Abstract
Although the coronary angiography (CAG) can visualize the improvement of luminal narrowing after stent implantation in coronary atherosclerotic lesions, it only provides indirect vessel information using contrast medium because of a shadow image at stented segments as well as adjacent reference segments. Intravascular ultrasound (IVUS) is capable of generating a cross-sectional anatomy of the vessel wall comparable to corresponding histologic image, resulting in providing more information of atherosclerotic coronary plaque either quantitatively or qualitatively. On the other hand, stent struts appear as focal, bright spots at cross-sectional and longitudinal images owing to a strong echoreflection by ultrasound beam. Thus, it allows detailed information regarding stent strut expansion, intra-stent luminal condition, and plaque characteristics at adjacent reference vessel area [1]. The routine use of IVUS in daily practice is still a matter of debate in current drug-eluting stent (DES) era, however, stent optimization by IVUS immediately after stent deployment has reported to improve clinical outcomes, especially during complex percutaneous coronary intervention (PCI) [2, 3]. This chapter reviews important IVUS findings after stent implantation and its clinical relevance.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction
Although the coronary angiography (CAG) can visualize the improvement of luminal narrowing after stent implantation in coronary atherosclerotic lesions, it only provides indirect vessel information using contrast medium because of a shadow image at stented segments as well as adjacent reference segments. Intravascular ultrasound (IVUS) is capable of generating a cross-sectional anatomy of the vessel wall comparable to corresponding histologic image, resulting in providing more information of atherosclerotic coronary plaque either quantitatively or qualitatively. On the other hand, stent struts appear as focal, bright spots at cross-sectional and longitudinal images owing to a strong echoreflection by ultrasound beam. Thus, it allows detailed information regarding stent strut expansion, intra-stent luminal condition, and plaque characteristics at adjacent reference vessel area [1]. The routine use of IVUS in daily practice is still a matter of debate in current drug-eluting stent (DES) era, however, stent optimization by IVUS immediately after stent deployment has reported to improve clinical outcomes, especially during complex percutaneous coronary intervention (PCI) [2, 3]. This chapter reviews important IVUS findings after stent implantation and its clinical relevance.
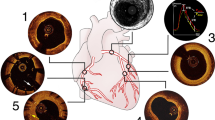
2 Evaluation of Stent Symmetry and Eccentricity
Symmetry index (SI) defines minimum stent diameter/maximum stent diameter (Fig. 7.1) [4]. Asymmetry index (AI) also can be used to express the stent symmetry: (1 − minimum stent diameter/maximum stent diameter) [5]. Because maximum and minimum stent diameters are the values throughout an entire stented segment, these diameters can derive from different cross section in the stented segment. A stent was characterized as asymmetric when the value of AI was over 0.3 (which corresponds to SI of 0.70 from the MUSIC study). Post-procedural asymmetry of device was associated with unfavorable clinical outcomes [6].
Eccentricity index (EI) was calculated as minimum stent diameter/maximum stent diameter to show the circularity of the cross section. Therefore, the calculation of minimum and maximum stent diameters were derived from the same cross section frame by frame and value was expressed as an average. A stent with EI ≥ 0.7 was defined as concentric while EI < 0.7 was defined as eccentric [7, 8]. The eccentricity of DES had been previously considered as one of the factors for restenosis, because of the higher possibility of the uneven diffusion of the drug into the arterial wall [9]. However, subsequent reports showed that eccentricity of DES did not have any clinical impact because DES powerfully suppressed the neointimal formation [8, 10].
3 Measurement of Minimal Stent Area
Minimal stent area (MSA ) of bare metal stent (BMS) for long-term patency was considered as 6.4–6.5 mm2 [11, 12], and adequate post-interventional MSA of DES was 5.0–5.7 mm2 (Fig. 7.2) [13,14,15]. In left main lesions, optimal MSA was reported as 8.7 mm2 in the MAIN-COMPARE (revascularization for unprotected left main coronary artery stenosis: comparison of percutaneous coronary angioplasty versus surgical revascularization) study [2]. Considering 4 segments of left main bifurcation, the best minimal stent area criteria to predict angiographic restenosis were 5.0 mm2 (ostial left circumflex artery), 6.3 mm2 (ostial left anterior descending artery), 7.2 mm2 (polygon of confluence [POC]), and 8.2 mm2 (proximal left main artery above the POC) (Fig. 7.3) [16].
