Abstract
Non-epithelial ovarian tumors have posed pathologic diagnosis and management challenges. The World Health Organization classification of Tumors of Female Reproductive Organs was revised in 2014, and the new version addresses several new concepts and the histological classification of non-epithelial ovarian tumors and tumor-like lesions that were not previously included. In the new WHO classification, sex cord-stromal tumors is divided into three categories, pure stromal tumor, pure sex cord tumor, and mixed sex-cord tumor.
This chapter reviews recent developments regarding the pathology, differential diagnosis, immunohistochemical markers, and genetics of poorly understood non-epithelial ovarian tumors, including sex cord-stromal tumors, immature teratoma, small cell carcinoma of the ovary, hypercalcemic type, and newly described non-epithelial tumors. Many of these neoplasms and those in the differential diagnosis occur predominantly in young women, and they can be aggressive and require specific chemotherapy. Some of non-epithelial neoplasms show histologically biphasic or epithelioid features, mimicking epithelial tumors. The recent discovery of somatic mutations in FOXL2 in adult granulosa cell tumors and germline and somatic mutations in DICER1 in Sertoli-Leydig cell tumors and SMARCA4 in small cell carcinoma, hypercalcemic type, contributes immunohistochemical analyses and molecular research of these tumors. A few non-epithelial tumors are not specific to the ovary and may arise more frequently at extraovarian sites. A correct diagnosis is imperative for appropriate therapies.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Non-epithelial tumor
- Sex cord-stromal tumor
- Sertoli-Leydig cell tumor
- Small cell carcinoma
- Hypercalcemia
6.1 Introduction
The new World Health Organization (WHO) classification of Tumors of Female Reproductive Organs addresses several new concepts and histological classifications that were not previously included [1]. Non-epithelial ovarian tumors have posed pathologic diagnosis and management challenges because general diagnostic pathologists and even gynecologic pathologists rarely encounter these lesions and it is very difficult to make a correct diagnosis. Furthermore gynecologists have no or little experience of treatments of rare ovarian tumors.
This chapter reviews recent developments regarding the pathology, differential diagnosis, and genetics of poorly understood non-epithelial ovarian tumors, including pure and mixed sex cord-stromal tumors (Table 6.1), immature teratoma, small cell carcinoma of the ovary, hypercalcemic type, and newly described non-epithelial tumors. Many of these neoplasms and those in the differential diagnosis occur predominantly in young women, and some of them can be aggressive and require specific chemotherapy. Some non-epithelial neoplasm show histologically biphasic or epithelioid features, mimicking epithelial tumors. Thus, a correct diagnosis is imperative for ensuring that appropriate treatment is administered. Due to the rarity of these tumors and the lack of knowledge about them, a special review and confirmation of the diagnosis by an expert gynecological pathologist is recommended [2]. A few of these lesions are not specific to the ovary and may occur more frequently at extraovarian sites, but the mere knowledge that they occasionally occur in or involve the ovary will facilitate their recognition by pathologists [2]. In addition, the recent discovery of mutations will aid molecular diagnosis and the development of relatively specific immunohistochemical markers.
6.2 Sex Cord-Stromal Tumors: Pure Stromal Tumors
6.2.1 Fibroma, Cellular Fibroma, and Fibrosarcoma
6.2.1.1 Clinical Features
Fibroma is a benign tumor composed of fibroblasts and collagen fibers. The mean age of patients with ovarian fibroma is about 50 years. Cellular fibroma can recur, and so clinical follow-up is necessary. Fibrosarcoma is a malignant mesenchymal tumor with a poor prognosis [3]. The standard treatment involves complete resection followed by chemotherapy.
