Abstract
I (Xiaofeng Liang) graduated from the Public Health Department, Shanxi Medical College University, in 1984 and was assigned to the Department of Epidemic Prevention, Gansu Provincial Health Bureau. My responsibility was for tuberculosis control and for managing the immunization program. It was from that time forward that I was bound inextricably with vaccination. It was also the beginning of my understanding that measles, polio, and other infectious diseases could be controlled by vaccination and that vaccination was critically important to the health of children.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
I (Xiaofeng Liang) graduated from the Public Health Department, Shanxi Medical College University, in 1984 and was assigned to the Department of Epidemic Prevention, Gansu Provincial Health Bureau. My responsibility was for tuberculosis control and for managing the immunization program. It was from that time forward that I was bound inextricably with vaccination. It was also the beginning of my understanding that measles, polio, and other infectious diseases could be controlled by vaccination and that vaccination was critically important to the health of children.
In the 1980s, polio, measles, and other vaccine-preventable diseases were prevalent in rural China; reducing the incidence of and mortality from these infectious diseases was a priority for protecting health and preventing epidemics. Most of the Health and Epidemic Prevention Stations (EPS) had not yet established a special department of the Expanded Program on Immunization (EPI), even though more and more people were engaged in the work of immunization. With China’s reform and opening-up policies, international organizations and friendly countries began to support China on immunization, and terms like “immunization” and “cold chain” were gradually coming into common use in professional departments and the medical community. I was involved in immunization activities, and the work was new to me. I eagerly anticipated the work and planned to devote myself fully to immunization!
1.1 Vaccination Before the 1970s
After becoming responsible for immunization, I often consulted experts in the Department of Epidemic Prevention and the Provincial EPS to better understand the history of vaccination. Director Chuanzhen Zhang and Vice Director Mingguang Tian helped me very much, and Director Guangxun Wang and Vice Director Zengrong Liu of the EPI Department in Gansu province EPS worked with me almost every day. They told me that in the early days of New China, infectious diseases, such as smallpox, were very serious and difficult to control. For example, with limited production capacity and supply of smallpox vaccine, the incidence and mortality rates of smallpox were very high among children. Fortunately, the new government placed prevention and control of infectious diseases in a very important position. On October 7, 1950, the Government Administration Council issued “Guidelines for Smallpox Vaccination Campaigns in Autumn” [1], which required implementation of a nationwide, free smallpox vaccination campaign. The campaign ultimately achieved coverage levels greater than 90% in most regions, with more than 500 million people vaccinated against smallpox in China between 1949 and 1952. As a result of this campaign, the incidence of smallpox decreased greatly – from 43,286 cases in 1950 to 847 in 1954. Smallpox was eradicated in China by 1961 – just 7 years later.
The Ministry of Health (MoH) established a BCG Promotion Committee at about the same time, with a charge to implement BCG vaccination to prevent serious tuberculosis. Annual vaccination during winter and spring against cholera, plague, typhus, typhoid, diphtheria, Japanese encephalitis, and pertussis was also implemented in some high-risk areas, effectively controlling epidemics of these infectious diseases. MoH issued a “Manual for Implementation of Vaccination” [1] for the first time in 1963 – the year I was born – and vaccination was gradually incorporated into the planned immunization program in each region, especially in urban areas. Universal children immunization was gradually improving.
The EPS system was abnormal during the “Cultural Revolution” period of 1965–1975. Health technical personnel were seriously depleted, and no one was responsible for the vaccination; management became poor, vaccination was sometimes disrupted, and immunization lagged. As a result, several infectious diseases that had previously been controlled re-emerged. Meningococcal meningitis was widely transmitted in the spring of 1967 due to the migration of a large number of people, to low vaccine coverage rates, and to the use of low-quality vaccines. Nationally, 3.044 million cases of meningococcal disease were reported in 1967 [1], which was the largest number of cases reported since the founding of the PRC. Poliomyelitis was a serious disease that caused a large number of deaths and disabilities among children. According to a survey in one province, between 1970 and 1972 coverage of polio vaccine hovered between 32% and 51.4% among children under the age of 7 years of age. A survey of 1281 polio cases in Jiangsu, Zhejiang, and Guangdong provinces found that none of the children who got polio had completed the polio vaccination schedule. The incidence of polio remained high, with a national annual incidence of greater than 2/100,000 in 1970–1973.
