Abstract
Research in patients with cancer and comorbidity poses methodological challenges due to heterogeneous study populations, difficulties with recruitment and a variety of relevant outcome measures. This chapter discusses methodological choices regarding study design to ensure best fit with the research questions regarding cancer and comorbidity, the most appropriate study populations and potential strategies to recruit patients, the availability and fit of data sources, methods to measure comorbidity, and relevant outcomes and strategies for statistical analyses with a particular focus on the handling of longitudinal data.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
Similarly to other areas of research, choosing a study design should be primarily guided by the research question one aims to answer (e.g. to describe a problem or to reject a hypothesis) taking into account the pros and cons of the design (such as the influence of recall bias and selection bias).
-
Cancer patients with comorbidity form an older and very heterogeneous study population and their recruitment is a major challenge. Strategies to improve recruitment come at considerable costs, because they require a substantial increase in time and efforts.
-
There is no single comorbidity measure available that satisfies all needs. A measure should be selected taking into account the research question, the available data sources, and the context of the study (e.g. community setting, nursing home, hospital).
-
Statistical analyses of studies involving cancer patients with comorbidity should take into account the skewedness and non-normality of data, dependence between longitudinal clinical data and cancer related outcomes, competing causes of death and individual illness trajectories.
12.1 Introduction
Comorbidity of cancer—the co-occurrence of cancer with one or more diseases within one person—is a phenomenon with consequences for the patient, his or her family and friends, the health care system and society at large. Similarly, clinical research in this patient population is associated with complex methodological considerations and decisions.
In a primary care based study Deckx et al. [1] reported that only 22 % of newly diagnosed cancer patients did not have any co-occurring chronic disease; the vast majority were suffering from diabetes, lipid disorders, ischemic heart disease, myocardial infarction, and/or chronic obstructive pulmonary disease (COPD). In addition to comorbidities present pre cancer diagnosis, Deckx et al. also found that in the period following a cancer diagnosis other new chronic diseases develop, sometimes as a result of cancer and/or its treatment (e.g. thrombosis), but overall in a similar pattern to people from a similar age without a cancer diagnosis. Other studies report slightly higher occurrence of comorbidity in cancer patients [2, 3], or report an increased incidence of specific disease, for example deep venous thrombosis [1, 4]. The presence of co-occurring conditions in cancer patients increases patients’ complexity at many levels. Interactions between diseases and their treatments may attenuate benefits and increase harms of any kind of diagnostic or therapeutic intervention. Patients may be overwhelmed by treatment burden resulting from multiple disorders and prioritization is needed. Therefore, a single-disease perspective on cancer falls short when managing real world patients. Research in this patient population has to take into account these clinical necessities but major challenges arise from this approach. In the following paragraphs we will focus on challenges related to research in cancer and comorbidity and some strategies to address these challenges will be provided.
Below, we summarize the key considerations that inform research in this field.
-
1.
Comorbidity and multimorbidity are related but distinct concepts (see also Chap. 1). Comorbidity is the presence of other chronic diseases in addition to cancer; hence the index disease is cancer. Multimorbidity on the other hand does not focus on an index disease but looks at the co-occurrence of multiple diseases and conditions as a whole. Both concepts are helpful in research (and practice) and should not be used interchangeably. For example, life expectancy of patients with chronic heart failure is comparable to that of patients with colon, prostate and breast cancer [5, 6]. Depending on the research question the condition identified as the index disease may vary (heart failure with comorbid cancer or cancer with comorbid heart failure) or should not follow a pre-specified hierarchy at all. The choice of the appropriate concept—comorbidity or multimorbidity—provides a framework for the study and its further operationalization supports the selection of outcome measures and procedures to control for potential confounders.
Many research considerations for comorbidity and multimorbidity are similar, given the overlap between both concepts. However, because this chapter focuses on research challenges in patients with cancer and chronic diseases, we will predominantly use the term ‘comorbidity’. We will only use the term ‘multimorbidity’ if the studies that are being discussed clearly focus on multimorbidity.
-
2.
The choice of the appropriate study design is of crucial importance. Although, the randomized controlled trial (RCT) design is the experimental gold standard in intervention research, it is often not possible to test the effectiveness of interventions such as a drug treatment in varying patterns of multimorbidity in cancer patients. RCTs may be conducted for the most important cancer-comorbidity combinations and observational studies may generate further evidence whether an intervention has comparable or attenuated benefits in cancer patients with and without comorbidity. Further, observational study designs are helpful to estimate harm in patients with cancer and comorbidity, e.g. arising from drug-disease and drug-drug interactions.
-
3.
Older and more vulnerable patients will have to be included in the study population to take comorbidity into account. This population has been generally excluded from randomized controlled trials [7], and in many other aspects of cancer research [8, 9]. Although, more research in this population is needed, research including an older and sicker population raises important methodological and ethical challenges relating to recruitment, survival of the fittest, and hence requires special attention of researchers in this area.
-
4.
Research in comorbidity of cancer cannot be limited to studies collecting primary data, given the enormous research needs and complexity. Other available data sources collected for different purposes (e.g. claims data), data from registries or research practice networks come to play. However, the use of these data is frequently hampered by their variable validity and difficulties arising from combining different data sources. Combining available data sources with additionally collected primary data may be preferable, but might not always be feasible.
-
5.
Comorbidity operationalization and measurement is needed to describe the morbidity of the included population, to adjust for confounding, and to be applied as an outcome in itself. With more than 10,000 known diseases the number of potential combinations is vast. However, existing measures reflect some ongoing discussion about definitions resulting in a multiplicity of operationalizations and instruments. Also, some of these instruments have been developed and validated in certain populations and are applied in others. Their use may be further complicated by limitations of available data sources.
-
6.
The choice of appropriate outcome measures may be difficult and has to go beyond the classical “hard outcomes”, such as survival and hospitalization. In particular in older patients with cancer and comorbidity, quality of life often outweighs length of survival [10]. In patient-centered care, the ultimate outcome measure would include those preferred by the patients. However, goal attainment scaling instruments have been restricted to rehabilitation medicine and have been rarely applied in cancer until now [11, 12]. Appropriate (age-adapted) measures of health related quality of life and functionality—including all domains of social, cognitive, mental, and physical functioning—should be applied to provide evidence to support decisions for or against certain treatments adequately. The choice of outcomes may also be challenging in epidemiological studies where research on the relationship between cancer, comorbidity, and other potential determinants goes beyond mere correlation.
-
7.
Statistical analyses in cancer research in general are not trivial, as they should often include time-dependent analyses to take into consideration that neoplasms have their specific natural course and that treatment at times is highly toxic. Often, cancer status is unclear, disease may be progressive despite aggressive treatment, and patients may develop serious toxicity as a consequence of the treatment. This has led to the development of oncology-specific outcomes such as disease free survival, prediction of toxicity, and tolerance to treatment, which may not reflect the interaction with comorbidity. Interferences from comorbidity or multimorbidity enhance the complexity of the statistical models and may hamper the transparency of analyses as well as the interpretation of the results.
Box 1: Research challenges in studying the comorbidity of cancer
-
Study design
-
Study population
-
Data sources
-
Measures and operationalization of comorbidity
-
Outcomes
-
Statistical analyses of longitudinal data.
12.2 Study Design—Design to Fit the Question
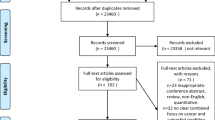
The choice of the appropriate study design is of crucial importance. The randomized controlled design is the gold standard when it comes to testing the effectiveness of an intervention. However, the possible combinations of cancer and different comorbid diseases are endless, which pushes us to explore other avenues. Generally, study designs can be subdivided in descriptive studies versus analytic studies, although there may be some overlap between both as well (see Fig. 12.1).
Study designs. Source [16]: adapted from http://www.cebm.net/study-designs/
Descriptive studies generally focus on describing the characteristics of a study population, i.e. the population of patients with cancer. The aim is to provide a picture of what is happening in a population, for example the prevalence and incidence of comorbidity in a population of cancer patients. This information is often gathered using cross-sectional observational studies (e.g. population surveys). Descriptive studies can also include qualitative studies. Qualitative studies generally aim to understand the experience of a certain problem. For example, a qualitative study design can be used to understand the impact of comorbidity on daily life in cancer patients or the impact of comorbidity on top of cancer [13]. They can also be used to understand the views of primary care physicians in the management of comorbidity in cancer patients, since primary care physicians are seen as experts in dealing with multimorbidity [14]. Other applications of a qualitative study designs are to generate hypotheses or to provide in-depth understanding of quantitative studies. For example, a qualitative study design can be used as part of a process evaluation of a new model of care that especially targets cancer patients with extra needs, such as other chronic health problems.
Analytic studies generally attempt to quantify a relationship between two or more factors. For example, analytic designs can be used to quantify the relation between comorbidity in cancer patients and different outcomes, such as treatment toxicity, disease-free survival, and overall survival. The best-known analytical study design is the randomized controlled trial, which is designed to test the effect of an intervention. In this respect, the effect of a new drug can be tested in the presence of comorbidity (e.g. compare a treatment group with and without comorbidity to standard care). These studies are often referred to as trials or experimental designs. Another type of analytic study design is the observational study. This includes cohort studies, and case control studies, and they are often used to evaluate the effect of an exposure on an outcome, for example, to investigate the effect of comorbidity (exposure) on cancer survival (outcome). However, there might be some overlap between descriptive and analytic study designs as well. Cross-sectional studies can be both descriptive and analytic. A population survey can be used to describe the prevalence of comorbidity in cancer patients (e.g. describe prevalence of comorbidity across different types of cancer and stage at diagnosis). However, it can also be used to analyze the relationship between two factors or groups (e.g. quantify the relation between presence or absence of comorbidity and cancer stage at diagnosis).
