Abstract
The development of needle and syringe exchange programs (NSPs) in China can be divided into two stages: the pilot (1997–2003) and the expansion (2003 to the present). During this time, the national approach to NSP transitioned from absolute prohibition to the publicly funded provision of these services for people who inject drugs (PWID) in areas without methadone maintenance treatment (MMT). While NSP has shown effectiveness at reducing HIV transmission and injection behaviors, there are implementation challenges to be addressed. Currently, there is limited coverage of ancillary services provided through NSP, insufficient provision of high-quality clean needles and syringes, lack of civil society involvement, discrimination, stigma against PWID, and difficulties in managing peer educators. Proposed recommendations include intensified advocacy for NSP targeted toward relevant government departments, merging of redundant NSP sites, strengthened quality control of NSP, increased provision of female-friendly services, and more rigorous evaluation of NSP effectiveness. The Chinese government has made significant progress in the evolution of NSP policy and has gained significant experience through research and practice. In conjunction with MMT services, NSP can contribute to the control of HIV transmission among PWID, and there is evidence in favor of further program expansion.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
This chapter will provide an overview of needle and syringe exchange programs (NSPs) in China as for people who inject drugs (PWID). NSPs are defined as “a legal harm reduction strategy to promote and increase the… availability and accessibility of sterile needles and syringes, using peer influence or other types of information and education strategies to promote these items, and to discourage the practice of sharing used injecting equipment among [PWID]” (Yap et al. 2002).
1.1 Historical Overview of Drug Use and HIV/AIDS in China
1.1.1 The First (1839–1842) and Second (1856–1860) Opium Wars
The use of opium in China started as early as the seventh century for medicinal and recreational purposes, and in the seventeenth century, Europeans introduced the practice of mixing opium with tobacco for smoking (Ebrey 2010). In the eighteenth century, the strong demand for Chinese tea drove large trade imbalances which favored China over European nations, including Great Britain. The British had colonized India and controlled its poppy fields. With the rise of opium/tobacco smoking in China leading to an increased demand for opium, the British sold opium to Chinese drug smugglers, thus ameliorating its trade problems.
As an increasing proportion of China’s population became dependent on opium, this sowed discord in China’s civil society and economy. Chinese authorities counteracted these growing problems by issuing increasingly strict bans on opium imports. Following the first edicts of 1729 and 1799, the Chinese Emperor decreed even more stringent laws against the importation and sale of opium in 1814 and 1831 to little effect. Opium dependency was widespread and affected many of the country’s high-ranking government leaders and military officers. Corruption became rampant during this period. With the growing number of citizens addicted to opium, the Daoguang Emperor took drastic steps to prohibit all opium trade in China. Court officials who advocated suppression superseded rival officials who supported legalization and taxation. In 1838, the Emperor sent Lin Zexu, a high-ranking scholar-official to Guangdong province, which was a major opium trading center. Upon his arrival, Lin arrested Chinese dealers and attempted to persuade foreign merchants to exchange their opium supplies for tea. When the foreign sellers did not comply, Lin forcefully seized and destroyed over 1.2 million kg (2.6 million lbs) of opium.
These actions prompted a series of events instigating the First Opium War, which lasted from September 1839 to August 1842. The war ended with a British victory and the signing of the Treaty of Nanking, the first in a series of “Unequal Treaties.” The Treaty of Nanking committed the Chinese to permitting free trade in opium, opening five ports to foreign merchants, ceding Hong Kong, and paying reparations. China suffered humiliating defeats in the First Opium War (1839–1842) to Britain and the Second Opium War (1856–1860) to Britain and France. By the end of the second war, having been occupied by foreign forces, China lifted the remaining restrictions on opium imports.
As a result of the treaties, China was forced to legalize of the opium trade. Opium dependence was widespread for most of the next century. In the early 1900s, scholars estimated that China was home to 21.5–25 million opium users, including nearly one in four men (Tibke 2017). For a more in-depth discussion of the history and aftermath of the opium wars, recommended books include “Imperial Twilight: The Opium War and the End of China’s Last Golden Age” by Stephen R. Platt and “The Opium Wars: The Addiction of One Empire and the Corruption of Another” by Frank Sanello and William Travis Hanes.
1.1.2 Opium After the Founding of the People’s Republic in 1949
Led by Mao Zedong, the People’s Republic of China was established in 1949. At the time, there were more than one million hectares of opium poppy growing in China and approximately 20 million opium users, accounting for 4.4% of the population. This proportion was as high as 25% in Yunnan province and 22% in Guizhou province (Zhang et al. 2004). The central government detained millions of drug users, executed dealers, and replanted opium-growing areas with new crops. On February 24, 1950, Premier Zhou Enlai issued a decree on the “prohibition of opium production, trade and consumption.” Opium control committees were established at multiple levels of government, starting at the county level. Four major national actions were implemented to achieve total prohibition of drug use: (1) registering opium users and seizing opium supplies, (2) setting up detoxification stations, (3) eliminating poppy cultivation, and (4) handing down draconian punishments for those convicted of trading drugs. Emphasis was placed on antidrug trafficking.
Additional efforts were developed and implemented in in southwest China, where opium use was higher. The “Regulation on Drug Control” was issued on May 1950 with the following targets:
-
1.
Closure of all “opium dens,” confiscation of the properties, smoking paraphernalia and drug supplies, and punishment of owners with severe sentences, including capital punishment.
-
2.
Prohibition of drug transportation and selling.
-
3.
Education and rehabilitation of opium users, both voluntary and coerced.
-
4.
Policy of “relief by production” for poppy-growing regions, wherein local governments assisted farmers in growing alternative crops with the condition that the farmers would need to repay the government after the harvest.
Through these measures, poppy cultivation was nearly eliminated in southwest China by 1951. Many drug traffickers were sentenced to death in Xi’an, Chengdu, Chongqing, Kunming, and other major cities. Large quantities of opium were burned in public. Through these measures, the newly established government sought to wipe out centuries of drug use in only 3 years. In 1953, China asserted that it had become a “drug-free nation” (Zhang and Chin 2015).
1.1.3 Opioid Trafficking and the Start of China’s HIV/AIDS Epidemic
China implemented major economic reform through the open-door policy in late 1970s, which had profound consequences for illicit drug use. A more permissive flow of goods between China and neighboring countries allowed opioid trafficking routes to emerge. China borders two major heroin-producing regions: the Golden Triangle (Myanmar, Laos, and parts of Thailand) along the southwest border and the Golden Crescent (Afghanistan, Iran, Pakistan) along the western border.
The Golden Triangle, particularly Myanmar, has been a major center of opium poppy cultivation (Chalk 2000). By the mid- to late 1980s, principal drug trafficking routes crossed from Myanmar into Yunnan province and from Vietnam into Guangxi province. The drugs were transported over inland routes passing through Sichuan, Guizhou, Gansu, Guangdong, and, less commonly, Xinjiang (Qian et al. 2006). The final destinations were usually North America, Australasia, and Northeast Asia (Chalk 2000). While most was export to other countries, the domestic demand for opioids also grew. In 1991, the number of drug users registered with public security was 148,000, a figure which rose quickly to 520,000 by 1995 (Li and Li 2013).
