Abstract
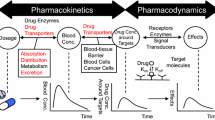
Biotransformation or metabolism is responsible for elimination of 70% of drugs available in the market today [1]. Drug-metabolizing enzymes (DMEs) are an assorted group of enzymes responsible for metabolizing xenobiotics such as drugs, carcinogens, pesticides, and food toxicants as well as endogenous compounds such as prostaglandins, steroids, and bile acids [2, 3]. R.T. Williams coined the concept of two-phase elimination of xenobiotics; reactions such as oxidation, reduction, and hydrolysis are categorized as phase I or activating reactions, while conjugation reactions constitutes phase II reactions and are generally detoxifying in nature [4]. Cytochrome P450 (CYP) families of enzymes are responsible for catalyzing majority of phase I reactions. Phase I reactions convert lipophilic molecules to their water-soluble counterparts [4]. Phase II reactions are catalyzed by enzymes such as uridine diphosphate glucuronosyltransferase (UGT), glutathione transferases (GSTs), N-acetyltransferase (NAT), and sulfotransferases (SULTs) [4]. Phase II enzymes catalyze conjugation of water-soluble molecules to intermediates of phase I reactions for the purpose of improving water solubility. In most cases, the net outcome of both phase I and phase II types of reactions is to impart hydrophilicity to xenobiotics and facilitate their elimination from the body. However, phase I and phase II reactions can also activate inert compounds to pharmacologically active entities [5], toxic end products, and procarcinogens into carcinogenic compounds [4, 6, 7]. CYPs and phase II metabolizing enzymes are known to exhibit polymorphism and have been associated with interindividual variability in drug response and toxicity.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
9.1 Introduction
Biotransformation or metabolism is responsible for elimination of 70% of drugs available in the market today [1]. Drug-metabolizing enzymes (DMEs) are an assorted group of enzymes responsible for metabolizing xenobiotics such as drugs, carcinogens, pesticides, and food toxicants as well as endogenous compounds such as prostaglandins, steroids, and bile acids [2, 3]. R.T. Williams coined the concept of two-phase elimination of xenobiotics; reactions such as oxidation, reduction, and hydrolysis are categorized as phase I or activating reactions, while conjugation reactions constitutes phase II reactions and are generally detoxifying in nature [4]. Cytochrome P450 (CYP) families of enzymes are responsible for catalyzing majority of phase I reactions. Phase I reactions convert lipophilic molecules to their water-soluble counterparts [4]. Phase II reactions are catalyzed by enzymes such as uridine diphosphate glucuronosyltransferase (UGT), glutathione transferases (GSTs), N-acetyltransferase (NAT), and sulfotransferases (SULTs) [4]. Phase II enzymes catalyze conjugation of water-soluble molecules to intermediates of phase I reactions for the purpose of improving water solubility. In most cases, the net outcome of both phase I and phase II types of reactions is to impart hydrophilicity to xenobiotics and facilitate their elimination from the body. However, phase I and phase II reactions can also activate inert compounds to pharmacologically active entities [5], toxic end products, and procarcinogens into carcinogenic compounds [4, 6, 7]. CYPs and phase II metabolizing enzymes are known to exhibit polymorphism and have been associated with interindividual variability in drug response and toxicity.
Interpatient variation of drug metabolism has paramount role in determining the safety and efficacy of drugs in various populations. Identification of acetylation polymorphism in the early 1960s was the very first evidence of polymorphism of drug-metabolizing enzymes [8]. The next crucial discovery in the area of pharmacogenetic variation in drug metabolism was the discovery of polymorphism in CYP 450 family of drug-metabolizing enzymes [1]. Since then, we have come a long way accepting the role of genetics in determining the fate of drug metabolism in individuals, as evidenced by the development of PCR-based tests enabling testing of common genetic polymorphisms of drug-metabolizing enzymes [1]. Although, the application of pharmacogenomics in regular clinical practice is not increasingly prevalent, constant efforts are made to advance toward having wider application of pharmacogenomics in clinical practice. The recent impetus from FDA to include pharmacogenetic information on approximately 10% of currently marketed drugs also attests to the fact that pharmacogenomics of drug metabolism is the need of the hour [1]. The number of drugs requiring pharmacogenetic tests is expected to grow in the future as more and more data is obtained on interpatient variations in the form of standardized clinical trials and post-marketing studies. The FDA is making constant efforts in providing detailed recommendations about the use of pharmacogenetic tests in clinical practice. The recommendations are updated on a quarterly basis [1].
The following sections will address the functional polymorphism of both phase I and phase II enzymes and their influence on safety and efficacy of drugs.
9.2 Phase I Metabolic Enzymes
Majority of phase I metabolism is catalyzed by Cytochrome P450 family of enzymes.
Cytochrome P450 are a large group of DME belonging to hemoproteins superfamily of enzymes. They are found mainly in hepatocytes but are also present in the small intestine, lungs, kidneys and brain. As shown in Fig. 9.1, CYP1, CYP2, and CYP3 are three major families responsible for the oxidative metabolism of drugs [9]. The human CYP genes are greatly polymorphic. The peer-reviewed information of various alleles is summarized at the human CYP allele nomenclature home page (www.cypalleles.ki.se) present on the server at Karolinska Institutet [10]. The website hosts information about more than 350 functionally different alleles [10]. According to the website, the highest numbers of alleles described are CYP2D6 (63 alleles), CYP 2B6 (28 alleles), CYP1B1 (26 alleles), and CYP2A6 (22 alleles) [10]. The functional CYP polymorphisms consist of gene deletions, gene duplications, and deleterious mutations creating inactive gene products [10]. Additionally, changes in amino acid sequence due to mutation can change the substrate specificity. The polymorphism in CYP enzymes can result in copy number variation where multiple functional gene copies of one allele can result in increased enzyme activity and increase in drug metabolism [11, 12]. The most important polymorphic CYP enzymes with respect to drug metabolism are CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9,CYP2C19, CYP2D6, and the CYP3As (Fig. 9.1) [10]. The following sections will address the polymorphism of above listed enzymes with special emphasis on clinical significance.
9.2.1 CYP 1A2
CYP1A2 is one of the major CYPs in the human liver amounting to be approximately 13–15% of total CYP enzymes and is responsible for metabolizing 15% of clinically available drugs such as clozapine, theophylline, tacrine, zolmitriptan, duloxetine, and verapamil to name few [13]. Environmental factors and genetic mutations are responsible for the large interindividual variability in the elimination of drugs metabolized by CYP1A2 [14, 15].
Various modeling studies have suggested that the majority of CYP1A2 substrates are hydrophobic with high logP values suggesting the role of hydrophobic interactions in the binding to CYP1A2 [15]. CYP1A2 along with CYP1A1 and 1B1 also play a crucial role in the bioactivation of procarcinogens such as aromatic amines and polycyclic aromatic hydrocarbons [16]. There are wide interindividual differences (10–200-fold) in CYP1A2 expression and activity [15]. There have been reports of approximately 15- and 40-fold interindividual variations in CYP1A2 mRNA and protein levels in human livers [17]. The frequencies of poor metabolizers who are nonsmokers were reported to be 5% in Australians, 14% in Japanese, and 5% in Chinese [18]. There is clear difference in increased CYP1A2 activity in different races; Swedes have 1.5-fold higher activity as compared to Koreans [19]. Asian and African populations have been reported to have lower CYP1A2 activity as compared to Caucasians [20]. The NCBI dbSNP database (www.ncbi.nlm.nih.gov) reports that more than 200 polymorphisms exist in CYP1A2 gene. Polymorphisms in CYP1A2*1C, CYP1A2*1D, CYP1A2*1E, and CYP1A2*1F were reported in Japanese population. Of the polymorphic alleles, CYP1A2*1C, *1D, *1F, and *1K have been associated with altered enzyme activity [13]. Concerning mutations in the regulatory regions, alleles CYP1A2*1F and CYP1A2*1K have received substantial attention [12]. The CYP1A2*1F allele contains 163C>T mutation in intron 1, and this has been shown to influence the inducibility of the gene and affect the intensity of increase of in vivo caffeine metabolism after both smoking [21, 22] and omeprazole treatment [23]. A variant of this allele is found in African populations [24]; in addition to 163C>T, it also contains −729C>T which abolishes binding site of an Ets nuclear factor resulting in significant decrease in CYP1A2 expression and caffeine metabolism.