6.2.1.2 Pathological Features
Fibroma is firm with a smooth, lobulated surface and average size is 6 cm. Cellular fibroma is mainly composed of solid components with white cut surface. Fibrosarcomas are large and soft and typically exhibit necrosis and hemorrhaging. Microscopically, fibromas are composed of fusiform and uniform cells arranged in a fascicular or whorled pattern. The stroma is fibrous with focal hyalinization or calcifications; however, approximately 10% of fibromas are hypercellular (little collagenous stroma is seen). Cellular fibroma is defined as fibroma group tumor with high cellularity, mild to moderate nuclear atypia, and 3 or few mitotic figures in 10/10HPF(high power fields). Cellular fibromas may have mitotic activity of > 4/10HPF (mitotically active cellular fibroma) [4] (Fig 6.1). Many ovarian tumors that have been reported as fibrosarcomas would now be considered to be mitotically active cellular fibromas. Fibrosarcomas are characterized by cellular spindle cell fibromatous lesions with moderate to marked nuclear atypia, 4 or more mitotic figures per 10/HPF, and atypical mitotic figures and necrosis [3] (Fig. 6.2). Fibrosarcomas are usually large and have often spread beyond the ovary at diagnosis. Their differential diagnoses include leiomyosarcoma, high-grade endometrial stromal sarcoma, gastrointestinal stromal sarcoma, and various types of primary or metastatic soft tissue sarcoma.
6.2.2 Thecoma
6.2.2.1 Clinical Features
Thecomas are gonadal stromal tumors that are predominantly composed of theca cell-like cells. In daily practice, thecomas are uncommon, whereas fibromas are relatively common. Thecomas usually occur in premenopausal or postmenopausal women, but can arise in children in rare cases. Luteinized thecomas occur at a younger age, usually in patients in their 20s or 30s. Premenopausal women display either endocrine-associated symptoms, such as irregular bleeding or amenorrhea, or nonspecific complaints, such as pelvic pain or abdominal distention. Luteinized thecomas can be estrogenic (50%), androgenic (11%), or nonfunctional (39%) [5]. Some patients with luteinized thecomas are virilized, whereas others show hyperestrogenic symptoms. Thecomas are benign, and excision is an appropriate treatment. The diagnosis of luteinized thecoma is restricted to luteinized thecomas associated with sclerosing peritonitis, a distinctive stromal tumor that is typically associated with sclerosing peritonitis [1].
6.2.2.2 Pathological Features
Macroscopically, thecomas are firm or hard tumors with a mean diameter of 7 cm. The cut surfaces of thecomas are solid and yellow or white. Cysts and calcifications may be present.
Histologically, thecomas are composed of fascicles or sheets of plump spindle-shaped or ovoid stromal cells that resemble the cells of the theca interna. Tumor cells have round or fusiform nuclei and amphophilic or lightly eosinophilic or clear cytoplasm (Fig. 6.3). Mitotic figures are rare. A variable number of fibroblasts are intermixed among the theca-like cells. From a practical point of view, the diagnosis of thecoma is restricted to tumors that show evidence of steroid hormone secretion, have a conspicuous tumor composed of cells with clear or vacuolated cytoplasm, or contain luteinized cells (Fig. 6.4). Immunohistochemically, most thecomas express inhibin and calretinin.
6.2.3 Sclerosing Stromal Tumor
Sclerosing stromal tumors are uncommon benign stromal tumors that mainly occur in teenagers and young women [6]. They should be treated by excision or unilateral salpingo-oophorectomy. Macroscopically, these tumors are firm and white to yellowish-white. Histologically, they are characterized by the lobular proliferation of tumor cells with staghorn or hemangiopericytomatous vascular spaces. Tumor cells include polygonal theca-like cells with vacuolated eosinophilic cytoplasm and fibroblast-like cells (Fig. 6.5). Immunohistochemically, their cells are positive for vimentin, inhibin, calretinin, signal transducer activator of transcription 6 (STAT6), and the estrogen and progesterone receptors.
6.2.4 Microcytic Stromal Tumor
6.2.4.1 Clinical Features
This tumor has recently been described by Irving and Young [1] as a previously uncharacterized ovarian neoplasm that exhibits prominent microcystic changes and is most likely of stromal origin. The reported cases involved patients who ranged in age from 26 to 63 (mean, 45) years, and most patients presented with a pelvic mass. Hormonal manifestations are rarely seen. Microcytic stromal tumors are unilateral and do not undergo extraovarian spread.