Minimal stent area (MSA) for left main bifurcation lesion. Considering 4 segments of left main bifurcation, the best MSA criteria were 5.0 mm2 (ostial left circumflex artery), 6.3 mm2 (ostial left anterior descending artery), 7.2 mm2 (polygon of confluence [POC]), and 8.2 mm2 (proximal left main artery above the POC)
4 Evaluation of Stent Expansion (Well Expansion vs. Underexpansion)
In the BMS era, MUSIC study (multicenter ultrasound stenting in coronaries study) defined adequate expansion as >90% of the average reference cross-sectional area (CSA), or >100% of a smaller reference CSA with complete apposition and symmetric expansion [4]. CRUISE (Can Routine Ultrasound Influence Stent Expansion) study showed better stent expansion of IVUS-guided PCI than angiography-guided PCI, especially in terms of target vessel revascularization (TVR), but not in mortality or myocardial infarction [17]. In contrast to the BMS era, early studies of IVUS-guided PCI with DES had no significant benefit in terms of TVR or clinical events. AVIO (Angiography Versus IVUS Optimization) study which defined optimal stent expansion as final minimum stent CSA of at least 70% of the hypothetical CSA of the fully inflated balloon used for post-dilatation did not show any difference in clinical outcome [18]. However, attention should be paid to avoid stent underexpansion. Several evidences indicate that stent underexpansion is one of the major causes of stent failure such as stent restenosis or stent thrombosis (Table 7.1) [14, 19,20,21]. ADAPT-DES (Assessment of Dual Antiplatelet Therapy With Drug-Eluting Stents) study showed reduction in stent thrombosis, myocardial infarction, and major adverse cardiac events by IVUS-guided optimization of stent expansion and apposition [22]. Representative IVUS images of underexpansion and well expansion are shown in Fig. 7.4.
A representative images of stent underexpansion and well expansion. A 53-year-old man was admitted with stable angina. The coronary angiogram (CAG) showed significant stenosis (dotted line) on mid and distal right coronary artery (RCA) (a). Two drug-eluting stents (Ultimaster 3.0 × 33 mm on mid RCA and Ultimaster 2.75 × 18 mm on distal RCA) were implanted separately and CAG after stent implantation showed stent underexpansion on distal RCA (b, arrow). Corresponding intravascular ultrasound image showed minimal stent area (MSA) of 2.57 mm2 (b1). After additional dilation with noncompliant balloon, CAG showed well expansion of distal stent (c, arrow) and MSA was increased as 5.06 mm2 (c1)
5 Detection of Stent Edge Dissection
Stent edge dissection is a tear in the plaque parallel to the vessel wall with visualization of blood flow in the false lumen <5 mm to a stent edge. The incidence of edge dissections by IVUS is approximately 10–20% and 40% of the IVUS-identified dissections was not detected by angiography [23,24,25]. Significant (major) edge dissections, defined by IVUS as lumen area < 4 mm2 or dissection angle ≥60°, have been associated with early stent thrombosis [26]. However, minor non-flow-limiting dissection at the edge of stent may not be associated with an increased incidence of clinical events although no consensus exists on an optimal strategy. Figure 7.5 is an example of stent edge dissection.
A case of stent edge dissection . A 60-year-old woman with stable angina showed calcified stenotic lesion (dotted line) on mid-right coronary artery (a). The coronary angiogram after drug-eluting stent implantation showed small dissection on proximal stent edge (b, arrow). Dissection flap (asterisk) was observed by intravascular ultrasound (c)
6 Detection of Acute Incomplete Stent Apposition
Incomplete stent apposition (ISA) , synonymous with stent malapposition, was defined as the absence of contact between at least one strut and the lumen wall that did not overlap a side branch with evidence of blood speckle behind the strut and can occur acutely after stent implantation (acute ISA) or develop over time (late-acquired ISA). Acute ISA is almost due to suboptimal stent deployment. The frequency of acute ISA has been reported to be nearly 10% and it appears not to be associated with increased cardiac events [27, 28].