A number of clinical studies have been conducted to study the impact of CYP1A2 polymorphisms on drug metabolism, clearance, and response. Resistance to clozapine therapy due to increased metabolism and lower plasma levels in smoking schizophrenic patients possessing CYP1A2*1F allele was reported [25, 26]. Higher concentrations of clozapine and its metabolite N-desmethylclozapine was detected in patient carrying the two CYP1A variants associated with reduced enzyme activity [27]. In spite of the absence of any functional gene variants, many epidemiological association studies have been published to link particular polymorphic sites to disease susceptibility [14, 15]. Numerous reports have surfaced suggesting the role of CYP1A2 polymorphism and susceptibility to cancers such as bladder cancer [28], adenocarcinoma, lung cancer [29], and head and neck squamous cell carcinoma [30]. Additionally, the relationship between polymorphism and disease susceptibility for conditions such as myocardial infarction, tardive dyskinesia, and schizophrenia as well as recurrent pregnancy loss was reported without much consensus information [14, 15].
9.2.2 CYP2A6
CYP2A6 is mainly expressed in hepatic tissue and is responsible for metabolizing several important therapeutic agents, toxins, and procarcinogens [31]. It is also known to be responsible for the metabolism of nicotine and its metabolite cotinine and is touted to be the responsible factor in interindividual variability in nicotine metabolism, smoking behavior, and the risk of tobacco-related cancer [32,33,34]. A large amount of interindividual variability in CYP2A6 activity is reported by the in vitro and in vivo estimation of CYP2A6 activity by measuring coumarin oxidation [35]. As with any polymorphic enzyme, CYP2A6 shows ethnic variation in interindividual variability with 1% Caucasians and 20% of Asians being PM. CYP2A6 expression can only be slightly induced suggesting that the environmental factors contribute very little to the CYP2A6 variability. Single amino acid deletion in CYP2A6*2 makes the enzyme inactive, whereas CYP2A6*4 has gene deletion causing decrease in enzyme activity and is seen in majority of PM in the Asian population. Additionally, the variants CYP2A6*5 and CYP2A6*20 result in abolished activity of the enzyme [10]. Eight additional CYP2A6 alleles (*6, *7, *10, *11, *12, *17, *18, and *19) lead to enzymes with limited activity [10]. As CYP2A6 is greatly involved in the metabolism of nicotine and cotinine, the genetic variations and interindividual difference play a role in smoking and tobacco-related cancer risks [32, 34].
9.2.3 CYP2B6
CYP2B6 is relevant for the metabolism of anticancer drugs such as cyclophosphamide and ifosfamide and HIV drugs like efavirenz and nevirapine [36,37,38]. The human CYP2B6 gene is highly polymorphic and has 29 allelic variants many of which are responsible for increased, decreased, or complete lack of activity [39]. The alleles with lower expression or activity includes CYP2B6*6, CYP2B6*16, and CYP2B6*18 [40, 41]. CYP2B6*6 variants are observed in 20–30% frequency in different populations; CYP2B6*16 and CYP2B6*18 occur commonly in Black population with the frequency of 7–9% [40, 41]. In various clinical studies, it has been proven that the subjects homozygous for combinations of the alleles including CYP2B6*6, CYP2B6*16, and CYP2B6*18 show lower rate of metabolism of CYP2B6 substrates [40, 41]. The 516G>T and 785A>G mutations resulting in amino acid substitutions and Q172H and K262R in CYP2B6*6 allele give rise to haplotypes with high or low activity of CYP2B6. The clinical relevance of CYP2B6-mediated interindividual variability still needs more investigation and development of efficient tools to predict the specific capacity for metabolism of CYP2B6 substrates.
9.2.4 CYP2C8
CYP2C8 is crucial for the metabolism of drugs such as repaglinide, rosiglitazone, pioglitazone, paclitaxel, chloroquine, amiodarone, and dapsone among others. The withdrawal of cerivastatin due to severe or sometimes fatal rhabdomyolysis was a strong evidence of relevance of CYP2C8-mediated drug interactions. Most of the cerivastatin adverse effects were observed when gemfibrozil, a CYP2C8 inhibitor, was coadministered [42, 43].
In vitro variation in the metabolism of CYP2C8 substrates and CYP2C8 expression is very large [44]; however, lack of standardized test to the phenotype activity makes the estimation of in vivo variation rather difficult.
Several coding region SNPs have been reported in the CYP2C8 gene with crucial interracial variations; CYP2C8*2 is observed in Africans, while CYP2C8*3 and CYP2C8*4 are mainly found in Caucasians [45, 46]. There are additional two SNPs, *1B and *1C, described in the promoter region of CYP2C8 [44]. In vitro studies using heterologous proteins revealed that CYP2C8.3 had reduced activity using paclitaxel as substrate; however, there was no difference in amiodarone metabolism. In vivo studies are inconclusive as mentioned above due to lack of proper evaluation tools. Two recently identified haplotypes of CYP2C8 have both lower and higher activity of the enzyme when tested with paclitaxel and repaglinide as substrates [47]. It was shown that high-activity allele carried CYP2C8*1B which binds nuclear factor, while Ile26Met present in CYP2C8*4 was part of the low-activity haplotype [10]. Therefore, CYP2C8 is a highly conversed gene that has no important functional allele or null alleles distributed among individuals. The clinical relevance of CYP2C8 needs further investigation and validation.
9.2.5 CYP2C9
CYP2C9 is mainly expressed in the liver forming 20% of the total CYP content and is the highest expressed among the CYP2C enzymes. CYP2C9 is responsible for metabolizing 10% of all drugs including nonsteroidal anti-inflammatory drugs (NSAIDs), antidiabetics, anti-infectives, hypnotics, antiepileptics, oral coagulants, sulfonylureas, psychotropics, and angiotensin receptor blockers [10]. A large interindividual variability in CYP2C9 activity is reported which is also responsible for interindividual variations in drug response and adverse effects. The variations could be the result of environmental factors, such as induction by prototypical CAR, GR, and PXR ligands through different elements in the promoter gene [48]. Multiple single nucleotide polymorphisms within CYP2C9 are reported, and at least 13 of these SNPs encode for CYP2C9 alleles [49, 50]. The polymorphic behavior of CYP2C9 is predominantly determined by two common coding variants, CYP2C9*2 (R144C) and CYP2C9*3 (I359L), both of which produces enzyme with decreased activity. CYP2C9*2 and CYP2C9*3 are present in Caucasians with 11 and 7% frequency, respectively. The frequency is lower in Africans and Asians [51]. It has been shown that the substrate affinity of CYP2C9.2 is unaffected for some substrates, whereas it is drastically reduced for the others [52]. However, CYP29.3 shows significant reduction in the catalytic activity as compared to the wild type [52]. The drugs metabolized by CYP2CP include S-warfarin, glimepiride, glyburide, tolbutamide, angiotensin receptor blockers, fluvastatin, and NSAIDs such as celecoxib, diclofenac, flurbiprofen, and ibuprofen [53]. CYP2C9*2 has significant impact on the clearance of S-warfarin, tolbutamide, and celecoxib and does not significantly impact others [53]. In case of CYP2C9*3 heterozygous individuals, the clearance for most substrates was 50% as compared to the wild type, while in case of CYP2C9*3 homozygous individuals, the reduction was five- to tenfold. All in all, CYP2C9 polymorphism is of great clinical significance and should be taken into account for effective therapeutic outcome.
9.2.6 CYP2C19
CYP2C19 is an important CYP enzyme located on chromosome 10. A range of drugs have been found to be substrates, inhibitors of inducers of this enzyme. Some of the important substrates of CYP2C19 are TCA and SSRI antidepressants, PPIs, antiplatelet drug clopidogrel, antiepileptics like diazepam, mephenytoin, phenobarbital, and anticancer drug cyclophosphamide. Polymorphism in CYP2C19 (mainly *2, *3) is responsible for poor metabolizer (PM) genotype in ~3–5% Caucasians and ~15–20% Asians [54]. The safety and/or efficacy of CYP2C19 substrates can be compromised in these individuals, and major clinical outcome is affected in PM. Sagar et al. studied the effect of CYP2C19 genotype affecting omeprazole metabolism and subsequently its effect on acid inhibition. They found that analysis of CYP2C19 genotype may be important to avoid negative effects on therapy especially for patients on long-term treatment [55]. Similarly, PMs can show reduced effectiveness to clopidogrel as it is not effectively converted to the active metabolite. Out of the total dose of clopidogrel administered, only 15% of prodrug is converted to the active metabolite, while the remaining 85% is converted to inactive derivatives by the action of esterases (Fig. 9.2). CYP2C9 contributes to 21% of the active metabolite generation [56]. CYP2C19*2 carriers have been reported to have diminished antiplatelet activity of clopidogrel due to reduction in generation of active metabolite [57, 58]. Omeprazole and clopidogrel which can be prescribed together as PPIs may reduce the risk of gastrointestinal bleeding in patients receiving clopidogrel after acute coronary syndrome or percutaneous coronary intervention. In this pharmacogenomic-based DDI, effects can be more pronounced. Lately, US FDA has issued a warning that PPI omeprazole reduces the antiplatelet effect of clopidogrel by about 50% by inhibiting CYP2C19 isoenzyme. Although the clinical outcome of this DDI is still not clear, caution must be exercised when using clopidogrel and omeprazole together. Polymorphism in CYP2C19 (*17) has been found to be responsible for extensive metabolizer (EM) status of a patient. Approximately 18–20% Caucasian and Ethiopians are found to be EMs and can affect metabolism of a variety of drugs [59]. Study shows that increased metabolism of omeprazole in carriers of CYP2C19*17 allele may be responsible for subtherapeutic drug expossure [60].