6.2.4.2 Pathological Features
Microcystic stromal tumors are solid-cystic, solid, or predominantly cystic and display a mean diameter of 8.7 cm. Their solid components are firm and tan or white-tan. Microscopically, these ovarian tumors contain microcysts with variable amounts of solid cellular tissue and fibrous stroma. In addition, they exhibit lobular demarcation as well as sharp separation from the ovarian stroma. The microcysts are characterized by small round to oval cystic spaces. Intracytoplasmic lumens or vacuoles are also present (Fig. 6.6). The tumor cells contain moderate abundant finely granular, eosinophilic cytoplasm and bland, round to oval or spindle-shaped nuclei with fine chromatin and indistinct nucleoli [7]. Mitotic figures are very rare. This type of tumor is characterized by an absence of morphological features that would result in any other specific diagnosis in the sex cord-stroma category, an absence of epithelial elements, and an absence of teratomatous or other germ cell elements [7]. Immunohistochemically, the tumors are strongly positive for CD10 and vimentin, but do not express S-100 protein, calretinin, inhibin, epithelial membrane antigen (EMA), cytokeratin (CK), melan A, and estrogen receptors, desmin, chromogranin A, synaptophysin, WT1, or CD34 [1].
6.3 Pure Sex Cord Tumors
6.3.1 Adult Granulosa Cell Tumor (AGCT)
6.3.1.1 Clinical Features
Granulosa cell tumor is the most common type of malignant sex cord-stromal tumor. There are two types of granulosa cell tumor, the adult type, which mainly occurs in premenopausal and postmenopausal women (mean age, 45–55 years), and juvenile granulosa cell tumors (JGCT), which mainly occur in children (mean age, 15 years) [1]. It is important that the distinction between AGCT and JGCT is made on the basis of the histology and not the patient age. The typical clinical presentation of AGCT is postmenopausal bleeding in older women and menorrhagia or amenorrhea in younger patients. Granulosa cell tumors typically secrete estrogen, and patients with these tumors exhibit endometrial hyperplasia (30–40%) or adenocarcinoma (5–10%) [8]. Granulosa cell tumors are typically unilateral and confined to the ovary at diagnosis.
The overall recurrence rate ranges from 10 to 30%. Metastases or recurrence is often detected more than 5 years after the initial treatment, particularly in the peritoneum and omentum. There is no correlation between the microscopic features of tumors, including mitotic activity, and outcomes.
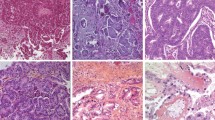
6.3.1.2 Pathological Features
Macroscopically, most AGCT are solid and cystic. The solid areas are soft to firm and yellow/brown to tan. Some tumors are predominantly cystic. The average size is about 10 cm. A variety of growth patterns are observed in AGCT, including admixtures of different patterns. The cells of such tumors often grow in microfollicular or diffuse patterns. Granulosa cell tumors consist of nests and sheets of granulosa cell-like cells punctuated by small spaces, which resemble Call-Exner bodies (Fig. 6.7). Occasionally, larger follicles are sometimes observed (the macrofollicular pattern). The cells of granulosa cell tumors are often arranged in cords, trabeculae, and ribbons (Fig. 6.8). In addition, they have scant pale cytoplasm and uniform, pale, round oval nuclei. Coffee bean-like nuclear grooves were considered to be a characteristic of granulosa cell tumors, but they are not seen every case, and they also occur in many other neoplasms, including Sertoli cell tumors and Sertoli-Leydig cell tumors. Brisk mitotic figures are seen in some lesions. Some AGCT have a JGCT component, and such tumors should be classified based on their predominant histology.
Immunohistochemically, granulosa cell tumors are usually positive for inhibin, calretinin, FOXL2 (forkhead box L2), WT1, and CD56, whereas they are negative for CK7 and EMA. A missense somatic point mutation that is characteristic of AGCT has recently been identified in the FOXL2 gene [9]. This mutation is seen in approximately 95% of AGCT.
6.3.2 Juvenile Granulosa Cell Tumor (JGCT)
6.3.2.1 Clinical Features
Fewer than 5% of granulosa cell tumors occur in children or teenagers. Almost all JGCT are unilateral, and more than 95% of them are confined to the ovary (stage I). The symptoms of JGCT are often caused by the estrogen they secrete. Young girls frequently display isosexual pseudoprecocity, whereas older children and premenopausal women develop menstrual abnormalities or amenorrhea. Associations have been detected between JGCT and Ollier (enchondromatosis) disease and Maffucci (enchondromatosis and multiple hemangiomas) syndrome [10]. The prognosis of patients with JGCT is better than that of patients with AGCT. JGCT are less likely to recur or metastasize. The long-term survival of patients with JGCT is good, but patients whose tumors rupture or who exhibit positive peritoneal cytology or extraovarian tumor spread are at significant risk of recurrence. Inhibin and Müllerian inhibitory substance are useful tumor markers for following up patients with JGCT.
