. 1962), Phyllostachys nigra (bamboo leaves), Passiflora edulis (passion flowers, juice and peel of passion fruit), Trollius chinensis Bunge (Golden Queen), Linum usitatissimum (flax) (Dubois and Mabry 1971), Jatropha gossypifolia (bellyache bush), Commelina communis (dayflower) (Shibano et al. 2008), Euterpe oleracea Mart. (acai palm) (Gallori et al. 2004), Ascarina lucida (Soltis and Bohm 1982), Roscoea capitata, Celtis africana (white stinkwood) (Perveen et al. 2011), Croton zambesicus (lavender croton) leaves (Wagner et al. 1970), Cajanus cajan (pigeon pea) leaves (Pal et al. 2011), Thlaspi arvense (field penny-cress) (Pang et al. 2013), Fagopyrum esculentum (buckwheat) (Krahl et al. 2008), Trigonella foenum-graecum L. (fenugreek) oils (He et al. 2014), Clinacanthus nutans (Sabah snake grass) leaves (Chelyn et al. 2014), and Polygonum orientale L. (Li et al. 2017a).
1.3.3 Pharmacological Properties
Orientin has been testified to possess numerous medicinal properties, such as antiaging, antiviral, antibacterial, antiinflammation, cardioprotective, antinociceptive, radioprotective, and neuroprotective effects. Orientin inhibits esophageal cancer (EC-109) cell development in a time-dependent and dose-dependent way. It has been found to downregulate the anti-apoptotic B-cell lymphoma 2 (Bcl-2) expression and induce early apoptosis in EC-109 cells. Orientin was found to have higher antitumorigenic effect, when compared to vitexin (an apigenin flavone glycoside). The researchers have doubted on the associated OH-groups at the 3′- and 4′-position of the B ring in orientin for the increased effect. Due to the presence of a single OH-group at the 4′-position of the B ring in vitexin, its was believed to be less effective (An et al. 2015). Orientin inhibited the multiplication of HeLa (cervical cancer) cells in a concentration-dependent way and stimulated apoptosis. It reduced anti-apoptotic Bcl-2 and enhanced pro-apoptotic Bax (bcl-2-like protein 4) protein levels in HeLa cells. Also, it instigated the proteolytic stimulation of protease enzymes, i.e., caspases (Guo et al. 2014). Orientin induces apoptosis and inhibited the proliferation of breast cancer (MCF-7) cells in a time- and dose-dependent way (Czemplik et al. 2016). However, so far, none of the information validates the influence of orientin against CRC. Further, the precise molecular mechanisms of action of cell inhibitory activities induced by orientin still remain unclear.
1.4 Experimental Colorectal Carcinogenesis
1.4.1 HT29 (Human Colorectal Adenocarcinoma) Cell Line
HT29 is a human colon adenocarcinoma with epithelial morphology. This cell line was firstly obtained from a Caucasian woman (aged 44 years) suffering from a cancer of the colon (Fogh and Trempe 1975). HT29 cells contain unique features, such as microvilli, microfilaments, lipid droplets, smooth and rough endoplasmic reticulum with free ribosomes, large vacuolated mitochondria with dark granules, and few primary and many secondary lysosomes (Martínez-Maqueda et al. 2015). These cells consume high levels of glucose, and hence in vitro growth of these cells needs a medium containing elevated levels of glucose. They propagate as a multi-layer of nonpolarized cells under standard conditions. After the treatment with inducers, these cells can be modulated to express various paths of absorptive cell differentiation, such as cell flattening, apical surfaces with brush border development, and formation of tight junctions among the adjoining cells. These intestinal cells are pluripotent and widely used to study cell differentiation mechanisms (Martínez-Maqueda et al. 2015). The p53 (a cellular tumor protein) antigen is overproduced in these cells. HT29 secretes pro-inflammatory cytokines, namely, tumor necrosis factor-α (TNF α) and interleukins (IL-1β and IL-6); chemokines (e.g., interferon-γ and IL-8); transforming growth factors (TGF-α and TGF-β); pro-angiogenic factors like vascular endothelial growth factor (VEGF) and IL-15; and immune-modulatory cytokines, such as granulocyte-macrophage colony-stimulating factor (GM-CSF), granulocyte colony-stimulating factor (GCSF), and IL-3 (Desai et al. 2013).
Orientin expressively inhibits the cell survival of HT29 in a concentration-dependent way. Further, microscopic interpretations suggested the cell shrinking from its polyhedral origin, membrane blebbing, round off, and cells in detached forms (Karthi et al. 2016). The oxidative stress-induced intracellular ROS (reactive oxygen species) generation in tumor cells serves to be one of the possible therapeutic strategies for combating CRC. Excessive generation of ROS may severely damage the genome and proteins, resulting to promote apoptosis (Han et al. 2013). Orientin triggers dose-dependent intracellular ROS generation extensively.
1.4.2 Chemically Induced Animal Models
Chemical carcinogens are extensively used to induce colonic epithelial lesions similar to human CRC. They include aromatic amines, 1,2-dimethylhydrazine (DMH), heterocyclic amines, azoxymethane (AOM), and alkylnitrosamide compounds. These carcinogens can be readily verified for their therapeutic effects in model animals of diverse genetic conditions, and the human CRC pathogenesis can be initiated successfully (De Robertis et al. 2011). The anticancer efficacy of chemopreventive agents is generally tested against carcinogen-induced preclinical models. The rodents (rat/mouse) are commonly established animal models of colon carcinogenesis. This is because their physiology is similar to humans. Also the cancer formation is rapid and reproducible and there is a possibility of studying adenoma-carcinoma sequences (Muthu et al. 2016).
1.4.2.1 DMH-Induced Experimental Colon Carcinogenesis
The procarcinogen 1,2-dimethylhydrazine dihydrochloride (DMH) was extensively used to stimulate colon tumors in rodents. It mimics human colon carcinoma in epithelial origin, morphology, anatomy, histology and tumor characteristics, thereby acting as an ultimate experimental model for chemoprevention studies (Manju and Nalini 2005; Nirmala and Ramanathan 2011; Muthu and Vaiyapuri 2013). DMH induced the transformation of pre-neoplastic aberrant crypt foci into adenomas and adenocarcinomas. DMH and its inter-metabolites (AOM and MAM) are a set of man-made composites with the general structure of cycasin (Liu et al. 2015). DMH uptake is threefold higher in the colorectal cells in contrast to the enterocytes. The cancer-causing effect of DMH occurs with a single dosage of injection or by giving a series of injections after every week. DMH injected at a dose between 10 and 20 mg/kg body weight (BW) produces adenomas and adenocarcinomas of the colon in rodents. After the administration, the malignant lesion is formed from the non-dysplastic mucosa, and later it completely develops within 4 to 30 weeks. About 80% of the treated mice can develop adenocarcinomas even when a lesser dose of drugs are administered (Machado et al. 2016). Injecting a small dosage (10 mg/kg) of dimethylhydrazine will lead to colorectal cancer development in rats with a latency duration of 1–2 years (Banerjee and Quirke 1998). The preneoplastic lesions namely the aberrant crypt foci (ACF) are the earliest marker of future neoplastic development that appears after exposing DMH for 14 days (Kilari et al. 2016).
