Abstract
Uterine leiomyoma shows a wide spectrum of morphologies and clinicopathological features. Thus, in both the clinical and pathological settings, it can be difficult to distinguish from leiomyosarcoma. In particular, patients scheduled for conservative laparoscopic procedures need careful preoperative evaluation, because in rare cases microscopic examination may instead reveal leiomyosarcoma. Clinicians should therefore be familiar with the variety of manifestations and imaging characteristics of both leiomyoma and leiomyosarcoma. In this chapter, the morphologic features and current diagnostic criteria for leiomyoma, as opposed to leiomyosarcoma, and the controversies regarding the diagnosis of borderline tumors are presented. The focus includes smooth muscle tumors of uncertain malignant potential.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1.1 Introduction
Leiomyoma, also called “fibroid,” is the most common benign mesenchymal tumor of the uterus. It shows a wide spectrum of morphologies and clinicopathological features such that both clinically and pathologically it can be difficult to distinguish leiomyoma from leiomyosarcoma. In the current standard of practice, patients favor conservative treatment of leiomyoma, especially laparoscopic surgery employing morcellation, rather than hysterectomy. However, in rare cases, on subsequent microscopic examination, the resected tumor will be diagnosed as leiomyosarcoma. Therefore, the preoperative evaluation of patients with suspected leiomyoma is crucial and requires that clinicians are familiar with the various clinicopathological expressions and imaging characteristics of leiomyoma and leiomyosarcoma. In this chapter, the morphologic features and current diagnostic criteria for leiomyoma, as distinct from leiomyosarcoma, are presented. The controversies regarding the diagnosis of borderline tumors are discussed as well, focusing on smooth muscle tumors of uncertain malignant potential (STUMPs).
1.2 General Aspects and Clinical Features
Leiomyoma is defined as a benign smooth muscle tumor characterized by a variety of morphological features. As the most common uterine neoplasm, it is identified in up to 75% of hysterectomy specimens. The uterine corpus accounts for 98% of the anatomic sites, and among up to 80% of patients, multiple tumors are detected. Although the majority of leiomyomas are asymptomatic, one-third of the patients will show clinical manifestations within the reproductive ages of 30–50, and 10% will undergo surgical management of the tumor. The clinical manifestation of leiomyoma depends on the size, location, and secondary changes of the tumor. Common symptoms include pelvic pain, mass, and genital bleeding. In pregnant women, the tumor may rapidly enlarge, while in menopausal women or those who have undergone oophorectomy, the mass typically shrinks. Leukocytosis occurs in association with secondary infection; erythrocytosis is rare and is induced by erythropoietin production by the tumor.
The management of leiomyoma patients varies based on the clinical manifestations and patient preference. Treatment options range from hormonal therapy to the removal of the tumor(s), whether by enucleation or total hysterectomy. Minimally invasive surgery, and specifically morcellation, has recently gained wider acceptance because of the short recovery time and the resulting improvement in the quality of life following tumor removal. However, careful preoperative evaluation of patients with suspected leiomyoma is mandatory because the diagnosis may turn out to be leiomyosarcoma. The latter accounts for 1–2% of all uterine malignancies, and in these cases the minimal procedure is inappropriate. The incidence of these unsuspected leiomyosarcomas is estimated to be <1% [1, 2]. Parker et al. reported that only one of 371 cases of apparent leiomyoma proved to be leiomyosarcoma [3]. Seidman reported that among 1091 uterine mesenchymal tumors removed by morcellation, two (0.18%) were malignant, including one endometrial stromal sarcoma (ESS) and one leiomyosarcoma [4]. In that particular series, surveillance was followed by laparotomy in 14 patients, and in nine (64.3%) intra-abdominal dissemination was identified, which included one cellular leiomyoma, four STUMPs, and four leiomyosarcomas [4]. A constellation of findings, including rapid enlargement of the mass, tumor heterogeneity, and the possible presence of necrosis, as seen on imaging studies, suggests the diagnosis of leiomyosarcoma. Such cases are deemed “suspicious,” which is an indication for hysterectomy. However, there is significant overlap in the clinical features of leiomyoma and leiomyosarcoma, and rapid enlargement of the tumor per se is a non-specific finding. Chan et al. reported older age, black race, large tumor size, and extrauterine disease as factors suggestive of leiomyosarcoma, based on data retrieved from the Surveillance, Epidemiology, and End Results database [5].
