Abstract
Rituximab is an important treatment option for Immunoglobulin G4-associated cholangitis (IgG4-SC). While steroids are the initial therapy for most patients, those with relapsing, recrudescent, or unresponsive disease are likely to respond to rituximab infusions. Patients who are intolerant of steroids are also likely to respond, and rituximab is effective as single-agent therapy. This chapter reviews the available evidence regarding rituximab therapy for IgG4-SC, describes patient selection, adverse effects, predictors of relapse, and indications for maintenance therapy, and presents an algorithm for use of rituximab in treatment of IgG4-SC.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
A steroid-responsive cholangiopathy associated with thyroiditis, sialoadenitis, and hypergammaglobulinemia was first described in 1963 [1] and again in 1979 [2], and the discovery by Japanese investigators of serum IgG4 as a biomarker of autoimmune pancreatitis [3] has led to increased recognition of both pancreatic and biliary IgG4-related disease (IgG4-RD). Hepatobiliary involvement by IgG4-RD is currently termed IgG4-associated sclerosing cholangitis (IgG4-SC) and in the past has been called IgG4-associated cholangitis (IAC) or IgG4-related cholangitis (IRC). IgG4-SC may involve the intrahepatic and/or extrahepatic bile ducts and may mimic the biliary strictures of chronic pancreatitis, hilar cholangiocarcinoma, or intrahepatic sclerosing cholangitis. Diagnosis of IgG4-SC may be particularly difficult if the biliary tree is the sole anatomical area affected. The classification and diagnostic approach to IgG4-SC are discussed in other chapters.
Although most cases of IgG4-SC are steroid responsive, some patients are unable to discontinue steroid therapy or relapse after steroids are withdrawn, and occasional patients do not respond adequately to steroid treatment [4]. This has led several investigators worldwide to explore alternative treatment strategies. In this chapter, we will focus on the role of rituximab (RTX) in the treatment of IgG4-SC.
Definition of Treatment Response
Successful treatment of IgG4-SC may not result in radiologic normalization of the biliary tree, and residual ductal strictures may be due to fibrosis that persists after the inflammatory process has resolved. Definition of treatment outcomes is important to guide judicious treatment decisions and for comparing effectiveness of different treatment modalities. We use the following terms and definitions for treatment response in IgG4-SC:
-
(a)
Complete remission: Resolution of symptoms and imaging or laboratory findings of active IgG4-RD (clinical, radiographic, and biochemical), without an ongoing need for medical therapy (Fig. 18.1)
-
(b)
Partial remission: Improvement without resolution of inflammatory changes, without an ongoing need for medical therapy
-
(c)
Incomplete remission: Improvement without resolution of inflammatory changes and with ongoing need for medical therapy to maintain response
-
(d)
Relapse: Development of symptoms, radiologic findings, and/or biochemical abnormalities consistent with a new or worsening inflammatory process after previous successful medical therapy, requiring retreatment
-
(e)
Recrudescence: Development of symptoms, radiologic findings, and/or biochemical abnormalities consistent with a new or worsening inflammatory process during steroid taper and requiring an increase in the dose of steroids or additional treatments
Rituximab (RTX)
RTX is a chimeric mouse-human monoclonal antibody that binds specifically to the CD20 antigen, a transmembrane receptor located on the cell surface of pre-B and mature B lymphocytes, and induces apoptosis. RTX was initially approved by the US Food and Drug Administration in 1997 to treat resistant B-cell non-Hodgkin lymphomas. Subsequently it was approved for use in rheumatoid arthritis and has been used off-label in other autoimmune and inflammatory conditions including systemic lupus erythematosus, idiopathic thrombocytopenic purpura, autoimmune hemolytic anemia, and pemphigus vulgaris. RTX was also shown to be effective in treating orbital pseudolymphoma [5], a manifestation of IgG4-RD, and pemphigus vulgaris, which is characterized by the presence of IgG4 antibodies. Primarily because of its efficacy in treatment of hematologic malignancies, RTX is on the World Health Organization’s List of Essential Medicines.
The physiological effect of RTX can be monitored by flow cytometry of peripheral blood. After RTX administration, B lymphocytes (CD19- or CD20-positive cells) disappear from the peripheral circulation. Flow cytometry can be performed at intervals (for instance, 6 months after induction RTX therapy and then every 3 months thereafter) to guide decisions about maintenance infusions, if desired. Human antichimeric antibodies (HACA) directed against the murine fragments of RTX have been described and may be associated with lack of therapeutic response [6].
