Abstract
Endometrial cancer is the most common malignancy of the gynecological tract, with an estimated 61,380 new cases and 10,920 deaths reported by National Institutes of Health for the United States in 2017. Although the dualistic model of endometrial cancer development (types I and II) has been a popular analytic model for more than a generation, this model may be overly simplistic in routine practice, and may not adequately address the marked clinicopathologic heterogeneity that is now recognized to exist within the disparate group of neoplasms that are collectively classified as “endometrial cancer”. A molecular-based classification of endometrial carcinoma from the Cancer Genome Atlas project (TCGA), based in part on a sequencing analysis of hundreds of endometrial cancers, generated four groups of endometrial carcinoma with corresponding molecular signatures. Thus far, this represents a promising classification scheme since it correlates better with prognosis and patient survival compared to all other available classifications. The TCGA study, as well as other molecular studies that have been published in the past two decades, have significantly improved our understanding of how endometrial cancers develop.
In this chapter, we summarize the most important advances in endometrial carcinogenesis by focusing on those advances with potential clinical implications for diagnosis and clinical management. Furthermore, we propose a unified pathologic classification for intraepithelial endometrial neoplasia.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Carcinogenesis
- Endometrioid Carcinoma
- Serous Carcinoma
- Endometrium;
- Molecular Subtypes
- PTEN
- CTNNB1
- beta-catenin
- Microsatellie Instability
- MSI
- DNA MMR
- mismatch repair proteins
- TP53
- p53
- K-ras
- PAX-2
- PIK3CA
16.1 Introduction
Current concepts of endometrial cancer successfully integrate traditional histopathology with pathogenetic mechanisms. Endometrial cancers have long been classified into two major subtypes (types I and II) based on light microscopic appearance, clinical behavior, and epidemiology [1]. Type I cancers, the prototype of which is endometrioid carcinoma, comprise approximately 75% of newly diagnosed endometrial cancers in North America. They are usually associated with unopposed estrogen exposure and are often preceded by precancerous lesions [2]. In contrast, type II endometrial cancers have non-endometrioid histology, typically endometrial serous carcinoma (ESC) , and pursue a much more aggressive clinical course. Endometrial serous carcinoma is not associated with excess estrogen, but, similar to their endometrioid counterparts, have precancerous lesions that have been identified [2]. The morphologic and clinical differences are largely paralleled by the genetic distinctions with notably different types of gene mutations between endometrioid and serous cancers [3, 4].
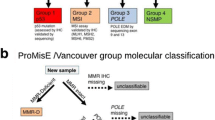
Comparative studies that have utilized genome-wide methods such as expression profiling have further broadened our understanding of relevant genetic basis for the differences between these two different histologic types of endometrial cancers [5, 6]. As previously noted, such dualistic model has traditionally been popular because it accurately distinguishes the most disparately behaving histotypes; however, it has become progressively clear to both clinicians and pathologists that the model is inadequate. Based on the dualistic model, patients with type I (endometrioid carcinoma) should have a very good prognosis; however, it is not an exceptionally rare event to see a low-stage, low-grade, ostensibly type I cancer with an aggressive pattern of recurrence that would be more expected in a type II cancer [7]. Endometrial clear cell carcinoma , which has traditionally been classified as one of the type II cancers, has a better prognosis than ESC and appears to be more prognostically heterogeneous [8, 9]. Diagnostic criteria to differentiate high-grade endometrioid carcinoma from ESC are suboptimal [10, 11], and in general the histotyping of high-grade endometrial carcinomas is associated with no more than moderate reproducibility. Furthermore, the spectrum of histotypes that are associated with a particular hormonal milieu evolves as the frequency of said milieu changes in patient subsets within the population. Advances in molecular technology have demonstrated areas of potential overlap between tumor histotypes that have traditionally been considered to be discordant. All of these factors have caused significant confusion in clinical practice, and has made clear that histologic based classification is far from perfect. Data from the Cancer Genome Atlas (TCGA), originally reported in 2013, has shifted the paradigm on how endometrial cancers are classified. It showed that a cohort of endometrioid and serous carcinomas can be classified into four molecular types based on their distinctive genetic characteristics [12]. More importantly, the molecular classification of these cancers appear to have a much better predictive value for patient survival than that the traditional dualistic model. In the following sections, we consider all available information to summarize the main molecular events that underlie the major histologic subtypes of endometrial cancers.
16.2 Endometrioid Carcinoma
16.2.1 The Role of Sex Steroid Hormone
-
Estrogens and progestins act reciprocally on hormonally responsive endometrial tissue to regulate risk of endometrial cancer. Estrogens induce endometrial cells to grow, while progestin causes cellular differentiation and has the ability to oppose the biologic effects of coexisting estrogens through downregulation of the estrogen receptor within the endometrial cells. For this reason, the biologic effects of admixtures of circulating progestins and estrogens are dominated by progesterone or progestins. Women exposed to estrogens without opposing effects of progestins show a dose- and duration-dependent 2- to 10-fold increased cancer risk [13, 14]. It is apparent that progestins have a protective effect, which reduces risk for endometrial cancer. There are multiple cellular and molecular mechanisms by which sex hormones affect endometrial cancer risk. We summarize the relevant mechanisms here.
-
Estrogen promotes cell proliferation and inhibits apoptosis through a complex downstream cascade of transcriptional changes including modulation of tumor suppressor function. One example is PTEN expression in normal endometrial glands, which is greatly elevated by estrogens and reduced by progestins during hormonal fluctuations of the normal menstrual cycle [15]. This reflects the role of PTEN as a regulator of mitosis and an inducer of apoptosis in the estrogen-stimulated proliferative endometrium; therefore, unopposed estrogen acts as a positive selection force for PTEN mutant cells. Apoptosis induced by progestins is partially mediated by increased expression of Bcl-2 and BAX. The ability of progestins to induce endometrial epithelial apoptotic cell death is extinguished after just a few days, but increases dramatically on withdrawal of progestins [16]. The relationship between hormones including exogenous hormones is summarized in Fig. 16.1.
16.2.2 Genetic Changes Involved in the Development of Endometrioid Carcinoma
Based on data from multiple genetic and clinicopathologic studies, we list here the common genetic changes in endometrioid endometrial cancers. These include, but are not limited to, specific mutations of PTEN, microsatellite instability (MSI), K-ras, and β-catenin (CTNNB1) genes.
PTEN Inactivation
Inactivation of the PTEN tumor suppressor gene (formerly known as MMAC1) is the most common genetic defect in endometrioid carcinoma and is seen in about 80% of tumors that are preceded by a histologically discrete precancerous lesion [17]. PTEN is a tumor suppressor gene encoding a lipid phosphatase which acts to maintain G1 arrest and enable apoptosis through three signal pathways: PI3K/AKT, FAK, and MAPK. The most commonly observed PTEN defect is inactivation of both alleles to generate a null expression of the protein, resulting in a complete loss of function. PTEN hemizygous inactivation may be still functionally significant when combined with abnormalities of other genes which converge on its downstream pathway. Additionally, PTEN promoter methylation is related with tumor metastasis and poor prognosis [18]. PTEN acts in opposition to phosphotidylinositol-3-kinase (PIK3CA) to control levels of phosphorylated AKT. PIK3CA mutation can be present simultaneously with PTEN mutation in about 30% of endometrioid cancer cases, indicating these two genes possibly have a synergistic effect for the cancer development [19]. PTEN also is suggested to be a target of microsatellite instability (MSI)-driven mutagenesis, and it is interesting that deletion of >/=3 basepairs in PTEN is more common in MSI-positive cancers than those without MSI [20].
16.2.3 MSI and DNA Mismatch Repair Gene Dysfunction
Microsatellites are short segments of repetitive DNA bases that are scattered throughout the genome; they are found predominantly in noncoding DNA. MSI is the propensity to develop changes in the number of repeat elements as compared with normal tissue due to DNA repair errors made during replication. MSI is due to inactivation of any of a number of intranuclear proteins that comprise the mismatch repair system (MMR), leading to accumulation of structural changes in coding and noncoding repetitive elements of many genes. The MMR system is very important for gene stability, and represents the third type of mechanism for tumorgenesis next to oncogenes and tumor suppressor genes. So far, nine MMR genes have been successfully identified, including hMSH2, hMSH3, hMSH4, hMSH5, hMSH6, hPMS1, hPMS2, hMLH1, and hMLH3. Because simple repeat sequences are unstable in cells with MSI, and most commonly the observed mutation is secondary to defective MLH1 expression (usually due to methylation). Since MLH1 is important in repair of short segments (two to four bases), and MSH2 and MSH6 serve to repair larger insertion-deletion mutations, the combined defect of the mismatch repair system results in inhibition of both small and large insertion-deletion mismatch repair. MSI may specifically inactivate those genes which contain susceptible repeat elements, such as PTEN, transforming growth factor β-receptor type II (TGF-βRII), BAX, insulin-like growth factor II receptor (IGFIIR) and other genetic changes, resulting in secondary tumor subclones with an altered capacity of cancer development.
