Abstract
Malaria is one of the major infectious diseases which continues to be a serious threat in the developing countries. The burden of malaria is getting even worse, because of increase in parasite resistance to the current antimalarial drugs. The resistance to insecticides by mosquitoes has also diminished the hope of malaria eradication in endemic areas. New drugs with unique structure and mechanism of action are immediate needs to treat malaria. The rapid spread of malaria parasite, resistant towards the efficacious artemisinin combination therapy has forced the antimalarial drug discovery programs to identify unique drug targets as well as safe, affordable, and effective new natural antimalarial agents that can compete with synthetic ones. Till date, natural compounds have provided the most effective antimalarials, such as quinine and artemisinin. This raises the possibility that plants might be the sources for more potential antimalaria products. The advantage of natural compounds for the development of drugs derives from their innate affinity for biological receptors, often affordable and accessible for developing countries. The ethnopharmacological approach in natural antimalarial discovery has led to identification of novel lead compounds against malaria. In this book chapter, we review the advancement in discovery of anti-malarial compounds isolated from natural resources.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Global Impact of Malaria
Malaria remains a major cause of death and morbidity worldwide. It has been ranked fourth among major infectious diseases in causing deaths after pneumococcal acute respiratory infections, HIV/AIDS and tuberculosis. Malaria continues to kill over a million people mainly in tropical countries and accounts for approximately 2.6% of the total disease burden of the world. Plasmodium falciparum accounts for the majority of malarial mortality, though the less virulent P. vivax and P. ovale also contribute significantly to morbidity. According to the WHO reported in 2016, 91 countries reported a total of 216 million cases of malaria, an increase of 5 million cases as compared to 2015. Although malaria incidence has fallen globally since 2010, the rate of decline has stalled and even reversed in some regions since 2014. Mortality rates have followed a similar pattern. The rapid increase in resistance of plasmodium to current antimalarials has made treatment ineffective and has caused major issues in the eradication of malaria. In addition, mosquitoes resistant to pesticides, restriction in the use of chemical sprays and lack of effective vaccines pose grave threats to global health. With global warming there is a sudden and dramatic resurgence of malaria in many countries. Moreover, no new synthetic antimalarial drug has been discovered over the past four decades. This warrants the urgent need for the development of new antimalarials.
2 Life Cycle of the Malarial Parasite and Clinical Features of Malaria
The malarial parasite has a complicated and fascinating lifecycle which promises different aspects to investigate in detail. The parasite completes its lifecycle in two different hosts – humans and female Anopheles mosquitoes. Life cycle of the parasite can be divided into three different stages:
2.1 Infection of a Human Host
When a plasmodium-infected female Anopheles mosquito bites human, it inoculates sporozoites into the human skin. Sporozoites enter liver cells and grow into tissue schizonts which rupture and release merozoites to the blood stream thus completing the pre-erythrocytic stage. At this stage, P. vivax and P. ovale can remain dormant as hypnozoites in the liver and relapses may occur within a week, or even years later.
2.2 Asexual Stage
Following the pre-erythrocytic stage, asexual stage begins in erythrocytes in which merozoites develop into ring and trophozoites that later convert to schizonts. Finally, the mature schizonts burst and release merozoites in blood stream. At this stage, patients show clinical symptoms leading to illness and complications.
2.3 Sexual Stage
Merozoites may also progress into sexual erythrocytic stages and develop into immature gametocytes, which are the precursors of male and female gametes. These are ingested by an Anopheles mosquito through a blood meal and undergo fertilization in the mosquito midgut forming oocyst. Oocyst subsequently undergoes multiple rounds of asexual replication resulting in the production of sporozoites. Rupture of the mature oocyst releases the sporozoites into the body cavity of the mosquito which migrates to the salivary glands, ready to infect another human host, thus completing the life cycle (Scherf et al. 2008).
