Abstract
Improvements of public health and advances in medicine after World War II have given Japan one of the highest average life expectancies in the world. Increased life expectancy means that more senior citizens will have serious physical and mental illness, which causes an increase in the number of the older people who need care for their daily livings as well as medical care for their chronic diseases. Informal care for the older people with disabilities has proven to be a heavy burden for their family caregivers in many countries, and women were assumed to provide the main source of support for family members in Western countries as well as in Japan. The value of filial piety, which is a social norm that parents should love and care for their children and that children in turn should respect and care for their parents, have been shared for many generations in East Asian nations including Japan. Therefore, Japanese caregivers are concerned about what others say when they use social care services for their parents. In April 2000, the public long-term care insurance system (LTCIS) for the older people was launched in Japan, making it the third country, after the Netherlands and Germany. In this chapter, we would like to introduce Japanese LTCIS and studies on burden/depression among caregivers before and after the introduction of this system.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
2.1 Introduction
Before World War II, the average life expectancy was shorter than 50 years (i.e., 43 years old for men and 44 years old for women in the 1890s and 46.9 years old for men and 49.6 years old for women in 1935) in Japan [1]. However, improvement of public health and advances in medicine after World War II have given Japan one of the highest average life expectancies in the world (i.e., 81.0 years old for men and 87.1 years old for women in 2016) [2], and the proportion of the elderly (i.e., 65 years old and older) increased from 4.9% in 1950 to 26.6% in 2015 [2]. The dramatic increase in the number of older people in this country is well documented [3]. Increased life expectancy means that more senior citizens will have serious physical and mental illness, which causes an increase in the number of senior citizens who need care in their daily lives. It is estimated that the number of older people with disabilities will reach 5.2 million in 2020 [4]. Demand for long-term care grows exponentially with age, and the bulk is much greater in the older ages (aged 75 years and older) than younger ages (younger than 75 years old) among the elderly.
In former days, family members took care of the disabled elderly with chronic illness in the traditional family system because most Japanese elderly, over 60% compared with 20% or less in Western countries, lived with their children [3].
For most adult children who live with the their parents before their parents develop chronic illnesses such as dementia, the change in role identity is a slow process, and the care needs of the aged parents may gradually increase, which may lead adult children to undertaking a family-caregiver identity without experiencing heavy stress [5]. Women were assumed to provide the main source of support for family members in Western countries [6] as well as in Japan [7, 8]. The value of filial piety, which is a social norm where parents should love and care for their children and that the children in turn should respect and care for their parents, have been shared for many generations in East Asian nations (China, Korea, and Japan) [9]. The study by Lee and Farran [10] compared depressive symptoms among South Korean, Korean-American, and Caucasian-American female family caregivers of older persons with dementia. In their study, the rates of the daughter and daughter-in-law (i.e., son’s wife) were greater than the rates of the wife in South Korean caregivers (81.0% vs. 16.0%) and in Korean-American caregivers (71.2% vs. 23.7%), while the rates of two groups were almost similar in Caucasian-American caregivers (50.0% vs. 48.7%) [10].
In contrast to Nordic countries where the ultimate responsibilities lies with the state rather than the family iteself, in Japan,the family care was the gratuious labor that a married woman performs among families [7, 8] and female family members (i.e., daughters, daughters-in-law (i.e., son’s wives), and wives) took care of aged family members under the influence of Confucianism (i.e., filial piety) [8]. However, the number of children in each family has dramatically decreased because the live birth rate (per every 1000 Japanese people) decreased from 28.1 in 1950 to 7.8 in 2016 [2]. According to the decreased birth rate, the average number of family members in each family decreased from 3.41 in 1970 to 2.42 in 2010 [11], which decreased power of family caregiving. Furthermore, the proportion of full-time workers increased from 31.8% in 1985 to 41.9% in 2010 among Japanese women with working age (i.e., 15–64 years old), while the proportion of those who take care of the housework for their family decreased from 34.8% in 1985 to 26.3% in 2010 [11], which also decreased the ability of family caregiving. In addition, the proportion of the elderly who lived with their children decreased from 69.0% in 1980 to 39.0% in 2015 [12], while the proportion of those who lived with their spouses only increased from 19.6% in 1980 to 38.9% in 2015 [12], which increased the rate of spouse-caregivers and male-caregivers among family caregivers of older people with disabilities in Japan.
Nowadays, many Japanese family caregivers often have to take care of their charges without help from other relatives, because they often live too far away to provide assistance from their relatives. Therefore, family caregivers are often both physically and mentally burdened with caring for their charges [4]. Except spouse-caregivers (i.e., retired husbands and wives, full-time homemakers), other family caregivers (i.e., daughters, sons, son’s wives) may be obliged to change their work from full-time to part-time or to retire before a retirement age in order to take care of the charges at home in Japan [7], which may financially burden caregivers as well.