Due to menstrual cycling, the normal endometrium undergoes constant remodeling and proliferation and thus has an increased propensity for replicative errors; therefore, the endometrium is highly dependent on the MMR system. As a result, MMR mutation has been shown to be present in 25–30% of type I endometrial carcinoma [21, 22]. MLH1 inactivation is the most common mechanism in MMR-related endometrial carcinoma and is accomplished by hypermethylation of CpG islands in the gene promoter, a process known as epigenetic silencing, which is related to sporadic endometrial carcinoma [23, 24]. Inherited or somatically acquired mutations of MSH6, another mismatch repair element, are also common in endometrial cancer patients with MSI-related tumors. A single nucleotide insertion (frameshift) mutation in MSH2 has been described less frequently in endometrial cancers with MSI; this deletion occurs in a string of eight consecutive adenosine residues. All these features may guide us to screen patients with Lynch syndrome (see below).
16.2.4 β-Catenin (CTNNB1) Alteration
β-Catenin is a cellular adhesion component of the E-cadherin-catenin unit, and is essential for cell differentiation and maintenance of normal tissue architecture. It plays an important role in signal transduction. Increased nuclear levels of β-catenin produce transcriptional activation through the LEF/Tcf and the ubiquitin-proteasome pathways.
CTNNB1 mutation improves its protein stability, and leads to its accumulation in the cytoplasm and nuclei. Additionally, it activates its downstream target genes, such as transitional factors of wnt pathway. Abnormal β-catenin expression may be seen in endometrioid carcinoma (33–47%), and rarely non-endometrioid subtypes (1–3%) [25]. In all endometrioid carcinoma with β-catenin mutation, ER and most of PR are positive, suggestive of an intimate relationship between β-catenin and ER [26]. It may represent a pathway to endometrial carcinogenesis, which can be associated with squamous differentiation, a common finding in endometrioid cancers and atypical polypoid adenomyomas . Although MSI, PTEN, and K-ras mutations frequently coexist with each other, these molecular abnormalities are not usually seen in tumors with β-catenin alterations [27]. CTNNB1 mutation can be seen in some atypical hyperplasia\EIN cases, indicating an early step of endometrial tumorigenesis. When mutation occurs, changes in β-catenin expression are usually seen throughout all tumor cells, suggesting a clonal expansion process. β-Catenin may also regulate the expression of the matrix metalloprotease-7, which would indicate a role in the establishment of the microenvironment necessary for initiation and maintenance of growth of the endometrioid cancers and their metastasis [28]. Of note, gain of function mutations in exon 3 of CTNNB1 gene at 3p21 are seen in 25–40% of endometrioid cancers [29], resulting in stabilization of the protein. Mutations in exon 3 of the CTNNB1 gene may identify low-grade, low-stage, endometrioid carcinomas at risk for recurrence [30, 31].
16.2.5 K-ras Mutation
K-ras mutations have been identified in 10–30% of endometrioid carcinomas as well as endometrial hyperplasia [32]. The latter suggests that K-ras mutation is an early event in carcinogenesis. Compared with endometrioid carcinoma, the rate of K-ras mutation in non-endometrioid cancers is relatively low. K-ras mutation may cause resistance to epidermal growth factor receptor (EGFR) inhibitors. There is a higher frequency of K-ras mutations in MSI cancers, and many of these are characterized as methylation-related GC → AT transitions. It has also recently found that K-ras mutations are more commonly seen in endometrioid carcinomas with mucinous differentiation or endometrial mucinous cancers [33, 34]. Accordingly, K-ras mutation analysis is not a suitable biomarker to differentiate endometrioid carcinoma from endometrial mucinous cancers. K-ras mutations have also been reported in associated with the microcystic elongated and fragmented (MELF) pattern of myometrial invasion in endometrioid carcinomas [35].
16.2.5.1 PAX 2
PAX2 is a gene that plays an important role in the embryonic development of the Mullerian and urogenital systems. It encodes a nuclear transcription factor, which is present in normal endometrium. Immunohistochemistry demonstrates nuclear staining in normal endometrial glands. Similar to PTEN, PAX2 does show loss in normal endometrium (36%), atypical hyperplasia or EIN (71%) and carcinoma (77%) as demonstrated by Monte et al. They suggest that a major mechanism of the development of atypical hyperplasia or EIN is the co-localization of PAX2 and PTEN within the same endometrial glands [36]. This “dual-hit” is thought to be the cause for the majority of sporadic endometrioid carcinomas, although the detailed molecular mechanisms are unclear. Many publications have sought to describe the relationship between PAX2 loss, the immunohistochemical findings, and the diagnosis of atypical hyperplasia or EIN [17, 37, 38], the overall conclusion in this setting is that PAX2 has been found to be useful in the diagnosis of atypical hyperplasia or EIN.
16.2.6 PI3K/AKT Pathway
The PI3K/AKT pathway is activated in a broad range of malignant tumors. Stimulating signals through receptor tyrosine kinases (RTKs) activate PI3K, which phosphorylates PIP2 to generate PIP3. PIP3 binds to AKT triggering a complex cascade of signals that regulate growth, proliferation, survival, and motility. PI3CA mutation is often combined with other genetic abnormalities, such as mutations in c-erB2, K-ras, and PTEN. The lipid phosphatase, PTEN, antagonizes this process by dephosphorylating PIP3 to inhibit activation of AKT. About 28% endometrioid carcinomas have PI3K mutations [39], but ESCs also have these mutations at comparable frequencies.
16.2.7 FGFR2 Alterations
FGFR2 activation can promote cell proliferation, migration, and survival. FGFR2 mutations are seen in 10–16% endometrioid cancers [40]. FGFR2 mutation is often companied by PTEN loss, while FGFR2 and K-ras mutations rarely coexist. Endometrioid carcinoma cell lines with EGFR2 mutations have been reported as sensitive to pan-FGFR inhibitor PD173074, suggesting that FGFR2 could be a new therapeutic target [41].
16.2.8 MicroRNA (miRNA)
MiRNA is a small noncoding RNA (containing about 22 nucleotides), widely found in plants, virus, animals, and human beings, which functions in RNA silencing and posttranscriptional regulation of gene expression. Abnormal MiRNA expression is closely related to tumorigenesis and cancer development. In patients with endometrioid carcinomas, cancer tissues and blood plasma have a higher level of miRNAs (including miRNA-99a, -100, and -199b), which are able to suppress tumor growth through the mTOR pathway. Similarly, deletion of both miRNA-410 and -487, located on 14q32, is associated with a poor prognosis in patients with endometrioid cancers [42]. In contrast to the above miRNA species, miRNA-200 family (including miRNA-200a, -200b, -200c, and -429) are highly expressed in low-grade endometrioid cancers, which may promote tumor growth and recurrence [43,44,45].
16.2.9 The Model of Endometrioid Carcinoma Development
Endometrioid carcinoma is frequently preceded by estrogen-induced changes commonly referred to as hyperplasia, some of which are monoclonal proliferations of genetically altered endometrial glands presenting as a discrete lesion termed endometrioid intraepithelial neoplasia (EIN). The common term “hyperplasia” historically was applied to all entities, with the implication that non-atypical and atypical hyperplasia subgroups correspond to benign and precancerous groups, respectively. In the 2014 WHO classification, atypical hyperplasia is considered to be equivalent to EIN. Notably, the 2014 WHO classification termed it “endometrioid” rather than “endometrial” intraepithelial neoplasia to further clarify its role as an endometrioid carcinoma precursor. Somatic mutation of endometrial epithelium is very common in “normal” endometrium, and occurs in advance of any discernible histopathologic changes. The term “latent precancer” has been applied to this condition to emphasize that endometrial cancer risk is not necessarily increased at this stage. This preclinical phase of disease is recognizable only through genetic analysis of mutant cells or identified by biomarkers such as loss of PTEN expression and acquisition of microsatellite instability, not by routine microscopy. Based on this understanding, endometrioid carcinoma develops from a latent precancer to precancer (atypical hyperplasia or EIN) , and to well-differentiated endometrioid carcinoma. The basic steps of cancer development as well as the main molecular alterations are summarized in Fig. 16.2.
