Abstract
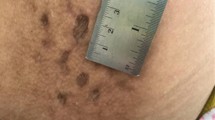
A 38-year-old male known alcohol abuser, chronic smoker, and IV drug abuser came to the emergency department in inebriated state. On examination, he was cachectic, stuporous with bilateral pin-point pupils. There were multiple black erythematous patches on forearm with multiple injection marks. His pulse rate was 46/min and blood pressure was 82/60 mmHg, and on auscultation, there were bilateral crepitations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
A 38-year-old male known alcohol abuser, chronic smoker, and IV drug abuser came to the emergency department in inebriated state. On examination, he was cachectic, stuporous with bilateral pin-point pupils. There were multiple black erythematous patches on forearm with multiple injection marks. His pulse rate was 46/min and blood pressure was 82/60 mmHg, and on auscultation, there were bilateral crepts.
Substance abuse may be persistent or sporadic, inconsistent with or unrelated to acceptable medical practice. This subset of patients may present to the hospital with acute intoxication, withdrawal, or infectious and other chronic complications related to drug abuse. They have overall better prognosis as compared to other critically ill patients, if diagnosed and managed timely. Narcotics, stimulants, and sedatives are the common prescription drugs of abuse. Patients may present with deliberate or accidental overdose.
Step 1: Initiate Resuscitation
-
Initial resuscitation should be done as mentioned in Chap. 23, Vol. 2.
-
In addition to routine investigations, CT Head should be done to rule out intracranial bleed in patients presenting as hypertension particularly with Stimulants abuse [i.e. Cocaine].
-
Give IV naloxone if respiratory depression and opioid abuse is a possibility as it rapidly reverses the respiratory depression and intubation can be avoided. This should be avoided in patient with history of chronic abuse of these substances as it may precipitate seizures and arrhythmias.
Airway
-
Management of airways is very important in poisoning. When intubation is necessary, rapid sequence induction is indicated using short-acting paralytic agents.
-
Urine toxicology screening should be obtained before administering any sedatives or hypnotics.
Breathing
-
A patient’s oxygenation status can be monitored with a bedside pulse oximeter.
-
Give oxygen by the nasal cannula or facemask to maintain SpO2 more than 95%.
-
The patient should be started on assisted ventilation if unable to maintain oxygenation or ventilation.
Circulation
-
Monitor pulse and blood pressure and do ECG.
-
Obtain a good peripheral line and start intravenous fluids.
Step 2: Initial Assessment
-
This subset of patients may present to the hospital with acute intoxication, withdrawal, or infectious and other chronic complications related to drug abuse.
The drugs of abuse can be classified into major groups (Table 15.1).
The initial evaluation of these patients has multiple physical, social, emotional, and medicolegal issues that should be addressed.
-
Complete and focused history should be taken from the patient, family, accompanying physician, or police, as mentioned in Chap. 14, Vol. 2.
-
Do detailed examination (Fig. 15.1):
-
Once the patient is stable, a more comprehensive physical and systemic examination should be performed.
-
Serial examinations are even more important to assess dynamic change in clinical appearance.
-
The systematic neurological evaluation is particularly important, in patients with altered mental status. Alert/verbal/painful/unresponsive scale (AVPU) is a simple rapid method of assessing consciousness in most poisoned patients.
-
Step 3: Diagnosis by Toxidromic Approach
The signs and symptoms of drugs of abuse are organized around the activity of six neurotransmitters (Table 15.2), with this activity being sufficiently unique to permit rapid identification of the specific drug responsible for a given clinical situation.
-
Based on history and examination, it may be possible to define a constellation of signs and symptoms or toxidromes, which may help in diagnosing the unknown poison and provide a specific antidote. Common toxidromes are listed in Chap. 14, Vol. 2.
Step 4: Diagnose Common Drug Abuse
-
1.
Alcohol
-
Acute effects:
-
CNS depressant.
-
In low doses, alcohol depresses inhibitory centers and resultant disinhibition (out-of-character activities).
-
At higher doses, alcohol inhibits excitatory centers.
