Abstract
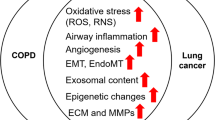
Chronic obstructive pulmonary disease (COPD) and lung cancer are caused by cigarette smoking, and there is increasing evidence linking the two diseases beyond a common etiology. COPD is widely considered to be a preneoplastic condition of smoking-related lung cancer. However, COPD is an independent risk factor for lung cancer and suggests some selected COPD phenotype in high-risk patients associates the development of lung cancer. Lung cancer patients with COPD have a significantly worse outcome than those without COPD. Thus, screening of patients with COPD for early detection of lung cancer using biomarkers and computed tomography has been suggested to improve outcomes. However, this approach of increased surveillance is hampered by the lack of sensitivity of treatment and the resulting large number of false-positive diagnoses. Improved understanding of the links between COPD and lung cancer and biomarkers that are more reliable may make this approach viable. In future, it may be possible to treat COPD patients with targeted therapies to reduce the risk of development of lung cancer.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The risk of lung cancer in patients with chronic obstructive pulmonary disease (COPD) is well established, and several mechanisms have been suggested to explain the strong association between emphysema and lung cancer. There are 55 carcinogens in cigarette smoke that have been evaluated by the International Agency for Research on Cancer (IARC) and for which there is “sufficient evidence for carcinogenicity” in laboratory animals or humans [1]. Thus, it is reasonable that both lung cancer and emphysema are associated with cigarette smoking, which, by generating reactive oxidant species (ROS), induces a chronic inflammatory state in the lung and results in DNA damage.
Typically, airway disease and smoking exposure are associated with proximal lung cancers, such as squamous cell carcinoma (SCC) and small cell lung carcinoma (SCLC), rather than adenocarcinoma. Squamous metaplasia is common in smokers and is associated with airway obstruction in COPD [2]. The function of bronchoalveolar stem cells (BASCs) is unknown, but these cells lead to Kras-induced lung adenocarcinoma in a mouse model [3]. Inflammatory mediators induced by cigarette smoke may promote growth of BASCs and stimulate nuclear factor-kB (NF-kB) and signal transducer and activator of transcription 3 (STAT3), which have key roles in development of lung cancer from COPD [4].
COPD is considered to be a preneoplastic condition of lung cancer, and about 2.2 % of COPD patients develop lung cancer per year [5]. The risk of lung cancer in patients with COPD is approximately fivefold greater than that of smokers without COPD, independent of age and amount of cigarette smoking [6]. Smoking is an independent risk factor for COPD. The genetic and biological characteristics of COPD are similar to those of lung cancer, but the mechanism of development of lung cancer in COPD is unknown. However, this mechanism seems to involve individual host susceptibility to cigarette smoke and features of heterogeneity between the two diseases. Further large cohort studies are needed in subjects with appropriate phenotypes to identify potential drivers and predict biomarkers for screening of COPD-associated lung cancer.
2 Screening for Early Detection of COPD-Associated Lung Cancer
2.1 Annual Computed Tomography (CT) for Lung Cancer Screening
It is unclear whether the degree of airflow limitation and alveolar destruction confers a regional or global risk of lung cancer. The incidence of lung cancer may be related to the severity of airspace destruction, as assessed by CT-based semiquantitative scoring of emphysema lesions in the lungs [7–9]. Emphysema lesions of ≥5 % on CT were found to be associated with a 3.8-fold increase in lung cancer risk among smokers [9]. An increased risk of lung cancer has also been found with more severe COPD, based on the percentage predicted forced expiratory volume in 1 s (FEV1) [7, 10, 11].
Screening of COPD patients for development of lung cancer using annual CT scans has been suggested for early detection. Patients with COPD and those with >35 pack-years of smoking have a significantly increased risk of death due to lung cancer, but CT screening was reported to have no significant effects on lung cancer mortality [12]. However, the National Lung Screening Trial (NLST) showed that low-dose CT screening is associated with a decrease in mortality from lung cancer of 20 %. In screening of patients with spirometric COPD, there was a twofold increase in lung cancer incidence and a trend favoring greater detection of early-stage cancers and fewer late-stage cancers in CT screening compared with chest radiography screening [13]. However, this result was associated with 96.4 % false-positive findings, and 38.8 % of patients with lung cancer were false negatives that were missed by CT screening [14]. Therefore, these approaches of increased surveillance are hampered by the lack of sensitivity of treatment and the large number of false-positive diagnoses [13].
