Abstract
Parkinson’s disease (PD), Alzheimer’s disease (AD) are very frequent human neurodegenerative diseases. Their pharmacological treatment has not been solved; therefore, there is a need to investigate and discover new drug candidates and new targets. Modification of endogenous chemicals can offer new candidates with improved therapeutic outcomes. Computational chemistry can support the discovery of such candidates and can further improve the execution speed, decrease cost and the usage of test animals. These methods for example can include cheminformatics, docking and molecular dynamics. Computational biology offers a way for discovery of novel pharmacological targets and can pinpoint the genetic background of such diseases. In this chapter, we would like to discuss the possible targets of the two most common neurological diseases, AD and PD. The known and the possible new targets are shown and their therapeutic importance is also detailed. In addition, the methods of their discovery is highlighted demonstrating the importance of the in silico discovery of new targets in neurological diseases.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Neurodegenerative Diseases
Amyotrophic lateral sclerosis (ALS), Cerebellar ataxia (CA), Parkinson’s disease (PD), Alzheimer’s disease (AD), and Motor Neuron disease (MND) are known as the most frequently occurring human neurodegenerative diseases. All of them are related to aging, and they are progressive disorders affecting certain classes of neurons found in the central nervous system (CNS). For example, PD is described by loss of nigrostriatal dopaminergic neurons in the substantia nigra pars compacta (SNc), which causes reduction in dopamine levels and cytoskeletal inclusion of Lewy bodies (Pandey et al. 2018).
Of all neurodegenerative diseases, AD is the most common, which was first identified as a primary cause of death for people suffering from mental illness (Katzman 1976). There are several hypotheses about the underlying reasons that can be classified into the following three categories (Herrup 2015): cellular, genetic, and molecular imbalances (Thai et al. 2017).
Its etiology is mainly unknown. It has already been demonstrated that oxidative stress can play a key role in the etiology of late onset neurodegenerative diseases (Flynn and Melov 2013). Oxidative stress was found to be relevant in a range of neurodegenerative diseases, and emerging evidence from in-vitro and in-vivo disease models demonstrates that oxidative stress can be important in general disease pathogenesis (Pandey et al. 2018).
Pharmacological treatment of neurodegenerative disorders has not been solved; therefore, there is a need to investigate new drug candidates. Modification of endogenous chemicals can offer new drug candidates with better potencies and/or further functions that may be of therapeutic benefit. Computational sciences can support the discovery of such candidates and can further improve the execution speed, decrease cost and the usage of test animals (Wenzel and Klegeris 2018). Computational biology offers a way for discovery of novel pharmacological targets and can pinpoint the genetic background of such diseases. While computational chemical approaches involve multiple methods that can support the discovery of new chemical entities. These methods for example include cheminformatics (Pandey et al. 2018), docking and molecular dynamics modeling (Thai et al. 2017).
Ziprasidone is an example of a recent drug candidate, which serves the basis of currently applied therapies in many countries for the treatment of bipolar disorder or psychosis. This dual-target antipsychotic treatment combines and optimizes the following pharmacophores: dopamine and naphthylpiperazine, a serotonin receptor ligand. Ziprasidone was shown to have less serious side effects compared to other antipsychotics (Wenzel and Klegeris 2018).
In this chapter, we would like to discuss the possible targets of the two most common neurological diseases, AD and PD. The known and the possible new targets are shown and their therapeutic importance is also detailed. In addition, the methods of their discovery is highlighted demonstrating the importance of the in-silico discovery of new targets in neurological diseases.
2 Alzheimer’s Disease (AD)
AD is the most common type of dementia in the population over age 65 (Dias Viegas et al. 2018). According to World Alzheimer’s Report, in 2015, more than 35 million people suffered from AD, and it is predicted to grow exponentially in the future (Sang et al. 2017).
AD is described by progressive loss in cognition, decrease in functional and motor capacity, damage in behavioral, social autonomy and finally death (Dias Viegas et al. 2018). AD is a result of a neurodegeneration, which is caused by extracellular β-amyloid plaques, while intracellular neurofibrillary tangles cause neurotoxicity and synaptic loss (Agatonovic-Kustrin et al. 2018).
Current clinical treatment is only palliative and restricted to five pharmaceuticals approved by the US FDA. These are donepezil, galantamine, hupersine A and rivastigmine, which are reversible or competitive acetylcholinesterase inhibitors (AChEI), and memantine, which is a non-competitive N-methyl-D-aspartate (NMDA) receptor antagonist (Agatonovic-Kustrin et al. 2018).
None of the approved drugs demonstrated adequate efficacy, tolerability in most patients. Current therapy only provides symptomatic cures and temporarily delay cognitive decline in about half of the patients, while having only a minor effect in severe, advanced cases (Blennow et al. 2006). Furthermore, they have some adverse effects such as diarrhea, dizziness, nausea, vomiting, because of their poor bioavailability, hepatotoxicity and non-selectivity (Agatonovic-Kustrin et al. 2018).
Current medication cannot even stop the progression of the disease. AD was already described by multiple physiological and biochemical malfunctions involving simultaneously operating chemical mediators and numerous protein targets (Dias Viegas et al. 2018). Some of the concerned factors are low levels of acetylcholine, beta amyloid (Aβ) deposits, tau protein hyperphosphorylation and aggregation, oxidative stress, neuroinflammation and dyshomeostasis of bio-metals (Jalili-Baleh et al. 2018).