1.3 Pathological Features
The current WHO classification, published in 2014, defines eight morphologic subtypes and four variants of leiomyoma. The latter, which account for approximately 10% of cases, are characterized by distinct growth patterns and clinicopathological features (Table 1.1) [6].
1.3.1 Gross Features
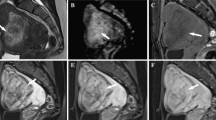
Uterine leiomyomas are typically multiple. Individual tumors range from 5 to 10 cm in their greatest dimension and can be microscopic or form a bulky mass exceeding 10 cm (Fig. 1.1a). On gross examination, these tumors are typically elastic hard, well-demarcated, and have smooth borders. Their cut surfaces are whitish to grayish, with a whorl or arabesque appearance due to interlacing fascicles of smooth muscle cells (Fig. 1.1b). Highly cellular variants and lipoleiomyoma may be yellowish in color (Fig. 1.1c); the former tend to be soft and fleshy on their cut surfaces. Secondary changes in the gross appearance of these tumors consist of hydropic changes, infarction-type necrosis (Fig. 1.1d), cystic degeneration, and dystrophic calcifications. Hydropic portions are translucent and in rare cases may result in the formation of a cystic cavity due to the accumulation of extracellular fluid. Hydropic change is also a feature of dissecting (cotyledonoid) leiomyoma. Infarction-type necrosis is recognized by the reddish to tan color of the tumor and is referred to as “beefy-red” or “red degeneration.” The ill-defined, confluent intramyometrial growth of numerous nodules is a characteristic of diffuse leiomyomatosis, and intravenous growth is seen in intravenous leiomyomatosis.
Leiomyoma. (a) The gross features of the cut surface show well-demarcated, whitish to grayish nodules in the myometrium. (b) Whorl formation due to interlacing fascicles of neoplastic cells, seen on the tumor’s cut surface. (c) Lipoleiomyoma is recognizable by its yellowish cut surface, due to the intermingling of mature adipocytes. (d) Tan and friable areas indicate infarct-type degeneration
Depending on the location, uterine leiomyoma is divided into submucosal, intramural (interstitial), and subserosal leiomyomas. Subserosal and submucosal tumors can be pedunculated, with a narrow pedicle. Pedunculated submucosal leiomyoma may protrude through the cervical canal and external os. Occasionally, detachment of the tumor from the uterus results in a so-called parasitic leiomyoma. The gross features of typical leiomyoma vs. leiomyosarcoma are summarized in Fig. 1.2 and Table 1.2.
1.3.2 Microscopic Features
Leiomyoma is typically composed of interlacing fascicles of spindle cells with an eosinophilic fibrillary cytoplasm (Fig. 1.3). The cell borders are indistinct, and the nuclei are elongated and blunt-ended (cigar-shaped). Nucleoli are absent or small, and mitotic figures are minimal. Nuclear palisading, thus mimicking schwannoma, is seen in some leiomyomas (Fig. 1.4). In the ordinary leiomyoma of pregnant patients, the cells may show nuclear enlargement, an abundant cytoplasm, and increased mitotic figures (Fig. 1.5). As mentioned above, secondary changes occur to various degrees in these tumors.
1.3.2.1 Cellular Leiomyoma
Occasionally, leiomyoma will show hypercellularity when compared with the normal myometrium of the uterine corpus and is thus referred to as a cellular leiomyoma (Fig. 1.6). The term “hypercellular” describes tumors with features of blue-cell tumor and a resemblance to endometrial stromal nodule or low-grade ESS. The neoplastic cells are short and spindle-shaped, with scant cytoplasm and a homogeneous nuclear morphology. The fascicular pattern may be obscured, particularly in the central area.
1.3.2.2 Leiomyoma with Bizarre Nuclei
Previously called atypical leiomyoma, symplastic leiomyoma, or bizarre leiomyoma, this variant is characterized by an admixture of large cells with multilobated or multiple nuclei that have an irregular configuration and nuclear hyperchromatism. These cells occur against a background of ordinary leiomyoma (Fig. 1.7). The distribution of the bizarre cells ranges from only focal to extensive. Frequently, the nuclei are smudgy and may show intranuclear cytoplasmic pseudo-inclusions. Mitotic figures are minimal, and coagulative tumor necrosis is absent, although infarct-type areas may be seen. Recent studies suggest that this variant is genetically heterogeneous. In a subset of cases, somatic mutation or deletion of the fumarate hydratase gene is detected [7, 8]. These tumors are characterized by staghorn vessels, prominent eosinophilic nucleoli with perinuclear halos, and eosinophilic cytoplasmic pseudo-inclusions, which are also features of hereditary leiomyomatosis and renal cell carcinoma, as discussed below [7]. The patients with this particular subtype show benign clinical course [9, 10].