Depending on the research question one aims to answer, a descriptive or more analytic design might be more appropriate. Below we will discuss some examples of different study designs that were used to study cancer and comorbidity. This is not a comprehensive overview of study design. For such an overview we refer to one of the many epidemiological handbooks, like the one from Rothman et al. [15].
As a first example, we will discuss the cross-sectional study design, which can be both descriptive and analytic. Using a Medicare Health Outcomes Survey, Smith et al. [2] illustrated the prevalence of the most common comorbid conditions in cancer patients. The sample of cancer patients that participated had a mean age of 75 years and 48 % of them were female. For this sample, they showed that 54 % of cancer patients had hypertension, 17 % had diabetes, and 10 % has had a myocardial infarction. These findings are descriptive. However, because this survey also included patients without cancer, Smith et al. were also able to analyze the prevalence of comorbid conditions in patients with and without cancer. They found that the prevalence of comorbid conditions was higher in cancer patients compared to patients without cancer (e.g. the prevalence of diabetes was 17 % in cancer patients compared to 16 % in patients without cancer, p < 0.0001) [2]. These findings are analytic. Unfortunately, a cross-sectional survey study-design has some limitations as well; it is based on self-reports, which makes it susceptible to recall-bias and its cross-sectional nature only enables one to show an association between two factors, not a direction of effect or causality. For example, Smith et al. showed the prevalence of comorbid conditions, however, they were not able to determine whether cancer patients are more likely to develop comorbid conditions after their diagnosis and treatment.
A cohort study on the other hand can provide an answer to this question. Cohort studies follow a group of persons forward in time from an exposure (e.g. diagnosis of cancer) to one or more outcomes (e.g. new chronic conditions). Deckx et al. [1] used a cohort study to assess the incidence of new comorbid conditions in cancer patients compared to patients without cancer, using data from a large primary care based cohort study. This cohort study includes approximately 135,000 people, participants are registered with a general practitioner (GP), and all their relevant health problems are recorded continuously in time. All patients with cancer were selected from this cohort and the incidence of new comorbid conditions—after the diagnosis of cancer—was assessed and compared to the patients without a diagnosis of cancer. They found that the incidence of new comorbid conditions was largely similar for patients with and without cancer. Although a cohort study is the best design to study the incidence and natural history of a problem, the disadvantages of this design are that it is very time-consuming and labor-intensive, it relies strongly on long-term and substantial commitments of the participants, and it is not feasible in rare disorders.
Case-control studies are much more efficient from this perspective. In case-control studies, patients with and without a disease (e.g. cancer) are recruited and information on the exposure is then gathered retrospectively (e.g. evaluate exposure to cigarettes in patients with and without lung cancer). For example, Hang et al. [17] conducted a large case-control study to investigate the effects of lifestyle factors and comorbidities on the risk for colorectal cancer. They recruited 1144 patients who were diagnosed with colorectal cancer and 60,549 community controls. Both groups were interviewed using structured questionnaires that included questions on comorbidity history and lifestyle factors. They found that four comorbid conditions (diabetes, hyperlipidemia, inflammatory bowel disease and polyps) and some lifestyle factors (e.g. reduced physical activity and eating red meat) were associated with an increased risk for colorectal cancer. Nevertheless, case-control studies have some limitations as well. For example, case-controls studies are prone to recall bias; patients with the disease are more (or less) likely to remember exposure compared to people without the disease. Also the selection of an appropriate control group might be difficult (selection bias); it is important that patients and controls are similar in all factors that could influence the relationship under study (e.g. selection of controls could have been inappropriate if they were generally younger and therefore had less or less severe comorbid conditions).
The latter is not an issue in a randomized controlled trial design. The random allocation of participants to the treatment or the placebo group should ensure that the two groups are balanced in terms of confounding factors (e.g. age and comorbid conditions are balanced across both groups). Klepin et al. [18] reported the results of a randomized controlled trial that focused on the influence of age and comorbidity. In the parent trial, women aged 65 years or older with stages I–III breast cancer were randomly allocated to standard adjuvant chemotherapy or capecitabine [19]. They found that women who were treated with standard chemotherapy had a lower risk of breast cancer recurrence and death than those treated with capecitabine. In the companion study it was explored if women with a greater number of comorbid conditions would experience more treatment toxicity during adjuvant chemotherapy, if they would have a shorter time to relapse, and reduced overall survival. It was shown that self-reported comorbidity was not associated with toxicity, or breast cancer relapse, regardless of treatment (standard/capecitabine). However, having four or more comorbid conditions was associated with shorter overall survival. Although this study was based on a randomized controlled trial design—which is considered to be the gold standard for clinical trials—even this study was not without limitations. For example, the authors acknowledged that the analyses were restricted to a selected population of women healthy enough to receive chemotherapy, which might contribute to a lower comorbidity burden at baseline. In unselected real world patients, some adjustments of chemotherapy regimen may be necessary to reduce toxicity. Here, an additional observational cohort study might provide insight in the treatment outcomes of women who are not fit enough to receive standard regimen.
In conclusion, no study design is perfect. Choosing a study design should be primarily guided by the research question one aims to answer, taking into account the pros and cons of the design.
12.3 Study Population—Tensions Between Homogeneity, Reproducibility and Recruitment
In studies evaluating an intervention, like randomized controlled trials, homogeneous study populations are often recruited, to enable more specific effect estimates and narrower confidence intervals. Historically, older patients have been underrepresented in clinical trials, as have been patients with (severe) comorbidity [7]. This is also true for trials evaluating cancer treatments [8, 9]. This approach, however, comes at the cost of a decreased possibility to generalize study results. As a result, there is a serious lack of information on both the efficacy and the effectiveness of cancer treatment in patients with comorbidity, as well as a lack of information regarding safety and adverse events of cancer treatment in this population. But also, other questions regarding burden of treatment, quality of survival, and acceptability of treatment in a vulnerable (older) population of cancer patients with comorbidity remain largely unanswered.
Trying to find answers to important research questions relating to the effectiveness of treatment, safety, and acceptability of treatment in more heterogeneous study populations is often jeopardized by the difficult recruitment of cancer patients with comorbidity. This has been identified as a major challenge in research with older cancer patients [20, 21]. Low inclusion rates have been attributed to limited physical and cognitive capacity of the patient, and insufficient awareness of the study by the treating physicians [21]. From the patients’ perspective, barriers to participation included feeling too anxious (40 %) or being not interested (25 %) [22]. In this respect, it is important to carefully plan the moment of recruitment, e.g. after the treatment plan is explained to the patient, when the first wave of anxiety has decreased. A number of other strategies have been recommended to help overcome age- and health-related barriers to participation [21–23]:
-
Providing information about the study in a written form, but always ensuring it is explained face-to-face as well
-
Including family members in the recruitment process; often they are concerned about the burden it will place on the patient
-
Informing and regularly reminding the entire hospital staff of the study
-
Researchers being present in the clinics as much as possible to reinforce the reminders when the physicians see their patients
-
Performing data collection face-to-face while the patient is hospitalized, during ambulatory care, or at home visits, ensuring no extra burden for the patients. If this is not feasible, ensure at least one face-to-face contact at the start of the study, so that the patient knows who is going to call them
-
Keeping the length of the interview acceptable (less than one hour)
-
Being flexible to reschedule interviews if the patient is not feeling well or if hospital appointments are postponed
-
Using the same interviewer as much as possible, also for follow-up data collection
-
Only providing a self-administered questionnaire if it is agreed with the patient that this is feasible.
Unfortunately, these strategies require considerable time and effort, which makes these types of studies even more expensive [21, 22].
12.4 Data Sources—Overcoming Silos
Although older people with comorbid conditions have been underrepresented in clinical cancer trials [8, 9], it is virtually impossible to do all cancer trials again given the heterogeneity of the population. Countless combinations of age cohorts with different combinations of comorbidity types and stages of cancer are possible. Therefore, the necessity arises to broaden the scope of research in comorbidity of cancer beyond studies collecting mere primary data.
Other available data sources collected for different purposes come to play as well. Information on diseases and other relevant measures can be collected using different methods and different resources, each with their own strengths and limitations.
-
1.
Patient self-reported. Methods to collect data directly from the patients are written or digital questionnaires, telephone or face-to-face interviews, using either closed or open-ended questions. This method of data collection is gathering information directly from the person under study, but the validity of information has to be taken into account. For clearly defined and more serious diseases, such as diabetes, myocardial infarction and also cancer, patient self-reports have high levels of agreement compared to physician-registered morbidity. However, for other diseases like rheumatoid arthritis, migraine, and chronic back problems, the agreement between patients and primary care physicians is limited [24]. This general problem may arise from the distinct representation of medical problems in patients and health professionals: physicians’ representation is mostly (data) driven, by biomedical knowledge underlying the disease (disease model), whereas patients’ representation is frequently based on narrative structures, the social and moral meaning attached to the dysfunction of the body which involves the disruption of the patient’s normal life (illness model) [25, 26]. Patients with cancer might overestimate or underestimate the presence of other diseases unconsciously, because of presumed associations between cancer and e.g. cardiovascular disease or certain life styles. Also, mental illness might cause patients to be more prone to recall or reporter bias than other somatic disease, due to cognitive or emotional dysfunction, experiences of taboo, shame or social desirability. Also, the accuracy of recall may be an important source of bias, depending on the time frame and subject and should be considered in the selection of data sources, the choice of measurement and the interpretation of results.
-
2.