-
-
Signs of chronic alcohol abuse:
-
Gastrointestinal—cirrhosis of the liver, peptic ulcer disease, gastritis, pancreatitis, and carcinoma
-
Cardiovascular—hypertension, cardiomyopathy, atrial fibrillation (“holiday heart syndrome”)
-
Neurological—peripheral neuropathy leading to ataxia, Wernicke encephalopathy, Korsakoff psychosis, and structural changes in the brain leading to dementia
-
Immunologic—suppression of neutrophil function and cell-mediated immunity
-
Endocrine—in males, increase in estrogen and decrease in testosterone, leading to impotence, testicular atrophy, and gynecomastia
-
Psychiatric—depression or anxiety disorders
-
-
-
2.
Opiates
-
Acute intoxication—decreased respiratory rate and pinpoint pupils, with complications including noncardiogenic pulmonary edema and respiratory failure.
-
Complications of chronic abuse are primarily infectious and include skin abscess at an injection site, cellulitis, mycotic aneurysms, endocarditis, talcosis, HIV, and hepatitis.
-
-
3.
Cocaine
Cocaine may be smoked, inhaled, used topically, or injected:
-
Acute cocaine intoxication may present with agitation, paranoia, tachycardia, tachypnea, hypertension, and diaphoresis.
-
Complications of acute and chronic use can include myocardial ischemia or infarction, stroke, pulmonary edema, and rhabdomyolysis.
-
-
4.
Amphetamines
Acute intoxication with amphetamines presents with signs of sympathetic nervous system stimulation, tachycardia, hypertension, anorexia, insomnia, and occasionally seizures.
-
5.
Hallucinogens
-
Different hallucinogens present with a variety of organ system effects.
-
Phencyclidine (PCP) has been known to cause muscle rigidity, seizures, rhabdomyolysis, and coma.
-
Anticholinergics have been associated with delirium, supraventricular tachycardia, hypertension, and seizures.
Other hallucinogens (e.g., lysergic acid diethylamide, peyote, marijuana, and nutmeg) rarely cause significant physical complications.
-
Step 5: Send Investigations
Patients:
-
Complete blood count
-
Serum electrolytes
-
Blood urea nitrogen, creatinine
-
Liver functions tests
-
Blood glucose, bicarbonate level
-
Arterial blood gases
-
ECG
-
Echocardiography
Special investigations:
-
Urine toxicology screening: In the patient with acute intoxication, urine screening for substances of abuse and a blood or breath alcohol level may be considered, but these generally do not alter management. Urine toxicology screening is needed for the following:
-
Amphetamines
-
Barbiturates
-
Benzodiazepines
-
Cannabinoids
-
Cocaine
-
Opioids
-
Phencyclidine
-
-
Caution: A single negative urine toxicology screening or urine immunoassay is not reliable, and repeat tests should be done after a few hours especially if clinical suspicion is high:
-
Blood toxicology profile—if available.
-
If the patient is a female of child-bearing age, a pregnancy test is essential.
-
Serum ethanol level, the anion gap, serum osmolality, and osmolal gap should be performed for alcohol intoxication.
-
A CT scan of the head is advised—if altered mental status is not explained or in the presence of new focal neurological deficit.
-
Step 6: General Management
-
The general principle of management of patients with suspected drug overdose or withdrawal is supportive and includes standard resuscitative measures.
-
Once the patient has been stabilized, the physician must consider how to minimize the bioavailability of toxin not yet absorbed, which antidotes (if any) to administer, and what other measures should be undertaken to enhance elimination.
-
After initial resuscitation, use the specific antidote when available.
The management of acute intoxication and withdrawal again will depend on the particular neurotransmitters involved (Table 15.2).
Step 7: Manage as per Specific Class
-
1.
Dissociative drugs
-
Acute intoxication: Haloperidol, a presynaptic dopamine antagonist, is useful for blocking significant symptoms of dissociative intoxication.
-
Dose: 1 mg IV every 15–20 min up to maximum 10 mg. This can be given orally or intramuscularly, too.
Alternative to haloperidol is risperidone.
-
Chronic intoxication: Desipramine for postwithdrawal depression.
-
-
2.
Opiates
-
Specific antidote (naloxone, naltrexone, naltrefene): Naloxone, at a dose of 0.1–0.4 mg or 0.01 mg/kg IV, may have to be repeated every 1–2 min.
-
Naloxone should not be used in patients with chronic abuse as it can precipitate seizures or withdrawal.
-
Withdrawal: Methadone is the drug of choice, but not easily available. Clonidine orally/Ryle’s tube 17 μg/kg/day in three to four doses can be used.
-
-
3.
Hallucinogens
-
Acute intoxication: Benzodiazepines (midazolam, diazepam, alprazolam) are the drug of choice.