1.4.2.2 Metabolism of DMH
DMH undergoes dehydrogenation in the liver and is metabolically activated to azoxymethane (AOM) and methylazoxymethanol (MAM) (Manju and Nalini 2010). Generally, DMH do not act as carcinogenic agent. However, it is metabolically activated (including N-oxidation and hydroxylation) into DNA reactive metabolites and exhibits its tumorigenic potential (Qi et al. 2015). The highly unstable MAM with a half-life of 12 h is metabolized further to form an active electrophilic methyldiazonium glucuronide by NAD + -dependent dehydrogenase. The methyldiazonium ion which has the capability to alkylate macromolecules excretes via bile and blood to reach the colonic lumen.
Cytochrome P450 enzymes are involved in the bioactivation of procarcinogens as they interfere with the polar functional groups via hydrolysis and redox mechanisms. The phase 2 enzymes, such as glutathione S-transferase (GST), N-acetyltransferase (NAT), DT-diaphorase (DTD), UDP-glucuronosyltransferase (UGT), and sulfotransferase (SULT), detoxify upon conjugation (Beyerle et al. 2015). Cytochrome P450-dependent monooxygenases (phase 1 enzymes) carry out a reaction to introduce –OH groups to produce methyldiazonium ions, which are highly reactive in nature, and this in turn alkylates DNA bases. The strong nucleophilic methyldiazonium ions interact with nucleotide bases to yield adducts. Both N7-methylguanine and O6-methylguanine induce the genetic mutations and tumor formation (Megaraj et al. 2014). O6-Methylguanine induces GC to AT transitions and k-ras protooncogene mutations in DMH-induced colorectal carcinogenesis. Phase 2 enzymes, such as GST and DTD, are known to detoxify the electrophilic intermediate compounds (Giftson et al. 2010).
1.5 Orientin Against Colon Cancer in Different Ways
1.5.1 Body Weight, Growth Rate, and Polyp’s Incidence
Body weight and growth rate typically controls the carcinogenicity rate in carcinogen-induced investigational animals (Manju and Nalini 2005). Loss in body weight in addition to growth rate in DMH alone induced rats could be because of increased cancer burden, lack of appetite followed by the higher incidence of polyps driven cachexia and anorexia (Vinothkumar et al. 2014a). Orientin increases the body weight despite the transformation induced by DMH, owing to their capability to reinstate the metabolic deregulation. The plant metabolites have been proven to gain body weight by restraining the cancer-causing agent-induced tumorigenicity and diminishing the incidence of polyps (Selvam et al. 2009).
1.5.2 Lipid Peroxidation and Antioxidant Status
Antioxidant and lipid peroxidation levels are anticipated to be the notorious markers for ascertaining the peril of oxidative damage-induced tumorigenesis (Thangaraj et al. 2018; Muthu and Vaiyapuri 2013). The significant increase in circulatory thiobarbituric acid reaction substances (TBARS) by the high ROS production and membrane crumbling leads to the transformation of epithelial cells (Perše 2013). Tumors acquire favorable conditions and proliferate rapidly in DMH-exposed rats where the lipid peroxidation is decreased (Giftson et al. 2010; Ghadi et al. 2009; Vinothkumar et al. 2014b). The decreased TBARS in colon tissues might be because of the concomitant resistance and reduced vulnerability of tumor cells to the ROS scavenging action (Muthu and Vaiyapuri 2013). Antioxidants defend cells from the oxidative damages via free radical scavenging activities. The antioxidants, such as CAT and SOD, primarily scavenge the reactive oxygen species; GPx detoxifies H2O2 and by this means counteracts reactive oxygen species. GSH and the dependent enzymes closely associate with innate defense (Siddique et al. 2017). The increased consumption of tissue antioxidants during DMH metabolite detoxification in tumor cells leads to their decreased level in DMH-alone-exposed rats. Orientin restores the antioxidant levels to put forth their scavenging action. The free -OH groups present in orientin make it an efficient antioxidative agent against ROS prompted by DMH and thereby exhibit their inhibitory prospective against colorectal carcinogenesis.
1.5.3 Xenobiotic Metabolizing Enzymes
DMH upon dehydrogenation in the liver forms azoxymethane (AOM) and methylazoxymethanol (MAM) intermediates (Manju and Nalini 2010). Phase 1 and phase 2 enzymes introduce polar or reactive groups into xenobiotics or carcinogens. Phase 1 enzymes stimulate the procarcinogens by introducing polar active groups, while the phase 2 enzymes detoxify after conjugating with the carcinogens (Padmavathi et al. 2006; Beyerle et al. 2015). Cytochrome P450 enzymes effectively convert lipophilic xenobiotics into more hydrophilic carcinogenic compounds (Sangeetha et al. 2012). The increased level of liver microsomal drug-metabolizing enzyme and intestinal epithelial cell phase 1 enzymes, i.e., CYP2E1, CYP450, and cytochrome b, exhibit DMH-induced carcinogenicity. The genotoxic intermediates produced by phase 1 enzymes covalently attach to form DNA adducts (Balaji et al. 2014). Similar to many flavonoids, orientin administration activates cytochrome P450 enzymes owing to the existence of –OH groups (Sangeetha et al. 2012). The phase 2 enzymes, comprising GST and DT-diaphorase, aid in the introduction of a polar or reactive group to xenobiotic compounds. DT-diaphorase, a widely distributed flavoprotein in animal tissues, detoxifies the quinone and its derivatives to protect against neoplasia (Mohan et al. 2006). Glutathione-S-transferase (GST) interrupts initiation of carcinogenesis by detoxifying hydroquinones and neutralizing electrophilic intermediates (Balaji et al. 2014). The increased level of phase 2 enzymes aids protection against carcinogens. The decreased phase 2 enzyme levels in the hepatic and colonic regions might be because of utilizing more detoxifying enzymes for counteracting DMH-induced malignant tumor formation. Orientin increased the level of phase 2 enzymes and detoxifies the carcinogens. Orientin diminishes active DMH metabolite formation and excretes carcinogen from the colonic lumen.
