Abstract
The cholangiographic findings of IgG4-related sclerosing cholangitis (IgG4-SC) are heterogeneous and can mimic other biliary diseases, making it difficult to diagnose IgG4-SC on the basis of biliary changes on cholangiography alone [1–3]. MRI with MR cholangiopancreatography (MRCP) can simultaneously provide imaging of wall thickening of the bile ducts and its enhancement patterns, the pattern and degree of biliary strictures, and other IgG4-related disease in different intra-abdominal organs, such as autoimmune pancreatitis, IgG4-related renal disease, and retroperitoneal fibrosis [4]. Therefore, MRI with MRCP is a useful noninvasive diagnostic tool for IgG4-SC.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- MR Cholangiopancreatography (MRCP)
- IgG4-related Sclerosing Cholangitis (IgG4-SC)
- Autoimmune Pancreatitis
- Biliary Changes
- Biliary Strictures
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The cholangiographic findings of IgG4-related sclerosing cholangitis (IgG4-SC) are heterogeneous and can mimic other biliary diseases, making it difficult to diagnose IgG4-SC on the basis of biliary changes on cholangiography alone [1,2,3]. MRI with MR cholangiopancreatography (MRCP) can simultaneously provide imaging of wall thickening of the bile ducts and its enhancement patterns, the pattern and degree of biliary strictures, and other IgG4-related disease in different intra-abdominal organs, such as autoimmune pancreatitis, IgG4-related renal disease, and retroperitoneal fibrosis [4]. Therefore, MRI with MRCP is a useful noninvasive diagnostic tool for IgG4-SC.
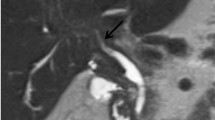
Cross-Sectional MR Imaging
The main finding of IgG4-SC on cross-sectional MRI is focal or diffuse wall thickening of the bile ducts, mostly associated with stenosis and mild dilatation of the upstream bile ducts [1, 5, 6]. The mean and median thicknesses of the involved common bile ducts are reported as 3 mm (standard deviation, 1.47 mm) and 4.3 mm (range, 2.5–9.7 mm), respectively [1, 5]. The involved thickened walls of the bile ducts are mostly concentric and homogeneously hypointense on T1-weighted images and isointense on T2-weighted images (88% and 75%, respectively) [1] (Fig. 9.1). In most cases, the thickened walls of the bile ducts are homogenously enhanced after administration of contrast materials (71.4–100%) and are iso- or hyperintense during the portal venous or delayed phases in comparison with adjacent hepatic parenchyma [1, 5, 6] (Fig. 9.1).
IgG4-related sclerosing cholangitis. (a) T1-weighted axial image shows a concentric thickened wall of the proximal common ducts with hypointensity (arrows) in comparison with the hepatic parenchyma. (b) T2-weighted axial image shows a homogenously isointense thickened wall of the proximal common ducts (arrows) in comparison with the hepatic parenchyma. (c, d) Contrast-enhanced axial (c) and coronal (d) images show a segmental thickened wall of the proximal common ducts (arrowheads) with homogeneous enhancement. The wall thickening looks symmetric. The bile duct lumen in the involved segment is visible although narrowed. (e) MR cholangiopancreatography depicts a long stricture of the proximal common ducts (>2 cm in length; arrowheads) as well as dilated intrahepatic bile ducts which mimics the features of cholangiocarcinoma. In this case, the pancreatic duct (arrows) looks normal
MR Cholangiopancreatography
The main feature of IgG4-SC on MRCP is the presence of focal or diffuse strictures in the bile ducts, which is one of the diagnostic criteria of IgG4-SC [4,5,6,7,8]. The most commonly involved location is the intrapancreatic common bile duct because of an association with simultaneous autoimmune pancreatitis in most cases [6, 9] (Fig. 9.2). In a recent retrospective study of 527 patients with IgG4-SC, intrapancreatic biliary strictures without any other strictures in the bile ducts were the most common finding (64%), followed by strictures in the biliary hilar portions (10%), both intrapancreatic and hilar portions (10%), and both intrahepatic and intrapancreatic portions (5–8%) [9] (Figs. 9.3 and 9.4). The lengths of biliary strictures are variable, focal (<3 mm), segmental (3–10 mm), or long (>10 mm) [1], although segmental or long biliary strictures are more common than focal strictures [2, 5, 10]. The strictures in the common bile ducts mostly show a smooth margin, gradual transition, and symmetry on MRCP (77.6–87.9%) [10]. A characteristic hourglass appearance in the involved common bile ducts, which indicates a smooth, symmetric, and gradual narrowing at both the proximal and distal ends of strictures with a fully visible lumen, is reported in 30.8% of cases of IgG4-SC of the common bile ducts on MRCP [10] (Fig. 9.5).
