Abstract
A 42 years old female, non smoker presented with fever, nasal discharge, cough and shortness of breath for the last five days. On examination, patient was conscious, RR 38/min, SPO2 80% on nasal prongs with 5 L/min, BP 130/70. His TLC was 5.2. Chest X-ray revealed bilateral infiltrates. Her throat swab came out as + H1N1. She was started on nonrebreathing mask with oxygen flow at 15 L/m. His SpO2 was still 86%. Patient was started on Heated Humidified high flow nasal canula at 60 L/m. She became comfortable and RR came down to 23/m after 10 min.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
A 42 years old female, non smoker presented with fever, nasal discharge, cough and shortness of breath for the last five days. On examination, patient was conscious, RR 38/min, SPO2 80% on nasal prongs with 5 L/min, BP 130/70. His TLC was 5.2. Chest X-ray revealed bilateral infiltrates. Her throat swab came out as + H1N1. She was started on nonrebreathing mask with oxygen flow at 15 L/m. His SpO2 was still 86%. Patient was started on Heated Humidified high flow nasal canula at 60 L/m. She became comfortable and RR came down to 23/m after 10 min.
In patient of hypoxemic respiratory failure, oxygen is applied via variable low-flow systems (e.g., nasal cannulae or face masks) or high-flow systems (e.g., Venturi masks, nonrebreathing reservoir mask) (Fig. 4.1). These conventional systems have lot of disadvantages. They deliver unreliable fraction of inspired oxygen and provide inadequate warming and humidification of inspired gas. In a patients with acute respiratory failure, peak inspiratory flow rate is high and often exceeds the oxygen flow delivered by these traditional oxygen devices, which results in flow starvation. High-flow nasal cannula (HFNC) oxygen therapy overcomes these limitations. HFNC is a technique of Oxygen therapy which delivers heated and humidified oxygen through a nasal cannula at high flow rates (~60 L/min)at higher oxygen concentration (FiO2 0.21–1). This has been found noninferior to NIV in mild hypoxemic respiratory failure and is recommended in some other clinical conditions. Moreover complications associated with NIV like lung injury and patient dysynchrony is increasingly being recognised.
Step 1: Resuscitate
-
The patient should be resuscitated as mentioned in Chap. 23, Vol. 2.
-
Look for hemodynamic instability, sensorium, and oxygenation by pulse oximetry.
-
If SpO2 is low, give oxygen. Titrate oxygen to keep SpO2 at 88–92%.
-
Check arterial blood gas (ABG) and initiate other investigations as mentioned below:
-
Hemogram, blood urea, serum creatinine, and serum electrolytes
-
Blood and sputum culture if infection is suspected
-
Chest skiagram
-
Electrocardiogram (ECG) and Echocardiogram (Echo)
-
Disease-specific treatment should be initiated.
Step 2: Choose a Noninvasive Respiratory Support-Assess the Need for NIV/HFNC
-
NIV or HFNC: Choosing among these options depends upon factors including need for ventilation and positive end expiratory pressure (PEEP) as well as patient preference and tolerance of the NIV mask (Table 4.1).
-
HFNC is unlikely to provide sufficient PEEP for those who need it (e.g., moderate to severe acute respiratory distress syndrome [ARDS]) and cannot be used for those who require NIV for ventilation (i.e., hypercapnic hypoxemic respiratory failure due to hypoventilation).
-
It is also unlikely to reduce the work of breathing as effectively as NIV.
-
There are two group of patients who are not given HFNC are those who improve on simple nasal canula and those who are intubated.
-
Although so far there are no defined clearcut indications of HFNC but it is being used for a variety of clinical conditions.
-
HFNC has lot of physiological advantages as mentioned below.
-
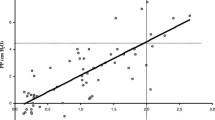
HFNC provides very high flow rates which can be adjusted to meet or exceed the patient’s inspiratory flow rate demands. This leads to less entrainment of room air, so it provides reliably delivered FiO2 and maintains a constant FiO2 despite a high patient minute ventilation. FiO2 may be titrated from) 0.21 to 1.0 by air/oxygen blender. High flow rates result in an improved breathing pattern by decreasing respiratory rate and increasing tidal volume (Fig. 4.2).
-
HFNC provides an anatomical oxygen reservoir in the nasopharynx and oropharynx due to a CO2 washout effect as a result of the high oxygen flow. This reduces dead space and the work of breathing in turn. This also helps in decreased rebreathing of CO2 in hypercapnic patient.
-
The continuous delivery of high flow, which impedes expiratory flow, generates a degree of PEEP. This PEEP effect results in increased end-expiratory lung volume, and thus alveolar recruitment. Flow rates of around 35 to 60 L/min generate mean expiratory pressures of 2 to 3 cm H2O with the mouth open and 5 to 7 cm H2O with the mouth closed.
-
The splinting of the upper airway also has the effect of reducing airflow resistance in the nasopharynx, thereby reducing the work of breathing.
