Abstract
Qualitative assessment was performed according to criteria of the American College of Cardiology clinical expert consensus document on IVUS and the Study Group on Intracoronary Imaging of the Working Group of Coronary Circulation and of the Subgroup on IVUS of the Working Group of Echocardiography of the European Society of Cardiology [1, 2].
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Qualitative assessment was performed according to criteria of the American College of Cardiology clinical expert consensus document on IVUS and the Study Group on Intracoronary Imaging of the Working Group of Coronary Circulation and of the Subgroup on IVUS of the Working Group of Echocardiography of the European Society of Cardiology [1, 2].
1 Plaque Morphology
IVUS cannot be used to detect and quantify specific histologic contents. The threshold between normal and abnormal is the subject of some debate, but more than 0.3 mm of intimal thickening is probably abnormal and can be used to distinguish from atherosclerosis. The maximal thickness of the intima-media complex or, more appropriately, the percentage of the total vessel area occupied by plaque is the most common quantitative indices used to define the severity of atherosclerotic involvement. Atherosclerotic lesions may be present in segments which are angiographically normal because compensatory total vessel enlargement in the early phases of atherosclerosis tends to keep the lumen constant. Lumen reduction does not occur, according to these pathology studies, until the plaque occupies more than 40% of the total cross-sectional vessel area. However, atherosclerotic lesions occupying less than 20 and 40% of the total vessel area can still be considered as lesions with a minimal and moderate atherosclerotic burden, respectively (Table 4.1) [1].
Atherosclerotic lesions are heterogeneous and include varying amounts of calcium, dense fibrous tissue, lipid, smooth muscle cells, thrombus, etc. By IVUS, imaging can grossly separate lesions into subtypes according to echodensity and the presence or absence of shadowing and reverberations (Table 4.2) [3].
1.1 Soft (Echolucent ) Plaque
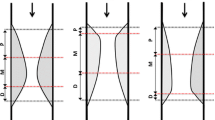
The term “soft” refers not to the plaque’s structural characteristics but rather to the acoustic signal that arises from low echogenicity. Soft plaque is less bright compared with reference adventitia. Soft plaque contains varying amounts of fibrous and fatty tissue. Reduced echogenicity may also result from a necrotic zone within the plaque, an intramural hemorrhage, or a thrombus (Fig. 4.1a).
Plaque morphology. (a) Soft (echolucent) plaque. Soft plaque is less bright compared with reference adventitia. Soft plaque contains varying amounts of fibrous and fatty tissue. (b) Fibrous plaque has an intermediate echogenicity between soft (echolucent) atheromas and highly echogenic calcific plaques. Fibrous plaque is as bright as or brighter than the adventitia without shadowing. (c, d) Calcified plaque is echodense (hyperechoic) plaque (brighter than the reference adventitia) that shadows using IVUS calcium can be localized and characterized as superficial [closer to tissue-lumen interface (c)] and deep [closer to the media-adventitia junction (d)]. (e) When there is no dominant plaque composition, the plaque was considered “mixed.” Mixed plaque is also called as “fibrocalcific,” “fibrofatty” plaque
1.2 Fibrous Plaque
Fibrous plaque has an intermediate echogenicity between soft (echolucent) atheromas and highly echogenic calcific plaques. Fibrous plaque represents the majority of atherosclerotic lesion. Fibrous plaque is as bright as or brighter than the adventitia without shadowing. Very dense fibrous plaques may produce sufficient attenuation to be misclassified as calcification with acoustic shadowing. Both calcified and fibrotic plaques are hyperechoic (Fig. 4.1b).
1.3 Calcified Plaque
Calcium is a powerful reflector of ultrasound. Calcific deposits appear as bright echoes that obstruct the penetration of ultrasound, a phenomenon known as “acoustic shadowing .” In practice calcium is echodense (hyperechoic) plaque (brighter than the reference adventitia) that shadows using IVUS calcium can be localized and characterized as superficial (closer to tissue-lumen interface) and deep (closer to the media-adventitia junction) and quantified according to its arc and length. The arc of calcium can be measured (in degrees) by using an electronic protractor centered on the lumen. Because of beam-spread variability at given depths within the transmitted beam, this measurement is usually valid only to ±15°. Semiquantitative grading has also been described, which classifies calcium as absent or subtending 1, 2, 3, or 4 quadrants. The length of the calcific deposit can be measured using motorized transducer pullback (Fig. 4.1c, d).