2.2 Screening Using Liquid Biomarkers
Early detection of lung cancer in high-risk individuals has been attempted using evaluation of serum tumor markers such as cancer antigen 19–9 (CA19-9) and CA125, which are increased in relation to the severity of COPD [15]. However, it is difficult to use markers to detect lung cancer in COPD, since the serum levels of carcinoembryonic antigen (CEA), neuron-specific enolase (NSE), and cytokeratin fragment 19 (CYFRA 21–1) do not differ between patients with lung cancer and those with nonneoplastic lung diseases such as acute pneumonia, COPD, and interstitial lung diseases [16, 17].
Methods used for early diagnosis of lung carcinoma, including biological tests of blood samples and multiplexed tumor-associated autoantibody-based blood tests, are inconclusive or require confirmation in larger cohorts [18]. A large prospective study of early detection of lung cancer in patients with lung impairment showed that serum p53Abs levels were associated with smoking level and lung function impairment, both of which are risk factors of cancer development. However, no occurrence of lung cancer was detected in follow-up of positive subjects [19].
Plasma cfDNA levels in patients with non-small cell lung cancer (NSCLC) are significantly higher than in patients with chronic respiratory inflammation and in healthy controls. The mechanism through which cfDNA is released into the bloodstream is unknown, but it is revealed that elevated plasma cfDNA levels in patients with NSCLC are primarily due to tumor development, which has clinical implications for lung cancer screening and early diagnosis [20]. Migration of circulating tumor cells (CTCs) into the bloodstream also seems to be an early event in carcinogenesis, based on data showing that tumors of size <1 mm are associated with the presence of CTCs in blood [21]. CTCs were detected in 3 % of COPD patients by the isolation by size of epithelial tumor cells (ISET) method in blood filtration size-based CTC selection. After a mean follow-up period of 3.2 years, a surveillance CT program revealed lung nodules with a mean size of 1.7 cm in diameter. All CTC-positive COPD patients had lung cancer of stage IA [22]. These results suggest that validation of liquid biomarkers for early detection of lung cancer in COPD patients is warranted in larger population-based studies in different ethnic groups.
2.3 Screening of Gene Mutations
Cigarette smoking is a major risk factor for COPD, but only a minority of smokers develop COPD, and this seems to depend on the host response against cigarette smoking [23]. A minor population of COPD patients with genetic susceptibility to COPD-associated lung cancer have DNA damage that results in occurrence of lung cancer. Genetic mapping has identified several single nucleotide polymorphisms (SNPs) that have been speculatively linked to COPD-associated lung cancer. In addition, genome-wide association studies (GWASs) have shown that lung cancer and COPD share some genetic mutations, independent of smoking. Genotypes with reduced α1-antitrypsin (A1AT) inhibitory capacity have an increased risk for lung cancer [24, 25]. Imbalance of oxidative stress and antioxidants is common in COPD and drives cancer onset through free radical-mediated DNA damage, repair of which may be impaired by mutations and polymorphisms. Mutation of antioxidant enzymes such as glutathione S-transferase μ1 (GSTM1) reduces lung tissue protection against damage-inducing substances in tobacco and increases the risk of lung cancer in patients with COPD compared to healthy subjects [26].
Epidemiological studies have consistently found associations between the chromosome 15q24–15q25.1 locus, which is linked to nicotine addiction, and lung cancer susceptibility in COPD [27]. The association with this locus encompasses four candidate genes (CHRNA3/CHRNA5, IREB2, PSMA4) and several functionally relevant SNPs in a region where the degree of linkage disequilibrium is still to be clarified. Genetic variation in the 15q25 locus, which encodes the nicotinic acetylcholine receptor subunits (CHRNA3/CHRNA5), has a strong association with tobacco consumption and is a risk factor for COPD and lung cancer [28]. Variants of IREB2, a mediator of iron homeostasis, have also been linked to COPD and lung cancer [29]. PSMA4 encodes a structural protein of the 20S proteasome core and has recently been associated with in vitro lung cancer cell proliferation and apoptosis. PSMA4 mRNA levels are increased in lung tumors compared with normal lung tissues [30]. The Hedgehog-interacting protein (HHIP), which mediates the epithelial response to smoking, including the epithelial-mesenchymal transition (EMT), is related to COPD and lung cancer, and genetic variants on the 4q31 (HHIP/glycophorin A (GYPA)) locus are also associated with lung cancer [31]. FAM13A protein has an N-terminal region containing a RhoGAP domain, which has tumor suppressor activity through inhibition of RhoA intracellular signal transduction. Genetic variants in FAM13A may determine susceptibility to COPD and lung cancer [32].