The State Council approved a document, “Report on Strengthening the Prevention and Treatment of Infectious Diseases,” which was written by MoH in the mid-1970s [1]. With the acceptance of that report, important attention was again paid to vaccination work. Special staff members were designated in EPSs at all levels to be responsible for vaccination, and vaccination services at the grassroots level developed and matured rapidly. A system of citizens’ vaccination cards was established; simple equipment for cold storage and transportation of vaccine was obtained; and the expanded program on immunization was implemented in many regions.
The cold chain is composed of cold rooms, refrigerated vehicles, freezers, refrigerators, cold boxes, and vaccine carriers that are collectively used for storage and transportation of vaccines. MoH issued “Notice of a Cooperative Project on Cold Chain between China and United Nations International Children’s Emergency Fund (UNICEF)” in December of 1981 [1], and this notice opened the door for cooperation with UNICEF, WHO, Japan International Cooperation Agency (JICA), and other international organizations. It was at this time that China’s government and UNICEF started their cooperative project on vaccine cold chain. First, a pilot project was initiated in Hubei, Guangxi, Fujian, Yunnan, and Sichuan provinces, where the climate is hot. Central and local governments actively cooperated by providing supplementary funding, and cold chain coverage increased rapidly. From 1996 to 2004, the China government used a World Bank loan to provide ten provinces, including Gansu province, with cold chain equipment. At that time, most families in China didn’t have refrigerators and refrigerated vehicles were rare. In general, health centers were not equipped with refrigerators, and no refrigerated equipment was available in village clinics for storage of vaccines and biological products. Construction and wide availability of the cold chain played an important role in improving the quality and effectiveness of vaccines.
I began my work in October 1984 as a new “recruit,” and in 1985 I participated in a national vaccination workshop in Changsha, Hunan Province. In the meeting an inscription by President Li Xiannian was shown: “Universal children’s immunization, promoting the healthy growth of offspring.” I also saw a number of domestic leaders who were responsible for the organization of immunization programs, including Wang Jian and Cao Qing from the MoH Department of Health and Epidemic Prevention, along with experts like Kai Zhao, Wenyuan Ze, Yongge He, Kaihua Sun, and Liandong Diao.
In 1986, Gansu province received funding from UNICEF to provide cold chain equipment for the 2.5-million-person Tianshui Prefecture. With the aid of international organizations like UNICEF and friendly countries, refrigerated vehicles, refrigerators, cold boxes, and cold carriers were gradually procured to establish a vaccine “cold chain” that went continuously from manufacturers to point of vaccination (PoV) clinics. Between 1986 and 1993, I visited the “Cold Chain Project Office” in Beijing’s EPS, which had been established by MoH and drivers from county EPSs, and drove vaccine transport vehicles assigned to each county in my province for the long journey back to the counties. It was at that time I began to know many colleagues, such as Qiyi Xie, Biao Guo, and Yanmin Liu. By the end of the last century, China had built a “cold chain” system for vaccine delivery and transportation across the entire country.
1.2 Vaccination Rates: Achieving the 3 “85% Goals”
The time I began work was the so-called golden era of EPI. The central and local governments attached great importance to EPI work. Mobilizing the public, increasing vaccination rates, and reducing the incidences of vaccine-preventable infectious diseases were the primary works of the Department of Health at each level. On August 15, 1985, on behalf of the Chinese government, President Li Xiannian committed to the goal of universal children immunization by 1990. The goal was to be achieved in two steps: first, vaccination rates should reach 85% in each province by 1988, and second, coverage should reach 85% in each county by 1990. These objectives were included in the 7th Five-Year Plan of the National Economic and Social Development. A National Immunization Coordination Committee was established in 1986, with members from MoH, the State Education Commission, China Women’s Federation, the Ministry of Broadcast and Television, the Ministry of Foreign Trade and Economic Cooperation, and the State Ethnic Affairs Committee. April 25 was designated as “National Children’s Immunization Day” [1].