1.4 Mixed Plaque
Plaques frequently contain more than one acoustical subtype. When there is no dominant plaque composition, the plaque was considered “mixed.” Mixed plaque is also called as “fibrocalcific ,” “fibrofatty ” plaque (Fig. 4.1e).
2 Vulnerable Plaque
No definitive IVUS features define a plaque as vulnerable. However, necropsy studies demonstrated that unstable coronary lesions are usually lipid rich with a thin fibrous cap. Accordingly, hypoechoic plaques without a well-formed fibrous cap are presumed to represent potentially vulnerable atherosclerotic lesions. The important mechanisms leading to the development of acute coronary syndrome (ACS) are rupture of a vulnerable plaque and subsequent thrombus formation. The majority of ACS events are the result of sudden luminal thrombosis, with 55–60% due to plaque rupture, 30–35% caused by plaque erosion, and a small portion resulting from a calcified nodule.
2.1 Plaque Rupture
Rupture of vulnerable plaque and/or endothelial erosions with subsequent thrombus formation are considered the main mechanisms implicated in the pathogenesis of ACS. Ruptured plaque contains a cavity that communicated with the lumen with an overlying residual fibrous cap fragment [4] (Figs. 4.2 and 4.5). Rupture sites separated by a length of artery containing smooth lumen contours without cavities are considered to represent different plaque ruptures (multiple plaque ruptures) (Fig. 4.3). Plaque rupture is closely related to obstructive thrombus formation, and the longitudinal morphology of plaque rupture also affects the coronary flow. The presence of thrombi may obscure IVUS detection of plaque rupture.
2.2 Thrombus
The identification of thrombus is one of the most difficult aspects of IVUS imaging [5, 6] (Figs. 4.4 and 4.5).
Clues to the presence of thrombus include the following [5, 6]:
-
1.
Sparkling or scintillating appearance
-
2.
Lobulated mass projecting into the lumen
-
3.
A distinct interface between the suspected thrombus and underlying plaque
-
4.
Identification of blood speckle within the thrombus indicating microchannels through the thrombus
-
5.
Mobility
Because of limited resolution of IVUS, the detection rate of thrombus by IVUS is not high. Injection of contrast or saline may disperse the stagnant flow, clear the lumen, and allow differentiation of stasis from thrombosis. However, none of these features is pathognomic for thrombus, and the diagnosis of thrombus by IVUS should always be considered presumptive.
2.3 Attenuated Plaque
Attenuated plaque is defined as hypoechoic plaque with deep ultrasound attenuation without calcification or very dense fibrous plaque [7] (Fig. 4.6). Wu et al. [8] reported that 78% of the AMI patients had attenuated plaques in HORIZONS-AMI trial. Lee et al. [9] reported that attenuated plaque was observed in 39.6% of STEMI and 17.6% of NSTEMI (p < 0.001), and the level of C-reactive protein (CRP) was higher; angiographic thrombus and initial Thrombolysis In Myocardial Infarction (TIMI) flow grade <2 were more common; IVUS lesion site plaque burden and remodeling index were significantly greater; lesion site luminal dimensions were significantly smaller; and thrombus, positive remodeling and plaque rupture were more common in AMI patients with attenuated plaque compared with those without attenuated plaque.
2.4 Calcified Nodule
Calcified nodule is an eruptive, dense, calcified mass often having an irregular surface appearance (Fig. 4.7). Lee et al. [10] reported the IVUS characteristics of calcified nodules, which include (1) a convex shape of the luminal surface, (2) a convex shape of the luminal side of calcium, (3) an irregular luminal surface, and (4) an irregular leading edge of calcium. Although calcified nodule is a marker for atherosclerosis, it is associated with fewer future cardiac events, suggesting quiescence rather than ongoing activity.