Smoking and oxidative stress can induce EMT-induced airway remodeling, which is related to the pathogenesis of COPD, and the occurrence of EMT in COPD may account for the high incidence of lung cancer in patients with COPD [33]. Recent GWASs have shown that germline variants in or close to EMT-related genes (e.g., Snai1, Slug) are associated with a risk for lung cancer or COPD [31]. The functional germline variant c.353T>C (p.Val118Ala) of Snai1 confers decreased risks of lung cancer and COPD, and this variant affects lung cancer risk through a mediation effect on COPD [34].
Screening of gene mutations as susceptibility loci for COPD-associated lung cancer, particularly in the 15q24–15q25 region, should be considered after sensitivity is determined in future studies. Monitoring of mutation-positive COPD patients may allow early diagnosis of lung cancer at lower cost than noninvasive screening for inflammatory cells in blood or sputum, rather than lung tissues from invasive diagnostic modalities such as fine-needle aspiration, transbronchial biopsy, and thoracoscopic surgery. Genetic variants might be predictors for the risk of COPD and lung cancer separately, as well as for the risk of development of lung cancer in patients with COPD (Table 18.1).
2.4 Screening of Epigenetic Changes
Epigenetic changes in COPD include higher levels of methylation induced by cigarette smoking, while altered expression of numerous oncogenes and tumor suppressor gene promoters is observed in most lung cancers. Methylation of CDKN2A, MGMT, CCDC37, and MAP1B is significantly associated with COPD and lung cancer. CDKN2A, which encodes tumor suppressors p16 (INK4A) and ARF, is a common methylation mark in COPD and lung cancer [35]. Such aberrant methylation of tumor suppressor genes in lung tissues and induced sputum may be a predictor for early diagnosis of COPD-associated lung cancer [36]. Epigenetic changes in noncoding RNAs, including microRNAs (miRNAs), which are small noncoding, single-stranded RNA molecules, may also be important. For example, miR-1 has been linked to cigarette smoking-related conditions such as heart disease and cancer [37] and is related to atrophy of skeletal muscle in patients with COPD compared with non-smoking controls [37]. miR-21 has roles in inflammation and carcinogenesis [38], whereas miR-146a suppresses inflammation and cancer cell proliferation [39]. However, the mechanisms of epigenetic biomarkers in COPD-associated lung cancer and their effects on prognosis remain poorly understood.
3 Management of Outcomes of COPD-Associated Lung Cancer
3.1 Management of Chronic Inflammation
Exposure to cigarette smoke causes inflammatory cells, particularly neutrophils and macrophages, to be recruited at the site of lung injury and activated to release neutrophil elastase (NE), serine and matrix metalloproteinases (MMPs), and ROS. A defect in A1AT contributes to degradation of elastin due to activation of NE and oxidative stress-mediated inflammation in the lung, resulting in development of emphysema and lung tumorigenesis [40, 41]. Many studies have shown that chronic inflammation in lung tissue and associated repair processes in COPD may initiate lung cancer [42, 43]. An excess of circulating inflammatory mediators such as IL-6, TNF-α, and IL-8 released from inflammatory cells maintains chronic systemic inflammation in patients with COPD and, thus, further contributes to carcinogenesis [44, 45]. Current therapies for COPD, including inhaled corticosteroids (ICS), long-acting muscarinic receptor antagonists (LAMAs), long-acting β2-agonists (LABAs), and theophylline, suppress inflammation in the lung and prevent spillover of inflammatory mediators into the systemic circulation. Theophylline indirectly suppresses NF-kB, which is a cause of persistent airway inflammation, and may reduce the risk of tumorigenesis by activating histone deacetylase 2 (HDAC2), which restores sensitivity to ICS in patients with COPD [46]. Thus, patients with COPD who are treated with ICS have a reduced incidence of lung cancer and lower mortality, which suggests that inhibition of inflammation can slow lung tumor onset [47]. However, large prospective trials have failed to demonstrate a survival benefit in chronic use of ICS with or without LABAs [48].