Clinician reported, usually written/digital. Clinical reports are likely to be accurate about treatments and issues related to the condition of interest, but clinicians may not be aware of, or may under-report, other health issues [27].
-
3.
Electronic medical records are valuable data sources and are often considered ‘gold standard’. A major advantage of medical records is that they are a good representation of daily practice, assuming that physicians keep written or digital track of their patient population. In case of longitudinal studies covering a large time-window, retrospective information going back into the 20th century might be less comprehensive, but increasingly electronic patient records are the norm and minimal data sets are increasingly required, also for refunding purposes. An important pitfall of medical records is that the quality of documentation may vary and that the information included is often strongly related to the reason for encounter. Further, the primary consideration of medical specialists is naturally related to the subjects of their discipline, whereas documentation of information on conditions that are out of scope might be lacking. In some countries, such as the UK and the Netherlands, where the general practitioner acts as a gate keeper in health care, the use of medical records from general practice might therefore provide the most comprehensive medical information.
-
4.
Research practice networks are increasingly common. In various Western countries, like the Netherlands, Belgium and the UK, where the vast majority of individuals are registered with a single general practice, registration networks continuously collect data about routine consultations such as the General Practice Research Database in UK. Data are extracted directly from the clinical record utilizing a combination of clinical codes and free text comments. Their strengths include large population sizes, longitudinal follow up, and cost avoiding the need to contact patients directly [28–31]. In some registration networks, hybrid data from medical records and annual questionnaires for research purposes are collected such as the Study into Medical Information and Lifestyle (SMILE) in Eindhoven attached to the Maastricht University [32].
-
5.
Cancer registries or extensive cohorts of patients diagnosed with cancer are available and often contain sufficient medical information to analyze the influence of comorbidity on cancer related outcomes [33, 34] and can be linked to hospitalization data [35] but facilities may vary widely between countries. Some cohorts specifically focus on other domains, such as sociodemographic and psychosocial evolutions [36]. Taking into account privacy legislation, possibilities to link databases are increasingly common [37] sometimes even encompassing several databases [38].
-
6.
Administrative databases, such as claims data from health care insurers usually cover large numbers of patients and contain very structured information. These databases are convenient for surveillance of survival and mortality [39], morbidity [40], recurrence rates [41], and treatment effects [42]. The main limitation of this type of databases is the lack of clinical, lifestyle and demographic data [42]. Also, it is recognized that routinely collected databases may underestimate the prevalence and incidence of comorbidity, because databases were not originally designed for research purposes and may suffer from incomplete coding, especially in the earlier years [37]. Additionally, information collected for reimbursement purposes may be distorted—in particular, where financial incentives may have unintended consequences such as fraudulence coding [43].
Given the enormous resources and costs which are spent to collect primary data and given the pitfalls in data documented for other than research purposes, activities to provide and share data sets of completed studies for secondary analyses should be a core research consideration in patients with cancer and chronic comorbidity [44]. Patients with comorbidity are frequently (but not always) excluded in cancer trials and under-reporting of comorbidity may pretend a distorted picture that no evidence is available for this patient group. However, individual patient data meta-analyses in large data sets may identify subgroups of sufficient sample size to answer questions of comparative effectiveness and harms in patients with cancer and high prevalent comorbidity, such as cardiovascular disease. Similarly, data exchange between cancer registries or administrative data bases may support research in patients with cancer and comorbidity of low prevalence in future but safety concerns of patients and stakeholders as well as technical challenges of the connection of data bases differing in structure have to be overcome [45–47].
12.5 Measures of Comorbidity—From Simple Count to Cancer Specific Index
There are many comorbidity measures available, developed for different purposes, each with their own flaws and benefits. Some list diseases separately, with or without weighing of the diseases, some present aggregate measures, and in the case of comorbidity of cancer many studies describe specific combinations (i.e. cancer plus specific chronic condition). Conditions taken into account in an index may be psychological or somatic, complaints or diagnoses, chronic or acute, including or excluding social aspects and functional status. Finally, there are proxy based indices, e.g. counting the number of chronic medications [48] or scoring of selected patterns of prescriptions such as the Chronic Disease Score (CDS) [49].
In many observational studies comorbidity can act as a serious confounder. When a large number of comorbid diseases may be relevant to take into account, controlling for individual comorbid diseases may not be practical for methodological reasons, including loss of power. Furthermore, it may be more appropriate to control for the overall burden of comorbidity, rather than the individual effect of each comorbid disease. In their systematic review Yurkovich et al. [42] showed that for specific applications (e.g. with cancer patients) often new indices were developed or existing indices were adapted for the use in specific patient groups.
Many different comorbidity indices have been validated for various outcomes, most often mortality or hospitalization, but only few have been tested in a population of (older) cancer patients. Lee et al. [34] evaluated the impact on management and prediction of outcomes in patients with oral squamous cell carcinoma (OSCC) using ECIS and CCIS. Mayr et al. [50] evaluated five comorbidity indices assessed preoperatively in patients with bladder cancer, scheduled to have a radical cystectomy. All five appeared to be predictive for cancer-independent mortality, but none of them predicted cancer specific mortality, when adjusting for other relevant characteristics (age, sex and cancer severity indicators).
Fröhner and Wirth [51] described the impact of comorbidity in patients with early prostate cancer and suggested a classification of relevant comorbidity for this patient group; comorbid diseases have prognostic and clinical relevance, i.e. be associated with an increased mortality risk. Furthermore, in order to be clinically relevant, these diseases should have a considerable impact on survival time and should occur rather frequently. Also Briganti et al. [52] studied the survival of patients with prostate cancer, taking into account type and severity of comorbidity.
Furthermore, definitions of comorbidity should both inform and reflect clinical practice. This objective may be difficult to achieve when epidemiology oriented definitions are less inclusive and aim at a limited set of clear-cut criteria. For ‘diseases’ with varying latency or a chronic course, developing a definition depends on decisions regarding the phase to monitor—asymptomatic, early disease, late disease—and the circumscription of the spectrum of morbidity [15]. Each of these definitions as Rothman et al. argue, would measure different segments of the population, each would have strengths and limitations, and each would require a unique approach, data source and monitoring system.
Moreover, it is important to distinguish comorbidity from complications of cancer. When complications are not considered separately, the total comorbidity burden will be overestimated [53]. This distinction is, however, not always evident: cancer and its treatments are well-recognized risk factors for venous thromboembolism (VTE), but not all VTEs in cancer patients are due to cancer treatment [54]. This underlines the relevance to distinguish between general susceptibility and disease related susceptibility/complications when analyzing comorbidity [55].
There are a number of studies to describe the co-occurrence of diseases known to share risk factors. Gottlieb et al. describe the prevalence of pulmonary comorbidity among patients with lung and head and neck cancer [56]. Knowing comorbidity that is pathophysiologically related to the index disease (such as COPD and lung cancer) and optimizing the treatment of comorbid diseases could influence interventions tested.
Below, some examples of indices and other measurements of comorbidity are specified and commented:
The Charlson comorbidity index (CCI) [57] is probably the most commonly used and cited comorbidity index. The National Cancer Institute comorbidity index was developed as an adaptation of the CCI [58]. However, the validation of the CCI was based on a relatively small cohort of general medical patients and was executed nearly 30 years ago. The CCI includes conditions that may not have an impact on survival among patients with cancer nowadays, because of substantial improvements in management (e.g. peptic ulcer disease), and it does not incorporate some that evidently have such impact (e.g. noncerebrovascular neurological conditions) [40]. Another limitation of the CCI is that it does not take into account some disorders that might affect prognosis or evolution of quality of life in cancer patients, like Parkinsonism, blood transfusions, transplantations, thromboses, lung embolisms, and angina pectoris [59]. Furthermore, Streiner and Norman [60] state that for a valid comorbidity index inclusion of as many relevant items (diseases) as possible, is more important than the weighting of individual conditions.
Also, cancer specific indices have been developed. The C3 Index [40] was developed as a cancer specific index using data from over 14,000 cancer patients, aiming to include all conditions that were likely to have an impact on functional status or length of life among cancer patients. They include conditions from other indices and conditions that were mentioned as relevant by clinical experts. The C3 index assesses the presence of 42 chronic conditions in five years previous to the diagnosis of cancer. Conditions are weighted to their impact on non-cancer mortality among cancer patients and then summed to arrive at an aggregated score. The C3 Index outperformed the CCI for the combined cancer types. The C3 Index was also used to evaluate of the impact of comorbidity on the stage of cancer at diagnosis [35]. Results indicated that (1) the presence of comorbidity increased the odds of a patient being diagnosed with distant metastases, (2) did not lead to earlier diagnosis, and (3) increased the likelihood of a patient receiving no staging of disease at diagnosis. The latter finding might be related to the fact that in case of severe comorbidity and hence poor prognosis, the clinician might decide not to extend diagnostics.
Guo et al. [61] assessed the prognostic value of the Adult Comorbidity Evaluation-27 (ACE-27), which was also developed for patients with cancer, on the course and prognosis of nasopharyngeal carcinoma. They found increasing levels of accurateness in patients with higher stages of cancer.
Apart from prognostic indices which predict hospitalization or death, other indices have been developed which differ in the selection of included diseases. For example, prognostic indices usually include asymptomatic but prognosis limiting diseases, such as hypertension but frequently exclude diseases without a short-term impact on mortality, such as osteoarthritis or mental illnesses other than dementia [57]. On the other hand, osteoarthritis may have a severe impact on physical functioning and mental illnesses on emotional or social well-being and all together may significantly reduce quality of life. Therefore, indices to predict other outcomes than mortality or health services utilization are needed. Recently, the health-related quality of life comorbidity index (HRQL-CI) has been developed and validated by Mukherjee et al. [62], using diseases that have the strongest association with health-related quality of life. Furthermore, Lorem et al. developed a comorbidity index named the health impact index, using self-rated health (SRH) as an outcome [63].