Rituximab is administered as a slow intravenous infusion. The optimum RTX regimen for treating IgG4-SC is unknown, and treatment regimens continue to evolve. Initially we used a lymphoma regimen that included induction with four weekly infusions of 375 mg/m2 followed by a maintenance infusion of 375 mg/m2 every 3 months for up to 2 years. Currently we typically prescribe two induction doses of 1000 mg spaced 2 weeks apart, with or without subsequent maintenance infusions of 1000 mg every 6 months or when B cells return in the peripheral blood. However, as the overall experience continues to grow, future studies are expected to further refine these regimens to optimize patient outcomes.
RTX in IgG4-SC
The overall experience with RTX for IgG4-SC is limited, and there are no randomized or placebo-controlled data available. A case of RTX therapy for IgG4-SC refractory to steroid therapy was reported in 2008 [4]. A case series of 12 patients with autoimmune pancreatitis, 7 with concomitant IgG4-SC, who were treated with RTX induction followed by maintenance dosing was reported in 2013 [7]. Of the seven patients with IgG4-SC, five had a complete remission, one had an incomplete remission (requiring low-dose steroid therapy), and one had a partial remission followed by worsening cholestasis and was found to have cholangiocarcinoma. The use of RTX was also described in a prospective open-label clinical trial of 30 patients with IgG4-RD, including 10 with IgG4-SC [8]. A treatment response was seen in 97% of patients in the trial, and all patients with IgG4-SC achieved a complete remission. In this cohort of patients, two induction doses of RTX were administered without maintenance therapy, and at 6 months postinduction, less than 80% of patients were steroid-free. In another retrospective study of 60 patients receiving RTX induction therapy for IgG4-RD, including five with biliary or hepatic IgG4-RD, almost half of patients had relapsed within 1 year [9]. We recently reviewed our institutional experience comparing RTX induction and maintenance therapy (n = 29) to induction therapy alone (n = 14) in pancreaticobiliary IgG4-RD, including 35 patients with IgG4-SC [10]. Overall, 86% patients in this study, the majority of whom had relapsing or recrudescent disease, were in steroid-free remission 6 months after initiating RTX. Relapses were more common in those treated with induction alone compared to those also receiving maintenance RTX (3-year event rate 45% vs. 11%). Maintenance therapy effectively prolonged remission, but the relapse rate after treatment discontinuation was not significantly different between the two groups. Although RTX was fairly well tolerated in this cohort, maintenance therapy was associated with an increased risk of bacterial infections, which occurred in 5 of 29 patients during maintenance therapy.
Adverse Effects of RTX
The adverse effects of RTX have been investigated in large series of patients receiving the drug for hematologic malignancies or other inflammatory diseases. In contrast to corticosteroids, the majority of patients receiving RTX experience no adverse effects of the drug. Certain adverse effects, such as tumor lysis syndrome and bowel perforation related to tumor lysis, are seen only in patients with malignancies. The main adverse effects of RTX in treatment of benign disorders are:
-
(a)
Infusion reactions. Mild infusion reactions are commonly Grade 1 or 2 reactions (characterized by a rash, pruritus, flushing, urticarial, nausea/vomiting, throat or chest tightness, or asymptomatic bronchospasm) and are usually treated by stopping the infusion, administering intravenous antihistamines (H1 and H2 blockers), allowing findings to resolve, and then resuming the infusion at a slower rate [11]. Patients with Grade 3 or 4 infusion reactions (including symptomatic bronchospasm, dyspnea, hypoxia, wheezing, anaphylaxis, or hypotension) may have recurrent symptoms during same-day rechallenge and may benefit from further evaluation prior to rechallenge [11]. Severe, sometimes fatal, infusion reactions, including anaphylaxis, shock, acute respiratory distress syndrome, and myocardial infarction, have been reported in 0.04–0.07% of patients receiving rituximab. Severe mucocutaneous reactions, including Stevens-Johnson syndrome, have also been reported. Premedications (often including methylprednisolone 100 mg IV, oral acetaminophen, and diphenhydramine) are given prior to infusions to decrease the incidence of infusion reactions.
Cytokine release syndrome may occur with rituximab infusions. This syndrome mimics sepsis and is characterized by fever, rigors, and hypotension. This adverse effect is uncommon, especially when premedications are administered.