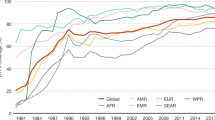
In March 1989 and 1991, MOH, WHO, and UNICEF jointly reviewed and confirmed that the BCG, oral poliovirus, DTP, and live, attenuated measles vaccination rates among 1-year-old children reached 85% by provincial and county levels, respectively, achieving the goal of universal access to childhood immunization. Incidence rates of infectious, vaccine-preventable diseases had also been significantly reduced.
The pilot evaluation for the first 85% goal was conducted in Gansu province. Longde Wang, Deputy Director of Gansu Health Bureau, who later became the Vice Health Minister, was in charge of health protection and epidemic prevention in Gansu. Zhao Wang, Deputy Director of the MoH Department of Health and Epidemic Prevention; Baoping Yang, Director of the Immunization Program Division; and Jingjin Yu organized the evaluation. The pilot evaluation greatly promoted immunization in Gansu province. As a scientific researcher in the Gansu Health Bureau’s Department of Health and Epidemic Prevention, I was responsible for the logistics of the pilot evaluation, along with support to leaders and experts from MoH.
In 1992, hepatitis B vaccine began to be managed by the children’s immunization program. BCG vaccine, oral poliovirus vaccine, DTP vaccine, and live, attenuated measles vaccination rates had attained 85% at the township level among 1-year-old children by 1996. China had made great progress in the work of immunization and was highly praised by the international community. MoH won a Silver Medal for Children’s Survival, awarded by UNICEF [1].
Once vaccine development, production, and supply issues were addressed, the priority of the universal immunization turned to management. That immunization in children in China achieved impressive results was due in part to the strong support from health administration departments at all levels. Immunization was the priority of public health and health sectors at all levels. In 1986, a special division of immunization was established in MoH that was responsible for managing the National Immunization Program (NIP). Since the beginning of the immunization division, a total of six people have served as director. I have had the honor to work with all of them, promoting together immunization in China. They are Baoping Yang, Jingjin Yu, Jun Zhou, Gang Cui, Quanle Li, and Ming Lu. Mr. Baoping Yang served as Director of the Department of Immunization, WHO Western Pacific Regional Office, and is now retired. Mr. Jingjin Yu is now the Director of the Department of Disease Control and Prevention, National Health and Family Planning Commission, still covering immunization. When I was the Director of NIP, China CDC, Jun Zhou was the Director, and certification of polio-free status after the importation of wild poliovirus in Qinghai was the priority. During this time we were planning a project with GAVI on hepatitis B vaccination and a measles control project in Guizhou. Mr. Gang Cui worked with me for the longest time, and together with provincial colleagues, we completed the hepatitis B vaccine GAVI project. We participated in the expansion of NIP to include more vaccines into the EPI system, promoted the use of auto-disposal syringes, established a surveillance system for adverse events following immunization (AEFI), and assisted with the prequalification of a Chinese JE vaccine. We properly addressed the Shanxi vaccine incident together with Director Jingjin Yu. We also took part in two events that could have had an important impact on the history of vaccination in China: the development of influenza A vaccine in 2009 and a national measles vaccine supplementary immunization activity in 2010.
1.3 A Series of Policies Developed to Promote Vaccination
Health services in rural China developed rapidly in the mid-1970s, with cooperative medical systems established in more than 70% of large cohort areas (administrative village, citizenship committees, hereinafter referred to as villages) across China. A team composed of 1.3 million barefoot doctors (village doctors) and 3.6 million health workers and midwives was established that provided medical and vaccination services. In 1978, the “Notice on the Strengthening of Immunization” was issued by MoH which required that “corresponding personnel must be designated in EPS to be responsible for immunization in all provinces, municipalities, and autonomous regions.” In 1982, MoH issued “National Immunization Regulations,” further requiring that teams should be constructed at EPSs to be responsible for EPI services. The vast cadre of rural doctors played a crucial role in improving vaccination rates as they went street by street and house by house to provide vaccinations. Because the cold chain system was not perfect, most vaccination was carried out in the cold winter season when the ground was full of ice and snow and mountain roads were slippery – to the point that some CDC staff and clinic doctors lost their lives. In Gansu, where I worked, there were several rural doctors who lost their lives because of traffic accidents during polio vaccination.
