Abstract
Epilepsy in pregnancy presents unique challenges to the clinician. Less than 1% of pregnant women experience seizure attack during pregnancy. Prompt management of these women in a timely fashion is essential to prevent fatal maternal and foetal complications. Pre-pregnancy counselling and dose adjustment of anti-epileptic drugs to maintain 9–12 month seizure-free period prior to pregnancy ensure minimal risk of seizure recurrence during pregnancy. This chapter mainly focuses on acute management of pregnant women presenting with seizure and status epilepticus during pregnancy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
Epilepsy is one of the most common neurological complications of pregnancy with a prevalence of 0.5–1% [1]. Epilepsy is a chronic disorder and is defined as one or more recurrent unprovoked seizures. Pregnant women with known epilepsy are advised to continue anti-epileptic medication to avoid maternal and foetal complication due to seizure. The goal of treatment is optimal control of seizure and minimal exposure of foetus to anti-epileptic medication. Various physiological, endocrine and psychological changes contribute to increase in seizure frequency during pregnancy. Most crucial to management is determining exact aetiology. Prompt and stepwise management of these patients in a multidisciplinary team involving obstetrician, gynaecologist and neurologist can prevent fatal complications to mother and foetus.
Seizure for the first time during pregnancy can have multiple differentials listed in Table 13.1. Management of a pregnant women presenting with epileptic fit involves a detailed history, physical examination, appropriate investigation and prompt treatment for seizure control. History taking is the most important tool in diagnosing seizure and should focus on symptoms during and after the seizure episode. Other associated factors to be taken into account include previous history of seizure, brain tumour or trauma, stroke, precipitating events (alcohol or medications) and past obstetrical history. Symptoms during seizure are usually described by an eyewitness and include presence of aura, changes in respiration, altered consciousness, bowel/bladder dysfunction and generalised or focal tonic-clonic movements. Seizure episode is usually followed by amnesia, weakness, headache, body aches and drowsiness. Physical examination includes pulse and blood pressure measurement and thorough neurological examination including optic fundi. Ancillary investigations include electroencephalography (EEG), imaging of the brain and laboratory studies. EEG is safe during pregnancy and is the recommended initial neurodiagnostic investigation. It is found to be normal in 50% of cases, and abnormality indicates risk of seizure recurrence and helps guide therapy. The American Academy of Neurology and the American Society of Epilepsy recommend computed tomography (CT) and magnetic resonance imaging (MRI) of the brain as initial neurodiagnostic tests to help determine underlying aetiology [2]. CT of the brain delivers <1 rad to foetus, and exposure below 5 rad is not associated with increased risk of foetal anomalies or pregnancy loss [3]. MRI has no radiation exposure and is more sensitive than CT but is costly and not readily available. Laboratory studies include full blood count, serum urea and electrolytes, blood sugars and urine protein estimation and toxicology screen.
2 Classification
The International Classification of Epileptic Seizures categorises seizures into two broad groups (International League against Epilepsy [4]):
-
1.
Partial seizures are due to initial activation of neurons in one hemisphere. They can be further subdivided into simple or complex:
-
(a)
Simple partial seizure: Consciousness maintained during ictal phase.
-
(b)
Complex partial seizure: Impaired consciousness during seizure episode.
-
(a)
-
2.
Generalised seizures: Arise due to activation of neurons in both hemispheres:
-
(a)
Convulsive: Presence of motor movements and impaired consciousness and can be myoclonic, clonic, tonic and tonic-clonic type.
-
(b)
Non-convulsive: Absence of motor concomitants.
-
(a)
3 Maternal and Foetal Complications
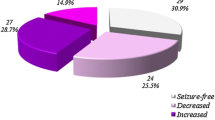
Epilepsy in pregnancy is a serious medical condition associated with both maternal and foetal complications enlisted in Table 13.2. Seizures especially status epilepticus during pregnancy and labour could be fatal for both foetus and mother. Pregnant women with epilepsy are advised to continue anti-epileptic medication to avoid serious maternal and foetal complications. The most important predictor of seizure during pregnancy is the occurrence of seizure prior to pregnancy. Women who had seizure in the month prior to pregnancy had a 15 times greater likelihood of having seizure during pregnancy. If the woman is seizure free for 9 months to 1 year prior to conception, 92% will not have seizure in pregnancy [5]. Polytherapy also increases risk of seizure during pregnancy [6]. Planned pregnancies have a lower likelihood of seizure during pregnancy as most of the women in this group are on monotherapy and not on valproate [7]. Various anti-epileptic drugs for particular seizure type are outlined in Table 13.3. Folic acid supplementation should be given to all women in reproductive age group to reduce risk of neural tube defects. Sodium valproate should be avoided in women of reproductive age as it is associated with highest risk of congenital malformation up to 11% when given in pregnancy [8]. If other anti-epileptics have failed and seizure can be controlled only on valproate, lowest dose preferably less than 700 mg should be used. Lamotrigine and levetiracetam are preferred over others because of least teratogenicity. Physiological changes in pregnancy can alter seizure frequency during pregnancy. Moreover hyperventilation of pregnancy, sleep deprivation and labour pains can lower seizure threshold in pregnancy.
4 Management of Pregnant Women Presenting with Seizure
In the antenatal period, women should be regularly assessed at each visit for triggers of seizure including fasting, sleep deprivation and stress. Prompt treatment of seizure if it occurs during pregnancy is essential to avoid maternal and foetal risks. Neurologist should be consulted if there is deterioration in seizure control and dose adjustments made accordingly.