IgG4-related sclerosing cholangitis and autoimmune pancreatitis. MR cholangiopancreatography demonstrates a long stricture of the distal common bile duct (>2 cm in length; arrowheads) with mild dilatation of the upstream bile ducts. Multiple segmental or long strictures of the pancreatic duct (arrows) without dilatation of the upstream pancreatic duct, a feature of autoimmune pancreatitis, are also seen
IgG4-related sclerosing cholangitis and autoimmune pancreatitis. MR cholangiopancreatography shows a long stricture of the proximal left and right hepatic ducts and common hepatic ducts (white arrows). The distal common bile duct is also involved (arrowhead). The multiple strictures of the pancreatic duct (black arrows) are suggestive of autoimmune pancreatitis
IgG4-related sclerosing cholangitis and autoimmune pancreatitis. MR cholangiopancreatography shows a characteristic hourglass appearance in the involved common bile duct (white arrows), which indicates a smooth, symmetric, and gradual narrowing at both the proximal and distal ends of strictures with a fully visible lumen. A long stricture of the pancreatic duct (black arrows) without dilatation of the upstream pancreatic duct is also noted
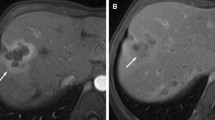
Other Organ Involvement in IgG4-Related Disease
The identification of IgG4-related disease in other intra-abdominal organs, one of the diagnostic criteria for IgG4-SC, is a very important clue in the diagnosis of IgG4-SC, allowing its differentiation from primary sclerosing cholangitis and cholangiocarcinoma [8, 11,12,13]. Therefore, MRI with MRCP, which can simultaneously show biliary strictures and pancreatic abnormalities, strictures of the main pancreatic duct, IgG4-related renal disease, and IgG4-related retroperitoneal fibrosis, is a very useful tool in the diagnosis of IgG4-SC. Accurate diagnosis of IgG4-SC in patients without other organ involvement is particularly difficult, as other biliary diseases may cause similar biliary changes on cholangiography.
On MRI with MRCP, the typical findings of the diffuse type of autoimmune pancreatitis are well known: diffuse enlargement of the pancreas, a capsule-like rim or halo around the pancreas, and diffuse or segmental irregular narrowing of the main pancreatic duct [4, 6] (Figs. 9.2, 9.3 and 9.5). The most common findings of IgG4-related renal disease are bilateral round or wedge-shaped peripheral cortical lesions with hypointensity on T2-weighted images, progressive enhancement (thus becoming indistinct as the phase passes) on contrast-enhanced T1-weighted images, and marked hyperintensity on diffusion-weighted images with high b values [6, 14, 15]. IgG4-related retroperitoneal fibrosis typically appears as a soft-tissue mass covering the abdominal aorta and its branches, or entrapping the ureters, and having variable signal intensity on T2-weighted images and variable enhancement on contrast-enhanced T1-weighted images, depending on the degree of active inflammation and maturity of the fibrous tissue [6, 7, 15].
Differential Diagnosis
Primary Sclerosing Cholangitis
On MRCP, primary sclerosing cholangitis (PSC) shows biliary changes that are the most difficult to distinguish from IgG4-SC with multiple biliary strictures, although the clinicopathological characteristics of both diseases are different from each other. MRI with MRCP findings that favor IgG4-SC over PSC include continuous involvement of the bile ducts instead of skip involvement, a thicker single-layer bile duct wall, diffuse wall thickening of the gallbladder, segmental or long strictures, and the presence of extrabiliary IgG4-related disease [1, 4,5,6,7, 16]. By contrast, those that favor PSC over IgG4-SC are focal stricture, multifocal and intrahepatic biliary stricture, and characteristic findings of PSC such as beaded, pruned tree, and diverticulum-like appearances [1, 4,5,6,7, 16].
Cholangiocarcinoma
IgG4-SC often mimics periductal infiltrating cholangiocarcinoma, particularly in cases with a single stricture in the hilar biliary portion or common bile duct. On MRI with MRCP, findings more likely to suggest IgG4-SC are multiple strictures with a smooth margin, gradual transition, symmetry, and hourglass appearance, and the presence of extrabiliary IgG4-related disease [4, 7, 10, 16]. By contrast, features favoring cholangiocarcinoma over IgG4-SC include a solitary lesion or stricture with irregular margins, abrupt transition, and asymmetry, indistinct outer margins, marked upstream biliary dilatation (>2 cm in diameter), the presence of an associated soft-tissue mass, and hyperenhancement relative to the hepatic parenchyma during the arterial or venous phases [4, 7, 10, 16].
References
Kim JH, Byun JH, Kim SY, Lee SS, Kim HJ, Kim MH, et al. Sclerosing cholangitis with autoimmune pancreatitis versus primary sclerosing cholangitis: comparison on endoscopic retrograde cholangiography, MR cholangiography, CT, and MRI. Acta Radiol. 2013;54:601–7.