Since then, EPI departments have been set up in EPSs in all provinces, autonomous regions, and municipalities (hereinafter referred to as provinces) and in all prefectures and cities (hereinafter referred to as prefectures); an EPI group was set up in departments of epidemic prevention in EPSs in all counties, districts (hereinafter referred to as counties), and specialized personnel were designated to be responsible for immunization programs in township hospitals. In the early 1990s, the Division of Immunization Management was set up in the MoH Department of Primary Health and Epidemic Prevention, and in 1989, the Immunization Technical Guidance Center was set up in the former Chinese Preventive Medicine Academy (CPMA), with Ke’an Wang acting as Director. The EPI office was placed in the Institute of Epidemiology and Microbiology. Experts, such as Rongzhen Zhang, Libi Zhang, Xia Liu, Mu Liu, Xu Zhu, Xiaojun Wang, Lixia Wang, Feng Chai, and Wenbo Xu, worked hard and played an important role in the construction of the technical platform for immunization, the development of technical guidance, and the work on international cooperation.
In 1995, I went to Beijing to pursue my master’s degree in “Social Medicine and Health Management” in CPMA. This major was later changed to the In-service Masters in Public Health, which was included in the In-service Masters Education program. While I was studying in Beijing, I participated in routine activities with the EPI Division in MoH. At this time, the focus of immunization was to eradicate polio. The Japan International Cooperation Agency (JICA) played a significant role through a number of senior experts to assist the construction of a national and provincial polio laboratory surveillance network in China, to provide kits and equipment, and to train, hand in hand, CDC staff in China with a group of young experts, including Li Li and Jie Lei. Long-term and short-term experts, such as Yuanren, Chiba, Tiezuo, Rushan, and Qingshui, devoted themselves to this work in China. Through their work, they also established deep friendships with Chinese experts.
In 2000, together with other countries in the Western Pacific Region, China achieved polio-free status, and Health Minister Wenkang Zhang attended the certification conference in Tokyo.
In June 2000, MoH held a “Seminar on Strategies for Hepatitis Control” that resulted in the development of a National Proposal on Hepatitis Control, which was submitted to the State Council. During this time, the GAVI China project was started, with the central government and GAVI providing half of the funding necessary to provide free hepatitis B vaccine for newborn infants in the western provinces. An immunization strategy was gradually formed that combined routine immunization, supplementary immunization activities, and emergency vaccination. Vaccination service frequencies increased in most areas, with the interservice period shortened.
1.4 Vaccination Management by Law
After I obtained my master’s degree, I had an opportunity to study at the medical school in the University of Miami in 1996. After returning to Gansu, I served as Deputy Director of Gansu province EPS, in charge of immunization. At that time, I worked with Hui Li, Director of the Department of Immunization, and Fuqiang Cui, Deputy Director of the Department of Immunization. Measles outbreaks were frequent in Gansu and other provinces, and together with Hui Li, I went to Wudu County to investigate and handle a measles outbreak. Due to the lower economic level in Longnan County, Gansu, the awareness of immunization among the general public was very weak. The POV workforce was lacking, and no funding was provided by the government to the township healthcare centers – almost leading to their closure. The majority of children living near hospitals developed measles; there were also many adult cases. In total, 12 patients died during the outbreak, which shocked me and gave us a profound lesson. I was transferred to work in the Chinese Academy of Preventive Medicine in 2000, and replaced Xinglu Zhang in 2001, serving as the Director of National Immunization Program (NIP), China CDC.
On the basis of the previous work in the National EPI Technical Guidance Center in CPMA, China CDC introduced professionals from provinces to expand the “national team.” Huaqing Wang, Li Li, Fuqiang Cui, Jingshan Zheng, and Dawei Liu – all excellent – were transferred from the province level. Zijian Feng, Deputy Director of China CDC, was transferred from Henan Province CDC. He and I were the leaders of NIP for more than a year. He is now the Deputy Director of China CDC in charge of vaccination. Biao Guo translated materials on immunization from WHO and other organizations and accumulated professional knowledge for EPI work in China. In December 2004 [1], the “Law on Infectious Disease Prevention and Control” was implemented, in which the vaccination card system was required and free EPI vaccines begun.