5 Management of Seizure in Labour
Convulsive status epilepticus during labour is rare and affects around 1% of women with epilepsy [9]. It is a life-threatening condition; hence precipitating factors should be avoided. If patient is on anti-epileptics, doses should not be missed during labour and delivery. Parenteral alternatives should be considered in case of excessive vomiting. One-to-one support of labouring patient minimises stress of labour and ensures safety in the event of a seizure attack. Adequate hydration and pain relief with epidural will minimise risks of seizures in labour. Left lateral tilt with oxygenation and airway should be maintained at all times. Treatment should be initiated as soon as possible to terminate seizure and prevent maternal and foetal hypoxia and foetal acidosis. Benzodiazepines are the drug of choice for convulsive status with lorazepam being the preferred drug in doses as described below [10]. Tocolytics are administered for persistent uterine hypertonus. Continuous electronic foetal monitoring is commenced once the mother is stabilised. If foetal heart rate deceleration persists beyond 5 min or seizures are refractory, then delivery should be expedited and caesarean performed if vaginal delivery is not imminent.
6 Status Epilepticus
Status epilepticus (SE) is the most serious labour room emergency in a patient with epilepsy. In this condition there is failure of normal mechanisms that serve to terminate seizures. It can be of the following types:
-
(a)
Convulsive status epilepticus (CSE): Characterised by continuous convulsive seizures lasting for more than 5 min or two or more seizures with loss of consciousness in between.
-
(b)
Non-convulsive status epilepticus (NCSE): Altered mental status from baseline lasting for at least 30 min and associated with EEG changes.
-
(c)
Refractory status epilepticus: Seizure activity that persists despite first- and second-line anti-epileptics.

Refractory Status Epilepticus (Lasting more than 60 min)
-
Admit patient to intensive care unit.
-
EEG monitoring.
-
Central venous access.
-
Mechanical ventilation.
-
Anaesthetic agent: Midazolam 0.2 mg/kg IV (maximum 10 mg) bolus over 2 min followed by 0.1–0.4 mg/kg/h continuous IV infusion. Alternatively propofol 2–5 mg/kg IV bolus followed by 5–10 mg/kg/h IV infusion can be administered.
-
Pharmacologic treatment is continued for 12 h after last seizure to maintain comatose state with EEG monitoring.
-
Anaesthetic infusion is reduced every 3 h with EEG monitoring during weaning phase.
6.1 Treatment After Control of Seizure
If patient is known case of epilepsy, anti-epileptic drugs are continued and dose adjusted according to serum levels. In patients presenting for the first time with seizures, phenytoin or valproate started to control status epilepticus should be continued.
7 Conclusion
The management of pregnant women with epilepsy is a challenge for clinicians. The goal of treatment is adequate seizure control and minimal exposure of foetus to anti-epileptic drugs. Most pregnant females with epilepsy will have a successful outcome of pregnancy, but pre-pregnancy planning is necessary for optimum control of epilepsy. Increased risk periods during pregnancy for seizure attack are intrapartum and postpartum. Prompt treatment and termination of seizure are paramount for maternal and foetal well-being. Multidisciplinary approach is required for successful outcome of pregnancy.
References
Edey S, Moran N, Nashef L. SUDEP and epilepsy-related mortality in pregnancy. Epilepsia. 2014;55:e72–4.
Krumholz A, Wiebe S, Gronseth G, et al. Practice parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): report of the quality standards sub- committee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2007;69(21):1996–2007.
Practice ACoO. ACOG Committee Opinion. Number 299, September 2004 (replaces No.158, September 1995). Guidelines for diagnostic imaging during pregnancy. Obstet Gynecol. 2004;104(3):647–51.
Proposal for revised clinical and electroencephalographic classification of epileptic seizures. From the commission on classification and terminology of the international league against epilepsy. Epilepsia. 1981;22(4):489–501.
Harden CL, Hopp J, Ting TY, et al. Practice parameter update: management issues for women with epilepsy-focus on pregnancy (an evidence-based review): obstetrical complications and change in seizure frequency. Neurology. 2009;73:126–32.
Thomas SV, Syam U, Devi SJ. Predictors of seizures during pregnancy in women with epilepsy. Epilepsia. 2012;53(5):e85–8.
Abe K, Hamada H, Yamada T, Obato-Yasuoka M, Minakami H, Yoshikawa H. Impact of planning of pregnancy in women with epilepsy on seizure control during pregnancy and on maternal and neonatal outcomes. Seizure. 2014;23:112–6.
Cunnington MC, Weil JG, Messenheimer JA, et al. Final results from 18 years of the international lamotrigine pregnancy registry. Neurology. 2011;76:1817–23.
EURAP Study Group. Seizure control and treatment in pregnancy: observations from the EURAP 1129 epilepsy pregnancy registry. Neurology. 2006;66:354–60.
Alldredge BK, Gelb AM, Isaacs SM, Corry MD, Allen F, Ulrich S, et al. A comparison of lorazepam, 1134 diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med. 2001;345:631–7.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Sharma, J.B., Gupta, M. (2020). Epilepsy. In: Sharma, A. (eds) Labour Room Emergencies. Springer, Singapore. https://doi.org/10.1007/978-981-10-4953-8_13
Download citation
DOI: https://doi.org/10.1007/978-981-10-4953-8_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-4952-1
Online ISBN: 978-981-10-4953-8
eBook Packages: MedicineMedicine (R0)