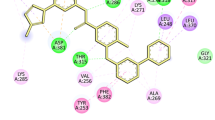
Several therapeutic strategies have been under exploration to increase older population functionally and life expectancy, like using acetylcholinesterase (AChE) and butyrylcholinesterase (BuChE) inhibitors to elevate cholinergic neurotransmission. Furthermore, prevention of Aβ deposition and oxidative damages in the brain are also an important parameter to decrease the pathological complications of AD (Fig. 22.1) (Jalili-Baleh et al. 2018).
Amyloid plaque formation in Alzheimer’s disease signaling interactive pathway. (Illustration reproduced courtesy of Cell Signaling Technology, Inc. (www.cellsignal.com))
Important to note that, many single-target candidates for neurodegenerative diseases that are effective in animal models finally have not been effective in human clinical trials (Zimmerman et al. 2007). The reasons for these failures can be for example, that the drug is not binding to its in-vivo human target or it is not reaching the human target in-vivo, which problems could be solved by modifying the structure or delivery method of the candidates. Another, more complicated problem can be, if the drug binding to a target does not lead to enough of an impact to reduce the signs and symptoms of the disease (Wenzel and Klegeris 2018). To develop new drugs, it can be important to use computational chemistry and cheminformatics to look for quantitative structure-activity relationships to identify molecules to inhibit the formation of Aβ (Nastase and Boyd 2012). Many in-silico approaches have been broadly applied for ‘single-target’ anti-AD drug research based on the conception of ‘therapeutic target’ including docking, molecular dynamics, quantum mechanics, and other methods that could result in quantitative structure. Novel approaches could support the development of ‘multi-target’ anti-AD drugs with integration of diverse sources of information, such as microarrays, literature mining-data or protein– protein interactions (PPIs) (Sun et al. 2013). In conclusion, computer-aided drug design has been one of the main tools used in drug discovery projects used to lower the cost and process time.
2.1 Pharmacological Targets
2.1.1 Acetylcholinesterase (AchE)
Disturbance in the acetylcholine (ACh) releasing cholinergic neurotransmission was shown to likely be coupled with the memory loss in the brain of AD patients. Several types of learning and cortex plasticity are dependent on Ach production. The cholinesterase enzymes lower the concentration of ACh through hydrolyzing it. Cholinesterase blockers can bind to these enzymes leading to higher levels of ACh in synapses (Kumar et al. 2016).
The relation between the malfunctions of neurotransmissions and AD severity revealed a rationale for the application of AchE inhibitors, like donepezil, rivastigmine and galantamine. Cholinesterase blockers can reversibly bind to cholinesterase enzyme, which is responsible for degradation of acetylcholine within the synaptic cleft and increases cholinergic transmission between neurons. Randomized controlled trials have showed significant proof of benefit of AchE inhibitors on cognitive and functional function, although these benefits tend to have only insignificant clinical effects (Epperly et al. 2017).
AchE inhibitors recommended to be used in association with other drugs for the most serious cases of the disease. This also demonstrates the importance of new multi-target (polypharmacological), anti-Alzheimer’s drug candidates (Qian et al. 2018). For instance, novel donepezil-derived N-acyl-aryl-hydrazone ligands with multifunctional purposes can be promising novel drug candidates for therapy. Donepezil’s AChE inhibitory activity as a reference drug for mild and moderate stages of the disorder and previous research studies on N-acylhydrazone moiety further support this idea. It can act as pharmacophore or auxophore subunit, with a broad range of bioactivity profile, depending on other functionalities present in the molecular structure. Pharmacological evaluation demonstrated that these derivative molecules showed significant AChE inhibitory activity (Silva et al. 2016) and antioxidant capacity with metal chelate ability (Turnaturi et al. 2016).
With these activities of basic chemicals, donepezil-derived N-acyl-aryl-hydrazone could have an effect through cholinergic signaling, excitotoxic mechanisms and the amyloid cascade, microglial cells and neuroinflammation, which play as key targets in the polypharmacology-derived concept of multi-target directed pharmaceuticals for AD (Dias Viegas et al. 2018).
2.2 Butyrylcholinesterase (BuChE)
The brain contains two known cholinesterases, acetylcholinesterase (AChE) and butyrylcholinesterase (BuChE). BuChE can be found at high concentrations in the plasma. Until today, its physiological role has not been understood yet. It can have a facilitating role in influencing synaptic transmission and act as a support for AChE. Normally, BuChE can hydrolyze ACh in case of total AChE inhibition. Moreover, high levels of BuChE in plasma also leads to protection for AChE by becoming a scavenger of cholinergic toxins (Agatonovic-Kustrin et al. 2018). Therefore, the inhibition of BuChE might be a successful therapeutic method for AD as well (Jalili-Baleh et al. 2018).
2.3 N-Methyl-D-Aspartate Receptor (NMDAR)
The NMDAR is an ionotropic glutamate receptor mediating glutamatergic transmission and affecting many functions in the central nervous system, such as plasticity, neurodevelopment, learning, synaptic and memory formation. Their over-activation leads to pathological excitotoxicity that can be associated with several neurodegenerative diseases, including AD. Memantine, the only noncompetitive NMDAR antagonist drug, inhibits the NMDAR ion channel (Deora et al. 2017).
2.4 β-Amyloid Precursor Protein Cleaving Enzyme 1 (BACE-1)
Aβ accumulation leads to extracellular and intracellular formation of plaques and neurofibrillary tangles in the brain, and causes neuronal death (Haghighijoo et al. 2017).