Bender et al. [64] evaluated the presence of symptom clusters in patients who have cancer as a comorbid disease to other chronic conditions. Their Comorbidity Questionnaire is a self-reported measure based on the CCI and modeled to assess conditions and symptoms.
The diversity of available measures reflects the fact that there is no single measure which satisfies all needs. Depending on the available data sources and the purpose for which the measure is intended, in research, comorbidity measure should be careful selected. Moreover, indices are often context-dependent from the characteristics of the population where they were derived from and underlie a change over time due to improved survival in conditions, changed (drug) treatments, and the overall demographic change. Therefore, indices such as the CDS have been adapted to certain populations and over time [65, 66] and others, such as the CCI may be outperformed by newer indices. However, it is increasingly popular to develop prognostic models and caution is needed about their methodological appropriateness in development and validation [67, 68].
12.6 Outcomes—Disease Related and Patient Related
The choice of appropriate outcome measures depends on a variety of factors, primarily on the main research question, feasibility, and methodological issues, such as study design and setting. Outcome measures shall be sensitive to changes, e.g. to detect pre- and post-intervention differences. These general requirements meet a number of challenges in patients with comorbidity such as confounding. Moreover, certain comorbidity may preclude the application of outcome measures such as the application of a questionnaire on cancer specific quality of life in patients with cognitive dysfunction. Apart from methodological issues, the key question is about the relevance of the outcome for patients. In patients with co- and multimorbidity, health outcomes shift from disease-specific to generic and patient’s values often swing from life expectancy to quality of life. Desired outcomes, such as symptom relief, preservation of physical, mental, and social functioning, or disease prevention are often of equal importance as the avoidance of undesired outcomes such as nausea, drowsiness, dizziness, lethargy, or confusion [69–71]. Considering this, research should provide effect estimates on efficacy/effectiveness with respect to a full range of holistic, cross-disease outcomes and should also provide sufficient information on potential harms. This evidence would support weighing of potential benefits and harms in decision making with patients with cancer and co-occurring conditions.
Studies that focus on comorbidity as the outcome have often investigated the association between cancer and susceptibility to subsequent comorbidity. In this respect, cancer has been suggested as an indicator of aging, showing through an increased susceptibility to comorbidity, also for young cancer survivors [72]. Studies that focus on comorbidity as a confounding factor generally focused on the effect of comorbidity on treatment decisions (e.g. treatment choices and adherence to clinical guidelines) and cancer-related outcomes (e.g. treatment tolerance, 5-year survival) [73].
Survival/mortality. When analyzing mortality after a certain treatment, comorbidity is an essential patient characteristic which has to be taken into account [37]. Moreover, attention should be paid to different time windows and specific comorbid conditions. Tovikkai et al. [37] showed changes in prevalence of comorbid conditions dependent on the study era, but also showed different effects in different time windows after liver transplantation, where chronic renal disease tended to be related to a short term (first 90 days) increase of mortality, whereas dementia seemed to be associated with an increased mortality after 5 years.
When different patient populations or clinical settings are considered the survival probabilities may differ significantly between patients with apparently identical levels of comorbidities [51].
Delay of the diagnosis of cancer/stage of cancer at diagnosis. Comorbidity has an impact on cancer stage at diagnosis, but until now findings regarding this subject are ambiguous, and there are explanations for both positive and negative relations. People with comorbidity in general have an increased number of contacts to health services, which may result in a so-called surveillance effect, leading to earlier diagnosis. On the other hand, comorbidity may also distract both the physician and the patient from early signs and symptoms of cancer, resulting in a diagnostic delay [35]. In case of severe comorbidity that causes a serious limitation of life expectancy, diagnostics do not always appear warranted. Finally, specific conditions or their treatments can have a direct influence on cancer growth [74]. When further analyzing this, also other characteristics have to be taken into account, because patients with more comorbid diseases are in general also older, more often female, and tend to have lower socio-economic status. Also, when relating summary measures of comorbidity to staging colorectal cancer at diagnosis, results are conflicting [75].
Treatment decisions/prognosis/recurrence of cancer. Comorbidity can have an important impact on the treatment decision making process for patients with cancer [76], e.g. in the administration of radiotherapy and chemotherapy [77]. Even though this is relevant and frequently applied in clinical practice, it is not common practice in oncology research.
Patient related outcome measures (PROMs). Of the PROMs, the most commonly applied are quality of life, functional status, and disease burden/treatment burden [78]. Quality of life measurement tools can be divided into generic tools and disease specific instruments. Generic quality of life tools can be used for all patient groups, irrespective the absence of presence of e.g. cancer. An important advantage of generic instruments is the generalizability of the results, allowing the comparison of quality of life in patients with different diseases, or diseases in different stages. Generic quality of life instruments usually cover multiple domains, possibly including less relevant domains when applied to patients with cancer. At the same time those general instruments are potentially lacking details on other relevant domains, such as side effects of e.g. chemotherapy. A subgroup of the generic quality of life instruments are the utility generating tools, to assess cost-effectiveness from a societal perspective, expressed quality adjusted life years (QALYs) [79]. Disease-specific quality of life measures contain domains relevant to that disease. In oncology the most commonly applied disease-specific quality of life tools are the EORTC QLQ-C30 [80] and the FACT-scale [81]. However, these instruments have been mainly designed for patients with advanced disease stages and may have limitations when applied to patients with localized disease [82]. For use in patients with localized prostate cancer, Schmidt and co-workers identified eight instruments, but only three out of eight instruments showed a good performance regarding development process, metric properties, and administrative issues [82]. To assist the selection of instruments, Valderas et al. developed a tool for the standardized assessment of patient-reported outcomes (EMPRO) [83].
12.7 Statistical Analyses of Longitudinal Data
Statistical analysis of cancer research data encompasses an extensive spectrum of methods and software tools for analysis and reporting. These methods and analyses also apply to oncological studies encompassing comorbidity:
-
Measures of cancer burden (incidence, prevalence, mortality, and survival);
-
Therapeutic endpoints in the various phases of oncology clinical trials, from phase I, phase II, up to phase III trials;
-
Validation of biomarkers in diagnosis and prognosis of cancer;
-
Overall and net survival, relative survival ratio, excess mortality hazard;
-
Survival of cancer with the relative survival design, including cohort, complete, period, and hybrid approaches;
-
Methods of handling missing data and data quality; and
-
Estimation of avoidable deaths and personal or population “cure”.
Examples of resources on cancer statistics include the National Cancer Institute’s (NCI) overview of SEER tools (SEER stands for Surveillance, Epidemiology, and End Results Program) [84] the International Agency for Research on Cancer (IARC) [85] and handbooks of statistics in oncology, such as Crowley and Hoering [85]. These resources provide overview of and insight in the tools and methods to analyze incidence, mortality, survival, prevalence, and other related cancer statistics. If no follow-up data are available, linear and logistic regression analysis of outcomes are standard techniques for describing the relationship between an exposure variable and an outcome variable. Comorbidity can be used both as input and output to such modelling, for which the reader is referred to the literature.
The emphasis here is on cancer and comorbidity from a longitudinal perspective. On the one hand, attention is paid to studies with the availability of short-term and long-term follow-up information on cancer patients. On the other hand, when cancer and comorbidities are considered from a chronic disease perspective, whence there is a need to monitor the late effects of the disease and the treatment as well as the potentially negative neurocognitive, somatic and psychosocial outcomes of cancer survivors [86]. It is, perhaps, overstated to claim that statistics in oncology research is more complex and time consuming compared to other therapeutic areas. However, it is true that the analysis of longitudinal data, and especially survival data (time to event), is inherently difficult. Nonetheless, taking cancer and comorbidity into account significantly complicates statistical analyses through:
-
Skewed and non-normal distributed data;
-
Dependence between longitudinal clinical data and cancer outcomes;
-
Competing causes of death;
-
Different illness trajectories.
Skewed and non-normal distributed data: survival analysis is in many ways like conventional statistical analyses: information is gathered on the outcome or response variable on the one hand and covariates of interest on the other hand. It differs, however, in a very intricate aspect: the event of interest may not occur for each subject under study. Not all subjects will experience the outcome during the course of observation, resulting in the absence of a time-to-event for that particular individual. This situation is referred to as censoring in the analysis of survival data, and a study subject for whom no time-to-event is available is called censored. A typical situation is one in which a survival study has to end due to, for example, time constraints or resource limitations. In this case, for subjects whose survival events have not occurred at the end of the study, their survival times are not observed exactly but are known to be greater than the end of the study end time i.e., they are right-censored. For subjects who have already had the event at the end of the study, the time-to-event is known exactly. In essence, censoring implicates that an observation on a survival time of interest is incomplete; the survival time is observed only to fall into a certain range instead of being known exactly. Censored data are different from missing data as censored observations still provide partial information, whereas missing observations provide no information about the variable of interest. Different types of censoring arise in practice, but the one that receives most of the attention in the literature is right censoring [87].
Censored data analysis requires special methods to compensate for the information lost by not knowing the time of failure of all subjects. In addition, survival data analysis must account for skewed data [88]. Some individuals will experience the event of interest much sooner or later than the majority of individuals under study, giving the overall distribution of failure times a skewed appearance and preventing the use of the normal distribution in the analysis. Mostly, logarithmic transformations are used to stabilize the variance and allow for non-symmetric confidence intervals. Thus, the analysis of survival data requires techniques that are able to incorporate the possibility of skewed and censored observations. The reader is referred to the many excellent books and reviews of the major approaches in survival analysis: the parametric approach (e.g. exponential model, the Weibull model, the log-normal and logistic models), the non-parametric approach (e.g. the log-rank test), and the semi-parametric approach, e.g. the Cox proportional hazard model, perhaps the most widely used model in in clinical survival analysis [88, 89].