Malaria is an acute febrile illness characterized by fever, headache, chills, muscular aches, weakness, vomiting, cough, diarrhea and abdominal pain. If patients are not treated at this stage, malaria develops into a severe illness which includes symptoms such as seizures, coma, metabolic acidosis, pulmonary edema, pneumonia and renal failure. Any of these complications can develop rapidly and progress to death within hours or days. All the clinical manifestations of malaria are associated with the asexual erythrocytic or blood stage parasites. In an individual lacking immunity, symptoms appear in 7 days or longer after the infectious mosquito bite. Clinical relapses may occur weeks to months after the first infection, if proper treatment regime is not followed by the patient. The patient experiences relapse at regular intervals of 48–72 h which is named as “short term relapses”. Some patients experience “long term relapses” after a gap of 20–60 days or more. In malaria caused by P. vivax and P. ovale, relapse occur due to reactivation of the dormant parasites called hypnozoites in the liver. In P. falciparum and P. malariae infections, recrudescence occurs because of the surviving parasites in red blood cells.
3 Diagnosis of Malaria
The clinical diagnosis of malaria depends on the symptoms of the patient which can vary from abdominal pain to anorexia. The detection is cumbersome considering the wide range of symptoms that also overlap with many other diseases. The laboratory diagnosis attains significance here as it can reduce the time for diagnosis thus preventing the transmission/spread of the disease. The peripheral blood from the patient is used to make thin and thick smears (thick for detecting the pathogen and thin for species confirmation), stained (usually with Giemsa) and viewed under the microscope to detect the parasite. A more sensitive microscopic technique is Quantitative Buffy Coat (QBC) test, in which parasite DNA is stained with fluorescent dyes, (e.g. acridine orange) detected by epi-fluorescent microscopy. Rapid Detection Kits which detect plasmodium-specific antigens are also gaining popularity as they reduce the time for diagnosis. The patient blood flows through a membrane containing malaria antigen-specific antibodies. The kits can be species-specific or can detect a pan-plasmodium protein like lactate dehydrogenase. Serological tests like Immunofluorescence antibody testing (IFA) are also in use, owing to their specificity and sensitivity. Molecular techniques like polymerase chain reaction (PCR) are being standardized to detect the pathogen at the DNA level, aiming to reduce the diagnosis time even further. Other molecular techniques at their infancy for malaria detection are real-time PCR, microarray and flow cytometry (Tangpukdee et al. 2009).
4 Natural Antimalarial Drugs Derived from Plants
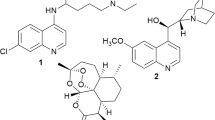
Historically, plants have been a prominent source of antimalarial drugs like quinine and artemisinin (Saxena et al. 2003). Compounds from Cinchona species are well known for their antimalarial properties and the constituent alkaloid, quinine remained the major antimalarial drug for many years but later this natural product was replaced by a series of synthetic drugs including eight aminoquinolines, four aminoquinolines and folic acid synthesis inhibitors. Plant products continue to make an immense contribution to malaria chemotherapy, either directly as antimalarial agents, or as important lead compounds for the discovery of more potent antimalarial drugs (Kaur et al. 2009; Chinsembu 2015). The Chinese traditional treatment of malaria includes the use of Artemisia annua and its active compound artemisinin. Artemisinin has more chemotherapeutic index than chloroquine and it is also used in choloquinine resistant strains of malaria. Another plant used as an antimalarial drug is a Chinese medicinal plant, Dichroea febrifuga. The active drug isolated from this plant is febrifugine. Febrifungine has been used against P. vivax and P. ovale but its harmful effect on liver makes it unacceptable as antimalarial drug. The important useful antimalarials derived from plants are given in Table 6.1.
5 Established Antimalarial Drug Classes and Their Sources
Apart from the decoctions and the isolated compounds, the plants themselves can be used as phytopharmaceuticals. Plant components can also provide templates for the development of structurally simpler analogues that serve as effective antimalarials. A vast majority of prescription drugs used today contain compounds that are directly or indirectly derived from plants (Oksman-Caldentey and Inzé 2004).
Antimalarials derived from plants are classified into Alkaloids, Terpenes, Quassinoids, Flavonoids, Limonoids, Chalcones, Peptides, Xanthones, quinones, coumarines and Lignans.
5.1 Alkaloids
Alkaloids are one of the most important classes of natural antimalarials since ancient time. The outstanding example in this class is quinine from Cinchona succirubra (Rubiaceae) used more than three centuries to treat malaria and its mechanism of action is hypothesized to inhibit parasite heme detoxification. Indole alkaloids are derived from the stem and root bark of Monodora angolensis and Isolona cauliflora plants. They are also isolated from the leaves of Glassocalyx brevipes and Strychnos usambarensis. Fruits of the plant Picralikma nitida are also used to isolate indole alkaloids to treat malaria.