Several reports [13, 14] demonstrated that a large amount of time spent on daily caregiving was related to the feeling among such caregivers of carrying an insupportable burden. It has been reported that caring for older people may induce depression in the caregivers [15]. Caregiver’s depression is an important social problem in Japan because it involves the potential risk of caregivers discontinuing caregiving at home [16].
2.2 Public Long-Term Care Insurance System for Older People in Japan
Long-term care services are needed for persons with long-standing physical or mental disabilities, who need assistance with basic activities of daily living (ADL) (e.g., bathing, dressing, eating, getting in and out of bed or chairs, moving around, and using the bathroom), many of whom are the highest age groups of the population (i.e., older people aged over 80) [17].
In Japan, the environment for older people and their caregivers has undergone momentous changes. In April 2000, to promote greater autonomy of the older people in their daily lives as well as to reduce burden on their caregivers, the public long-term care insurance system (LTCIS) for older people was launched in Japan, making it the third country [18, 19], after the Netherlands [20] and Germany [21], to provide such insurance.
The fundamental purpose of LTCIS is the establishment of what can be called “universalism” in care policies for older people [22]. First, under the new public LTCIS, all of the older people in Japan, who need assistance with basic ADL, can use the care services for the older people, according to the Government-Certified Disability Index (GCDI) (i.e., degree of need of care; “Yokaigodo” in Japanese) [23], while the care services for the older people in Japan were formerly reserved for users from low-income households before LTCIS was implemented (i.e., under the old selective tax scheme). Second, the users themselves can determine their individual need for services under LTCIS, while the administration of service was determined by public administrative agencies before LTCIS [19]. Under LTCIS, the older people and their caregivers are entitled to decide both the kind and the amount of services they wish to use according to their need of care within the limits of GCDI [19, 23] (i.e., degree of need of care). Third, LTCIS allows both profit-based and nonprofit private organizations to provide care services for older people, while the service providers were confined to municipal governments and nonprofit private organizations stipulated by the Social Welfare Law before LTCIS. Fourth, the insured persons are required to bear the co-payment (i.e., 10%) depending on the service utilized under LTCIS, while the older people (65.0 years old and older) paid only limited fees before LTCIS. Last, the middle aged (40–64 years old) are also required to become members of LTCIS in order to assist in bearing the cost of this insurance system, due to their parents possibly using services under LTCIS.
However, some problems about the LTCIS were pointed out before its introduction [24]. First, the insurer is not a country but cities, towns, and villages which have big variability in financial power. Therefore, the quality and the kind of care services that insured persons receive as well as share of insurance premiums may be different between insurers (i.e., cities, towns, and villages) [24]. Second, family care is still the gratuitous labor even after the introduction of the LTCIS in Japan. In contrast, German family caregivers receive money of reward for caring for older people at home, although they receive much less money than “performance in kind” to provide public assistance by furnishing care services [24], which suppress the expenditure and may evade large deficits in Germany.
After Japan, South Korea launched a public long-term care insurance system (LTCIS) for older people in 2008 [25]. Ham [25] pointed out several problems about the LTCIS in South Korea such as (1) deficiencies in the system and service contents, (2) problems with privatization of care services (e.g., commercial operation, lower service levels, workers’ wage exploitation, and worsening worker conditions), (3) difficult accessibility to service use, (4) regional disparity in services, and (5) improper self-paid insurance premiums (i.e., decreased usage of services in the poor senior citizens and increased usage of services in rich senior citizens).
In Japan, under LTCIS, the insured senior citizens (65.0 years old and older) increased from 21.65 million in 2000 to 33.87 million in 2016, while the senior citizens in need of care increased from 2.18 million in 2000 to 6.22 million in 2016 [2]. The older people with disabilities can use services according to their GCDI (i.e., degree of need of care) under LTCIS. However, some of the senior citizens are obliged to abandon their right to use certain parts of the services under LTCIS due to not being able to afford the self-pay financial burden of all the services that they have the right to use according to their GCDI. Before the introduction of LTCIS, the senior citizens in the poor class did not have to pay money to use any service under the old selective tax scheme. On the other hand, after the introduction of LTCIS, only the very poor senior citizens who live on welfare do not have to pay money (i.e., the co-payment) for care services under LTCIS. Therefore, the poor senior citizens, those who do not live on welfare, have more difficulty accessing the care services under LTCIS than under the old selective tax scheme. On the other hand, with reduced self-payment under LTCIS and the ability to use care services with the co-payment (10%), the senior citizens in the middle and upper class can use more services under LTCIS than under the old selective tax scheme. After saving 90% of money for care services under LTCIS, they can pay for more additional services out of pocket.