Dependence between longitudinal clinical data and cancer outcomes: Complicating it even more, standard statistical tools for the analysis of censored observations assume random censoring: event time and censoring time should be independent. However, in reality this might not be the case. A negative association between censoring and event time could occur when patients who are entering the study later have a better prognosis due to increased experience of surgeons. A positive association between censoring and event time occurs when patients are leaving the study because their health status is getting worse.
When event time and censoring time are not independent, the proportional hazards assumption of the commonly used Cox proportional hazard model does not hold. Several approaches exist to overcome this problem by extending the Cox proportional hazard model. One possible approach is to stratify a patient group, according to the values of some variable, mostly a variable which is considered a confounder rather than the main exposure of interest, e.g. comorbidity. The effect of the confounder is not estimated, but its effects are controlled for. An example is a study evaluating the therapeutic effects of intraperitoneal chemotherapy in which comorbidity is used as confounder variable [90]. A second approach is to include an exposure-time interaction term; that is to model the dynamic behavior of time-dependent variables. The third approach is to split the follow-up time into different periods. The latter puts emphasis on an important aspect of survival analysis: the choice of the time axis, because risks sets of patients will correspond to the choices made. The fourth approach is to model the complex changes over time itself, for example, by choosing one of the many available parametric models. Such models may be of particular use when the aim is to predict survival probabilities in different groups. If multiple pathologies are considered, which may have a distinct time scale, then such an approach might be conceivable. This is a technical and complex issue, for which the reader is referred to the specialized literature [91]. Van Houwelingen and Putter [92] show that within a short-term scope of the study the violations of the survival models are limited and small, whereas the effects will show up in large studies with long follow up.
This becomes more intricate, when addressing issues of variability in treatment response and chances of complete remission in patients with cancer, particularly when addressing heterogeneous patient populations, such as patients with comorbidity.
Competing causes of death: The literature on these combined or joint models is extensive and good examples are described by Fieuws et al. [93] and Brant et al. [94]. Studies including comorbidity or multimorbidity in such models are scarce. A notable exception is a study by Bayliss et al. [33] who analyzed a cohort of 6500 adults with initial cancer diagnosis between 2001 and 2008, SEER 5-year survival probability equal to or greater than 26 %, and a range of cardiovascular comorbidities. They modeled the competing risks by comparing different, cause-specific Cox proportional hazard models. Following cancer diagnosis, it was shown that 15.3 % of causes of death were attributed to cancer deaths, 5.1 % to serious cardiovascular deaths and 8.3 % of death from other causes. Thus, it was shown that in oncology populations, comorbidities interact to affect the competing risks of different outcomes. Another example is the nationwide, cohort study by Erichsen et al. [95], with 56,963 colorectal cancer (CRC) patients and five times as many patients from the general population (N = 271,670) matched by age, gender, and specific comorbidities. Among CRC patients with low comorbidity scores the 0-1 year mortality rate was 415 out of 1000-person-years (95 % CI: 401;430) and the interaction estimating the excess mortality rate in patients with both CRC and comorbidity accounts for 9.3 % of this rate. For patients with a severe comorbidity score the interaction consists of 34 % of the mortality. The interaction between CRC and comorbidity limited influence on mortality beyond 1 year after diagnosis, except again for the interaction between colorectal cancer and a high comorbidity burden accounting for 14 % of mortality 2-5 year after diagnosis. In sum, the authors showed that comorbidity interacts with colorectal cancer to increase the rate of mortality beyond that explained by the independent effects of CRC and comorbid conditions.
This shows that when taking comorbidity into account one often faces the problem of competing causes of death; the patient group under study may be more likely to die from complications due to the comorbid condition rather than due to the cancer [96–98]. Binbing et al. described a method to estimate the personal cure rate of cancer patients using population-based grouped cancer survival data [99]. Cancer patients are subject to multiple competing risks of death and may die from causes other than the cancer diagnosed. The probability of not dying from the cancer diagnosed, which is one of the patients’ main concerns, is sometimes called the “personal cure” rate. Binbing et al. [99] used two approaches of modelling competing-risk survival data, namely cause-specific hazards approach, and the mixture model approach. The authors used the colorectal survival data from the SEER Programme of the NCI (N = 199,715 colorectal cancer patients diagnosed between 1975 and 2002), with a maximum follow-up time of 28 years. They applied the models in particular, because comorbidity for cancer patients may limit treatments and increases the risk of death from other causes. Usually comorbidity from competing causes increases with advancing age and is greater for patients in poor health.
The above shows that statistical analysis of cancer survival data is a delicate issue by itself. The study of the intricate relationships between cancer—occurrence as well as recurrence—and comorbidity, complicates statistical analysis in various ways. The integration of comorbidity in the statistical analysis in cancer research emphasizes the need for:
-
The multi-adjustment of cancer survival not only for age, stage, and other cancer-related factors, but also for the co-occurring diseases
-
Multi-variable modelling of the excess hazard of death (due to comorbidity)
-
The comparison with different statistical tools, e.g. with Cox and Poisson approaches. The analysis of heterogeneity, variability and chance of health risks in various subgroups (stratified according to age, sex, and comorbidity). Some subjects might be more prone or more likely to experience an event. Normally, in most clinical applications, survival analysis implicitly assumes a homogeneous population to be studied. This means that all individuals sampled in that study are subject, in principle, to the same risk (e.g., risk of death and risk of disease recurrence). In many applications, the study population cannot be assumed to be homogeneous but must be considered as a heterogeneous sample, i.e., a mixture of individuals with different hazards. For example, in many cases, it is impossible to measure all relevant covariates related to the disease of interest [98, 100, 101] and special approaches are required to include heterogeneity in the analysis, e.g. different forms of frailty models [100, 102].
Taking into account the illness trajectory: In longitudinal study approaches data on patient characteristics, clinical data, and survival data are frequently collected simultaneously. For example, in many medical studies, clinical researchers collect patients’ information (e.g. blood pressures, X-ray measures) repeatedly over time and they are also interested in the time to recovery, recurrence of a disease (i.e. cancer) or death.
As such, longitudinal approaches are becoming increasingly important. Longitudinal approaches can be subdivided in:
-
1.
Adaptive designs
-
2.
Reciprocal designs: randomized clinical trial methodologies, e.g. potential clinical outcome model, causal modelling, propensity stratification integrated within observational studies; observational methodologies integrated within oncology trials [103]
-
3.
Trajectories: population-based and personalized trajectories.
Longitudinal clinical data and survival data are often associated in several ways, with the time to event (death) being associated with the longitudinal trajectories of clinical characteristics. Separate analyses of longitudinal clinical data and survival data may lead to inefficient and biased results as they do not take the underlying relationship between one another into account. In these settings, the multivariate longitudinal profiles and the event information need to be combined. Several methods have been proposed to combine longitudinal clinical data with event history data (e.g. survival, recurrence) [104, 105]. Most statistical methods, such as linear regression models, logistic regression models and survival models, are based on the assumption that the observations in a sample are independent of each other and that is the value of one observation is not influenced by the value of another. This assumption of independence will be violated if the data are clustered. Clustering or correlation is at hand, if observations in one cluster tend to be more similar to each other than in the rest of the sample. Clustered data usually arise when subjects are grouped, e.g. in cluster randomized trials of general practices or hospitals, family studies or cluster sampled surveys. Also when subjects are repeatedly measured as in longitudinal studies there are often clustered data (within subjects, e.g. the repeated measurement of blood pressure). In analyzing clustered data, connectedness of data has to be taken into account by aggregating data, or applying advanced statistical methods such as Generalized Estimating Equations or random effect models [106]. More information on these advanced statistical methods can, for example, be found in Hox [107] or Hox and Roberts [108].
Patients with comorbidity may face different illness trajectories, an important aspect of disease that is often neglected in current research. While a great deal of literature concerns the prediction of risk and the prognosis of co-occurring diseases in patients with multimorbidity, relatively little research is concerned with the course or “trajectory” of the illness of patients with multimorbidity [109]. Most multimorbidity studies focus on the identification of specific disease combinations in patient populations, based on one index disease and additional diseases, either in general or specific population-based studies or in administrative databases. In recent years a few studies investigated multimorbidity patterns, using data mining techniques, e.g. factor analysis methods, to investigate clusters of diseases. However, these studies are cross-sectional and investigate prevalence patterns in specific age groups, and restrict comorbidities to lists of common chronic conditions [110, 111].
Few studies have analyzed such multimorbidity patterns integrated with cancer as one of the health conditions. Islam et al. [112], reported three important multimorbidity patterns, one of which included cancer, coronary heart disease and stroke. Vos et al. [109] showed that 49 % of patients with more than ten chronic health conditions had at least one diagnosis of cancer during the course of their life. Jensen et al. [113], investigated a population-wide registry data, covering 6.2 million cancer patients of Denmark, and showed distinct disease development patterns for different types of cancer. For example, they showed a clustering of malignant neoplasms of the prostate and secondary malignant neoplasms of other sites. However, research on disease trajectories is rather limited and more research into the patterns and relating characteristics for different types of cancer as well different age and gender groups is needed.
With the growing population of patients with cancer together with other chronic health conditions [114], integrative analysis of cancer and multimorbidity is urgent. Two major challenges are open. One is to connect multimorbidity research with the rapid developments in integrative cancer data analysis; cancer informatics; and high-dimensional data analysis [115]. The other challenge is to elaborate and implement a longitudinal approach, from a clinical and a family practice perspective. Studies of multimorbidity patterns over long time periods are scarce [109, 116].