As has been seen in other countries, the channels for moving opioids are physical determinants of the spread of the HIV/AIDS epidemic (Rhodes et al. 2005). Using molecular epidemiology, researchers were able to link HIV subtypes to specific trafficking routes and pinpoint the flow of drugs through southern China (Beyrer et al. 2000). The first HIV outbreak in China was identified in 1989 among PWID in the city of Ruili in Yunnan province, which lies along the border with Myanmar (Ma et al. 1990). Numerous studies from the early 1990s warned that high needle sharing among PWID was the source of rapid HIV transmission and suggested prevention efforts, such as encouraging PWID to sterilize needles by bleaching (Wu et al. 1996; Xia et al. 1994; Zheng et al. 1994; Zheng 1991).
By 1995, HIV prevalence among PWID in Yunnan had risen to over 20%, and 12 of the 17 prefectures reported at least one case of HIV infection (Chen et al. 1996; Lu et al. 2004; Xiao et al. 2007). Nationally, only one of eight national sentinel sites for PWID reported HIV cases in 1995, but this low prevalence did not hold. Two years later, three of 22 surveillance sites reported an average of 6.6% prevalence among PWID (Qian et al. 2006). From there, the HIV epidemic in China spread quickly over the next 5 years. By 2002, all 31 provinces, autonomous regions, and municipalities on mainland China reported HIV infections among PWID, and individual sites started to report alarmingly high HIV prevalence in this population, including 14% in Jiangxi, 16–20% in Sichuan, 17–19% in Guizhou, and 15–20% in Hunan (Qian et al. 2005). Throughout the 2000s, the national average HIV prevalence among PWID hovered around 10% (Zhang et al. 2013).
2 Overview of Needle and Syringe Exchange Programs
To address the dual epidemics of injection drug use and HIV/AIDS, China was pushed to adopt public health strategies. A number of countries had set up opioid substitution treatment programs as well as NSPs. The first NSP was started in Amsterdam, The Netherlands, in 1984 to control the spread of hepatitis B and was soon followed by initiatives in other countries (Heimer et al. 1998; Lurie et al. 1998; Strathdee et al. 1999). In the 1980s and early 1990s, the rise of the HIV epidemic among PWID motivated a more widespread adoption of harm reduction programs, including NSPs. Out of the urgent need to curb drug-related behavior and crime, China followed suit in establishing methadone maintenance treatment (MMT) clinics and NSPs (see Chap. 9 for more information). As of 2018, NSPs operate in 86 countries (Stone and Shirley-Beavan 2018).
NSP is a social service based on the pragmatic principle of harm reduction, which is aimed at minimizing negative consequences associated with drug use (Marlatt 1996). At NSP sites, PWID may obtain clean hypodermic needles and associated injection equipment for free or at a non-prohibitive cost. Many programs are called “exchanges” because some programs require exchanging used needles for an equal number of new needles in order to encourage the safe disposal of used equipment. Access to sterile needles and syringes are considered a standard component of a comprehensive HIV prevention program for PWID. The international acceptance of NSPs is indicative of a practical approach to HIV prevention and an endorsement of public health evidence, which is conclusive that NSPs do not encourage drug use and that needle exchanges can be effective in reducing HIV incidence (Fernandes et al. 2017; Smith et al. 2012).
NSP is strongly endorsed by the World Health Organization (WHO). There is well-established evidence that HIV transmission through blood may be effectively averted through needle exchanges as these programs empower PWID to protect themselves and others from HIV (Aspinall et al. 2014; Fernandes et al. 2017; UNAIDS 2010). NSP may also reduce hepatitis C infection, although the research on this is inconclusive (Fernandes et al. 2017; Platt et al. 2017). By offering an accessible alternative to needle sharing, HIV transmission within PWID communities can be brought under control. Other data show that NSPs help people stop drug use through referral to drug treatment programs (Lurie et al. 1993). With sufficient coverage, NSPs in low- and middle-income countries can reach similar effectiveness at reducing HIV transmission as NSPs in high-income countries (Des Jarlais et al. 2013).
There is also widespread research showing that NSPs are cost-effective (Lurie et al. 1998; Wodak and Cooney 2006; Zhang et al. 2011). Wilson et al. (2015) estimated that the operation of NSPs cost $23–71 per person per year. Compared to the costs of providing a lifetime of antiretroviral therapy (ART), NSP is an extremely inexpensive intervention, and this finding has been reaffirmed by studies in countries across a spectrum of financial and geographical settings. Each infection averted through NSP implementation can save significant public health resources.
3 History of Needle and Syringe Exchange Programs in China
3.1 Evolution of Policies
The Chinese government issues national statements to lay out its priorities and to establish multiyear action plans for HIV prevention and control. China’s policies toward harm reduction—particularly NSPs—have evolved dramatically over the past two decades (Hammett et al. 2008). Recent national policies have specifically stated official support for the provision of NSPs (see Table 10.1). In the action plan for 2001–2005, NSPs were explicitly noted as implementation aims: “Needle and syringe social marketing will be actively conducted. Clean needle and syringe usage will be promoted” (The State Council 2001). This was followed by a speech in 2004 by State Council Premier Wu Yi: “Pilot needle and syringe exchange programs implemented in recent years has been proved to be effective. It should be unswervingly scaled up in the future to prevent further HIV transmission among injecting drug users” (Wu 2004). The 2006–2010 action plan stated that it was necessary to “scale-up needle and syringe exchange programs to reduce HIV transmission among drug users” and that “clean needles and syringes should be provided to no less than 50% of injecting drug users in areas with needle and syringe exchange programs by the end of 2010” (The State Council 2006a). Further State Council documents that have explicitly supported NSPs as effective intervention measures have been published in 2006 and 2010 (The State Council 2006b, 2010). Similar recommendations of NSP also appeared in the latest action plans—notably, China’s 12th and 13th Five-Year Action Plan for HIV Prevention and Control states that “comprehensive intervention measures should be implemented among drug users [and] continuously implement needle and syringe exchange program in areas without methadone maintenance treatment services” (The State Council 2012, 2017).
At the provincial level, Guangxi, Yunnan and Xinjiang have led the way in strengthening harm reduction interventions (Hammett et al. 2008). Despite the established science showing the effectiveness of NSP and other harm reduction services, China’s support for NSP should not be taken for granted. China’s embrace of a harm reduction strategy has required years of painstaking educational and collaborative efforts between multiple governmental agencies with competing priorities (Hammett et al. 2008). Significant investment of political capital is needed to successfully establish and scale up NSPs, often in an environment of public misunderstanding. Harm reduction in many other countries continue to face entrenched opposition (Stone and Shirley-Beavan 2018). In 2018, NSPs operate in only 86 countries, less than half of the 179 countries reporting injecting drug use (Stone and Shirley-Beavan 2018).
3.2 Pilot Programs and Initial National Expansion
The first NSP in China was started in 1998 as a pilot program in Longchuan county, Yunnan province (Li and Li 2013). The program provided approximately 300 clean needles and syringes to PWID. An initial evaluation on acceptability found that the program was received positively among PWID, which was an encouraging sign for further program development. A larger second acceptability and feasibility study was conducted a year later (Yang et al. 2003). From August 1999 to September 2001, researchers from the Yunnan Institute for Drug Abuse studied the acceptance and feasibility of NSPs at three clinics. Over the course of 2 years, clean needles and syringes were made available to PWID who visited the clinics. Focus group discussions and in-depth interviews revealed high acceptability by PWID and their relatives (Yang et al. 2003). However, some resistance from the clinic staff was noted. Clients were not followed through the study so changes in needle-sharing behavior could not be measured.