16.2.10 Lynch Syndrome-Related Endometrial Cancer
In endometrial cancers, MSI is very common. There are two conditions which may result in MSI. One is hypermethylation of the MLH1 gene promoter resulting in gene silencing. Hypermethylation is a common epigenetic event seen in 15–25% of corresponding sporadic cancers. The second condition is a germ line mutation of one or more of MMR genes (MLH1, MSH2, MSH6, or PMS2). Mutations of the above genes can induce MSI resulting in development of Lynch syndrome (LS), an autosomal dominant inherited cancer susceptibility syndrome, also known as hereditary non-polyposis colon cancer (HNPCC) . Women with LS have a 40–60% chance of presenting with endometrial cancer, usually the endometrioid variant, as their first clinical manifestation. Among LS-related endometrial cancers, mutation of MSH2 is the most common (50–66%), and MLH1 (24–40%) and MSH6 (10–13%) are less frequent [46]. LS-related endometrial cancers have some special characteristics : the mean age is younger than the general population; there may be a lack of estrogen overstimulation; they have a tendency to involve the lower uterine segment (LUS) ; and they demonstrate mixed tumor histology, with increased tumor-infiltrating lymphocytes, and a Crohn-like inflammatory infiltrate at the tumor invading edge [47]. It should be noted that these morphologic findings are not specific and have a low predictive value for the presence of LS. This is the main reason universal screening by MMR immunohistochemistry is being employed in many medical centers.
16.2.11 Progestin-Resistant Endometrial Cancer
To preserve fertility, progestin has historically been administered to significant subsets of young patients with clinical stage I, grade 1 endometrial adenocarcinoma; however, a significant proportion of such cancers do not respond. Although the underlying mechanism of such resistance remain to be entirely clarified, some recently obtained insights are outlined below.
16.2.11.1 Progesterone Receptor (PR)
High-level expression of PRA and PRB has been associated with a decreased risk of persistence or progression, whereas low or absent PR in endometrial cancer cells is associated with a poor response to progesterone therapy. Moreover, progestin may activate the PI3K/AKT pathway independent of PR mediation in PR-negative or low-expression endometrial cancer cells. Inhibition of the PI3K/AKT pathway may restore PR expression and progestin sensitivity in some progestin-resistant endometrial cancer [48, 49]. From this perspective, manipulation of PI3K/AKT pathway remains a consideration for the clinical management of such patients after appropriate clinical validations.
16.2.12 Epidermal Growth Factor Receptor (EGFR) and Other Genes
High levels of EGFR expression have been reported in progestin-resistant endometrial cancer. Furthermore increased EGFR expression in endometrial cancer cell lines leads to reduced sensitivity to progestin treatment and decreased PR-B expression. As a result, the EGFR tyrosine kinase-specific inhibitor , Gefitib, may be useful in the treatment of endometrioid carcinoma [50]. Additionally, it has been found that Fas and FasL expression inhibits apoptosis [51]. The overexpression of Survivin through activation of Nrf2/AKR1C1 pathway may also contribute progestin resistance [52,53,54]. The clinical impact of these findings has yet to be determined as they are mostly in the research stage.
16.3 Endometrial Serous Carcinoma
Endometrial serous carcinoma (ESC) constitutes no more than 10% of all endometrial cancers, but frequently presents at an advanced stage and has a significantly worse prognosis than more common low- and intermediate-grade endometrioid cancers. ESC’s potential for rapid tumor progression, as well as the high mortality that is associated with advanced stage disease, both underscore the importance of understanding endometrial serous carcinogenesis so that its precancers can be diagnosed, and effective therapeutic intervention can be administered.
Serous carcinoma arises predominantly in resting endometrium , manifesting first as p53 immunoreactive, morphologically normal endometrial cells (p53 signatures ), evolving to endometrial glandular dysplasia (EmGD) , which is the first morphologically identifiable precancerous lesion, then to serous endometrial intraepithelial carcinoma (SEIC, a carcinoma with a noninvasive growth pattern in the uterus but commonly associated extrauterine disease) , and finally invasive ESC. This model of ESC development [2] has recently been recapitulated by a genetically engineered mouse model as well as in thoroughly described in other publications [55] (Figs. 16.3 and 16.4). Importantly, EmGD is a lesion that can be diagnosed by routine microscopic evaluation whose ablation or removal may potentially offer the opportunity to prevent the development of the associated malignancy.
16.3.1 Molecular Alterations in Endometrial Serous Neoplasia
There have been numerous studies on the molecular events underlying endometrial serous carcinogenesis. Some of these molecular events are also present in its precursor lesions, facilitating our understanding of the development of ESC. Whole exome sequencing of ESC cases has identified somatic mutations in TP53 (81.6%), PIK3CA (23.7%), FBXW7 (19.7%), and PPP2R1A (18.4%) among the 76 cases that were evaluated [56]. Zhao et al. found an increased mutational burden for TP53, PIK3CA, PPP2R1A, KRAS, FBXW7, and CHD4/Mi2b, along with amplification of chromosome segments containing ERBB2 and CCNE1 [57]. Comparable figures for Jones et al. included TP53 (76%), PIK3CA (29%), FBXW7 (12%), and K-ras (9.3%) [58], whereas Le Gallo et al. found somewhat different frequencies, with high frequency somatic mutations identified in the following genes: CHD4 (17%), EP300 (8%), ARID1A (6%), TSPYL2 (6%), FBXW7 (29%), SPOP (8%), MAP3K4 (6%), and ABCC9 (6%) [59].
16.3.1.1 Mutation of TP53
The p53 tumor suppressor gene, which is located on chromosome 17p 13.1, is the most commonly altered gene in human cancers [60, 61]. It is also the most important single gene for the generation of ESC [55]. Overexpression of the p53 protein, as assessed by immunohistochemistry, has been found in approximately 80–90% of ESC cases [62, 63], which is an extraordinarily high-rate supporting a significant role for TP53 gene alterations in endometrial serous carcinogenesis. Based on previous studies, the frequency of TP53 gene mutations in exons 5 to 8 from laser captured microdissected samples increases from p53 signature glands (42%), to EmGD (43%), to SEIC , (63–72%), and to ESC (96%) [64]. This is in contrast to the benign endometrial control uteri, where no TP53 gene mutation is present in non-signature glands [64, 65]. From these studies, and others, the logical conclusion is that TP53 gene mutation is a critical early step in endometrial serous carcinogenesis [2]. The importance of TP53 mutation in the development of ESC is further supported by a TP53 knockout mouse model, which recapitulates all the developmental processes observed in the humans [55]. Representative pictures of the ESC developmental model are illustrated in Fig. 16.5. This model recapitulates and confirms the process of ESC development in humans and is a useful foundation for further studies of ESC pathogenesis, early cancer detection, prevention, and clinical intervention.
Other non-TP53 related molecular events that may be significant in the development of ESC are summarized below.
16.3.1.2 PPP2R1A Mutations
Somatic missense mutations in the Ser/Thr protein phosphatase 2A (PP2A) scaffold subunit gene PPP2R1A have been identified in 18–40% of ESC. PPP2R1A plays a critical role in diverse cellular functions, including negative regulation of cellular proliferation and potential tumor suppression [56, 66,67,68]. PPP2R1A mutations are also seen in subsets of carcinosarcomas, but are apparently uncommon in other histotypes. Accordingly, they may not only be directly involved in endometrial serous carcinogenesis but may also form a serous histotype-related molecular target.
16.3.1.3 Cyclin E/FBXW7 Oncogenic Pathways
Approximately 45% of ESC display amplification of the CCNE1 gene as assessed by in situ hybridization [69]. The CCNE1 gene encodes the cyclin E1 protein, which is overexpressed by IHC in approximately 90% of ESC [70]. Cyclin E is a downstream molecule of F-box and WD repeat domain-containing 7 (FBXW7), which is mutated in 10–30% of ESC. CCNE1 amplifications have been identified in aggressive subsets of endometrioid carcinoma [71]; however, their significance in ESC is presently unclear.