3 Angiographic Aneurysms
Maehara et al. [4] reported IVUS findings in 77 consecutive patients with an aneurysmal dilatation (defined as a lesion lumen diameter 25% larger than reference) in a native coronary artery diagnosed by angiography. IVUS true aneurysms were defined as having an intact vessel wall and a maximum lumen area 50% larger than proximal reference (Fig. 4.8). IVUS pseudoaneurysms had a loss of vessel wall integrity and damage to adventitia or perivascular tissue. Complex plaques were lesions with ruptured plaque or spontaneous or unhealed dissection. Twenty-one lesions (27%) were classified as true aneurysms, 3 (4%) were classified as pseudoaneurysms, 12 (16%) were complex plaques, and the other 41 (53%) were normal arterial segments adjacent to ≥1 stenosis. Therefore, only one third of angiographically diagnosed aneurysms had the IVUS appearance of a true or pseudoaneurysm. Instead, most angiographically diagnosed aneurysms had the morphology of complex plaques or normal segments with adjacent stenoses.
True aneurysm . True aneurysm in 30-year-old female with acute myocardial infarction. (a) Computed tomography showed true huge aneurysm (arrow) in middle right coronary artery. (b) Intravascular ultrasound true aneurysm which was defined as having an intact vessel wall and a maximum lumen area 50% larger than proximal reference
4 Angiographically Ambiguous Lesions
Angiographically ambiguous lesions may include (1) intermediate lesions of uncertain stenotic severity, (2) aneurysmal lesions, (3) ostial stenoses, (4) disease at branching sites, (5) tortuous vessels, (6) left main stem lesions, (7) sites with focal spasm, (8) sites with plaque rupture, (9) dissection after coronary angioplasty, (10) intraluminal filling defects, (11) angiographically hazy lesions, and (12) lesions with local flow disturbances. IVUS is frequently employed to examine lesions with the above characteristics, in some cases providing additional evidence useful in determining whether the stenosis is clinically significant (i.e., difficult to assess left main or borderline stenosis with continued symptoms). However, it must be emphasized that IVUS does not provide physiologic information per se.
5 Myocardial Bridge
The muscle overlying the intramyocardial segment of an epicardial coronary artery is termed a myocardial bridge, and the artery coursing within the myocardium is called a tunneled artery. It is characterized by systolic compression of the tunneled segment. The “half-moon phenomenon ” is a characteristic IVUS finding. It seems specific for the existence of myocardial bridging inasmuch as it is only found in tunneled segments but not in proximal or distal segments or in other arteries. In the presence of a half-moon phenomenon on IVUS, milking can be provoked by intracoronary provocation tests, even if the bridge was angiographically undetectable. IVUS pullback studies supported the absence of atherosclerosis within tunneled segments, although ≈90% of patients showed plaque formation proximal to the bridge. When deep tunneled segments approach the right ventricular subendocardium, the trabeculated right chamber myocardium and the right ventricular cavity may be visible on IVUS.
6 Spontaneous Dissection
Spontaneous coronary artery dissection is a rare cause of acute coronary syndrome (ACS) and sudden death. IVUS showed an entry intimal tear with an intimal flap dividing the true lumen from the false one at the dissection site. Usually, the false lumen has a larger area than the true lumen (Fig. 4.9).
7 Chronic Total Occlusion
Fujii et al. [11] published an excellent paper describing IVUS findings in 83 CTOs interrogated with IVUS immediately after antegrade wire crossing and small caliber balloon inflation. Procedures were performed in four Japanese centers with procedures performed between 2003 and 2005. This study found nearly all lesions contained calcium (96%) although in many, (68%), this was mild. The authors were able to define the proximal cap according to angiographic landmarks and observing abrupt morphology change on IVUS. The proximal cap was a location where calcium was concentrated, particularly in blunt stump CTOs. A calcified arc was demonstrated in the wall opposite the side branch in 74% of this morphology. A smaller proportion had calcification found perpendicular to the side-branch origin, and a small number were found on the ipsilateral aspect as the side branch.