In 2000, the National Center for AIDS/STD Control and Prevention (NCAIDS), Chinese Center for Disease Control and Prevention (CDC), conducted a study in Guangxi province (Ming et al. 2005). Health workers and peer educators provided clean needles and syringes, collected used injection equipment, disseminated health education pamphlets, and provided face-to-face health counseling for 1 year. PWID completed questionnaires on HIV risk and injection practices behaviors before after the pilot intervention. In 1 year, the program was able to halve the number of PWID reporting needle sharing from 60.6% at baseline to 30.3% at the end.
To evaluate the effectiveness of NSP in China more rigorously, NCAIDS researchers launched a prospective community-randomized HIV prevention trial in 2001 (Wu et al. 2007). Four counties and townships in Guangxi and Guangdong provinces were selected with one randomized to intervention and the other to control in each province. An NSP program, including promotion of safe injection norms and increased access to clean needles over a 12-month period, was provided to PWID. Cross-sectional surveys at baseline and follow-up compared changes in drug-using behaviors and HIV and HCV incidence in the intervention and control communities. The results revealed that needle-sharing behaviors were similar in the two groups at baseline (68.4% vs. 67.8%), and dropped significantly to 35.3% in the intervention community and remained relatively stable in the control community (62.3%) after a 12-month intervention.
The first bilateral cross-border intervention to include Chinese PWID was supported by the US National Institutes of Health and the Ford Foundation and led by an international team of experienced researchers. The intervention used peer educator outreach to facilitate a large-scale distribution of sterile needles and syringes, ampoules of sterile water, and condoms (Des Jarlais et al. 2007; Hammett et al. 2012). Starting in 2002, implementation took place at five sites in Lang Son province, Vietnam, and four sites in Ning Ming County, Guangxi province, China, and in each country, an average of 10,000–15,000 needles and syringes were distributed per month. The intervention yielded drastic reductions in HIV prevalence as measured by serial cross-sectional surveys: compared to baseline, HIV prevalence and incidence fell by approximately half after 2 years and by three quarters at 3 years in both countries (Table 10.2).
These early pilot programs showed promise for the feasibility and acceptability of NSP in China (Lin et al. 2004; Yap et al. 2002). Program officials and local stakeholders gained valuable knowledge on the implementation of NSP. The Chinese central government has designated special annual funds for HIV prevention since the early 2000s. The Chinese Ministry of Health (which has been superseded by the National Health Commission) launched the China Comprehensive AIDS Response Program (China CARES) starting in 2003, covering a total of 127 counties (Han et al. 2010). Fifty-eight out of 127 counties named the prevention of HIV transmission among PWID as a core issue, signaling a prioritization of harm reduction measures. Officials established MMT programs in counties with more than 500 registered drug users and NSP services in counties with lower than 500 registered drug users. By the end of March 2008, over 250 NSP sites had been established across 50 counties and had served over 45,000 PWID (Wu 2008). Following the approach set by the UK project, NSP included fixed and mobile services. Furthermore, new models of NSP were adapted for local contexts, including services at health institutions at subcounty (i.e., village and township) administrative levels. These new delivery models allowed NSP to be more flexible, tailored, and accessible for local PWID populations (China Comprehensive AIDS Response Program office 2009).
3.3 International Cooperation
Through much of the 2000s, expansion of NSP access in China was facilitated through support from international programs (Wu et al. 2011). Several major programs are discussed below: World Bank Loan Health Nine Project-HIV/STD Prevention and Control, China-UK HIV Prevention and Care Project, China-Australian Agency for International Development HIV Asian Regional Program in Guangxi Autonomous Region and Yunnan Province, and the China-Australia HIV Prevention and Care Program in Xinjiang Uyguar Autonomous Region.
The World Bank Loan Health Nine Project-HIV/STD Prevention and Control was supported by the World Bank from July 1999 to June 2008. One of the primary goals of the project was to achieve improved prevention and control of HIV/AIDS, other sexually transmitted, and other blood-borne infections by “implementing comprehensive and multi-sectoral public health programs at the provincial level, and by building technical capacity at the central level” (World Bank 2009). The program sought to develop a series of innovative, replicable, and cost-effective measures for HIV/STD prevention and control at the national level as well as four provinces with high HIV burdens: Fujian, Guangxi, Shanxi, and Xinjiang.
With the support of the Health Nine Project, China made several substantial advancements in NSP scale-up. In 2004, experts developed a manual to standardize the implementation of NSP based on experiences from China’s pilot programs. The manual was distributed to sites across China. The Health Nine Project also held workshops to put together different stakeholders and program officials to increase communication across sites. A harm reduction workshop among drug users was held in Sichuan province in 2003. A conference on harm reduction in Sichuan province in 2003 was the first professional workshop on interventions for PWID in China, and it was attended by delegates from six provinces, including Sichuan, Guangdong, Guangxi, and Xinjiang. A related workshop on HIV prevention services for PWID was held in Xinjiang in 2005. This brought together provincial health officials sixteen provinces to share perspectives and evidence on best practices among drug users for scaling up programs, including NSP (Wang et al. 2008).
Other ongoing programs were supported through bilateral funding, most notably from the United Kingdom’s Department for International Developent (DFID) and Australia’s Agency for International Development (AusAID). The China-UK HIV/AIDS Prevention and Care Project ran from August 2000 to June 2006 in Yunnan and Sichuan provinces with the aim of building scalable treatment and care interventions and to increase technical capacity of HIV response infrastructure. A major component of the UK project was the training of peer educators to disseminate knowledge on HIV prevention among PWID (Project Office of China-UK HIV/AIDS Prevention and Care Project 2006). The first NSP supported by the UK project was initiated in March 2002; by the end of the project, NSP had been implemented in 17 counties in Sichuan and 19 counties in Yunnan. In urban areas, fixed-site NSPs were established at easily accessible sites, while mobile NSPs were created for rural areas. Staff assigned to mobile NSPs included peer educators who undertook fieldwork to identify PWID in need of services. The implementation of these two NSP models increased acceptability and further expanded coverage of NSP.
AusAID also sponsored key NSP projects. The China-AusAID HIV/AIDS Asian Regional Program ran from July 2002 to June 2012. An objective of the project was to reduce HIV transmission by providing a community-based comprehensive intervention among PWID in Guangxi and Yunnan, which had the most serious drug epidemic in China. NSP was implemented in all of the six project counties in Guangxi and 19 project counties in Yunnan. More than 20,000 PWID received clean needle and syringes from the project and about 16,000 PWID were referred to MMT, ART, or HIV testing (Project Office of China-Australian Agency for International Development HIV/AIDS Asian Regional Program 2012).
AusAID also supported a China-Australia HIV Prevention and Care Program in Xinjiang from March 2002 to February 2009 (Zeng 2006; Wu et al. 2011). The program was implemented in four counties in Xinjiang with the aim of reducing needle sharing. An estimated 4000 PWID were involved in the program. More than 2500 PWID were referred to either HIV testing, ART, or MMT. The final evaluation survey indicated that proportion of needle sharing was reduced to 12%. The NSP in Xinjiang has been lauded by the HIV special ambassador of the secretary-general of the United Nations and experts from the WHO (Xinjiang Autonomous Region Center for Disease Control and Prevention 2008).