3.2 Management of Oxidative Stress
The free radical hypothesis suggests that reactive nitrogen and oxygen species (RNOS) drive accumulation of cell and DNA damage, which results in mutations and cancer initiation if incorrectly repaired. RNOS can degrade proteins, including tumor suppressors, leading to cell division and decreased apoptosis and DNA repair [49], which results in cancer promotion and progression. Antioxidant therapy for reduction of the risk of lung cancer using vitamin C, vitamin E, or N-acetyl cysteine (NAC) may be of benefit for patients with COPD. However, supplementation with vitamins E or C was shown to have no significant effect on total cancer incidence in the USA [50, 51], and 2-year NAC supplementation resulted in no survival or event-free survival benefit in patients with lung cancer, most of whom were previous or current smokers [52].
3.3 Management of Angiogenesis
A recent study suggested that hypoxic regions of the lung may have a role in the association between COPD and lung cancer. The hypoxia-inducible factor (HIF) family, HIF-1α and HIF-2α, is well known as inducers of VEGF-mediated angiogenesis and is likely to play a role in the increased cancer risk in COPD [53, 54]. HIF-2α overexpression in a conditionally expressed mutant mouse model of lung carcinogenesis resulted in larger tumors [55]. However, HIF-2α deletion unexpectedly showed an increase in tumor burden, associated with a decrease in a candidate tumor suppressor gene.
Serum VEGF levels are significantly associated with clinical staging and lower survival of patients with NSCLC [56]. Bevacizumab is a recombinant, humanized, monoclonal antibody against VEGF that is approved as first-line treatment of NSCLC based on data from randomized phase III clinical trials [57]. In COPD pathogenesis, epithelial cell injury mediated by oxidative stress may induce a decrease in lung VEGF levels, resulting in promotion of COPD. Inhibition of VEGF receptors induces alveolar septal cell apoptosis and leads to enlargement of air spaces, indicative of emphysema [58]. These results suggest that bevacizumab-based chemotherapy for COPD-associated lung cancer may be disadvantageous for COPD management. However, some studies have linked COPD with increased expression of VEGF in bronchial tissue [59], and activation of NF-kB in COPD promotes HIF stabilization [60]. The significance of VEGF production in patients with COPD remains unclear, but inflammation and hypoxia regulation may have some impact on the prognosis of COPD-associated lung cancer. Thus, the response to specific treatment for tumors arising in a hypoxic lung-induced VEGF production might be exploitable in patients with underlying COPD.
3.4 Management of Extracellular Matrix Regulation
Neutrophil elastase (NE) has a well-known effect on elastin fiber degradation that results in emphysema and promotes lung tumor growth in a Kras mouse model of lung adenocarcinoma [61]. The relationship of NE activity with poor outcomes in human lung cancer has not been established, but drugs that inhibit NE activity might be of value as therapeutic prevention for COPD-associated lung cancer.
Members of the MMP family are matrix-degrading enzymes in emphysema and lung cancer and may be mechanistic links between COPD and lung cancer by contributing to lung tissue destruction in emphysema and promoting lung tumor growth and invasiveness. The activities of MMP9 (gelatinase B) in BAL fluid and serum correlate with COPD severity [62, 63], and MMP9 is essential for tumor angiogenesis in animal models [64]. MMP1 (collagenase I) contributes to growth of most solid tumors and promotes metastasis [65]. Overexpression of MMP1 in transgenic mice causes development of emphysema [66], and polymorphisms in the MMP1 promoter predict disease severity in patients with COPD [67]. MMP12, a somewhat macrophage-specific proteinase, is a stimulator of emphysema, and its activity has been associated with disease severity in COPD [68]. Interestingly, MMP12 is known more as a tumor suppressor and not as a target for treatment of lung cancer [69] (Table 18.2).
The effects of AZD1236, a selective MMP9 and MMP12 inhibitor, on emphysematous lung tissue degradation were evaluated in patients with moderate-to-severe COPD, but AZD1236 and other MMP inhibitors do not improve lung function and symptoms [70]. Similarly, other MMP inhibitors, marimastat (BB2516) and BAY12-9566, failed to improve survival in patients with advanced NSCLC [71]. Clinical trials have yet to demonstrate significant increases in overall survival and toxicity remains an issue.