6.3.2.2 Pathological Features
The average size is about 12 cm, and most of them exhibit a mixed solid-cystic appearance, but some are completely solid or cystic. Their solid areas are yellow or tan. Hemorrhaging is sometimes seen, but necrosis is uncommon.
Microscopically, JGCT show a multinodular growth pattern, and macrofollicular, solid, and cystic growth patterns are characteristic of JGCT. Follicles often vary in size and shape and contain mucinous material (Fig. 6.9), macrofollicles are lined by one or more layers of granulosa cells and are surrounded by a rim of theca cells. Solid areas are composed of sheets of granular cells made up of an admixture of theca cells or fibroblasts. The microfollicular, insular patterns and trabeculae seen in AGCT are rarely observed in JGCT. Tumor cells have large and round nuclei and amphophilic or pink cytoplasm. In addition, they lack coffee bean-like nuclear grooves and may contain conspicuous nucleoli. Some tumor cells have enlarged pleomorphic nuclei, and multinucleated cells can also be observed (Fig. 6.10). Mitotic figures tend to be numerus with an average around 6/10HPF.
The immunohistochemical features of JGCT are similar to those of AGCT. A small minority of JGCT express FOXL2, and the FOXL2 mutation that occurs in AGCT is generally absent in JGCT [10], indicating that these two tumors, both of which are composed of granulosa cells, probably have different pathogenic mechanisms. Immunohistochemistry is of considerable value for differentiating JCGT from small cell carcinoma, hypercalcemic type (SCCHT); SCCHT does not exhibit nuclear immunoreactivity for SMARCA4 (INI1) and is focally positive for EMA, while JGCT is positive for sex cord markers, negative for EMA, and exhibits positive nuclear staining for SMARCA4.
6.3.3 Sex Cord Tumor with Annular Tubules (SCTAT)
6.3.3.1 Clinical Features
About a third of patients with SCTAT have Peutz-Jeghers syndrome (PJS) [11, 12]. In these patients, the lesions are found incidentally, are often bilateral, and grossly appear to be yellow nodules of up to 3 cm in diameter. In patients without PJS (sporadic), SCTAT tumors are always unilateral, moderately large, and present as palpable masses. In patients with PJS, SCTAT presents at a mean age of 27 years, whereas it tends to appear around 34 years in patients without PJS. Subsets of both sporadic and PJS-associated SCTAT might be associated with hyperestrinism and menstrual irregularities. SCTAT is primarily treated with surgery, and PJS-associated tumors are entirely benign (albeit multifocal). About one-fifth of sporadic cases is clinically malignant and spread via the lymphatics. Recurrent lesions often occur late. Patients with PJS carry a 5–15% risk of developing sex cord-stromal tumors (SCTAT). PJS is characterized by a germline mutation of the STK 11 (serine threonine kinase 11) gene on chromosome 19p. Patients with PJS are at very high risk of gastrointestinal and non-gastrointestinal cancer (carcinoma of the gastrointestinal tract, pancreas, and breast) [13] and adenoma malignum (gastric-type mucinous adenocarcinoma) (10% risk) of the uterine cervix.
6.3.3.2 Pathological Features
SCTAT is a distinctive type of ovarian neoplasm with morphological features that are intermediate between those of granulosa cell tumors and Sertoli cell tumors. While differentiation into either of the two latter tumors can occur in some cases, Scully reported that the distinctive architecture of SCTAT, which involves simple and complex ring-shaped tubules, warrants a separate designation [11].
PJS-associated and sporadic SCATAT histologically consist of well-circumscribed round nests of cells and a mixture of simple and complex ring-shaped tubules, which contain hyalinized basement membrane-like material (Fig. 6.11). The nests or tubules are composed of uniform cells with peripherally located nuclei and a moderate amount of cytoplasm. Multiple tumorlets form single tubules or clusters of tubules, and calcifications are scattered within the ovarian stroma. Large tumors in non-PJS patients can exhibit extensive hyalinization of the tubules and stroma. Ultrastructural examinations demonstrate bundles of Charcot-Bottcher filaments in some cases of SCTAT, leading some authorities to consider this neoplasm as a subtype of Sertoli or granulosa cell tumor [14]. However, the distinctive features of SCTAT and its frequent association with PJS warrant its classification as a specific form of sex cord-stromal tumor. Immunohistochemically, SCTAT shows positive staining for inhibin, calretinin, vimentin, and CK, but is negative for EMA.