The Global Fund AIDS Program Round Four was approved under these circumstances in 2005. The aim of the project was to reduce HIV transmission among PWID and FSW through intervention measures including health communication campaigns, voluntary counseling and testing, MMT, NSP, condom promotion, STI management, and ART. The target areas included 76 counties from seven provinces with high levels of drug use—Guangxi, Guizhou, Hunan, Jiangxi, Sichuan, Xinjiang, and Yunnan. More than 110 NSP sites were established supported by the project (Office for Global Fund AIDS Program Round Four 2010) (Tables 10.3 and 10.4).
3.4 Current NSP Status
In China, the drug user population is approximately 2.5 million; among these individuals, around 40% use opiates (Degenhardt et al. 2017; National Narcotics Control Commission 2016). For centuries, the most widely used class of illicit drugs was opioids—specifically opium and heroin—but in the mid-2010s, synthetic drugs, such as crystal methamphetamine and ketamine, rose sharply in popularity (Zhang and Chin 2015). In China, at the latest count in 2017, 12 provinces had implemented NSP with a total of 741 sites. These sites distributed 11 million needles to over 56,000 PWID, making China one of the highest distributors of needles in Asia (National Health and Family Planning Commission 2015; Stone and Shirley-Beavan 2018). The number of approximately 200 needles and syringes per attendee per year has been consistent since 2008 (Stitzer 2006).
NSP is effective in achieving reductions in HIV transmission in China. Evidence indicates that both HIV and HCV incidence can decrease after the establishment of an NSP intervention in China (Wu et al. 2007). This finding is consistent with multiple subsequent reports that PWID who had ever used NSP services were significantly less likely to have HIV infection, compared with those who had never used NSP services (Luo et al. 2013; Wu et al. 2017). Overall, there is compelling evidence that NSP significantly reduces needle-sharing behavior among PWID in China (Bao et al. 2007; Chen et al. 2007; Ma 2004; Qu et al. 2006; Xia et al. 2009; Xue et al. 2011).
There are several models of NSP service delivery adopted across China. Services may be managed and located at a range of venues: CDCs, community health service centers, township hospitals, village clinics and pharmacies. NSPs managed and staffed by the local CDC are the most common and are usually housed at the same physical site. In many counties, clean needles are also available at pharmacies for legal purchase. Clients can travel to an NSP service site to obtain clean needles. Alternatively, some NSPs have staffs, clinicians, or peer educators who make visits to homes and to areas where PWID tend to congregate (Table 10.5).
The most effective NSPs have several shared characteristics:
-
1.
Establishing multi-sectoral cooperation across different governmental divisions: health department, public security bureaus, narcotics control divisions, and local community organizations.
-
2.
Conducting a comprehensive needs assessment prior to program initiation to better understand the needs of the local PWID.
-
3.
Providing a range of services to supplement needle and syringe exchange, such as counseling, condom distribution, and referrals to MMT.
-
4.
Adapting NSP models based on the geographical distribution of the clients.
-
5.
Engaging peer educators who are at the core of recruitment of PWID, distribution of clean needles and syringes, and collection of used needles and syringes.
3.5 Relationship Between MMT and NSP
NSP and MMT have both been effective intervention measures in reducing HIV prevalence and incidence in China (see Chap. 9 for information). However, these two services have been met with unequal public receptions. MMT has attracted more attention and is much more favorably received by the public compared to NSP. As a biomedical intervention, MMT is more easily understood by the public and allows people to better conceptualize drug dependence as a complex disease, rather than a moral failing. While MMT can directly facilitate the cessation of opioid use, clients who attend NSP still continue to actively use drugs, and this leads to a common misconception that providing free or subsidized injection equipment suggests tacit government consent toward drug use (Koo et al. 2015).
Both NSP and MMT are key components of a comprehensive harm reduction package for PWID. There is long-standing evidence that engagement in NSP can promote enrollment in MMT, which is a strong argument in favor of NSP implementation (Hagan et al. 2000; Strathdee et al. 1999; Wodak and Cooney 2006). The provision of NSP—both independently and in conjunction with MMT—has a critical role in HIV prevention. NSP can address several weaknesses of MMT. First, MMT clinics require a heavier investment of time, money, and workforce training. There are also legal restrictions on the locations of MMT clinics and the availability of methadone (Disease Control Bureau 2006). MMT clinics require highly trained staff members who are familiar with the clinical management of methadone dosage, including the relationship to overdose (Marienfeld et al. 2015). Particularly in rural areas, it may be difficult to accumulate enough financial and human resources support. Where MMT clinics cannot be feasibly established for logistical or cost-effectiveness reasons, NSP can fill a gap in HIV prevention services. Furthermore, MMT programs often struggle with high rates of active drug use during MMT as well as attrition from treatment. Current or previous MMT clients who continue to inject drugs can still utilize NSP to decrease the risk of HIV and HCV transmission. NSP can also maintain a degree of connection between clients and the harm reduction infrastructure. Finally, there are also some PWID who refuse MMT out of a fear of being identified by government officials. NSP may be an acceptable alternative to these clients because no real-name identification is required to obtain or exchange needles.
4 Challenges
A multifaceted range of challenges affect NSPs, and some are described below. While some are unique to China, others are universal barriers to NSP implementation.
4.1 Decreased Support from International and Local Nongovernmental Organizations (NGOs)
As described above, international cooperation has had an instrumental role in scaling-up of NSP in China by providing financial support, technical capacity, and training. Major funding has been provided by the World Bank, the UK’s DFID, AusAID, and the Global Fund (Liu et al. 2007). In recent years, with China’s increasing economic power, international organizations have withdrawn or successively decreased their HIV-related grants to China. Funding from DFID, World Bank, and AusAID ended in 2006, 2008, and 2012, respectively. Most notably, the Global Fund withdrew its aid to China at the end of 2012, which prompted a transition period for China’s HIV funding strategy. NSP have a more uncertain future in China because of the loss of international funding; moreover, the loss of technical support has also posed a challenge to the sustainability of NSP. While the Chinese central government continues to fund NSP, the cumulative annual amount has dropped markedly, which has been reflected in a reduction of NSP sites. The decentralization of the Chinese health system also means that support for NSP is highly variable across local governments, fluctuating based on the level of regional economic development and government officials’ attitude toward NSPs. In addition, as sexual transmission has become the predominant HIV transmission mode in China, health officials and staff in some areas that formerly dealt with a dual epidemic of drug abuse and HIV have felt that China’s HIV response should be reorienting priorities and shifting resources toward other key risk populations, particularly men who have sex with men.
Although roughly half of NSPs in China were funded by international organizations, the majority of NSPs are run or implemented primarily by the China government agencies and with little involvement from domestic NGOs. However, local NGOs have their own unique strengths that allow them to implement NSP effectively, which have not been sufficiently leveraged. NGOs work on the ground and have intimate links with drug users, instilling trust in their clients in this service. NGOs’ active involvement in implementation should be increased to complement government-run NSP sites.
4.2 Conflicts with Public Security
Although support for harm reduction including NSPs has been written into national and provincial policies, there is resistance from some government divisions. A major barrier to NSP implementation is the lack of support from public security officials; in a national survey, two-thirds expressed negative attitudes toward NSP (NCAIDS 2011; Zhang et al. 2015). In a separate qualitative study, officers from the Narcotics Division of Public Security in Hunan province were interviewed (Koo et al. 2015). Although the Narcotics Division has joint responsibility (with the CDC and the health bureau) for coordinating NSPs, 24 of 32 questioned the legitimacy of NSPs, and 16 thought that NSPs encouraged ongoing drug use. This degree of hostility toward NSPs is a clear impediment to the stated public health aims.