The concept of distinct trajectories of illness over time is well established in other advanced diseases [117, 118]. Longitudinal analysis of multimorbidity, however, is complex. Varying definitions of multimorbidity exist and different scopes of time windows are abound. If a research time-frame is short, a point in time (time independent, cross-sectional) comorbidity measure is sufficient. Many studies are longitudinal, raising questions how best to measure comorbidity over time [39]. Different approaches are available to model and analyze the multiple events and multiple pathways in these trajectories [87, 105].
The new developments include time-dependent covariates, recurrent events, quantile regression in identifying important prognostic factors for patient subpopulations and joint modelling such as quality of life and time to event data. Similarly, there is an explosion in new areas of statistics, such as space and time modelling, which might help to track an individual’s lifetime exposure while taking into account other clinically relevant histories, or track an individual’s access to cancer screening or treatment services. There is a rather large literature on Bayesian methods for survival data [89, 119]. It is not possible to do justice here to Bayesian methods and the many computational advances of recent years.
12.8 Recommendations for Future Research
-
Hospitals and research institutes should actively seek collaboration to join expertise and facilitate large epidemiological studies that include patients with different comorbid diseases, or disease patterns. This can also facilitate more efficient recruitment of patients.
-
Evidence on comparative effectiveness and safety of treatment in patients with cancer and comorbidity is needed and serious efforts should be made to share data of completed trials to conduct individual patient data meta-analyses and investigate subpopulations of sufficient sample size.
-
More input from patients in research is required, e.g. involvement in writing patient information or in developing strategies to recruit patients.
-
Research should further elicit the construction of patient’s preferences and the process of prioritization of conditions and treatments in patients with cancer and multiple disorders.
-
Comorbidity should always be taken into account, because of the proven impact on diagnostics, therapeutic decisions, psychosocial needs, and other needs during follow-up care. Furthermore, comorbidity as well as cancer are related to aging, and both are increasingly considered chronic health status, underlining the importance of studying the two as combined concepts.
-
When studying cancer and comorbidity, it is relevant to distinguish between complications of cancer regimen (long-term and late effects of treatments) and comorbidity.
12.9 Conclusions
Comorbidity is frequent in clinical practice amongst patients with cancer, but in scientific research too often comorbidity is ignored or methods are applied that insufficiently take into account comorbidity. It is, however, of vital importance to recognize the impact of comorbidity on a broad spectrum of outcomes when studying patients with cancer and comorbidity. Though complex to handle, ignoring or avoiding comorbidity in research is not an option.
The population of patients with cancer and comorbid conditions is a heterogeneous group. If it is decided to focus on a more homogeneous subgroup, results are more specific, but lack external validity and generalizability to the heterogeneous group of cancer patients.
Recruitment of (older) patients with cancer and comorbidity is a major challenge. Strategies to improve recruitment come at considerable costs because they require a substantial increase in time and efforts.
There is no single comorbidity measure available that satisfies all needs. A measure should be selected taking into account the research question, the available data sources, and the context of the study (e.g. community setting, nursing home, hospital).
Statistical analyses of studies encompassing oncological patients with comorbidity should reckon with complexity due to skewedness and non-normality of data, dependence between longitudinal clinical data and cancer related outcomes, competing causes of death and individual illness trajectories.
References
Deckx L, van den Akker M, Metsemakers J, Knottnerus A, Schellevis F, Buntinx F (2012) Chronic diseases among older cancer survivors. J Cancer Epidemiol 2012:206414
Smith AW, Reeve BB, Bellizzi KM, Harlan LC, Klabunde CN, Amsellem M, Bierman AS, Hays RD (2008) Cancer, comorbidities, and health-related quality of life of older adults. Health Care Financ Rev 29(4):41–56
Khan NF, Mant D, Carpenter L, Forman D, Rose PW (2011) Long-term health outcomes in a British cohort of breast, colorectal and prostate cancer survivors: a database study. Br J Cancer 105(Suppl 1):S29–S37
Ording AG, Horvath-Puho E, Lash TL, Ehrenstein V, Borre M, Vyberg M, Sorensen HT (2015) Prostate cancer, comorbidity, and the risk of venous thromboembolism: a cohort study of 44,035 Danish prostate cancer patients, 1995–2011. Cancer 121(20):3692–3699
Stewart S, Ekman I, Ekman T, Oden A, Rosengren A (2010) Population impact of heart failure and the most common forms of cancer: a study of 1 162 309 hospital cases in Sweden (1988 to 2004). Circ Cardiovasc Qual Outcomes 3(6):573–580
Quinn M, Babb P, Brock A (2001) Chronic heart failure: management of chronic heart failure in adults in primary and secondary care (CG108). In: Cancer trends in England and Wales 1950–1999. NICE National Institute for Health + Clinical Excellence, AHRQ Agency for Healthcare Research + Quality, The Stationary Office, London. Available from http://guidance.nice.org.uk/CG108
Shenoy P, Harugeri A (2015) Elderly patients’ participation in clinical trials. Perspect Clin Res 6(4):184–189
Hutchins LF, Unger JM, Crowley JJ, Coltman CA Jr, Albain KS (1999) Underrepresentation of patients 65 years of age or older in cancer-treatment trials. N Engl J Med 341(27):2061–2067
Mohile S, Dale W, Magnuson A, Kamath N, Hurria A (2013) Research priorities in geriatric oncology for 2013 and beyond. Cancer Forum 37(3):216–221
Balducci L, Fossa SD (2013) Rehabilitation of older cancer patients. Acta Oncol 52(2):233–238
Reuben D, Tinetti M (2012) Goal-oriented patient care—an alternative health outcomes paradigm. N Engl J Med 366(9):777–779
Blom JW, El Azzi M, Wopereis DM, Glynn L, Muth C, van Driel ML (2015) Reporting of patient-centred outcomes in heart failure trials: are patient preferences being ignored? Heart Fail Rev 20(4):385–392
Millman J, Galway K, Santin O, Reid J (2016) Cancer and serious mental illness—patient, caregiver and professional perspectives: study protocol. J Adv Nurs 72(1):217–226
Sada YH, Street RL Jr, Singh H, Shada RE, Naik AD (2011) Primary care and communication in shared cancer care: a qualitative study. Am J Manag Care 17(4):259–265
Rothman K, Greenland S, Lash T (2008) Modern Epidemiology, 3rd ed. Lippincot Williams & Wilkins, Philadelphia (Wolters Kluwer Health)
CEBM. Study Designs. Available from http://www.cebm.net/study-designs/. Cited 16 Mar 2016
Hang J, Cai B, Xue P, Wang L, Hu H, Zhou Y, Ren S, Wu J, Zhu M, Chen D, Yang H, Wang L (2015) The joint effects of lifestyle factors and comorbidities on the risk of colorectal cancer: a large chinese retrospective case-control study. PLoS ONE 10(12):e0143696
Klepin HD, Pitcher BN, Ballman KV, Kornblith AB, Hurria A, Winer EP, Hudis C, Cohen HJ, Muss HB, Kimmick GG (2014) Comorbidity, chemotherapy toxicity, and outcomes among older women receiving adjuvant chemotherapy for breast cancer on a clinical trial: CALGB 49907 and CALGB 361004 (alliance). J Oncol Pract 10(5):e285–e292
Muss HB, Berry DA, Cirrincione CT, Theodoulou M, Mauer AM, Kornblith AB, Partridge AH, Dressler LG, Cohen HJ, Becker HP, Kartcheske PA, Wheeler JD, Perez EA, Wolff AC, Gralow JR, Burstein HJ, Mahmood AA, Magrinat G, Parker BA, Hart RD, Grenier D, Norton L, Hudis CA, Winer EP (2009) Adjuvant chemotherapy in older women with early-stage breast cancer. N Engl J Med 360(20):2055–2065
Gridelli C (2001) The ELVIS trial: a phase III study of single-agent vinorelbine as first-line treatment in elderly patients with advanced non-small cell lung cancer. Elderly lung cancer vinorelbine Italian study. Oncologist 6(Suppl 1):4–7
Hempenius L, Slaets JP, Boelens MA, van Asselt DZ, de Bock GH, Wiggers T, van Leeuwen BL (2013) Inclusion of frail elderly patients in clinical trials: solutions to the problems. J Geriatr Oncol 4(1):26–31
Puts MT, Monette J, Girre V, Wolfson C, Monette M, Batist G, Bergman H (2009) Participation of older newly-diagnosed cancer patients in an observational prospective pilot study: an example of recruitment and retention. BMC Cancer 9:277
Deckx L (2015) The older cancer patient. Consequences of cancer and ageing, in Biomedical Sciences Group, Faculty of Medicine, Department of Public Health and Primary Care. KU Leuven: Leuven
