Abstract
A 1-year-old Japanese female patient with motor retardation was brought to our outpatient clinic by her mother. The child was found to have high serum creatine kinase (CK) level according to the 1-year-old medical checkup and was recommended further evaluation. The girl, the second child in her family, was born at full term in a local hospital and, after birth, was transferred to a general hospital because of muscle hypotonus, poor eye opening and sucking, and a high serum CK level (5461 IU/L: normal ranges are between 40 and 310 IU/L). She was followed up because her doctors considered these symptoms to arise from neonatal asphyxia. The infant developed quickly after 2 weeks, and her serum CK level decreased to normal. She grew up slightly slowly and acquired head control at 5 months of age (commonly acquired at 3–4 months after birth); she could not roll over at 7 months and rehabilitation was started. At 1 year of age, her muscle tonus remained decreased, and her serum CK level was elevated again (7532 IU/L). She could not stand up without support.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Case Report
A 1-year-old Japanese female patient with motor retardation was brought to our outpatient clinic by her mother. The child was found to have high serum creatine kinase (CK) level according to the 1-year-old medical checkup and was recommended further evaluation. The girl, the second child in her family, was born at full term in a local hospital and, after birth, was transferred to a general hospital because of muscle hypotonus, poor eye opening and sucking, and a high serum CK level (5461 IU/L: normal ranges are between 40 and 310 IU/L). She was followed up because her doctors considered these symptoms to arise from neonatal asphyxia. The infant developed quickly after 2 weeks, and her serum CK level decreased to normal. She grew up slightly slowly and acquired head control at 5 months of age (commonly acquired at 3–4 months after birth); she could not roll over at 7 months and rehabilitation was started. At 1 year of age, her muscle tonus remained decreased, and her serum CK level was elevated again (7532 IU/L). She could not stand up without support.
Physical examination revealed that the child could not fully raise her arms or sit for >10 s. She presented general hypotonia and depressed deep tendon reflex and joint contracture of both ankles, although her hip and knee joints still retained full range of movement. Laboratory studies revealed high levels of serum CK, lactate dehydrogenase, aspartate aminotransferase, and alanine aminotransferase. However, normal results were obtained in other laboratory tests, such as complete blood count and analyses of renal function and electrolytes. Results of Giemsa banding analysis, used for detecting chromosomal abnormality, were also normal. Brain MRI showed symmetrical unmyelinated changes in frontal white matter in T2-weighted images, and pachygyria was observed predominantly in frontotemporal lobes (Fig. 20.1). To identify the underlying genetic cause, commercially available genetic testing was performed.
The child was brought to our hospital every 6 months after definitive diagnosis . At age 18 months, she began uttering a few words without meaning, such as “Dah.” She could also roll over by herself and raise her arms fully. At age 2 years, she exhibited febrile seizures lasting several minutes when she was infected with roseola infantum. However, electroencephalography results were normal, and her seizures were considered typical febrile seizures that were unrelated to the disease. Echocardiography results were also normal in her 2-year-old medical checkup. At age 3 years, the child could speak two-word sentences such as “Where mom?;” such two-word sentences are commonly spoken starting at 2 years of age. She could move on her knees, but could not stand or walk unassisted. Overall, she grew up slower than normal infants in terms of motor function and intelligence and continuously presented elevated levels of serum CK.
2 Diagnosis
2.1 Approach to Diagnosis
Congenital muscle weakness is caused by diverse neuromuscular and connective tissue diseases (Table 20.1). The most critical consideration for diagnosis is the determination of the neuroanatomical location of the deficit, based on various medical histories and examinations. Motor deficit can be caused by diseases of the brain, spinal cord, peripheral nerve, neuromuscular junction, and muscle (Fig. 20.2). The most important examination here is for deep tendon reflexes: If the deep tendon reflex is depressed, the responsible lesion can be narrowed down to being below the spinal cord (peripheral nerve, neuromuscular junction, or muscle). For differentiating between the diseases in adults, the crucial analyses are electromyography (EMG) and nerve conduction study. However, EMG studies cannot be readily used for neonates and infants because they cannot move in response to the doctor’s instructions. In such cases, marked elevation of CK levels suggests muscle diseases (myopathies) such as muscular dystrophies.