Naphthyl isoquinolines have been used as antimalarials. Leaves of Ancistrocladus robertsoniorum and Ancistrocladus tanzaniensis are main source of naphthyl isoquinolines. Root of Vepris uguenensis and Toddalia asiatica are also used to extract furoquinolines. Other alkaloid classes isolated from different plants that have been used as antimalarial medicines are bisbenzyl isoquinolines, protoberberines, aporphines and manzamines.
5.2 Terpenoids
Terpenoids also show promising antimalarial activity and are classified as Sesquiterpenes, Triterpenes and Diterpenes. Leaves of African plants Vernonia amygdalina and Vernonia brachycalyx are important source of sesquiterpenes. The fruits of Reneilmia cincinnataare also used to isolate this class of antimalarials. Diterpenes are isolated from the seeds of Aframomum zambesiacum.
5.3 Quassinoids
Quassinoids are a group of degraded triterpenes found in the family Simaroubaceae. These bioactive phytochemicals belong to the triterpene chemical family. The main active compounds in quassinoids are ailanthionone, glaucarubinone, and holacanthone. Extracts of Ailanthus altissima, member of simaroubaceae have been used against P. falciparum in-vitro. A study suggests that root bark of Simaba orinocensis is also an important source of quassinoids (Muhammad et al. 2004).
5.4 Flavonoids
Several bioactive flavonoids have been derived from medicinal plants growing in Africa. It is believed that flavonoids exhibit antimalarial activity by inhibiting the influx of L-glutamine and myoinositol into infected erythrocytes. Stem bark of Erythrina abyssinica and root bark of Friesodielsia obovata are the sources of antimalarials flavonoids. Stem bark of Morus mesozygia and Erythrina sacleuxii are also major sources of antimalarial flavonoids.
5.5 Limonoids
Limonoids are produced by Meliaceae species. A well-known representative of this family is Azadirachta indica (Neem tree), a widely used antiplasmodial plant in Asia and is known to contain nimbolide, the active antimalarial principle (Rochanakij et al. 1985).
5.6 Chalcones
Chalcones are active in-vitro against P. falciparum and are shown to exhibit antimalarial action by protease inhibition. Few known Chalcones are Licochalcone A isolated from Glycyrrhiza inflata (Chen et al. 1994), (+)-Nyasol isolated from Asparagus africanus (Oketch-Rabah et al. 1997) and pinostrobin from Cajanus cajan (Ducker-Eshun et al. 2004).
5.7 Antimalarial Peptides
Antimalarial peptides (AMPs) isolated from various sources have been proven to possess antimalarial activity. Fungal cyclic tetrapeptide (apicidin) isolated from Fusarium pallidoroseum, is orally active against P. berghei at nanomolar concentrations. It inhibits protozoal histone deacetylase (HAD) thereby interfering with transcriptional control and cell proliferation (Singh et al. 1996).
Dermaseptin S4 (ALWMTLLKKVLKAAAKAALNAVLVGANA) and Dermaseptin S3 (ALWKNMLKGIGKLAGKAALGAVKKLVGAES) are antimicrobial peptides isolated from frog skin which are active against the parasite (Ghosh et al. 1997). Two cyclodepsipeptides, beauvericin and beauvericin Awere isolated from the insect pathogenic fungus Paecilomyces tenuipes BCC 1614, exhibiting moderate antiplasmodial activities against K1 strain (Nilanonta et al. 2000). Jasplakinolide (Jonckers et al. 2002), a cyclic peptide isolated from the marine sponge Jaspis sp. markedly decreased parasitemia of P. falciparum by virtue of an apical protrusion that appears to interfere with the erythrocyte invasion by the merozoites (Mizuno et al. 2002).
5.8 Xanthones
Xanthones are phenolic secondary metabolites derived from Calophyllum and Garcinia species of the Clusiaceae family, found to be active against the parasites.