9.2.7 CYP2D6
CYP2D6 encompasses the largest number of protein variants among all the CYPs. CYP2D6 is responsible for metabolizing a large number of drugs (~50%) in the market today, and polymorphism in CYP2D6 can significantly affect metabolism of these drugs, thus altering therapeutic outcome. Some of the important CYP2D6 substrates are TCAs, SSRIs, typical antipsychotics, opioid analgesics, antiemetics, β-blockers, and some antiarrhythmics [61]. CYP2D6 is the only CYP enzyme which is not inducible, and so the interindividual variation is a result of genetic variations. The polymorphism of CYP2D6 is of great clinical significance due to its role in metabolizing the large number of currently used drugs. More than 63 different functional CYP2D6 have been reported, and they are classified into alleles causing abolished, decreased, normal, and ultrarapid enzyme activity. Different protein variants account for normal (*1, *2), extensive (*1xN, *2xN, *33, *35x2), intermediate (*9, *10, *17, *29, *41, *49, *50, *54, *55, *59, *72), and poor metabolizers (*3–*8, *11–*16, *18–*21, *31, *36, *38, *40, *42 *44, *47, *51, *56, *62) of CYP2D6 [10, 61]. CYP2D6*4 allele is found to be higher in Caucasians, *10 in Asians, and *17 in Africans. PM 7–10% in Caucasians [62,63,64,65,66] is mainly due to CYP2D6*3 and*4. Only up to 1% Asians are PMs. CYP2D6*10 is the most frequent allele in Asians, and this variation accounts for 50–70% variation due to CYP2D6 protein variants [67]. CYP2D6*17 is most frequently seen in Africans, and it has been estimated that Zimbabweans account for 34% CYP2D6 variation due to CYP2D6*17 alone [68]. Although the PM phenotypes are at higher risk for adverse drug reactions, the UM phenotype areas are also vulnerable to adverse reactions as a result of high concentration of metabolite. A tragic example of UM experiencing adverse effects is incidence of death of a healthy newborn as a result of breastfeeding by a UM mother taking high dose of codeine for the mitigation of postpartum pain; codeine was metabolized into morphine (Fig. 9.3) which was transmitted to the infant via breast milk in toxic quantities leading to severe respiratory depression and death [69]. It is reported that in UMs, the concentration of metabolites can go up to 10–30-fold as compared to normal metabolizers. The other side of the coin is that UMs can be unresponsive to drugs such as antidepressant due to extensive inactivation of the drugs [70].
CYP2D6 is involved in metabolism of tamoxifen to yield active and much potent metabolite endoxifen. CYP2D6 PMs will show reduced response when tamoxifen is used for treatment of breast cancer. Besides that, inhibitors of CYP2D6 also led to lower than normal levels of plasma endoxifen [71,72,73]. Some studies show that PM with breast cancer demonstrated a shorter time to recurrence or shorter survival time [74,75,76]. However, some retrospective studies do not agree with this. Still PM of tamoxifen can affect clinical outcome, and caution should be exercised in prescribing tamoxifen to these patients. Drugs such as antidepressants that are known to decrease the activity of CYP2D6 will have decrease in therapeutic activity of tamoxifen.
CYP2D6 polymorphism has significant effect on tramadol drug therapy. Tramadol is metabolized to an active metabolite, O-demethyl tramadol, by CYP2D6. The CYP2D6 genotype has shown to be the determinant factor in dictating concentration of O-demethyl tramadol thereby affecting the efficacy of tramadol [77]. PMs for CYP2D6 have less response to postoperative tramadol analgesia as compared to the EMs [78].
All in all, the polymorphism of CYP2D6 is the most clinically relevant polymorphism affecting drug therapy [79]. Genotyping will help in explaining the non-responsiveness or susceptibility to adverse reactions of CYP2D6 substrates in various individuals.
9.2.8 CYP3A4/5/7
The clinically relevant members of CYP3A isoform include CYP3A4, 3A5, and 3A7. All three enzyme subfamilies have wide substrate specificity due to which they are the most important drug-metabolizing subfamily. CYP3As are expressed primarily in liver and intestine and is responsible for metabolizing 45–60% of currently marketed drugs. CYP3A isoforms are also responsible for first-pass metabolism of its substrates. CYP3A expression and activity are affected by a combination of genetic, nongenetic, and environmental factors resulting in vast interindividual variability [80]. Up to 40-fold interindividual variations are seen for substrates such as triazolam, midazolam, and ciclosporin [81]. CYP3A4 has the highest activity toward common CYP3A substrates as compared to other isoforms [82]. In case of CYP3A5 and CYP3A7, clinically significant variations includes CYP3A5*3 and 7 and CYP3A7*1B and *1C, respectively [80]. In spite of having the large contribution of CYP3A4 toward drug metabolism and also associated variability, the polymorphisms affecting CYP3A4 are not widely reported except the most recent report of *22 allele. The effect of polymorphisms in CYP3A5 and CYP3A7 on drug metabolism is dependent on the concomitant expression status of CYP3A4 [81]. The following subsections will briefly address the polymorphisms in CYP3A4, 5, and 7.
Extensive studies of allelic variants of CYP3A4 have revealed variant proteins of CYP3A4 with diminished activity (*6, *17, and *20). These alleles are not considered as the reason for interindividual variations due to their low frequency of occurrence. It has been shown that the difference in transcription rate of CYP3A4 is the main cause of interindividual variability [83]. Despite multiple efforts, the exact mechanism of CYP3A4 expression variability is still unknown.
CYP3A5 is highly polymorphic as a result of mutations that drastically reduce the enzyme activity. The common variations include, CYP3A5*3, 6, and 7 out of which CYP3A5*3 is the most common defective allele with an allele frequency of about 90, 75, and 20% in Caucasians, Asians, and Africans, respectively [84, 85]. However, CYP3A5*6 and CYP3A5*7 are not present in Caucasians and Asians and are 17 and 8% in Africans, respectively [86]. As mentioned above, many drugs metabolized by CYP3A5 are also substrates for CYP3A4, so distinguishing the effect of CYP3A5 polymorphism on drug metabolism is rather difficult.
CYP3A7 is mainly expressed in fetus, with its expression starting after 50–60 days of gestation and continuing up to 6 months of postnatal age [87]. The interindividual variation of CYP3A7 is important because the enzyme is responsible for metabolizing endogenous compounds and xenobiotics reaching the fetus through maternal circulation; the degree and extent of metabolism will have an effect on embryotoxicity and teratogenicity. CYP3A7 shows one frameshift mutation (CYP3A7*2) [88] and one coding polymorphism (CYP3A7*2). The CYP3A7*2 SNP codes for enzyme have slightly higher activity than CYP3A7*1 and have an allele frequency of 8, 28, and 62% in Caucasians, Asians, and Africans, respectively [89]. In vitro studies using fetal liver microsomes did not report any significant differences in the metabolism of dehydroepiandrosterone (DHEAS) by the liver carrying CYP3A7*2 and CYP3A7*1 [90]. In addition to polymorphisms resulting in alternative CYP3A7 proteins, a genetic promoter CYP3A7*1C is reported to be pertinent for the expression of CYP3A7 [91]. The carriers of CYP3A7*1C alleles have high expression of CYP3A7 which showed decreased DHEAS levels in a small clinical study conducted in 208 elderly women and 345 elderly men [92]. There were some reports of correlating CYP3A7*1C expression and bone density in elders, but the findings were inconclusive. The effect of CYP3A7 polymorphism on drug metabolism and disease pathology needs further research.
9.3 Phase II Metabolic Enzymes
Phase II reactions involve conjugation of functional groups with endogenous molecules generally aimed at increasing water solubility of xenobiotics. Some of the important phase II reactions are sulfonylation/sulfation, glucuronidation, acylation, methylation, and amino acid and glutathione conjugations as shown in Fig. 9.4. Different types of enzymes are involved in these conjugation reactions, and polymorphism in these enzymes can significantly affect drug’s safety and efficacy, two important criteria due to which drug fails in clinic. Given below are some of the important reactions and enzymes involved in phase II metabolism.