3.5 Drug Potency
Increasing intracellular levels of cAMP induce cancer cell death in vitro. Theophylline, which elevates intracellular cAMP, induces cancer cell apoptosis and thus may be a potential anticancer drug in combination with other chemotherapeutic agents [72]. COX2 generates prostaglandin E2 (PGE2), which strongly elevates intracellular cAMP, but PGE2 also promotes carcinogenesis in several ways, including increased resistance to apoptosis, increased angiogenesis, and enhanced invasion [73]. Celecoxib, a COX2-selective inhibitor, may reduce the cancer risk in a high-risk smoking population based on reduction of proliferation markers in the bronchial epithelium [74]. Celecoxib increased progression-free survival in combination treatment in patients with lung adenocarcinoma cancer with biomarkers for high metabolism of PGE2 in urine [75] and reduced progression of cigarette smoke-induced pulmonary emphysema by suppression of NF-kB-regulated anti-inflammatory effects in an animal model [76]. Oral prostacyclin (iloprost) also has a tumor-suppressive effect and displays antiproliferative and antimetastatic properties [77]. However, the proven benefits of celecoxib and iloprost are limited to patients with established COPD. A nonselective COX inhibitor, indomethacin, and a nonselective PDE inhibitor, IBMX, significantly inhibit proliferation of SCLC cells with neuronal characteristics in vitro [78]. Beta-adrenergic receptors co-express COX2 in lung adenocarcinoma tissue [79], and indacaterol, an ultra-long-acting inhaled β2-agonist (LABA), inhibits NF-kB activity and reduces expression of NF-kB target genes related to COPD and lung cancer, including MMP9 [80]. This suppresses tumor cell invasion and migration in vitro, but the effect on outcomes for lung cancer in human study is unknown.
Non-neuronal ACh activates downstream NF-kB signaling and acts as an autoparacrine growth factor to stimulate cell proliferation and promote epithelial-mesenchymal transition (EMT) in NSCLC via activation of the M2 muscarinic receptor (M2R) [81, 82]. Expression of another mAChR, M3R, is significantly increased in NSCLC and is correlated with tumor metastasis and poor survival. M3R enhances expression and activity of MMP9 through PI3K/Akt, which promotes migration and invasion of NSCLC cells, and blockade of M3R suppresses proliferation, invasion, and migration of NSCLC and SCLC cells [83–85]. R2HBJJ has high affinity to M3 and M1 AChRs and markedly suppresses growth of NSCLC cells [86]. These findings indicate that M2R and M3R antagonists may be beneficial therapy for COPD-associated lung cancer. Such compounds are currently used for COPD treatment, including LAMAs, LABAs, and theophylline, but they may be toxic at higher concentrations required for anticancer treatment according to the results from these in vitro experiments. There are currently no clinical trials of these drugs in lung cancer patients.
4 Treatment of COPD-Associated Lung Cancer
4.1 Thoracic Surgery
Severe airway obstruction, advanced clinical stage, and higher age are independent factors associated with an indication for thoracic surgery in COPD-associated lung cancer [87]. Comorbidities such as COPD can have a significant effect on long-term survival due to an influence on treatment indication, complication rate, and treatment efficacy. COPD and smoking are significant independent risk factors for postoperative pulmonary complications such as atelectasis and pneumonia and are associated with a poorer long-term outcome [88]. Patients receiving curative surgery for NSCLC who have co-existing COPD have worse survival than their counterparts with better pulmonary function. Notably, the treatment-naïve COPD patients who have improved preoperative symptoms and pulmonary function by inhaled tiotropium starting 2 weeks prior to surgery demonstrated better postoperative pulmonary functions than expected [89].
Higher COPD grades have more postoperative pulmonary complications and poorer long-term survival because of higher rates of recurrence of lung cancer (Fig. 18.1) [90]. In patients with stage I resected NSCLC, COPD is an independent predictor of reduced recurrence-free survival, and these patients are at higher risk of recurrence than patients without COPD [91, 92]. Therefore, it is important to identify patients with early-stage NSCLC for more aggressive treatment. Clinical studies are needed in patients with lung cancer to determine how COPD promotes recurrence and affects the indication for adjuvant chemotherapy following curative resection.
Overall survival after pulmonary resection for lung cancer. The 5-year survival rates in the non-COPD, mild, moderate, and severe COPD groups were 61.5, 50.2, 55.3, and 25.1 %, respectively [90]
4.2 Chemotherapy and Molecular Targeted Therapy
Although there is not yet strong evidence for specific difference in management for lung cancer comorbidity with COPD, the patients with high age, poor overall PS, and severe impaired lung function associated with COPD are generally restricted to receive the appropriate platinum-based standard chemotherapy for the high risk of adverse effects. Thus, they often receive single-agent chemotherapy or choose best supportive care due to rapid progression to death. The mild COPD patients with advanced metastatic disease who received chemotherapy can delayed progression, palliate symptom, and improved overall survival and did not find significant differences in improved treatment outcome between mild COPD and non-COPD [93]. However, COPD exacerbations by airway infections and other factors often prevent the chemotherapy, and once acute exacerbation has occurred, the mortality rate is high in patients with COPD-associated lung cancer during chemotherapy.