5.9 Quinones
Quinones have been found to possess antiplasmodial activity (Carvalho et al. 1988). Among naphthoquinones isolated from higher plants, Plumbagin possess the strongest antimalarial activity against P. falciparum (Likhitwitayawuid et al. 1993).
5.10 Coumarins
Coumarins such as 20-epicycloisobrachy coumarinone epoxide, I clausarin, dentatin, O-methylexostemin phenylcoumarins etc. (Kaur et al. 2009) have shown good antimalarial activity.
5.11 Synthetic Compounds
Quinine which was used from ancient times was later replaced by synthetic compounds like Pamaquin, Chloroquin, Piperquin etc. Some of them like pamaquin were terminated because to their high toxicity. Another major drug artemisinin, a sesquiterpenoid obtained from plant used in Chinese traditional medicine. Though a potent drug, it had a short pharmacological span as it gets metabolized fast. So, chemical derivatives of Artemesinin, like artesunate are developed to overcome these limitations. It is also derivatized to produce dihydroartemisinin and Artemether. Dimers, trimers and tetramers of artemisinin are also produced to increase the drug potency. A different approach is to have conjugate hybrids of different drugs (for example, dihydroartemisinin and quinine) (Pinheiro Luiz et al. 2018).
6 Bioprospecting and Antimalarial Drugs
Bioprospecting refers to identification and commercialization of biologically active compounds from the nature. It aims at systematic search for such compounds, utilization of traditional knowledge to generate income, commercialization of biodiversity and proper management of resources.
6.1 Phytomedicines
The classical pharmacological approach involves the transfer of a potential drug from the laboratory to the hospitals (bench-to-bedside). This process is time consuming and laborious. The traditional medicine has witnessed the use of plant decoctions to treat different illnesses including malaria. Reverse pharmacological approach (Bedside-to-bench) cuts down the time used by the classical approach by making use of the traditional medicine. The antimalarial decoctions are now extensively studied to identify and estimate their activity.
6.2 Semisynthetic Phtyomedicines
Semisynthetic phtyomedicines with improved qualities are also being developed. The compounds found in these plants may be too complex to manufacture or too expensive to extract. The strategy to use the plants themselves as medicines in such cases paves way to the development of phytomedicines. The mode of production should be cost-effective and efficient. It is equally important to ensure that the phytomedicines are safe as there are numerous unknown compounds also being administered. The major challenges in the use of phytomedicines are:
-
(a)
Lack of complete botanical information about the plants.
-
(b)
Unpredictability in the effects of abiotic and biotic factors on the plant and in turn, its antimalaria activity.
-
(c)
Variations in the concentration of the active ingredient based on the plant part or the batch used.
Thorough evaluation and standardization are crucial before introducing a phytomedicine to clinics.
6.3 Anti-malarial Agents from Endophytic Fungi
Endophytic fungi, present mainly in phyla Ascomycota and Basidiomycota, are associated with different plants. Endophytic fungi are being identified as the prominent sources of structurally unique bioactive natural products. The secondary metabolites isolated from endophytic fungi, possessing antimalarial potential may compose the base for the synthesis of novel drugs which might be utilized to withstand malaria and its resistance. Epoxycytochalasin H a Secondary metabolites isolated from Diaporthe miriciae has high antimalarial activity against the chloroquine-resistant strain of P. falciparum, with an IC50 approximatly 3.5-fold lower than that with chloroquine (Ferreira et al. 2017).
Fusarium sp. endophytic in marine algae and Nigrospora sp. endophytic in trees have also show anti-plasmodium activity (Kaushik et al. 2014).
Endophytic fungi such as Paecilomyces lilacinus, Penicillium janthinellum and Paecilomyces sp. isolated from the bark of Symphonia globulifera show antiplasmodial potency (Ateba et al. 2018).
6.4 Antimalarial Drug from Endophytic Bacteria
Endophytic bacteria, such as Streptomyces, have the potential to act as a source for novel bioactive molecules with medicinal properties. Three endophytic streptomyces isolates named SUK8, SUK10 and SUK27 which were obtained from the Malaysian plants Scindapsus hederaceus, Shorea ovalis and Zingiber spectabile respectively have antimalarial activity (Baba et al. 2015).