Myopathies can be divided into two major categories: inherited and acquired. Acquired myopathies are further classified by etiology into, for example, inflammatory myopathies, infectious myopathies, toxic myopathies, and myopathies associated with systemic diseases. Conversely, inherited myopathies are classified into muscular dystrophies, congenital myopathies, metabolic myopathies, and mitochondrial myopathies. Most cases of infant myopathies are inherited, particularly congenital myotonic dystrophy and congenital myopathies, and these myopathies cannot be differentiated through EMG studies and routine laboratory testing. Certain myopathies present characteristic symptoms, such as a high-arched palate in congenital myopathies, but these are not definitive symptoms. Genetic testing and/or muscle biopsies are frequently necessary for definitive diagnosis, and electroencephalography and neuroimaging are also useful for diagnosis. The recent, unprecedented progress made in molecular-genetic, ultrastructural, and biochemical studies on myopathies, especially muscular dystrophies, has revealed the mechanisms underlying these diseases and provided diagnostic tools. In the case reported here, a combination of motor deficits resulting from muscle involvement and brain malformation strongly suggested Fukuyama congenital muscular dystrophy (FCMD).
2.2 Epidemiology of FCMD
Muscular dystrophy represents a group of genetic disorders that cause progressive weakness and loss of muscle volume. FCMD is an autosomal recessive muscular dystrophy and is the most common childhood muscular dystrophy after Duchenne muscular dystrophy (DMD) in Japan. FCMD, which was first characterized by Dr. Yukio Fukuyama, is caused by mutation in the gene fukutin (FKTN) . The disease incidence is ~3/100,000, and one person in approximately 90 is expected to be a heterozygous carrier. A few cases of muscular dystrophy patients harboring fukutin mutations have also been reported from countries other than Japan.
2.3 Physical Symptoms and Signs
FCMD is characterized by severe congenital muscular dystrophy (CMD), abnormal neuronal migration associated with mental retardation and epilepsy, and frequent eye abnormalities (Fukuyama et al. 1981). Patients with FCMD manifest muscle weakness and hypotonia by early infancy (floppy infant). In approximately half of the cases, poor sucking and weak crying are documented during the neonatal period. The infants also present motor development delay, which is why parents bring them to the clinic. Most FCMD patients can remain sitting by the age of 2 years, but they rarely show the ability to remain standing or walking unassisted. They also present pseudohypertrophy in the calves by early childhood. Joint contractures are not detected at birth, but most patients reveal hip, knee, and ankle contracture before they are 1 year old. Myopathic face resulting from facial muscle involvement gradually strengthens, and a tendency for the mouth to remain open persists from infancy onward. FCMD patients who live more than 10 years tend to develop slowly progressive myocardial involvements, including fibrosis of the myocardium, which finally result in cardiac failure.
Brain structural defects—such as brain malformations characterized by micropolygyria of the cerebrum and cerebellum, type II lissencephaly (cobblestone lissencephaly), and cerebellar cysts—are associated with FCMD. Mental retardation is also a characteristic of FCMD patients, whose IQ scores range between 30 and 50. Few patients speak only two-word sentences (such as “Mom come”) throughout life. Seizures occur in nearly 70% of the cases, and eye abnormalities also occur, including myopia, cataract, abnormal eye movement, pale optic disc, and retinal detachment. Thus, FCMD is a genetic disorder that includes the involvement of the muscle, eye, and brain. Most patients do not develop the ability to work, and they die by the age of 20 years.
2.4 Laboratory Findings
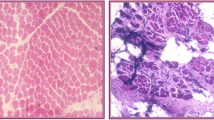
Serum CK levels of FCMD patients are elevated >tenfold above normal, which means that muscle tissue is being destroyed in these patients. The levels of aspartate aminotransferase, alanine aminotransferase, and lactate dehydrogenase also increase together with marked CK elevation, because these enzymes are present in not only hepatocytes but also skeletal muscle tissue. The results of muscle imaging, such as MRI , ultrasound imaging, and CT scanning, frequently show signal abnormalities due to fatty infiltration, which follows the muscle destruction. These imaging studies also help in identifying the muscle that is optimal for biopsy, and muscle biopsies reveal myopathic changes suggesting muscular dystrophy, including necrotic and regenerating processes, fibrosis, central nuclei, and variation in fiber size. However, given the development of molecular-genetic testing, muscle biopsy is no longer necessary for FCMD diagnosis. Furthermore, brain MRI reveals brain malformations , which include polymicrogyria, pachygyria, and agyria of the cerebrum and cerebellum. T2-weighted high intensity in the white matter, absence of the corpus callosum, and hypoplasia of the pons are also observed. The major mutation in FCMD is a 3-kb SINE-VNTR-Alu (SVA) retrotransposal insertion into the 3′-UTR of fukutin in Japanese patients (described in detail in the following section) (Fig. 20.3). PCR-based molecular-genetic testing for the presence of this mutation is frequently performed for the molecular diagnosis of FCMD (Watanabe et al. 2005). The results of this genetic test revealed that our patient carried a homozygous retrotransposon insertion.