Amyloid beta peptides are produced by proteolytic cleavage of APP (amyloid precursor protein) by BACE-1 enzyme as a first step, then by γ-secretases as a second step (Thai et al. 2017). Therefore, BACE1 blockers that reduce the production of all forms of Aβ can serve as potential drug candidates for AD therapy (Haghighijoo et al. 2017).
Haghighijoo and coworkers designed new 3-methylquinazolin-4(3H)-one hydrazones as potential nonpeptide BACE1 blockers, like 2-(2-(2,3-dichlorobenzylidene) hydrazinyl)-3-methylquinazolin-4(3H)-one, which had an acceptable blood brain barrier (BBB) crossing, Caco-2 permeability and logS value, in contrast with peptidic compounds with low blood brain barrier (BBB) crossing, poor oral bioavailability and susceptibility to P-glycoprotein (Pgp) transport (Haghighijoo et al. 2017).
2.5 Peroxisome Proliferator-Activated Receptor γ (PPARγ)
The peroxisome proliferator-activated receptor γ (PPARγ) is a ligand-inducible transcription factor that regulates genes involved in inflammation control. For instance, it blocks proinflammatory gene expression in microglia by suppressing the action of NF-κB. Moreover, PPARγ regulates genes with role in lipid and carbohydrate metabolism, which is important, because number of studies show that higher cellular cholesterol levels trigger high amyloid beta production. Therefore, PPARγ agonists have been advanced as a novel disease altering approach to AD treatment (Thai et al. 2017; Combarros et al. 2011).
2.6 The Liver X Receptor (LXR)
LXR is in close relation with PPARs, thus it can be considered as a target for AD treatment. It has two isoforms LXRα and LXRβ. According to a study with AD mouse model, treatment with LXRα agonist T090131 can lower Aβ formation (Koldamova et al. 2005), however, T090131 was shown to enhance plasma and liver triglycerides, underlining that this compound is not a good drug candidate. These results confirm the importance of LXR agonists, and highlight the role of drug discovery to find a good drug candidate without side effects (Mandrekar-Colucci and Landreth 2011).
2.7 Cathepsin B (CatB)
CatB can be a potential therapeutic target to decrease neuroinflammation that adds to the progression of neurodegenerative disorders. In patients with AD, CatB activity is increased in the central nervous system and blood serum, while its activity decreases in monocytes, lymphocytes compared to normal, same age people. Blocking CatB bioactivity can possibly slow down the progression of AD (Wenzel and Klegeris 2018).
2.8 Monoacylglycerol Lipases (MAGLs)
MAGLs being part of the endocannabinoid system, modulating pain, cognition and several immune functions (Wenzel and Klegeris 2018). MAGL belongs to the lipid-metabolizing enzymes in the serine hydrolase superfamily. Inhibition of MAGL was shown to downregulate proinflammatory cytokines and prostaglandins. Moreover, it can increase glial cell-derived neurotrophic factor and transforming growth factor, that promote the survival of neurons and glial cells (Fernández-Suárez et al. 2014). Another important factor, inhibition of MAGL does not lead to gastric hemorrhages, in contrast to anti-inflammatory therapies that modify prostaglandin synthesis. However, blocking MAGL can raise microglial activation marker ionized calcium binding adaptor molecule 1 (Fernández-Suárez et al. 2014). Accordingly, blocking MAGL could serve as an important strategy for designing drugs to hinder the progression of AD (Wenzel and Klegeris 2018).
2.9 Dual Specificity Phosphatase 2 (DUSP 2)
DUSP 2 enzyme inactivates via dephosphorylation of the phospho-amino acid residues on mitogen-activated protein kinases (MAPKs). These kinases play an important role in mitogenic signal transduction, stress responses, cell survival, apoptosis. That is why, application of DUSP 2 inhibitors in drug design could be a successful way for modulating the inflammatory cascades of neurodegenerative disorders (Wenzel and Klegeris 2018).
2.10 Multi-target Therapeutic Methods to Neurodegeneration
Animal models of neurodegenerative disorders can show effective single-target drugs, however most of them have not been effective in human clinical studies of AD. The reasons behind these failures involve (a) the drug does not bind to the in-vivo human target; (b) does not reach the human target in-vivo, (c) the drug-target interaction is compensated, (d) the drug administered to patients at an late stage of the disease, and (e) variability in the endpoints can mask the beneficial effect of the drug (Wenzel and Klegeris 2018).
Ligands (MTDLs) affecting multiple targets with more than two complementary bioactivities in a single drug molecule can show relevant advantages for the treatment of complex diseases like AD (Jalili-Baleh et al. 2018). This single-molecule approach can decrease side effects and drug interactions of MTDLs compared to combinations of single-target drug (Wenzel and Klegeris 2018).
AP2469 is one of the well-known coumarin-based MTDL with AChE and beta-secretase blocking activities, and having anti-Aβ aggregating, antioxidant, and neuroprotective characteristics. Therefore, coumarin-based MTDLs can be successful drug candidates for AD (Tarozzi et al. 2014).
MTDLs act by creating a combinatory effect on multiple proteins in the biological network simultaneously, which may lower the therapeutic dose, and improving therapeutic efficacy, preventing drug resistance, and reducing side effects (Kalash et al. 2017).