After the revision of LTCIS, the financial support to reduce the financial burden of the poor senior citizens was offered, while the rate of co-payment was increased from 10% to 20% for the rich senior citizens (i.e., one fifth of the older people) in 2015 [2]. However, ownership of expensive real estate does not always mean that the senior citizens and their caregivers are rich enough to pay higher rate (20%) of self-payment for care services under LTCIS. Although some of the frail elderly and their caregivers (e.g., the older people with disabilities and their spouses aged over 80 years old, the older people with disabilities and their adult children who have no income) live in the residents at the place with high land prices, these older people with disabilities and family caregivers may abandon their right to use parts of the services under LTCIS, because they do not have enough money (i.e., income or savings in their banks) to pay higher rates (20%) of self-payment for all care services that they have the right to use according to their GCDI (i.e., degree of need of care).
In Nordic countries such as Sweden, the ultimate responsibility for the older people with disabilities lies with the state rather than with the family itself [26]. Mikami [26] reported the five basic ideas of welfare for the older people in Sweden, which were normalization (i.e., continue to live in the usual living environment), view a person as a whole (i.e., view a person from psychological, physical, and social aspects), self-determination (i.e., recognize and respect rights to decide one’s way of life), social participation (i.e., take part in community activities), and activation (i.e., assist the elderly to perform leisure activities according to his/her ability and interests).
Maintaining an active life is believed to help the older people to preserve their physical and mental health [27]. Fratiglioni et al. [27] suggested that all of the social, mental, and physical lifestyle components have a protective effect against dementia. Therefore, the older people should not change their residence in late life. However, there are a few older people who sell their residence in order to use care services under LTCIS. For the prevention of dementia, the care system for the older people to cover the minimum care services for all older people with no co-payment may be desirable in order to ensure the safety net for the older people.
2.3 Burden Among Family Caregivers of Older People
2.3.1 Factors Related to a Heavy Burden/Depression Among Family Caregivers of Older Persons with Disabilities
Informal care for the older persons with disabilities has proved to be a heavy burden and source of depression for family caregivers [28,29,30,31,32,33,34,35].
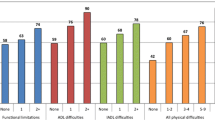
Table 2.1 illustrates the factors related to the burden/depression among family caregivers of the older persons with disabilities in Japan.
2.3.1.1 The Characteristics of the Older Persons Who Are Cared by Their Family Caregivers
Older persons with severe dementia [33, 35], older persons who have behavioral and psychological symptoms of dementia (BPSD) [32,33,34, 36], and older persons of the male sex [34,35,36,37,38,39] show a positive association with an increased risk of burden among family caregivers, while older persons with severe limitations in activities of daily living (ADL) (i.e., bedridden elderly) are less likely to increase the risk of a heavy burden than older persons with light/moderate limited ADL [32]. These findings may be partly explained in the following ways. First, most caregivers are females (e.g., wives, daughters, son’s wives) in Japan. Second, it may be more physically burdensome to care for males than females because males are heavier than females. Second, it may be more difficult to care for male patients with dementia than female patients with dementia when patients have behavioral problems because males are generally physically stronger than females. Third, patients with severe dementia may have many BPSD. Last, older persons with dementia, who have severe limitations of ADL (i.e., bedridden elderly), are not able either to leave their bed in order to use violence on their caregivers or to wander around, while the older persons with dementia, who have light/moderate limitation of ADL, are able to do so.
2.3.1.2 The Characteristics of Family Caregivers
Spouse-caregivers [34, 37, 38], aged caregivers [35,36,37], those with ill health [35, 38, 39], those with chronic diseases [34, 37, 38, 40], and caregivers who are concerned about what others say [37, 40] are more likely to feel a heavier burden than their counterparts, while caregivers who have an adequate income [35] are less likely to feel a heavy burden than their counterparts.
The proportion of the senior citizens (i.e., 65 years old and older) was 27.3% in 2016 [2]. Among the households with senior citizens, 31.1% are households of only a married couple (husband and wife) [2]. Husbands and wives care for their disabled spouses with obligation and love in Japan [7]. However, old spouse-caregivers with chronic diseases may have uneasiness toward health. They may be afraid that there is nobody who will take care of their husbands/wives if they themselves are greatly impacted by their own disease.
Caregivers who are concerned about what others say [37, 40] are more likely to feel a heavier burden than their counterparts. Arai et al. [41, 42] reported that caregivers of the disabled elderly who are concerned about what others think or say were less likely to use public services than those who did not. Those who are concerned about what others say may feel a heavy burden because they hesitate to use social services under LTCIS.
2.3.1.3 The Care Setting
Caregivers who spend a long time with daily caregiving [33,34,35,36,37,38] and those who cannot go out without their charges/ those who have no hours relieved of their duties [33, 34, 38] are more likely to feel a heavier burden than their counterparts, while caregivers who find it convenient to use services [33] are less likely to do so than their counterparts. A heavy burden among caregivers may increase the risk of discontinuation of caregiving [16, 43] or inadequate care (i.e., abuse) [44, 45]. Therefore, we should provide enough social services for the frail elderly and their family caregivers in order to reduce time spent on daily caregiving and to give caregivers hours free from caregiving. Furthermore, caregiver’s concern about what others say deters caregivers from using social services [41, 42]. Education not only for the frail elderly and their caregivers but also for the general population is needed so that anyone can use social services without feeling humiliated.