-
(b)
Infectious complications. Rituximab can cause reactivation of hepatitis B virus (HBV) infection, sometimes leading to fulminant hepatitis. Patients who are hepatitis B surface antigen (HBsAg) positive are at high risk. Patients who are HBsAg negative but have HBV core antibodies (HBcAb+) are also at risk of reactivation, even if HBV DNA is undetectable in their blood [12], and in such patients suppressive therapy with a nucleotide or nucleoside analog should be considered for the duration of rituximab therapy (i.e., until B cells return to the peripheral circulation). In addition, reactivation of tuberculosis (TB) may occur on rituximab therapy, and guidelines recommend screening patients for TB exposure (for instance, with a QuantiFERON test) prior to prescribing RTX.
Serious bacterial infections may occur at an increased rate in patients receiving RTX. In a registry analysis of patients with rheumatoid arthritis receiving RTX, predisposing factors for bacterial infections included age, comorbidities, and low initial serum immunoglobulin G levels [13]. Patients with baseline serum IgG levels of <6 g/L may be at a fivefold increased risk, and this should be taken into account when considering RTX therapy.
-
(c)
Progressive multifocal leukoencephalopathy (PML). PML is a frequently fatal demyelinating infection of the central nervous system caused by reactivation of JC polyomavirus infection. Neurologic presentation is highly variable depending on the regions of the brain that are affected. PML has been associated with RTX therapy, however the absolute risk is small (estimated at 1 in 20,000 rheumatoid arthritis patients receiving RTX) [14]. Pretreatment screening for JC virus infection is not recommended as over half of the adult American population has serologic evidence of prior infection.
-
(d)
Cytopenias and hypogammaglobulinemia. These may develop following RTX induction therapy, and low immunoglobulin levels may be associated with increased rates of bacterial infections. Neutropenia is uncommon, may occur up to 1 year after RTX therapy, and is probably not an absolute contraindication to repeat RTX treatment.
Predictors of Relapse After RTX Induction Therapy
In our experience, elevated pre-RTX alkaline phosphatase levels are associated with a higher risk of relapse. Compared to patients with AIP, those with IgG4-SC were three times more likely to relapse if their alkaline phosphatase normalized with induction RTX therapy and six times more likely to relapse if their alkaline phosphatase did not normalize with induction therapy [10]. These findings highlight the high risk of disease recurrence in patients with IgG4-SC, many of whom will need repeat courses of treatment or maintenance treatment to prevent progressive liver disease.
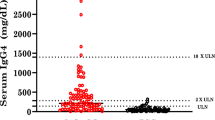
In studies of various manifestations of IgG4-RD treated with RTX, elevations in pretreatment serum IgG4, immunoglobulin E (IgE), and blood eosinophil concentrations independently predicted future relapses in IgG4-RD. [9] Data from our center suggest that younger age and a higher IgG4-RI (IgG4-Responder Index) [15] score after induction RTX therapy are also associated with a higher likelihood of relapse in pancreaticobiliary IgG4-RD. [10] Future studies aimed at identifying predictors of relapse after RTX induction therapy are needed to identify the optimum duration of RTX treatment and guide accurate selection of patients who would benefit the most from maintenance RTX therapy.
Which Patients Should Be Considered for RTX Therapy?
While steroids remain the mainstay of initial treatment for IgG4-RD, relapse is likely in those with proximal biliary strictures. We have seen relapsing IgG4-SC rapidly lead to decompensated biliary cirrhosis and death. Therefore we monitor patients for relapse after successful steroid therapy, including periodic measurement of serum liver tests to detect recurrent cholestasis, and promptly advise additional therapy when relapse occurs. In our experience, traditional oral immunomodulators are not effective for prevention of relapse [7], and we no longer use these drugs routinely in our practice, favoring RTX therapy in patients with relapsing disease. In addition, we may consider RTX as an initial therapeutic option in patients with a history of or risk factors for steroid intolerance and in those who are not responding to steroid therapy or unable to successfully taper steroids. An algorithm for treatment of IgG4-SC incorporating RTX therapy is shown in Fig. 18.2. Prior to initiating RTX therapy, we measure serum IgG levels and screen patients for tuberculosis, HIV, hepatitis B, and hepatitis C.