3 Importance of Novel in-silico Ligands
Over the past few years, several small molecules or bioproducts have been under development as a therapy for Alzheimer’s disease, such as small molecule drugs and antibodies. There are some successful natural product based approaches, such as the Ginkgo biloba extract EGb761 and Salvia officinalis extracts have been shown to have anti-oxidative, anti-apoptosis, neuroprotective and neuromodulatory effects. Ginkgo biloba could improve attention and memory performance in patients as observed during a phase III clinical study (Sun et al. 2013).
Huperzia serrata was also studied in clinical trials focusing on the component named Huperzine A (a blood-brain barrier permeable alkaloid) The study showed significant improvements (Sun et al. 2013).
Nordihydroguaiaretic acid from Larrea tridentates was shown to block cholinesterase similarly to the marketed drugs and even has further antiaggregation effect on Aβ. Flavonols and flavones, myricetin and quercetin demonstrated very good BACE1 inhibitory effect (Kumar et al. 2016).
Sarsasapogenin, from the rhizomes of Anemarrhena asphodeloides Bunge, and its derivatives was shown to have neuroprotective activities. Its piperazine derivatives were active against cell injury induced by hydrogen peroxide, lipopolysaccharide and beta amyloid (Yang et al. 2018).
Actinomycetales are considered as prolific producers of a wide variety of bioactive secondary metabolites, such as antibiotics (Mohammadipanah et al. 2012), enzyme inhibitors (Imada 2005), anti-angiogenic and proangiogenic agents (Azarakhsh et al. 2017).
Research for natural anti-AChE metabolites from marine sources, found Actinobacteria, Streptomyces sp. UTMC 1334. Its extract and its high percentage of pyrrole derivatives revealed both anti-acetylcholinesterase and anti-oxidant activities, that might be potentially useful as an adjuvant candidate in the treatment of cognitive disorders (Almasi et al. 2018).
Apelin is a neuropeptide from bovine stomach extracts. It is an endogenous ligand of the APJ receptor (Tatemoto et al. 1998). The apelin/APJ system has various important functions, such as cardiac contractility, blood pressure regulation, glucose metabolism, immunity, water homeostasis, cell proliferation, angiogenesis, neuroprotection (Wu et al. 2017). A study showed that serum levels of apelin-13 decreased in patients with AD. Apelin can lower the production of Aβ by reducing the amount of APP and blocking the activity of β-secretase, and by raising the levels of ABCA1 and increasing the activity of Neprilysin, can lead to degradation of Aβ and lower its accumulation. Apelin may be able to decrease phosphorylation and accumulation of tau protein (Masoumi et al. 2018).
To explore more effective drugs for the treatment of AD, various molecules against known and novel targets of AD could be designed using computational approaches. Dual or multiple inhibitors that block two or more targets of AD can also be studied. Currently there is no treatment to prevent or cure AD but several approved drugs treat several of the symptoms and improve quality of life. Targeting the direct cause of neuronal degeneration could offer a rational strategy and potentially further novel prospects for the treatment of AD (Kumar et al. 2016).
4 Parkinson’s Disease (PD)
PD was first described by James Parkinson, in 1817, as a neurological disturbance showing symptoms like resting tremor and a distinctive form of the progressive motor disorder, designated as shaking palsy or paralysis agitans (Parkinson 2002). Today, it is considered the most common neurodegenerative disorder after Alzheimer’s Disease (AD). PD is generally defined as a progressive, irreversible, chronic neurological disorder characterized by increasingly disabling motor symptoms. These are associated to impaired coordinated movements involving bradykinesia, resting tremor, cogwheel rigidity, postural instability, and gait disorders (Dauer and Przedborski 2003). The majority of PD patients suffer from motor disabilities and numerous non-motor symptoms as well that finally lead to decreased the quality of life (Poewe 2008).
Mechanisms, neuropathology, pathophysiology features involve neuronal loss in specific areas of the substantia nigra and widespread intracellular α-synuclein protein accumulation. These two main pathologies are specific for a definitive diagnosis of idiopathic type PD. In the early-stage disorder, loss of dopaminergic neurons is limited to the ventrolateral substantia nigra with relative sparing of dopaminergic neurons in other areas. The dramatic loss of these dopaminergic neurons even in the early phase reveals that the degeneration here begins before the onset of motor symptoms.
The other characteristic neuropathology is the abnormal occurence of α-synuclein (Lewy bodies) in the cytoplasm. In patients suffering from AD, there is a different pattern of α-synuclein pathology, that is characteristic for limbic brain regions. Despite heritable forms of PD only occur 5–10% in all patients, they provided important clues to the mechanisms. Some of the PD associated gene-coded proteins are related to a set of signaling pathways that may trigger such a neuropathology that resembles sporadic type PD. Moreover, large genome-wide association studies (GWAS) showed that some of these genes are also affected in sporadic PD. Among the examples are: α-synuclein proteostasis, oxidative stress, calcium homeostasis, mitochondrial function, axonal transport, neuroinflammation. Interesting enough that several lines of evidence showed mitochondrial dysfunction as a key element in the pathogenesis of PD. A new theory is one of a vicious cycle in which α-synuclein aggregation and mitochondrial dysfunction facilitate each other, which could provide an explanation why these cellular modifications occur together in degenerating neurons in PD (Poewe et al. 2017).