3 Biochemical and Molecular Perspectives
3.1 Identification of Fukutin, the Gene Responsible for FCMD
The causative gene for FCMD was identified through positional cloning by Toda and colleagues and named fukutin (Kobayashi et al. 1998). Fukutin, a 461-amino-acid protein, contains a hydrophobic transmembrane region followed by a stem region and a putative catalytic domain. Fukutin also contains a conserved DxD motif that is present in several glycosyltransferases. Bioinformatic analysis has revealed that fukutin shows sequence similarities to bacterial proteins involved in polysaccharide/phosphorylcholine modification and to a yeast protein involved in mannosyl phosphorylation of oligosaccharides; however, the activity of fukutin long remained unidentified.
The major mutation in FCMD was identified as a 3-kb SVA retrotransposon insertion in the 3′ noncoding region of fukutin, which accounts for ~87% of the FCMD chromosome (Kobayashi et al. 1998). FCMD is the first human disease identified to be caused by an ancient retrotransposal integration. The retrotransposal insertion leads to abnormal splicing through exon trapping, which results in aberrant mRNA splicing (Taniguchi-Ikeda et al. 2011). A rare alternative donor site in exon 10 is activated and trapped by an alternative acceptor site in the SVA retrotransposon, creating an additional and aberrant exonic sequence (exon 11); the abnormal splicing excises the authentic stop codon and produces another stop codon located in exon 11 (Fig. 20.3). The resulting product truncates the fukutin C-terminus and adds 129 amino acids encoded by the SVA retrotransposon .
According to genetic calculation, the FCMD founder retrotransposal mutation was introduced into the Japanese population 100 generations ago, i.e., the founder lived approximately 2000–2500 years ago. This was the period during which the Yayoi people migrated from Korea and China and intermingled with the indigenous Jomon population, generating the modern Japanese people. Other mutations in fukutin, such as frameshift, nonsense, and missense mutations, have been also reported. Patients harboring compound heterozygous SVA insertion and other pathological mutations frequently develop more severe or milder phenotypes than other FCMD patients depending on the deleterious effects of the mutations. Non-Japanese FCMD patients carry either homozygous or heterozygous mutations other than the founder SVA insertion.
3.2 Abnormal Glycosylation in FCMD
In 2001, Hayashi and colleagues reported that staining by the monoclonal antibody IIH6, which recognizes glycosylated α-dystroglycan (α-DG), is decreased in FCMD biopsies (Hayashi et al. 2001). Subsequently, the Campbell group reported similar abnormal glycosylation in patients with muscle-eye-brain disease (MEB) and Walker-Warburg syndrome (WWS) and showed that the abnormal glycosylation leads to a loss of the ligand-binding activity of α-DG (Michele et al. 2002). The abnormal glycosylation of α-DG was also later reported in patients with CMD and limb-girdle muscular dystrophy (LGMD). These discoveries established a newly recognized disease entity, muscular dystrophy caused by abnormal glycosylation of α-DG, referred to as dystroglycanopathy (DGpathy) . As described in the following sections, 18 genes are currently recognized as DGpathy causative genes. Although DGpathies are biochemically characterized by abnormal glycosylation of α-DG and are clinically associated with severe CMD and brain abnormalities, a considerable number of patients exhibit abnormal glycosylation of α-DG but show only mild muscular dystrophy without brain malformations . Numerous studies on the genotype-phenotype correlation within large cohorts of DGpathy patients have confirmed that a wide clinical spectrum is associated with mutations in specific causative genes. The most severe end of the spectrum is characterized by CMD with extensive structural abnormality in the brain and eye, which typically results in early infantile death. Conversely, patients at the mildest end of the spectrum might present in adult life with LGMD without brain or eye involvement.
In 2007, Muntoni and colleagues proposed a clinical classification system comprising seven broad phenotypic categories (Godfrey et al. 2007). DGpathy was first categorized into four groups: (a) WWS/WWS-like , (b) MEB/FCMD-like , (c) CMD, and (d) LGMD. Categories (c) and (d) were further classified into these subgroups: (c-1) CMD with mental retardation and cerebellar involvement as the only structural brain abnormality, (c-2) CMD with mental retardation and a structurally normal brain, (c-3) CMD with no abnormal cognitive development , (d-1) LGMD with mental retardation , and (d-2) LGMD without mental retardation. Later, new Online Mendelian Inheritance in Man (OMIM) entries created a simplified classification scheme for DGpathy (MDDG, muscular dystrophy-dystroglycanopathy ) by combining three broad phenotypic groups and gene defects (Godfrey et al. 2011). First, DGpathy was divided into three groups: (A) CMD with brain/eye abnormalities, (B) CMD with milder brain structural abnormalities, and (C) LGMD. Second, the causative gene was indicated numerically; for example, POMT1 is “1” and fukutin is “4.” According to this classification , typical FCMD is named “MDDG type A4.”