1.3.2.3 Mitotically Active Leiomyoma
Tumor in which the number of mitotic figures is increased to 5 or more per 10 high-power fields (10HPF) and without coagulative tumor necrosis or diffuse moderate to severe nuclear atypia is diagnosed as mitotically active leiomyoma [6]. The mitotic counts may be more than 10 per 10HPF, but atypical mitotic figures are absent. This particular variant is frequently seen in women of reproductive age and may be associated with hormonal therapy. With their hypercellularity and/or bizarre nuclei, these tumors can be a diagnostic challenge.
1.3.2.4 Hydropic Leiomyoma
Liquefaction degeneration can be seen to varying degrees in leiomyoma (Fig. 1.8). Edematous change imparts a clear appearance to the tumor and when extensive results in cystic cavity formation, which should be distinguished from myxoid degeneration, described below. Tumors with extensive hydropic change may be confused with myxoid leiomyosarcoma and in those characterized by a perinodular distribution with intravenous leiomyomatosis [11].
1.3.2.5 Apoplectic Leiomyoma
This variant refers to a tumor with extensive infarct-type necrosis that develops in a patient on progesterone therapy. The necrotic area is generally extensive, and in the periphery there may be a granulation tissue-type reaction with or without hemorrhage (Fig. 1.9), surrounded by hypercellular areas with increased mitotic figures. In later stages, the necrotic foci are replaced by extensive hyalinization.
1.3.2.6 Lipomatous Leiomyoma (Lipoleiomyoma)
A mixture of ordinary leiomyoma and mature adipocytes defines lipomatous leiomyoma (Fig. 1.10). The adipocyte content varies, and tumors with abundant adipocytes appear yellowish on gross examination. While it is not uncommon to see a minimal number of adipocytes intermingled with leiomyoma, there are no quantitative criteria for the designation of this variant. Lipoleiomyoma may arise as a consequence of lipomatous metaplasia in a pre-existing leiomyoma. The subset of these tumors with anomalous arterial blood vessels is considered to be choristomatous in nature [12].
1.3.2.7 Epithelioid Leiomyoma
Epithelioid leiomyoma, previously called leiomyoblastoma, is composed of polyhedral, ovoid, or round cells with an eosinophilic cytoplasm. The cells are arranged in sheets, cords, trabeculae, nests, or individually (Fig. 1.11). Clear-cell features may also be detected in these tumors. Coagulative tumor necrosis is absent, and the number of mitotic figures is minimal. It should be kept in mild that epithelioid leiomyosarcoma can be cytologically bland and shows low mitotic activity. At least six mitotic figures per 10HPF justify the diagnosis of epithelioid leiomyosarcoma. The majority of tumors regarded as extrauterine “epithelioid leiomyoma” or “leiomyoblastoma” previously represent epithelioid form of extraintestinal GIST.
1.3.2.8 Myxoid Leiomyoma
The appearance of myxoid change, characterized by the accumulation of Alcian blue-positive acidic mucin between tumor cells, in a smooth muscle tumor is an alarming sign that should prompt the pathologist to consider myxoid leiomyosarcoma (Fig. 1.12). As in epithelioid leiomyosarcoma, mitotic activity is minimal, with only one to two mitoses per 10HPF indicative of malignancy. The diagnosis of myxoid leiomyoma also requires that the tumor is well-demarcated and has a smooth border and that mitotic figures should be two or less per 10HPF.
1.3.2.9 Dissecting (Cotyledonoid) Leiomyoma (“Sternberg Tumor”)
Rarely, a leiomyoma will dissect the myometrium to extend outside the uterus, in which case it is referred to as dissecting leiomyoma. Extensive protrusion and marked hydropic changes may impart a resemblance to cotyledon of the placenta and thus is designated as “cotyledonoid” (Fig. 1.13a, b) [13]. Microscopically, dissecting leiomyoma usually shows a swirling pattern of growth with extensive liquefaction degeneration (Fig. 1.13c).