16.3.1.4 BRCA Mutations
Some preliminary lines of evidence are suggestive of a relationship between the risk for breast cancers and endometrial cancers. One study from Sweden found that 7.28% of patients undergoing genetic counseling for an increased risk of breast cancer had family histories of both endometrial and breast cancer [72]. One large cohort study demonstrated that about 20% of women with ESC had a prior history of breast cancer and the ESC patients with breast cancer history tend to be younger than those patients without breast cancer history [73]. There are also reports suggesting a relationship between the germline BRCA1 mutation and ESC [74, 75]. The risk for serous/serous-like endometrial carcinoma is increased in BRCA1+ women [75]. This risk should be considered when discussing the advantages and risks of hysterectomy at the time of RRSO in BRCA1+ women.
16.3.1.5 Alterations of Extracellular Adhesion Molecules
Overall, studies on role of extracellular adhesion molecules in ESC development are relatively rare compared to studies on oncogenes and tumor suppressor genes. Changes in extracellular adhesion molecules may be related to the easy detachment of neoplastic cells in ESC and SEIC which explains their very high-rate of extrauterine metastasis. E-cadherin and claudins are the two extracellular molecules that likely contribute to the ability of ESC to shed and spread to distant sites. It has been reported that the downregulation of E-cadherin is associated with the progression of endometrial cancers [76,77,78,79]. Additionally, the adhesion molecule CD44 may play a role. CD44 is a protein involved in cell adhesion and lymphocyte homing, and one of its isoforms, CD44v6, may be related to capillary lymphatic space invasion and metastasis. A significant loss of CD44 and its isoform CD44v6 has been found in ESC compared with that of endometrioid cancers [80].
Alterations in intercellular adhesion molecules likely facilitate the trans-tubal spread of endometrial serous cancer cells, which explains why these cancers frequently present at advanced stages. This has been demonstrated in a previous study where 6 (67%) of 9 SEIC cases demonstrated carcinomatous deposits in the pelvis or peritoneal cavity [81]. Among those cases, about half showed free-floating serous carcinoma in the tubal lumen. These findings suggest that at least some of the extrauterine diseases evolve via trans-tubal metastasis, a contention that is supported by identical clones that is found in ESC, SEIC, and serous carcinomas at extrauterine sites [82, 83].
16.3.1.6 Amplification of HER2/neu
HER2/neu, also known as C-erbB2, is a proto-oncogene that encodes the human epidermal growth factor receptor 2. Amplification of the HER2/neu gene and overexpression of the HER2/neu protein have been demonstrated in many tumors, including ESC. Although expression of HER2/neu is mainly seen in ESC and advanced stage disease, it has been observed that cases of EmGD and SEIC demonstrate overexpression of HER2/neu by immunohistochemistry. There is no clinical role for use of HER2/neu in the diagnosis of ESC or its precursors at this point.
16.3.1.7 PIK3CA Mutations
Possible driver mutations in the PIK3CA/AKT/mTOR pathway have been identified in 24–29% of ESC [56, 58]. In vitro studies have shown that oncogenic PIK3CA mutations are common in HER2/neu-amplified ESC, and that this may represent a mechanism of resistance to anti-HER2 treatment [84], which can be overcome by dual HER2/PIK3CA targeting [85].
16.3.1.8 Overexpression of p16
The tumor suppressor protein p16 is also known as CDKN2A. Studies on this molecule are mainly related to HPV-related cancers and precancers, but p16 overexpression has also been demonstrated in the majority of cases of ESC, with one report showing 92% of ESC cases (22/24) with p16 overexpression, as compared to less than 25% of endometrioid cases [86]. Interestingly, the mechanisms of p16 overexpression in ESC may be related to the inactivation of Rb gene rather than through a HPV E7 protein regulation as HPV DNA in situ hybridization was negative in all ESC cases in one study [87]. By gene expression profiling, p16 is significantly upregulated in ESC above normal endometrial cells and endometrioid carcinomas, all of which suggests dysregulation of the p16INKA/Cyclin D-CDK/pRb-E2F pathway [88, 89]. Additionally, it has been observed that p16 protein is overexpressed in lesions of EmGD and SEIC (Zheng et al., unpublished). In a clinical setting, diffuse, strong staining is usually supportive of a diagnosis of ESC or serous EIC.
16.3.1.9 Other Molecular Changes
Overexpression of Insulin-like growth factor II m-RNA binding protein 3 (IMP3) is typically expressed in embryonic tissues but rarely in adult tissue with the exception of placenta and gonads. IMP3 was found to be expressed in 3 (14%) of 21 EmGD, 16 (89%) of 18 serous EIC, and 48 (94%) of 51 ESC. In contrast, none of 35 EIN and only 5 (7%) of 70 endometrioid cancers exhibited IMP3 overexpression [90]. The findings suggest that IMP3 expression is more associated with endometrial serous cancer development and may contribute to its aggressive clinical behavior. The transcription factor NF-E2-related factor 2 (Nrf2) is thought to enhance resistance of cancer cells to chemotherapeutic drugs and was found to be expressed in 41 (89%) of 46 ESC cases, compared with marginal expression in endometrioid cancers and no expression in benign endometria [91]. Moreover, Nrf2 was also identified in EmGD and serous EIC in 40% and 75% of cases, respectively [91]. The relationship between Nrf2 and p53 mutation in latent precancer (p53 signature ) and precancerous lesions has yet to be fully elucidated.
The molecular changes in the process of ESC development are summarized in Fig. 16.6.
16.3.2 The Model of Endometrial Serous Carcinogenesis
Previously, it was suggested that ESC arises from SEIC in atrophic endometria via an estrogen independent “de novo” process [3, 92]. It has been proposed that SEIC is a likely precursor lesion for ESC [3, 93, 94]. From a developmental and evolutionary point of view, this was probably correct, since the occurrence of the fully developed ESC typically appears later than the lesions of SEIC. However, this “precursor” concept is misleading as the “precursor” lesion of a given malignancy is not necessarily synonymous with its “precancer ” lesion. Indeed, published data indicate that many observers, including gynecologists and pathologists, accepted SEIC as a precancer or, “noninvasive” cancer, controversially in the past. Many patients with SEIC experience recurrence or intra-abdominal serous carcinomatosis after simple hysterectomy without staging due to the limited understanding of this unusual “intraepithelial” carcinoma. It is now known that up to two-thirds of SEIC may be associated with extrauterine disease [2], the phenomenon is likely to be trans-tubal metastasis as discussed above.
There are several drawbacks of this “atrophic endometrium (AE) → SEIC → ESC” carcinogenesis model. First, this model does not incorporate the presence of dysplastic lesions bridging the gap between completely benign endometrium and frankly malignant SEIC . In the majority of other human organs, accepted models of epithelial carcinogenesis typically involve an evolution from benign epithelium → dysplasia (lesions in transition) → intraepithelial carcinoma or carcinoma in situ → invasive carcinoma. This is also supported by tubal serous carcinogenesis in which an intermediate lesion, termed “tubal lesions in transition (TILT)” links normal looking tubal mucosa to tubal intraepithelial carcinoma . Secondly, SEIC and/or ESC are not always associated with atrophic endometrium. Many gynecologic pathologists have identified ESC cases that mimicked endometrioid carcinoma partially because of the presence of non-atrophic background endometrium. One possibility is that ESC cases that were diagnosed more than 40 years ago were associated with an atrophic background more often because a limited number of women at that time were undergoing hormone replacement therapy . Hormone replacement therapy has become more popular in postmenopausal women in the recent past (although this practice is falling out of style due to its known side effects). The utilization of these hormones may help to explain why 40% of the background non-neoplastic endometrium in women diagnosed with ESC or SEIC were non-atrophic (34% proliferative, 6% hyperplastic) in one analysis [95]. These findings suggest that SEIC or ESC can derive not only from atrophic endometrium but also from resting or even hyperplastic endometrium depending on an individual woman’s hormonal status. Finally, SEIC does not meet the criteria of “precancer” given its many shared features with ESC, including morphology, molecular biology, clinical behavior, and management [3, 63, 81, 95,96,97,98]. Accordingly, SEIC is best viewed as ESC with a noninvasive growth pattern in the uterus, rather than a precancerous lesion in the process of ESC development [2, 81]. Understanding the nature of SEIC—as an ESC without myometrial invasion but with a significant potential for extrauterine spread—will help to prevent the undertreatment of afflicted patients. The diagnostic term “SEIC ” or “EIC” should not be used in the clinic without an explanatory comment in order to avoid management confusion [99]. Alternative terms such as ESC with a size description may suffice for diagnostic and management purposes.