1.5.4 ACF Formation
Aberrant crypt foci are surrogate precursor lesions of colon cancer distinguished from the usual crypts based on their size, shape, thickness, and the pattern of staining (Bird and Good 2000; Rodrigues et al. 2002). The aberrant crypt with high multiplication rate, i.e., >4 crypts/focus, and their number are the indication of colorectal cancer incidence (Aranganathan and Nalini 2009). The carcinogen-induced rats show higher incidences of ACF and cancer frequency (Baskar et al. 2011). The bioactive compounds inhibiting ACF would also promote the antitumorigenicity (Sengottuvelan et al. 2006; Muthu and Vaiyapuri 2013). ACF shows the initiation of colorectal cancer formation and their increased numbers and multiplicity of crypt suggest the advancement and progress of cancer. Orientin inhibits the ACF progression and suppresses the transformation to malignant neoplasia. The protective activity is ascribed to the antioxidative efficiency of orientin and the metabolic activation of xenobiotic enzymes. The capability of orientin to reinstate DMH-stimulated histological changes authenticates its anticancer and antiinflammatory potentials.
1.5.5 Tumor Marker Levels
An early identification and lessening of precancerous lesions can be made possible by the quantification of serum markers, which may curtail the incidences and death rate of CRC. The assessment of tumor marker levels in serum acts as the prominent markers owing to their ease of handling and economical. The Serological cancer markers (CEA and CA 19–9) are synthesized and liberated into the interstitial fluid and then enters lymph to enter circulation (Narimatsu et al. 2010). Cells holding a higher metastatic potential express these intracellular adhesive proteins on their surface. CEA, the glycosylated immunoglobulin, is the most often characterized tumor-associated antigen and widely existing biomarker for CRC patients. CEA is found in high levels during the malignant and metastatic stages compared to benign conditions (Shitrit et al. 2005). CEA levels in the columnar epithelial cells and goblet cells vary with tumor staging (Flamen et al. 2001). The elevated levels of CEA found in DMH-stimulated experimental animals are most probably linked with tumor size, stage, multiplication, and tumor site. Orientin is reported to moderate CEA levels via reducing the rate of tumor development. CA 19–9 is one of more familiar cancer markers for diagnosing CRC. The increased level of this glycolipid is highly correlated with increased CRC mortality cases. The increased CA 19–9 levels is highly related to perineural and lymphatic invasions, leading to metastatic tumors (Fernandez-Fernandez et al. 1995). The decline in the levels of CA 19–9 after injecting orientin hypothesizes the antitumor action, similar to that of umbelliferone (Muthu and Vaiyapuri 2013). Moreover, orientin treatment for the whole period revealed a strong influence of its cancer preventive potential in DMH-prompted colorectal cancer-possessing experimental animals.
1.5.6 Mast Cell Infiltration
Infiltration of mast cells acts as the finest marker for beginning of inflammatory process. The innate cells of the immune system alter the progression of adenomas into carcinoma initiation by eliciting inflammatory reactions (Khan et al. 2013). Mast cell infiltration is apparently observed in the submucosal layer of DMH-treated animals, which aggravates constant inflammation in the tumor microenvironment. Orientin reduced mast cell infiltration to indicate that it has a potential antiinflammatory activity and also anti-angiogenic potential. The reported antiinflammatory effect of orientin was similar to carvacrol and umbelliferone (Muthu and Vaiyapuri 2013; Arivalagan et al. 2015).
1.5.7 Tumor Cell Proliferation
The reliability of intestinal mucosa is maintained by the crucial mechanism of cell proliferation. The deregulation of cancer cell multiplication recurrently effects in hypergenesis and oncogenesis (Lee and Yun 2010). The nucleolus-associated chromosomal regions (nucleolar organizer regions) are positioned on the acrocentric chromosomes short arm. NORs containing the acidic proteins are silver-stained (AgNORs), and they serve as the investigative or predictive marker of cell multiplication/proliferation (Gundog et al. 2015). In cancerous cells, the cell proliferation is positively linked to AgNORs/nucleus (Sengottuvelan et al. 2006). The total number of AgNORs/nucleus determines cancer succession and the developmental phases. The black dots visualized are utilized as prognostic indicators for cell spread/propagation (Arivalagan et al. 2015). The aggregated numbers of AgNORs/nucleus in the colonic epithelium were found to be higher in DMH-treated experimental animals (Sengottuvelan et al. 2006; Muthu et al. 2016). Orientin decreases the number of AgNORs/nucleus owing to its role in preventing the proliferation of cancer cells. Umbelliferone was earlier reported to decrease the number of AgNORs/nucleus in enterocytes (Muthu et al. 2016; Mariyappan et al. 2017).
Proliferating cell nuclear antigen (PCNA), a non-histone nuclear acidic protein (of 36 KDa), is presumed as an intermediate biomarker of cell proliferation (Aranganathan and Nalini 2013). The expression of PCNA was high in the nuclei of multiplying cells in the growth (G1) phase and early synthetic (S) phase of cell cycle. PCNA monomers enclose the DNA strand like a ring and hold DNA polymerase δ (DNA Pol δ) to the template strand as a clamp to cause hyperproliferation (Mohania et al. 2014). Another proliferating antigen, Ki67 expresses only during G1, S, and G2 phases, but not in the G0 phase. The augmented nuclear expression of PCNA and Ki67 in DMH-induced rats indicates a high proliferation of colonic epithelial cells (Sekar et al. 2016). The suppression of cell proliferation represents one of the protecting actions against DMH-treated colon cancer. Orientin was shown to decrease the expressions of PCNA, Ki67, and their labeling indices. Orientin inhibits cell proliferation by its anti-apoptotic activities (Karthikkumar et al. 2015).
1.5.8 NF-κB and Inflammatory Cytokine Expression
Tumors develop and promote the inflammatory signals in and around the microenvironment. NF-κB activation allows translocation of NF-κB dimer to initiate the transcription of pro-inflammatory cytokines and the downstream target genes (Umesalma and Sudhandiran 2010). The degree of inflammations in DMH-treated animals was apparent by increased NF-κB expression. Orientin reduced the expression of NF-κB owing to its antiinflammatory potentials against DMH-treated inflammations. The inflammatory cytokines (IL-6 and TNF-α) are produced in the tumor microenvironment, which regulates proliferation and apoptosis. The increased TNF-α level during chronic inflammation upholds tumor propagation and metastatic behavior (Colussi et al. 2013). IL-6 is mostly formed by macrophages and monocytes, following the activation of NF-κB. IL-6 plays a huge role during the acute inflammation, tumor cell multiplication, and apoptotic mediated cell death (Dai et al. 2014). TNF-α and IL-6 inhibition serve one of the effective approaches in the treatment of CRC. The elevated production of cytokines during DMH-induced inflammatory response gets downregulated because of the inhibitory potential of orientin (Nash and Ward 2014).