1.3.2.10 Diffuse Leiomyomatosis
The extensive involvement of the myometrium by numerous leiomyomatous nodules that result in uterine enlargement is referred to as diffuse leiomyomatosis [14]. These nodules are mostly microscopic and poorly demarcated. Except for the growth pattern, the morphology is similar to that of ordinary leiomyoma (Fig. 1.14).
1.3.2.11 Intravenous Leiomyomatosis
This rare variant is characterized by an extensive, intravenous smooth muscle proliferation (Fig. 1.15) [15, 16]. The tumor frequently extends to vessels outside the myometrium, including the inferior vena cava, the cardiac cavity, and, in rare cases, the pulmonary artery. Morphologically, these leiomyomas are bland and may show features of cellular, epithelioid, lipomatous, or myxoid leiomyoma, or bizarre nuclei [16]. Since focal intravascular extension is also a feature of usual leiomyoma, this variant should be diagnosed based on the grossly visible worm-like appearance of the tumor. Rare cases of pulmonary metastasis have been reported as well [16, 17]. The clinical course is generally benign even in cases with metastasis [16, 17]. The pathogenesis of intravenous leiomyomatosis and benign metastasizing leiomyoma may be a vascular microinvasion of uterine leiomyoma in the initial phase of tumorigenesis [18].
1.3.2.12 Metastasizing Leiomyoma
Pulmonary nodules may be identified >10 years after a hysterectomy for uterine leiomyoma or in uncertain conditions [19]. Six pulmonary nodules measuring 1.8 cm in diameter are detected on average [19]. They show features of ordinary leiomyoma (Fig. 1.16a) and are thus well-demarcated and have a smooth border (Fig. 1.16b), but with pre-existing bronchiolar epithelium entrapped in the nodule (Fig. 1.16c). Some authors postulate that metastasizing leiomyoma is actually a slow-growing, low-grade leiomyosarcoma [19], but the term metastasizing leiomyoma has been retained because of the prolonged survival of patients after removal of the nodules and hormonal therapy.
1.3.3 Differential Diagnosis
Leiomyosarcoma, a malignant smooth muscle tumor, typically shows at least two of the following three features: (1) geographic coagulation tumor necrosis, (2) diffuse moderate and severe cytologic atypia, and (3) >10 mitotic figures per 10 HPF (Table 1.3) [20]. Hypercellularity and infiltrating growth are common. Epithelioid and myxoid variants can be pitfalls since the mitotic count is generally low. Thus, the criteria of five and two mitoses per 10HPF, respectively, and infiltrating growth should be employed in establishing the diagnosis of these leiomyosarcoma variants [21, 22]. Similar diagnostic criteria can be applied to distinguish diffuse leiomyomatosis, dissecting leiomyoma, intravenous leiomyomatosis, and metastasizing leiomyoma from leiomyosarcoma. Mimics of mitotic figures, including apoptotic bodies, karyorrhexis, aggregations of hematoxylin, and mast cells, should not be counted. Non-atypical mitosis may be seen in pregnant women or those on progesterone therapy. Infarct-type necrosis, also known as hyaline necrosis, is encountered in young women, especially in those who are pregnant or who are being treated with a gonadotropin-releasing hormone analog, such as leuprolide acetate, or by transarterial embolization. Torsion of a subserosal leiomyoma may result in the same morphology. In contrast to the extensive area of necrosis surrounded by a zone of gradual organization and marked by granulation tissue or hyalinization, geographic tumor necrosis is characterized by a spotty distribution and the irregular configuration of the necrotic areas, distinct borders, and preservation of the tumor vessels and surrounding neoplastic component. Immunohistochemical panels may be used to identify the tumor. The absence of estrogen receptor expression, a mutant pattern of p53 staining, p16 immunoreactivity, and an increased Ki-67 labeling index suggest the diagnosis of leiomyosarcoma, but the pathologist should be aware that in exceptional cases the tumor will be a leiomyosarcoma.