EGFR mutations and ALK rearrangements are major drivers in non-smoker lung adenocarcinoma, and these patients may be particularly responsive to molecular targeted therapy. In contrast, patients with COPD-associated NSCLC have a low prevalence of EGFR mutations and ALK rearrangements, but these are linked to COPD severity and more frequent poorly differentiated lung cancer with a poor prognosis [87, 94]. In a comparison of the molecular features of COPD-associated adenocarcinoma with those of smoke-related adenocarcinoma without COPD, Schiavon et al. found that EGFR mutation did not differ between the two groups, but KRAS mutation was higher in smokers than in COPD patients [95].
In contrast to idiopathic interstitial pneumonias, the presence of COPD is not recognized as a significant risk factor for drug-induced interstitial lung disease associated with lung cancer treatment. Expression of EGFR is higher in lung cancer patients and in COPD patients [96]. Thus, EGFR inhibition has been examined in COPD as a method to prevent stimulation of mucous hypersecretion, but the initial studies have produced negative findings [97].
4.3 Radiation Therapy
Stereotactic body radiotherapy (SBRT) is standard of care for early-stage non-small cell lung cancer at high risk of surgical complications and associated with excellent local control (∼90 % at 3 years). In previous retrospective study, 32 % of stage I lung cancer patients with COPD who underwent SBRT had radiation pneumonitis, and COPD and the Brinkman index were statistically significant risk factors for the development of radiation pneumonitis. However, SBRT-mediated radiation pneumonitis did not associate OS, and thus SBRT can be tolerated in early lung cancer patients with COPD [98]. Severity of radiation pneumonitis associated higher in patients with a high V20 (≥25 %) value and severe low-attenuation area (LAA) grade on CT scans [99]. In contrast, patients with severe emphysema had a low risk of radiation pneumonitis following SBRT rather than normal lung function and with mild emphysema. Furthermore, fewer pack-years smoked among COPD patients were the strongest predictor for severe radiation pneumonitis [100, 101].
SBRT can be considered as therapeutic option in patients with higher operative risks, such as the elderly and patients with severe COPD. However, previous studies still provide controversial results about the risk of radiation pneumonitis in severe COPD patients. Further follow-up study might be needed to evaluate the tolerability to SBRT in COPD-associated lung cancer patients.
4.4 Immunotherapy
Chronic inflammation is a common feature in COPD and lung cancer, but the characteristics of immune cells in COPD differ from those found in lung cancer. Immune cells in BAL fluid from COPD patients tend to shift toward the T helper 1 (TH1) phenotype with interferon-γ (IFNγ) production [102]. In contrast, immune cells in most solid tumors show a trend for the TH2 phenotype with infiltration of immunosuppressive cells in tumor tissue. These cells include myeloid-derived suppressor cells (MDSCs) and regulatory T cells (TRegs) and express programmed cell death protein 1 (PD-1) on the cell surface, which results in suppression of cytotoxic T lymphocyte function and enhanced tumor viability [103, 104]. The use of PD-1- and PD-L1-blocking antibodies in therapy for NSCLC is focused on increasing cytotoxic T cell activity, which increases the cancer antigen-mediated immune response. Increasing PD-L1 expression in tumor tissue was observed in smokers and associated with more pack-years [105] and anti-PD-1/PD-L1 treatment prolonged OS in NSCLC patients with smoking history [106]. An increased proportion of CD8+ T cells in lung parenchyma in COPD patients has been described, and the PD-1 pathway has been suggested to be relevant in COPD pathogenesis. CD8+ T cells expressing PD-1 are present at higher levels in blood from COPD patients and are correlated with disease severity [107–109]. Furthermore, virus-induced expression of PD-L1, the ligand for PD-1, is decreased in COPD macrophages, with a corresponding increase in IFNγ release from infected COPD lungs resulting in increased severity of viral infection, prolonged viral shedding, and structural lung damage associated with exacerbations [110]. Although, anti-PD-1/PD-L1 treatment may associate better clinical outcome in smoking related lung cancers patients with COPD, we should note that the use of PD-1- and PD-L1-blocking antibodies may have indirect effects against chronic inflammation-mediated COPD development and aberrant immune regulation, especially during exacerbation of COPD. Aminophylline, which is often used as a bronchodilator for COPD patients, also has an unexpected effect on lymphocyte regulation and synergistically accelerates lymphocyte cell division in patients with lung cancer undergoing chemotherapy [111].