4.1 Pharmacological Targets
4.1.1 Dopaminergic Pharmacological Targets
Losing dopaminergic neurons in the substantia nigra pars compacta causes striatal dopamine depletion, which is the underlying mechanism in the cardinal motor symptoms. The systemic administration of the dopamine precursor amino acid, the LDOPA showed a breakthrough in the therapy a 50 years ago. Since then, other relevant advances in the understanding of the molecular pharmacology have demonstrated further targets for presynaptic or postsynaptic dopaminergic therapies (PD Med Collaborative Group et al. 2014).
4.1.2 Catechol-O-Methyltransferase Targets
Current LDOPA preparations include blockers of aromatic amino acid decarboxylase enzyme (AADC) like carbidopa or benserazide. These prevent peripheral metabolism of dopamine and support better bioavailability. The peripheral metabolism of LDOPA is done via a secondary metabolic pathway involving ortho-methylation of l-DOPA through catechol-O-methyltransferase (COMT) activity. Therefore, inhibition of COMT can improve bioavailability and the half-life of l-DOPA. Increasing the half life of l-DOPA doses by the application of COMT inhibitors became a first-line therapy in many patients (Ferreira et al. 2016).
4.1.3 Monoamine Oxidase Type B (MAOB) Inhibitors
Oxidation by MAOB in glial cells is an important mechanism for clearance of synoptically excreted dopamine, in addition to presynaptic reuptake by the dopamine transporter. Blocking MAOB raises synaptic dopamine levels, leads to symptomatic efficacy. Recent studies established the antiparkinsonian efficacy of monotherapy using selegiline and another novel MAOB inhibitor rasagiline, which was shown to be effective in combination with l-DOPA in patients with motor fluctuations. While selegiline, rasagiline are irreversible blockers, there is a novel and promising reversible inhibitor, safinamide, on the market (Schapira 2011).
4.1.4 Dopamine Agonists
The dopamine activity on striatal medium spiny neurons is regulated by two classes of dopamine receptors. Dopaminomimetics have direct activity to dopamine receptors (dopamine receptor agonist) targeting the D2 receptor family. These were applied as PD treatment first in the 1970s with bromocriptine and have since become an important treatment method for motor symptoms. First drugs belonging to this class were ergoline derivatives, that also activate 5-hydroxytryptamine (5-HT) receptors, such as 5-HT2B subtype. Later, these became linked to pleuropulmonary and cardiac valvular fibrosis, raising important safety concerns (Connolly and Lang 2014).
4.1.5 Non-dopaminergic Pharmacological Targets
Despite the relevant effect of dopaminergic therapy on PD, there is still a clear need for further therapies targeting other pharmacological routes. The symptom that need to be addressed by such therapies include the complications of l-DOPA treatment, such as motor fluctuations and l-DOPA-induced dyskinesia, l-DOPA-resistant (‘non-dopaminergic’) motor features like treatment-resistant tremor, postural instability, falls, swallowing, speech disturbances. Today, the only effective therapy for l-DOPA-induced dyskinesia is amantadine, an N-methyl-d-aspartate receptor antagonist (Kalia et al. 2013).
The breakthrough for DBS as a therapy for PD arrived in 1993 when novel concepts of the basal ganglia circuitry led to the identification of the subthalamic nucleus as a new target for DBS. DBS is based on the observation that high-frequency (100–200 Hz) electrical stimulation of specific brain targets can mimic the effect of a region without the need for damaging brain tissue, and it involves the implantation of an electrode in brain tissue (Chandra et al. 2018).
5 Nano-particle Mediated Inhibition of Parkinson’s Disease Using Computational Biology Approach
Research for the development of such approaches that can accelerate intracerebral dopamine concentrations and/or stimulates central dopamine receptors was carried out by the application of nanoparticles (NPs). It was shown to be a revolutionary treatment because of their site directed target delivery and ability to penetrate through the blood-brain barrier (BBB). For example, NPs surface linked with peptidomimetic antibodies was demonstrated as a molecular Trojan horse that can transport bulky molecules such as drugs and genes across the BBB. Moreover, biocompatible gold nanoparticles (AuNPs) were also shown to induce a strong α-synuclein aggregation. Other NPs, like graphene and superparamagnetic iron-oxide nanoparticles (SPIONs) demonstrated that they can block the Aβ fibrillation process (Seppi et al. 2011).
Phosphodiesterases (PDEs), found in several regions of the human brain, represent a class of enzymes that selectively cleave cyclic adenosine monophosphate (cAMP) and/or cyclic guanosine monophosphate (cGMP). They are well-known as therapeutic applications for erectile dysfunction and pulmonary hypertension (PDE5 inhibitors) and severe Chronic Obstructive Pulmonary Disease (PDE4 inhibitors), there are other different isoforms of PDEs, which are captivating the interest of scientists looking for new targets for neurodegenerative diseases. Blocking PDE4, PDE7 and PDE10 seems to be involved in protecting dopaminergic neurons. A study focused on a class of derivatives like berberine (isolated from Berberis sp.), and other plants because in traditional Chinese medicine berberine and its analogues have long been reported to have several bioactive and therapeutic roles. These are for example, anticancer, endocrine, cardiovascular, anti-inflammatory and immunomodulatory activities. The activity of berberine on animal models is, while berberine was shown to block PDE activity, a study on its potential effect on other targets that can be included in the anti-PD activity was proven. A combined in-silico evaluation study revealed that berberine and its synthetic derivatives can play a role in the onset and the progression of the neurodegeneration (Zanforlin et al. 2017).
