Abstract
Lung cancer is a major cause of cancer-related death in Japan, and the overall survival rate was still poor. The majority of individuals diagnosed with lung cancer are elderly people aged ≥65 years. Although chronic inhalation of cigarette smoke is a major risk factor to the development of lung cancer, genetic factors have been implicated to account for some of the observed differences in lung cancer susceptibility. A number of studies have examined lung cancer susceptibility based on the presence of high-frequency, low-penetrance genetic polymorphisms. As exposure to harmful chemicals or reactive oxygen species via cigarette smoking is thought to contribute to the development of lung cancer, genetic polymorphisms involved in xenobiotic metabolism, DNA repair, and inflammation might be promising candidates. In order to evaluate whether the impact of genetic polymorphisms on lung cancer differs between elderly and younger people, we evaluated potential 31 genetic polymorphisms in a stratified analysis by age category (aged ≥65 and <65 years). Seven polymorphisms, namely, CYP1A1 rs4646903, CYP1A1 rs1048943, GSTM1 deletion, GSTP1 rs1695, SULTA1 rs9282861, TP53BP1 rs560191, and CRP rs2794520, were associated with lung cancer risk in the elderly. However, there was little difference in the impact of polymorphism on lung cancer risk between the elderly and non-elderly groups. In this chapter, we would like to discuss the importance of the prevention of smoking (the best established and strongest avoidable risk factor) at early age for successful aging.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
11.1 Introduction
Improvement of public health and advances in medicine after World War II have given Japan one of the highest average life expectancies in the world (i.e., 81.0 years old for men and 87.1 years old for women in 2016), and the proportion of the elderly (people aged ≥65 years) increased from 4.9% in 1950 to 27.3% in 2016 [1]. Increased life expectancy means the increased number of the elderly who need medical care.
Tobacco smoking is the largest single recognized cause of human cancer in Western countries [2]. Cigarette smoking alone account for about 30% of all cancer deaths in the United States and an estimated 16% of all cancers worldwide [2]. Tobacco smoking is associated with an increased risk of malignancies of both organs in direct contact with smoke, such as the esophagus and lung, and organs not in direct contact with smoke, such as the kidneys [3].
As shown in Table 11.1, cancer has been the leading cause of death in Japan since 1981 and is the major causes of death for over three decades in Japan [1]. Cerebrovascular diseases (CVD) were the leading cause of death for three decades before 1980. Heart disease deaths outnumbered CVD deaths for 1985–2016 except for the period from 1995 to 1996. Infectious diseases [tuberculosis (predominantly lung tuberculosis), pneumonia, bronchitis, gastroenteritis] were the major cause of death in Japan before 1950. As of 2016, lung cancer is the first cause of cancer death for men and the second cause of cancer death for women in an all Japanese population [1]. Table 11.2 illustrates that lung cancer mortality rate among men (242.4 per 100,000) is also the highest among all site-specific cancer death rates in the elderly (people aged ≥65 years) in Japan [1].
Lung cancer has become the most frequent malignant neoplasm among men in most countries, and a parallel increase in incidence is seen among women in Western countries although lung cancer was a rare disease before the beginning of the twentieth century [4]. As shown in Table 11.3, tobacco smoking increases the risk of lung cancer, while a diet rich in fruits and vegetables has a protective effect against lung cancer [4,5,6]. Washio et al. [7] conducted a case-control study in Hokkaido, Northern Japan, and found that current smokers (vs. non-smokers, odds ratio (OR) = 4.65, 95% confidence intervals (CI) = 2.17–9.97) and old age (65 years old and over vs. 40–64 years old, OR = 2.31, 95% CI = 1.41–3.80) increased the risk of lung cancer, and short sleeping time (5 h/day or less vs. 6 h/day or more, OR = 2.47, 95% CI = 0.97–6.32) showed a nonsignificantly increased lung cancer risk after controlling age, sex, and smoking status [7]. On the other hand, never smokers (vs. ex-smokers, OR = 0.28, 95% CI = 0.14–0.56), high intake of green tea (7 cups/day and over vs. 0–6 cups/day, OR = 0.38, 95% CI = 0.14–0.995), and frequent consumption of green and yellow vegetables (4 days/week vs. 0–3 days/week, OR = 0.46, 95% CI = 0.26–0.81) reduced the risk of lung cancer after controlling age, sex, and smoking status [5].
Since our health status in the later life is influenced by the life experience throughout life, health promotion from pregnancy and childhood to old age is important to avoid unhealthy aging. We should remember not only tobacco smoking but also exposure to environmental tobacco smoke increases the risk of cancer [5].