-
The metabolic load associated with warming and increasing the humidity of inspired gas is averted as the gas is optimally conditioned before delivery in HFNC.
-
Conditioning of gas prevents airway desiccation, improves mucociliary function, facilitates clearance of secretions, and is associated with less atelectasis.
-
Conventional oxygen devices and NIV delivering dry and unwarmed gas are associated with mask discomfort, claustrophobia, oronasal dryness, eye irritation, nasal and eye trauma, gastric distension, and aspiration.
-
Indications (Table 4.2)
Acute Mild Hypoxemic Respiratory Failure
-
The main use of HFNC is to provide a relatively high FiO2 to patients with acute hypoxemic respiratory failure (AHRF) with PaO2/FiO2 ratio 150–300.
-
HFNC has successfully been used in AHRF due to severe influenza, ARDS, congestive heart failure, hematologic malignancies and organ transplant.
-
The results of HFNC use failed to consistently demonstrate an improvement in mortality, intubation rates, length of stay in nonhypercapnic hypoxemic respiratory failure.
-
A meta-analysis of 13 randomized trials failed to demonstrate a decrease in the rate of intubation or mortality.
-
Most of trials in ARDS have consistently shown that HFNC decreases the work of breathing, decrease respiratory rate and increases patient comfort.
Cardiogenic Pulmonary Edema
-
HFNC has been shown to improve oxygenation, comfort, respiratory rate and heart rate in patients with AHRF.
-
However, HFNC has not shown a consistent and convincing benefit in intubation rates and survival in Cardiogenic pulmonary edema.
Preintubaton Oxygenation
-
HFNC is an acceptable way of providing oxygen to patients both before (preoxygenation) and during (to prevent desaturation) endotracheal intubation.
-
NIV for pre-oxygenation must be stopped during laryngoscopy, and thus does not enable oxygenation during intubation. In contrast, HFNC therapy can be continued uninterrupted throughout thereby provided prolonged non hypoxemic apnea time.
-
Post extubation respiratory compromise: Elective use of HFNC post extubation has been found to reduce reintubation rates in post cardiothoracic surgery, abdominal surgery or general ICU patients who are both at high or low risk for reintubation. HFNC performed equally well compared to NIV in these circumstances and was more acceptable to patients.
-
HFNC improves physiological parameters like respiratory rate, and increase end-expiratory lung volume.
-
It decreases the requirement for CPAP and re-intubation rates but does not improve P/F ratio and atelectasis.
-
Post extubation HFNC can be used successfully in prevention and treatment of postoperative respiratory failure.
During Invasive Procedures
-
Invasive procedures that are associated with hypoxemia.
-
Hypoxemic patients undergoing fibreoptic bronchoscopy can successfully be oxygenated with HFNC.
Chronic Obstructive Pulmonary Disease
-
HFNC therapy may be useful in stable hypercapnic COPD patients . It could also be used in acute setting for patients intolerant of NIV.
-
HFNC does not reduce frequency of COPD exacerbations but reduces the duration.
End-of-Life Care
-
HFNC is a useful modality for patients not suitable for intubation, or patients requiring palliative care.
Immunocompromised Patients
-
HFNC is feasible and safe in selected groups of immunocompromised patients with acute hypoxemic respiratory failure.
-
Careful patient selection is essential for the success of HFNC, as patients most likely to benefit are those with mild-to-moderate forms of acute hypoxemic respiratory failure if there are no contraindications (Table 4.3).
Step 3: Initiating HFNC Application
HFNC has following components (Fig. 4.3):
-
Gas source, blender: An air/oxygen blender, allows the inspiratory fraction of oxygen (FiO2) from 0.21 to 1.0 in a flow of up to 60–70 L/min. The flow rate (ranging from 5 to 60 L/min) and FiO2 (0.21 to 1) are set at the air/oxygen blender.
-
Humidifier: Humidity can be provided by a disposable vapour transfer cartridge, a heated plate humidifier or a bubble humidifier. The gas is heated and humidified through an active heated humidifier and delivered via a single-limb heated inspiratory circuit. The patient breathes the heated and humidified gas through nasal wide bore cannulas.
-
Nasal interface: Nasal cannulas are available in different sizes. Most interfaces have wide-bore, soft contoured nasal prongs designed to reduce gas jetting, while some use the traditional narrow-bore nasal cannula.
The gas is heated to 37 C and humidified 100% with the active humidifier and is delivered through the heated circuit through a nasal canula at high flow at least 60 L/min.
HFNC should be applied if there is no contradictions.
Connecting the Patient
-
Explain the therapy to the patient.
-
Check the proper sized nasal prongs that sits well into the nares. Nasal cannulae should fit snugly and it should be ensured that nasal cannulae occlude no more than 50% of the nostril.