5 Conclusion
The incidence of COPD is a robust predictor of poor survival in lung cancer. Therefore, early detection of lung cancer is important in high-risk COPD subpopulations to prevent development of lung cancer. Although many approaches to predict the onset of lung cancer in patients with COPD have been proposed, most of them were still provided by experimental evidences (Table 18.3). Larger studies are needed to validate the potential of early diagnostic identification of COPD-associated lung cancer, along with further evidence of the efficacy of targeted therapies. Follow-up studies are also needed to evaluate the impact on patients with an increased risk of lung cancer and assess the predictive value of biomarkers for early detection of lung cancer in at-risk patients with COPD.
References
Hoffmann D, Hoffmann I. The changing cigarette, 1950–1995. J Toxicol Environ Health. 1997;50(4):307–64.
Araya J, Cambier S, Markovics JA, Wolters P, Jablons D, Hill A, et al. Squamous metaplasia amplifies pathologic epithelial-mesenchymal interactions in COPD patients. J Clin Invest. 2007;117(11):3551–62.
Kim CF, Jackson EL, Woolfenden AE, Lawrence S, Babar I, Vogel S, et al. Identification of bronchioalveolar stem cells in normal lung and lung cancer. Cell. 2005;121(6):823–35.
Houghton AM, Mouded M, Shapiro SD. Common origins of lung cancer and COPD. Nat Med. 2008;14(10):1023–4.
Rodriguez-Roisin R, Soriano JB. Chronic obstructive pulmonary disease with lung cancer and/or cardiovascular disease. Proc Am Thorac Soc. 2008;5(8):842–7.
Young RP, Hopkins RJ, Christmas T, Black PN, Metcalf P, Gamble GD. COPD prevalence is increased in lung cancer, independent of age, sex and smoking history. Eur Respir J. 2009;34(2):380–6.
de Torres JP, Bastarrika G, Wisnivesky JP, Alcaide AB, Campo A, Seijo LM, et al. Assessing the relationship between lung cancer risk and emphysema detected on low-dose CT of the chest. Chest. 2007;132(6):1932–8.
Zulueta JJ, Wisnivesky JP, Henschke CI, Yip R, Farooqi AO, McCauley DI, et al. Emphysema scores predict death from COPD and lung cancer. Chest. 2012;141(5):1216–23.
Li Y, Swensen SJ, Karabekmez LG, Marks RS, Stoddard SM, Jiang R, et al. Effect of emphysema on lung cancer risk in smokers: a computed tomography-based assessment. Cancer Prev Res (Phila). 2011;4(1):43–50.
Maldonado F, Bartholmai BJ, Swensen SJ, Midthun DE, Decker PA, Jett JR. Are airflow obstruction and radiographic evidence of emphysema risk factors for lung cancer? A nested case–control study using quantitative emphysema analysis. Chest. 2010;138(6):1295–302.
Wilson DO, Weissfeld JL, Balkan A, Schragin JG, Fuhrman CR, Fisher SN, et al. Association of radiographic emphysema and airflow obstruction with lung cancer. Am J Respir Crit Care Med. 2008;178(7):738–44.
Wille MM, Dirksen A, Ashraf H, Saghir Z, Bach KS, Brodersen J, et al. Results of the randomized Danish lung cancer screening trial with focus on high risk profiling. Am J Respir Crit Care Med. 2016;193(5):542–51.
Young RP, Duan F, Chiles C, Hopkins RJ, Gamble GD, Greco EM, et al. Airflow limitation and histology shift in the national lung screening trial. The NLST-ACRIN cohort substudy. Am J Respir Crit Care Med. 2015;192(9):1060–7.
National Lung Screening Trial Research T, Aberle DR, Berg CD, Black WC, Church TR, Fagerstrom RM, et al. The National Lung Screening Trial: overview and study design. Radiology. 2011;258(1):243–53.