11.2 Case-Control Study to Investigate Association Between Genetic Polymorphism and Lung Cancer Risk
11.2.1 Background
Although tobacco smoking is a convincing risk factor for lung cancer, approximately one in ten smokers develops lung cancer in their lifetime indicating an interindividual variation in susceptibility to tobacco smoking [8]. Individuals may have a unique combination of polymorphic traits that modify genetic susceptibility and response to tobacco smoking. Chemical substances in tobacco smoke must be metabolically activated to exert their noxious effects by phase I enzymes, but this is counteracted by the ongoing detoxification of activated substances (carcinogens in most situations) by phase II enzymes. Therefore, DNA damage itself is a balance between phase I and II metabolic enzymes, many of which are polymorphic. The capacity to repair DNA damage induced by activated carcinogens is also a genetic factor that may affect lung cancer risk. Furthermore, exposure to reactive oxygen species (ROS) via cigarette smoking is thought to contribute to the development of lung cancer [9]. Phase I enzymes contribute to the formation of ROS, whereas phase II enzymes play a critical role in the detoxification and reduction of ROS [10]. Chronic inflammation has been implicated in the development of several human malignancies, including lung cancer [11]. Pulmonary inflammation may promote tumor formation by the generation of ROS and secretion of cytokines, chemokines, and pro-angiogenic factors [12]. Lung cancer susceptibility may be associated with genetic polymorphisms involved in the inflammatory response.
The primary advantage of genetic markers is to allow the identification of a high-risk group for lung cancer and guide individualized therapy. Thus, reliable genetic markers for lung cancer are urgently required. It has been hypothesized that the rise in cancer diagnosis for elderly persons may be due to DNA damage by ROS [13]. In this chapter, we reanalyzed the data from our case-control studies [14,15,16,17,18,19,20,21] limited to elderly people aged 65 years and over, with special reference to genetic polymorphisms involved in xenobiotic metabolism, DNA repair, and inflammation. For comparison, the same polymorphisms among the non-elderly population (<65 years) were determined.
11.2.2 Materials and Methods
11.2.2.1 Study Subjects and Data Collection
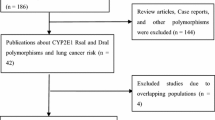
Lung cancer patients were enrolled in Kyushu University Hospital (Research Institute for Diseases of the Chest, Kyushu University) and its collaborating hospitals. The suitable cases (n = 462) were patients with primary lung cancer that were newly diagnosed and histologically confirmed during the period from 1996 to 2008. The participation rate among the cases was 100%. Histological types were categorized into four major types according to the International Classification of Diseases for Oncology (ICD-O), second edition: adenocarcinoma (8140, 8211, 8230–8231, 8250–8260, 8323, 8480–8490, 8550–8560, 8570–8572), squamous cell carcinoma (8050–8076), small cell carcinoma (8040–8045), and large cell carcinoma (8012–8031, 8310). Controls (n = 379) were the hospitalized patients without clinical history of any type of malignancy, ischemic heart disease, or chronic respiratory disease during the same period. Controls were not, individually or in larger groups, matched to cases. Controls were approached by their attending physicians to be recruited as control subjects. None of the controls refused to participate in this study. A self-administered questionnaire was used to collect data on demographic and lifestyle factors such as age, years of education, smoking, alcohol consumption, environmental tobacco exposure from spouse, etc. All subjects were unrelated ethnic Japanese. The details have been described elsewhere [14,15,16,17,18,19,20,21]. The study subjects were stratified by age group, namely, the elderly group (people aged ≥65 years, 303 cases and 114 controls) and the non-elderly group (people aged <65 years, 159 cases and 265 controls). A total of 462 cases and 379 controls were included in this analysis.
The study protocol was approved by our institutional review board, and all participants were provided written informed consent.
11.2.2.2 Genetic Analysis
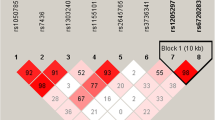
Genomic DNA was extracted from blood samples. Genotyping of 31 polymorphisms (xenobiotic metabolism, CYP1A1 rs464903, CYP1A1 rs1048943, CYP1A2 rs76551, CYP1A2 rs2069514, CYP2A6 deletion, CYP2A13 rs8192789, CYP2E1 rs2031920, MPO rs2333227, GSTM1 deletion, GSTT1 deletion, GSTP1 rs1695, NQO1 rs1800566, SULT1A1 rs9282861, NAT2 genotypes determined by NAT2*4, *5B, *6A, or *7B allele; DNA repair, ERCC2 rs13181, XRCC1 rs25487, AXRCC3 rs861539, OGG1 rs1052113, TP53 rs1042522, TP53BP1 rs560191; and inflammation, IL1B1 rs1143634, IL6 rs1800796, IL8 rs4073, IL10 rs180871, IL13 rs1800925, CRP rs2794520, NOS2 rs2297518, CYBA rs4673, TNFA rs1799724, TNFRA2 rs1061622, NFkB rs283649) was conducted with blinding to case-control status. The details of the methods have been described elsewhere [14,15,16,17,18,19,20,21]. For quality control, both assays were repeated on a random 5% of all samples, and the replicates were 100% concordant.