2.3.2 Factors Related to Ill Health Among Family Caregivers of Older Persons in Japan
Family caregivers are often both physically and mentally burdened with caring for older persons at home [4, 46].
A cross-sectional study was conducted in order to evaluate the factors related to ill health among 344 family caregivers of the older persons with home-visiting nursing services [47]. In this study, a Japanese version of the Center for Epidemiologic Studies Depression (CES-D) scale [48, 49] and a Japanese version of the Zarit Caregiver Burden Interview (J-ZBI) [50,51,52] were used to evaluate the depressive state and burden of family caregivers. Among them, 134 caregivers (39.0%) answered that they were in ill health, while 210 caregivers (61.0%) answered that they were in good health [47]. Caregivers in ill health were older (66.2 ± 12.2 years old vs. 60.6 ± 13.5 years old, p < 0.05) and more depressed (CES-D, 20.5 ± 10.4 vs. 13.5 ± 9.0, p < 0.05) and felt a heavier burden (J-ZBI, 13.5 ± 9.0 vs. 29.2 ± 17.5, p < 0.05) than those in good health [41]. Compared with their counterparts, they were more likely to be spousal caregivers (57.5% vs. 37.1%, p < 0.05) and less likely to be adult children caregivers (25.4% vs. 25.4%, p < 0.05) and were more likely to care for males (52.2% vs. 35.7%, p < 0.05) than those in good health [47]. In addition, family caregivers with ill health are more likely to take care of older persons who have behavioral and psychological symptoms of dementia than their counterparts (33.6% vs. 20.5%, p < 0.05) [47]. Furthermore, home-help service (61.9% vs. 46.2%, p < 0.05) was more commonly used in caregivers in ill health than those in good health. Even after controlling for other factors, depression (odds ratio = 2.04, 95% confidence interval: 1.18–3.57), spousal caregivers (odds ratio = 1.92, 95% confidence interval: 1.19–3.13), caring for older persons who have behavioral and psychological symptoms of dementia (odds ratio = 1.96, 95% confidence interval: 1.14–3.33), and the usage of home-help services (odds ratio = 1.67, 95% confidence interval: 1.03–2.70) were associated with an increased risk of ill health among family caregivers [47]. Since this study was a cross-sectional study, the usage of a home-help service may not be the cause of ill health but the result of ill health among family caregivers. The finding in this study is consistent with the result of the study in Australia [53], which showed an inverse association between well-being and burden as well as a positive association between depression and burden among caregivers of persons with dementia.
Among the community-dwelling Japanese senior citizens (i.e., 65 years old and older), 68.2% of males and 69.1% of female had chronic diseases and attended hospitals as outpatients in 2016, while, among the community-dwelling Japanese advanced elderly persons (i.e., 75 years old and older), 72.5% of males and 73.0% of females did so in 2016 [2]. On the other hand, among the community-dwelling Japanese in their 50s (i.e., 50–59 years old), 41.2% of males and 42.6% of females had chronic diseases and attended hospitals as outpatients in 2016 [2]. Therefore, it may be plausible that older caregivers such as spouse-caregivers are more likely to feel ill health than younger caregivers such as adult child caregivers.
2.3.3 Depressive Rates Among Family Caregivers of the Older People Around the Introduction of Public Long-Term Care Insurance System for the Older People in Japan
The rates of depressed family caregivers of the senior citizens who used home-visiting nursing services around the time of the introduction of the public long-term care insurance system (LTCIS) for the older people were 50.3–56.3% [34, 54] before LTCIS and 34.2–48.4% [34, 35, 54] after LTCIS. The rate of depression among caregivers only slightly decreased after LTCIS compared with the rate before LTCIS. However, the rate of depression is much higher than the rate of depression among the community-dwelling older people (5.3%) [49]. Since a caregiver’s depression is a risk factor for the discontinuation of caregiving [16], care managers and municipal public nurses should take care of not only the older persons with disabilities but also caregivers in order to prevent caregivers’ depression.
Before LTCIS, caregivers who consulted with physicians about their own health (odds ratio = 2.99, 95% confidence interval: 1.60–5.60), those who felt ill health (odds ratio = 5.17, 95% confidence interval: 2.71–9.87), those who cared for older persons who have behavioral and psychological symptoms of dementia (odds ratio = 2.75, 95% confidence interval: 1.44–5.25), and those who attended the elderly more than 16 h/day (odds ratio = 2.77, 95% confidence interval: 1.36–5.67) showed a positive association with the depression of caregivers after controlling for caregiver’s age and sex, district, and life events (e.g., death of family members, divorce, loss of employment) [34]. On the other hand, after LTCIS, caregivers who were spouses (odds ratio = 2.92, 95% confidence interval: 1.42–6.01), those who consulted with physicians about their own health (odds ratio = 4.01, 95% confidence interval: 1.97–8.17), those who felt ill health (odds ratio = 6.19, 95% confidence interval: 2.92–13.12), those who cared for males (odds ratio = 2.79, 95% confidence interval: 1.35–5.74), those who cared for older persons who have behavioral and psychological symptoms of dementia (odds ratio = 2.35, 95% confidence interval: 1.14–4.81), and those who could not go out without accompanying their charges (odds ratio = 2.78, 95% confidence interval: 1.30–5.88) were associated with an increased risk of depression after controlling for caregiver’s age and sex, district, and life events [34].