7 Detection of Tissue Protrusion (Plaque Prolapse and Intra-stent Thrombus)
Tissue protrusion (TP ) was defined as a visible tissue extrusion through the stent struts by IVUS (Fig. 7.6) [29, 30]. Although thrombus was characterized by heterogeneous echodensity tissue with a sparkling pattern by IVUS [31], the accurate discrimination of atherosclerotic plaque and thrombus within stent is very difficult because of limited resolution of IVUS. Thus, TP includes plaque and/or thrombus extrusion within stent [32]. The incidence of TP has been reported in various ranges between 20% and 73%, depended on characteristics of enrolled patients (Table 7.2) [29, 30, 32,33,34,35,36]. In fact, TP is likely to develop in patients with acute coronary syndrome, especially ST-segment elevation myocardial infarction owing to a higher chance of thrombus or friable plaque compared to stable patients [32, 35] and receiving longer stent probably caused by unequal distribution of inflation pressure during stent deployment [30, 34]. Other predictors of TP are larger reference lumen area, greater plaque burden, more plaque rupture, attenuated plaque, positive vascular remodeling, and virtual histology thin-cap fibroatheroma by IVUS [30, 32]. The clinical impact of TP remains a controversy. Previous studies suggested that TP after stent implantation may increase the risk of stent thrombosis [26, 37]. Other studies, however, have been failed to show this relationship [29, 32, 38].
Representative cases of tissue protrusion . A 65-year-old man was admitted with ST-segment elevation myocardial infarction (a). The coronary angiogram (CAG) after drug-eluting stent (DES) implantation showed no luminal narrowing within stented segments (a1, arrow). Correspondingly, intravascular ultrasound (IVUS) revealed tissue protrusion (plaque and/or thrombus) between stent struts (a2, arrowheads). A 55-year-old woman was admitted with ST-segment elevation myocardial infarction (b). The CAG after DES implantation showed mild luminal narrowing within stented segments (b1, arrow). Correspondingly, IVUS revealed tissue protrusion (most likely thrombus) between stent struts (b2, arrowheads)
Although some investigators demonstrated greater cardiac enzyme elevation after stent implantation in patients with TP, it did not translate into the increased risk of stent thrombosis or periprocedural myocardial infarction [30, 32]. An IVUS substudy from ADAPT-DES reported the 2-year clinical outcomes of TP after stenting. At 2-year clinical follow-up, there was no difference in the rate of major adverse cardiac events between patients with or without TP. Interestingly, patients with TP showed a less frequency of clinically driven target lesion revascularization at 2 years (1.9% vs. 4.0%, p = 0.008), probably due to larger minimal stent area at the end of procedure [32]. Taken together, TP may influence the early clinical phase rather than late clinical stage after stent implantation even though its clinical significance is still uncertain.
8 Evaluation of Full Lesion Coverage
IVUS can assess plaque amount in atherosclerotic coronary lesion, enabling to determine reference segment during stent implantation. Based on IVUS examination, reference segment is defined as <40% of plaque burden at cross-sectional image adjacent to the lesion [39]. Early IVUS study has demonstrated that angiographically normal looking segments, namely reference vessel segments, have 30–50% of plaque burden at cross-sectional image [40]. Several studies have shown that a reference segment that has >50% of plaque burden at cross-sectional area may increase the risk of target lesion revascularization or restenosis at follow-up after DES implantation (Fig. 7.7) (Table 7.3) [41,42,43]. Recent study also reported plaque burden with a cutoff value of 54.7% at less than 1 mm from proximal stent edge as a predictor of stent edge restenosis after everolimus-eluting stent implantation [43]. During or after stent deployment, thus, estimation of plaque amount at landing point determined by IVUS can assess future clinical outcomes.