6 Importance of in-silico Target Discovery
Until today, four signaling pathways were shown to be implicated in familial parkinsonism. These are synaptic neurotransmission, endosomal trafficking, lysosomal autophagy, mitochondrial metabolism. Although these processes can be separate, they employ very similar signalling pathways, therefore they may be temporally and functionally related. For instance, synaptic dysfunction, resulting from or leading to alpha-synucleinopathy, can do harm on balancing exo- and endocytosis, neurotransmission or early endosomal receptor recycling. These changes will influence the flux through the endosomal pathway and ultimately lead to autophagy and lysosomal fusion with multivesicular bodies (Gao et al. 2013).
As a conclusion, further genomic, genetic investigations should be done in the future. Knowledge of the pathogenic signaling pathways underlying the etiology and ontology of PD is needed for therapeutic development. The understanding of the normal physiology of certain neuronal populations, signaling pathways and the role of individual proteins, is essential. Understanding parkinsonism and genetic insights can be unbiased and unequivocal but those insights should be carefully considered. Genetic association studies do not provide clear picture and further work is required to fully understand the specific contribution of GWAS, let alone to translate the information from such studies into novel therapeutic methods for idiopathic PD. When interpreting linkage and exome studies, the phenotypes and families have to be also considered. Several neuroscience studies on PD was done using model systems with toxin administration, and these may not accurately reflect the human condition. Why the substantia nigra pars compacta is selectively lost in PD stays still questionable, but through human genetics we now have relevant molecular targets and research tools to study this. With such advances, therapeutic prospects for disease modification (neuroprotection) should be treated with true optimism (Lin and Farrer 2014).
7 Conclusion
One of the most common neurodegenerative disease is Alzheimer’s, which is characterized by progressive loss in cognition, decrease in motor and functional capacity, impairment in behavioral and social autonomy and death (Dias Viegas et al. 2018). Current clinical treatment of AD is only palliative and restricted to five prescription pharmaceutical drugs approved by the US FDA, which are not demonstrated good efficacy and tolerability over a wide range of patients (Blennow et al. 2006). Therefore, there is a need to investigate new drug candidates. Some of the FDA approved drugs are listed in Table 22.1. There are more potential pharmacological targets, which are studied in different projects using computational science, like acetylcholinesterase, butyrylcholinesterase, N-methyl-D-aspartate receptor, β-amyloid precursor protein cleaving enzyme 1, peroxisome proliferator-activated receptor γ, liver X receptor, cathepsin B monoacylglycerol lipases and Dual Specificity Phosphatase 2. Animal models of neurodegenerative diseases can show effective single-target drugs, but most of them have not been effective in human clinical trials of AD. Therefore, researchers need to focus on multitarget-directed ligands with two or more complementary biological activities in a single drug molecule to display significant advantages against complex diseases like AD (Kalash et al. 2017).
Parkinson’s disease is the second recurrent neurodegenerative disorder after AD. It is progressive, irreversible and characterized by increasingly disabling motor symptoms. As it’s pharmacological treatment has not been solved; therefore, there is a need to investigate and discover new drug candidates and targets, next to the known ones (dopaminergic pharmacological targets, catechol-O-methyltransferase, monoamine oxidase type B inhibitors, dopamine agonists and non-dopaminergic pharmacological targets).
To develop new drugs, it is necessary to use computational chemistry and cheminformatics to search for quantitative structure-activity relationships to identify, for example, inhibitors of key enzymes (Nastase and Boyd 2012). New approaches could facilitate the development of ‘multi-target’ anti-AD drugs with integration of various sources of information, such as microarrays, literature mining-data, protein– protein interactions (Sun et al. 2013).
In conclusion, computer-aided drug design has been one of the major tools applied in drug discovery programs used to reduce the cost and process time.
References
Agatonovic-Kustrin S, Kettle C, Morton DW. A molecular approach in drug development for Alzheimer’s disease. Biomed Pharmacother. 2018;106:553–65.
Almasi F, Mohammadipanah F, Adhami HR, Hamedi J. Introduction of marine-derived Streptomyces sp. UTMC 1334 as a source of pyrrole derivatives with anti-acetylcholinesterase activity. J Appl Microbiol. 2018;5:1370–82.
Alzheimer’s association. FDA approved treatments for Alzheimer’s 800.272.3900 alz.org ®. 2017.
Azarakhsh Y, Mohammadipanah F, Nassiri SM, Siavashi V, Hamedi J. Isolation and screening of proangiogenic and antiangiogenic metabolites producing rare actinobacteria from soil. J Appl Microbiol. 2017;122:1595–602.
Blennow K, de Leon MJ, Zetterberg H. Alzheimer’s disease. Lancet (London, UK). 2006;368:387–403.
Cell Signaling Technology, Inc. (www.cellsignal.com).
Chandra KA, Bharadwaj S, Kumar S, Wei DQ. Nano-particle mediated inhibition of Parkinson’s disease using computational biology approach. PMC Sci Rep. 2018;8:9169.
Combarros O, Rodríguez-Rodríguez E, Mateo I, Vázquez-Higuera JL, Infante J, Berciano J, Sánchez-Juan P. APOE dependent-association of PPAR- genetic variants with Alzheimer’s disease risk. Neurobiol Aging. 2011;(3):547.e1–6.
Connolly BS, Lang AE. Pharmacological treatment of Parkinson disease: a review. JAMA. 2014;311:1670–83.
Dauer W, Przedborski S. Parkinson’s disease, mechanisms and models. Neuron. 2003;39:889–909.