In 2005 the State Council developed and issued the “Regulations on Vaccine Distribution and Vaccination Management” [1], with a principle of “person-oriented” services. The government provides “public products” to the people so that the general public has full access to services for the prevention and control of vaccine-preventable diseases (VPD) and is protected with public health rights. Vaccines were divided into two categories. The first category referred to free vaccines provided by government to citizens, which should be administered in accordance with the requirements of government. The first category of vaccines includes vaccines in the NIP, Provincial Immunization Programs, and vaccines for emergency or campaign use, as determined by government or health administrative departments at the county level and above. The second category of vaccines refers to other vaccines voluntarily received by citizens, with payment out-of-pocket. After the “regulations” were issued, a system to qualify vaccinators was inaugurated which required that only individuals (medical practitioners, physician assistants, nurses, or village doctors) who participated in a training course and passed a test organized by the county-level health administrative departments were qualified to provide vaccination services. To further develop the immunization program, in 2007 the State Council decided to include more vaccines into NIP, with an ultimate total of 14 different vaccines, including hepatitis B vaccine, BCG, and many others. The number of NIP vaccines was expanded from 6 to 14, for provision at no charge to age-eligible individuals. The number of NIP vaccine-preventable disease increased from 7 to 15. Expansion of NIP vaccines was notable for its inclusion of meningococcal vaccine and Japanese encephalitis vaccine. After several years of immunization, with an increase in vaccination coverage, the incidences of meningococcal meningitis and Japanese encephalitis were reduced to below a hundred.
1.5 NIP Vaccine-Preventable Infectious Diseases: Transitioning from Common to Rare
It is the 30th year since I graduated from the university, and I deeply appreciate that the NIP vaccine-preventable diseases have decreased from common to rare, dropping to the historically lowest level. Thanks to the effort of several generations of immunization staff, transmission of these diseases has been effectively controlled.
1.5.1 Achievements in Polio Control
Reporting of polio cases began in 1953, with annual reports of 20,000–43,000 cases in the early 1960s. Since 1965, the use of oral poliovirus vaccine (OPV) manufactured in China has been promoted nationwide, with vaccination rates increasing with time and resulting in substantial decreases in the incidence of and death from polio. The incidence of polio decreased by 37% from the 1970s compared with the 1960s [1].
In the 1990s, polio eradication activities were carried out all over China. On top of routine immunization, mass catch-up immunization campaigns were conducted that rapidly improved population immunity levels. An effective immunity barrier against the spread of poliovirus was established in China that blocked the spread of native, wild poliovirus and decreased the incidence of polio year by year [1]. Since 1994, when the last polio case caused by wild poliovirus was reported, China has continuously maintained polio-free status. In 2000, China was certified as polio-free, which was confirmed by WHO.
In 2011, just as I left the position of NIP Director, a polio outbreak due to an imported poliovirus occurred in southern Xinjiang. Through virological analysis, it was confirmed that the outbreak was caused by a virus imported from Pakistan. In total, 21 cases were confirmed, and about half the cases were among adults, with a maximum age of 51 years. At that time, as an expert, I went to the site with Health Minister Zhu Chen and Vice Minister Li Yin. Looking at the serious faces of the two ministers, I really felt deep remorse. Tears came down especially hard when Director Yu Wang and I saw a 26-year-old Uighur male patient infected with polio who was paralyzed in both legs. I couldn’t tell whether to feel guilt, sympathy, or something else.
Just 1 year before the outbreak, we sent a supervision group led by Jingui Chu to southern Xinjiang to monitor the polio vaccine supplementary immunization. They found that immunization in southern Xinjiang was weak and reported this finding to MoH. The newly appointed Deputy Director, Zhenglong Lei, and Quanle Li, Director of Division of Immunization, went to Xinjiang to supervise immunization. However, their finding didn’t arouse enough attention by local leaders and professional department staff, and so this disaster occurred. More than 430 staff members from CDCs of other provinces were deployed to Xinjiang to assist in the response to the outbreak. The WHO office also sent staff to participate in the response; MoH and China CDC sent a long-term expert team to Xinjiang. The central government used the Air Force to transport the vaccines from Beijing to southern Xinjiang. A year later, WHO evaluated and confirmed that China had remained polio-free, and praised China’s emergency response, which had set an example for the world.