2.3.4 The Characteristics of the Home-Visiting Nursing Service Users Under the Public Long-Term Care Insurance System
As shown in Table 2.2, home-visiting nursing service users increased from 198,839 in September 2007 to 265,024 in September 2013 [55, 56], which means that the number of home-visiting nursing service users increased by 30% during this period. Among them, almost 50% of the users needed “medication administration and management” by home-visiting nurses, over 30% of users received medical care for their decubitus ulcer, over 10% of users needed care for their bladder dwelling balloon catheter, almost 10% of users had gastric fistula catheters, and over 8% of users needed support for home oxygen therapy. Although the proportion was small, home-visiting nurses took care of the patients with mechanical ventilation, those with intravenous hyperalimentation, and those with chemotherapy for cancer as well.
However, all users cannot use home-visiting nursing services every day. Under LTCIS, the frail elderly have to use the care services for the older peoples according to the Government-Certified Disability Index (GCDI) (i.e., degree of need of care), which means that older persons themselves have to pay 100% of the charge for the usage of services greater than the limits under LTCIS. Therefore, all users cannot use home-visiting nursing services every day, and not a few family caregivers may feel caregiver’s burden because caregivers themselves have to take care of the older persons who need medical care at home after nurses return to the nursing stations.
2.3.5 Caring for Cancer Patients at Home
Cancer is a leading cause of death for the general population as well as for senior citizens in Japan [2]. Cancer patients are often not discharged from hospitals because of severe pain, and pain management is one of the most important factors for the cancer patients to stay at home. Although the proportion was small, home-visiting nurses took care of cancer patients undergoing chemotherapy (0.3–0.5%) as well as cancer patients who need pain control with the medicine (2.6%) [55, 56]. Hashimoto et al. [57] reported that more than half (56%) of cancer patients with home palliative care had severe pain. There may be different responses to the pain medicine between the patients. In their survey, 259 out of 290 cancer patients lived with family [57]. As problems in family care, 116 family members (40%) felt a burden of caregiving, while 41 patients (14%) had no family caregivers. Among 284 patients who were followed until death, 242 patients (85%) died at home [57]. Among these patients who died at home, 238 patients (98%) used home-visiting nursing service, and 127 patients (52%) received strong opioids [57].
Ishi et al. [58] reported that family caregivers who cared for terminal cancer patients at home experienced several difficulties. Cancer patients showed excruciating pain even with pain medicine and difficulty in caring due to the reluctance of using opioids [58]. When there is a difference in opinions between family members as to pain control due to side effects such as sedation by opioids, caregivers may feel difficulties in utilizing nursing interventions. Due to these problems, family caregivers agonized about facing the limitations of caregiving due to increasing pain in the patients [58], which may increase the burden of family caregivers. Some caregivers were modest and hesitated to ask a nurse to come and care for cancer patients at night, while others thought that home-visiting nurses were not trained well enough to care for cancer patients at home [58]. These findings suggest that well-trained home-visiting nurses may play an important role in caring for patients with medical care such as cancer patients at home.
2.4 Discussion
Improvement of public health and advances in medicine after World War II have given Japan one of the highest life expectancies in the world (i.e., 81.0 years for males and 87.1 years for females in 2016) [2]. The number of older people is estimated to increase from 33.9 million in 2015 to 37.8 million in 2035 [2]. On the other hand, live birth rate (per 1000 Japanese population) decreased from 28.1 in 1950 [59] to 7.8 in 2016 [2]. Because the birth rate dropped sharply after the postwar baby boom, population aging is proceeding more rapidly than any other industrialized nation [3]. The increased number of older people led to an increase in the number of the older persons with chronic diseases. As shown in Table 2.3, the proportion of those who have chronic diseases and attend hospitals as outpatients increased from 56.9% for males and 64.5% for females in 1998 [58] to 68.2% for males and 69.1% for females in 2016 [2] among the older people who live in the community in Japan. These findings may suggest that the older people who need medical care increased in the community during these 20 years and will increase from now on for a while.
In 1972, the free medical care programs for the older people started at the national level, and the regular health insurance system raised the coverage ratio to 100% for the older patients, paid for by the Finance Ministry subsidy [3]. Today, however, consumers (the older persons with disabilities) have to pay a 10% nursing service/caring service fee under LTCIS because the coverage ratio is 90% for users [2]. Since financial burden was found to be related to a heavier burden of family caregivers [35], a financial burden may restrain caregivers from using social services. Care managers and municipal public nurses should help family caregivers so that they can use free services such as municipal services and informal services.