11.2.2.3 Statistical Analysis
Comparisons of means, proportions, and medians were based on the unpaired t test, χ 2 test, and Wilcoxon rank-sum test, respectively. The distribution of the genotypes of polymorphisms in controls was compared with that expected from Hardy-Weinberg equilibrium (HWE) by the chi-square (Pearson) test. Unconditional logistic regression was used to compute the ORs and their 95% CIs, with adjustments for several covariates. Subjects were considered current smokers if they smoked or stopped smoking less than 1 year before either the date of diagnosis of lung cancer or the date of completion of the questionnaires (controls). Never smokers were defined as those who had never smoked in their lifetime. Former smokers were those who had stopped smoking 1 or more years before either the date of diagnosis of lung cancer or the date of completion of the questionnaires (controls).
Based on “Healthy Japan 21” (National Health Promotion in the twenty-first century), heavy drinkers were defined as those who drank more than 60 g of alcohol per day. As “Healthy Japan 21” has emphasized drinking an appropriate volume of alcohol (20 g of alcohol per day), appropriate drinkers were defined as those who did not exceed 20 g of alcohol intake per day. The appropriate volume of alcohol use may have a protective effect on life expectancy and morbidity [22]. Unlike cigarette smoke, ingested alcohol is eliminated from the body by various metabolic mechanisms, and the alcohol elimination process begins almost immediately. Significant relationships between excessive drinking and lung cancer have been reported, while appropriate drinking has not shown the same effects [23]. In terms of alcohol consumption, the subjects were classified into the following three groups based on their intake for at least 1 year: those who drank more than 60 g of alcohol per day (heavy drinkers), those who drank more than 20 g of alcohol per day but not exceeding 60 g per day (moderate drinkers), and those who drank less than 20 g of alcohol per day (appropriate drinkers). Appropriate drinkers included infrequent and nondrinkers because the lung cancer risks were comparable among them [17].
Genotype impact was assessed by a score test for each genotype as follows: (0) homozygous for the major allele, (1) heterozygous, and (2) homozygous for the minor allele. All statistical analyses were performed using the computer program STATA Version 14.2 (STATA Corporation, College Station, TX). All P values were two-sided, with those less than 0.05 considered statistically significant.
11.2.3 Results
11.2.3.1 Characteristics of Study Subjects
Table 11.4 summarizes the distributions of selected characteristics among subjects [14,15,16,17,18,19,20,21]. As controls were not selected to match lung cancer patients on age and sex, there were significant differences in age (P < 0.001) between lung cancer patients and controls in both the elderly and non-elderly groups. Sex ratio was significantly different between cases and controls in the non-elderly group (P = 0.001). Compared with control subjects, lung cancer patients were more likely to report a history of smoking in the both groups (P < 0.001). Pack-years of smoking were significantly different between cases and controls in the two groups. We excluded pack-years (the number of packs of cigarettes smoked/day multiplied by years of smoking) from the logistic models because of high correlation with age (avoiding the problem of potential collinearity). Compared with control subjects, lung cancer patients were more likely to report a history of alcohol drinking in the non-elderly group (P = 0.001).
11.2.3.2 Association Between Genetic Polymorphisms Involved in Xenobiotic Metabolism and Lung Cancer Risk
The genotype frequencies of 14 polymorphisms were consistent with Hardy-Weinberg equilibrium (HWE) among controls, except for CYP2E1 rs2031920 (P = 0.016) in the elderly group (data not shown). As shown in Table 11.5 [14, 15, 18, 20, 24, 25], the minor homozygotes of CYP1A1 rs4646903 (OR = 2.36, 95% CI = 1.13–4.94) were significantly associated with an increased lung cancer risk even after adjustment for age, sex, education, smoking status, and drinking status. With the increasing number of the C allele, there was a significant trend of higher risk of lung cancer (P trend = 0.019). The null genotype of the GSTM1 deletion polymorphism was at a 1.61-fold (95% CI = 1.01–2.55) increased risk of lung cancer. CYP1A1 rs1048943 (OR = 1.64, 95% CI = 1.03–2.62), GSTP1 rs1695 (OR = 2.25, 95% CI = 1.29–3.92), and SULT1A1 rs9282861 (OR = 1.64, 95% CI = 1.001–2.69) were associated with lung cancer risk under a dominant genetic model.