van den Akker M, van Steenkiste B, Krutwagen E, Metsemakers JF (2015) Disease or no disease? Disagreement on diagnoses between self-reports and medical records of adult patients. Eur J Gen Pract 21(1):45–51
Emson HE (1987) Health, disease and illness: matters for definition. CMAJ 136(8):811–813
Patel VL, Arocha JF, Kushniruk AW (2002) Patients’ and physicians’ understanding of health and biomedical concepts: relationship to the design of EMR systems. J Biomed Inform 35(1):8–16
De-loyde KJ, Harrison JD, Durcinoska I, Shepherd HL, Solomon MJ, Young JM (2015) Which information source is best? Concordance between patient report, clinician report and medical records of patient co-morbidity and adjuvant therapy health information. J Eval Clin Pract 21(2):339–346
Garcia Rodriguez LA, Perez Gutthann S (1998) Use of the UK general practice research database for pharmacoepidemiology. Br J Clin Pharmacol 45(5):419–425
Truyers C, Goderis G, Dewitte H, van den Akker M, Buntinx F (2014) The Intego database: background, methods and basic results of a Flemish general practice-based continuous morbidity registration project. BMC Med Inform Decis Mak 14:48
Walley T, Mantgani A (1997) The UK general practice research database. Lancet 350(9084):1097–1099
Van den Akker M, Metsemakers J, Limonard C, Knottnerus J (2004) General practice: a gold mine for research. Data and scientific use of the registration network family practices. Maastricht: Unigraphic
van den Akker M, Spigt MG, de Raeve L, van Steenkiste B, Metsemakers J, van Voorst E, de Vries H (2008) The SMILE study: a study of medical information and lifestyles in Eindhoven, the rationale and contents of a large prospective, dynamic cohort study. BMC Publ Health 8:19
Bayliss E, Reifler L, Zeng C, McQuillan D, Ellis J, Steiner J (2014) Competing risks of cancer mortality and cardiovascular events in individuals with multimorbidity. J Comorbidity 4:29–36
Lee CC, Ho HC, Su YC, Chen PC, Yu CH, Yang CC (2015) Comparison of different comorbidity measures for oral cancer patients with surgical intervention: a longitudinal study from a single cancer center. Auris Nasus Larynx
Gurney J, Sarfati D, Stanley J (2015) The impact of patient comorbidity on cancer stage at diagnosis. Br J Cancer 113(9):1375–1380
Dunn J, Ng SK, Holland J, Aitken J, Youl P, Baade PD, Chambers SK (2013) Trajectories of psychological distress after colorectal cancer. Psychooncology 22(8):1759–1765
Tovikkai C, Charman SC, Praseedom RK, Gimson AE, van der Meulen J (2015) Time-varying impact of comorbidities on mortality after liver transplantation: a national cohort study using linked clinical and administrative data. BMJ Open 5(5):e006971
Beckmann KR, Bennett A, Young GP, Cole SR, Joshi R, Adams J, Singhal N, Karapetis C, Wattchow D, Roder D (2016) Sociodemographic disparities in survival from colorectal cancer in South Australia: a population-wide data linkage study. BMC Health Serv Res 16(1):24
Wang CY, Baldwin LM, Saver BG, Dobie SA, Green PK, Cai Y, Klabunde CN (2009) The contribution of longitudinal comorbidity measurements to survival analysis. Med Care 47(7):813–821
Sarfati D, Gurney J, Stanley J, Salmond C, Crampton P, Dennett E, Koea J, Pearce N (2014) Cancer-specific administrative data-based comorbidity indices provided valid alternative to Charlson and National Cancer Institute Indices. J Clin Epidemiol 67(5):586–595
Deshpande AD, Schootman M, Mayer A (2015) Development of a claims-based algorithm to identify colorectal cancer recurrence. Ann Epidemiol 25(4):297–300
Yurkovich M, Avina-Zubieta JA, Thomas J, Gorenchtein M, Lacaille D (2015) A systematic review identifies valid comorbidity indices derived from administrative health data. J Clin Epidemiol 68(1):3–14
Glasziou PP, Buchan H, Del Mar C, Doust J, Harris M, Knight R, Scott A, Scott IA, Stockwell A (2012) When financial incentives do more good than harm: a checklist. BMJ 345:e5047
Taichman DB, Backus J, Baethge C, Bauchner H, de Leeuw PW, Drazen JM, Fletcher J, Frizelle FA, Groves T, Haileamlak A, James A, Laine C, Peiperl L, Pinborg A, Sahni P, Wu S (2016) Sharing clinical trial data: a proposal from the international committee of medical journal editors. Lancet 387(10016):e9–e11
Weitzman ER, Kaci L, Mandl KD (2010) Sharing medical data for health research: the early personal health record experience. J Med Internet Res 12(2):e14
Weitzman ER, Kelemen S, Kaci L, Mandl KD (2012) Willingness to share personal health record data for care improvement and public health: a survey of experienced personal health record users. BMC Med Inform Decis Mak 12:39
Wen KY, Kreps G, Zhu F, Miller S (2010) Consumers’ perceptions about and use of the internet for personal health records and health information exchange: analysis of the 2007 health information national trends survey. J Med Internet Res 12(4):e73
Perkins AJ, Kroenke K, Unutzer J, Katon W, Williams JW Jr, Hope C, Callahan CM (2004) Common comorbidity scales were similar in their ability to predict health care costs and mortality. J Clin Epidemiol 57(10):1040–1048
von Korff M, Wagner E, Saunders K (1992) A chronic disease score from automated pharmacy data. J Clin Epidemiol 45(2):197–203
Mayr R, May M, Martini T, Lodde M, Comploj E, Pycha A, Strobel J, Denzinger S, Otto W, Wieland W, Burger M, Fritsche HM (2012) Comorbidity and performance indices as predictors of cancer-independent mortality but not of cancer-specific mortality after radical cystectomy for urothelial carcinoma of the bladder. Eur Urol 62(4):662–670
Frohner M, Wirth MP (2012) Age and comorbidity in early prostate cancer. Urologe A 51(10):1356–1361
Briganti A, Spahn M, Joniau S, Gontero P, Bianchi M, Kneitz B, Chun FK, Sun M, Graefen M, Abdollah F, Marchioro G, Frohenberg D, Giona S, Frea B, Karakiewicz PI, Montorsi F, Van Poppel H, Jeffrey Karnes R (2013) Impact of age and comorbidities on long-term survival of patients with high-risk prostate cancer treated with radical prostatectomy: a multi-institutional competing-risks analysis. Eur Urol 63(4):693–701
Ording AG, Sorensen HT (2013) Concepts of comorbidities, multiple morbidities, complications, and their clinical epidemiologic analogs. Clin Epidemiol 5:199–203
Lee A, Levine M (2003) Four topics in venous thromboembolism. venous thromboembolism and cancer: risks and outcomes. Circulation 107(1):17–21
Van den Akker M, Vos R, Knottnerus J (2006) In an exploratory prospective study on multimorbidity general and disease related susceptibility could be distinguished. J Clin Epidemiol 59(9):934–939
Gottlieb M, Marsaa K, Godtfredsen NS, Mellemgaard A (2015) Prevalence and management of pulmonary comorbidity in patients with lung and head and neck cancer. Acta Oncol 54(5):767–771
Charlson M, Pompei P, Ales K, MacKenzie C (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 40(5):373–383
Klabunde CN, Legler JM, Warren JL, Baldwin LM, Schrag D (2007) A refined comorbidity measurement algorithm for claims-based studies of breast, prostate, colorectal, and lung cancer patients. Ann Epidemiol 17(8):584–590
Deckx L, van Abbema D, Nelissen K, Daniels L, Stinissen P, Bulens P, Linsen L, Rummens JL, Robaeys G, de Jonge ET, Houben B, Pat K, Walgraeve D, Spaas L, Verheezen J, Verniest T, Goegebuer A, Wildiers H, van den Berkmortel F, Tjan-Heijnen VC, Buntinx F, van den Akker M (2011) Study protocol of KLIMOP: a cohort study on the wellbeing of older cancer patients in Belgium and the Netherlands. BMC Publ Health 11:825
Streiner D, Norman GR (2008) Health measurement scales. Oxford University Press, Oxford/New York/Tokyo
Guo R, Chen XZ, Chen L, Jiang F, Tang LL, Mao YP, Zhou GQ, Li WF, Liu LZ, Tian L, Lin AH, Ma J (2015) Comorbidity predicts poor prognosis in nasopharyngeal carcinoma: development and validation of a predictive score model. Radiother Oncol 114(2):249–256
Mukherjee B, Ou HT, Wang F, Erickson SR (2011) A new comorbidity index: the health-related quality of life comorbidity index. J Clin Epidemiol 64(3):309–319
Lorem GF, Schirmer H, Emaus N (2016) Health impact index. Development and validation of a method for classifying comorbid disease measured against self-reported health. PLoS ONE 11(2):e0148830
Bender CM, Engberg SJ, Donovan HS, Cohen SM, Houze MP, Rosenzweig MQ, Mallory GA, Dunbar-Jacob J, Sereika SM (2008) Symptom clusters in adults with chronic health problems and cancer as a comorbidity. Oncol Nurs Forum 35(1):E1–E11
Johnson ML, El-Serag HB, Tran TT, Hartman C, Richardson P, Abraham NS (2006) Adapting the Rx-Risk-V for mortality prediction in outpatient populations. Med Care 44(8):793–797
Vitry A, Wong SA, Roughead EE, Ramsay E, Barratt J (2009) Validity of medication-based co-morbidity indices in the Australian elderly population. Aust NZ J Publ Health 33(2):126–130
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD). Ann Intern Med 162(10):735–736
Hemingway H, Croft P, Perel P, Hayden JA, Abrams K, Timmis A, Briggs A, Udumyan R, Moons KG, Steyerberg EW, Roberts I, Schroter S, Altman DG, Riley RD (2013) Prognosis research strategy (PROGRESS) 1: a framework for researching clinical outcomes. BMJ 346:e5595