Local public security staff are known to harass and arrest NSP attendees. Police in China are authorized to place drug users in involuntary detention for up to several months (Huang et al. 2011). Thus, as might be expected, most PWID are fearful of being arrested if police see them at an NSP site (Sullivan and Wu 2007). However, despite China’s scaled-up network of compulsory detoxification centers, there is no compelling evidence that enforced rehabilitation yields positive health outcomes (Stone and Shirley-Beavan 2018; Sun et al. 2001; Werb et al. 2016). On the contrary, compulsory treatment centers may expose PWID to increased harm if access to HIV testing and treatment is not reliable (Tibke 2017). The current punitive legal framework and unsupportive social environment undermines the confidence of NSP staff and deters PWID from attending NSPs and MMT. Without improved coordination of public health and policing strategies, the full benefits of harm reduction cannot be delivered.
4.3 Low Service Coverage
NSPs in China lack adequate coverage to have a maximal impact on the HIV epidemic among PWID. Currently, NSP services are accessed by approximately 56,000 PWID, a figure that has decreased over recent years and represents a minority of Chinese PWID. Approximately 200 needles/syringes per PWID are distributed annually—a figure well short of what is required to curb HIV epidemic (Burrows 2006). In 2016, the WHO revised their recommendation for NSPs to provide 300 needles per PWID per year by 2030, and China will require substantial efforts to meet this target (Stone and Shirley-Beavan 2018).
Services provided at individual sites could also be subpar. Insufficient outreach, peer education, and lack of awareness of NSP may be dampening NSP access, which has been noted in qualitative studies (Philbin and Zhang 2014; Stone and Shirley-Beavan 2018). The majority of the NSPs in China run by local CDCs provide services during normal working hours (Wang et al. 2016). Other delivery services such as mobile vans, vending machines, and night services have demonstrated effectiveness in other countries (Miller et al. 2002; Wood et al. 2003). However, these service delivery strategies are rarely used in China.
The service levels and other components of NSPs vary across the country. The concentration of NSP sites differs greatly across the country, and NSP is completely unavailable in some provinces. Notably, 90% of NSP sites are located in the seven provinces with the highest levels of drug use. Sites are highly variable, which is seen in the number of PWID served and the number of clean needle and syringes distributed, which can range from dozens to thousands per year per person. Furthermore, there are disparities in comprehensiveness of services provided; some stations only provide clean needle and syringes, while others provide supplementary services, including referrals to MMT, ART, and employment opportunities.
4.4 Discrimination and Stigma
PWID face high levels of societal discrimination and stigma in their communities. Only one-third of respondents to a national survey had a positive attitude toward NSP (NCAIDS 2011). It was even reported that 30.9% of attendees of NSP reported experiencing discrimination and stigma from NSP site staff, who should be advocates for their clients (Sun et al. 2013). As mentioned above, local public security officers and neighborhood residents often think that NSPs encourage continued drug injection (Koo et al. 2015). Some communities and residents also worry that the establishment of an NSP site would cause PWID to gather and cause neighborhood crime to increase. Even if they tolerate the establishment of a nearby NSP, non-PWID community members rarely became involved in supporting the program. Stigma toward people living with HIV, including PWID, is directly linked to diminished access to HIV care, lower HIV medication adherence, and poorer mental health (Wolfe et al. 2010).
4.5 Ancillary Services Provided in NSP Need to Be Expanded
In order to effectively reduce HIV transmission, NSPs in China also should provide ancillary services such as HIV testing and counseling in addition to distributing clean needles and reclaiming used needles. However, despite the need for these additional services, their availability remains very limited. NSP sites should be an important platform for offering comprehensive services and interventions to PWID such as primary medical care, HIV testing and counseling, condom distribution, and overdose prevention. Comprehensive services not only promote the health of PWID but also attract more PWID to be engage with NSPs.
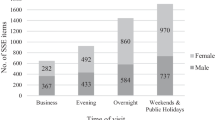
Services should also be adapted for gender sensitivity. The proportion of female PWIDs is much smaller than male PWIDs (15% vs. 85%) (NCAIDS 2011). However, there still needs to be a focus on female PWID needs as they are more vulnerable to acquiring HIV than male PWID due to biological and social vulnerability as well as a high possibility of involvement in sex work to maintain drug use (Hail-Jares et al. 2016; Tang et al. 2015). Furthermore, female PWID are rarely able to inject first when sharing drugs and needles. To date, there are very few harm reduction services that have been tailored specifically for the needs of female PWID.
4.6 Management of Peer Educators Needs to Be Strengthened
In China, more than half of NSP attendees received clean needles and syringes and related information through peer educators (Li et al. 2013). The capacity, motivation, input of both the time and energy of peer educators, and their performance have greatly influenced the quality of NSP service (Xia et al. 2009). Accordingly, the management of peer educators is quite important to implementing a successful NSP; however, it is difficult to reliably monitor and evaluate peer educators’ performance. The current practice is to measure indicators such as the number of PWID recruited, the number of syringes distributed, the numbers of condoms and educational pamphlets distributed, and the number of referrals to HIV testing and counseling. However, the reliability of these numbers and service quality are hard to validate and properly evaluate.
4.7 Distributing Better Syringes
Syringes vary in design. Some are high dead-space syringes (HDSS) which retain substantially more blood—corresponding to a higher possibility of HIV exposure and transmission—than low dead-space syringes (LDSS). Therefore, NSPs should carefully select the type of syringes being distributed. HDSS usually have detachable needles, and fluid is retained in the needle, needle hub, and syringe tip; in contrast, LDSS have permanently attached needles that extend through the syringe tip to the base of the syringe barrel. LDSS only retain fluid in the needle itself. Studies have suggested that HIV transmission among PWID may not occur when most PWID in an area are using LDSS (Bobashev and Zule 2010). Despite this clear potential reduction in HIV risk, syringes distributed by NSP or sold on the market are almost all HDSS, and LDSS are rarely seen or known. It is necessary to evaluate the potential improvement in effectiveness of replacing HDSS with LDSS at NSPs.
In addition, low-quality needles and syringes provided by NSP might not be used by PWID even if given for free. Currently, at most NSPs in China, syringes are purchased by the provincial health bureau, which often results in only one size and type of needles and syringes being given out. As a result, injecting needs of PWID are often not met, and they may not willing to use the needles and syringes provided, especially low-quality ones. Funding and planning for the purchasing of NSP-distributed injection equipment needs to be flexible and carefully considered with input from local PWID themselves.
5 Future Recommendations
First, more advocacy for NSP is needed for relevant government departments to decrease stigma and discrimination, to improve coordination between agencies with competing motives, and to obtain more government support. There needs to be continued support of policies that can create an environment conducive to harm reduction, strengthen government financial support, and develop closer participation by NGOs at NSPs. PWID advocates and policymakers both play important roles, not only for the sustainability and expansion of NSP services but also for capacity building to deliver such services with the ultimate goal of reducing HIV transmission.
Second, some NSP sites in China should be consolidated. The number of NSPs in different provinces varies from none to over a hundred. The number of PWID attending each NSP also varies greatly from a few to hundreds per month. If less-utilized and redundant NSP sites are merged according to the distribution and needs of PWID, the limited available financial and staff support will be more concentrated, and these services can be provided in a more cost-effective way. By pooling site resources, it may be possible to provide additional or improved ancillary services, including services targeted toward female PWID.