7 Potential Drug Targets and Semisynthetic Compounds
Apicoplasts are vestigial non-photosynthetic plastids, a characteristic feature of the Apicomplexan parasites, including P. falciparum. These membrane- bound organelles are absent in the hosts thus any drug targeting molecules within the Apicoplast will be highly specific in action. Enzymes involved in several metabolic pathways (Fatty acid, isoprenoid, haem biosynthesis, Fe-S clusters) located in Apicoplasts have been considered as drug targets (Fig. 6.1). Fatty acid biosynthesis involves multiple enzymes like Fatty Acid Synthases (FAS), beta-keto acyl ACP synthase I/II (Fab B/F), beta-keto acyl ACP reductase (FabG) and beta- hydoxyacyl ACP dehydratase (FabZ). These enymes when inhibited can affect different stages of the life cycle of the malaria parasite. Some of them are observed to be stage-specific. For instance, FAS II is crucial for the liver stage development (Carlton et al. 2002). Another enzyme, Pyruvate dehydrogenase is essential for the transition from liver stage to the blood stage (Pei et al. 2010).
Isoprenoid biosynthetic pathway is also subjected to thorough analysis to identify potential drug targets. There are different steps which can be blocked in the parasite to prevent its survival and multiplication. Dolichol gets phosphorylated to form dolichol phosphate which is important in the synthesis of glycoproteins. Glycoproteins are required for the differentiation of the parasite in the erythrocytes (Kimura et al. 1996). It also acts as a donor of mannose in the form of Dolichol-P-Mannose, synthesized by dolichol phosphate mannose synthase (DPM). The precursors isopentenyl pyrophosphate (IPP) and dimethylallyl pyrophosphate (DMAPP) produced in the apicoplast are exported into the cytoplasm where they are consumed by the isoprenoid and prenylated protein synthesis pathways. They can also be synthesized by the nonmevalonate pathway- the enzymes of which are also under consideration as drug targets (Cassera et al. 2004).
Rapid multiplication of the pathogen in the erythrocytes demands vast supplies of phospholipids for the synthesis of new cell membranes. The precursors are transported from host cells and are converted into phospholipids by the pathogen’s enzymatic pathways. The PMT gene in P. falciparum encodes the phosphoethanolamine methyltransferase that specifically methylates phosphoethanolamine to phosphocholine (p-Cho). The gene is essential for the organism’s survival and multiplication (Via et al. 2005; Holz 1977; Pessi and Ben Mamoun 2006). Compounds that target the transport of either raw materials or conversion of them to the required products- alone or in combination- will make attractive drug candidates for the treatment of malaria.
Prenylation is a post-translational modification that requires protein farnesyl transferases (PFTs). Many PFT inhibitors (PFTIs) are under study to evaluate their antiparasite activity (Olepu et al. 2008).
8 Challenges and Future Perspectives
Highly adaptability and increase in drug resistance behaviour of P. falciparum continues to be a major problem in fight against malaria. The parasite resistance to anti-malarial agents has presented a major barrier to successful disease management in endemic areas and has probably contributed to the resurgence of infection and the increase in malaria-related deaths in recent years. Efforts to develop new antimalarial drugs have increased substantially in the last few years, both as a result of awareness of the global importance of fighting against malaria and the dedicated public –private partnership strategy to discover, develop and deliver new drugs. However, multidrug resistance of P. falciparum has led to an urgent need for the development and implementation of new drugs for the treatment of the malaria parasite. Artemisinin and its derivatives are becoming important and used preferably in combination with a second antimalarial agent to increase the efficacy and combat the resistance of the parasite. However, cost production and pharmacological issues associated with artemisinin derivatives and potential partner drugs are hindering the implementation of combination therapies. Moreover, the development of novel antimalarials is an expensive and slow process and the implementation of new drug policies need resources which are not easily available in the third world.
Resistance should be the prime determinant of the use of a drug. It is critical that decisions regarding which drug regimen to change to, and how to implement the changes, are made in a way that maximizes the benefit to the patient while minimizing the risk of the development of drug resistance.