Endometrial stromal tumor, particularly stromal nodule and low-grade ESS, may be confused with cellular leiomyoma. The presence of both thick muscular vessels, in contrast to spiral artery-type small vessels, and a distinct interlacing fascicular pattern is indicative of leiomyoma. Immunohistochemical studies may be of limited value, because low-grade ESS occasionally shows smooth muscle differentiation and may thus be positive for smooth muscle markers, while leiomyoma may be diffusely and strongly positive for CD10, a marker of endometrial stromal cells [23]. Therefore, a constellation of findings, including growth pattern, cell morphology, and the results of immunohistochemistry using a panel of antibodies, is needed to establish the diagnosis.
Perivascular epithelioid cell tumor (PEComa) is a mimic of leiomyoma, although it is composed of rather spindle or epithelioid cells with clear or pale eosinophilic cytoplasm, showing vascular network. There may be extensive sclerosis. It can be associated with lymphangioleiomyomatosis and occasionally is associated with tuberous sclerosis. PEComa shows immunoreactivity for melanocytic markers including HMB45, Melan-A, and MiTF, as well as smooth muscle markers.
1.4 Hereditary Leiomyomatosis and Renal Cancer Syndrome (HLRCC)
This autosomal dominant disorder is associated with germline alterations in the fumarate hydratase gene, including point mutations and partial or complete deletions [24]. HLRCC is characterized by the coexistence of uterine and cutaneous leiomyomas and papillary renal cell carcinoma type 2 [25]. The type of renal cell carcinoma is diagnosed in approximately 30% of patients with this syndrome [24] and has an aggressive clinical behavior [26]. The patients tend to be younger than those with sporadic leiomyoma. Uterine tumor shows features of leiomyoma with bizarre nuclei. Prominent red or orange nucleoli with a perinuclear halo are considered to be a characteristic of HLRCC [7].
1.5 Extrauterine Leioyomatosis
Other than intravenous leiomyomatosis involving extrauterine vessels, in rare cases, including diffuse peritoneal leiomyomatosis and nodal leiomyomatosis [27], an extrauterine smooth muscle proliferation may be associated with uterine leiomyoma.
1.6 Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP)
STUMP is defined as a smooth muscle tumor in which the risks of recurrence and metastasis are uncertain; thus, the term refers to a diagnostic category rather than a distinct entity. STUMPs include (1) leiomyoma, (2) leiomyosarcoma that cannot be recognized as such based on the current diagnostic criteria, and (3) true borderline smooth muscle tumors that are biologically intermediate between leiomyoma and leiomyosarcoma. The third category appears to account for a minority of these cases. Indeed, limited sampling or limited experience may cause the pathologist to underevaluate leiomyosarcoma and instead diagnose STUMP. Therefore, the diagnosis of STUMP should be avoided as possible and is only rarely made.
From the clinical point of view, uterine smooth muscle tumor other than ordinary leiomyoma and leiomyosarcoma is classified as tumor with recurrent and/or metastatic potential and tumor with little or no recurrent and/or metastatic potential [2]. The former includes STUMP, intravenous leiomyomatosis, and benign metastasizing leiomyoma, whereas the latter leiomyoma with bizarre nuclei, mitotically active leiomyoma, cellular leiomyoma, dissecting leiomyoma, myxoid leiomyoma, epithelioid leiomyoma, and diffuse leiomyomatosis [2].
Morphologically, STUMPs are divided into tumors with prototypical smooth muscle differentiation and tumors with an unusual differentiation or uncharacteristic morphology, such as myxoid and epithelioid features. From the pathological point of view, ambiguity with respect to the nature of the necrosis, degree of differentiation, or mitotic count may prompt a pathological diagnosis of STUMP. For example, it may be difficult to distinguish coagulation necrosis from infarct-type necrosis. Epithelioid and myxoid leiomyosarcomas are diagnosed based on criteria that are different from those of the usual type of leiomyosarcoma. Tumors with a myxoid and epithelioid morphology with moderate to severe cytologic atypia and 5 or less and 2 more less mitotic figures per 10HPF, respectively, are categorized as STUMPs.
In a series from a single institution that included 16 cases of STUMP diagnosed by well-established criteria and with a follow-up interval of 21–192 months (mean, 80.8, and median, 51.5), Ip et al. reported that 2 patients (13%) had recurrent tumors in the pelvis, 51 and 15 months after the initial operation. Both patients were alive 74 and 48 months after recurrence, respectively [28]. The authors thus recommended that STUMP patients be followed every 6 months with a checkup of symptoms and general and pelvic examinations and every 12 months with imaging studies, including a chest X-ray to exclude pulmonary metastasis and pelvic ultrasonography, computed tomography, or magnetic resonance imaging to detect new lesions, for a minimum of 5 years, followed by annual surveillance for a further 5 years [2].