Third, the impact of NSP on HIV transmission should be evaluated by a cohort study or serial cross-sectional surveys of HIV prevalence and risk behaviors among PWID. NSP in China has been implemented for years, but rigorous evaluation of its impact on HIV incidence has been relatively limited. Though a number of studies have focused on reductions in needle sharing and increases in condom use and HIV awareness, few studies have examined reduction of HIV infection among NSP attendees (Bao et al. 2007; Chen et al. 2007; Luo et al. 2013; Ma 2004; Qu et al. 2006; Xia et al. 2009; Xue et al. 2011). The available research points to NSP effectiveness, but the lack of large-scale studies demonstrating the impact of NSPs on HIV transmission may have to do with continuing debates on NSP validity and a hostile environment. A rigorously designed study with high enrollment of PWID and/or covering a large geographic region should be planned and implemented to observe the effects of NSP over time. With reliable data, the impact of NSP on HIV transmission could be evaluated to better align the goals of public health and public security and to create more political buy-in.
Finally, quality control for NSP needs to be strengthened. Local, rather than central, authorities are responsible for the running and managing the NSPs. While the decentralization of NSP has potential benefits (e.g., being more quickly responsive to the specific needs of local PWID), it has also resulted in considerable variability in the performance of sites depending on the level of local government support and staff capacity. As a guiding institution, NCAIDS could provide standardized management, such as developing implementation manuals, providing detailed guidelines, and strengthening supervision of local NSPs.
6 Conclusion
NSP is an important component of a comprehensive public health response to the HIV epidemic among PWID. Strong international evidence shows that NSPs are a highly cost-effective approach to significantly decrease HIV prevalence among this population. In China, NSPs have been operating for more than 15 years. The official Chinese government stance toward HIV prevention and harm reduction services, including NSP, have evolved significantly during this time. To its great credit, China’s national government has listened to the scientific research community’s recommendations and has prioritized the public health benefits of NSP, even when public security bureau and community opinions are wary or at worst, directly hostile. Experiences and lessons for operating successful NSPs have been earned through research and practice. Although many challenges still exist, there is no doubt that individuals have directly benefited from this service and will continue to do so. The goal of controlling HIV transmission among PWID can be achieved through NSP, especially in conjunction with MMT and HIV services. At a time when expansion of NSPs is urgently needed around the world, we hope that China’s experience can offer valuable insight for other countries investing in NSP scale-up.
References
Aspinall EJ, Nambiar D, Goldberg DJ, Hickman M, Weir A, Van Velzen E, Palmateer N, Doyle JS, Hellard ME, Hutchinson SJ. Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: a systematic review and meta-analysis. Int J Epidemiol. 2014;43(1):235–48.
Bao YG, Duo L, Zhang XD, Xue MH, Kong XS, Ma YX, Yang HM, Li MY, Yang LH, Zhao XR, He LP. The result analysis in drug users needle syringe comprehensive intervention activities at four counties in Yunnan. Chin J Prim Med Pharm. 2007;14(12):2025–7.
Beyrer C, Razak MH, Lisam K, Chen J, Liu W, Yu XF. Overland heroin trafficking routes and HIV-1 spread in south and south-east Asia. AIDS. 2000;14(1):75–83.
Bobashev GV, Zule WA. Modeling the effect of high dead-space syringes on the human immunodeficiency virus (HIV) epidemic among injecting drug users. Addiction. 2010;105(8):1439–47.
Burrows D. Rethinking coverage of needle exchange programs. Subst Use Misuse. 2006;41(6–7):1045–8.
Chalk P. Southeast Asia and the Golden Triangle’s Heroin trade: threat and response. Stud Conflict Terrorism. 2000;23(2):89–106.
Chen HH, Zhang JP, Kou JD, Zhang Y, Zhang XB, Jia MH, Bi XQ, Ma YL, Liang YB, Yang CJ, Pan SF, An XJ. The trend of HIV spread across the whole province of Yunnan—surveillance report of Yunnan 1995. Zhongguo Xing Bing Ai Zi Bing Fang Zhi. 1996;2:54–7.
Chen LK, Li WJ, Mai RJ, Liu CJ, Fan ZF, Chen ZF, Feng JP. Assessment of results of exchange of syringe among drug users in preventing the transmission of HIV/AIDS. China Trop Med. 2007;7(11):2138–42.
China Comprehensive AIDS Response Program Office. Evaluation report of China Comprehensive AIDS Response Program. Beijing: China Comprehensive AIDS Response Program Office; 2009.
Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, Stone J, Cunningham EB, Trickey A, Dumchev K, Lynskey M, Griffiths P, Mattick RP, Hickman M, Larney S. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–207.
Des Jarlais DC, Kling R, Hammett TM, Ngu D, Liu W, Chen Y, Binh KT, Friedmann P. Reducing HIV infection among new injecting drug users in the China-Vietnam Cross Border Project. AIDS. 2007;21(Suppl 8):S109–14.
Des Jarlais DC, Feelemyer JP, Modi SN, Abdul-Quader A, Hagan H. High coverage needle/syringe programs for people who inject drugs in low and middle income countries: a systematic review. BMC Public Health. 2013;13:53.
Disease Control Bureau, The Ministry of Health. Manual of community-based opiate substitution treatment among durg users. 2006.
Ebrey PB. Manchus and imperialism: the Qing Dynasty 1644–1900. In: Ebrey PB, editor. The Cambridge Illustrated History of China. 2nd ed. Cambridge: Cambridge University Press; 2010. p. 236.
Fernandes RM, Cary M, Duarte G, Jesus G, Alarcao J, Torre C, Costa S, Costa J, Carneiro AV. Effectiveness of needle and syringe programmes in people who inject drugs – an overview of systematic reviews. BMC Public Health. 2017;17(1):309.
Hagan H, McGough JP, Thiede H, Hopkins S, Duchin J, Alexander ER. Reduced injection frequency and increased entry and retention in drug treatment associated with needle-exchange participation in Seattle drug injectors. J Subst Abus Treat. 2000;19(3):247–52.
Hail-Jares K, Choi S, Duo L, Luo Z, Huang ZJ. Occupational and demographic factors associated with drug use among female sex workers at the China-Myanmar border. Drug Alcohol Depend. 2016;161:42–9.
Hammett TM, Wu Z, Duc TT, Stephens D, Sullivan S, Liu W, Chen Y, Ngu D, Des Jarlais DC. ‘Social evils’ and harm reduction: the evolving policy environment for human immunodeficiency virus prevention among injection drug users in China and Vietnam. Addiction. 2008;103(1):137–45.
Hammett TM, Des Jarlais DC, Kling R, Kieu BT, McNicholl JM, Wasinrapee P, McDougal JS, Liu W, Chen Y, Meng D, Doan N, Huu Nguyen T, Ngoc Hoang Q, Van Hoang T. Controlling HIV epidemics among injection drug users: eight years of cross-border HIV prevention interventions in Vietnam and China. PLoS One. 2012;7(8):e43141.
Han M, Chen Q, Hao Y, Hu Y, Wang D, Gao Y, Bulterys M. Design and implementation of a China comprehensive AIDS response programme (China CARES), 2003–08. Int J Epidemiol. 2010;39(Suppl 2):47–55.
Heimer R, Khoshnood K, Bigg D, Guydish J, Junge B. Syringe use and reuse: effects of needle exchange programs in three cities. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18(Suppl 1):S37–44.