1.5.9 Pro-Inflammatory Enzymes
Inducible nitric oxide synthase (iNOS), the pro-inflammatory mediator, synthesizes nitric oxide (NO), which arbitrates inflammation and persuades tumorigenesis. The carcinogen-induced tumor-bearing rats increased iNOS expression, thereby promoting the invasiveness and metastatic potential (Muthu et al. 2016). iNOS overexpression in colonic cells associates with CRC pathogenesis, where it restrains apoptosis via nitrosylation of caspases. NO impedes DNA repair mechanisms and leads to cytokine post-translational modifications which further influence the commencement and progression of CRC (Narayanan et al. 2003). Orientin distinctly improves the expression of iNOS in DMH-induced rats.
Cyclooxygenase enzymes (COX-2) catalyze prostaglandin synthesis from arachidonic acid, which gets induced at the inflammatory phase and overexpressed in colonic adenocarcinoma (Hamiza et al. 2012a, b). The inflammatory chemokines, cytokines, and tumor promoters induce COX-2 activation (Peng et al. 2013). COX-2 enzymes express higher in cancerous cells via the activation of NF-κB mediated inflammatory cytokine pathway. The increase in COX-2 expression in DMH induced rats was due to its anti-apoptotic effect on colon cancerous cells (Srimuangwong et al. 2012). Orientin distinctly decreased COX-2 expression and corroborates their inhibitory action against inflammation-linked colon tumorigenesis. Orientin suppress the overexpression of inflammatory cytokines due to DMH treatment, thereby validating their antiinflammatory and antiproliferative effects.
1.5.10 Cell Cycle Arrest
The cell cycle dysregulation and avoidance of apoptotic mediated cell death are the familiar events in CRC development (Wu et al. 2018). Arresting of cell cycle at a particular checkpoint and apoptotic induction are the most commonly used mechanisms in the chemoprotection of tumors (Song et al. 2017). The cell cycle checkpoints reinforce the differentiating cells from DNA damages and control the genomic integrity. Orientin stimulated cell cycle arrest at G0/G1 phase in a concentration-dependent way. The stimulated cyclin-dependent serine/threonine kinases and their regulatory cyclin subunits regulate cell cycle progression. These cyclin/CDK complexes act as a biomarker for tumor cell multiplication and targets for anticancer drug development (Peyressatre et al. 2015). Among the different cyclin/CDK complexes, cyclin D and cyclin E along with CDK2 and CDK4 control mitotic division and advance the cell cycle through G1 phase. Orientin noticeably reduced the expression of cyclin D1, cyclin E, and the cyclin-dependent kinases, CDK2 and CDK4. Pelargonidin also showed the reduced expression of CDKs and cyclins in colorectal cancer cell line, HT29 (Karthi et al. 2016). Orientin elevates p21WAF1/CIP1, the chief inhibitor of cyclin D/CDK complex. p21WAF1/CIP1 mediates G0/G1 phase arrest in HT29 cells (Kan et al. 2013). CDK4 activated phosphorylation of Rb trigger the disruption of tumor suppressors which further discharges E2F and initiates G1 to S phase transition (Asghar et al. 2015). Orientin reduces the expression of pRb and thereby inhibits G1 to S phase transition.
1.5.11 Apoptosis
Apoptosis is a complex sequence, which regulates cell proliferation and protects cells from being malignant by getting rid of immortal or repaired cells. Multiple signals trigger the loss of mitochondrial membrane potential with the successive release of cytochrome C from cytosol in carcinogen-induced cancer cells (Lemieszek et al. 2016). Apoptosis is conceivably the powerful defense mechanism of many chemotherapeutic agents toward CRC. The evolutionarily conserved members of Bcl-2 protein family such as Bcl-2 and Bax regulate apoptosis. The pro-apoptotic Bax confines to mitochondria and triggered cytochrome C release leading to caspase-mediated cell death. The prosurvival Bcl-2 binds along with Bax to avert its oligomerization and thwarts mitochondrial membrane depolarization and thereby cytochrome C release (Ding et al. 2010; Tanwar et al. 2010). Orientin decreased the level of anti apoptotic Bcl-2 and Bcl-XL with the increased pro apoptotic Bax and Bid levels which obviously demonstrated the immense potential of Orientin in regulation of Bcl-2 family proteins and apoptotic induction in colon tumor cells. Orientin activates mitochondria-mediated apoptosis in DMH-induced CRC-bearing rats by the simultaneous increase of cytosolic cytochrome C with a decrease in Bcl-2/Bax ratio. Orientin increases caspase 3 and caspase 9 expression in tumor-bearing rats. Caspases are the aspartate-specific cysteine proteases that play a decisive role in apoptotic process. The binding of cytosolic cytochrome C with Apaf-1 activates caspase 9, the initiator caspase, and in turn activates the caspase 3, the downstream effector which leads to intrinsic apoptosis (Sengottuvelan et al. 2009). Orientin activates mitochondria-mediated intrinsic apoptosis in DMH-induced CRC-bearing rats.
Orientin induces Smac/DIABLO release in HT29 cells, along with cytochrome C, thereby neutralizing inhibitor of apoptosis proteins (IAPs) (Srinivasula et al. 2000; Endo et al. 2009; Abdel-Magid 2017). The cytochrome C associates with apoptotic protease-activating factors (Apaf-1) and procaspase 9 to form apoptosome and commence the activation of caspase cascade. The binding of Apaf-1 triggers a conformational change in procaspase 9 to caspase 9 (Omer et al. 2017). Orientin increases caspases (caspase 9 and caspase 3) and cleavage of poly(ADP-ribose) polymerases. Orientin induces apoptosis primarily in the intrinsic pathway (Jiang et al. 2017; Li et al. 2017b). Orientin decreased the expression of inhibitor of apoptosis protein family members, XIAP and Survivin, in HT29 cells due to the release of cytochrome C and the depolarization of mitochondrial membrane potential (Abdel-Magid 2017). Orientin increased expression of tumor suppressor p53 and induced overexpression of p21WAF1/CIP1. The increased level of γ-H2AX in Orientin treated tumor cells serves as a hallmark of DNA damages which confirms the DNA damage induced in HT29 cells.