Suzuki et al. [12] described IVUS findings in 79 CTO lesions and found moderately strong correlations between lesion age and indices of calcification assessed by IVUS. Some very recent CTOs were heavily calcified suggesting that the CTO had arisen in a vessel with well-entrenched atheroma.
8 Summary
IVUS is reliable and established imaging modality to evaluate coronary lesion with high sensitivity and specificity. IVUS is very helpful to define plaque morphology according to echodensity and the presence or absence of shadowing and reverberations and to detect vulnerable plaque and aneurysm and to define angiographically ambiguous lesions and to detect myocardial bridge, spontaneous dissection, and chronic total occlusion.
References
Di Mario C, Görge G, Peters R, Kearney P, Pinto F, Hausmann D, et al. Clinical application and image interpretation in intracoronary ultrasound. Study Group on Intracoronary Imaging of the Working Group of Coronary Circulation and of the Subgroup on Intravascular Ultrasound of the Working Group of Echocardiography of the European Society of Cardiology. Eur Heart J. 1998;19:207–29.
Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, et al. American College of Cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (IVUS): a report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001;37:1478–92.
Tobis JM, Mallery J, Mahon D, Lehmann K, Zalesky P, Griffith J, et al. Intravascular ultrasound imaging of human coronary arteries in vivo. Analysis of tissue characterizations with comparison to in vitro histological specimems. Circulation. 1991;83:913–26.
Maehara A, Mintz GS, Bui AB, Walter OR, Castagna MT, Canos D, et al. Morphologic and angiographic features of coronary plaque rupture detected by intravascular ultrasound. J Am Coll Cardiol. 2002;40:904–10.
Chemarin-Alibelli MJ, Pieraggi MT, Elbaz M, Carrié D, Fourcade J, Puel J, Tobis J. Identification of coronary thrombus after myocardial infarction by intracoronary ultrasound compared with histology of tissues sampled by atherectomy. Am J Cardiol. 1996;77:344–9.
Frimerman A, Miller HI, Hallman M, Laniado S, Keren G. Intravascular ultrasound characterization of thrombi of different composition. Am J Cardiol. 1994;73:1053–7.
Endo M, Hibi K, Shimizu T, Komura N, Kusama I, Otsuka F, et al. Impact of ultrasound attenuation and plaque rupture as detected by intravascular ultrasound on the incidence of no-reflow phenomenon after percutaneous coronary intervention in ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2010;3:540–9.
Wu X, Mintz GS, Xu K, Lansky AJ, Witzenbichler B, Guagliumi G, et al. The relationship between attenuated plaque identified by intravascular ultrasound and no-reflow after stenting in acute myocardial infarction: the HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trial. JACC Cardiovasc Interv. 2011;4:495–502.
Lee SY, Mintz GS, Kim SY, Hong YJ, Kim SW, Okabe T, et al. Attenuated plaque detected by intravascular ultrasound: clinical, angiographic, and morphologic features and post-percutaneous coronary intervention complications in patients with acute coronary syndromes. JACC Cardiovasc Interv. 2009;2:65–72.
Lee JB, Mintz GS, Lisauskas JB, Biro SG, Pu J, Sum ST, et al. Histopathologic validation of the intravascular ultrasound diagnosis of calcified coronary artery nodules. Am J Cardiol. 2011;108:1547–51.
Fujii K, Ochiai M, Mintz GS, Kan Y, Awano K, Masutani M, et al. Procedural implications of intravascular ultrasound morphologic features of chronic total coronary occlusions. Am J Cardiol. 2006;97:1455–62.
Suzuki T, Hosokawa H, Yokoya K, Kojima A, Kinoshita Y, Miyata S, et al. Time-dependent morphologic characteristics in angiographic chronic total coronary occlusions. Am J Cardiol. 2001;88:167–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Hong, Y.J. (2018). Qualitative Assessment of Native Lesion. In: Hong, MK. (eds) Coronary Imaging and Physiology. Springer, Singapore. https://doi.org/10.1007/978-981-10-2787-1_4
Download citation
DOI: https://doi.org/10.1007/978-981-10-2787-1_4
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-2786-4
Online ISBN: 978-981-10-2787-1
eBook Packages: MedicineMedicine (R0)