1.7 Prognosis and Predictive Factors
The clinical course of patients with the usual type of leiomyoma or its variants is benign, although a variety of complications may affect the quality of life in a subset of patients. In addition, variants such as intravenous leiomyomatosis may recur, including with inferior vena cava or intracardiac extension. Metastasizing leiomyoma also has an indolent clinical course but may cause respiratory failure due to the enlargement of the tumor.
Rare examples of leiomyosarcoma arising in leiomyoma have been described in the English medical literature [29]. Features of a bona fide leiomyoma may be identified in leiomyosarcoma, but the relationship between the two components is not well understood.
References
Leibsohn S, d’Ablaing G, Mishell DR Jr, Schlaerth JB. Leiomyosarcoma in a series of hysterectomies performed for presumed uterine leiomyomas. Am J Obstet Gynecol. 1990;162:968–74; discussion 74–6.
Ip PP, Tse KY, Tam KF. Uterine smooth muscle tumors other than the ordinary leiomyomas and leiomyosarcomas: a review of selected variants with emphasis on recent advances and unusual morphology that may cause concern for malignancy. Adv Anat Pathol. 2010;17:91–112.
Parker WH, Fu YS, Berek JS. Uterine sarcoma in patients operated on for presumed leiomyoma and rapidly growing leiomyoma. Obstet Gynecol. 1994;83:414–8.
Seidman MA, Oduyebo T, Muto MG, Crum CP, Nucci MR, Quade BJ. Peritoneal dissemination complicating morcellation of uterine mesenchymal neoplasms. PLoS One. 2012;7:e50058.
Chan JK, Gardner AB, Thompson CA, Kapp DS. The use of clinical characteristics to help prevent morcellation of leiomyosarcoma: an analysis of 491 cases. Am J Obstet Gynecol. 2015;213:873–4.
Oliva E, Carcangiu ML, Carinelli SG, Ip P, Loening T, Longacre TA, Nucci MR, Prat J, Zaloudek CJ. Mesenchymal tumours. In: Kurman RJ, Carcangiu ML, Herrington CS, Young RH, editors. WHO classification of tumours of female reproductive organs. Lyon: IARC; 2014.
Bennett JA, Weigelt B, Chiang S, Selenica P, Chen YB, Bialik A, Bi R, Schultheis AM, Lim RS, Ng CKY, Morales-Oyarvide V, Young RH, Reuter VE, Soslow RA, Oliva E. Leiomyoma with bizarre nuclei: a morphological, immunohistochemical and molecular analysis of 31 cases. Mod Pathol. 2017;30:1476–88.
Zhang Q, Poropatich K, Ubago J, Xie J, Xu X, Frizzell N, Kim J, Kong B, Wei JJ. Fumarate hydratase mutations and alterations in leiomyoma with bizarre nuclei. Int J Gynecol Pathol. 2017. https://doi.org/10.1097/PGP.0000000000000447.
Kefeli M, Caliskan S, Kurtoglu E, Yildiz L, Kokcu A. Leiomyoma with bizarre nuclei: clinical and pathologic features of 30 patients. Int J Gynecol Pathol. 2017. https://doi.org/10.1097/PGP.0000000000000425.
Croce S, Young RH, Oliva E. Uterine leiomyomas with bizarre nuclei: a clinicopathologic study of 59 cases. Am J Surg Pathol. 2014;38:1330–9.
Clement PB, Young RH, Scully RE. Diffuse, perinodular, and other patterns of hydropic degeneration within and adjacent to uterine leiomyomas. Problems in differential diagnosis. Am J Surg Pathol. 1992;16:26–32.
Shintaku M. Lipoleiomyomatous tumors of the uterus: a heterogeneous group? Histopathological study of five cases. Pathol Int. 1996;46:498–502.
Roth LM, Reed RJ, Sternberg WH. Cotyledonoid dissecting leiomyoma of the uterus. The Sternberg tumor. Am J Surg Pathol. 1996;20:1455–61.
Lapan B, Solomon L. Diffuse leiomyomatosis of the uterus precluding myomectomy. Obstet Gynecol. 1979;53:82S–4S.