Mass production of the existing natural compounds should go parallel with the search for new drug candidates. Traditional medicines are used by ~80% of Africans as a first response to ailment. Many of the traditional medicines (for instance, the local plants in the Amazon region) have demonstrable anti-plasmodial activities. Protecting the effective use of a drug must rank as a number-one priority for research and control programs. It is suggested that rigorous evaluation of traditional medicines involving controlled clinical trials in parallel with agronomical development for more reproducible levels of active compounds could improve the availability of drugs at an acceptable cost and a source of income in malaria endemic countries (Ginsburg and Deharo 2011). Ventures like African Network for Drugs and Diagnostics Innovation (ANDI) aim at bridging the gap between the research and marketing of antimalarial drugs obtained from such plant resources. Endophytes that widely colonize healthy tissues of plants have been shown to synthesize a great variety of secondary metabolites that might possess antiplasmodial benefits.
The development of functional assays to investigate essential molecular mechanisms during malaria’s liver stage is critical for the validation of new targets to drive antimalarial drug discovery. One underexplored avenue is the manipulation of essential host targets to kill or block Plasmodium parasites.
9 Conclusion
Malaria is still a major threat, difficult to diagnose and treat, owing to its general symptoms and emerging multidrug resistance. Judicious use of the existing drugs and identification of new drugs can help in the combat against malaria. Improvement of the diagnostic methods can increase their sensitivity, making the early detection possible. On a final note, it is essential that any policy decisions to implement more expensive antimalarials are funded by substantially increased inputs from donor nations. An integrated approach of bioprospecting, efficient manufacture, policy making, appropriate distribution and careful use of the drugs can help in the long-standing combat against malaria.
References
Ateba JET, Toghueo RMK, Awantu AF, Mba’ning BM, Gohlke S, Sahal D, Rodrigues-Filho E, Tsamo E, Boyom FF, Sewald N, Lenta BN. Antiplasmodial properties and cytotoxicity of endophytic fungi from Symphonia globulifera (Clusiaceae). J Fungi. 2018;4(2):E70.
Baba MS, Zin NM, Hassan ZAA, Latip J, Pethick F, Hunter IS, et al. In vivo antimalarial activity of the endophytic actinobacteria, Streptomyces SUK 10. J Microbiol. 2015;53(12):847–55.
Carlton JM, Angiuoli SV, Suh BB, Kooij TW, Pertea M, Silva JC, Ermolaeva MD, Allen JE, Selengut JD, Koo HL, Peterson JD, Pop M, Kosack DS, Shumway MF, Bidwell SL, Shallom SJ, van Aken SE, Riedmuller SB, Feldblyum TV, Cho JK, et al. Genome sequence and comparative analysis of the model rodent malaria parasite Plasmodium yoelii. Nature. 2002;419(6906):512–9.
Carvalho LH, Rocha EMM, Raslan DS, Oliveira AB, Krettli AU. In vitro activity of natural and synthetic naphthoquinones against erythrocytic stages of Plasmodium falciparum. Braz J Med Biol Res. 1988;21:485–7.
Cassera MB, Gozzo FC, D’Alexandri FL, et al. The methylerythritol phosphate pathway is functionally active in all intraerythrocytic stages of Plasmodium falciparum. J Biol Chem. 2004;279(50):51749–59.
Challand S, Willcox M. A clinical trial of the traditional medicine Vernonia amygdalina in the treatment of uncomplicated malaria. J Altern Complement Med. 2009;15(11):1231–7.
Chen M, Theander TG, Christensen BS, Hviid L, Zhai L, Kharazmi A. Licochalcone A, a new antimalarial agent, inhibits in vitro growth of the human malaria parasite Plasmodium falciparum and protects mice from P. yoelii infection. Antimicrob Agents Chemother. 1994;38:1470–5.
Chinsembu KC. Plants as antimalarial agents in Sub-Saharan Africa. Acta Trop. 2015;152:32–48.
Ducker-Eshun G, Jaroszewski JW, Asomaning WA, Oppong-Boachie F, Brøgger Christensen S. Antiplasmodial constituents of Cajanus cajan. Phytother Res. 2004;18:128–30.
Ferreira M, Cantrell C, Wedge D, Gonçalves V, Jacob M, Khan S, Rosa CA, Rosa L. Antimycobacterial and antimalarial activities of endophytic fungi associated with the ancient and narrowly endemic neotropical plant Vellozia gigantea from Brazil. Mem Inst Oswaldo Cruz. 2017;112:692–7.