Representative cases of appropriate (a–c) and inappropriate (d–f) location of drug-eluting stent (DES) based on post-stenting intravascular ultrasound findings. A 49-year-old man with acute myocardial infarction was treated with a second-generation DES 3.0 × 30 mm (dotted line) at mid to proximal left anterior descending artery (a). There is a well-expanded and apposed struts at the proximal (b2) and distal (b3) edges of stent. In addition, less than 50% of plaque burden is observed at proximal (b1) and distal (b4) reference segments, suggesting that the location of deployed stent is appropriate. A 68-year-old man with stable angina was treated with a second-generation DES 3.0 × 16 mm (dotted line) at mid right coronary artery (d). There is a well-expanded and apposed struts at the proximal (e2) and distal (e3) edges of stent. However, more than 50% of plaque burden is observed at proximal (e1) and distal (e4) reference segments, suggesting that the location of deployed stent is inappropriate
9 Evaluation of Plaque Characteristics at Stented or Reference Segments
IVUS can provide qualitative and quantitative change of plaque characteristics at stented segments as well as adjacent reference segments by serial IVUS examination. Analysis of radiofrequency backscatter signals of IVUS allows us to understand whether stent strut is placed underlying necrotic core or not at reference segments due to capability of tissue characterization at adjacent segment to the stent [44]. One investigator reported that a higher frequency of plaque vulnerability behind the stent strut as well as at reference segments in DES-treated lesions compared to BMS by virtual histology IVUS (VH-IVUS) [44]. Another long-term serial VH-IVUS study demonstrated similar change of neointimal tissue characterization beyond 3 years between DES and BMS [45]. On the other hand, a recent study suggested that decrease in plaque located behind the stent area may be associated with neointimal proliferation at follow-up after BMS implantation [46].
10 Impact on Final Procedure During Stent Deployment
The most important utility of IVUS after stent implantation is that it can provide information whether additional procedure is needed or not. An IVUS substudy from ADAPT-DES showed that the operator changed the PCI strategy based on IVUS findings in three fourth of 3349 patients including the use of a larger stent or balloon (38%) and a longer stent (22%), higher inflation pressure (23%), additional post-stent dilatation due to underexpansion (13%) or incomplete apposition (7%), and additional stent implantation (8%) [22]. Among them, post-stenting IVUS was performed in 93% of patients (Fig. 7.8). A study by Kim et al. also reported that post-stenting IVUS findings contributed to performance of additional balloon inflation or stent implantation [47].
The frequency and detailed information of changed the percutaneous coronary intervention (PCI) strateg y after procedural intravascular ultrasound use (data from ADAPT-DES study) [22]. The operator changed the PCI strategy in 74% (2484/3349) of patients to choose (1) a larger stent or balloon (in 38% [943/2484] of cases); (2) higher inflation pressures (in 23% [564/2484] of cases); (3) a longer stent (in 22% [546/2484] of cases); (4) additional post-stent dilatation because of incomplete expansion (in 13% [329/2484]) or incomplete stent apposition (in 7% [166/2484]); and/or (5) additional stent placement (in 8% [197/2484])
11 Summary
Since stent optimization has been reported to be associated with clinical events, IVUS assessment after stent implantation might be important in a clinical point of view. Although the clinical relevance of stent eccentricity, acute stent malapposition, and tissue protrusion was a matter of debate, numerous studies have shown that smaller MSA, stent underexpansion, and major edge dissection were independent predictors of poor clinical outcomes. Even in the current era of bioresorbable scaffold, improved procedural results under IVUS guidance still contribute to avoidance of early scaffold failure. In conclusion, post-stenting IVUS can offer qualitative as well as quantitative information within and adjacent stented segments that may expand our comprehensive understanding during procedure. Importantly, the major role of IVUS after stent implantation is that IVUS-driven suboptimal procedure results can provide a clue of whether operator should perform additional intervention during stenting procedure for making better acute and long-term clinical outcomes.
References
Yoon HJ, Hur SH. Optimization of stent deployment by intravascular ultrasound. Korean J Intern Med. 2012;27(1):30–8.
Park SJ, Kim YH, Park DW, Lee SW, Kim WJ, Suh J, et al. Impact of intravascular ultrasound guidance on long-term mortality in stenting for unprotected left main coronary artery stenosis. Circ Cardiovasc Interv. 2009;2(3):167–77.
Hong SJ, Kim BK, Shin DH, Nam CM, Kim JS, Ko YG, et al. Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: the IVUS-XPL randomized clinical trial. JAMA. 2015;314(20):2155–63.
de Jaegere P, Mudra H, Figulla H, Almagor Y, Doucet S, Penn I, et al. Intravascular ultrasound-guided optimized stent deployment. Immediate and 6 months clinical and angiographic results from the multicenter ultrasound stenting in coronaries study (MUSIC study). Eur Heart J. 1998;19(8):1214–23.
Brugaletta S, Gomez-Lara J, Diletti R, Farooq V, van Geuns RJ, de Bruyne B, et al. Comparison of in vivo eccentricity and symmetry indices between metallic stents and bioresorbable vascular scaffolds: insights from the ABSORB and SPIRIT trials. Catheter Cardiovasc Interv. 2012;79(2):219–28.