Subjects aged <65 years based on 159 cases and 365 controls were genotyped for comparison. There was somewhat difference in the impact of polymorphism on lung cancer risk between subjects aged ≥65 years and those <65 years. Unlike with the results from elderly, CYP2A6 deletion, NQO1 rs1800566, and NAT2 polymorphisms were significantly associated with lung cancer risk. GSTM1 deletion and GSTP1 rs1695 polymorphisms were not significantly associated with lung cancer risk. As there was an overlap between the CIs of the ORs for each polymorphism in the two groups, it can be assumed that there is no statistically significant difference in the ORs between the two groups.
11.2.3.3 Association Between Genetic Polymorphisms Involved in DNA Repair and Lung Cancer Risk
The genotype frequencies of six polymorphisms were all in agreement with the HWE in controls (data not shown). As shown in Table 11.6 [16, 18, 24], only TP53BP1 rs560191 was significantly associated with lung cancer risk. The ORs of lung cancer for the Glu/Glu genotype and Asp/Glu genotype were 0.40 (95% CI = 0.20–0.80) and 0.56 (95% CI = 0.33–0.95), respectively. Decreasing numbers of the Asp allele decreased lung cancer risk in a dose-dependent manner (P trend = 0.006). A statistically significant decreased lung cancer risk was found under dominant model (OR = 0.51, 95% CI = 0.31–0.85).
Unlike with the results from elderly, ERCC2 rs13181 and XRCC1 rs25487 polymorphisms were significantly associated with lung cancer risk among subjects aged <65 years. As there was an overlap between the CIs of the ORs for each polymorphism, the differences are not statistically significant.
11.2.3.4 Association Between Genetic Polymorphisms Involved in Inflammation and Lung Cancer Risk
The genotype frequencies of 11 polymorphisms were in agreement with the HWE in controls, except for CYBA rs4673 in the elderly group (P = 0.039) and IL1B1 rs1143634 in the non-elderly group (P = 0.028). Table 11.7 illustrates association between genetic polymorphisms involved in inflammation and lung cancer risk [17, 19, 21, 26]. The CT genotype of CRP rs2794520 (OR = 1.67, 95% CI = 1.02–2.73) was significantly associated with an increased risk of lung cancer. A statistically significant increased lung cancer risk was found under dominant model (OR = 1.73, 95% CI = 1.09–2.76). A dose-dependent relationship (P trend = 0.024) was revealed between number of the C (T) allele and lung cancer risk. There was little difference in the impact of polymorphism on lung cancer risk between elderly and non-elderly subjects.
11.2.4 Discussion
The selected 31 polymorphisms involved in xenobiotic metabolism, DNA repair, and inflammatory response were determined in a total of 417 elderly subjects (303 lung cancer cases and 114 controls) and 424 non-elderly subjects (159 lung cancer patients and 265 controls). Seven polymorphisms, namely, CYP1A1 rs4646903, CYP1A1 rs1048943, GSTM1 deletion, GSTP1 rs1695, SULTA1 rs9282861, TP53BP1 rs560191, and CRP rs2794520, were associated with lung cancer risk in the elderly group. CYP2E1 rs2031920 and CYBA rs4673 in elderly controls and IL1B1 rs1143634 in non-elderly controls deviated from HWE.
In our previous case-control studies [14, 16,17,18,19, 21, 27, 28], the minor homozygotes of CYP1A1 rs4646903 (OR = 2.63, 95% CI = 1.61–4.28), CYP1A1 rs1048943 (OR = 2.86, 95% CI = 1.54–5.32), GSTP1 rs1695 (OR = 3.22, 95% CI = 1.12–9.30), CRP rs2794520 (OR = 1.92, 95% CI = 1.10–3.38), and TP53BP1 rs560191 (OR = 0.46, 95% CI = 0.29–0.74) were significantly associated with an increased lung cancer risk in the whole population (462 lung cancer cases and 379 controls). Similarly, the null genotype of the GSTM1 deletion polymorphism was at a 1.38-fold (95% CI = 1.01–1.89) increased risk of lung cancer 1.38 (1.01–1.89) in the whole population. Although the authors did not report the association between SULT1A1 rs9282861 and lung cancer risk, SULT1A1 rs9282861 was associated with lung cancer risk under dominant model (OR = 1.33, 95% CI = 1.00–1.76, P = 0.05) in a recent meta-analysis [29]. The observed ORs of lung cancer for these polymorphisms were consistent with those from a considerable amount of studies, including our previous studies, but attenuated due to a reduced sample size. Basically, the impact of selected genetic polymorphisms on lung cancer may be similar between the elderly population and the non-elderly population. Our findings suggest the impact of selected genetic polymorphisms on lung cancer is independent of age.