3.3 DG
DG was originally identified from skeletal muscle as a component of the dystrophin-glycoprotein complex (DGC). Mutations in dystrophin cause Duchenne and Becker muscular dystrophies, the most frequently occurring muscular dystrophies worldwide. The DGC forms a structural linkage between the basement membrane and the actin cytoskeleton , and this provides physical strength to the skeletal muscle cell membrane. Within the DGC, DG functions as a central axis by anchoring dystrophin beneath the cell membrane and binding to basement membrane proteins (such as laminin) on the cell exterior (Fig. 20.4). DG is composed of α and β subunits, both of which are expressed from a single mRNA and cleaved into α-DG and β-DG during posttranslational modification. α-DG is a highly glycosylated extracellular protein, and it functions as a ligand-binding subunit that interacts with several ligand proteins, which commonly contain laminin G-like (LG) domains. The ligands known to bind to α-DG include laminins, perlecan, agrin, neurexin, and pikachurin. β-DG is a transmembrane subunit that anchors α-DG on the cell surface and binds to dystrophin intracellularly. α-DG consists of three domains: two globular domains at the N- and C-termini and a mucin-like domain between them. The mucin-like domain contains >40 Ser/Thr residues that form O-glycan clusters. The N-terminal globular domain is essential for producing O-glycosylation in the mucin-like domain; however, the N-terminal domain is cleaved and shed from the α-DG core portion after the completion of glycosylation and therefore is not present in mature α-DG.
Schematic representation of the dystrophin-glycoprotein complex (DGC). DGC links the basement membrane to the cytoskeleton (left). DG functions as the cellular receptor for matrix proteins, and the sugar chains on α-DG are essential for ligand binding. Abnormally glycosylated α-DG loses the ligand-binding activities and is associated with DGpathy (right)
3.4 Sugar-Chain Structure of α-DG and Its Biosynthetic Enzymes
In the early 2000s, in addition to fukutin, several genes were identified whose mutations cause abnormal glycosylation of α-DG: POMT1, POMT2, POMGNT1, fukutin-related protein (FKRP) , and LARGE. The genes have been identified as causative genes for WWS , MEB , CMD, or LGMD (MDC1C and LGMD2I). After 2012, additional genes responsible for DGpathy were identified, and as of 2017, the list includes 18 genes (Table 20.2). Currently, DGpathies can be classified as primary DGpathies (affecting the DG gene directly), secondary DGpathies (affecting genes that directly modify DG), and tertiary DGpathies (caused by mutations in genes that indirectly affect DG function). As the DGpathy genes were identified, the sugar-chain structure of α-DG was revealed in a stepwise manner. In this chapter, we introduce the sugar-chain structure of α-DG and the enzymes involved in its biosynthesis.
-
1.
CoreM1
In 1997, Endo and colleagues identified a unique O-mannose (O-Man)-type glycan from bovine peripheral nerve α-DG (Gal-GlcNAc-Man-O). This structure was later named CoreM1 (Fig. 20.5). CoreM1 is the first O-Man-type glycan identified in mammals. The initial Man transfer to the Thr/Ser residues of α-DG is catalyzed by a POMT1/POMT2 (protein O-mannosyl transferase 1/2) heterocomplex, which uses dolichol-phosphate-mannose (Dol-P-Man) as the Man donor substrate (Manya et al. 2004). The GlcNAcβ1-2Man linkage is synthesized by POMGnT1, which transfers GlcNAc from a UDP-GlcNAc to O-Man (Yoshida et al. 2001). CoreM1 was originally considered a ligand-binding moiety; however, enzymatic removal of Gal and GlcNAc from CoreM1 does not affect the ligand-binding activity of the protein. Conversely, disruption of CoreM1 biosynthesis in either human (POMGnT1-mutant-carrying patients) or mouse (POMGnT1-deficient mice) results in loss of ligand-binding activity of α-DG, which indicates that CoreM1 plays a critical role in the functional maturation of α-DG.
-
2.