Nakazawa T, Ohara H, Sano H, Aoki S, Kobayashi S, Okamoto T, et al. Cholangiography can discriminate sclerosing cholangitis with autoimmune pancreatitis from primary sclerosing cholangitis. Gastrointerst Endosc. 2004;60:937–44.
Hamano H, Kawa S, Uehara T, Ochi Y, Takayama M, Komatsu K, et al. Immunoglobulin G4-related lymphoplasmacytic sclerosing cholangitis that mimics infiltrating hilar cholangiocarcinoma: part of a spectrum of autoimmune pancreatitis? Gastrointerst Endosc. 2005;62:152–7.
Zen Y, Kawakami H, Kim JH. IgG4-related sclerosing cholangitis: all we need to know. J Gastroenterol. 2016;51:295–312.
Tokala A, Khalili K, Menezes R, Hirschfield G, Jhaveri K. Comparative MRI analysis of morphologic patterns of bile duct disease in IgG4-related systemic disease versus primary sclerosing cholangitis. AJR Am J Roentgenol. 2014;202:536–43.
Martínez-de-Alegría A, Baleato-González S, García-Figueiras R, Bermúdez-Naveira A, Abdulkader-Nallib I, Daz-Peromingo J. IgG4-related disease from head to toe. Radiographics. 2015;35:2007–35.
Vlachou PA, Khalili K, Jang HJ, Fischer S, Hirschfield GM, Kim TK. IgG4-related sclerosing disease: autoimmune pancreatitis and extrapancreatic manifestations. Radiographics. 2011;31:1379–402.
Ohara H, Okazaki K, Tsubouchi H, Inui K, Kawa S, Kamisawa T, et al. Clinical diagnostic criteria of IgG4-related sclerosing cholangitis 2012. J Hepatobiliary Pancreat Sci. 2012;19:536–42.
Tanaka A, Tazuma S, Okazaki K, Nakazawa T, Inui K, Chiba T, et al. Clinical features, response to treatment, and outcomes of IgG4-related sclerosing cholangitis. Clin Gastroenterol Hepatol. 2017;15:920–6.
Kim JH, Byun JH, Lee SJ, Park SH, Kim HJ, Lee SS, et al. Differential diagnosis of sclerosing cholangitis with autoimmune pancreatitis and periductal infiltrating cancer in the common bile duct at dynamic CT, endoscopic retrograde cholangiography and MR cholangiography. Eur Radiol. 2012;22:2502–13.
Moon SH, Kim MH, Lee JK, Baek S, Woo YS, Cho DH, et al. Development of a scoring system from differentiating IgG4-related sclerosing cholangitis from primary sclerosing cholangitis. J Gastroenterol. 2017;52:483–93.
Yata M, Suzuki K, Furuhashi N, Kawakami K, Kawai Y, Naganawa S. Comparison of the multideteror-row computed tomography findings of IgG4-related sclerosing cholangitis and extrahepatic cholangiocarcinoma. Clin Radiol. 2016;71:203–10.
Oh HC, Kim MH, Lee KT, Lee JK, Moon SH, Song TJ, et al. Clinical clues to suspicion of IgG4-associated sclerosing cholangitis disguised as primary sclerosing cholangitis or hilar cholangiocarcinoma. J Gastroenterol Hepatol. 2010;25:1831–7.
Seo N, Kim JH, Byun JH, Lee SS, Kim HJ, Lee MG. Immunoglobulin G4-related kidney disease: a comprehensive pictorial review of the imaging spectrum, mimickers, and clinicopathological characteristics. Korean J Radiol. 2015;16:1056–67.
Sohn JH, Byun JH, Yoon SE, Choi EK, Park SH, Kim MH, et al. Abdominal extrapancreatic lesions associated with autoimmune pancreatitis: radiological findings and changes after therapy. Eur J Radiol. 2008;67:497–507.
Seo N, Kim SY, Lee SS, Byun JH, Kim JH, Kim HJ, et al. Sclerosing cholangitis: clinicopathologic features, imaging spectrum, and systemic approach to differential diagnosis. Korean J Radiol. 2016;17:25–38.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Science+Business Media Singapore
About this chapter
Cite this chapter
Byun, J.H. (2019). Imaging: MRI with MRCP. In: Kamisawa, T., Kim, MH. (eds) IgG4-Related Sclerosing Cholangitis. Springer, Singapore. https://doi.org/10.1007/978-981-10-4548-6_9
Download citation
DOI: https://doi.org/10.1007/978-981-10-4548-6_9
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-4547-9
Online ISBN: 978-981-10-4548-6
eBook Packages: MedicineMedicine (R0)