In contrast to SEIC , EmGD meets the majority of criteria required to label a lesion as a precancer (as defined by a group of experts in the 2006 NCI consensus conference) [100]. This rationale may be summarized as follows: (1) EmGD lesions are morphologically identifiable (detailed diagnostic criteria are described in Chap. 17). (2) cytologically, direct transition between EmGD and SEIC, but not between EmGD and ESC, have been described [95]. (3) comparison of the extent, and range, of genomic damage between EmGD and ESC (including SEIC) explains their differing morphology and behavior [95, 101]. A p53 mutational analysis of laser capture microdissected endometrial samples demonstrated that TP53 mutations increased in a progressive fashion from EmGD (16/37, 43%) to serous EIC (18/25, 72%) and ESC (21/23, 91%) [64]. In addition, IMP3 showed an increased level of expression from EmGD (3/21, 14%) to SEIC (16/18, 89%) and to ESC (48/51, 94%) [90]. (4) Identical TP53 mutations have been found in EmGD and serous EIC or ESC [64]. (5) In a retrospective study, EmGD was found to be present and identifiable in endometrial biopsies taken prior to the development of ESC, indeed it has been estimated that a diagnosis of EmGD in an endometrial biopsy may confer up to a ninefold increased risk of developing ESC [102]. (6) A mouse model with p53 selectively knockout in the mullerian system has accurately recapitulated all of the processes detailed above [2]. Such findings at least partially indicate a lineage continuity between EmGD and ESC, therefore providing a reasonable evidence that ESC likely arises in EmGD [2].
Molecular changes typically occur prior to morphologic changes, which, in the case of serous carcinogenesis, has been identified as a group of benign-appearing endometrial glands/epithelia with intense p53 IHC staining, designated “p53 signatures” [65]. These p53 signatures were frequently found in the benign-appearing endometrium adjacent to ESC and only rarely in the endometrium adjacent to endometrioid carcinomas or in noncancerous uteri, and have been found to display a frequency of p53 gene mutation that is similar to lesions of EmGD .
Overall, the totality of available clinicopathologic and molecular evidence supports the concept of EmGD as the precancer for ESC, with p53 signatures representing a latent precancer in the process of endometrial serous carcinogenesis. This understanding begets the model of endometrial serous carcinogenesis from resting endometrium → p53 signature → EmGD → SEIC → ESC (Figs. 16.3–16.6).
16.4 Endometrial Clear Cell Carcinoma and Other Endometrial Cancers, Including Carcinosarcoma and Dedifferentiated Carcinoma
As listed in the 2014 WHO classification, endometrial cancers have multiple histologic types. Among them, knowledge of the carcinogenesis of endometrial clear cell carcinoma (ECCCs) , carcinosarcoma, dedifferentiated/undifferentiated carcinoma, and other rare cancers of the endometrium are very much limited. This chapter will only briefly discuss a few key points of the genesis of these cancers.
16.4.1 Endometrial Clear Cell Carcinoma
Clear cell carcinoma of the endometrium is a rare type of endometrial cancer that has generally been considered to follow an aggressive course, although reported patient outcomes have been variable. Although ECCCs were not included in the original The Cancer Genome Atlas (TCGA) dataset [12], a few recent studies have established that ECCC is a molecularly heterogeneous histotype that may show features of ESC , endometrioid carcinoma, neither or both. TCGA-like molecular subsets are demonstrable in this tumor type [103, 104]. The variable biologic behavior of this tumor was highlighted in a recent genetic landscape study [105]. DeLair et al. performed a rigorous histopathological review , immunohistochemical analysis, and massively parallel sequencing targeting of 300 cancer-related genes of 32 pure ECCCs. Eleven (34%), seven (22%), and six (19%) ECCCs showed abnormal expression patterns for p53, ARID1A, and at least one DNA mismatch repair (MMR) protein, respectively. Targeted sequencing data were obtained from 30 of the 32 ECCs included in this study, and these revealed that two ECCCs (7%) were ultramutated and harbored mutations affecting the exonuclease domain of DNA polymerase epsilon (POLE) . In POLE wild-type ECCCs, TP53 (46%), PIK3CA (36%), PPP2R1A (36%), FBXW7 (25%), ARID1A (21%), PIK3R1 (18%), and SPOP (18%) were the genes most commonly affected by mutations. ECCCs less frequently harbored mutations affecting CTNNB1 and PTEN but more frequently harbored PPP2R1A and TP53 mutations than non-POLE endometrioid carcinomas compared to the original TCGA—endometrial cancer study [12]. Compared to ESC results obtained by TCGA study, ECCCs less frequently harbored TP53 mutations. When a surrogate model for the molecular-based TCGA classification [12] is used, all molecular subtypes previously identified in endometrioid and serous endometrial cancers are present in the studied cases of ECCCs. These include ultramutated , MMR-deficient, copy-number high with TP 53 mutation, and copy-number low (endometrioid-like) with wild-type TP53 [105]. These ECCC cases, except those with copy-number high serous-like cancers, have had a significantly better prognosis than the authors expected [105]. Such findings show that ECCCs constitute a histologically and genetically heterogeneous group of tumors with varying outcomes. Accordingly, previous categorizations of ECCCs as type II or as being inherently aggressive cancers require a reevaluation.
16.4.2 Endometrial Carcinosarcoma
Carcinosarcoma of the endometrium is a rare gynecological neoplasm, which accounts for <3% of all uterine malignancies . Traditionally this tumor has been regarded as a subtype of uterine sarcoma, and its origin remains controversial. The exact nature and prognosis was not clear in the past.
The carcinomatous components may correspond to any Mullerian type, but the majority are high-grade, such as serous carcinoma . This type of tumor is broadly divided into two groups, homologous and heterologous, depending on the characteristics of the stroma or mesenchymal components. Both epithelial and mesenchymal components can be either intimately admixed or sharply demarcated, additionally, the components vary from relatively equal distribution to dramatically different proportions.
Traditionally, there have been four theories regarding the histogenesis of endometrial carcinosarcoma. (1) The collision theory suggests that the epithelial and mesenchymal elements have arisen independently and collide yielding a single mixed tumor; (2) the combination theory suggests that both components are derived from a single stem cell that has undergone divergent differentiation early in its evolution; (3) a composition tumor that is an endometrial carcinoma with reactive, atypical stroma; and (4) the conversion theory that suggests that the sarcomatous element is derived from carcinoma during the evolution of the tumor. It is believed that endometrial carcinosarcomas have a Mullerian duct origin and a capacity to differentiate into various mesenchymal and epithelial components. This “conversion theory” has been broadly accepted. Carcinosarcomas are mostly of monoclonal origin with the carcinomatous component being the driving force. At the molecular level, the conversion from epithelial to mesenchymal phenotype is likely through an epithelial-mesenchymal transition (EMT) process since the genetic changes in sarcoma are similar with the accompanied carcinomas [106, 107].
The pattern of metastasis in carcinosarcoma depends on dominancy of the type of tumor components. Most studies suggest that the behavior of carcinosarcomas is mainly governed by the carcinomatous component. Carcinoma typically spread through the lymphatic channels to nearby lymph nodes, while sarcomas frequently metastasize to the peritoneal cavity or hematogenously spread to distant organs. In sarcoma, lymph node metastasis is very uncommon. The majority of metastatic carcinosarcoma consist only of the carcinomatous component. Such observations suggest that the carcinomatous component is predominantly responsible for most metastasis and sarcomatous component plays only a minor role.
16.4.3 Endometrial Undifferentiated and Dedifferentiated Carcinoma
Undifferentiated endometrial carcinoma is a highly aggressive subtype of endometrial cancer. Histologically, undifferentiated endometrial carcinoma is composed of sheet-like monotonous and discohesive tumor cells, which typically possess scant to moderate amount of cytoplasm. These tumors lack any evidence of glandular formation or significant squamous differentiation. Because of this undifferentiated appearance, a definitive diagnosis may be difficult to impossible on biopsy specimens. Ancillary immunohistochemical analysis will essentially be negative for pankeratin, lymphoid markers, melanoma markers, epithelial membrane antigen (only rare cells), estrogen receptor, PAX8, and E-cadherin (relative to grade 3 endometrioid carcinomas) and can be used to support its diagnosis. Of note, CK18 may strongly stain rare cells. MMR protein immunohistochemistry may be useful as about half of undifferentiated endometrial carcinomas are MMR protein-deficient, whereas MMR protein deficiency is comparatively uncommon in other uterine malignancies [108].
Dedifferentiated endometrial carcinoma contains a component of undifferentiated carcinoma in addition to a component of typically low-grade endometrioid-type carcinoma. The undifferentiated component of dedifferentiated endometrial carcinoma exhibits similar histologic and immunophenotypic features to those seen in pure undifferentiated endometrial carcinomas. It is important to distinguish these tumors from other high-grade carcinoma as their behavior is significantly more aggressive.