Ghosh JK, Shaool D, Guillaud P, Ciceron L, Mazier D, Kustanovich I, et al. Selective cytotoxicity of dermaseptin S3 toward intraerythrocytic Plasmodium falciparum and the underlying molecular basis. J Biol Chem. 1997;272:31609–16.
Ginsburg H, Deharo E. A call for using natural compounds in the development of new antimalarial treatments – an introduction. Malar J. 2011;10(Suppl 1):S1.
Grellier P, Ramiaramanana L, Millerioux V, Deharo E, Schrével J, Frappier F, Trigalo F, Bodo B, Pousset J-L. Antimalarial activity of cryptolepine and isocryptolepine, alkaloids isolated from Cryptolepis sanguinolenta. Phytother Res. 1996;10:317–21.
Holz GG Jr. Lipids and the malarial parasite. Bull WHO. 1977;55(2–3):237–48.
Jang CS, Fu FY, Wang CY, Huang KC, Lu G, Chou TC. Ch’ang Shan, a Chinese antimalarial drug. Science. 1946;103(2663):59.
Jiménez-Díaz MB, Mulet T, Viera S, Gómez V, Garuti H, Ibáñez J, Alvarez-Doval A, Shultz LD, Martínez A, Gargallo-Viola D, Angulo-Barturen I. Improved murine model of malaria using Plasmodium falciparum competent strains and non-myelodepleted NOD-scid IL2Rgammanull mice engrafted with human erythrocytes. Antimicrob Agents Chemother. 2009;53(10):4533–6.
Jonckers THM, van Miert S, Cimanga K, Bailly C, Colson P, De PauwGillet MC, van den Heuvel H, Claeys M, Lemière F, Esmans EL, Rozenski J, Quirijnen L, Maes L, Dommisse R, Lemière GL, Vlietinck A, Pieter L. Synthesis, cytotoxicity, and antiplasmodial and antitrypanosomal activity of new neocryptolepine derivatives. J Med Chem. 2002;45:3497–508.
Kaur K, Jain M, Kaur T, Jain R. Antimalarials from nature. Bioorg Med Chem. 2009;17:3229–56.
Kaushik N, Murali TS, Sahal D, Suryanarayanan T. A search for antiplasmodial metabolites among fungal endophytes of terrestrial and marine plants of southern India. Acta Parasitol. 2014;59:745–57.
Kimura EA, Couto AS, Peres VJ, Casal OL, Katzin AM. N-linked glycoproteins are related to schizogony of the intraerythrocytic stage in Plasmodium falciparum. J Biol Chem. 1996;271(24):14452–61.
Likhitwitayawuid K, Angerhofer CK, Cordell GA, Pezzuto JM. Cytotoxic and antimalarial bisbenzylisoquinoline alkaloids from Stephania erects. J Nat Prod. 1993;56:30–8.
MacKinnon S, Durst T, Arnason JT. Antimalarial activity of tropical Meliaceae extracts and Gedunin derivatives. J Nat Prod. 1997;60(4):336–41.
Mesia M, Cimanga RK, Dhooge L, Cos P, Apers S, Totte J, Tona GL, Pieters L, Vlietinck A, Maes L. Antimalarial activity and toxicity evaluation of a quantified Nauclea pobeguinii extract. J Ethnopharmacol. 2010;131(1):10–6.
Mizuno Y, Makioka A, Kawazu S, Kano S, Kawai S, Akaki M, Aikawa M, Ohtomo H. Effect of jasplakinolide on the growth, invasion, and actin cytoskeleton of Plasmodium falciparum. Parasitol Res. 2002;88(9):844–8.
Mueller MS, Runyambo N, Wagner I, Borrmann S, Dietz K, Heide L. Randomized controlled trial of a traditional preparation of Artemisia annua L. (Annual Wormwood) in the treatment of malaria. Trans R Soc Trop Med Hyg. 2004;98(5):318–21.
Muhammad I, Bedir E, Khan SI, Tekwani BL, Khan AI, Takamatsu S, Pelletier J, Walker L. A new antimalarial quassinoid from Simaba orinocensis. J Nat Prod. 2004;67(5):772–7.