-
Withdrawal: Fluoxetine can be given orally.
-
-
4.
Sedative–hypnotic drugs
-
Acute intoxication: For supportive management, flumazenil is the specific antidote for benzodiazepines but can precipitate seizures or withdrawal in patients with chronic abuse.
-
Chronic intoxication/withdrawal:
Barbiturates: The equivalent dose of phenobarbitone for a period, which depends on the duration of action of the abused drug for withdrawal effect. Flumazenil can cause seizure in chronic intoxication of barbiturates.
Benzodiazepines : Long-acting like chlordiazepoxide (Librium) orally/Ryle’s tube maximum up to 25 mg, three to four times a day, or lorazepam 1–2 mg three to four times a day.
Alcohol: Same as benzodiazepines. If chronic abuse give thiamine 200 mg.
-
-
5.
Stimulant drugs
-
Acute intoxication: Benzodiazepines (lorazepam) are the drug of choice.
-
Chronic abuse: Bromocriptine and/or desipramine can be given orally.
-
Summary
-
Patients with substance abuse may present to the hospital with acute intoxication, withdrawal, or infectious and other chronic complications related to drug abuse.
-
Initial resuscitation should be done using the ABCDE approach.
-
Based on detailed history and clinical examination, it may be possible to define a constellation of signs and symptoms or toxidromes, which may help in diagnosing the unknown poison.
-
Specific investigations may be required to diagnose specific substance abuse.
-
After initial resuscitation, use the specific antidote when available.
Suggested Reading
Betten DP, Vohra RB, Cook MD, Matteucci MJ, Clark RF. Antidote use in the critically ill poisoned patient. J Intensive Care Med. 2006;21(5):255–77. The more commonly used antidotes that may be encountered in the intensive care unit (N-acetylcysteine, ethanol, fomepizole, physostigmine, naloxone, flumazenil, sodium bicarbonate, octreotide, pyridoxine, cyanide antidote kit, pralidoxime, atropine, digoxin immune Fab, glucagon, calcium gluconate and chloride, deferoxamine, phytonadione, botulism antitoxin, methylene blue, and Crotaline snake antivenom) are reviewed
Chang G, Kosten TR. Detoxification. In: Lowinson JH, Ruiz P, Millman RB, Langrod JG, editors. Substance abuse: a comprehensive textbook. 4th ed. Baltimore: Lippincott, Williams & Wilkins; 2004. p. 579–86.
Holstege CP, Borek HA. Toxidromes. Crit Care Clin. 2012;28(4):479–98. This article reviews the general approach to the poisoned patient, specifically focusing on the utility of the toxidrome. A toxidrome is a constellation of findings, either from the physical examination or from ancillary testing, which may result from any poison. There are numerous toxidromes defined in the medical literature. This article focuses on the more common toxidromes described in clinical toxicology
Marraffa JM, Cohen V, Howland MA. Antidotes for toxicological emergencies: a practical review. Am J Health Syst Pharm. 2012;69(3):199–212. This review highlights the role pharmacists can play a key role in reducing poisoning and overdose injuries and deaths by assisting in the early recognition of toxic exposures and guiding emergency personnel on the proper storage, selection, and use of antidotal therapies
Moeller KE, Kissack JC, Atayee RS, Lee KC. Clinical interpretation of urine drug tests: what clinicians need to know about urine drug screens. Mayo Clin Proc. 2017;92:774–96. pii: S0025-6196(16)30825-4. In this report, technical information related to detection methods of urine drug tests that are commonly used are provided, an overview of false-positive/false-negative data for commonly misused substances in the following categories: cannabinoids, central nervous system (CNS) depressants, CNS stimulants, hallucinogens, designer drugs, and herbal drugs of abuse are given . Brief discussions of alcohol and tricyclic antidepressants as related to urine drug tests is described . The goal of this review was to provide a useful tool for clinicians when interpreting urine drug test results and making appropriate clinical decisions on the basis of the information presented
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Singh, O., Nasa, P., Juneja, D. (2020). Drug Abuse. In: Chawla, R., Todi, S. (eds) ICU Protocols. Springer, Singapore. https://doi.org/10.1007/978-981-15-0902-5_15
Download citation
DOI: https://doi.org/10.1007/978-981-15-0902-5_15
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-0901-8
Online ISBN: 978-981-15-0902-5
eBook Packages: MedicineMedicine (R0)