It has been suggested that inactivation of core components of the switch/sucrose non-fermentable (SWI/SNF) chromatin remodeling complex proteins, specifically ARID1A/ARID1B (co-inactivation), BRG1 (encoded by SMARCA4), and INI1 (encoded by SMARCB1) as the likely molecular triggers underlying the apparent “dedifferentiation” of low-grade endometrioid carcinoma in about 70% of cases [109]. The loss of these core SWI/SNF complex proteins has been hypothesized to prevent müllerian epithelial differentiation, thereby arresting tumor cells in an undifferentiated state with significantly reduced level or even absent expression of Pax-8 and estrogen receptor, in contrast to that of the differentiated endometrioid component. Undifferentiated carcinomas with SWI/SNF complex-inactivation are more commonly associated with extrauterine disease and have a significantly worse prognosis [110]. Although dedifferentiated carcinomas behave badly in general, they do not universally behave poorly if associated with a POLE mutation [111]. Such findings further emphasize the importance of understanding the endometrial cancers at the molecular level.
16.5 A Proposed Unified Pathologic Nomenclatural Classification of Endometrial Preneoplasia
As discussed above, this chapter has primarily focused on the most common histologic types of endometrial cancer, including endometrioid and serous carcinomas, and briefly covered clear cell, undifferentiated, and dedifferentiated carcinoma . Diverse nomenclatures have been proposed for the various putative precursor lesions for these entities, the totality of which may potentially cause confusion in clinical practice. It has been suggested that an expanded definition of the term “endometrial intraepithelial neoplasia, EIN” that encompasses all the major histotypes should be included in each category as prefix. For endometrioid lesions, the proposal entails adoption of the EIN system advanced by Mutter and colleagues, in which a distinction is made between benign endometrial hyperplasia and strictly defined EIN; the latter would henceforth be referred to as “Endometrioid EIN.” For serous lesions, the proposal entails discontinuation of the term “Endometrial Intraepithelial Carcinoma, ” as these lesions may metastasize and should be considered a special form of ESC. The precancerous lesion described previously as EmGD would be referred to as “Serous EIN” under the proposal. Similarly, the previously characterized putative precursor lesion for clear cell carcinomas will be designated “Clear cell EIN. ” This system is envisioned as one that can readily incorporate new information such as grading, or the description of precursors, for the other histotypes (Fig. 16.7). Much is unknown about the nature, morphologic spectrum , and clinical significance of endometrial precancers. It is hoped that the system proposed herein would provide a coherent nomenclatural framework in which candidate lesions can be investigated and reported in daily surgical pathology practice in a more uniformed manner.
References
Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983;15:10–7.
Zheng W, Xiang L, Fadare O, Kong B. A proposed model for endometrial serous carcinogenesis. Am J Surg Pathol. 2011;35:e1–e14.
Sherman ME, Bur ME, Kurman RJ. p53 in endometrial cancer and its putative precursors: evidence for diverse pathways of tumorigenesis. Hum Pathol. 1995;26:1268–74.
Coller HA, Grandori C, Tamayo P, et al. Expression analysis with oligonucleotide microarrays reveals that MYC regulates genes involved in growth, cell cycle, signaling, and adhesion. Proc Natl Acad Sci U S A. 2000;97:3260–5.
Risinger JI, Maxwell GL, Chandramouli GV, et al. Microarray analysis reveals distinct gene expression profiles among different histologic types of endometrial cancer. Cancer Res. 2003;63:6–11.
Zorn KK, Bonome T, Gangi L, et al. Gene expression profiles of serous, endometrioid, and clear cell subtypes of ovarian and endometrial cancer. Clin Cancer Res. 2005;11:6422–30.
Clarke BA, Gilks CB. Endometrial carcinoma: controversies in histopathological assessment of grade and tumour cell type. J Clin Pathol. 2010;63:410–5.
Fadare O, Zheng W, Crispens MA, et al. Morphologic and other clinicopathologic features of endometrial clear cell carcinoma: a comprehensive analysis of 50 rigorously classified cases. Am J Cancer Res. 2013;3:70–95.
Han G, Soslow RA, Wethington S, et al. Endometrial carcinomas with clear cells: a study of a heterogeneous group of tumors including interobserver variability, mutation analysis, and immunohistochemistry with HNF-1beta. Int J Gynecol Pathol. 2015;34:323–33.
Felix AS, Brasky TM, Cohn DE, et al. Endometrial carcinoma recurrence according to race and ethnicity: an NRG oncology/gynecologic oncology group 210 study. Int J Cancer. 2017;
Gilks CB, Oliva E, Soslow RA. Poor interobserver reproducibility in the diagnosis of high-grade endometrial carcinoma. Am J Surg Pathol. 2013;37:874–81.
Cancer Genome Atlas Research N, Kandoth C, Schultz N, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67–73.
Potischman N, Hoover RN, Brinton LA, et al. Case-control study of endogenous steroid hormones and endometrial cancer. J Natl Cancer Inst. 1996;88:1127–35.
Effects of hormone replacement therapy on endometrial histology in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. The Writing Group for the PEPI Trial. JAMA. 1996;275:370–5.
Mutter GL, Lin MC, Fitzgerald JT, Kum JB, Eng C. Changes in endometrial PTEN expression throughout the human menstrual cycle. J Clin Endocrinol Metab. 2000;85:2334–8.
Zheng W, Baker HE, Mutter GL. Involution of PTEN-null endometrial glands with progestin therapy. Gynecol Oncol. 2004;92:1008–13.
Mutter GL, Lin MC, Fitzgerald JT, et al. Altered PTEN expression as a diagnostic marker for the earliest endometrial precancers. J Natl Cancer Inst. 2000;92:924–30.
Salvesen HB, MacDonald N, Ryan A, et al. PTEN methylation is associated with advanced stage and microsatellite instability in endometrial carcinoma. Int J Cancer. 2001;91:22–6.
Oda K, Stokoe D, Taketani Y, McCormick F. High frequency of coexistent mutations of PIK3CA and PTEN genes in endometrial carcinoma. Cancer Res. 2005;65:10669–73.
Cohn DE, Basil JB, Venegoni AR, et al. Absence of PTEN repeat tract mutation in endometrial cancers with microsatellite instability. Gynecol Oncol. 2000;79:101–6.
Burks RT, Kessis TD, Cho KR, Hedrick L. Microsatellite instability in endometrial carcinoma. Oncogene. 1994;9:1163–6.
Catasus L, Machin P, Matias-Guiu X, Prat J. Microsatellite instability in endometrial carcinomas: clinicopathologic correlations in a series of 42 cases. Hum Pathol. 1998;29:1160–4.
Esteller M, Catasus L, Matias-Guiu X, et al. hMLH1 promoter hypermethylation is an early event in human endometrial tumorigenesis. Am J Pathol. 1999;155:1767–72.
Duggan BD, Felix JC, Muderspach LI, et al. Microsatellite instability in sporadic endometrial carcinoma. J Natl Cancer Inst. 1994;86:1216–21.
Moreno-Bueno G, Hardisson D, Sanchez C, et al. Abnormalities of the APC/beta-catenin pathway in endometrial cancer. Oncogene. 2002;21:7981–90.
Koul A, Willen R, Bendahl PO, Nilbert M, Borg A. Distinct sets of gene alterations in endometrial carcinoma implicate alternate modes of tumorigenesis. Cancer. 2002;94:2369–79.
Palacios J, Gamallo C. Mutations in the beta-catenin gene (CTNNB1) in endometrioid ovarian carcinomas. Cancer Res. 1998;58:1344–7.
Brabletz T, Jung A, Dag S, Hlubek F, Kirchner T. beta-catenin regulates the expression of the matrix metalloproteinase-7 in human colorectal cancer. Am J Pathol. 1999;155:1033–8.
Fukuchi T. Pathology division NCCRITJSMHKSS. Beta-catenin mutation in carcinoma of the uterine endometrium. Cancer Res. 1998;58:3526.
Liu Y, Patel L, Mills GB, et al. Clinical significance of CTNNB1 mutation and Wnt pathway activation in endometrioid endometrial carcinoma. J Natl Cancer Inst. 2014;106
Kurnit KC, Kim GN, Fellman BM, et al. CTNNB1 (beta-catenin) mutation identifies low grade, early stage endometrial cancer patients at increased risk of recurrence. Mod Pathol. 2017;30:1032–41.