1.6 Conclusions
Colorectal cancer is one of the most diagnosed cancers, which can be protected or prevented with the chemotherapeutic agents; however, the available drugs have shown systemic toxicity and drug resistance which makes the treatment a challenging issue. A positive correlation exists between flavonoid-rich sources and lowers the risk of colorectal cancer. The above discussed contents explored the effect of dietary flavonoid, orientin, and validated its anti-carcinogenic effect in human colorectal adenocarcinoma HT29 cells and DMH-induced colorectal cancer-bearing Wistar rats. Orientin induces mitochondria-mediated intrinsic apoptosis in colorectal cancer cells and arrests tumor growth by interrupting cell proliferation and inflammatory signaling pathways. Orientin exerts a regulatory effect on major signaling pathways linked with colon cancer progression, namely PTEN/PI3/Akt and Wnt/β-catenin pathways. Overall, this chapter suggests that orientin can be a novel chemotherapeutic agent for controlling CRC.
References
Abdel-Magid AF (2017) Modulation of the inhibitors of apoptosis proteins (IAPs) activities for cancer treatment. ACS Med Chem Lett 8(5):471–473
Akhtar MS, Swamy MK (eds) (2018) Anticancer plants: mechanisms and molecular interactions. Springer International, Singapore
An F, Wang S, Tian Q, Zhu D (2015) Effects of orientin and vitexin from Trollius chinensis on the growth and apoptosis of esophageal cancer EC-109 cells. Oncol Lett 10(4):2627–2633
Anwar N, Teo YK, Tan JB (2019) The role of plant metabolites in drug discovery: current challenges and future perspectives. In: Natural bio-active compounds. Springer, Singapore, pp 25–51
Aranganathan S, Nalini N (2009) Efficacy of the potential chemopreventive agent, hesperetin (citrus flavanone), on 1,2-dimethylhydrazine induced colon carcinogenesis. Food ChemToxicol 47(10):2594–2600
Aranganathan S, Nalini N (2013) Antiproliferative efficacy of hesperetin (citrus flavonoid) in 1,2-dimethylhydrazine-induced colon cancer. Phytother Res 27(7):999–1005
Arivalagan S, Thomas NS, Chandrasekaran B, Mani V, Siddique AI, Kuppsamy T, Namasivayam N (2015) Combined therapeutic efficacy of carvacrol and X-radiation against 1,2-dimethyl hydrazine-induced experimental rat colon carcinogenesis. Mol Cell Biochem 410(1–2):37–54
Asghar U, Witkiewicz AK, Turner NC, Knudsen ES (2015) The history and future of targeting cyclin-dependent kinases in cancer therapy. Nat Rev Drug Discov 14(2):130
Balaji C, Muthukumaran J, Nalini N (2014) Chemopreventive effect of sinapic acid on 1,2-dimethylhydrazine-induced experimental rat colon carcinogenesis. Human Exp Toxicol 33(12):1253–1268
Banerjee A, Quirke P (1998) Experimental models of colorectal cancer. Dis Colon Rectum 41(4):490–505
Baskar AA, Ignacimuthu S, Michael GP, Al Numair KS (2011) Cancer chemopreventive potential of luteolin-7-O-glucoside isolated from Ophiorrhiza mungos Linn. Nutr Cancer 63(1):130–138
Beyerle J, Frei E, Stiborova M, Habermann N, Ulrich CM (2015) Biotransformation of xenobiotics in the human colon and rectum and its association with colorectal cancer. Drug Metabol Revi 47(2):199–221
Bhatia VJ, Nair SS (2018) Nutraceuticals as potential Chemopreventive agents: a review. Nat Prod J 8(1):3–13
Bird RP, Good CK (2000) The significance of aberrant crypt foci in understanding the pathogenesis of colon cancer. Toxicol Lett 112:395–402
Chahar MK, Sharma N, Dobhal MP, Joshi YC (2011) Flavonoids: a versatile source of anticancer drugs. Pharmacogn Rev 5(9):1
Chang H, Lei L, Zhou Y, Ye F, Zhao G (2018 Jul) Dietary flavonoids and the risk of colorectal cancer: an updated meta-analysis of epidemiological studies. Nutrients 10(7):950
Chelyn JL, Omar MH, Yousof M, Akmal NS, Ranggasamy R, Wasiman MI, Ismail Z (2014) Analysis of flavone C-glycosides in the leaves of Clinacanthus nutans (Burm. f.) Lindau by HPTLC and HPLC-UV/DAD. Scientific World J 2014:724267
Colussi D, Brandi G, Bazzoli F, Ricciardiello L (2013) Molecular pathways involved in colorectal cancer: implications for disease behavior and prevention. Int J Mol Sci 14(8):16365–16385
Czemplik M, Mierziak J, Szopa J, Kulma A (2016) Flavonoid C-glucosides derived from flax straw extracts reduce human breast cancer cell growth in vitro and induce apoptosis. Front Pharmacol 7:282
Dai Y, Jiao H, Teng G, Wang W, Zhang R, Wang Y, Hebbard L, George J, Qiao L (2014) Embelin reduces colitis-associated tumorigenesis through limiting IL-6/STAT3 signaling. Mol Cancer Therap 13(5):1206–1216
De Robertis M, Massi E, Poeta ML, Carotti S, Morini S, Cecchetelli L, Signori E, Fazio VM (2011) The AOM/DSS murine model for the study of colon carcinogenesis: from pathways to diagnosis and therapy studies. J Carcinog 10(1):9. https://doi.org/10.4103/1477-3163.78279
Desai S, Kumar A, Laskar S, Pandey B (2013) Cytokine profile of conditioned medium from human tumor cell lines after acute and fractionated doses of gamma radiation and its effect on survival of bystander tumor cells. Cytokine 61(1):54–62
Devi PU, Nayak V, Kamath R (2004) Lack of solid tumour protection by ocimum extract and its flavonoids orientin and vicenin. Curr Sci 25:1401–1404
Ding J, Zhang Z, Roberts GJ, Falcone M, Miao Y, Shao Y, Zhang XC, Andrews DW, Lin J (2010) Bcl-2 and Bax interact via the BH1–3 groove-BH3 motif interface and a novel interface involving the BH4 motif. J Biol Chem 285(37):28749–28763
Dubois J, Mabry TJ (1971) The C-glycosylflavonoids of flax, Linum usitatissimum. Phytochemistry 10(11):2839–2840
Endo K, Kohnoe S, Watanabe A, Tashiro H, Sakata H, Morita M, Kakeji Y, Maehara Y (2009) Clinical significance of Smac/DIABLO expression in colorectal cancer. Oncol Rep 21(2):351–355