It is really true that immunization cannot be slackened!
1.5.2 Implementation of Measles Elimination
In the 1960s, during the pre-measles vaccine era, there were measles epidemics every 2–3 years. Almost everyone was infected during childhood – in fact, it was difficult to avoid the infection [1]. In 1965, a measles vaccine was used in China for the first time, resulting in a continuous drop in incidence and mortality of measles since that time. The incidence and mortality of measles had decreased by more than 95% in 1990 compared with 1978. In 1998, China MoH proposed to accelerate measles control and developed a “Measles Control Action Plan” with an objective to lower the incidence below 8/100,000 total population. All provinces responded positively to the plan and took action to control measles.
A national measles vaccine supplementary immunization activity (SIA) was conducted in 2010 with more than 100 million age-eligible children immunized during two rounds of measles vaccination. There are many stories to tell when speaking of the SIA. In retrospect, the greatest barrier was communication and publicity. It was the first time that 100 million children under the age of 4 years were vaccinated against measles within 1 week. We thought that the measles vaccine was a commonly used NIP vaccine, with many sub-national SIAs conducted in the provinces, causing few problems. We subsequently found out that our social mobilization was not sufficient, and we didn’t report this clearly to the leadership team. In the preparatory stage, Dr. Yu Wang, Director of China CDC, discussed the SIA twice with me and Huiming Luo, Deputy Director of NIP. Dr. Wang was concerned that the general public and the media might have a strong reaction. Full of confidence, I said, “no problem!” But later wide doubts appeared, especially through Internet rumors. The leadership team felt under a great deal of pressure, and the SIA was almost stopped before it started. Finally, MoH decided to carry out the SIA on time, with WHO officials providing answers to questions by mainstream media. Minister Zhu Chen and Vice Minister Li Yin personally took me to explain the SIA to influential leaders and media opinion leaders. I also asked an expert on immunization from Peking University Health Science Center to come to the NIP office to discuss the rationale for this campaign and to resolve his doubts. In the end, everyone agreed to take their children to receive measles vaccine.
I still remember when the first dose of measles vaccine was administered in Sanjianfang community in Beijing Institute of Biological Products, with two ministers personally supervising the vaccination, with rescue equipment and emergency medicines on hand, and with an ambulance in the community health center prepared for anything. The scene is still vivid before my eyes.
1.5.3 Hepatitis B
Hepatitis B virus is highly epidemic in China. According to a national serological epidemiology survey for viral hepatitis in 1992, HBsAg carriers accounted for 9.8% of the total population [1]. In 2002, hepatitis B vaccine was included in NIP with a focus on improving the vaccination rate among children in rural areas of middle and western China. A national serological survey in 2006 showed that the HBsAg carriage rate was 7.2% (0.96% among children 1–4 years old), having decreased by 26.4% compared with 1992. Through hepatitis B vaccination of newborns in China, the current generation of children has been effectively protected against hepatitis B. The progress of hepatitis B prevention and control is significant. An objective to reduce HBsAg rate to less than 2% in children under the age of 5 by 2012 that was proposed by WHO was achieved in advance in China. In 2014, the HBsAg prevalence remained below 2% in children under 5 years of age according to a national serological survey of viral hepatitis.
Here, thanks to the support by national major special funding, I took the lead, while Fuqiang Cui and Li Li were responsible for the implementation of two national serological surveys on hepatitis B to understand the epidemiology of hepatitis B. In particular, hepatitis B vaccine was demonstrated to have protected children. Thinking of this, I am full of pride and honor simultaneously!
1.5.4 Hepatitis A
The reported incidence of hepatitis A has been on the decline since the 1990s, and the number and size of public health emergency events have decreased year by year and to a record been low in year 2012 [1].
In 2007, hepatitis A vaccine was integrated into the immunization program for 18-month-old children for routine vaccination. With emergency vaccination in flooded areas, earthquake-hit areas, and areas with high incidences, vaccination reduced the number of cases of hepatitis A [1].