9.3.1 Glucuronidation
UDP (uridine diphosphate)-glucuronosyltransferases commonly known as UGTs are the most common group of glucuronidation enzymes. Some of the common functional groups susceptible to glucuronidation are hydroxyl (–OH), amine (–NH2), and carboxyl (–COOH) groups. Generally, glucuronide conjugates are much less active than the parent molecule and result in terminal metabolite that can be readily eliminated by kidneys. Some of the common drug substrates for UGTs are NSAIDs, acetaminophen, hydroxysteroids, benzodiazepines, irinotecan, indacaterol, and nilotinib. UGTs are mainly represented by three gene subfamilies: UGT1A, UGT2A, and UGT2B. Protein variants of diverse UGTs have been reported that affects biotransformation and clearance of drugs. Some of these variants have clinically significant effect on the efficacy and/or safety of drugs. One important example is the metabolism of irinotecan, a topoisomerase II inhibitor indicated for metastatic colorectal cancer. As shown in Fig. 9.5, UGT1A1, UGT1A6, and UGT 1A7 are mainly involved in glucuronidation of active metabolite of irinotecan. Gene variant UGT1A1*28 has been found to be mainly responsible in diminishing metabolism of active metabolite leading to clinically relevant toxicities like neutropenia and diarrhea [93, 94]. FDA has updated irinotecan label recommending dose reduction for individuals having homozygous alleles of UGT1A1*28. Studies have shown that gene variant UGT1A1*6 can also affect glucuronidation during irinotecan metabolism [95].
Similarly, drugs can inhibit protein variants of UGTs and may result in toxicity arising due to altered metabolism of endogenous molecules. One such example is the use of HIV protease inhibitor – atazanavir; this drug inhibits UGT1A1, UGT1A3, and UGT1A4. It has been found that individuals homozygous for UGT1A1*28 receiving atazanavir showed higher incidence of jaundice due to altered metabolism of bilirubin, a well-known substrate for UGTs [96].
Similarly, there are studies on significance of role of the UGT1A8*2 variant allele on mycophenolate mofetil-induced diarrhea [97] and diclofenac-induced hepatotoxicity due to genetic variation in UGT2B7, CYP2C8, and ABCC2 [98].
9.3.2 Methylation
Methylation is a very important phase II reaction mainly targeting endogenous molecules containing hydroxyl (–OH), amine (–NH2), or thiol (–SH) functional groups. Catecholamines like epinephrine and norepinephrine are deactivated by catechol-O-methyltransferases (COMT) that catalyze the transfer of a methyl group to one of the catechol hydroxyls. Similarly, N-methylation of norepinephrine to epinephrine is mediated by phenylethanolamine N-methyltransferase in kidneys. S-adenosyl methionine (SAM) was found to be a common cofactor mediating methylation. Some of the important methylating enzymes exhibiting clinically significant polymorphism are thiopurine methyltransferases (TMPTs) and COMT.
9.3.2.1 Thiopurine Methyltransferase (TMPT)
Thiopurines represent three important drugs useful as immunosuppressant or as anticancer. Azathioprine (Imuran) is useful to prevent organ rejection and other autoimmune diseases like Crohn’s diseases and ulcerative colitis (UC). 6-mercaptopurine or 6-MP (Purinethol) is generally useful for treating certain types of leukemia and also acts as immunosuppressive agent for Crohn’s diseases and UC. Thioguanine or 6-TG (Tabloid) is another purine antagonist that acts as an antimetabolite and interferes with the synthesis and metabolism of endogenous purine nucleotides. As shown in Fig. 9.6, 6-MP and 6-TG must be converted to active thiopurine ribonucleotide by HGPRT (hypoxanthine-guanine phosphoribosyltransferase). This intermediate is then methylated by TMPT to form active S-methylthiopurine ribonucleotide to exert cytotoxic action. TMPT is also an important enzyme to terminate the effects on 6-MP or 6-TG by methylation. Individuals with polymorphism in TMPT have less capacity to deactivate these thiopurines which leads to overproduction to cytotoxic thiopurine nucleotides. These excessive activated nucleotides can result in life-threatening toxicities like myelosuppression. Further, clinical efficacy will be compromised due to altered metabolism. Similarly, as shown in Fig. 9.7, azathioprine first gets converted to 6-MP nonenzymatically, but the next activation step requires HGPRT similar to 6-MP and 6-TG metabolism. Subsequently TMPT is required to terminate this drug’s effect. So, protein variants of TMPT can alter azathioprine’s clinical outcome as well.
At the molecular level, TMPT*3 is the most common protein variant that accounts for three fourth defective alleles in TMPT. TMPT variants *2, *3A, and *3B are common polymorphisms seen. Allele frequency varies by ethnic population, and it has been found that *3A is the most common variant in Caucasians, while *3C is the most common variant in Asians and African-Americans [99].
FDA updated labels of azathioprine and thiopurines to include information about TMPT polymorphism and recommends testing of TMPT genotype of a patient before starting therapy with these drugs. Depending on TMPT genotype, either dose can be modified to achieve similar therapeutic outcomes or alternative therapies can be prescribed in patients found to be homozygous. For example, ~10% Caucasians are found to be poor TMPT metabolizers and dose of azathioprine and thiopurine may be decreased by 10–15- fold to avoid myelosuppression and to keep drug plasma levels within therapeutic window.
9.3.2.2 Catechol O-Methyltransferase
COMT has been involved in metabolism of a number of drugs as well as endogenous molecules like central neurotransmitters. Polymorphism in COMT has been reported among various ethnic groups, and the frequency of homozygous and heterozygous alleles varies. For example, it has been found that 50% Caucasian are heterozygous and 25% are homozygous for COMT allele [100]. However COMT variation on drug levels has not found to be much clinically significant so far.
9.3.3 Acetylation
N-acetyltransferases (NATs) catalyzes the acetylation reactions generally for amine (–NH2) groups and less commonly hydroxyl (–OH) and thiol (–SH) groups. There are two isoforms of NAT commonly known as NAT1 and NAT2. Protein variants NAT1*10 and *11 alleles are generally referred to as fast acetylators. Genetic variation in NAT2 is much more common, and a number of variants like *5, *6, *7, *10, *14, and *167 are responsible for altered enzyme activity. Patients are mainly categorized as fast acetylators, normal acetylators, or slow acetylators depending upon their NAT genotype variations. Allele frequency varies among different ethnic groups as well as within same group [101].
NAT protein variants can affect levels of antituberculosis drug regimen (rifampin, isoniazid, and pyrazinamide) as well as antihypertensive combination (hydralazine-isosorbide). One well-known example of polymorphism in NAT2 is seen with metabolism of hydralazine. As shown in Fig. 9.8, hydralazine undergoes acetylation to form inactive acetylated metabolite. In slow acetylators, drug stays in plasma for much longer time (plasma t1/2 can be increased from 2 to 4 h to up to 8 h) and increases incidence of systemic lupus erythematosus (SLE). In fast acetylators, a subtherapeutic response is achieved which is most commonly seen in 50% African-Americans and Caucasians and the majority of American Indians, Eskimos, and Chinese population.
9.3.4 Sulfation/Sulfonylation
Sulfotransferases (SULTs) catalyze the transfer of sulfonyl (–SO3H) group to various drug molecules containing hydroxyl (–OH), thiol (–SH), and amine (–NH2) functional groups. For example, sulfonylation is the major route of acetaminophen metabolism in children where –OH group is conjugated with sulfonyl group to inactive the drug. Two important genes that exhibit polymorphism are SULT1A1 and SULT1A2. One important example of influence of protein variants of SULTs is seen with endoxifen, an active metabolite of tamoxifen. It undergoes sulfonylation at hydroxyl (–OH) group, and protein variants in SULT1A1*2 and *3 may be responsible for decreased therapeutic response. It has been found that SULT1A1*1 leads to rapid sulfonylation of endoxifen which may lead to apoptosis in a breast cancer [102]. This suggests that SULTs can play a role in improving survival in cancer patients and also in decreased therapeutic response. However, so far no recommendations have been made by the FDA. So, polymorphism can sometimes be helpful in understanding a drug’s efficacy and individualize drugs based on patient’s genotype.
9.3.5 Glutathione (GSH) Conjugation
Glutathione S-transferases (GSTs) catalyze the transfer of tripeptide molecule glutathione (GSH) to electrophilic centers in a drug molecule. Resulting S-bridge between glutathione and the drug results from covalent bond formation, and this drug-glutathione S-conjugate can be eliminated as such or can further degrade tripeptide for elimination. Anticancer alkylating agents and platinum compounds are major targets for metabolism by GSTs. There are different types of GST like GSTP, GSTA, GSTT, GSTO, GSTZ, and GSTS located on different chromosomes. These GSTs can have protein variants affecting metabolism of drugs or elimination of their metabolites. For example, GSTP1 is involved in metabolism in platinum compounds (cisplatin, oxaliplatin) and may metabolize these drugs faster to diminish their therapeutic effects. It has been reported that patients with ovarian cancer showing GSTP1*B polymorphism may have better progression-free survival than patients with GSTP1*A [103]. On the other hand, decreased activity of GSTP1 with protein variant can decrease metabolism of platinum compounds and can lead to toxicity. Similarly, GSTA1*B lead to increased therapeutic effects of cyclophosphamide and increased survival in breast cancer patients [104]. Another anticancer drug busulfan undergoes significant metabolism by GSH, and significant differences in plasma levels of drug in different patient populations have been reported [105]. Further studies are needed to really understand the role of protein variants of GST on the safety and efficacy of these anticancer compounds.