Fernandez-Fernandez L, Tejero E, Tieso A (1995) Significance of CA 72-4 in colorectal carcinoma. Comparison with CEA and CA 19-9. Eur J Surg Oncol 21(4):388–390
Flamen P, Hoekstra O, Homans F, Van Cutsem E, Maes A, Stroobants S, Peeters M, Penninckx F, Filez L, Bleichrodt R (2001) Unexplained rising carcinoembryonic antigen (CEA) in the postoperative surveillance of colorectal cancer: the utility of positron emission tomography (PET). Eur J Cancer 37(7):862–869
Fogh J, Trempe G (1975) New human tumor cell lines. In: Human tumor cells in vitro. Springer, New York, pp 115–159
Gallori S, Bilia AR, Bergonzi MC, Barbosa WLR, Vincieri FF (2004) Polyphenolic constituents of fruit pulp of Euterpe oleracea Mart. (Açai palm). Chromatographia 59(11–12):739–743
Ghadi FE, Ghara AR, Bhattacharyya S, Dhawan DK (2009) Selenium as a chemopreventive agent in experimentally induced colon carcinogenesis. World J Gastrointest Oncol 1(1):74
Giftson JS, Jayanthi S, Nalini N (2010) Chemopreventive efficacy of gallic acid, an antioxidant and anticarcinogenic polyphenol, against 1,2-dimethyl hydrazine induced rat colon carcinogenesis. Investig New Drugs 28(3):251–259
Gundog M, Yildiz OG, Imamoglu N, Aslan D, Aytekin A, Soyuer I, Soyuer S (2015) Prognostic significance of two dimensional AgNOR evaluation in local advanced rectal cancer treated with chemoradiotherapy. Asian Pac J Cancer Prev 16(18):8155–8161
Guo Q, Tian X, Yang A, Zhou Y, Wu D, Wang Z (2014) Orientin in Trollius chinensis Bunge inhibits proliferation of HeLa human cervical carcinoma cells by induction of apoptosis. Monatshefte für Chemie-Chemical Monthly 145(1):229–233
Hamiza OO, Rehman MU, Tahir M, Khan R, Khan AQ, Lateef A, Ali F, Sultana S (2012a) Amelioration of 1,2 dimethylhydrazine (DMH) induced colon oxidative stress, inflammation and tumor promotion response by tannic acid in Wistar rats. Asian Pac J Cancer Prev 13(9):4393–4402
Hamiza OO, Rehman MU, Tahir M, Khan R, Khan AQ, Lateef A, Ali F, Sultana S (2012b) Amelioration of 1,2 dimethylhydrazine (DMH) induced colon oxidative stress, inflammation and tumor promotion response by tannic acid in Wistar rats. Asian Pac J Cancer Prevent 13(9):4393–4402
Han MH, Park C, Jin C-Y, Kim G-Y, Chang Y-C, Moon S-K, Kim W-J, Choi YH (2013) Apoptosis induction of human bladder cancer cells by sanguinarine through reactive oxygen species-mediated up-regulation of early growth response gene-1. PLoS One 8(5):e63425
He Y, Lv H, Wang X, Suo Y, Wang H (2014) Isolation and purification of six bioactive compounds from the seeds of Trigonella foenum-graecum L. using high-speed counter-current chromatography. Separ Sci Technol 49(4):580–587
Idrees M, Tejani M (2019) Current treatment strategies for elderly patients with metastatic Colon Cancer. Cureus 11(5):1–7
Jain C, Khatana S, Vijayvergia R (2019) Bioactivity of secondary metabolites of various plants: a review. Int J Pharm Sci 1:494–404
Jiang Y, Wang X, Hu D (2017) Furanodienone induces G0/G1 arrest and causes apoptosis via the ROS/MAPKs-mediated caspase-dependent pathway in human colorectal cancer cells: a study in vitro and in vivo. Cell Death Dis 8(5):e2815
Kan WLT, Yin C, Xu HX, Xu G, To KKW, Cho CH, Rudd JA, Lin G (2013) Antitumor effects of novel compound, guttiferone K, on colon cancer by p21Waf1/Cip1-mediated G0/G1 cell cycle arrest and apoptosis. Int J Cancer 132(3):707–716
Karthi N, Kalaiyarasu T, Kandakumar S, Mariyappan P, Manju V (2016) Pelargonidin induces apoptosis and cell cycle arrest via a mitochondria mediated intrinsic apoptotic pathway in HT29 cells. RSC Adv 6(51):45064–45076
Karthikkumar V, Sivagami G, Viswanathan P, Nalini N (2015) Rosmarinic acid inhibits DMH-induced cell proliferation in experimental rats. J Basic Clin Physiol Pharmacol 26(2):185–200
Khan R, Khan AQ, Lateef A, Rehman MU, Tahir M, Ali F, Hamiza OO, Sultana S (2013) Glycyrrhizic acid suppresses the development of precancerous lesions via regulating the hyperproliferation, inflammation, angiogenesis and apoptosis in the colon of Wistar rats. PLoS One 8(2):e56020
Kilari BP, Kotakadi VS, Penchalaneni J (2016) Anti-proliferative and apoptotic effects of Basella rubra (L.) Against 1,2-Dimethyl Hydrazine-induced colon carcinogenesis in rats. Asian Pac J Cancer Prev 17:73–80
Koeppen B, Smit C, Roux D (1962) The flavone C-glycosides and flavonol O-glycosides of Aspalathus acuminatus (rooibos tea). Biochem J 83(3):507
Krahl M, Back W, Zarnkow M, Kreisz S (2008) Determination of optimised malting conditions for the enrichment of rutin, vitexin and orientin in common buckwheat (Fagopyrum esculentum Moench). J Inst Brew 114(4):294–299
Kumar S, Pandey AK (2013) Chemistry and biological activities of flavonoids: an overview. Sci World J 2013:1
Lee S-J, Yun CC (2010) Colorectal cancer cells–proliferation, survival and invasion by lysophosphatidic acid. Int J Biochem Cell Biol 42(12):1907–1910
Lemieszek MK, Ribeiro M, Alves HG, Marques G, Nunes FM, Rzeski W (2016) Boletus edulis ribonucleic acid–a potent apoptosis inducer in human colon adenocarcinoma cells. Food Funct 7(7):3163–3175
Li F, Zong J, Zhang H, Zhang P, Xu L, Liang K, Yang L, Yong H, Qian W (2017a) Orientin reduces myocardial infarction size via eNOS/NO signaling and thus mitigates adverse cardiac remodeling. Front Pharmacol 8:926
Li M, Song L-H, Yue GG-L, Lee JK-M, Zhao L-M, Li L, Zhou X, Tsui SK-W, Ng SS-M, Fung K-P (2017b) Bigelovin triggered apoptosis in colorectal cancer in vitro and in vivo via upregulating death receptor 5 and reactive oxidative species. Sci Rep 7:42176