1.5.5 Meningococcal Meningitis
There were many epidemics of meningococcal meningitis (MM) (referred to as epidemic meningitis, mainly caused by serogroup A) with variable intensity in China. Five national epidemics were recorded – in 1938, 1949, 1959, 1967, and 1977. The most serious epidemic was in 1967 with an incidence of 403/100,000, with more than 3.044 million cases across rural and urban China [1]. In 1980, China began to use a meningococcal polysaccharide vaccine, and outbreaks of meningococcal meningitis were effectively controlled. In 1984 a comprehensive prevention and control strategy with universal immunization using meningococcal polysaccharide vaccine was implemented as a priority which resulted in a continuous decrease in incidence. The incidence of MM was maintained at less than 10/100,000 through the 1990s and less than 0.1/100,000 since 2000. China-produced meningococcal conjugate vaccine A + C was initially marketed in 2007, and the disease incidence dropped to 0.09/100,000 that year. In 2007, MM vaccines were integrated into NIP, which further reduced the incidence of MM [1].
When it comes to meningococcal meningitis, an outbreak by serogroup C in Anhui province in the beginning of 2004 should be mentioned. In Hefei city, an outbreak of meningococcal meningitis occurred among primary school students. The outbreak was confirmed by academician Jianguo Xu to be caused by serogroup C. Dr. Xu’s paper was published in The Lancet. This was the first serogroup C outbreak in China. I was in Anhui to organize the vaccine supply for supplementary immunization and lead the investigation. It was a thrilling war.
1.5.6 Japanese Encephalitis
The incidence of Japanese encephalitis (JE) increased since the early 1950s in China, reaching its first peak in 1966 and second peak in 1971, with more than 150,000 (incidence of 20.6/100,000) cases and 170,000 cases (incidence of 20.9/100,000) reported, respectively. The epidemics spread to the northeast and northwest of China. Starting in the 1980s, the incidence began to decrease significantly and dropped to less than 1/100,000 after 1998. The incidence showed a continuous decline after 2000 and has been maintained at historic lower levels [1].
When I worked in Gansu, I had never seen JE. But when I moved to Beijing, together with Feng Yang (Deputy Director of the Office of Emergency Response, National Health and Family Planning Commission) and Rongmeng Jiang (a famous expert at Beijing Ditan Hospital, with whom I worked on Ebola in Sierra Leone in 2014 for 2 months), I went to Xishuangbanna, Yunnan province, to handle a JE outbreak. There, I witnessed a 19-year-old stiffly lying in his father’s arms, who could not speak and who could only pray from his eyes. The reason he developed JE was easy to understand – he had no money for vaccination, and he lived with his father in a sugarcane field that was full of mosquitoes.
1.5.7 Pertussis and Diphtheria
Pertussis:
the incidence of pertussis in China ranged between 100/100,000 and 200/100,000 in the pre-vaccine era, with epidemics every 3–5 years. The pertussis incidence decreased substantially during the EPI era. However, an “underestimate” of incidence has been controversial in recent years due to antibiotic overuse. Prevention and control of bacterial diseases have again received attention by relevant disease control departments [1].
Diphtheria:
the morbidity and mortality from diphtheria have been greatly reduced during the EPI era, and the incidence in recent years has been reduced to a surprisingly low level. Between 2003 and 2006, only ten cases were reported in China, and no cases have been reported since 2007 [1].
1.5.8 Development and Vaccination of Influenza A (H1N1) Vaccine
A pandemic caused by influenza A (H1N1) occurred in 2009. In early June, China established a coordination mechanism for development and research and production of influenza A (H1N1) vaccine composed of the National Development and Reform Commission, MoH, the Ministry of Industry, China FDA, China CDC, the Chinese Institute of Control Pharmaceutical and Biological Products, and ten influenza vaccine manufacturers. China CDC organized and implemented a clinical trial of influenza A (H1N1) vaccine. More than 13,000 volunteers were vaccinated with the vaccine. All NIP staff went to the sites for implementation of this trial. Thanks to the support by colleagues of the provincial CDC, this historically largest vaccine clinical trial in China was successfully completed. Huaqing Wang and I witnessed the first dose injected to Minister Zhu Chen in his office, after he volunteered to receive the vaccine.
At the beginning of June, China’s H1N1 influenza vaccine production companies obtained vaccine seed virus from WHO and developed/produced the vaccine according to the production process of seasonal influenza vaccine for clinical trials. The clinical trial began on July 22, and applications for licensure by eight producers were submitted starting in early September after on-site inspection, registration inspection, review, and evaluation.