CoreM3
In 2010, Campbell and colleagues identified another type of O-Man glycan in recombinant α-DG expressed in HEK293 cells (GalNAc-GlcNAc-Man-O), which was later named CoreM3 (Fig. 20.5). CoreM3 serves as a scaffold for the building of the ligand-binding moiety on the core protein of α-DG (as described below) (Yoshida-Moriguchi et al. 2013; Yoshida-Moriguchi and Campbell 2015). The initial Man transfer is catalyzed by the enzymatic action of the POMT1/POMT2 complex as in the case of CoreM1. The GlcNAcβ1-4Man linkage is synthesized by POMGnT2, which transfers GlcNAc from a UDP-GlcNAc. The GalNAcβ1-3GlcNAc linkage is synthesized by B3GalNT2, which transfers GalNAc from a UDP-GalNAc. The O-Man residue in CoreM3 is phosphorylated at the 6 position, and the phosphate group is added from ATP by protein O-mannose kinase (POMK). The physiological role of this phosphorylation is unknown, but it is likely required for subsequent modification of CoreM3 with the ribitol phosphate group (see below).
-
3.
Matriglycan (LARGE-glycan)
The overexpression of LARGE, whose mutations were identified in MDC1D patients and in the spontaneous mutant Large myd mouse, increases the glycosylation and ligand-binding activities of α-DG. This unique feature suggested that LARGE is involved in the biosynthesis of the ligand-binding moiety of α-DG. In 2012, LARGE was identified to possess two glycosyltransferase activities, α3-xylosyltransferase and β3-glucuronyltransferase activities, which generate the [−3GlcAβ1-3Xylα1] (GlcA-Xyl) repeat from UDP-Xyl and UDP-GlcA (Inamori et al. 2012). Enzymatically synthesized [−3GlcAβ1-3Xylα1] repeats interact with laminin and are recognized by IIH6 antibody, and therefore the repeat structure serves as the ligand-binding motif of α-DG and is named “matriglycan” (Fig. 20.5). A recent crystal structure analysis revealed the atomic details of DG-ligand binding. A single GlcA-Xyl disaccharide straddles a Ca2+ ion in the LG4 domain of laminin α2 (Briggs et al. 2016). This chelating binding mode explains the high affinity of this protein-carbohydrate interaction. Moreover, multiple GlcA-Xyl repeats are predicted to increase the apparent affinity for the LG domains present in ligand proteins by favoring rapid rebinding after dissociation. Accordingly, long repeats (>13) effectively bind to laminins, although the number of repeats present in a single matriglycan remains unknown.
For the initiation of matriglycan formation, an acceptor primer structure, GlcAβ1-4Xyl, is necessary. This structure is synthesized by B4GAT1, previously known as β3GnT1, which exhibits β4-glucuronyltransferase activity by using a donor UDP-GlcA to form the GlcAβ1-4Xyl linkage that can be elongated by LARGE with matriglycan (Yoshida-Moriguchi and Campbell 2015). For the matriglycan modification, in addition to the LARGE enzyme activities and the acceptor primer structure, physical interaction between LARGE and the α-DG N-terminal domain is required (Kanagawa et al. 2004). Thus, the N-terminal domain serves as a recognition motif for LARGE, thereby providing substrate specificity for this unique modification. A mutation in the N-terminal domain of α-DG was identified in a patient with LGMD with cognitive impairment, and the mutation reduced LARGE recognition and therefore resulted in diminished LARGE-dependent matriglycan modification (Hara et al. 2011). This was the first case in which a mutation in the DG gene (DAG1) itself was shown to cause muscular dystrophy (“primary” DGpathy).
-
4.
Tandem ribitol phosphate
In 2016, Toda and colleagues showed the presence of novel moiety between matriglycan and CoreM3 by mass spectrometry analysis (Kanagawa et al. 2016). The moiety contains a GlcA-Xyl disaccharide and a tandem ribitol 5-phosphate (RboP) (Fig. 20.5). Whereas the GlcA-Xyl disaccharide serves the acceptor primer for LARGE, the tandem RboP links the primer GlcA-Xyl to the GalNAc residue in CoreM3. Ribitol is a sugar alcohol that was not known to be used in mammals before this finding, whereas RboP was initially recognized as a component of the teichoic acids present in bacterial cell walls. In bacteria, the RboP polymer is synthesized by enzymes that use CDP-Rbo as a donor substrate, and CDP-Rbo is synthesized by the enzyme TarI from cytidine triphosphate (CTP) and RboP. TarI shares homology with a DGpathy protein, isoprenoid synthase domain containing (ISPD), and, notably, ISPD was shown to possess CDP-Rbo synthase activity. Subsequently, the tandem RboP structure was shown to be synthesized through the sequential enzymatic actions of fukutin and FKRP : Fukutin transfers RboP from a CDP-Rbo to GalNAc in CoreM3, and then FKRP transfers RboP from a CDP-Rbo to the first RboP. Missense mutations found in DGpathy patients carrying mutant fukutin or FKRP reduced the RboP transferase activities. NMR analysis revealed the anomeric conformation to be Rbo5P-1Rbo5P-3GalNAc. Lastly, TMEM5 was shown to exhibit Xyl transferase activity by using UDP-Xyl as a donor substrate and to form a Xylβ1-4Rbo5P linkage that connects matriglycan and the tandem Rbo5P (Manya et al. 2016). This Xyl residue is a part of the acceptor primer for matriglycan formation. TMEM5 was recently renamed RXYLT1 on the basis of its function (Rbo5P β1,4-Xyl transferase).