Engelsen IB, Akslen LA, Salvesen HB. Biologic markers in endometrial cancer treatment. APMIS. 2009;117:693–707.
Xiong J, He M, Jackson C, et al. Endometrial carcinomas with significant mucinous differentiation associated with higher frequency of k-ras mutations: a morphologic and molecular correlation study. Int J Gynecol Cancer. 2013;23:1231–6.
Xiong J, He M, Hansen K, et al. The clinical significance of K-ras mutation in endometrial “surface epithelial changes” and their associated endometrial adenocarcinoma. Gynecol Oncol. 2016;142:163–8.
Stewart CJ, Amanuel B, Grieu F, Carrello A, Iacopetta B. KRAS mutation and microsatellite instability in endometrial adenocarcinomas showing MELF-type myometrial invasion. J Clin Pathol. 2010;63:604–8.
Monte NM, Webster KA, Neuberg D, Dressler GR, Mutter GL. Joint loss of PAX2 and PTEN expression in endometrial precancers and cancer. Cancer Res. 2010;70:6225–32.
Quick CM, Laury AR, Monte NM, Mutter GL. Utility of PAX2 as a marker for diagnosis of endometrial intraepithelial neoplasia. Am J Clin Pathol. 2012;138:678–84.
Jeffus SK, Winham W, Hooper K, Quick CM. Secretory endometrial intraepithelial neoplasia. Int J Gynecol Pathol. 2014;33:515–6.
Yuan TL, Cantley LC. PI3K pathway alterations in cancer: variations on a theme. Oncogene. 2008;27:5497–510.
Byron SA, Gartside M, Powell MA, et al. FGFR2 point mutations in 466 endometrioid endometrial tumors: relationship with MSI, KRAS, PIK3CA, CTNNB1 mutations and clinicopathological features. PLoS One. 2012;7:e30801.
Byron SA, Pollock PM. FGFR2 as a molecular target in endometrial cancer. Future Oncol. 2009;5:27–32.
Torres A, Torres K, Pesci A, et al. Diagnostic and prognostic significance of miRNA signatures in tissues and plasma of endometrioid endometrial carcinoma patients. Int J Cancer. 2013;132:1633–45.
Lee JW, Park YA, Choi JJ, et al. The expression of the miRNA-200 family in endometrial endometrioid carcinoma. Gynecol Oncol. 2011;120:56–62.
Xiong H, Li Q, Liu S, et al. Integrated microRNA and mRNA transcriptome sequencing reveals the potential roles of miRNAs in stage I endometrioid endometrial carcinoma. PLoS One. 2014;9:e110163.
Karaayvaz M, Zhang C, Liang S, Shroyer KR, Ju J. Prognostic significance of miR-205 in endometrial cancer. PLoS One. 2012;7:e35158.
Bonadona V, Bonaiti B, Olschwang S, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA. 2011;305:2304–10.
Wang Y, Wang Y, Li J, et al. Lynch syndrome related endometrial cancer: clinical significance beyond the endometrium. J Hematol Oncol. 2013;6:22.
Upson K, Allison KH, Reed SD, et al. Biomarkers of progestin therapy resistance and endometrial hyperplasia progression. Am J Obstet Gynecol. 2012;207:36 e1–8.
Gu C, Zhang Z, Yu Y, et al. Inhibiting the PI3K/Akt pathway reversed progestin resistance in endometrial cancer. Cancer Sci. 2011;102:557–64.
Xu Y, Tong J, Ai Z, Wang J, Teng Y. Epidermal growth factor receptor signaling pathway involved in progestin-resistance of human endometrial carcinoma: In a mouse model. J Obstet Gynaecol Res. 2012;38:1358–66.
Wang S, Pudney J, Song J, et al. Mechanisms involved in the evolution of progestin resistance in human endometrial hyperplasia--precursor of endometrial cancer. Gynecol Oncol. 2003;88:108–17.
Chen X, Zhang Z, Feng Y, et al. Aberrant survivin expression in endometrial hyperplasia: another mechanism of progestin resistance. Mod Pathol. 2009;22:699–708.
Wang Y, Wang Y, Zhang Z, et al. Mechanism of progestin resistance in endometrial precancer/cancer through Nrf2-AKR1C1 pathway. Oncotarget. 2016;7:10363–72.
Fan R, Wang Y, Wang Y, Wei L, Zheng W. Mechanism of progestin resistance in endometrial precancer/cancer through Nrf2-survivin pathway. Am J Transl Res. 2017;9:1483–91.
Wild PJ, Ikenberg K, Fuchs TJ, et al. p53 suppresses type II endometrial carcinomas in mice and governs endometrial tumour aggressiveness in humans. EMBO Mol Med. 2012;4:808–24.
Kuhn E, Wu RC, Guan B, et al. Identification of molecular pathway aberrations in uterine serous carcinoma by genome-wide analyses. J Natl Cancer Inst. 2012;104:1503–13.
Zhao S, Choi M, Overton JD, et al. Landscape of somatic single-nucleotide and copy-number mutations in uterine serous carcinoma. Proc Natl Acad Sci U S A. 2013;110:2916–21.
Jones NL, Xiu J, Reddy SK, et al. Identification of potential therapeutic targets by molecular profiling of 628 cases of uterine serous carcinoma. Gynecol Oncol. 2015;138:620–6.
Le Gallo M, O'Hara AJ, Rudd ML, et al. Exome sequencing of serous endometrial tumors identifies recurrent somatic mutations in chromatin-remodeling and ubiquitin ligase complex genes. Nat Genet. 2012;44:1310–5.
Pietsch EC, Sykes SM, McMahon SB, Murphy ME. The p53 family and programmed cell death. Oncogene. 2008;27:6507–21.
Harris CC. p53: at the crossroads of molecular carcinogenesis and risk assessment. Science. 1993;262:1980–1.
Zheng W, Cao P, Zheng M, Kramer EE, Godwin TA. p53 overexpression and bcl-2 persistence in endometrial carcinoma: comparison of papillary serous and endometrioid subtypes. Gynecol Oncol. 1996;61:167–74.
Zheng W, Khurana R, Farahmand S, et al. p53 immunostaining as a significant adjunct diagnostic method for uterine surface carcinoma: precursor of uterine papillary serous carcinoma. Am J Surg Pathol. 1998;22:1463–73.
Jia L, Liu Y, Yi X, et al. Endometrial glandular dysplasia with frequent p53 gene mutation: a genetic evidence supporting its precancer nature for endometrial serous carcinoma. Clin Cancer Res. 2008;14:2263–9.
Zhang X, Liang SX, Jia L, et al. Molecular identification of “latent precancers” for endometrial serous carcinoma in benign-appearing endometrium. Am J Pathol. 2009;174:2000–6.
Nagendra DC, Burke J 3rd, Maxwell GL, Risinger JI. PPP2R1A mutations are common in the serous type of endometrial cancer. Mol Carcinog. 2012;51:826–31.
McConechy MK, Anglesio MS, Kalloger SE, et al. Subtype-specific mutation of PPP2R1A in endometrial and ovarian carcinomas. J Pathol. 2011;223:567–73.
Haesen D, Abbasi Asbagh L, Derua R, et al. Recurrent PPP2R1A mutations in uterine cancer act through a dominant-negative mechanism to promote malignant cell growth. Cancer Res. 2016;76:5719–31.
Kuhn E, Bahadirli-Talbott A, Shih IM. Frequent CCNE1 amplification in endometrial intraepithelial carcinoma and uterine serous carcinoma. Mod Pathol. 2014;27:1014–9.
Cocco E, Lopez S, Black J, et al. Dual CCNE1/PIK3CA targeting is synergistic in CCNE1-amplified/PIK3CA-mutated uterine serous carcinomas in vitro and in vivo. Br J Cancer. 2016;115:303–11.
Nakayama K, Rahman MT, Rahman M, et al. CCNE1 amplification is associated with aggressive potential in endometrioid endometrial carcinomas. Int J Oncol. 2016;48:506–16.
von Wachenfeldt A, Lindblom A, Gronberg H, et al. A hypothesis-generating search for new genetic breast cancer syndromes-a national study in 803 Swedish families. Hered Cancer Clin Pract. 2007;5:17–24.
Liang S, Pearl M, Liang S, et al. Personal history of breast cancer as a significant risk factor for endometrial serous carcinoma in women </= 55 years Old. Int J Cancer. 2011;128(4):763–70.