Liu Y, Yin T, Feng Y, Cona MM, Huang G, Liu J, Song S, Jiang Y, Xia Q, Swinnen JV (2015) Mammalian models of chemically induced primary malignancies exploitable for imaging-based preclinical theragnostic research. Quant Imag Med Surg 5(5):708
Machado VF, Feitosa MR, JJRd R, Féres O (2016) A review of experimental models in colorectal carcinogenesis. J Coloproctol (Rio de Janeiro) 36(1):53–57
Manju V, Nalini N (2005) Chemopreventive efficacy of ginger, a naturally occurring anticarcinogen during the initiation, post-initiation stages of 1,2 dimethylhydrazine-induced colon cancer. Clin Chim Acta 358(1–2):60–67
Manju V, Nalini N (2010) Effect of ginger on lipid peroxidation and antioxidant status in 1,2-dimethyl hydrazine induced experimental colon carcinogenesis. J Biochem Technol 2(2):161–167
Mariyappan P, Kalaiyarasu T, Manju V (2017) Effect of eriodictyol on preneoplastic lesions, oxidative stress and bacterial enzymes in 1,2-dimethyl hydrazine-induced colon carcinogenesis. Toxicol Res 6(5):678–692
Martínez-Maqueda D, Miralles B, Recio I (2015) HT29 cell line. In: The impact of food bioactives on health. Springer, Cham, pp 113–124
Megaraj V, Ding X, Fang C, Kovalchuk N, Zhu Y, Zhang Q-Y (2014) Role of hepatic and intestinal p450 enzymes in the metabolic activation of the colon carcinogen azoxymethane in mice. Chem Res Toxicol 27(4):656–662
Mohan KVPC, Kumaraguruparan R, Prathiba D, Nagini S (2006) Modulation of xenobiotic-metabolizing enzymes and redox status during chemoprevention of hamster buccal carcinogenesis by bovine lactoferrin. Nutrition 22(9):940–946
Mohania D, Kansal VK, Kruzliak P, Kumari A (2014) Probiotic dahi containing Lactobacillus acidophilus and Bifidobacterium bifidum modulates the formation of aberrant crypt foci, mucin-depleted foci, and cell proliferation on 1,2-dimethylhydrazine-induced colorectal carcinogenesis in Wistar rats. Rejuv Res 17(4):325–333
Muthu R, Vaiyapuri M (2013) Synergistic and individual effects of umbelliferone with 5-fluorouracil on tumor markers and antioxidant status of rat treated with 1,2-dimethylhydrazine. Biomed Aging Pathol 3(4):219–227
Muthu R, Selvaraj N, Vaiyapuri M (2016) Anti-inflammatory and proapoptotic effects of umbelliferone in colon carcinogenesis. Human Exp Toxicol 35(10):1041–1054
Narayanan BA, Narayanan NK, Simi B, Reddy BS (2003) Modulation of inducible nitric oxide synthase and related proinflammatory genes by the omega-3 fatty acid docosahexaenoic acid in human colon cancer cells. Cancer Res 63(5):972–979
Narimatsu H, Sawaki H, Kuno A, Kaji H, Ito H, Ikehara Y (2010) A strategy for discovery of cancer glyco-biomarkers in serum using newly developed technologies for glycoproteomics. FEBS J 277(1):95–105
Nash L, Ward W (2014) Tea flavonoids stimulate mineralization in osteoblast-like cells (259.7). FASEB J 28(1_supplement):259–257
Nirmala P, Ramanathan M (2011) Effect of kaempferol on lipid peroxidation and antioxidant status in 1,2-dimethyl hydrazine induced colorectal carcinoma in rats. Eur J Pharmacol 654(1):75–79
Omer FAA, Hashim NBM, Ibrahim MY, Dehghan F, Yahayu M, Karimian H, Salim LZA, Mohan S (2017) Beta-mangostin from Cratoxylum arborescens activates the intrinsic apoptosis pathway through reactive oxygen species with downregulation of the HSP70 gene in the HL60 cells associated with a G0/G1 cell-cycle arrest. Tumor Biol 39(11):1010428317731451
Padmavathi R, Senthilnathan P, Sakthisekaran D (2006) Therapeutic effect of propolis and paclitaxel on hepatic phase I and II enzymes and marker enzymes in dimethylbenz (a) anthracene-induced breast cancer in female rats. Comp Biochem Physiol Part C: Toxicol Pharmacol 143(3):349–354
Pal D, Mishra P, Sachan N, Ghosh AK (2011) Biological activities and medicinal properties of Cajanus cajan (L) Millsp. J Adv Pharm Technol Res 2(4):207
Panche AN, Diwan AD, Chandra SR (2016) Flavonoids: an overview. J Nutr Sci 5:e47
Pang S, Ge Y, Wang LS, Liu X, Lin CW, Yang H (2013) Isolation and purification of orientin and isovitexin from Thlaspi arvense linn. In: Advanced materials research. Trans Tech Publications, Switzerland, pp 615–618
Peng L, Zhou Y, Wang Y, Mou H, Zhao Q (2013) Prognostic significance of COX-2 immunohistochemical expression in colorectal cancer: a meta-analysis of the literature. PLoS One 8(3):e58891
Perše M (2013) Oxidative stress in the pathogenesis of colorectal cancer: cause or consequence? BioMed Res Int 2013:725710
Perveen S, El-Shafae AM, Al-Taweel A, Fawzy GA, Malik A, Afza N, Latif M, Iqbal L (2011) Antioxidant and urease inhibitory C-glycosylflavonoids from Celtis africana. J Asian Nat Prod Res 13(9):799–804
Peyressatre M, Prével C, Pellerano M, Morris M (2015) Targeting cyclin-dependent kinases in human cancers: from small molecules to peptide inhibitors. Cancers 7(1):179–237
Qi G, Zeng S, Takashima T, Nozoe K, Shobayashi M, Kakugawa K, Murakami K, Jikihara H, Zhou L, Shimamoto F (2015) Inhibitory effect of various breads on DMH-induced aberrant crypt foci and colorectal tumours in rats. BioMed Res Int 2015
Ricciardiello L, Ahnen DJ, Lynch PM (2016 Jun) Chemoprevention of hereditary colon cancers: time for new strategies. Nat Rev Gastroenterol Hepatol 13(6):352
Rodrigues MAM, Silva L, Salvadori DMF, De Camargo J, Montenegro M (2002) Aberrant crypt foci and colon cancer: comparison between a short-and medium-term bioassay for colon carcinogenesis using dimethylhydrazine in Wistar rats. Braz J Med Biol Res 35(3):351–355
Roy A, Jauhari N, Bharadvaja N (2018) Medicinal plants as a potential source of chemopreventive agents. In: Anticancer plants: natural products and biotechnological implements. Springer, Singapore, pp 109–139