-
5.
Dol-P-Man synthesis pathway
As mentioned above while describing CoreM1, the initial Man transfer to the Thr/Ser residues in α-DG requires the POMT1/POMT2 enzyme complex and its donor substrate Dol-P-Man. Thus, defects in the Dol-P-Man biosynthesis pathway can result in abnormal O-mannosylation of α-DG, and, accordingly, mutations in certain proteins involved in this pathway cause DGpathies (Table 20.2). The synthesis of Dol-P-Man from GDP-Man and dolichol phosphate is catalyzed by the DPM synthase complex, which consists of the catalytic component DPM1 and the ER-localized transmembrane proteins DPM2 and DPM3. Dolichol kinase (DOLK) is responsible for the formation of dolichol phosphate. GDP-mannose pyrophosphorylase B (GMPPB) is the β-subunit of the essential enzyme GDP-mannose pyrophosphorylase, which catalyzes the formation of GDP-mannose from mannose-1-phosphate and GTP. Consequently, mutations in DOLK or GMPPB could result in a decrease in Dol-P-Man levels.
Dol-P-Man also acts as a Man donor in N-glycosylation and in glycophosphatidylinositol-anchor biosynthesis. Therefore, defects in the Dol-P-Man pathway affect these modifications and are associated with human diseases. Congenital disorder of glycosylation (CDG) is a heterogeneous group of rare genetic disorders that were originally defined as diseases caused by defects in the N-glycosylation process, and CDG has now been reclassified to include O-linked and lipid glycosylation defects. Notably, mutations in DPM1, DPM2, or DPM3 have been identified in patients presenting DGpathy with type I CDG, and mutations in DOLK have been discovered in patients with CDG and dilated cardiomyopathy , whose heart tissue showed abnormal O-mannosylation of α-DG. Overall, mutations in the genes introduced in this section and in ISPD indirectly affect α-DG function; thus, the diseases caused by these gene mutations are categorized as tertiary DGpathies.
4 Therapy
4.1 Cellular Pathogenesis of FCMD
Studies conducted using genetically modified disease-model animals have contributed substantially to our understanding of the molecular and cellular pathogenesis of single-gene disorders. Here, we introduce the DGpathy cellular pathogenesis revealed by studies performed using fukutin-deficient FCMD model animals. Because embryonic lethality was exhibited by fukutin or DG gene-knockout mice that were generated through targeted disruption of fktn or dag1, respectively, several lines of tissue-selective conditional knockout (cKO) mice have been generated for disrupting the expression of fktn or dag1. In DGpathy, the loss of ligand-binding activity of α-DG due to abnormal glycosylation leads to a disruption of the linkage between the basement membrane and the cytoskeleton. Accordingly, ultrastructural abnormality, in which the basement membrane was detached from the muscle cell membrane, was detected in the skeletal muscle of both myofiber-selective DG-deficient mice and mice that were spontaneously Large-defective, the Large myd DGpathy mice. These structural abnormalities render muscles prone to contraction-induced injuries, eventually leading to the necrosis of muscle cells. Membrane fragility that triggers disease manifestation is also observed in myofiber-selective fukutin cKO mice ; however, mice with myofiber-selective loss of DG or fukutin exhibit only mild muscular dystrophy, which indicates that membrane fragility is not sufficient for explaining the severe muscle pathology of DGpathy.
Myofiber damage leads to the activation of satellite cells, which are muscle-specific stem cells; activated satellite cells differentiate into muscle precursor cells (MPCs) and then into myoblasts, which eventually fuse into myotubes. Thus, through this process, skeletal muscle can undergo regeneration. MPC-selective fukutin-cKO mice show severe muscular dystrophy with reductions in the number of satellite cells, MPC proliferation/differentiation activities, and muscle regeneration activity (Kanagawa et al. 2013). The severity of these abnormalities increases as the disease progresses. Therefore, α-DG plays critical roles in the maintenance of satellite cell viability and MPC activities, and defects in the functions of these cells correlate with disease severity. Moreover, the absence of α-DG glycosylation during postnatal/juvenile muscle growth and development has been proposed to potentially affect muscle degeneration and/or dystrophic pathology in later stages. In FCMD and Large myd mice, neuromuscular junction formation is aberrant and numerous immature muscle fibers are present, and this suggests that impaired differentiation signals from the aberrant neuromuscular junctions and the maturational delay in muscle fibers underlie the etiology of DGpathy. Thus, in addition to muscle membrane fragility, muscle maturation and regeneration processes appear to be involved in the pathogenesis of DGpathy.