-
HFNC can be started with flow rates of around 30 L/min. Flow rates should be increased in 5 to 10 L/min increments, aiming to reduce respiratory rate, or until further increases are not tolerated. Patient discomfort is usually due to the velocity of gas rather than the flow itself, and can be mitigated by using a large-bore cannula.
-
In case of persistent discomfort, the flow can be decreased down to a minimum of 30 L/min
-
-
Flows should be titrated to a maximum flow of 60 L/min depending on patient comfort.
-
Select the FiO2 to obtain the desired arterial oxygen saturation. Within 2 h it should be possible to reduce the FiO2 and clinical stabilization should be observed.
-
Set humidifier on the desired temperature. Temperature may be reduced if the patient complains that the gas is too warm.
Step 5: Monitoring of a Patient on HFNC
Monitoring should be done as in any other patient on any respiratory support ICU (Table 4.4).
-
HFNC therapy should be provided in controlled setting with close monitoring for signs of respiratory failure that necessitate intubation and mechanical ventilation.
-
Look for failure to adequately improve oxygenation within an hour of HFNC initiation, and increase of respiratory rate and presence of thoracoabdominal asynchrony. Discontinue if the patient is not improving or deteriorating. Delaying intubation increases mortality like in a patient on NIV.
-
In most cases, nebulized medication is given directly by mouthpiece and not delivered through HFNC equipment. However, aerosol delivery may not be guaranteed at high flows.
-
HFNC can be delivered in a less controlled environment once the patient is improving.
Step 6: Look for Complications and Treat them
-
HFNC is usually well tolerated and complications are rare in adults.
-
Blocked cannulae due to secretions.
-
Local trauma, discomfort and pressure areas, epistaxis, abdominal distension, aspiration, and, rarely, barotrauma.
-
Failure of HFNC may result in delayed intubation and worse clinical outcomes in patients with respiratory failure.
Step 7: Discontinuation of HFNC
-
This should begin with FiO2, while maintaining a steady flow rate.
-
Once FiO2 is <0.4 to 0.5, than reduce flow rates.
-
Convert to conventional low-flow oxygen once the flow rate reaches ≤20 L/min and FiO2 ≤ 0.4.
Step 8: Maintain HFNC Device
-
HFNC devices should be cleaned and disinfected before use in a new patient.
-
Consumables need to be replaced for every new patient.
-
For prolonged treatment, the breathing tube and humidifying chamber kit should be replaced every 14 days, and the patient interface every 7 days.
Conclusions: Much of the proven benefit of HFNC is subjective and physiologic. HFNC is an alternative to other high-flow systems and NIV. The choice between these systems depends on patient and clinician preference, need for ventilation and PEEP, severity of hypoxemia and institutional availability.
Suggested Reading
Guitton C, Ehrmann S, Volteau C, Colin G, Maamar A, Jean-Michel V, Mahe P, Landais M, Brule N, Bretonnière C, Zambon O, Vourc’h M. Nasal high-flow preoxygenation for endotracheal intubation in the critically ill patient: a randomized clinical trial. Intensive Care Med. 2019;45(4):447–5. Compared with standard bag mask oxygenation, preoxygenation with HFNC in the ICU did not improve the lowest SpO2 during intubation in the non-severely hypoxemic patients but led to a reduction in intubation-related adverse events
Hare A. High-flow nasal cannula therapy in adults. Clin Pulm Med. 2017;24(3):95–104. A review article
Helviz Y, Einav S. A systematic review of the high-flow nasal cannula for adult patients. Crit Care. 2018;22(1):71. A systematic review of the high-flow nasal cannula for adult patients
Hill NS. High flow nasal cannula, is there a role in COPD? Tanaffos. 2017;16(Suppl 1):S12. A reviw article
Mauri T, Turrini C, Eronia N, Grasselli G, Volta CA, Bellani G, et al. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195:1207–15. HFNC exerts multiple physiologic effects including less inspiratory effort and improved lung volume and compliance in acute hypoxemic respiratory failure. These benefits might underlie the clinical efficacy of HFNC
Nishimura M. High-flow nasal cannula oxygen therapy in adults. J Intensive Care. 2015;3:15–23. A review article
Ou X, Hua Y, Liu J, Gong C, Zhao W. Effect of high-flow nasal cannula oxygen therapy in adults with acute hypoxemic respiratory failure: a meta-analysis of randomized controlled trials. Can Med Assoc J. 2017;189(7):E260–7. The intubation rate with HFNC oxygen therapy was lower than the rate with conventional oxygen therapy and similar to the rate with noninvasive ventilation among patients with acute hypoxemic respiratory failure
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Chawla, R., Todi, S. (2020). High Flow Nasal Canula (HFNC). In: Chawla, R., Todi, S. (eds) ICU Protocols. Springer, Singapore. https://doi.org/10.1007/978-981-15-0898-1_4
Download citation
DOI: https://doi.org/10.1007/978-981-15-0898-1_4
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-0897-4
Online ISBN: 978-981-15-0898-1
eBook Packages: MedicineMedicine (R0)