Sangeetha N, Viswanathan P, Balasubramanian T, Nalini N (2012) Colon cancer chemopreventive efficacy of silibinin through perturbation of xenobiotic metabolizing enzymes in experimental rats. Eur J Pharmacol 674(2–3):430–438
Sekar V, Anandasadagopan SK, Ganapasam S (2016) Genistein regulates tumor microenvironment and exhibits anticancer effect in dimethyl hydrazine-induced experimental colon carcinogenesis. Biofactors 42(6):623–637
Selvam JP, Aranganathan S, Gopalan R, Nalini N (2009) Chemopreventive efficacy of pronyl-lysine on lipid peroxidation and antioxidant status in rat colon carcinogenesis. Fund Clin Pharmacol 23(3):293–302
Sengottuvelan M, Senthilkumar R, Nalini N (2006) Modulatory influence of dietary resveratrol during different phases of 1,2-dimethylhydrazine induced mucosal lipid-peroxidation, antioxidant status and aberrant crypt foci development in rat colon carcinogenesis. Biochim Biophys Acta 1760(8):1175–1183
Sengottuvelan M, Deeptha K, Nalini N (2009) Influence of dietary resveratrol on early and late molecular markers of 1,2-dimethylhydrazine–induced colon carcinogenesis. Nutrition 25(11–12):1169–1176
Shibano M, Kakutani K, Taniguchi M, Yasuda M, Baba K (2008) Antioxidant constituents in the dayflower (Commelina communis L.) and their α-glucosidase-inhibitory activity. J Nat Med 62(3):349
Shitrit D, Zingerman B, Shitrit AB-G, Shlomi D, Kramer MR (2005) Diagnostic value of CYFRA 21-1, CEA, CA 19-9, CA 15-3, and CA 125 assays in pleural effusions: analysis of 116 cases and review of the literature. Oncologist 10(7):501–507
Siddique AI, Mani V, Arivalagan S, Thomas NS, Namasivayam N (2017) Asiatic acid attenuates pre-neoplastic lesions, oxidative stress, biotransforming enzymes and histopathological alterations in 1,2-dimethylhydrazine-induced experimental rat colon carcinogenesis. Toxicol Mech Method 27(2):136–150
Soltis DE, Bohm BA (1982) Flavonoids of Ascarina lucida. J Nat Prod 45(4):415–417
Song X-L, Zhang Y-J, Wang X-F, Zhang W-J, Wang Z, Zhang F, Zhang Y-J, Lu J-H, Mei J-W, Hu Y-P (2017) Casticin induces apoptosis and G0/G1 cell cycle arrest in gallbladder cancer cells. Cancer Cell Int 17(1):9
Srimuangwong K, Tocharus C, Tocharus J, Suksamrarn A, Chintana PY (2012) Effects of hexahydrocurcumin in combination with 5-fluorouracil on dimethylhydrazine-induced colon cancer in rats. World J Gastroenterol 18(47):6951
Srinivasula SM, Datta P, Fan X-J, Fernandes-Alnemri T, Huang Z, Alnemri ES (2000) Molecular determinants of the caspase-promoting activity of Smac/DIABLO and its role in the death receptor pathway. J Biol Chem 275(46):36152–36157
Tanwar L, Vaish V, Sanyal SN (2010) Chemopreventive role of etoricoxib (MK-0663) in experimental colon cancer: induction of mitochondrial proapoptotic factors. Eur J Cancer Prev 19(4):280–287
Thangaraj K, Natesan K, Settu K, Palani M, Govindarasu M, Subborayan V, Vaiyapuri M (2018) Orientin mitigates 1,2-dimethylhydrazine induced lipid peroxidation, antioxidant and biotransforming bacterial enzyme alterations in experimental rats. J Cancer Res Therap 14(6):1379
Tungmunnithum D, Thongboonyou A, Pholboon A, Yangsabai A (2018 Sep) Flavonoids and other phenolic compounds from medicinal plants for pharmaceutical and medical aspects: an overview. Medicines 5(3):93
Tuorkey MJ (2016) Molecular targets of luteolin in cancer. Eur J Cancer Prev 25(1):65
Umesalma S, Sudhandiran G (2010) Differential inhibitory effects of the polyphenol ellagic acid on inflammatory mediators NF-κB, iNOS, COX-2, TNF-α, and IL-6 in 1,2-dimethylhydrazine-induced rat colon carcinogenesis. Basic Clin Pharmacol Toxicol 107(2):650–655
Vinothkumar R, Kumar RV, Karthikkumar V, Viswanathan P, Kabalimoorthy J, Nalini N (2014a) Oral supplementation with troxerutin (trihydroxyethylrutin), modulates lipid peroxidation and antioxidant status in 1,2-dimethylhydrazine-induced rat colon carcinogenesis. Environ Toxicol Pharmacol 37(1):174–184
Vinothkumar R, Kumar RV, Sudha M, Viswanathan P, Balasubramanian T, Nalini N (2014b) Modulatory effect of troxerutin on biotransforming enzymes and preneoplasic lesions induced by 1,2-dimethylhydrazine in rat colon carcinogenesis. Exp Mol Pathol 96(1):15–26
Wagner H, Horhammer L, Kiraly I (1970) Flavone-C-glycosides in Croton zambezicus. Phytochemistry 9:897
Wu X, Song M, Qiu P, Li F, Wang M, Zheng J, Wang Q, Xu F, Xiao H (2018) A metabolite of nobiletin, 4′-demethylnobiletin and atorvastatin synergistically inhibits human colon cancer cell growth by inducing G0/G1 cell cycle arrest and apoptosis. Food Funct 9(1):87–95
Youns M, Hegazy WAH (2017) The natural flavonoid fisetin inhibits cellular proliferation of hepatic, colorectal, and pancreatic cancer cells through modulation of multiple signaling pathways. PLoS One 12(1):e0169335
Zamora-Ros R, Shivappa N, Steck SE, Canzian F, Landi S, Alonso MH, Hébert JR, Moreno V (2015) Dietary inflammatory index and inflammatory gene interactions in relation to colorectal cancer risk in the Bellvitge colorectal cancer case–control study. Genes Nutri 10(1):447
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Vaiyapuri, M., Natesan, K., Vasamsetti, B.M.K., Mekapogu, M., Swamy, M.K., Thangaraj, K. (2020). Orientin: A C-Glycosyl Flavonoid that Mitigates Colorectal Cancer. In: Swamy, M. (eds) Plant-derived Bioactives. Springer, Singapore. https://doi.org/10.1007/978-981-15-2361-8_1
Download citation
DOI: https://doi.org/10.1007/978-981-15-2361-8_1
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-2360-1
Online ISBN: 978-981-15-2361-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)