9.3.6 Amino Acid Conjugation
Various amino acids like glycine glutamine, arginine, and taurine can conjugate with carboxyl (–COOH) functional group present in drug molecules. This is an important metabolic pathway for some drugs like valproic acid and salicylic acid. However, so far there are not many reports on significantly altered drug levels due to polymorphism in enzymes catalyzing amino acid conjugations.
9.3.7 Impact of Polymorphism on Phase II Enzymes
The FDA periodically updates drug labels as critical information related to pharmacogenomics of existing drugs become available, and this can potentially affect clinical outcome. This section provides information about some important phase II enzymes and their effect on product labeling that the US FDA has updated based on pharmacogenomics information that came to surface after the drug was approved in the market. Labeling information pertaining to pharmacogenomics of drugs can be found at the FDA website, (http://www.accessdata.fda.gov/scripts/cder/drugsatfda/).
9.3.8 Role of Microbiome in Drug Metabolism
The human intestine is home to a complex community of microorganisms known as the gut microbiota which has undergone coevolution with its host [106]. The microbes function as an organ within themselves with metabolic, immunologic, and endocrine-like actions that can affect human health [107]. Advances in molecular techniques have made it possible for a reliable assessment of gut bacteria. The three types of bacteria that dominate human gut include Firmicutes (Gram-positive), Bacteroidetes (Gram-negative), and Actinobacteria (Gram-positive) [108]. Changes in the structure and diversity of the microbiome can affect the overall health of the host and pathological states such as inflammatory bowel diseases (IBD), obesity, and diabetes [109,110,111]. Another important area where microbiome has a role is in drug metabolism. Microbiome expresses a wide range of enzymes which have the ability to metabolize drugs efficiently and extensively [112]. More than 30 drugs and other bioactive molecules are reported to undergo modification/metabolism by gut microbiome [113]. The number of the drugs continues to grow as more and more evidence becomes available from in vitro and clinical studies. Deducing the exact mechanism of action and the type of microorganisms involved remains unclear due to the complexity of the microbiome. The types of reaction catalyzed by gut microbiome include azoreduction, nitroreduction, sulfoxide reduction, N-oxide reduction, hydrolysis, acetylation, and deacetylation [114]. Multiple studies have shown that the gut microbiome can affect the pharmacokinetics of orally administered drugs having significant impact on the bioavailability [115]. There is interindividual variability in the population and structure of gut microbiome; therefore, it can be assumed that the variability will be reflected in the degree of metabolic reactions catalyzed by these microorganisms. Microbiome-catalyzed drug metabolism complicates the interindividual variability of drug metabolism, which varies from individual to individual as a result of pharmacogenomics.
Conclusion
Drug metabolism is a very complex phenomenon which varies across the patient population due to pharmacogenomics of the drug-metabolizing enzymes and the host microbiome. Pharmacogenomics of the drug-metabolizing enzymes has been studied in detail; there is plenty of data supporting the variability. However, the variability due to metabolism by microbiome is an evolving field, which should become clearer as we gather evidence and understand the whole process with time. Therefore, it is the need of the hour to look at the interpatient variability from both microbiome and pharmacogenomics of DME point of view.
References
Williams JA, Hyland R, Jones BC, Smith DA, Hurst S, Goosen TC, Peterkin V, Koup JR, Ball SE (2004) Drug-drug interactions for UDP-glucuronosyltransferase substrates: a pharmacokinetic explanation for typically observed low exposure (AUCi/AUC) ratios. Drug Metab Dispos 32(11):1201–1208
Coon MJ (2005) Cytochrome P450: nature’s most versatile biological catalyst. Annu Rev Pharmacol Toxicol 45:1–25
Guengerich FP, Rendic S (2010) Update information on drug metabolism systems-2009, part I. Curr Drug Metab 11(1):1–3
Goldstein JA, Faletto MB (1993) Advances in mechanisms of activation and deactivation of environmental chemicals. Environ Health Perspect 100:169–176
Fura A, Shu YZ, Zhu M, Hanson RL, Roongta V, Humphreys WG (2004) Discovering drugs through biological transformation: role of pharmacologically active metabolites in drug discovery. J Med Chem 47(18):4339–4351
Kalgutkar AS, Vaz AD, Lame ME, Henne KR, Soglia J, Zhao SX, Abramov YA, Lombardo F, Collin C, Hendsch ZS, Hop CE (2005) Bioactivation of the nontricyclic antidepressant nefazodone to a reactive quinone-imine species in human liver microsomes and recombinant cytochrome P450 3A4. Drug Metab Dispos 33(2):243–253
Kalgutkar AS, Henne KR, Lame ME, Vaz AD, Collin C, Soglia JR, Zhao SX, Hop CE (2005) Metabolic activation of the nontricyclic antidepressant trazodone to electrophilic quinone-imine and epoxide intermediates in human liver microsomes and recombinant P4503A4. Chem Biol Interact 155(1–2):10–20
Evans DA, White TA (1964) Human acetylation polymorphism. J Lab Clin Med 63:394–403
Gardiner SJ, Begg EJ (2006) Pharmacogenetics, drug-metabolizing enzymes, and clinical practice. Pharmacol Rev 58(3):521–590
Ingelman-Sundberg M, Sim SC, Gomez A, Rodriguez-Antona C (2007) Influence of cytochrome P450 polymorphisms on drug therapies: pharmacogenetic, pharmacoepigenetic and clinical aspects. Pharmacol Ther 116(3):496–526
Redon R, Ishikawa S, Fitch KR, Feuk L, Perry GH, Andrews TD, Fiegler H, Shapero MH, Carson AR, Chen W, Cho EK, Dallaire S, Freeman JL, Gonzalez JR, Gratacos M, Huang J, Kalaitzopoulos D, Komura D, MacDonald JR, Marshall CR, Mei R, Montgomery L, Nishimura K, Okamura K, Shen F, Somerville MJ, Tchinda J, Valsesia A, Woodwark C, Yang F, Zhang J, Zerjal T, Armengol L, Conrad DF, Estivill X, Tyler-Smith C, Carter NP, Aburatani H, Lee C, Jones KW, Scherer SW, Hurles ME (2006) Global variation in copy number in the human genome. Nature 444(7118):444–454
Stranger BE, Nica AC, Forrest MS, Dimas A, Bird CP, Beazley C, Ingle CE, Dunning M, Flicek P, Koller D, Montgomery S, Tavare S, Deloukas P, Dermitzakis ET (2007) Population genomics of human gene expression. Nat Genet 39(10):1217–1224
Zhou SF, Yang LP, Zhou ZW, Liu YH, Chan E (2009) Insights into the substrate specificity, inhibitors, regulation, and polymorphisms and the clinical impact of human cytochrome P450 1A2. AAPS J 11(3):481–494
Zhou SF, Di YM, Chan E, Du YM, Chow VD, Xue CC, Lai X, Wang JC, Li CG, Tian M, Duan W (2008) Clinical pharmacogenetics and potential application in personalized medicine. Curr Drug Metab 9(8):738–784
Gunes A, Dahl ML (2008) Variation in CYP1A2 activity and its clinical implications: influence of environmental factors and genetic polymorphisms. Pharmacogenomics 9(5):625–637
Guengerich FP, Shimada T (1998) Activation of procarcinogens by human cytochrome P450 enzymes. Mutat Res 400(1–2):201–213