Future Directions
Although available data support a role of RTX in managing patients with IgG4-SC, several key questions remain unanswered at this time. Most importantly, the optimum duration of RTX therapy needs to be better defined. It is also equally important to study long-term adverse effects of RTX, to explore alternative treatments that might more reliably induce a sustained clinical remission, and identify biomarkers that predict relapse and can be used to individualize therapy. Randomized clinical trials are needed to study the role of RTX as first-line therapy in IgG4-SC with the goal of sustained remission, improved patient outcomes, and cost-effectiveness.
Conclusion
The management of patients with IgG4-SC poses several challenges. Diagnosis may be difficult, response to steroid therapy may be suboptimal, and relapse is common. For patients with relapsing disease or contraindications to steroid use, RTX is the only agent currently available that will reliably induce remission. Maintenance therapy with RTX appears to effectively prolong remission and may be warranted, particularly in patients with persistent or recurrent serum alkaline phosphatase elevations. Patients receiving RTX should be screened and monitored for infections and should receive infusions in a therapeutic infusion center where infusion reactions can be properly assessed and treated.
References
Bartholomew LG, Cain JC, Woolner LB, et al. Sclerosing cholangitis: its possible association with Riedel’s struma and fibrous retroperitonitis. Report of two cases. N Engl J Med. 1963;269:8–12.
Sjogren I, Wengle B, Korsgren M. Primary sclerosing cholangitis associated with fibrosis of the submandibular glands and the pancreas. Acta Med Scand. 1979;205:139–41.
Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001;344:732–8.
Topazian M, Witzig TE, Smyrk TC, et al. Rituximab therapy for refractory biliary strictures in immunoglobulin G4-associated cholangitis. Clin Gastroenterol Hepatol. 2008;6:364–6.
Witzig TE, Inwards DJ, Habermann TM, et al. Treatment of benign orbital pseudolymphomas with the monoclonal anti-CD20 antibody rituximab. Mayo Clin Proc. 2007;82:692–9.
Lunardon L, Payne AS. Inhibitory human antichimeric antibodies to rituximab in a patient with pemphigus. J Allergy Clin Immunol. 2012;130(3):800.
Hart PA, Topazian MD, Witzig TE, et al. Treatment of relapsing autoimmune pancreatitis with immunomodulators and rituximab: the Mayo Clinic experience. Gut. 2013;62:1607–15.
Carruthers MN, Topazian MD, Khosroshahi A, et al. Rituximab for IgG4-related disease: a prospective, open-label trial. Ann Rheum Dis. 2015;74:1171–7.
Wallace ZS, Mattoo H, Mahajan VS, et al. Predictors of disease relapse in IgG4-related disease following rituximab. Rheumatology (Oxford). 2016;55:1000–8.
Majumder S, Mohapatra S, Lennon R, et al. Rituximab maintenance therapy decreases relapse rate of pancreaticobiliary IgG4-related disease. Gastroenterology. 2017;152:S127.
Levin AS, Otani IM, Lax T, et al. Reactions to rituximab in an outpatient infusion Center: a 5-year review. J Allergy Clin Immunol Pract. 2017;5:107–113 e1.
Tang Z, Li X, Wu S, et al. Risk of hepatitis B reactivation in HBsAg-negative/HBcAb-positive patients with undetectable serum HBV DNA after treatment with rituximab for lymphoma: a meta-analysis. Hepatol Int. 2017;11(5):429–33.
Gottenberg JE, Ravaud P, Bardin T, et al. Risk factors for severe infections in patients with rheumatoid arthritis treated with rituximab in the autoimmunity and rituximab registry. Arthritis Rheum. 2010;62:2625–32.
Molloy ES, Calabrese CM, Calabrese LH. The risk of progressive multifocal Leukoencephalopathy in the biologic era: prevention and management. Rheum Dis Clin N Am. 2017;43:95–109.
Carruthers MN, Stone JH, Deshpande V, et al. Development of an IgG4-RD responder index. Int J Rheumatol. 2012;2012:259408.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Science+Business Media Singapore
About this chapter
Cite this chapter
Majumder, S., Topazian, M.D. (2019). Treatment: Rituximab. In: Kamisawa, T., Kim, MH. (eds) IgG4-Related Sclerosing Cholangitis. Springer, Singapore. https://doi.org/10.1007/978-981-10-4548-6_18
Download citation
DOI: https://doi.org/10.1007/978-981-10-4548-6_18
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-4547-9
Online ISBN: 978-981-10-4548-6
eBook Packages: MedicineMedicine (R0)