Suwannasom P, Sotomi Y, Ishibashi Y, Cavalcante R, Albuquerque FN, Macaya C, et al. The impact of post-procedural asymmetry, expansion, and eccentricity of bioresorbable everolimus-eluting scaffold and metallic everolimus-eluting stent on clinical outcomes in the ABSORB II trial. JACC Cardiovasc Interv. 2016;9(12):1231–42.
von Birgelen C, Gil R, Ruygrok P, Prati F, Di Mario C, van der Giessen WJ, et al. Optimized expansion of the Wallstent compared with the Palmaz-Schatz stent: on-line observations with two- and three-dimensional intracoronary ultrasound after angiographic guidance. Am Heart J. 1996;131(6):1067–75.
Nakano M, Wagatsuma K, Iga A, Nii H, Amano H, Toda M, et al. Impact of highly asymmetric stent expansion after sirolimus-eluting stent implantation on twelve-month clinical outcomes. J Cardiol. 2007;49(6):313–21.
Hwang CW, Wu D, Edelman ER. Physiological transport forces govern drug distribution for stent-based delivery. Circulation. 2001;104(5):600–5.
Mintz GS, Weissman NJ. Intravascular ultrasound in the drug-eluting stent era. J Am Coll Cardiol. 2006;48(3):421–9.
Morino Y, Honda Y, Okura H, Oshima A, Hayase M, Bonneau HN, et al. An optimal diagnostic threshold for minimal stent area to predict target lesion revascularization following stent implantation in native coronary lesions. Am J Cardiol. 2001;88(3):301–3.
Doi H, Maehara A, Mintz GS, Yu A, Wang H, Mandinov L, et al. Impact of post-intervention minimal stent area on 9-month follow-up patency of paclitaxel-eluting stents: an integrated intravascular ultrasound analysis from the TAXUS IV, V, and VI and TAXUS ATLAS workhorse, long lesion, and direct stent trials. JACC Cardiovasc Interv. 2009;2(12):1269–75.
Sonoda S, Morino Y, Ako J, Terashima M, Hassan AH, Bonneau HN, et al. Impact of final stent dimensions on long-term results following sirolimus-eluting stent implantation: serial intravascular ultrasound analysis from the sirius trial. J Am Coll Cardiol. 2004;43(11):1959–63.
Hong MK, Mintz GS, Lee CW, Park DW, Choi BR, Park KH, et al. Intravascular ultrasound predictors of angiographic restenosis after sirolimus-eluting stent implantation. Eur Heart J. 2006;27(11):1305–10.
Song HG, Kang SJ, Ahn JM, Kim WJ, Lee JY, Park DW, et al. Intravascular ultrasound assessment of optimal stent area to prevent in-stent restenosis after zotarolimus-, everolimus-, and sirolimus-eluting stent implantation. Catheter Cardiovasc Interv. 2014;83(6):873–8.
Kang SJ, Ahn JM, Song H, Kim WJ, Lee JY, Park DW, et al. Comprehensive intravascular ultrasound assessment of stent area and its impact on restenosis and adverse cardiac events in 403 patients with unprotected left main disease. Circ Cardiovasc Interv. 2011;4(6):562–9.
Fitzgerald PJ, Oshima A, Hayase M, Metz JA, Bailey SR, Baim DS, et al. Final results of the can routine ultrasound influence stent expansion (CRUISE) study. Circulation. 2000;102(5):523–30.
Chieffo A, Latib A, Caussin C, Presbitero P, Galli S, Menozzi A, et al. A prospective, randomized trial of intravascular-ultrasound guided compared to angiography guided stent implantation in complex coronary lesions: the AVIO trial. Am Heart J. 2013;165(1):65–72.
Fujii K, Carlier SG, Mintz GS, Yang YM, Moussa I, Weisz G, et al. Stent underexpansion and residual reference segment stenosis are related to stent thrombosis after sirolimus-eluting stent implantation: an intravascular ultrasound study. J Am Coll Cardiol. 2005;45(7):995–8.
Okabe T, Mintz GS, Buch AN, Roy P, Hong YJ, Smith KA, et al. Intravascular ultrasound parameters associated with stent thrombosis after drug-eluting stent deployment. Am J Cardiol. 2007;100(4):615–20.