6.4 Mixed Sex Cord-Stromal Tumors
6.4.1 Sertoli-Leydig Cell Tumor (SLCT)
The WHO classification divides SLCT into retiform and well, moderately, and poorly differentiated variants. The moderately differentiated, poorly differentiated, and retiform variants sometimes contain heterologous elements.
6.4.1.1 Clinical Features
SLCT mainly arise in relatively young patients (mean age, 25 years). The retiform variant usually occurs in particularly young patients (mean age, 15 years). The symptoms of SLCT are related to the presence of an ovarian mass and virilization. Approximately 50% of SLCT secrete steroid hormones, which can also cause symptoms, and 40% of patients are virilized [15]. The serum testosterone and urine 17-ketosteroid levels of SLCT patients are increased. Most tumors are unilateral and confined to the ovary at presentation. Well-differentiated SLCT is clinically benign and does not recur after complete excision. The prognosis of patients with intermediate and poorly differentiated SLCT is generally favorable, but patients with poorly differentiated SLCT can exhibit an aggressive clinical course.
6.4.1.2 Pathological Features
Macroscopically, SLCT are usually solid and partly cystic, and the solid areas of SLCT are firm or soft and yellow or tan. Well-differentiated SLCT exhibit a mean size of 5 cm, whereas the intermediate and poorly differentiated types both display a mean size of 15 cm. Poorly differentiated tumors tend to be larger than those demonstrating intermediate differentiation [15].
Well-differentiated SLCT is histologically characterized by hollow or closed tubules lined by columnar Sertoli cells and surrounded by a fibrous stroma. Aggregates of luteinized Leydig cells are often observed (Fig. 6.12). Reinke crystalloids are rarely found in Leydig cells. Cellular atypia and mitotic figures are rare in well-differentiated SLCT.
Intermediate and poorly differentiated SLCT are composed of mature and immature Sertoli cells. Various proliferative patterns are seen in such tumors, including well-formed tubules, ill-defined tubules, trabeculae, and cord-like arrangements (Fig. 6.13). The tubules have a retiform appearance in 10–25% of intermediate and poorly differentiated tumors. The retiform tubules are branched and lined by low columnar to cuboidal cells. Bizarre cells can also be seen, but this does not appear to be an adverse prognostic finding. Cases of SLCT involving a predominant retiform growth pattern should be diagnosed as retiform variant (Fig. 6.14). In poorly differentiated tumors, the sarcomatous proliferation of immature stromal cells is predominant (Fig. 6.15). Brisk mitotic figures are also seen.
Heterologous elements are seen in 20–25% of intermediate and poorly differentiated SLCT. Intestinal-type mucinous epithelial tissue is the most common heterologous element (Fig. 6.16). Mucinous components can be composed of mucinous cystadenoma, a mucinous borderline tumor, or mucinous adenocarcinoma. Carcinoid cells, cartilage, neuroblasts, and rhabdomyoblasts have also been observed in such heterologous elements [16].
Immunohistochemically, most mature and immature Sertoli cells are positive for CK, but negative for EMA. Most cases of SLCT show positive membrane staining for CD99 and nuclear staining for WT1. The stromal cells of such tumors are positive for vimentin. Sertoli cells and Leydig cells are positive for inhibin (Fig. 6.17) and calretinin. Sertoli-form endometrioid adenocarcinoma of the ovary mimics SLCT, but is positive for EMA and negative for inhibin and calretinin. Histologically, Sertoli-form endometrioid adenocarcinoma displays greater cellular atypia, more irregular tubular arrangements, and necrosis.
6.5 Immature Teratoma
6.5.1 Clinical Features
Immature teratoma is one of most common malignant germ cell tumor of the ovary. This tumor occurs predominantly in children and young adult. The clinical presentation is nonspecific, such as abdominal discomfort, pelvic pain, abdominal swelling, or a palpable abdominal mass. They are unilateral and spread mainly to the pelvic and peritoneum by implantation.
6.5.2 Pathologic Features
Macroscopically immature teratoma is a predominantly solid tumor. The cut surface is gray or brown and soft. It may contain cysts, hemorrhage, and necrosis.