Departure from HWE can imply the presence of selection bias (lack of representation of the general population) in this population because this study was free from the possibility of genotyping error (e.g., systematic misgenotyping of heterozygotes as homozygotes or vice versa or nonrandomness of missing data), assay nonspecificity, or possible population admixture/stratification [30, 31]. The Japanese population sample could be expected to have a relatively low risk of population stratification effects [32, 33] in comparison to Caucasian populations that have a geographically broader-based inheritance. The deviation from HWE is most likely due to chance. For example, no controls had the TT genotype of CYP2E1 rs2031920 in this study. If one control had possessed the TT genotype, there was no longer a deviation from HWE in controls (P = 0.053). On the other hand, two controls had the TT genotype of CYBA rs4673. If one control had possessed the TT genotype, there was no longer a deviation from HWE in controls (P = 0.359). It is plausible that the deviation from HWE was due to chance in this study.
Understanding the genetic basis of complex diseases has been increasingly emphasized as a means of achieving insight into disease pathogenesis, with the ultimate goal of improving preventive strategies, diagnostic tools, and therapies. Case-control genetic association studies such as ours aim to detect association between genetic polymorphisms and disease. Although case-control genetic association studies can measure statistical associations, they cannot test causality. Determining genetic causation of disease is a process of inference, which requires supportive results from multiple association studies and basic science experiments combined. Furthermore, a concern with respect to genetic association studies has been lack of replication studies, especially contradictory findings across studies. Replication of findings is very important before any causal inference can be drawn. Testing replication in different populations is an important step. Additional studies are warranted to replicate our and others’ findings from case-control genetic association studies.
In summary, CYP1A1 rs4646903, CYP1A1 rs1048943, GSTM1 deletion, GSTP1 rs1695, SULTA1 rs9282861, TP53BP1 rs560191, and CRP rs2794520 were associated with lung cancer risk in the elderly population. The impact of selected genetic polymorphisms on lung cancer is independent of age. Future studies involving larger control and case populations will undoubtedly lead to a more thorough understanding of the role of genetic polymorphisms in lung cancer development among elderly.
11.3 Conclusion
Our health status in the later life is influenced by the life experience throughout life. Therefore, health promotion to reduce the risk of chronic diseases such as cancers is important to obtain healthy aging. Lung cancer is the most common cancer worldwide [34], which is the leading cause of cancer death in Japan [1].
Similar to the population as a whole, to adequately control risk factors for lung cancer, such as avoiding the exposure of harmful cigarette smoke and increasing fruits consumption [4,5,6] (Table 11.3), might be linked to a healthy life and/or a longer life expectancy of the elderly. For example, even a 60-year-old cigarette smoker could gain at least 3 years of life expectancy by stopping [35]. It is accepted that oxidative damage contributes greatly to the aging process and the development of various diseases [36]. Antioxidants can decrease the oxidative damage by reacting with free radicals or by inhibiting their activity. Fruits are a source of vitamin C and other antioxidants such as carotenoids, flavonoids, and polyphenols. Therefore, fruits can be used to benefit human health issues related to retarding aging (increase in life expectancy). Due to prolonging life expectancy and the increased risk of lung cancer with aging, lung cancer is common in the elderly. As lung cancer has a relatively long latency period from the time of initial exposure to the onset of symptoms, anti-smoking education programs should be introduced at an early age.
In addition to primary prevention, secondary prevention (i.e., early detection of asymptomatic lung cancer) is also important for our good health status in the later life. Among both men and women, the incidence of lung cancer is low in persons under age 45 and increases with age [4]. Therefore, screening for lung cancer after the middle ages is important to detect asymptomatic lung cancer as well as to avoid unhealthy aging.
Krabbe and Lotan suggested to us that newly diagnosed bladder cancer patients should also be screened for lung cancer because a small number (i.e., 4–5%) of bladder cancer patients were also diagnosed with lung cancer [37]. As bladder cancer and lung cancer have shared risk factors (i.e., tobacco smoking [8] and arsenic in drinking water [38]) and inherited susceptibility (i.e., GSM1 deletion polymorphism and NAT2 [39]) and lung cancer is the most common death from cancer, it is appropriate that Krabbe and Lotan recommend urologists to advise bladder cancer patients to undergo screening of lung cancer [40]. Therefore, we should advise patients with smoking-related cancers other than lung cancer to undergo screening for lung cancer because tobacco smoking is associated with an increased risk of malignancies of both organs in direct contact with smoke and organs not in direct contact with smoke [3].