Huang K, Zhang L, Liu J. Drug problems in contemporary China: a profile of Chinese drug users in a metropolitan area. Int J Drug Policy. 2011;22(2):128–32.
Koo FK, Chen X, Chow EPF, Jing J, Zheng J, Zhao J, Zhang L. Barriers and Potential Improvements for Needle and Syringe Exchange Programs (NSPs) in China: a qualitative study from perspectives of both health and public security sectors. PLoS One. 2015;10(6):e0130654.
Li Z. Current status and challenges of needle exchange program in China. In: Wang L, editor. Epidemic and Control of HIV/AIDS in China. Beijing: Beijing Publishing House; 2006.
Li J, Li X. Current status of drug use and HIV/AIDS prevention in drug users in China. J Food Drug Anal. 2013;21(4, Suppl):S37–41.
Li RJ, Lan GH, Li ML, Huang YM, Wang L. Analysis on impact factors of needle exchange program among injecting drug users in Guangxi. Chin J AIDS STD. 2013;19(7):507–13.
Lin P, Fan ZF, Yang F, Wu ZY, Wang Y, Liu YY, Ming ZQ, Li WJ, Luo W, Fu XB, Mai XR, Xu RH, Feng WY, He Q. Evaluation of a pilot study on needle and syringe exchange program among injecting drug users in a community in Guangdong, China. Zhonghua Yu Fang Yi Xue Za Zhi. 2004;38(5):305–8.
Liu B, Sullivan S, Wu Z. An evaluation of needle exchange programmes in China. AIDS. 2007;21(Suppl 8):S123–8.
Lu L, Jia MH, Zhang XB, Luo HB, Ma YL, Fu LR, Lu JY. Analysis for epidemic trend of acquired immunodeficiency syndrome in Yunnan Province of China. Zhonghua Yu Fang Yi Xue Za Zhi. 2004;38(5):309–12.
Luo W, Wu ZY, Poundstone K, McGoogan JM, Dong W, Pang L, Rou KM, Wang CH, Cao XB. Needle and syringe exchange programs and prevalence of HIV infection among intravenous drug users in China. Hoboken, NJ: Addiction; 2013.
Lurie PE, Reingold AL, Bowser B, Chen D, Foley J, Guydish J, et al. The public health impact of needle exchange programs in the United States and abroad. San Francisco, CA: University of California, Berkeley, School of Public Health; The Institute for Health Studies; 1993.
Lurie P, Gorsky R, Jones TS, Shomphe L. An economic analysis of needle exchange and pharmacy-based programs to increase sterile syringe availability for injection drug users. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18(Suppl 1):S126–32.
Ma GL. Evaluating the initial effectiveness of a syringe exchange program in reducing HIV-risk behaviors among injection drug users in a county of Guangxi province, China. Beijing: Master Peking Union Medical College; 2004.
Ma Y, Li Z, Zhang K, Yang W, Ren X. HIV was first discovered among injection drug users in China. Chin J Epidemiol. 1990;11(3):184–5.
Marienfeld C, Liu P, Wang X, Schottenfeld R, Zhou W, Chawarski MC. Evaluation of an implementation of methadone maintenance treatment in China. Drug Alcohol Depend. 2015;157:60–7.
Marlatt GA. Harm reduction: come as you are. Addict Behav. 1996;21(6):779–88.
Miller CL, Tyndal M, Spittal P, Li K, Palepu A, Schechter MT. Risk-taking behaviors among injecting drug users who obtain syringe from pharmacies, fixed sites, and mobile van needle exchanges. J Urban Health. 2002;79(2):257–65.
Ming ZQ, Wu ZY, Liu W, et al. Effectiveness of needle exchange combined with peer education among IDUs in Guangxi. China J AIDS/STD. 2005;11(3):188–91.
National Health and Family Planning Commission. 2015 China AIDS response progress report. 2015. http://www.unaids.org/sites/default/files/country/documents/CHN_narrative_report_2015.pdf.
National Narcotics Control Commission. Annual report on drug control in China 2016. Beijing: National Narcotics Control Commission; 2016.
NCAIDS. Evaluation report for needle and syringe exchange program in China (unpublished). 2011.
Office for Global Fund AIDS Program Round Four. Progress report of global fund AIDS program round four. 2010.
Philbin MM, Zhang F. Exploring stakeholder perceptions of facilitators and barriers to using needle exchange programs in Yunnan Province, China. PLoS One. 2014;9(2):e86873.
Platt L, Minozzi S, Reed J, Vickerman P, Hagan H, French C, Jordan A, Degenhardt L, Hope V, Hutchinson S, Maher L, Palmateer N, Taylor A, Bruneau J, Hickman M. Needle syringe programmes and opioid substitution therapy for preventing hepatitis C transmission in people who inject drugs. Cochrane Database Syst Rev. 2017;9:Cd012021.
Project Office of China-Australian Agency for International Development HIV/AIDS Asian Regional Program. Progress report of China–Australian. Beijing: Agency for International Development HIV/AIDS Asian Regional Program in Guangxi Autonomous Region and Yunnan Province; 2012.
Project Office of China-UK HIV/AIDS Prevention and Care Project. Progress report for China-UK HIV/AIDS Prevention and Care Project. 2006.
Qian HZ, Vermund SH, Wang N. Risk of HIV/AIDS in China: subpopulations of special importance. Sex Transm Infect. 2005;81(6):442–7.
Qian HZ, Schumacher JE, Chen HT, Ruan YH. Injection drug use and HIV/AIDS in China: review of current situation, prevention and policy implications. Harm Reduct J. 2006;3:4.
Qu ZW, Wu ZH, Shen DQ, HB P. Effectiveness of clean needle exchange programs on HIV/AIDS prevention in Hongjiang District, Hunan Province. Pract Prevent Med. 2006;13(1):85–6.
Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–44.
Smith K, Bartlett N, Wang N. A harm reduction paradox: comparing China’s policies on needle and syringe exchange and methadone maintenance. Int J Drug Policy. 2012;23(4):327–32.
Stitzer M. Contingency management and the addictions. Addiction. 2006;101(11):1536–7.
Stone K, Shirley-Beavan S. Global state of harm reduction 2018. London: Harm Reduction International; 2018.
Strathdee SA, Celentano DD, Shah N, Lyles C, Stambolis VA, Macalino G, Nelson K, Vlahov D. Needle-exchange attendance and health care utilization promote entry into detoxification. J Urban Health. 1999;76(4):448–60.
Sullivan SG, Wu Z. Rapid scale up of harm reduction in China. Int J Drug Policy. 2007;18(2):118–28.
Sun B, Ye Y, Qin L. An analysis of relapse factors of 615 heroin addicts. Chin J Drug Depend. 2001;10(3):214–6.
Sun YY, Yu XM, Sun JP, Xue H, Wang G, Wang J, Wang L. Analysis of utilization situation of harm reduction services among drug users and its impact factors. J Peking Univ (Health Sci). 2013;45(3):387–91.
Tang Z, Zhang C, Li X, Liu Y, Su S, Zhou Y, Shen Z. HIV risk among female sex workers with different patterns of drug use behaviors in Southwest China: a cross-sectional study. AIDS Care. 2015;27(3):293–300.
The State Council. China HIV/AIDS prevention and control action plan (2001–2005). Beijing: State Council; 2001.