Washio et al. [47] found that depression increased the risk of ill health among family caregivers even after controlling for other factors. On the other hand, Oura et al. [34] reported that caregivers who consulted with physicians about their own health had an increased risk of depression, even after controlling for other factors. Since caregiver’s depression increases the risk of the discontinuation of caregiving [16], it may be one of the most important requirements for successful caregiving that the aged caregivers take care of caregivers themselves as well as their aged charges especially when old caregivers care for older persons with disabilities. In order to reduce caregiver’s burden as well as to prevent caregivers’ ill health, municipal public nurses should help family caregivers feel free to use municipal services for the older persons with disabilities.
Spending a long time caring for an older person with disabilities every day is suggested to increase the burden of family caregivers [33,34,35,36,37,38], while having time relieved of their duties is suggested to reduce the burden of family caregivers [33, 34, 38]. In order to reduce caregiver’s burden, care managers should advise family caregivers to use respite care services, which give caregivers a short-term break from their usual care commitment. Informal care provided by other family members, relatives, friends, or neighbors is also helpful to give family caregivers a short time break from their duties as well as to reduce the sense of loneliness among family caregivers, which may also reduce the burden of family caregivers.
In conclusion, in order to promote greater autonomy of the older persons with disabilities as well as to reduce the burden on their family caregivers, LTCIS was launched in Japan. In our studies [34, 35, 54], however, the proportion of depressed family caregivers were 50.3–56.3% before LTCIS and 34.2–48.4% after LTCIS. These findings may suggest that the rate of depressed family caregivers only slightly decreased after LTCIS compared with the rate prior to LTCIS. In Japan, there may be several barriers for the older people and their caregivers to access social services. Some caregivers may hesitate to use social services because they are concerned about what others say under the influence of Confucianism (i.e., children should care for their parents by themselves), while others may abandon their right to use a part of services under LTCIS because they do not have enough money for the co-payment for all care services that they have the right to use under LTCIS. We should remove the barriers for older persons with disabilities and their caregivers to use social services under the LTCIS. Education for the community residents should be recommended so that anyone can use social services without feeling humiliated. In addition, municipal services and/or informal services should be provided when the older people and their caregivers cannot afford to use social service under the LTCIS.
References
Ministry of Health and Welfare. Annual report of health and welfare. Tokyo: Ministry of Health and Welfare; 1978. (In Japanese). http://www.mhlw.go.jp/toukei_hakusho/hakusho/kousei/1978/dl/03.pdf. Accessed 19 Dec 2017
Health, Labour and Welfare Statistics Association. Trend of national health 2017–2018. Tokyo: Health, Labour and Welfare Statistics Association; 2017. (in Japanese)
Cambell JC. How policies change: the Japanese government and the aging society. Princeton: Princeton University Press; 1992.
Maeda D. The outline of new public long-term care insurance program. In: Takagi F, editor. Aging in Japan, vol. 2003. Tokyo: Japan Aging Research Center; 2003. p. 188–91.
Montogomery RJV, Rowe JM, Kosloski K. Family caregiving. In: Blackburn JA, Dulmus CN, editors. Handbook of gerontology: evidence-based approaches to theory, practice, and policy. Hoboken, NJ: John Willey & Sons, Inc.; 2007. p. 426–54.
Barnes M. Caring and social justice. New York: Palgrave Macmillan; 2006.
Ueno C. Sociology of the care, way to the welfare society of the person concerned sovereignty. Tokyo: Ohta Shuppan; 2011. (in Japanese)
Arai Y, Ikegami N. How will Japan cope with the impending surge of dementia? In: Wimo A, Jönsson B, Karlson G, Winblad A, editors. Health economics of dementia. Chichester: John Wiley & Sons; 1998. p. 275–84.
Sung KT (2007). Respect and care for the elderly: the East Asian way, Lanham, MD: University Press of America Inc.
Lee EE, Farran CJ. Depression among Korean, Korean American, and Caucasian American family caregivers. J Transcult Nurs. 2004;15(1):18–25.
Statistics Bureau, Ministry of Internal Affairs and Communications. 2010 national census: the Japanese population and household according to the life-stage. Tokyo: Ministry of Internal Affairs and Communications; 2014. (in Japanese). http://www.stat.go.jp/data/kokusei/2010/life.htm. Accessed 19 Dec 2017
Cabinet Office, Government of Japan. Koureishakai Hakusho 2017 (White paper for the Aged Society 2017). Tokyo: Cabinet Office, Government of Japan; 2017. (in Japanese)
Rabins PV, Fitting MD, Esatham J, et al. Emotional adaptation over time in caregivers for chronically ill elderly people. Age Aging. 1990;19:185–90.