Abnormal glycosylation of α-DG is also regarded as one of the main causes of brain malformation , characterized by polymicrogyria. The surface of the cerebral cortex is covered by the glia-limitans/basement-membrane complex, which prevents the overmigration of neurons . In FCMD and other DGpathy models, breakdown of the basement membrane leads to a protrusion of neurons into the subarachnoid space where the basement membrane breaches are observed. These abnormalities are possibly the underlying causes of cortical dysplasia and type II lissencephaly (Michele et al. 2002). α-DG is expressed in radial glia and presumably plays a role in physically connecting the glia limitans to the basement membrane. During the developmental growth of the embryonic brain, abnormally glycosylated α-DG might be incapable of maintaining sufficient physical strength and/or plasticity of the glia-limitans/basement-membrane complex against an expanding cortical surface area. Intriguingly, neuron-selective DG cKO and Large myd mice show impairment of long-term potentiation at CA3–CA1 synapses. DG is known to be expressed at the postsynaptic apparatus, but the precise mechanism that mediates the impairment of synaptic plasticity remains to be elucidated.
4.2 Therapeutic Strategies
Effective therapies for FCMD or DGpathies have not yet been established. However, because the molecular basis of FCMD and related DGpathies has been clarified, effective clinical treatments should be developed in the future. Conversely, at the laboratory level, several therapeutic strategies have been proposed. Gene replacement is one of the most rational strategies for DGpathies because these are single-gene disorders. Supporting this view, adeno-associated virus vector-mediated fukutin delivery results in improvement of the disease pathology in fukutin-deficient model mice (Kanagawa et al. 2013). Here, we introduce innovative treatment strategies based on the molecular pathogenesis of FCMD and DGpathy with RboP deficiency.
Most FCMD patients carry the founder SVA retrotransposal insertion in the 3′-UTR of fukutin. This insertion contains a strong splice acceptor site, which induces a rare alternative donor site in the final exon, thus causing abnormal mRNA splicing (exon trapping) (Taniguchi-Ikeda et al. 2011). Notably, introduction of antisense oligonucleotides that target the splice acceptor, the predicted exonic splicing enhancer, and the intronic splicing enhancer prevented the pathogenic exon trapping by SVA in the cells of FCMD patients and model mice. This resulted in the rescue of normal fukutin mRNA expression and protein production and, consequently, the restoration of α-DG glycosylation and laminin-binding activity. This treatment strategy can potentially be applied to almost all FCMD patients in Japan and can therefore be the first radical clinical treatment for DGpathies.
As described in the previous section, CDP-Rbo is an essential donor substrate for fukutin and FKRP to build the tandem RboP structure. Thus, reduction or loss of cellular CDP-Rbo due to ISPD mutations impairs RboP modifications, and this results in a failure of functional glycan synthesis on α-DG. These abnormalities directly underlie the molecular pathology of ISPD-deficient-type DGpathy. In ISPD-deficient cells, CDP-Rbo supplementation was shown to rescue RboP modification of α-DG. Although the details of the biosynthetic pathway of Rbo5P, an essential metabolite required for ISPD-dependent CDP-Rbo synthesis, remain incompletely elucidated, potential pathways for Rbo5P synthesis have been proposed (Gerin et al. 2016). Addition of D-ribose or ribitol, which are candidate metabolites in these pathways, led to an increase in CDP-Rbo levels in cells overexpressing ISPD, and ribitol supplementation in drinking water led to an increase in muscle CDP-Rbo levels in wild-type mice. These data suggest that supplementation of D-ribose or ribitol might effectively increase cellular Rbo5P level and might also enhance CDP-Rbo synthase activity of disease-causing mutant ISPD proteins that exhibit reduced affinity for the substrate Rbo5P. Further studies involving the use of animal models will be necessary for developing CDP-ribitol or metabolite supplementation therapy.
End-of-Chapter Questions
-
1.
Immunostaining performed on a patient’s biopsy samples indicates abnormal glycosylation of α-DG. Clinical manifestation also suggests that the patient suffers from DGpathy. However, whole-exon sequencing of the 18 recognized DGpathy genes indicates no mutations in these genes. Why do you suspect that the patient has DGpathy?
-
2.
Discuss the advantages of investigating the effects of disease-causing mutations in ISPD, fukutin, and FKRP on the activity of the encoded enzymes when considering therapy.
-
3.