The State Council. China’s action plan for reducing and preventing the spread of HIV/AIDS (2006–2010). Beijing: State Council; 2006a.
The State Council. Regulations on AIDS prevention and treatment. Beijing: State Council; 2006b.
The State Council. Announcement of the state council on strengthen HIV/AIDS prevention and control. Beijing: State Council; 2010.
The State Council. China’s 12th five year action plan for HIV/AIDS prevention and control. Beijing: State Council; 2012.
The State Council. China’s 13th five year action plan for HIV/AIDS prevention and control. Beijing: State Council; 2017.
Tibke P. Drug dependence treatment in China: a policy analysis, 2017. 2017. http://fileserver.idpc.net/library/IDPC-briefing-paper_China-drug-treatment.pdf.
UNAIDS. Call for urgent action to improve coverage of HIV services for injecting drug users. Beijing: UNAIDS; 2010.
Wang L, Wang Y, Jin S, Wu Z, Chin DP, Koplan JP, Wilson ME. Emergence and control of infectious diseases in China. Lancet. 2008;372(9649):1598–605.
Wang C, Shi CX, Zhang B, Chen H, Wang H, Zhang N, Rou K, Cao X, Luo W, Wu Z. HIV seroconversion and risk factors among drug users receiving methadone maintenance treatment in China: a qualitative study. Drug Alcohol Depend. 2016;167:169–74.
Werb D, Kamarulzaman A, Meacham MC, Rafful C, Fischer B, Strathdee SA, Wood E. The effectiveness of compulsory drug treatment: a systematic review. Int J Drug Policy. 2016;28:1–9.
Wilson DP, Donald B, Shattock AJ, Wilson D, Fraser-Hurt N. The cost-effectiveness of harm reduction. Int J Drug Policy. 2015;26:S5–S11.
Wodak A, Cooney A. Do needle syringe programs reduce HIV infection among injecting drug users: a comprehensive review of the international evidence. Subst Use Misuse. 2006;41(6–7):777–813.
Wolfe D, Carrieri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review of barriers and ways forward. Lancet. 2010;376(9738):355–66.
Wood E, Kerr T, Spittal PM, Small W, Tyndall MW, O'Shaughnessy MV, Schechter MT. An external evaluation of peer-run “unsanctioned” syringe exchange program. J Urban Health. 2003;80(3):455–64.
World Bank. China – Ninth Health Project (English). Washington, DC: World Bank; 2009. http://documents.worldbank.org/curated/en/885981468215102925/China-Ninth-Health-Project.
Wu Y. Catching the opportunity and promoting HIV/AIDS prevention and control. 2004.
Wu Z. Summary of the HIV/AIDS prevention in 2007 and workplan for 2008. Presented at the 2008 annual meeting of the provincial AIDS directors, Beijing. 2008.
Wu Z, Detels R, Zhang J, Duan S, Cheng H, Li Z, Dong L, Huang S, Jia M, Bi X. Risk factors for intravenous drug use and sharing equipment among young male drug users in Longchuan County, south-west China. AIDS. 1996;10(9):1017–24.
Wu Z, Luo W, Sullivan SG, Rou K, Lin P, Liu W, Ming Z. Evaluation of a needle social marketing strategy to control HIV among injecting drug users in China. AIDS. 2007;21(Suppl 8):S115–22.
Wu Z, Wang Y, Mao Y, Sullivan SG, Juniper N, Bulterys M. The integration of multiple HIV/AIDS projects into a coordinated national programme in China. Bull World Health Organ. 2011;89(3):227–33.
Wu Q, Kamphuis C, Duo L, Luo J, Chen Y, Richardus JH. Coverage of harm reduction services and HIV infection: a multilevel analysis of five Chinese cities. Harm Reduct J. 2017;14(1):10.
Xia M, Kreiss JK, Holmes KK. Risk factors for HIV infection among drug users in Yunnan province, China: association with intravenous drug use and protective effect of boiling reusable needles and syringes. AIDS (London). 1994;8(12):1701–6.
Xia JQ, Yu GH, Wang X. Effectiveness of needle exchange programs combined with peer education among IDUs. Chin J PHM. 2009;25(6):586–7.
Xiao Y, Kristensen S, Sun J, Lu L, Vermund SH. Expansion of HIV/AIDS in China: lessons from Yunnan Province. Soc Sci Med. 2007;64(3):665–75.
Xinjiang Autonomous Region Center for Disease Control and Prevention. Progress report of China-Australia HIV/AIDS prevention and care program in Xinjiang autonomous region. 2008.
Xue HM, Duo L, Yang LH, Deng L, Zhong JR. Evaluation and analysis to clean needle syringe comprehensive intervention of mainline drug addicts in HAARP counties of Yunnan province. Soft Sci Health. 2011;25(12):845–8.
Yang F, Luo J, Da Y, Yang MB, et al. A pilot project on social marketing of needle exchange and condom promotion in drug users. Chin J AIDS/STD. 2003;2:100–2.
Yap L, Wu Z, Liu W, Ming Z, Liang S. A rapid assessment and its implications for a needle social marketing intervention among injecting drug users in China. Int J Drug Policy. 2002;13:57–68.
Zeng Y. The Yining city injecting drug user harm reduction program: experience gained, expansion achieved. Urumqi: Xinjiang HIV/AIDS; 2006.
Zhang SX, Chin K-L. A people’s war: China’s struggle to contain its illicit drug problem. Brookings Institution, Washington, DC. 2015.
Zhang SM, Shi JH, Zhang XY. The history of narcotics control in China. Beijing: China People’s Public Security University Press; 2004. p. 213.
Zhang L, Yap L, Xun Z, Wu Z, Wilson DP. Needle and syringe programs in Yunnan, China yield health and financial return. BMC Public Health. 2011;11(1):250.
Zhang L, Chow EP, Jing J, Zhuang X, Li X, He M, Sun H, Li X, Gorgens M, Wilson D, Wang L, Guo W, Li D, Cui Y, Wang L, Wang N, Wu Z, Wilson DP. HIV prevalence in China: integration of surveillance data and a systematic review. Lancet Infect Dis. 2013;13(11):955–63.
Zhang L, Yap L, Reekie J, Liu W, Chen Y, Wu Z, Wand H, Butler T. Drug use and HIV infection status of detainees in re-education through labour camps in Guangxi Province, China. Int J Environ Res Public Health. 2015;12(5):4502–19.
Zheng XW. A preliminary study on the behavior of 225 drug abusers and the risk factors of HIV infection in Ruili county Yunnan Province. Zhonghua Liu Xing Bing Xue Za Zhi. 1991;12(1):12–4.
Zheng X, Tian C, Choi KH, Zhang J, Cheng H, Yang X, Li D, Lin J, Qu S, Sun X, et al. Injecting drug use and HIV infection in southwest China. AIDS. 1994;8(8):1141–7.
Acknowledgments
The authors would like to thank Willa Dong for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Luo, W., Shi, C.X., Li, Z., Han, L. (2020). National Needle and Syringe Exchange Program. In: Wu, Z., Wang, Y., Detels, R., Bulterys, M., McGoogan, J. (eds) HIV/AIDS in China. Springer, Singapore. https://doi.org/10.1007/978-981-13-8518-6_10
Download citation
DOI: https://doi.org/10.1007/978-981-13-8518-6_10
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-8517-9
Online ISBN: 978-981-13-8518-6
eBook Packages: MedicineMedicine (R0)