Walker AJ, Acock AC, Bowman SR, et al. Amount of care given and caregiving satisfaction: a latent growth curve analysis. J Gerontol B Psychol Sci Soc Sci. 1996;51(B):130–42.
Barnes CL, Given BA, Given CW. Caregivers of elderly relatives; spouses and adult children. Health Soc Work. 1992;17:282–9.
Arai Y, Sugiura M, Washio M, Miura H, Kudo K. Caregiver depression predicts early discontinuation of care for disabled elderly at home. Psychiatry Clin Neurosci. 2001;55:379–82.
Organisation for Economic Co-operation and Development. The OECD health project, long-term care for older people. Paris: OECD Publishing; 2005. ISBN 92-64-00848-9
Arai Y. Insurance for long-term care planned in Japan. Lancet. 1997;350:1831.
Arai Y, Kudo K, Washio M. Caring for Japan’s elderly. Lancet. 1998;352:1393.
Campen C, Gameren E. Eligibility for long-term care in the Netherlands: development of a decision support system. Health Soc Care Community. 2005;13:287–96.
Tesch-Romer C. Intergenerational solidarity and caregiving. Z Gerontol Geriatr. 2001;34:28–33.
Shimizu Y. Development of public long term care insurance and future direction of the elderly care. In: Takagi F, editor. Aging in Japan, vol. 2003. Tokyo: Japan Aging Research Center; 2003. p. 197–204.
Arai Y, Zarit SH, Kumamoto K, Takeda A. Are there inequities in the assessment of dementia under Japan’s LTC insurance system? Int J Geriatr Psychiatry. 2003;18:346–52.
Yamada M. Characteristic of the care service and policy: comparison between Japan and Germany. In: Nishimura S, editor. Iryohakusho (Annual report of medical care). Tokyo: Nihon-iryo-kikaku; 1998. p. 45–73. (in Japanese).
Ham IW. Long-term care insurance system of South Korea: achievements and issues at the point of one year from enforcement. Hyoron Shakaikagaku (Soc Sci Rev). 2010;90:75–97. (in Japanese)
Mikami F. Welfare services for the elderly. In: Maruo N, Shionoya Y, editors. Social security system of the advanced countries, social security in Sweden. Tokyo: University of Tokyo Press; 1999. p. 253–74. (in Japanese).
Fratiglioni L, Paillard-Borg S, Winblad B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 2004;3:343–53.
Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20:649–55.
Montgomery RJV, Gonyea JG, Hooyman NR. Caregiving and experience of subjective and objective burden. Fam Relat. 1985;34:19–26.
Fitting M, Rabins P, Lucas MJ, Eastham J. Caregivers for dementia patients: a comparison of husband and wives. Gerontologist. 1986;26:248–52.
Gallagher D, Rose J, Rivera P, Lovett S, Thompson LW. Prevalence of depression in family caregivers. Gerontologist. 1989;29:449–56.
Arai Y, Washio M. Burden felt by family caring for the elderly members needing care in southern Japan. Aging Ment Health. 1999;3:158–64.
Arai Y, Kumamoto K, Washio M, Ueda T, Miura H, Kudo K. Factors related to feelings of burden among caregivers looking after impaired elderly in Japan under the Long-Term Care Insurance System. Psychiatry Clin Neurosci. 2004;58:396–402.
Oura A, Washio M, Arai Y, Ide S, Yamasaki R, Wada J, Kuwahara Y, Mori M. Depression among caregivers of the frail elderly in Japan before and after the introduction of the public long-term care insurance system. Z Gerontol Geriatr. 2007;40:112–8.
Arai Y, Kumamoto K, Mizuno Y, Washio M. Depression among family caregivers of community-dwelling older people who used services under the long term care insurance program: a large-scale population-based study in Japan. Aging Ment Health. 2014;18(1):81–91.
Washio M, Nogami Y, Motoyama S, Yamasaki R, Horiguchi I, Toyoshima Y. Burden among family caregivers of the elderly in need of care and factors related to their burden before and after the revision of public long-term care insurance system. Rinsho To Kenkyu. 2015;92(10):1311–6. (in Japanese)
Toyoshima Y, Washio M, Horiguchi I, Yamasaki R, Onimaru M, Nakamura K, Miyabayashi I, Arai Y. Undue concern for other’s opinion is related to depression among family caregivers disabled elderly in southern Japan. Int Med J. 2016;23(1):30–3.
Washio M, Arai Y, Izumi H, Mori M. Burden on family caregivers of frail elderly persons one year after the introduction of public long term care insurance service in the Onga District, Fukuoka Prefecture: evaluation with a Japanese version of the Zarit caregiver burden interview. Nihon Ronen Igaku Zasshi. 2003;40:147–55. (in Japanese)
Washio M, Oura A, Arai Y, Mori M. Depression among caregivers of the frail elderly, three years after the introduction of public long-term care insurance for the elderly. Int Med J. 2003;10:179–83.