Ikeya K, Jaiswal AK, Owens RA, Jones JE, Nebert DW, Kimura S (1989) Human CYP1A2: sequence, gene structure, comparison with the mouse and rat orthologous gene, and differences in liver 1A2 mRNA expression. Mol Endocrinol 3(9):1399–1408
Zhou SF, Liu JP, Chowbay B (2009) Polymorphism of human cytochrome P450 enzymes and its clinical impact. Drug Metab Rev 41(2):89–295
Kall MA, Clausen J (1995) Dietary effect on mixed function P450 1A2 activity assayed by estimation of caffeine metabolism in man. Hum Exp Toxicol 14(10):801–807
Relling MV, Lin JS, Ayers GD, Evans WE (1992) Racial and gender differences in N-acetyltransferase, xanthine oxidase, and CYP1A2 activities. Clin Pharmacol Ther 52(6):643–658
Ghotbi R, Christensen M, Roh HK, Ingelman-Sundberg M, Aklillu E, Bertilsson L (2007) Comparisons of CYP1A2 genetic polymorphisms, enzyme activity and the genotype-phenotype relationship in Swedes and Koreans. Eur J Clin Pharmacol 63(6):537–546
Sachse C, Brockmoller J, Bauer S, Roots I (1999) Functional significance of a C→A polymorphism in intron 1 of the cytochrome P450 CYP1A2 gene tested with caffeine. Br J Clin Pharmacol 47(4):445–449
Han XM, Ouyang DS, Chen XP, Shu Y, Jiang CH, Tan ZR, Zhou HH (2002) Inducibility of CYP1A2 by omeprazole in vivo related to the genetic polymorphism of CYP1A2. Br J Clin Pharmacol 54(5):540–543
Aklillu E, Carrillo JA, Makonnen E, Hellman K, Pitarque M, Bertilsson L, Ingelman-Sundberg M (2003) Genetic polymorphism of CYP1A2 in Ethiopians affecting induction and expression: characterization of novel haplotypes with single-nucleotide polymorphisms in intron 1. Mol Pharmacol 64(3):659–669
Eap CB, Bender S, Jaquenoud Sirot E, Cucchia G, Jonzier-Perey M, Baumann P, Allorge D, Broly F (2004) Nonresponse to clozapine and ultrarapid CYP1A2 activity: clinical data and analysis of CYP1A2 gene. J Clin Psychopharmacol 24(2):214–219
Ozdemir V, Kalow W, Okey AB, Lam MS, Albers LJ, Reist C, Fourie J, Posner P, Collins EJ, Roy R (2001) Treatment-resistance to clozapine in association with ultrarapid CYP1A2 activity and the C→A polymorphism in intron 1 of the CYP1A2 gene: effect of grapefruit juice and low-dose fluvoxamine. J Clin Psychopharmacol 21(6):603–607
Melkersson KI, Scordo MG, Gunes A, Dahl ML (2007) Impact of CYP1A2 and CYP2D6 polymorphisms on drug metabolism and on insulin and lipid elevations and insulin resistance in clozapine-treated patients. J Clin Psychiatry 68(5):697–704
Pavanello S, Mastrangelo G, Placidi D, Campagna M, Pulliero A, Carta A, Arici C, Porru S (2010) CYP1A2 polymorphisms, occupational and environmental exposures and risk of bladder cancer. Eur J Epidemiol 25(7):491–500
B’Chir F, Pavanello S, Knani J, Boughattas S, Arnaud MJ, Saguem S (2009) CYP1A2 genetic polymorphisms and adenocarcinoma lung cancer risk in the Tunisian population. Life Sci 84(21–22):779–784
Olivieri EH, da Silva SD, Mendonca FF, Urata YN, Vidal DO, Faria Mde A, Nishimoto IN, Rainho CA, Kowalski LP, Rogatto SR (2009) CYP1A2*1C, CYP2E1*5B, and GSTM1 polymorphisms are predictors of risk and poor outcome in head and neck squamous cell carcinoma patients. Oral Oncol 45(9):e73–e79
Xu C, Goodz S, Sellers EM, Tyndale RF (2002) CYP2A6 genetic variation and potential consequences. Adv Drug Deliv Rev 54(10):1245–1256
Kamataki T, Fujieda M, Kiyotani K, Iwano S, Kunitoh H (2005) Genetic polymorphism of CYP2A6 as one of the potential determinants of tobacco-related cancer risk. Biochem Biophys Res Commun 338(1):306–310
Malaiyandi V, Sellers EM, Tyndale RF (2005) Implications of CYP2A6 genetic variation for smoking behaviors and nicotine dependence. Clin Pharmacol Ther 77(3):145–158
Mwenifumbo JC, Tyndale RF (2009) Molecular genetics of nicotine metabolism. Handb Exp Pharmacol 192:235–259
Pearce R, Greenway D, Parkinson A (1992) Species differences and interindividual variation in liver microsomal cytochrome P450 2A enzymes: effects on coumarin, dicumarol, and testosterone oxidation. Arch Biochem Biophys 298(1):211–225
Holzinger ER, Grady B, Ritchie MD, Ribaudo HJ, Acosta EP, Morse GD, Gulick RM, Robbins GK, Clifford DB, Daar ES, McLaren P, Haas DW (2012) Genome-wide association study of plasma efavirenz pharmacokinetics in AIDS Clinical Trials Group protocols implicates several CYP2B6 variants. Pharmacogenet Genomics 22(12):858–867
Turpeinen M, Raunio H, Pelkonen O (2006) The functional role of CYP2B6 in human drug metabolism: substrates and inhibitors in vitro, in vivo and in silico. Curr Drug Metab 7(7):705–714
Owen A, Pirmohamed M, Khoo SH, Back DJ (2006) Pharmacogenetics of HIV therapy. Pharmacogenet Genomics 16(10):693–703
Jinno H, Tanaka-Kagawa T, Ohno A, Makino Y, Matsushima E, Hanioka N, Ando M (2003) Functional characterization of cytochrome P450 2B6 allelic variants. Drug Metab Dispos 31(4):398–403
Rotger M, Tegude H, Colombo S, Cavassini M, Furrer H, Decosterd L, Blievernicht J, Saussele T, Gunthard HF, Schwab M, Eichelbaum M, Telenti A, Zanger UM (2007) Predictive value of known and novel alleles of CYP2B6 for efavirenz plasma concentrations in HIV-infected individuals. Clin Pharmacol Ther 81(4):557–566
Wang J, Sonnerborg A, Rane A, Josephson F, Lundgren S, Stahle L, Ingelman-Sundberg M (2006) Identification of a novel specific CYP2B6 allele in Africans causing impaired metabolism of the HIV drug efavirenz. Pharmacogenet Genomics 16(3):191–198
Ishikawa C, Ozaki H, Nakajima T, Ishii T, Kanai S, Anjo S, Shirai K, Inoue I (2004) A frameshift variant of CYP2C8 was identified in a patient who suffered from rhabdomyolysis after administration of cerivastatin. J Hum Genet 49(10):582–585
Ozaki H, Ishikawa CT, Ishii T, Toyoda A, Murano T, Miyashita Y, Shirai K (2005) Clearance rates of cerivastatin metabolites in a patient with cerivastatin-induced rhabdomyolysis. J Clin Pharm Ther 30(2):189–192
Bahadur N, Leathart JB, Mutch E, Steimel-Crespi D, Dunn SA, Gilissen R, Houdt JV, Hendrickx J, Mannens G, Bohets H, Williams FM, Armstrong M, Crespi CL, Daly AK (2002) CYP2C8 polymorphisms in Caucasians and their relationship with paclitaxel 6alpha-hydroxylase activity in human liver microsomes. Biochem Pharmacol 64(11):1579–1589
Soyama A, Saito Y, Komamura K, Ueno K, Kamakura S, Ozawa S, Sawada J (2002) Five novel single nucleotide polymorphisms in the CYP2C8 gene, one of which induces a frame-shift. Drug Metab Pharmacokinet 17(4):374–377
Cavaco I, Stromberg-Norklit J, Kaneko A, Msellem MI, Dahoma M, Ribeiro VL, Bjorkman A, Gil JP (2005) CYP2C8 polymorphism frequencies among malaria patients in Zanzibar. Eur J Clin Pharmacol 61(1):15–18
Rodriguez-Antona C, Niemi M, Backman JT, Kajosaari LI, Neuvonen PJ, Robledo M, Ingelman-Sundberg M (2008) Characterization of novel CYP2C8 haplotypes and their contribution to paclitaxel and repaglinide metabolism. Pharmacogenomics J 8(4):268–277
Ferguson SS, LeCluyse EL, Negishi M, Goldstein JA (2002) Regulation of human CYP2C9 by the constitutive androstane receptor: discovery of a new distal binding site. Mol Pharmacol 62(3):737–746
Si D, Guo Y, Zhang Y, Yang L, Zhou H, Zhong D (2004) Identification of a novel variant CYP2C9 allele in Chinese. Pharmacogenetics 14(7):465–469
Maekawa K, Harakawa N, Sugiyama E, Tohkin M, Kim SR, Kaniwa N, Katori N, Hasegawa R, Yasuda K, Kamide K, Miyata T, Saito Y, Sawada J (2009) Substrate-dependent functional alterations of seven CYP2C9 variants found in Japanese subjects. Drug Metab Dispos 37(9):1895–1903