On September 8, 2009, Health Minister Zhu Chen said China was the first country in the world with an H1N1 influenza vaccine. Zhu Chen said at a press release that China successfully conducted a clinical trial of the vaccine and demonstrated the safety and effectiveness of H1N1 influenza vaccine on September 7. After licensure, the State Food and Drug Administration released the first batch of qualified vaccine, and China became the first country with an H1N1 influenza vaccine.
Subsequently, high-quality AEFI surveillance was conducted; AEFIs were reported daily. A study to determine whether there was a relationship between acute flaccid paralysis and the H1N1 vaccine was published in the New England Journal of Medicine; the study provided strong evidence that the H1N1 vaccine would not cause GBS.
1.6 The Future of Immunization Program
I left NIP, China CDC, after working there for 10 years. My mind is still attached to NIP. China’s EPI has achieved fruitful outcomes. Through the effort of several generations of EPI staff, smallpox and polio were eradicated; China has moved solidly toward the goal of measles elimination; the HBsAg prevalence declined greatly; incidences of hepatitis A, meningococcal disease, and Japanese encephalitis have decreased continuously. Especially since 1978, when EPI was implemented, the incidence of NIP vaccine-preventable infectious disease has decreased by 99%. NIP has played an invaluable role in the protection of people’s health, increasing life expectancy, resulting in huge economic benefits and persistent social benefits.
However, with the progress and expanding of immunization program, China’s NIP faces an unprecedented opportunity for development and at the same time faces many difficulties.
When the essay was close to being completed, the “illegal sales of vaccine in Ji’nan Shandong” occurred. The impact of the event on vaccination was unprecedented in terms of the scale and significance. Its conclusion will reveal itself later.
Due to an imbalance of economic development in China, neither a long-term financing-guaranteed mechanism for vaccination nor policies for financing the immunization program were established in some areas – especially in remote and poor areas. Financing challenges affect equity of EPI services. Major barriers to further development of NIP include the following: (1) inclusion of vaccination into the primary public health services, (2) funding for expansion of cold chain equipment, (3) subsidies for immunization services and emergency vaccination at the grassroots level, and (4) funding for NIP team construction. At the same time, we have to (1) prevent and block the transmission of imported poliovirus and maintain polio-free status, (2) rapidly control intermittent measles epidemics, (3) provide immunization services for migrant populations, (4) develop new vaccines and combination vaccines, (5) reduce vaccine wastage, (6) eliminate unsafe injection during vaccination, and (7) improve the sub-optimal AEFI compensation mechanism. The above issues may impede achievement of equity for the children’s access to immunization services.
With the progress of China EPI, we need to (1) accelerate financing mechanisms for immunization; (2) strengthen the NIP team and manage the migrant population; (3) learn from international experiences to develop a reasonable vaccine evaluation mechanism; (4) fully utilize expert consultation to develop technical guidance and fully use the information management system; (5) develop new vaccines and combination vaccine by thorough integration of research, academia, and industry; and (6) continue maintaining “polio-free” status, eliminate measles, and control hepatitis B – all these to contribute to disease prevention and control in China.
China’s immunization program will be upgraded to a new level with its brilliant future and with universal access to immunization services. At the same time, China’s vaccines will be exported to Asia and to the world to make new contributions to global immunization efforts. We believe that vaccination will continue to benefit children and make contributions to achieving the goals in Healthy China 2030.
Reference
Wang Guoqiang. Disease control and prevention of China-60 years. Beijing: China Population Press; 2015. p. 259–94.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd. & People's Medical Publishing House, PR of China
About this chapter
Cite this chapter
Liang, X., Liu, Y. (2019). My Experience as Director of the National Immunization Program (Historical Review). In: Liang, X. (eds) Immunization Program in China. Public Health in China, vol 3. Springer, Singapore. https://doi.org/10.1007/978-981-13-2438-3_1
Download citation
DOI: https://doi.org/10.1007/978-981-13-2438-3_1
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-2437-6
Online ISBN: 978-981-13-2438-3
eBook Packages: MedicineMedicine (R0)