Histologically, a mixed mature and mature element is found in most tumors. Recognition of immature neuroectodermal element is most important to make a diagnosis of immature teratoma. These include sheets of mitotically active immature neuroepithelial cells, tubules lined by columnar embryonal cells with stratified hyperchromatic nuclei, nests of neuroblasts, Homer-Wright rosettes, mitotically active glia, and primitive retina with melanin pigments (Figs. 6.18 and 6.19). Immature cartilage, adipose, bone, and skeletal muscle are often present.
Immature teratoma should be histologically graded [1]:
-
Grade 1: Tumors with rare foci of immature neuroepithelial tissue that occupy < low power fields (40×) in any slide (low grade).
-
Grade 2: Tumors with similar elements, occupying 1–3 power fields (40×) in any slide (high grade).
-
Grade 3: Tumors with large amount of immature neuroepithelial tissue occupying > 3 low power field (40×) in any slide (high grade).
Grade 1 cases are not treated and grade 2 and 3 are treated with same chemotherapy. Stage and grade of the primary tumor and metastases remain important predictive factor. In approximately one-third of cases, gliomatosis peritonei is observed [20]. This lesion has been considered a possible metastasis from teratoma; however, it may represent an independent lesion, probably peritoneal metaplasia [17]. The presence of gliomatosis peritonei does not indicate adverse clinical effect.
6.6 Small Cell Carcinoma of Ovary, Hypercalcemic Type
6.6.1 Clinical Features
Small cell carcinoma of the ovary, hypercalcemic type (SCCHT), is a rare neoplasm that occurs in young females. Its histogenesis is unclear, and it is categorized as a miscellaneous tumor in the revised WHO classification [1].
The reported patients with SCCHT ranged in age from 14 months to 43 (mean, 24) years [18,19,20,21,22,23]. Most patients present with signs and symptoms related to an abdominal or pelvic mass, but in rare cases, patients will present with clinical symptoms related to hypercalcemia. Approximately 66% of patients present with hypercalcemia [19]. Some studies have serologically documented the presence of parathyroid hormone-related protein. This type of ovarian carcinoma has a dismal prognosis. About 50% of such tumors have spread beyond the ovary at the time of laparotomy. The overall survival rate of SCCHT is approximately 16%.
6.6.2 Pathological Features
SCCHT typically appear as yellowish-white, soft solid tumors with marked hemorrhaging and necrosis. SCCHT exhibit a mean diameter of 15 cm. Most SCCHT are unilateral (Fig. 6.20).
SCCHT are histologically composed of small to medium-sized round cells arranged in a solid sheet or follicular pattern (Figs. 6.21 and 6.22). Follicles that vary from small to large in size are considered to be an important feature of SCCHT, and such follicles are seen in about 80% of these tumors. The follicles contain periodic acid–Schiff-positive proteinaceous material. SCCHT usually display moderate atypia and numerous mitotic figures (typical frequency, >20/10 HPF) (Fig. 6.22). Furthermore, tumor necrosis and hemorrhaging are often prominent, whereas the stroma is fibrous but inconspicuous. In addition, a “large cell-type” variant of SCCHT, which is sometimes called “rhabdoid tumor of the ovary,” is also known to exist [23] (Fig. 6.23).
Immunohistochemically, SCCHT are focally positive for EMA and low molecular weight CK. Nuclear staining for p53 is often observed, and diffuse strong nuclear staining for WT1 is seen in most cases. A minority of tumors show focal staining for neuroendocrine markers, such as CD56, chromogranin A, or synaptophysin. Staining for CD99, desmin, inhibin, calretinin, and thyroid transcription factor-1 (TTF-1) is negative.
Recently, inactivating mutations in SMARCA4, a member of the switch/sucrose non-fermenting chromatin remodeling complex, have been identified as driving events in most cases of SCCHT [24], and SCCHT exhibits complete immunohistochemical loss of SMARCA4 (INI1) (Fig. 6.24) [25]. Thus, SMARCA4 immunohistochemistry is a highly valuable tool for identifying SCCHT.