Schwarz UI (2003) Clinical relevance of genetic polymorphisms in the human CYP2C9 gene. Eur J Clin Investig 33(Suppl 2):23–30
Thijssen HH, Ritzen B (2003) Acenocoumarol pharmacokinetics in relation to cytochrome P450 2C9 genotype. Clin Pharmacol Ther 74(1):61–68
Kirchheiner J, Brockmoller J (2005) Clinical consequences of cytochrome P450 2C9 polymorphisms. Clin Pharmacol Ther 77(1):1–16
Desta Z, Zhao X, Shin JG, Flockhart DA (2002) Clinical significance of the cytochrome P450 2C19 genetic polymorphism. Clin Pharmacokinet 41(12):913–958
Sagar M, Tybring G, Dahl ML, Bertilsson L, Seensalu R (2000) Effects of omeprazole on intragastric pH and plasma gastrin are dependent on the CYP2C19 polymorphism. Gastroenterology 119(3):670–676
Kazui M, Nishiya Y, Ishizuka T, Hagihara K, Farid NA, Okazaki O, Ikeda T, Kurihara A (2010) Identification of the human cytochrome P450 enzymes involved in the two oxidative steps in the bioactivation of clopidogrel to its pharmacologically active metabolite. Drug Metab Dispos 38(1):92–99
Collet JP, Hulot JS, Anzaha G, Pena A, Chastre T, Caron C, Silvain J, Cayla G, Bellemain-Appaix A, Vignalou JB, Galier S, Barthelemy O, Beygui F, Gallois V, Montalescot G (2011) High doses of clopidogrel to overcome genetic resistance: the randomized crossover CLOVIS-2 (Clopidogrel and Response Variability Investigation Study 2). JACC Cardiovasc Interv 4(4):392–402
Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, Walker JR, Antman EM, Macias W, Braunwald E, Sabatine MS (2009) Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med 360(4):354–362
Sim SC, Risinger C, Dahl ML, Aklillu E, Christensen M, Bertilsson L, Ingelman-Sundberg M (2006) A common novel CYP2C19 gene variant causes ultrarapid drug metabolism relevant for the drug response to proton pump inhibitors and antidepressants. Clin Pharmacol Ther 79(1):103–113
Baldwin RM, Ohlsson S, Pedersen RS, Mwinyi J, Ingelman-Sundberg M, Eliasson E, Bertilsson L (2008) Increased omeprazole metabolism in carriers of the CYP2C19*17 allele; a pharmacokinetic study in healthy volunteers. Br J Clin Pharmacol 65(5):767–774
Teh LK, Bertilsson L (2012) Pharmacogenomics of CYP2D6: molecular genetics, interethnic differences and clinical importance. Drug Metab Pharmacokinet 27(1):55–67
Nakamura K, Goto F, Ray WA, McAllister CB, Jacqz E, Wilkinson GR, Branch RA (1985) Interethnic differences in genetic polymorphism of debrisoquin and mephenytoin hydroxylation between Japanese and Caucasian populations. Clin Pharmacol Ther 38(4):402–408
Lee EJ, Nam YP, Hee GN (1988) Oxidation phenotyping in Chinese and Malay populations. Clin Exp Pharmacol Physiol 15(11):889–891
Bertilsson L, Lou YQ, Du YL, Liu Y, Kuang TY, Liao XM, Wang KY, Reviriego J, Iselius L, Sjoqvist F (1992) Pronounced differences between native Chinese and Swedish populations in the polymorphic hydroxylations of debrisoquin and S-mephenytoin. Clin Pharmacol Ther 51(4):388–97106
Roh HK, Dahl ML, Johansson I, Ingelman-Sundberg M, Cha YN, Bertilsson L (1996) Debrisoquine and S-mephenytoin hydroxylation phenotypes and genotypes in a Korean population. Pharmacogenetics 6(5):441–447
Tateishi T, Chida M, Ariyoshi N, Mizorogi Y, Kamataki T, Kobayashi S (1999) Analysis of the CYP2D6 gene in relation to dextromethorphan O-demethylation capacity in a Japanese population. Clin Pharmacol Ther 65(5):570–575
Johansson I, Oscarson M, Yue QY, Bertilsson L, Sjoqvist F, Ingelman-Sundberg M (1994) Genetic analysis of the Chinese cytochrome P4502D locus: characterization of variant CYP2D6 genes present in subjects with diminished capacity for debrisoquine hydroxylation. Mol Pharmacol 46(3):452–459
Masimirembwa C, Persson I, Bertilsson L, Hasler J, Ingelman-Sundberg M (1996) A novel mutant variant of the CYP2D6 gene (CYP2D6*17) common in a black African population: association with diminished debrisoquine hydroxylase activity. Br J Clin Pharmacol 42(6):713–719
Koren G, Cairns J, Chitayat D, Gaedigk A, Leeder SJ (2006) Pharmacogenetics of morphine poisoning in a breastfed neonate of a codeine-prescribed mother. Lancet 368(9536):704
Kawanishi C, Lundgren S, Agren H, Bertilsson L (2004) Increased incidence of CYP2D6 gene duplication in patients with persistent mood disorders: ultrarapid metabolism of antidepressants as a cause of nonresponse. A pilot study. Eur J Clin Pharmacol 59(11):803–807
Borges S, Desta Z, Li L, Skaar TC, Ward BA, Nguyen A, Jin Y, Storniolo AM, Nikoloff DM, Wu L, Hillman G, Hayes DF, Stearns V, Flockhart DA (2006) Quantitative effect of CYP2D6 genotype and inhibitors on tamoxifen metabolism: implication for optimization of breast cancer treatment. Clin Pharmacol Ther 80(1):61–74
Gjerde J, Hauglid M, Breilid H, Lundgren S, Varhaug JE, Kisanga ER, Mellgren G, Steen VM, Lien EA (2008) Effects of CYP2D6 and SULT1A1 genotypes including SULT1A1 gene copy number on tamoxifen metabolism. Ann Oncol 19(1):56–61
Jin Y, Desta Z, Stearns V, Ward B, Ho H, Lee KH, Skaar T, Storniolo AM, Li L, Araba A, Blanchard R, Nguyen A, Ullmer L, Hayden J, Lemler S, Weinshilboum RM, Rae JM, Hayes DF, Flockhart DA (2005) CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst 97(1):30–39
Bijl MJ, van Schaik RH, Lammers LA, Hofman A, Vulto AG, van Gelder T, Stricker BH, Visser LE (2009) The CYP2D6*4 polymorphism affects breast cancer survival in tamoxifen users. Breast Cancer Res Treat 118(1):125–130
Goetz MP, Knox SK, Suman VJ, Rae JM, Safgren SL, Ames MM, Visscher DW, Reynolds C, Couch FJ, Lingle WL, Weinshilboum RM, Fritcher EG, Nibbe AM, Desta Z, Nguyen A, Flockhart DA, Perez EA, Ingle JN (2007) The impact of cytochrome P450 2D6 metabolism in women receiving adjuvant tamoxifen. Breast Cancer Res Treat 101(1):113–121
Schroth W, Antoniadou L, Fritz P, Schwab M, Muerdter T, Zanger UM, Simon W, Eichelbaum M, Brauch H (2007) Breast cancer treatment outcome with adjuvant tamoxifen relative to patient CYP2D6 and CYP2C19 genotypes. J Clin Oncol 25(33):5187–5193
Stamer UM, Musshoff F, Kobilay M, Madea B, Hoeft A, Stuber F (2007) Concentrations of tramadol and O-desmethyltramadol enantiomers in different CYP2D6 genotypes. Clin Pharmacol Ther 82(1):41–47
Stamer UM, Lehnen K, Hothker F, Bayerer B, Wolf S, Hoeft A, Stuber F (2003) Impact of CYP2D6 genotype on postoperative tramadol analgesia. Pain 105(1–2):231–238
El-Mallakh RS, Roberts RJ, El-Mallakh PL, Findlay LJ, Reynolds KK (2016) Pharmacogenomics in psychiatric practice. Clin Lab Med 36(3):507–523
Wojnowski L, Kamdem LK (2006) Clinical implications of CYP3A polymorphisms. Expert Opin Drug Metab Toxicol 2(2):171–182
Lakhman SS, Ma Q, Morse GD (2009) Pharmacogenomics of CYP3A: considerations for HIV treatment. Pharmacogenomics 10(8):1323–1339
Williams JA, Ring BJ, Cantrell VE, Jones DR, Eckstein J, Ruterbories K, Hamman MA, Hall SD, Wrighton SA (2002) Comparative metabolic capabilities of CYP3A4, CYP3A5, and CYP3A7. Drug Metab Dispos 30(8):883–891
Hirota T, Ieiri I, Takane H, Maegawa S, Hosokawa M, Kobayashi K, Chiba K, Nanba E, Oshimura M, Sato T, Higuchi S, Otsubo K (2004) Allelic expression imbalance of the human CYP3A4 gene and individual phenotypic status. Hum Mol Genet 13(23):2959–2969
Hustert E, Zibat A, Presecan-Siedel E, Eiselt R, Mueller R, Fuss C, Brehm I, Brinkmann U, Eichelbaum M, Wojnowski L, Burk O (2001) Natural protein variants of pregnane X receptor with altered transactivation activity toward CYP3A4. Drug Metab Dispos 29(11):1454–1459