Hornreich G, Beller U, Lavie O, et al. Is uterine serous papillary carcinoma a BRCA1-related disease? Case report and review of the literature. Gynecol Oncol. 1999;75:300–4.
Shu CA, Pike MC, Jotwani AR, et al. Uterine cancer after risk-reducing salpingo-oophorectomy without hysterectomy in women with BRCA mutations. JAMA Oncol. 2016;2:1434–40.
Holcomb K, Delatorre R, Pedemonte B, et al. E-cadherin expression in endometrioid, papillary serous, and clear cell carcinoma of the endometrium. Obstet Gynecol. 2002;100:1290–5.
Mell LK, Meyer JJ, Tretiakova M, et al. Prognostic significance of E-cadherin protein expression in pathological stage I-III endometrial cancer. Clin Cancer Res. 2004;10:5546–53.
Nofech-Mozes S, Khalifa MA, Ismiil N, et al. Immunophenotyping of serous carcinoma of the female genital tract. Mod Pathol. 2008;21:1147–55.
Sakuragi N, Nishiya M, Ikeda K, et al. Decreased E-cadherin expression in endometrial carcinoma is associated with tumor dedifferentiation and deep myometrial invasion. Gynecol Oncol. 1994;53:183–9.
Soslow RA, Shen PU, Isacson C, Chung MH. The CD44v6-negative phenotype in high-grade uterine carcinomas correlates with serous histologic subtype. Mod Pathol. 1998;11:194–9.
Zheng W, Schwartz PE. Serous EIC as an early form of uterine papillary serous carcinoma: recent progress in understanding its pathogenesis and current opinions regarding pathologic and clinical management. Gynecol Oncol. 2005;96:579–82.
Kupryjanczyk J, Thor AD, Beauchamp R, et al. Ovarian, peritoneal, and endometrial serous carcinoma: clonal origin of multifocal disease. Mod Pathol. 1996;9:166–73.
Baergen RN, Warren CD, Isacson C, Ellenson LH. Early uterine serous carcinoma: clonal origin of extrauterine disease. Int J Gynecol Pathol. 2001;20:214–9.
Black JD, Lopez S, Cocco E, et al. PIK3CA oncogenic mutations represent a major mechanism of resistance to trastuzumab in HER2/neu overexpressing uterine serous carcinomas. Br J Cancer. 2015;113:1641.
Lopez S, Cocco E, Black J, et al. Dual HER2/PIK3CA targeting overcomes single-agent acquired resistance in HER2-amplified uterine serous carcinoma cell lines in vitro and in vivo. Mol Cancer Ther. 2015;14:2519–26.
Reid-Nicholson M, Iyengar P, Hummer AJ, et al. Immunophenotypic diversity of endometrial adenocarcinomas: implications for differential diagnosis. Mod Pathol. 2006;19:1091–100.
Chiesa-Vottero AG, Malpica A, Deavers MT, et al. Immunohistochemical overexpression of p16 and p53 in uterine serous carcinoma and ovarian high-grade serous carcinoma. Int J Gynecol Pathol. 2007;26:328–33.
Santin AD, Zhan F, Cane S, et al. Gene expression fingerprint of uterine serous papillary carcinoma: identification of novel molecular markers for uterine serous cancer diagnosis and therapy. Br J Cancer. 2005;92:1561–73.
Maxwell GL, Chandramouli GV, Dainty L, et al. Microarray analysis of endometrial carcinomas and mixed mullerian tumors reveals distinct gene expression profiles associated with different histologic types of uterine cancer. Clin Cancer Res. 2005;11:4056–66.
Zheng W, Yi X, Fadare O, et al. The oncofetal protein IMP3: a novel biomarker for endometrial serous carcinoma. Am J Surg Pathol. 2008;32:304–15.
Jiang T, Chen N, Zhao F, et al. High levels of Nrf2 determine chemoresistance in Type II endometrial cancer. Cancer Res. 2010;70(13):5486–96.
Lax SF, Kurman RJ. A dualistic model for endometrial carcinogenesis based on immunohistochemical and molecular genetic analyses. Verh Dtsch Ges Pathol. 1997;81:228–32.
Sherman ME, Bitterman P, Rosenshein NB, Delgado G, Kurman RJ. Uterine serous carcinoma. A morphologically diverse neoplasm with unifying clinicopathologic features. Am J Surg Pathol. 1992;16:600–10.
Ambros RA, Sherman ME, Zahn CM, Bitterman P, Kurman RJ. Endometrial intraepithelial carcinoma: a distinctive lesion specifically associated with tumors displaying serous differentiation. Hum Pathol. 1995;26:1260–7.
Zheng W, Liang SX, Yu H, et al. Endometrial glandular dysplasia: a newly defined precursor lesion of uterine papillary serous carcinoma. Part I: morphologic features. Int J Surg Pathol. 2004;12:207–23.
Liang SX, Chambers SK, Cheng L, et al. Endometrial glandular dysplasia: a putative precursor lesion of uterine papillary serous carcinoma. Part II: molecular features. Int J Surg Pathol. 2004;12:319–31.
Wheeler DT, Bell KA, Kurman RJ, Sherman ME. Minimal uterine serous carcinoma: diagnosis and clinicopathologic correlation. Am J Surg Pathol. 2000;24:797–806.
Tashiro H, Isacson C, Levine R, et al. p53 gene mutations are common in uterine serous carcinoma and occur early in their pathogenesis. Am J Pathol. 1997;150:177–85.
Fadare O, Zheng W. Insights into endometrial serous carcinogenesis and progression. Int J Clin Exp Pathol. 2009;2:411–32.
Berman JJ, Albores-Saavedra J, Bostwick D, et al. Precancer: a conceptual working definition-results of a Consensus conference. Cancer Detect Prev. 2006;30:387–94.
Liang SX, Cheng L, Chambers SK, et al. Endometrial glandular dysplasia, a newly defined precursor lesion of uterine papillary serous carcinoma: Part II, molecular features. Int J Surg Pathol. 2004;12:319–31.
Zheng W, Liang SX, Yi X, et al. Occurrence of endometrial glandular dysplasia precedes uterine papillary serous carcinoma. Int J Gynecol Pathol. 2007;26:38–52.
Hoang LN, McConechy MK, Meng B, et al. Targeted mutation analysis of endometrial clear cell carcinoma. Histopathology. 2015;66:664–74.
Le Gallo M, Rudd ML, Urick ME, et al. Somatic mutation profiles of clear cell endometrial tumors revealed by whole exome and targeted gene sequencing. Cancer. 2017;123:3261–8.
DeLair DF, Burke KA, Selenica P, et al. The genetic landscape of endometrial clear cell carcinomas. J Pathol. 2017;243:230–41.
Zhao S, Bellone S, Lopez S, et al. Mutational landscape of uterine and ovarian carcinosarcomas implicates histone genes in epithelial-mesenchymal transition. Proc Natl Acad Sci U S A. 2016;113:12238–43.
Cherniack AD, Shen H, Walter V, et al. Integrated Molecular Characterization of Uterine Carcinosarcoma. Cancer Cell. 2017;31:411–23.
Garg K, Leitao MM Jr, Kauff ND, et al. Selection of endometrial carcinomas for DNA mismatch repair protein immunohistochemistry using patient age and tumor morphology enhances detection of mismatch repair abnormalities. Am J Surg Pathol. 2009;33:925–33.
Karnezis AN, Hoang LN, Coatham M, et al. Loss of switch/sucrose non-fermenting complex protein expression is associated with dedifferentiation in endometrial carcinomas. Mod Pathol. 2016;29:302–14.
Kobel M, Hoang LN, Tessier-Cloutier B, et al. Undifferentiated endometrial carcinomas show frequent loss of core switch/sucrose nonfermentable complex proteins. Am J Surg Pathol. 2018;42(1):76–83.
Rosa-Rosa JM, Leskela S, Cristobal-Lana E, et al. Molecular genetic heterogeneity in undifferentiated endometrial carcinomas. Mod Pathol. 2016;29:1594.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Science Press & Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Zheng, W., Fadare, O., Quick, C.M. (2019). Endometrial Carcinogenesis. In: Zheng, W., Fadare, O., Quick, C., Shen, D., Guo, D. (eds) Gynecologic and Obstetric Pathology, Volume 1. Springer, Singapore. https://doi.org/10.1007/978-981-13-3016-2_16
Download citation
DOI: https://doi.org/10.1007/978-981-13-3016-2_16
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-3015-5
Online ISBN: 978-981-13-3016-2
eBook Packages: MedicineMedicine (R0)