Marshall JF, Morris DS. Intravenous leiomyomatosis of the uterus and pelvis: case report. Ann Surg. 1959;149:126–34.
Clement PB, Young RH, Scully RE. Intravenous leiomyomatosis of the uterus. A clinicopathological analysis of 16 cases with unusual histologic features. Am J Surg Pathol. 1988;12:932–45.
Mulvany NJ, Slavin JL, Ostor AG, Fortune DW. Intravenous leiomyomatosis of the uterus: a clinicopathologic study of 22 cases. Int J Gynecol Pathol. 1994;13:1–9.
Canzonieri V, D'Amore ES, Bartoloni G, Piazza M, Blandamura S, Carbone A. Leiomyomatosis with vascular invasion. A unified pathogenesis regarding leiomyoma with vascular microinvasion, benign metastasizing leiomyoma and intravenous leiomyomatosis. Virchows Arch. 1994;425:541–5.
Kayser K, Zink S, Schneider T, Dienemann H, Andre S, Kaltner H, Schuring MP, Zick Y, Gabius HJ. Benign metastasizing leiomyoma of the uterus: documentation of clinical, immunohistochemical and lectin-histochemical data of ten cases. Virchows Arch. 2000;437:284–92.
Zaloudek CZ, Hendrickson MR, Soslow RA. Mesenchymal tumors of the uterus. In: Kurman RJ, editor. Blaustein’s pathology of the female genital tract. 6th ed. New York: Springer; 2011. p. 455–527.
King ME, Dickersin GR, Scully RE. Myxoid leiomyosarcoma of the uterus. A report of six cases. Am J Surg Pathol. 1982;6:589–98.
Atkins K, Bell S, Kempson RL, Hendrickson MR. Myxoid smooth muscle tumors of the uterus. Mod Pathol. 2002;14:132A.
Oliva E, Young RH, Amin MB, Clement PB. An immunohistochemical analysis of endometrial stromal and smooth muscle tumors of the uterus: a study of 54 cases emphasizing the importance of using a panel because of overlap in immunoreactivity for individual antibodies. Am J Surg Pathol. 2002;26:403–12.
Vocke CD, Ricketts CJ, Merino MJ, Srinivasan R, Metwalli AR, Middelton LA, Peterson J, Yang Y, Linehan WM. Comprehensive genomic and phenotypic characterization of germline FH deletion in hereditary leiomyomatosis and renal cell carcinoma. Genes Chromosomes Cancer. 2017;56:484–92.
Launonen V, Vierimaa O, Kiuru M, Isola J, Roth S, Pukkala E, Sistonen P, Herva R, Aaltonen LA. Inherited susceptibility to uterine leiomyomas and renal cell cancer. Proc Natl Acad Sci U S A. 2001;98:3387–92.
Grubb RL III, Franks ME, Toro J, Middelton L, Choyke L, Fowler S, Torres-Cabala C, Glenn GM, Choyke P, Merino MJ, Zbar B, Pinto PA, Srinivasan R, Coleman JA, Linehan WM. Hereditary leiomyomatosis and renal cell cancer: a syndrome associated with an aggressive form of inherited renal cancer. J Urol. 2007;177:2074–9; discussion 9–80.
Rigaud C, Bogomoletz WV. Leiomyomatosis in pelvic lymph node. Arch Pathol Lab Med. 1983;107:153–4.
Ip PP, Cheung AN, Clement PB. Uterine smooth muscle tumors of uncertain malignant potential (STUMP): a clinicopathologic analysis of 16 cases. Am J Surg Pathol. 2009;33:992–1005.
Yanai H, Wani Y, Notohara K, Takada S, Yoshino T. Uterine leiomyosarcoma arising in leiomyoma: clinicopathological study of four cases and literature review. Pathol Int. 2010;60:506–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Mikami, Y. (2018). Histopathology of Uterine Leiomyoma. In: Sugino, N. (eds) Uterine Fibroids and Adenomyosis. Comprehensive Gynecology and Obstetrics. Springer, Singapore. https://doi.org/10.1007/978-981-10-7167-6_1
Download citation
DOI: https://doi.org/10.1007/978-981-10-7167-6_1
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-7166-9
Online ISBN: 978-981-10-7167-6
eBook Packages: MedicineMedicine (R0)