Deora GS, Kantham S, Chan S, Dighe SN, Veliyath SK, McColl G, Parat MO, McGeary RP, Ross BP. Multifunctional analogs of kynurenic acid for the treatment of Alzheimer’s disease: synthesis, pharmacology and molecular modeling studies. ACS Chem Neurosci. 2017;8(12):2667–75.
Dias Viegas FP, de Freitas Silva M, Divino da Rocha M, Castelli MR, Riquiel MM, Machado RP, et al. Design, synthesis and pharmacological evaluation of N-benzyl-piperidinyl-aryl-acylhydrazonederivatives as donepezil hybrids: discovery of novel multi-target anti-alzheimer prototype drug candidates. Eur J Med Chem. 2018;147:48–65.
Epperly T, Dunay MA, Boice JL. Alzheimer disease: pharmacologic and nonpharmacologic therapies for cognitive and functional symptoms. Am Fam Physician. 2017;95:771–8.
Fernández-Suárez D, Celorrio M, Riezu-Boj JI, Ugarte A, Pacheco R, González H, Oyarzabal J, Hillard CJ, Franco R, Aymerich MS. The monoacylglycerol lipase inhibitor JZL184 is neuroprotective and alters glial cell phenotype in the chronic MPTP mouse model. Neurobiol Aging. 2014;35:2603–16.
Ferreira JJ, Lees A, Rocha JF, Poewe W, Rascol O, Soares-da-Silva P, Bi-Park 1 Investigators. Opicapone as an adjunct to levodopa in patients with Parkinson’s disease and end-of-dose motor fluctuations: a randomised, doubleblind, controlled trial. Lancet Neurol. 2016;15:154–65.
Flynn JM, Melov S. SOD2 in mitochondrial dysfunction and neurodegeneration. Free Radic Biol Med. 2013;62:4–12.
Gao L, Fang JS, Bai XY, Zhou D, Wang YT, Liu AL, Du GH. In silico target fishing for the potential targets and molecular mechanisms of baicalein as an antiparkinsonian agent: discovery of the protective effects on NMDA receptor-mediated neurotoxicity. Chem Biol Drug Des. 2013;81:675–87.
Haghighijoo Z, Firuzi O, Hemmateenejad B, Emami S, Edraki N, Miri R. Synthesis and biological evaluation of quinazolinone-based hydrazones with potential use in Alzheimer’s disease. Bioorg Chem. 2017;74:126–33.
Herrup K. The case for rejecting the amyloid cascade hypothesis. Nat Neurosci. 2015;18:794–9.
Houghton D, Hurtig H, Metz S, Giroux M, Petzinger G, Fisher B, Hawthorne L, Jakowec M. Parkinson’s disease medications. National Parkinson Foundation. 2018. www.parkinson.org.
Imada C. Enzyme inhibitors and other bioactive compounds from marine actinomycetes. Antonie Van Leeuwenhoek. 2005;87:59–63.
Jalili-Baleh L, Forootanfar H, Küçükkılınç TT, Nadri H, Abdolahi Z, Ameri A, Jafari M, Ayazgok B, Baeeri M, Rahimifard M, Abbas Bukhari SN, Abdollahi M, Ganjali MR, Emami S, Khoobi M, Foroumadi A. Design, synthesis and evaluation of novel multi-target-directed ligands for treatment of Alzheimer’s disease based on coumarin and lipoic acid scaffolds. Eur J Med Chem. 2018;152:600–14.
Kalash L, Val C, Azuaje J, Loza MI, Svensson F, Zoufir A, Mervin L, Ladds G, Brea J, Glen R, Sotelo E, Bender A. Computer-aided design of multi-target ligands at A1R, A2AR and PDE10A, key proteins in neurodegenerative diseases. J Cheminform. 2017;30:67.
Kalia LV, Brotchie JM, Fox SH. Novel nondopaminergic targets for motor features of Parkinson’s disease: review of recent trials. Mov Disord. 2013;28:131–44.
Katzman R. The prevalence and malignancy of Alzheimer disease: a major killer. Arch Neurol. 1976;33:217–8.
Koldamova RP, Lefterov IM, Staufenbiel M, Wolfe D, Huang S, Glorioso JC, et al. The liver X receptor ligand T0901317 decreases amyloid β production in vitro and in a mouse model of Alzheimer’s disease. J Biol Chem. 2005;280:4079–88.
Kumar A, Nisha CM, Silakari C, Sharma I, Anusha K, Gupta N, Nair P, Tripathi T, Kumar A. Current and novel therapeutic molecules and targets in Alzheimer’s disease. J Formos Med Assoc. 2016;115:3–10.
Lin MK, Farrer MJ. Genetics and genomics of Parkinson’s disease. Genome Med. 2014;6:48.
Mandrekar-Colucci S, Landreth GE. Nuclear receptors as therapeutic targets for Alzheimer’s disease. Expert Opin Ther Targets. 2011;15:1085–97.
Masoumi J, Abbasloui M, Parvan R, Mohammadnejad D, Pavon-Djavid G, Barzegari A, Abdolalizadeh J. Apelin, a promising target for Alzheimer disease prevention and treatment. Neuropeptides. 2018;70:76–86.
Mohammadipanah F, Matasyoh J, Hamedi J, Klenk HP, Laatsch H. Persipeptides A and B, two cyclic peptides from Streptomyces sp. UTMC 1154. Bioorg Med Chem. 2012;20:335–9.