Kuehl P, Zhang J, Lin Y, Lamba J, Assem M, Schuetz J, Watkins PB, Daly A, Wrighton SA, Hall SD, Maurel P, Relling M, Brimer C, Yasuda K, Venkataramanan R, Strom S, Thummel K, Boguski MS, Schuetz E (2001) Sequence diversity in CYP3A promoters and characterization of the genetic basis of polymorphic CYP3A5 expression. Nat Genet 27(4):383–391
Lee SJ, Usmani KA, Chanas B, Ghanayem B, Xi T, Hodgson E, Mohrenweiser HW, Goldstein JA (2003) Genetic findings and functional studies of human CYP3A5 single nucleotide polymorphisms in different ethnic groups. Pharmacogenetics 13(8):461–472
Stevens JC, Hines RN, Gu C, Koukouritaki SB, Manro JR, Tandler PJ, Zaya MJ (2003) Developmental expression of the major human hepatic CYP3A enzymes. J Pharmacol Exp Ther 307(2):573–582
Lee SS, Jung HJ, Park JS, Cha IJ, Cho DY, Shin JG (2010) Identification of a null allele of cytochrome P450 3A7: CYP3A7 polymorphism in a Korean population. Mol Biol Rep 37(1):213–217
Rodriguez-Antona C, Sayi JG, Gustafsson LL, Bertilsson L, Ingelman-Sundberg M (2005) Phenotype-genotype variability in the human CYP3A locus as assessed by the probe drug quinine and analyses of variant CYP3A4 alleles. Biochem Biophys Res Commun 338(1):299–305
Leeder JS, Gaedigk R, Marcucci KA, Gaedigk A, Vyhlidal CA, Schindel BP, Pearce RE (2005) Variability of CYP3A7 expression in human fetal liver. J Pharmacol Exp Ther 314(2):626–635
Sim SC, Edwards RJ, Boobis AR, Ingelman-Sundberg M (2005) CYP3A7 protein expression is high in a fraction of adult human livers and partially associated with the CYP3A7*1C allele. Pharmacogenet Genomics 15(9):625–631
Smit P, van Schaik RH, van der Werf M, van den Beld AW, Koper JW, Lindemans J, Pols HA, Brinkmann AO, de Jong FH, Lamberts SW (2005) A common polymorphism in the CYP3A7 gene is associated with a nearly 50% reduction in serum dehydroepiandrosterone sulfate levels. J Clin Endocrinol Metab 90(9):5313–5316
Hasegawa Y, Ando Y, Shimokata K (2006) Screening for adverse reactions to irinotecan treatment using the invader UGT1A1 molecular assay. Expert Rev Mol Diagn 6(4):527–533
Burchell B, Soars M, Monaghan G, Cassidy A, Smith D, Ethell B (2000) Drug-mediated toxicity caused by genetic deficiency of UDP-glucuronosyltransferases. Toxicol Lett 112-113:333–340
Satoh T, Ura T, Yamada Y, Yamazaki K, Tsujinaka T, Munakata M, Nishina T, Okamura S, Esaki T, Sasaki Y, Koizumi W, Kakeji Y, Ishizuka N, Hyodo I, Sakata Y (2011) Genotype-directed, dose-finding study of irinotecan in cancer patients with UGT1A1*28 and/or UGT1A1*6 polymorphisms. Cancer Sci 102(10):1868–1873
Rodriguez-Novoa S, Barreiro P, Jimenez-Nacher I, Soriano V (2006) Overview of the pharmacogenetics of HIV therapy. Pharmacogenomics J 6(4):234–245
Woillard JB, Rerolle JP, Picard N, Rousseau A, Drouet M, Munteanu E, Essig M, Marquet P, Le Meur Y (2010) Risk of diarrhoea in a long-term cohort of renal transplant patients given mycophenolate mofetil: the significant role of the UGT1A8 2 variant allele. Br J Clin Pharmacol 69(6):675–683
Daly AK, Aithal GP, Leathart JB, Swainsbury RA, Dang TS, Day CP (2007) Genetic susceptibility to diclofenac-induced hepatotoxicity: contribution of UGT2B7, CYP2C8, and ABCC2 genotypes. Gastroenterology 132(1):272–281
Salavaggione OE, Wang L, Wiepert M, Yee VC, Weinshilboum RM (2005) Thiopurine S-methyltransferase pharmacogenetics: variant allele functional and comparative genomics. Pharmacogenet Genomics 15(11):801–815
Lachman HM, Papolos DF, Saito T, Yu YM, Szumlanski CL, Weinshilboum RM (1996) Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics 6(3):243–250
Meyer UA, Zanger UM (1997) Molecular mechanisms of genetic polymorphisms of drug metabolism. Annu Rev Pharmacol Toxicol 37:269–296
Nowell S, Sweeney C, Winters M, Stone A, Lang NP, Hutchins LF, Kadlubar FF, Ambrosone CB (2002) Association between sulfotransferase 1A1 genotype and survival of breast cancer patients receiving tamoxifen therapy. J Natl Cancer Inst 94(21):1635–1640
Peklak-Scott C, Smitherman PK, Townsend AJ, Morrow CS (2008) Role of glutathione S-transferase P1-1 in the cellular detoxification of cisplatin. Mol Cancer Ther 7(10):3247–3255
Sweeney C, Ambrosone CB, Joseph L, Stone A, Hutchins LF, Kadlubar FF, Coles BF (2003) Association between a glutathione S-transferase A1 promoter polymorphism and survival after breast cancer treatment. Int J Cancer 103(6):810–814
Slattery JT, Sanders JE, Buckner CD, Schaffer RL, Lambert KW, Langer FP, Anasetti C, Bensinger WI, Fisher LD, Appelbaum FR et al (1995) Graft-rejection and toxicity following bone marrow transplantation in relation to busulfan pharmacokinetics. Bone Marrow Transplant 16(1):31–42
Ley RE, Hamady M, Lozupone C, Turnbaugh PJ, Ramey RR, Bircher JS, Schlegel ML, Tucker TA, Schrenzel MD, Knight R, Gordon JI (2008) Evolution of mammals and their gut microbes. Science 320(5883):1647–1651
O’Hara AM, Shanahan F (2006) The gut flora as a forgotten organ. EMBO Rep 7(7):688–693
Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M, Gill SR, Nelson KE, Relman DA (2005) Diversity of the human intestinal microbial Flora. Science 308(5728):1635–1638
Ferreira CM, Vieira AT, Vinolo MAR, Oliveira FA, Curi R, Martins FDS (2014) The central role of the gut microbiota in chronic inflammatory diseases. J Immunol Res 2014:12
Forslund K, Hildebrand F, Nielsen T, Falony G, Le Chatelier E, Sunagawa S, Prifti E, Vieira-Silva S, Gudmundsdottir V, Krogh Pedersen H, Arumugam M, Kristiansen K, Yvonne Voigt A, Vestergaard H, Hercog R, Igor Costea P, Roat Kultima J, Li J, Jørgensen T, Levenez F, Dore J, Meta HIT c, Bjørn Nielsen H, Brunak S, Raes J, Hansen T, Wang J, Dusko Ehrlich S, Bork P, Pedersen O (2015) Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 528(7581):262–266
Koeth RA, Wang Z, Levison BS, Buffa JA, Org E, Sheehy BT, Britt EB, Fu X, Wu Y, Li L, Smith JD, DiDonato JA, Chen J, Li H, Wu GD, Lewis JD, Warrier M, Brown JM, Krauss RM, Tang WHW, Bushman FD, Lusis AJ, Hazen SL (2013) Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med 19(5):576–585
Mikov M (1994) The metabolism of drugs by the gut flora. Eur J Drug Metab Pharmacokinet 19(3):201–207
Kang MJ, Kim HG, Kim JS, Oh DG, Um YJ, Seo CS, Han JW, Cho HJ, Kim GH, Jeong TC, Jeong HG (2013) The effect of gut microbiota on drug metabolism. Expert Opin Drug Metab Toxicol 9(10):1295–1308
Jourova L, Anzenbacher P, Anzenbacherova E (2016) Human gut microbiota plays a role in the metabolism of drugs. Biomed Pap 160(3):317–326
Saad R, Rizkallah MR, Aziz RK (2012) Gut Pharmacomicrobiomics: the tip of an iceberg of complex interactions between drugs and gut-associated microbes. Gut Pathog 4(1):1–13
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Gupta, S.V. (2018). Genomics and Drug-Metabolizing Enzymes and Its Application in Drug Delivery: Evaluating the Influence of the Microbiome. In: Pathak, Y. (eds) Genomics-Driven Healthcare. Adis, Singapore. https://doi.org/10.1007/978-981-10-7506-3_9
Download citation
DOI: https://doi.org/10.1007/978-981-10-7506-3_9
Published:
Publisher Name: Adis, Singapore
Print ISBN: 978-981-10-7505-6
Online ISBN: 978-981-10-7506-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)