Washio M, Takeida K, Arai Y, Shang E, Oura A, Mori M. Depression among caregivers of the frail elderly with visiting nursing services in the northernmost city of Japan. Int Med J. 2015;22(4):250–3.
Arai Y, Sugiura M, Miura H, Washio M, Kudo K. Undue concern for other’s opinions deters caregivers of impaired elderly from using public services in rural Japan. Int J Geriatr Psychiatry. 2000;15:961–8.
Arai Y, Washio M, Miura H, Kudo K. Dementia care in Japan: insurance for long term care legislation in Japan. Int J Geriatr Psychiatry. 1998;13:572–3.
Arai Y, Zarit SH, Sugiura M, Washio M. Patterns of outcome of caregiving for the impaired elderly: a longitudinal study in rural Japan. Aging Ment Health. 2002;6(1):39–46.
Ueda T. Inadequate care by family caregiver of frail elderly living at home. Nihon Koshu Eisei Zassgi. 2000;47(3):264–74. (in Japanese)
Nitta J, Kumamoto K, Arai Y. Burden felt by family caregivers of the elderly registered with visiting nurses’ stations in Kyoto. Nihon Ronen Igaku Zasshi. 2005;42:181–5. (in Japanese)
Arai Y, Zarit SH. Exploring strategies to alleviate caregiver burden: effects of the national long-term care insurance scheme in Japan. Psychogeriatrics. 2011;11(3):183–9.
Washio M, Toyoshima Y, Arai Y. Factors related to ill health among family caregivers of the older people. 17th Annual Meeting of Japan Society of Health Promotion, Nisshin City, Aichi Prefecture, Japan, Feb 2016. (in Japanese).
Radloff L. The CES-D scale: a self-reported depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Ihara K. Depressive states and their correlates in elderly people in a rural community. Nihon Koshu Eisei Zasshi. 1993;40(2):85–94. (in Japanese)
Zarit SH, Zarit JM. The memory and behavior problems checklist-1987R and the burden interview. Philadelphia, PA: Pennsylvania University; 1987.
Arai Y. The Japanese version of the Zarit Caregiver Burden Interview (J-ZBI). Nippon Rinsho. 2011;69(8):459–63. (in Japanese)
Arai Y, Kudo K, Hosokawa T, Washio M, Miura H, Hisamichi S. Reliability and validity of the Japanese version of the Zarit Caregiver Burden Interview. Psychiatry Clin Neurosci. 1997;51:281–7.
McConaghy R, Caltabiano ML. Caring for a person with dementia: exploring relationships between perceived burden, depression, coping and well-being. Nurs Health Sci. 2005;7:81–91.
Washio M, Arai Y, Oura A, et al. Care burden and depression among caregivers of the frail elderly with home-visiting nursing service before and after the introduction of the public long-term care insurance for the elderly: the findings from the studies until the fifth year of the insurance system. Rinsho To Kenkyu. 2005;82:1366–70. (in Japanese)
Ogino H, Toyoshima Y, Haruna S, Moriyama H, Matsuda S, Washio M. Factors related to a heavy burden among family caregivers of the frail elderly who use home-visit nursing care services in rural area of the Tokai region. Rinsho To Kenkyu. 2017;94(12):1557–62. (in Japanese)
Portal Site of Official Statistics of Japan (e-Stat). Number of clients who use home-visiting nursing care, details of nursing services in September, degree of need of care. In: Ministry of health, labour and welfare. National survey of nursing-care service facilities; 2017. (in Japanese). http://www.estat.go.jp. Accessed 06 Dec 2017.
Hashimoto K, Sato K, Uchiumi J, et al. Current home palliative care for terminally ill cancer patients in Japan. Palliat Care Res. 2015;10(1):153–61. (in Japanese)
Ishi Y, Miyashita M, Sato K, Ozawa T. Difficulties in caring for terminal cancer patients at home: family caregivers’ and homecare providers’ perspectives. Nihon Gan Kango Gakkaishi. 2011;25(1):24–36. (in Japanese)
Health and Welfare Statistics Association. Trend of national health 2000. Tokyo: Health and Welfare Statistics Association; 2000. (in Japanese)
Health and Welfare Statistics Association. Trend of national health 2004. Tokyo: Health and Welfare Statistics Association; 2004. (in Japanese)
Health and Welfare Statistics Association. Trend of national health 2010–2011. Tokyo: Health and Welfare Statistics Association; 2010. (in Japanese)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Washio, M., Toyoshima, Y., Miyabayashi, I., Arai, Y. (2019). Burden Among Family Caregivers of Older People Who Need Care in Japan. In: Washio, M., Kiyohara, C. (eds) Health Issues and Care System for the Elderly. Current Topics in Environmental Health and Preventive Medicine. Springer, Singapore. https://doi.org/10.1007/978-981-13-1762-0_2
Download citation
DOI: https://doi.org/10.1007/978-981-13-1762-0_2
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1761-3
Online ISBN: 978-981-13-1762-0
eBook Packages: MedicineMedicine (R0)