Liu X, Doi H, Maehara A, Mintz GS, Costa Jde R Jr, Sano K, et al. A volumetric intravascular ultrasound comparison of early drug-eluting stent thrombosis versus restenosis. JACC Cardiovasc Interv. 2009;2(5):428–34.
Witzenbichler B, Maehara A, Weisz G, Neumann FJ, Rinaldi MJ, Metzger DC, et al. Relationship between intravascular ultrasound guidance and clinical outcomes after drug-eluting stents: the assessment of dual antiplatelet therapy with drug-eluting stents (ADAPT-DES) study. Circulation. 2014;129(4):463–70.
Liu X, Tsujita K, Maehara A, Mintz GS, Weisz G, Dangas GD, et al. Intravascular ultrasound assessment of the incidence and predictors of edge dissections after drug-eluting stent implantation. JACC Cardiovasc Interv. 2009;2(10):997–1004.
Hong MK, Park SW, Lee NH, Nah DY, Lee CW, Kang DH, et al. Long-term outcomes of minor dissection at the edge of stents detected with intravascular ultrasound. Am J Cardiol. 2000;86(7):791–5. A9
Sheris SJ, Canos MR, Weissman NJ. Natural history of intravascular ultrasound-detected edge dissections from coronary stent deployment. Am Heart J. 2000;139(1 Pt 1):59–63.
Choi SY, Witzenbichler B, Maehara A, Lansky AJ, Guagliumi G, Brodie B, et al. Intravascular ultrasound findings of early stent thrombosis after primary percutaneous intervention in acute myocardial infarction: a harmonizing outcomes with revascularization and stents in acute myocardial infarction (HORIZONS-AMI) substudy. Circ Cardiovasc Interv. 2011;4(3):239–47.
Steinberg DH, Mintz GS, Mandinov L, Yu A, Ellis SG, Grube E, et al. Long-term impact of routinely detected early and late incomplete stent apposition: an integrated intravascular ultrasound analysis of the TAXUS IV, V, and VI and TAXUS ATLAS workhorse, long lesion, and direct stent studies. JACC Cardiovasc Interv. 2010;3(5):486–94.
Kimura M, Mintz GS, Carlier S, Takebayashi H, Fujii K, Sano K, et al. Outcome after acute incomplete sirolimus-eluting stent apposition as assessed by serial intravascular ultrasound. Am J Cardiol. 2006;98(4):436–42.
Sohn J, Hur SH, Kim IC, Cho YK, Park HS, Yoon HJ, et al. A comparison of tissue prolapse with optical coherence tomography and intravascular ultrasound after drug-eluting stent implantation. Int J Cardiovasc Imaging. 2015;31(1):21–9.
Hong YJ, Jeong MH, Ahn Y, Sim DS, Chung JW, Cho JS, et al. Plaque prolapse after stent implantation in patients with acute myocardial infarction: an intravascular ultrasound analysis. JACC Cardiovasc Imaging. 2008;1(4):489–97.
Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, et al. American College of Cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (IVUS). A report of the American College of Cardiology Task Force on clinical expert consensus documents. J Am Coll Cardiol. 2001;37(5):1478–92.
Qiu F, Mintz GS, Witzenbichler B, Metzger DC, Rinaldi MJ, Duffy PL, et al. Prevalence and clinical impact of tissue protrusion after stent implantation: an ADAPT-DES intravascular ultrasound substudy. JACC Cardiovasc Interv. 2016;9(14):1499–507.
Hong MK, Park SW, Lee CW, Kang DH, Song JK, Kim JJ, et al. Long-term outcomes of minor plaque prolapsed within stents documented with intravascular ultrasound. Catheter Cardiovasc Interv. 2000;51(1):22–6.
Kim SW, Mintz GS, Ohlmann P, Hassani SE, Fernandez S, Lu L, et al. Frequency and severity of plaque prolapse within Cypher and Taxus stents as determined by sequential intravascular ultrasound analysis. Am J Cardiol. 2006;98(9):1206–11.
Maehara A, Mintz GS, Lansky AJ, Witzenbichler B, Guagliumi G, Brodie B, et al. Volumetric intravascular ultrasound analysis of paclitaxel-eluting and bare metal stents in acute myocardial infarction: the harmonizing outcomes with revascularization and stents in acute myocardial infarction intravascular ultrasound substudy. Circulation. 2009;120(19):1875–82.