Nastase AF, Boyd DB. Simple structure-based approach for predicting the activity of inhibitors of beta-secretase (BACE1) associated with Alzheimer’s disease. J Chem Inf Model. 2012;52:3302–7.
Pandey S, Singh B, Yadav SK, Mahdi AA. Novel biomarker for neurodegenerative diseases- motor neuron disease (MND), cerebellar ataxia (CA) and Parkinson’s disease (PD). Clin Chim Acta. 2018;485:258–61.
Parkinson J. An essay on the shaking palsy. 1817. J Neuropsychiatr Clin Neurosci. 2002;14:223–36.
PD Med Collaborative Group, Gray R, Ives N, Rick C, Patel S, Gray A, Jenkinson C, McIntosh E, Wheatley K, Williams A, Clarke CE. Long-term effectiveness of dopamine agonists and monoamine oxidase B inhibitors compared with levodopa as initial treatment for Parkinson’s disease (PD MED): a large, open-label, pragmatic randomised trial. Lancet. 2014;384:1196–205.
Poewe W. Non-motor symptoms in Parkinson’s disease. Eur J Neurol Suppl. 2008;1:14–20.
Poewe W, Seppi K, Tanner CM, Halliday GM, Brundin P, Volkmann J, Schrag AE, Lang AE. Parkinson disease. Nat Rev Dis Prim. 2017;3:17013.
Qian S, He L, Wang Q, Wong YC, Mak M, Ho CY, Han Y, Zuo Z. Intranasal delivery of a novel acetylcholinesterase inhibitor HLS-3 for treatment of Alzheimer’s disease. Life Sci. 2018;207:428–35.
Sang Z, Wang K, Wang H, Wang H, Ma Q, Han X, Ye M, Yu L, Liu W. Design, synthesis and biological evaluation of 2-acetyl-5-O-(aminoalkyl) phenol derivatives as multifunctional agents for the treatment of Alzheimer’s disease. Bioorg Med Chem Lett. 2017;27:5046–52.
Schapira AH. Monoamine oxidase B inhibitors for the treatment of Parkinson’s disease: a review of symptomatic and potential disease-modifying effects. CNS Drugs. 2011;25:1061–71.
Seppi K, Weintraub D, Coelho M, Perez-Lloret S, Fox SH, Katzenschlager R, Hametner EM, Poewe W, Rascol O, Goetz CG, Sampaio C. The Movement Disorder Society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson’s disease. Mov Disord. 2011;26:S42–80.
Silva GS, Figueiró M, Tormena CF, Coelho F, Almeida WP. Effects of novel acylhydrazones derived from 4-quinolone on the acetylcholinesterase activity and Aβ 42 peptide fibrils formation. J Enzyme Inhib Med Chem. 2016;6366:1–7.
Sun Y, Zhu R, Ye H, Tang K, Zhao J, Chen Y, Liu Q, Cao Z. Towards a bioinformatics analysis of anti-Alzheimer’s herbal medicines from a target network perspective. Brief Bioinform. 2013;14:327–43.
Tarozzi A, Bartolini M, Piazzi L, Valgimigli L, Amorati R, Bolondi C, et al. From the dual function lead AP2238 to AP2469, a multi-target-directed ligand for the treatment of Alzheimer’s disease. Pharmacol Res Perspect. 2014;2:e00023.
Tatemoto K, Hosoya M, Habata Y, Fujii R, Kakegawa T, Zou MX, Kawamata Y, Fukusumi S, Hinuma S, Kitada C. Isolation and characterization of a novel endogenous peptide ligand for the human APJ receptor. Biochem Biophys Res Commun. 1998;251:471–6.
Thai NQ, Nguyen HL, Linh HQ, Li MS. Protocol for fast screening of multi-target drug candidates: application to Alzheimer’s disease. J Mol Graph Model. 2017;77:121–9.
Turnaturi R, Oliveri V, Vecchio G. Biotin-8-hydroxyquinoline conjugates and their metal complexes: exploring the chemical properties and the antioxidant activity. Polyhedron. 2016;110:254–60.
Wenzel TJ, Klegeris A. Novel multi-target directed ligand based strategies for reducing neuroinflammation in Alzheimer’s disease. Life Sci. 2018;207:314–22.
Wu L, Chen L, Li L. Apelin/APJ system: a novel promising therapy target for pathological angiogenesis. Clin Chim Acta. 2017;466:78–84.
Yang GX, Ge SL, Wu Y, Huang J, Li SL, Wang R, Ma L. Design, synthesis and biological evaluation of 3-piperazinecarboxylate sarsasapogenin derivatives as potential multifunctional anti-Alzheimer agents. Eur J Med Chem. 2018;156:206–15.
Zanforlin E, Zagotto G, Ribaudo G. The medicinal chemistry of natural and semisynthetic compounds against Parkinson’s and Huntington’s diseases. ACS Chem Neurosci. 2017;11:2356–68.
Zimmerman G, Lehar J, Keith C. Multi-target therapeutics: when the whole is greater than the sum of the parts. Drug Discov Today. 2007;12:34–42.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Nagy, A., Polgar, T. (2019). In-silico Targets in Neurodegenerative Disorders. In: Kumar, S., Egbuna, C. (eds) Phytochemistry: An in-silico and in-vitro Update. Springer, Singapore. https://doi.org/10.1007/978-981-13-6920-9_22
Download citation
DOI: https://doi.org/10.1007/978-981-13-6920-9_22
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-6919-3
Online ISBN: 978-981-13-6920-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)