In addition to environmental factors, a substantial number of genetic polymorphisms have been determined as possible risk factors for lung cancer [41,42,43]. Global estimates suggest that approximately 25% of lung cancer cases worldwide occur among never smokers [44, 45]. Family history has been reported a simple proxy for genetic risk and is influenced by both shared and individual environmental exposures [46]. Understanding the underlying genetic factors will have a high degree of availability for clarifying the etiology of lung cancer and in identifying high-risk individuals for targeted screening and/or prevention based on a combination of genetic and environmental factors in the elderly population as well as the population as a whole.
In the end, the impact of genetic factors on lung cancer may be unrelated to age. Tobacco smoking is the best established and strongest avoidable risk factor for lung cancer. Although tobacco smoking is associated with an increased risk of malignancies of both organs in direct contact with smoke and organs not in direct contact with smoke [3] as well as an increased risk of cardiovascular diseases or chronic obstructive pulmonary disease [47], more than 30% of Japanese boys experienced tobacco smoking before becoming junior high school students [48, 49], and more than 10% of Japanese girls did so before becoming senior high school students [49]. As healthy aging is a lifelong process, anti-smoking education from an early age and the prevention of tobacco smoking throughout the lifetime are important for healthy aging.
References
Health, Labour and Welfare Statistics Association. Trend of national health 2017/2018. Tokyo: Health, Labour and Welfare Statistics Association; 2017 (in Japanese).
Thun MJ, Henley SJ. Tobacco. In: Schottenfeld D, Fraumeni Jr JF, editors. Cancer epidemiology and prevention. New York: Oxford University Press; 1996. p. 217–42.
Gajalakshmi CK, Jha P, Ranson K, Nguyen S. Global patterns of smoking and smoking-attributable mortality. In: Jha P, Chalouplca F, editors. Tobacco control in developing countries. New York: Oxford University Press; 2000. p. 11–39.
Boffetta P, Trichopoulos D. Cancer of the lung, larynx, and pleura. In: Adami HO, Hunter D, Trichopoulos D, editors. Text of cancer epidemiology. New York: Oxford University Press; 2002. p. 248–80.
World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington, DC: AICR/WCRF; 2007.
http://epi.ncc.go.jp/files/02_can_prev/matrix_170801JP.pdf (ver. 20170801).
Washio M, Tanaka Y, Inomata S, Takahashi H, Saitoh S, Miura T, et al. Smoking increases the risk of lung cancer while green tea and green and yellow vegetables reduces the risk: a case-control study of lung cancer in Hokkaido. Rinsho To Kenkyu. 2016;93(1):93–6 (in Japanese).
Doll R, Peto R. The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. J Natl Cancer Inst. 1981;66(6):1191–308.
Tafani M, Sansone L, Limana F, Arcangeli T, De Santis E, Polese M, et al. The interplay of reactive oxygen species, hypoxia, inflammation, and sirtuins in cancer initiation and progression. Oxidative Med Cell Longev. 2016;2016:3907147. https://doi.org/10.1155/2016/3907147.
Nebert DW. Role of genetics and drug metabolism in human cancer risk. Mutat Res. 1991;247(2):267–81.
Bartsch H, Nair J. Chronic inflammation and oxidative stress in the genesis and perpetuation of cancer: role of lipid peroxidation, DNA damage, and repair. Langenbeck’s Arch Surg. 2006;391(5):499–510. https://doi.org/10.1007/s00423-006-0073-1.
Smith CJ, Perfetti TA, King JA. Perspectives on pulmonary inflammation and lung cancer risk in cigarette smokers. Inhal Toxicol. 2006;18(9):667–77. https://doi.org/10.1080/08958370600742821.
Barrera G. Oxidative stress and lipid peroxidation products in cancer progression and therapy. ISRN Oncol. 2012;2012:137289. https://doi.org/10.5402/2012/137289.
Kiyohara C, Yamamura KI, Nakanishi Y, Takayama K, Hara N. Polymorphism in GSTM1, GSTT1, and GSTP1 and susceptibility to lung cancer in a Japanese population. Asian Pac J Cancer Prev. 2000;1(4):293–8.
Kiyohara C, Takayama K, Nakanishi Y. CYP2A13, CYP2A6, and the risk of lung adenocarcinoma in a Japanese population. J Health Sci. 2005;51(6):658–66. https://doi.org/10.1248/jhs.51.658.
Kiyohara C, Horiuchi T, Miyake Y, Takayama K, Nakanishi Y. Cigarette smoking, TP53 Arg72Pro, TP53BP1 Asp353Glu and the risk of lung cancer in a Japanese population. Oncol Rep. 2010;23(5):1361–8.