Fried T, McGraw S, Agostini J, Tinette M (2008) Views of older persons with multiple morbidities on competing outcomes and clinical decision-making. JAGS 56:1839–1844
Fried TR, Tinetti M, Agostini J, Iannone L, Towle V (2011) Health outcome prioritization to elicit preferences of older persons with multiple health conditions. Patient Educ Couns 83(2):278–282
Muth C, van den Akker M, Blom JW, Mallen CD, Rochon J, Schellevis FG, Becker A, Beyer M, Gensichen J, Kirchner H, Perera R, Prados-Torres A, Scherer M, Thiem U, van den Bussche H, Glasziou PP (2014) The Ariadne principles: how to handle multimorbidity in primary care consultations. BMC Med 12:223
Henderson TO, Ness KK, Cohen HJ (2004) Accelerated aging among cancer survivors: from pediatrics to geriatrics. Am Soc Clin Oncol Educ Book, pp e423–e430
Meneses K, Benz R, Azuero A, Jablonski-Jaudon R, McNees P (2015) Multimorbidity and breast cancer. Semin Oncol Nurs 31(2):163–169
Giovanucci E, Harlan D, Archer M, Bergenstal R, Gaprstur S, Habel LA, Pollak M, Regensteiner J, Yee D (2010) Diabetes and cancer: a consensus report. Diab Care 33(7):1674–1685
Corkum M, Urquhart R, Kendell C, Burge F, Porter G, Johnston G (2012) Impact of comorbidity and healthcare utilization on colorectal cancer stage at diagnosis: literature review. Cancer Causes Control 23(2):213–220
Stairmand J, Signal L, Sarfati D, Jackson C, Batten L, Holdaway M, Cunningham C (2015) Consideration of comorbidity in treatment decision making in multidisciplinary cancer team meetings: a systematic review. Ann Oncol 26(7):1325–1332
Rodrigues G, Sanatani M (2012) Age and comorbidity considerations related to radiotherapy and chemotherapy administration. Semin Radiat Oncol 22(4):277–283
Wister AV, Levasseur M, Griffith LE, Fyffe I (2015) Estimating multiple morbidity disease burden among older persons: a convergent construct validity study to discriminate among six chronic illness measures, CCHS 2008/09. BMC Geriatr 15:12
Schölzel-Dorenbos C (2012) Quality of life [Kwaliteit van leven], in cancer in older patients [Kanker bij ouderen]. In: Wymenga A et al. (ed). De Tijdstroom, Utrecht
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J et al (1993) The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 11(3):570–579
Schmidt S, Garin O, Pardo Y, Valderas JM, Alonso J, Rebollo P, Rajmil L, Garcia-Forero C, Ferrer M (2014) Assessing quality of life in patients with prostate cancer: a systematic and standardized comparison of available instruments. Qual Life Res 23(8):2169–2181
Valderas JM, Ferrer M, Mendivil J, Garin O, Rajmil L, Herdman M, Alonso J (2008) Development of EMPRO: a tool for the standardized assessment of patient-reported outcome measures. Value Health 11(4):700–708
National Cancer Institute (2015) Surveillance, epidemiology, and end results program. Available from: http://seer.cancer.gov/seerstat/. Cited on 16 Mar 2016
Crowley R, Hoering A (2012) Handbook of statistics in clinical oncology, 3rd ed. CRC Press, Seattle
Rubin G, Berendsen A, Crawford SM, Dommett R, Earle C, Emery J, Fahey T, Grassi L, Grunfeld E, Gupta S, Hamilton W, Hiom S, Hunter D, Lyratzopoulos G, Macleod U, Mason R, Mitchell G, Neal RD, Peake M, Roland M, Seifert B, Sisler J, Sussman J, Taplin S, Vedsted P, Voruganti T, Walter F, Wardle J, Watson E, Weller D, Wender R, Whelan J, Whitlock J, Wilkinson C, de Wit N, Zimmermann C (2015) The expanding role of primary care in cancer control. Lancet Oncol 16(12):1231–1272
Kleinbaum D, Klein M (2012) Survival analysis. A self-learning text, 3rd ed. Springer, New York
Verbeke G (2009) Biostatistics in oncology trials: survival analysis. “why clinicians hope for survivors and statisticians for deaths”. Available from: https://perswww.kuleuven.be/~u0018341/documents/oncology.pdf. Cited on 8 Mar 2016
Kalbfleisch J, Prentice R (2002) The statistical analysis of failure time data, 2nd ed. John Wiley, New York
Chang YH, Li WH, Chang Y, Peng CW, Cheng CH, Chang WP, Chuang CM (2016) Front-line intraperitoneal versus intravenous chemotherapy in stage III–IV epithelial ovarian, tubal, and peritoneal cancer with minimal residual disease: a competing risk analysis. BMC Cancer 16(1):235
Perperoglou A, Keramopoullos A, van Houwelingen HC (2007) Approaches in modelling long-term survival: an application to breast cancer. Stat Med 26(13):2666–2685
van Houwelingen H, Putter H (2012) Dynamic prediction in clinical survival analysis. CRC Press, Boca Raton
Fieuws S, Verbeke G, Maes B, Vanrenterghem Y (2008) Predicting renal graft failure using multivariate longitudinal profiles. Biostatistics 9(3):419–431
Brant L, Sheng S, Morrell C, Verbeke G, Lesaffre E, Carter H (2003) Screening for prostate cancer by using random-effects models. J Roy Stat Soc Ser A 166:51–62
Erichsen R, Horvath-Puho E, Iversen LH, Lash TL, Sorensen HT (2013) Does comorbidity interact with colorectal cancer to increase mortality? A nationwide population-based cohort study. Br J Cancer 109(7):2005–2013
Fine J, Gray R (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509
Putter H, Fiocco M, Geskus RB (2007) Tutorial in biostatistics: competing risks and multi-state models. Stat Med 26(11):2389–2430
Scrucca L, Santucci A, Aversa F (2010) Regression modeling of competing risk using R: an in depth guide for clinicians. Bone Marrow Transplant 45(9):1388–1395
Binbing Y, Tiwari RC, Feuer EJ (2011) Estimating the personal cure rate of cancer patients using population-based grouped cancer survival data. Stat Methods Med Res 20(3):261–274
Haller B, Schmidt G, Ulm K (2013) Applying competing risks regression models: an overview. Lifetime Data Anal 19(1):33–58
Satagopan JM, Ben-Porat L, Berwick M, Robson M, Kutler D, Auerbach AD (2004) A note on competing risks in survival data analysis. Br J Cancer 91(7):1229–1235
Cox D (1972) Regression models and life tables (with discussion). J R Statist Soc B 34:187–220
Hernan MA (2010) The hazards of hazard ratios. Epidemiology 21(1):13–15
Singer J, Willett J (2003) Applied longitudinal data analysis. Modeling change and event occurrence. University Press, Oxford
Diggle P, Heagerty P, Liang K, Zeger S (2013) Analysis of longitudinal data. In: Oxford statistical science series, 2nd ed. Oxford University Press, Oxford
Kirkwood B, Sterne J (2003) Essential medical statistics, 2nd ed. Blackwell Science, Oxford
Hox J (2010) Multilevel analysis: techniques and applications, 2nd ed. Routledge, New York
Hox J, Roberts K (2011) Handbook of advanced multilevel analysis. Routledge, New York
Vos R, van den Akker M, Boesten J, Robertson C, Metsemakers J (2015) Trajectories of multimorbidity: exploring patterns of multimorbidity in patients with more than ten chronic health problems in life course. BMC Fam Pract 16:2
van den Bussche H, Koller D, Kolonko T, Hansen H, Wegscheider K, Glaeske G, von Leitner EC, Schäfer I, Schön G (2011) Which chronic diseases and disease combinations are specific to multimorbidity in the elderly? Results of a claims data based cross-sectional study in Germany. BMC Publ Health 11:101
Newcomer S, Steiner J, Bayliss E (2011) Identifying subgroups of complex patients with cluster analysis. Am J Manag Care 17(8):e324–e332
Islam MM, Valderas JM, Yen L, Dawda P, Jowsey T, McRae IS (2014) Multimorbidity and comorbidity of chronic diseases among the senior Australians: prevalence and patterns. PLoS ONE 9(1):e83783
Jensen AB, Moseley PL, Oprea TI, Ellesoe SG, Eriksson R, Schmock H, Jensen PB, Jensen LJ, Brunak S (2014) Temporal disease trajectories condensed from population-wide registry data covering 6.2 million patients. Nat Commun 5:4022
Sorensen HT (2013) Multimorbidity and cancer outcomes: a need for more research. Clin Epidemiol 5(Suppl 1):1–2
Wei Y (2015) Integrative analyses of cancer data: a review from a statistical perspective. Cancer Inform 14(Suppl 2):173–181
Hsu HC (2015) Trajectories of multimorbidity and impacts on successful aging. Exp Gerontol 66:32–38
Wong A, Boshuizen HC, Schellevis FG, Kommer GJ, Polder JJ (2011) Longitudinal administrative data can be used to examine multimorbidity, provided false discoveries are controlled for. J Clin Epidemiol 64(10):1109–1117
Huntley A, Johnson R, Purdy S, Valderas J, Salisbury C (2012) Measures of multimorbidity and morbidity burden for use in primary care and community settings: a systematic review and guide. Ann Fam Med 10(2):134–141
Ibrahim J, Chen M, Sinha D (2001) Bayesian Survival Analysis. Springer series in statistics. Springer, New York
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media Singapore
About this chapter
Cite this chapter
van den Akker, M., Deckx, L., Vos, R., Muth, C. (2016). Research Considerations in Patients with Cancer and Comorbidity. In: Koczwara, B. (eds) Cancer and Chronic Conditions. Springer, Singapore. https://doi.org/10.1007/978-981-10-1844-2_12
Download citation
DOI: https://doi.org/10.1007/978-981-10-1844-2_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-1843-5
Online ISBN: 978-981-10-1844-2
eBook Packages: MedicineMedicine (R0)