6.6.3 Differential Diagnosis
The differential diagnoses of SCCHT include sex cord-stromal tumors, small blue round cell tumor neoplasms, and pulmonary-type ovarian small cell carcinoma. SCCHT is often confused with granulosa cell tumors [10, 26]. Adult granulosa cell tumors are rare in the young. Most SCCHT have spread beyond the ovary at presentation, which is unusual in both variants of granulosa cell tumor. Granulosa cell tumors are usually positive for inhibin-alpha and calretinin, but negative for EMA. These features are opposite to those of SCCHT. Pulmonary-type small cell carcinoma lacks the follicular arrangement that is characteristic of SCCHT and is positive for neuroendocrine markers. SCCHT, particularly the large cell variant, can be misdiagnosed as undifferentiated carcinoma or melanoma. The large cell variant of SCCHT should always be considered in young patients with suspected undifferentiated carcinoma, and a diligent search for typical small cell carcinoma foci, including the presence of follicles, should be performed.
6.7 Solid Pseudopapillary Neoplasm of the Ovary
These tumors are histologically and immunohistochemically identical to pancreatic solid pseudopapillary neoplasms [27, 28]. The reported patients with solid pseudopapillary neoplasms of the ovary ranged in age from 17 to 57 years. Macroscopically, these tumors are solid and cystic, and histologically they exhibit diffuse, pseudopapillary, nested, and microcystic growth patterns (Fig. 6.25). In these lesions, the tumor cells have a moderate amount of pale or eosinophilic cytoplasm and uniform round nuclei. Mitoses and atypia are rare. In addition, they are positive for beta-catenin and negative for E-cadherin. The differential diagnoses of solid pseudopapillary neoplasm of the ovary include sex cord-stromal tumors, steroid cell tumors, and struma ovarii. This type of tumor rarely occurs at extrapancreatic sites [29]. Deshpande et al. [27] reported that one of three patients died of their disease and that these tumors exhibit necrosis, lymphovascular invasion, and brisk mitotic figures [27].
Conclusion
Non-epithelial ovarian tumors have posed pathologic diagnosis, and a correct diagnosis is imperative for appropriate therapies. Many of these neoplasms and those in the differential diagnosis occur predominantly in young women, and they can be aggressive and require specific chemotherapy. Some of non-epithelial neoplasms show histologically biphasic or epithelioid features, mimicking epithelial tumors. A few non-epithelial tumors are not specific to the ovary and may arise more frequently at extraovarian sites. The recent discovery of somatic mutations in FOXL2 in adult granulosa cell tumors and germline and somatic mutations in DICER1 in Sertoli-Leydig cell tumors and SMARCA4 in small cell carcinoma, hypercalcemic type, contributes immunohistochemical analyses and molecular research of these tumors.
References
Kurman RJ, Carcangiu ML, Herrington SC, et al. WHO classification of tumours of female reproductive organs. Lyon: IARC Press; 2014.
Foulks WD, Gore M, McCluggage WG. Rare non-epithelial ovarian neoplasms: pathology, genetics and treatment. Gynecol Oncol. 2016;142:190–8.
Prat J, Scully RE. Cellular fibromas and fibrosarcomas of the ovary: a comparative clinicopathologic analysis of seventeen cases. Cancer. 1981;47:2663–70.
Irving JA, Alkushi A, Young RH, et al. Cellular fibromas of the ovary: a study of f75 cases including 40 mitotically active tumors emphasizing their distinction from fibrosarcoma. Am J Surg Pathol. 2006;30:929–38.
Zhang J, Young RH, Arseneau J, et al. Ovarian stromal tumors containing lutein or Leydig cells (luteinized thecomas and stromal Leydig tumors): a clinicopathological analysis of 50 cases. Int J Gynecol Pathol. 1982;1:270–85.
Chalvardijan A, Scully RE. Sclerosing stromal tumors of the ovary. Cancer. 1973;31:664–70.
Irving JA, Young RH. Microcystic stromal tumor of the ovary. Report of 16 cases of a hitherto uncharacterized distinctive ovarian neoplasm. Am J Surg Pathol. 2009;33:367–75.
Pautier P, Lhomme C, Culine S, et al. Adult granulosa – cell tumor of the ovary: a retrospective study of 45 cases. Int J Gynecol Cancer. 1997;7:58–65.
Shah AF, Kobel M, Senz J, et al. Mutation of FOXL2 in granulosa-cell tumors of the ovary. N Engl J Med. 2009;360:2719–29.
Young RH, Dickersin GR, Scully RE. Juvenile granulosa cell tumor of the ovary: a clinicopathological analysis of 125 cases. Am J Surg Pathol. 1984;8:575–96.