Kiyohara C, Horiuchi T, Takayama K, Nakanishi Y. IL1B rs1143634 polymorphism, cigarette smoking, alcohol use, and lung cancer risk in a Japanese population. J Thorac Oncol. 2010;5(3):299–304. https://doi.org/10.1097/JTO.0b013e3181c8cae3.
Kiyohara C, Horiuchi T, Takayama K, Nakanishi Y. Genetic polymorphisms involved in carcinogen metabolism and DNA repair and lung cancer risk in a Japanese population. J Thorac Oncol. 2012;7(6):954–62. https://doi.org/10.1097/JTO.0b013e31824de30f.
Kiyohara C, Horiuchi T, Takayama K, Nakanishi Y. Genetic polymorphisms involved in the inflammatory response and lung cancer risk: a case-control study in Japan. Cytokine. 2014;65(1):88–94. https://doi.org/10.1016/j.cyto.2013.09.015.
Kakino K, Kiyohara C, Horiuchi T, Nakanishi Y. CYP2E1 rs2031920, COMT rs4680 polymorphisms, cigarette smoking, alcohol use and lung cancer risk in a Japanese population. Asian Pac J Cancer Prev. 2016;17(8):4063–70.
Yamamoto Y, Kiyohara C, Suetsugu-Ogata S, Hamada N, Nakanishi Y. Biological interaction of cigarette smoking on the association between genetic polymorphisms involved in inflammation and the risk of lung cancer: a case-control study in Japan. Oncol Lett. 2017;13(5):3873–81. https://doi.org/10.3892/ol.2017.5867.
Holman CD, English DR, Milne E, Winter MG. Meta-analysis of alcohol and all-cause mortality: a validation of NHMRC recommendations. Med J Aust. 1996;164(3):141–5.
Benedetti A, Parent ME, Siemiatycki J. Lifetime consumption of alcoholic beverages and risk of 13 types of cancer in men: results from a case-control study in Montreal. Cancer Detect Prev. 2009;32(5–6):352–62.
Kiyohara C, Nakanishi Y, Takayama K, Horiuchi T, Miyake Y. Molecular epidemiologic study of lung cancer on interaction between smoking and genetic factors. The 2009 Grant-in-Aid for Scientific Research (B) Report (Grant Number: 7390175), Japan Society for the Promotion of Science [cited 1 Feb 2018]. https://kaken.nii.ac.jp/file/KAKENHI-PROJECT-17390175/17390175seika.pdf (in Japanese).
Kiyohara C, Nakanishi Y, Horiuchi T, Takayama K. Genome epidemiologic study on lung cancer and estrogen-related genes. The 2017 Grant-in-Aid for Scientific Research (B) Report (Grant Number: 25293143), Japan Society for the Promotion of Science [cited 1 Feb 2018]. https://kaken.nii.ac.jp/file/KAKENHI-PROJECT-25293143/25293143seika.pdf (in Japanese).
Kiyohara C, Nakanishi Y, Takayama K, Horiuchi T. Genome epidemiologic study on lung cancer and inflammation-related genes. The 2013 Grant-in-Aid for Scientific Research (B) Report (Grant Number: 21390190), Japan Society for the Promotion of Science [cited 1 Feb 2018]. https://kaken.nii.ac.jp/file/KAKENHI-PROJECT-21390190/21390190seika.pdf (in Japanese).
Kiyohara C, Nakanishi Y, Inutsuka S, Takayama K, Hara N, Motohiro A, et al. The relationship between CYP1A1 aryl hydrocarbon hydroxylase activity and lung cancer in a Japanese population. Pharmacogenetics. 1998;8(4):315–23.
Kiyohara C, Horiuchi T, Takayama K, Nakanishi Y. Methylenetetrahydrofolate reductase polymorphisms and interaction with smoking and alcohol consumption in lung cancer risk: a case-control study in a Japanese population. BMC Cancer. 2011;11:459. https://doi.org/10.1186/1471-2407-11-459.
Liao SG, Liu L, Zhang YY, Wang Y, Wang YJ. SULT1A1 Arg213His polymorphism and lung cancer risk: a meta-analysis. Asian Pac J Cancer Prev. 2012;13(2):579–83.
Hosking L, Lumsden S, Lewis K, Yeo A, McCarthy L, Bansal A, et al. Detection of genotyping errors by hardy-Weinberg equilibrium testing. Eur J Hum Genet. 2004;12(5):395–9. https://doi.org/10.1038/sj.ejhg.5201164.
Gomes I, Collins A, Lonjou C, Thomas NS, Wilkinson J, Watson M, et al. Hardy-Weinberg quality control. Ann Hum Genet. 1999;63(Pt 6):535–8. https://doi.org/10.1017/S0003480099007824.