Shimohama T, Ako J, Yamasaki M, Otake H, Tsujino I, Hasegawa T, et al. SPIRIT III JAPAN versus SPIRIT III USA: a comparative intravascular ultrasound analysis of the everolimus-eluting stent. Am J Cardiol. 2010;106(1):13–7.
Hong YJ, Jeong MH, Choi YH, Song JA, Kim DH, Lee KH, et al. Impact of tissue prolapse after stent implantation on short- and long-term clinical outcomes in patients with acute myocardial infarction: an intravascular ultrasound analysis. Int J Cardiol. 2013;166(3):646–51.
Jin QH, Chen YD, Jing J, Tian F, Guo J, Liu CF, et al. Incidence, predictors, and clinical impact of tissue prolapse after coronary intervention: an intravascular optical coherence tomography study. Cardiology. 2011;119(4):197–203.
Weissman NJ, Palacios IF, Nidorf SM, Dinsmore RE, Weyman AE. Three-dimensional intravascular ultrasound assessment of plaque volume after successful atherectomy. Am Heart J. 1995;130(3 Pt 1):413–9.
Mintz GS, Painter JA, Pichard AD, Kent KM, Satler LF, Popma JJ, et al. Atherosclerosis in angiographically “normal” coronary artery reference segments: an intravascular ultrasound study with clinical correlations. J Am Coll Cardiol. 1995;25(7):1479–85.
Morino Y, Tamiya S, Masuda N, Kawamura Y, Nagaoka M, Matsukage T, et al. Intravascular ultrasound criteria for determination of optimal longitudinal positioning of sirolimus-eluting stents. Circ J. 2010;74(8):1609–16.
Kang SJ, Cho YR, Park GM, Ahn JM, Kim WJ, Lee JY, et al. Intravascular ultrasound predictors for edge restenosis after newer generation drug-eluting stent implantation. Am J Cardiol. 2013;111(10):1408–14.
Takahashi M, Miyazaki S, Myojo M, Sawaki D, Iwata H, Kiyosue A, et al. Impact of the distance from the stent edge to the residual plaque on edge restenosis following everolimus-eluting stent implantation. PLoS One. 2015;10(3):e0121079.
Kubo T, Maehara A, Mintz GS, Garcia-Garcia HM, Serruys PW, Suzuki T, et al. Analysis of the long-term effects of drug-eluting stents on coronary arterial wall morphology as assessed by virtual histology intravascular ultrasound. Am Heart J. 2010;159(2):271–7.
Kitabata H, Loh JP, Pendyala LK, Omar A, Ota H, Minha S, et al. Intra-stent tissue evaluation within bare metal and drug-eluting stents > 3 years since implantation in patients with mild to moderate neointimal proliferation using optical coherence tomography and virtual histology intravascular ultrasound. Cardiovasc Revasc Med. 2014;15(3):149–55.
Andreou I, Takahashi S, Tsuda M, Shishido K, Antoniadis AP, Papafaklis MI, et al. Atherosclerotic plaque behind the stent changes after bare-metal and drug-eluting stent implantation in humans: implications for late stent failure? Atherosclerosis. 2016;252:9–14.
Kim IC, Yoon HJ, Shin ES, Kim MS, Park J, Cho YK, et al. Usefulness of frequency domain optical coherence tomography compared with intravascular ultrasound as a guidance for percutaneous coronary intervention. J Interv Cardiol. 2016;29(2):216–24.
Maehara A, Ben-Yehuda O, Ali Z, Wijns W, Bezerra HG, Shite J, et al. Comparison of stent expansion guided by optical coherence tomography versus intravascular ultrasound: the ILUMIEN II study (observational study of optical coherence tomography [OCT] in patients undergoing fractional flow reserve [FFR] and percutaneous coronary intervention). JACC Cardiovasc Interv. 2015;8(13):1704–14.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Cho, YK., Hur, SH. (2018). IVUS: Post-Evaluation After Stenting. In: Hong, MK. (eds) Coronary Imaging and Physiology. Springer, Singapore. https://doi.org/10.1007/978-981-10-2787-1_7
Download citation
DOI: https://doi.org/10.1007/978-981-10-2787-1_7
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-2786-4
Online ISBN: 978-981-10-2787-1
eBook Packages: MedicineMedicine (R0)