Scully RE. Sex cord tumor with annular tubules. A distinctive ovarian tumor of the Peutz-Jeghers syndrome. Cancer. 1970;5:1107–21.
Young RH, Welch WR, Dickerson GR, Scully RE. Ovarian sex cord tumor with annular tubules. Cancer. 1982;50:1384–402.
Giardiello FM, et al. Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology. 2000;119:1447–53.
Ahn GH, Chi JG, Lee SK. Ovarian sex cord tumor with annular tubules. Cancer. 1986;57:1066–73.
Young RH, Scully RE. Ovarian Sertoli-Leydig cell tumors: a clinicopathologic analysis of 207 cases. Am J Surg Pathol. 1985;9:543–69.
Young RH, Prat J, Scully RE. Ovaria Sertoli-Leydig cell tumors with heterologous elements. I. Gastrointestinal epithelium and carcinoid: a clinicopathologic analysis of 36 cases. Cancer. 1982;50:2448–58.
Ferguson AW, Katabuchi H, Ronnett BM, Cho KR. Glial implants in gliomatosis peritonei arise from normal tissue, not from the associated teratoma. Am J Pathol. 2001;159:51–5.
Dickersin GR, Kline IW, Scully RE. Small cell carcinoma of the ovary with hypercalcemia. A report of 11 cases. Cancer. 1982;49:188–97.
Young RH, Oliva E, Scully RE. Small cell carcinoma of the ovary, hypercalcemic type: a clinicopathologic analysis of 150 cases. Am J Surg Pathol. 1994;18:1102–16.
McCluggage WG, Oliva E, Connolly LE, McBride HA, Young RH. An immunohistochemical analysis of ovarian small cell carcinoma of hypercalcemic type. Int J Gynecol Pathol. 2004;23:330–6.
Florell SC, Bruggers CS, Matlak M, Young RH, Lowichik A. Ovarian small cell carcinoma of the hypercalcemic type in a 14-month-old: the youngest reported case. Med Pediatr Oncol. 1999;32:304–7.
Clement PB. Selected miscellaneous ovarian lesions: small cell carcinoma, mesothelial lesions, mesenchymal and mixed neoplasms, and non-neoplastic lesions. Mod Pathol. 2005;18:113–29.
Fukunaga M, Endo Y, Nomura K, Ushigome S. Small cell carcinoma of the ovary: a case report of large cell variant. Pathol Int. 1997;47:250–5.
Wang X, Haswell JR, Roberts CW. Molecular pathway: SW1/SNF (BAF) complexes are frequently mutated in cancer-mechanisms and potential therapeutic insights. Clin Caner Res. 2014;20:21–7.
Agaimy A, Thiel F, Hartmann A, Fukunaga M. SMARCA4-deficient undifferentiated carcinoma of the ovary (small cell carcinoma, hypercalcemic type): clinicopathologic and immunohistochemical studies of 3 cases. Ann Diagn Pathol. 2015;19:153–7.
Zaloudek C, Norris HJ. Granulosa tumors of the ovary in children. A clinical and pathologic study of 32 cases. Am J Surg Pathol. 1982;6:503–12.
Deshpande V, Olive E, Young RH. Solid pseudopapillary neoplasm of the ovary: a report of 3 primary ovarian tumors resembling those of the pancreas. Am J Surg Pathol. 2010;10:1514–20.
Abraham SC, Klimstra DS, Wilents RE, et al. Solid-pseudopapillary tumors of the pancreas are genetically distinct from pancreatic ductal adenocarcinomas and almost always harbor beta-catenin mutations. Am J Pathol. 2002;160:1361–9.
Fukunaga M. Pseudopapillary solid cystic tumor arising from an extrapancreatic site. Arch Pathol Lab Med. 2001;125:1368–71.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Fukunaga, M. (2017). Pathology of Non-epithelial Ovarian Tumors. In: Katabuchi, H. (eds) Frontiers in Ovarian Cancer Science. Comprehensive Gynecology and Obstetrics. Springer, Singapore. https://doi.org/10.1007/978-981-10-4160-0_6
Download citation
DOI: https://doi.org/10.1007/978-981-10-4160-0_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-4159-4
Online ISBN: 978-981-10-4160-0
eBook Packages: MedicineMedicine (R0)