Haga H, Yamada R, Ohnishi Y, Nakamura Y, Tanaka T. Gene-based SNP discovery as part of the Japanese Millennium Genome Project: identification of 190,562 genetic variations in the human genome. Single-nucleotide polymorphism. J Hum Genet. 2002;47(11):605–10. https://doi.org/10.1007/s100380200092.
Yamaguchi-Kabata Y, Nakazono K, Takahashi A, Saito S, Hosono N, Kubo M, et al. Japanese population structure, based on SNP genotypes from 7003 individuals compared to other ethnic groups: effects on population-based association studies. Am J Hum Genet. 2008;83(4):445–56. https://doi.org/10.1016/j.ajhg.2008.08.019.
WHO. Lung cancer. In: Stewart BW, Kleihues P, editors. World cancer report. Lyon: International Agency for Research on Cancer Press; 2003. p. 182–7.
Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328(7455):1519. https://doi.org/10.1136/bmj.38142.554479.AE.
Riscuta G. Nutrigenomics at the interface of aging, lifespan, and cancer prevention. J Nutr. 2016;146(10):1931–9. https://doi.org/10.3945/jn.116.235119.
Krabbe LM, Lotan Y. Should patients newly diagnosed with bladder cancer be screened for lung cancer? Int J Urol. 2016;23(4):346–7. https://doi.org/10.1111/iju.13052.
International Agency for Research on Cancer. Some drinking-water disinfectants and contaminants, including arsenic, vol. 84. Lyon: World Health Organization; 2004.
Hietanen E, Husgafvel-Pursiainen K, Vainio H. Interaction between dose and susceptibility to environmental cancer: a short review. Environ Health Perspect. 1997;105(Suppl 4):749–54.
Washio M. Editorial comment to should patients newly diagnosed with bladder cancer be screened for lung cancer? Int J Urol. 2016;23(4):347. https://doi.org/10.1111/iju.13064.
Truong T, Sauter W, McKay JD, Hosgood HD 3rd, Gallagher C, Amos CI, et al. International Lung Cancer Consortium: coordinated association study of 10 potential lung cancer susceptibility variants. Carcinogenesis. 2010;31(4):625–33. https://doi.org/10.1093/carcin/bgq001.
Hung RJ, Christiani DC, Risch A, Popanda O, Haugen A, Zienolddiny S, et al. International Lung Cancer Consortium: pooled analysis of sequence variants in DNA repair and cell cycle pathways. Cancer Epidemiol Biomarkers Prev. 2008;17(11):3081–9. https://doi.org/10.1158/1055-9965.Epi-08-0411.
Kiyohara C, Yoshimasu K, Takayama K, Nakanishi Y. Lung cancer susceptibility: are we on our way to identifying a high-risk group? Future Oncol (London, England). 2007;3(6):617–27. https://doi.org/10.2217/14796694.3.6.617.
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55(2):74–108.
Sun S, Schiller JH, Gazdar AF. Lung cancer in never smokers—a different disease. Nat Rev Cancer. 2007;7(10):778–90. https://doi.org/10.1038/nrc2190.
Cote ML, Liu M, Bonassi S, Neri M, Schwartz AG, Christiani DC, et al. Increased risk of lung cancer in individuals with a family history of the disease: a pooled analysis from the International Lung Cancer Consortium. Eur J Cancer. 2012;48(13):1957–68. https://doi.org/10.1016/j.ejca.2012.01.038.
Jamrozik K. Tobacco and cardiovascular disease. In: Boyle P, Gray N, Henningfield J, Seffrin J, Zatonski W, editors. Tobacco and public health: science and policy. New York: Oxford University Press Inc.; 2004. p. 549–76. ISBN: 0-19-852687-3.
Washio M, Kiyohara C, Morioka S, Mori M. The experiences of smoking in school children up to and including high school ages and the current status of smoking habits; a survey of male high school students in Japan. Asian Pac J Cancer Prev. 2003;4:344–51.
Washio M, Kiyohara C, Oura A, Mori M. Smoking in youth: a review. In: Lapointe MM, editor. Adolescent smoking and health research. New York: Nova Science Publishers Inc.; 2008. p. 191–205. ISBN: 987-1-60456-046-6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kiyohara, C., Nakanishi, Y., Washio, M. (2019). Lung Cancer in the Elderly: The Most Dominant Cause of Cancer Death in Japan. In: Washio, M., Kiyohara, C. (eds) Health Issues and Care System for the Elderly. Current Topics in Environmental Health and Preventive Medicine. Springer, Singapore. https://doi.org/10.1007/978-981-13-1762-0_11
Download citation
DOI: https://doi.org/10.1007/978-981-13-1762-0_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1761-3
Online ISBN: 978-981-13-1762-0
eBook Packages: MedicineMedicine (R0)