The major mutation in FCMD is a retrotransposon insertion in the gene fukutin, which accounts for ~87% of the FCMD chromosome. This is considered to be due to the founder effect. Discuss other examples of genetic disorders associated with the founder effect.
References
Briggs DC, Yoshida-Moriguchi T, Zheng T et al (2016) Structural basis of laminin binding to the LARGE glycans on dystroglycan. Nat Chem Biol 12:810–814
Fukuyama Y, Osawa M, Suzuki H (1981) Congenital progressive muscular dystrophy of the Fukuyama type – clinical, genetic and pathological considerations. Brain and Development 3:1–29
Gerin I, Ury B, Breloy I et al (2016) ISPD produces CDP-ribitol used by FKTN and FKRP to transfer ribitol phosphate onto α-dystroglycan. Nat Commun 7:11534
Godfrey C, Clement E, Mein R et al (2007) Refining genotype–phenotype correlations in muscular dystrophies with defective glycosylation of dystroglycan. Brain 130:2725–2735
Godfrey C, Foley AR, Clement E et al (2011) Dystroglycanopathies: coming into focus. Curr Opin Genet Dev 21:278–285
Hara Y, Balci-Hayta B, Yoshida-Moriguchi T et al (2011) A dystroglycan mutation associated with limb-girdle muscular dystrophy. N Engl J Med 364:939–946
Hayashi YK, Ogawa M, Tagawa K et al (2001) Selective deficiency of α-dystroglycan in Fukuyama-type congenital muscular dystrophy. Neurology 57:115–121
Inamori K, Yoshida-Moriguchi T, Hara Y et al (2012) Dystroglycan function requires xylosyl- and glucuronyltransferase activities of LARGE. Science 335:93–96
Kanagawa M, Saito F, Kunz S et al (2004) Molecular recognition by LARGE is essential for expression of functional dystroglycan. Cell 117:953–964
Kanagawa M, Yu CC, Ito C et al (2013) Impaired viability of muscle precursor cells in muscular dystrophy with glycosylation defects and amelioration of its severe phenotype by limited gene expression. Hum Mol Genet 22:3003–3015
Kanagawa M, Kobayashi K, Tajiri M et al (2016) Identification of a post-translational modification with ribitol-phosphate and its defect in muscular dystrophy. Cell Rep 14:2209–2223
Kobayashi K, Nakahori Y, Miyake M et al (1998) An ancient retrotransposal insertion causes Fukuyama-type congenital muscular dystrophy. Nature 394:388–392
Manya H, Chiba A, Yoshida A et al (2004) Demonstration of mammalian protein O-mannosyltransferase activity: coexpression of POMT1 and POMT2 required for enzymatic activity. Proc Natl Acad Sci U S A 101:500–505
Manya H, Yamaguchi Y, Kanagawa M et al (2016) The muscular dystrophy gene TMEM5 encodes a ribitol β1,4-xylosyltransferase required for the functional glycosylation of dystroglycan. J Biol Chem 291:24618–24627
Michele DE, Barresi R, Kanagawa M et al (2002) Post-translational disruption of dystroglycan-ligand interactions in congenital muscular dystrophies. Nature 418:417–422
Taniguchi-Ikeda M, Kobayashi K, Kanagawa M et al (2011) Pathogenic exon-trapping by SVA retrotransposon and rescue in Fukuyama muscular dystrophy. Nature 478:127–131
Watanabe M, Kobayashi K, Jin F et al (2005) Founder SVA retrotransposal insertion in Fukuyama-type congenital muscular dystrophy and its origin in Japanese and Northeast Asian populations. Am J Med Genet 138A:344–348
Yoshida A, Kobayashi K, Manya H et al (2001) Muscular dystrophy and neuronal migration disorder caused by mutations in a glycosyltransferase, POMGnT1. Dev Cell 1:717–724
Yoshida-Moriguchi T, Campbell KP (2015) Matriglycan: a novel polysaccharide that links dystroglycan to the basement membrane. Glycobiology 25:702–713
Yoshida-Moriguchi T, Willer T, Anderson ME et al (2013) SGK196 is a glycosylation-specific O-mannose kinase required for dystroglycan function. Science 341:896–899
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kanagawa, M., Tokuoka, H., Toda, T. (2019). Fukuyama Congenital Muscular Dystrophy and Related Diseases. In: Oohashi, T., Tsukahara, H., Ramirez, F., Barber, C., Otsuka, F. (eds) Human Pathobiochemistry. Springer, Singapore. https://doi.org/10.1007/978-981-13-2977-7_20
Download citation
DOI: https://doi.org/10.1007/978-981-13-2977-7_20
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-2976-0
Online ISBN: 978-981-13-2977-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)