Nilanonta C, Isaka M, Kittakoop P, Palittapongarnpim P, Kamchonwongpaisan S, Pittayakhajonwut D, Tanticharoen M, Thebtaranonth Y. Antimycobacterial and antiplasmodial cyclodepsipeptides from the insect pathogenic fungus Paecilomyces tenuipes BCC 1614. Planta Med. 2000;66:756–8.
Oketch-Rabah HA, Dossaji SF, Christensen SB, Frydenvang K, Lemmich E, Cornett C, Olsen CE, Chen M, Kharazmi A, Theander T. Antiprotozoal compounds from Asparagus africanus. J Nat Prod. 1997;60(10):1017–22.
Oksman-Caldentey KM, Inzé D. Plant cell factories in the post-genomic era: new ways to produce designer secondary metabolites. Trends Plant Sci. 2004;9:433–40.
Olepu S, Suryadevara PK, Rivas K, et al. 2-Oxo-tetrahydro-1,8-naphthyridines as selective inhibitors of malarial protein farnesyltransferase and as anti-malarials. Bioorg Med Chem Lett. 2008;18(2):494–7.
Pei Y, Tarun AS, Vaughan AM, Herman RW, Soliman JM, Erickson-Wayman A, Kappe SH. Plasmodium pyruvate dehydrogenase activity is only essential for the parasite’s progression from liver infection to blood infection. Mol Microbiol. 2010;75(4):957–71.
Pessi G, Ben Mamoun C. Pathways for phosphatidylcholine biosynthesis: targets and strategies for antimalarial drugs. Future Med Future Lipidol. 2006;1(2):173–80.
Pinheiro Luiz CS, Feitosa LM, Da Silviera FF, Boechat N. Current antimalarial therapies and advances in the development of semi-synthetic artemisinin derivatives. Ann Braz Acad Sci. 2018;90(1 Suppl. 2):1251–71.
Rochanakij S, Thebtaranonth Y, Yenjai C, Yuthavong Y. Nimbolide, a constituent of Azadirachta indica, inhibits Plasmodium falciparum in culture. Southeast Asian J Trop Med Public Health. 1985;16(1):66–72.
Saxena S, Pant N, Jain DC, Bhakuni RS. Antimalarial agents from plant sources. Curr Sci. 2003;85:1314–29.
Scherf A, Lopez-Rubio JJ, Riviere L. Antigenic variation in Plasmodium falciparum. Annu Rev Microbiol. 2008;62:445–70.
Singh SB, Zink DL, Polishook JD, Dombrowski AW, Darkin-Rattray SJ, Schmatz DM, Goetz MA. Apicidins: novel cyclic tetrapeptides as coccidiostats and antimalarial agents from Fusarium pallidoroseum. Tetrahedron Lett. 1996;37(45):8077–80.
Tangpukdee N, Duangdee C, Wilairatana P, Krudsood S. Malaria diagnosis: a brief review. Korean J Parasitol. 2009;47(2):93–102.
Via HJ, Ben Mamoun C, Sherman IW. Plasmodium lipids: metabolism and function in molecular approaches to malaria. Washington, DC: ASM Press; 2005. p. 327–52.
Wells TNC. Natural products as starting points for future antimalarial therapies: going back to our roots? Malar J. 2011;10(Suppl 1):S3.
Willcox ML, Graz B, Falquet J, Sidibé O, Forster M, Diallo D. Argemone mexicana decoction for the treatment of uncomplicated falciparum malaria. Trans R Soc Trop Med Hyg. 2007;101(12):1190–8.
Acknowledgments
A.N acknowledges the Jawaharlal Nehru Centre for Advanced Scientific Research (JNCASR), Bangalore. K.S acknowledges Department of Medicine, University of California. L.S.R acknowledges Institut Pasteur.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Narayanan, A., Sindhe, K.M.V., Rai, L.S. (2019). Drug Resistance in Plasmodium sp. and Novel Antimalarial Natural Products-Emerging Trends. In: Kumar, S., Egbuna, C. (eds) Phytochemistry: An in-silico and in-vitro Update. Springer, Singapore. https://doi.org/10.1007/978-981-13-6920-9_6
Download citation
DOI: https://doi.org/10.1007/978-981-13-6920-9_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-6919-3
Online ISBN: 978-981-13-6920-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)