Bulut I, Arbak P, Coskun A, Balbay O, Annakkaya AN, Yavuz O, et al. Comparison of serum CA 19.9, CA 125 and CEA levels with severity of chronic obstructive pulmonary disease. Med Princ Pract. 2009;18(4):289–93.
Hillas G, Moschos C, Dimakou K, Vlastos F, Avgeropoulou S, Christakopoulou I, et al. Carcinoembryonic antigen, neuron-specific enolase and cytokeratin fragment 19 (CYFRA 21–1) levels in induced sputum of lung cancer patients. Scand J Clin Lab Invest. 2008;68(7):542–7.
Sanguinetti CM, Riccioni G, Marchesani F, Pela R, Cecarini L. Bronchoalveolar lavage fluid level of carcinoembryonic antigen in the diagnosis of peripheral lung cancer. Monaldi Arch Chest Dis. 1995;50(3):177–82.
Farlow EC, Patel K, Basu S, Lee BS, Kim AW, Coon JS, et al. Development of a multiplexed tumor-associated autoantibody-based blood test for the detection of non-small cell lung cancer. Clin Cancer Res. 2010;16(13):3452–62.
Mattioni M, Chinzari P, Soddu S, Strigari L, Cilenti V, Mastropasqua E. Serum p53 antibody detection in patients with impaired lung function. BMC Cancer. 2013;13:62.
Szpechcinski A, Chorostowska-Wynimko J, Struniawski R, Kupis W, Rudzinski P, Langfort R, et al. Cell-free DNA levels in plasma of patients with non-small-cell lung cancer and inflammatory lung disease. Br J Cancer. 2015;113(3):476–83.
Pantel K, Brakenhoff RH, Brandt B. Detection, clinical relevance and specific biological properties of disseminating tumour cells. Nat Rev Cancer. 2008;8(5):329–40.
Ilie M, Hofman V, Long-Mira E, Selva E, Vignaud JM, Padovani B, et al. “Sentinel” circulating tumor cells allow early diagnosis of lung cancer in patients with chronic obstructive pulmonary disease. PLoS One. 2014;9(10):e111597.
Laniado-Laborin R. Smoking and chronic obstructive pulmonary disease (COPD). Parallel epidemics of the 21 century. Int J Environ Res Public Health. 2009;6(1):209–24.
Yang P, Sun Z, Krowka MJ, Aubry MC, Bamlet WR, Wampfler JA, et al. Alpha1-antitrypsin deficiency carriers, tobacco smoke, chronic obstructive pulmonary disease, and lung cancer risk. Arch Intern Med. 2008;168(10):1097–103.
Yang P, Bamlet WR, Sun Z, Ebbert JO, Aubry MC, Krowka MJ, et al. Alpha1-antitrypsin and neutrophil elastase imbalance and lung cancer risk. Chest. 2005;128(1):445–52.
Dialyna IA, Miyakis S, Georgatou N, Spandidos DA. Genetic polymorphisms of CYP1A1, GSTM1 and GSTT1 genes and lung cancer risk. Oncol Rep. 2003;10(6):1829–35.
Amos CI, Wu X, Broderick P, Gorlov IP, Gu J, Eisen T, et al. Genome-wide association scan of tag SNPs identifies a susceptibility locus for lung cancer at 15q25.1. Nat Genet. 2008;40(5):616–22.
Hung RJ, McKay JD, Gaborieau V, Boffetta P, Hashibe M, Zaridze D, et al. A susceptibility locus for lung cancer maps to nicotinic acetylcholine receptor subunit genes on 15q25. Nature. 2008;452(7187):633–7.
Du Y, Xue Y, Xiao W. Association of IREB2 gene rs2568494 polymorphism with risk of chronic obstructive pulmonary disease: a meta-analysis. Med Sci Monit. 2016;22:177–82.
Liu Y, Liu P, Wen W, James MA, Wang Y, Bailey-Wilson JE, et al. Haplotype and cell proliferation analyses of candidate lung cancer susceptibility genes on chromosome 15q24-25.1. Cancer Res. 2009;69(19):7844–50.
Young RP, Whittington CF, Hopkins RJ, Hay BA, Epton MJ, Black PN, et al. Chromosome 4q31 locus in COPD is also associated with lung cancer. Eur Respir J. 2010;36(6):1375–82.
Young RP, Hopkins RJ, Hay BA, Whittington CF, Epton MJ, Gamble GD. FAM13A locus in COPD is independently associated with lung cancer – evidence of a molecular genetic link between COPD and lung cancer. Appl Clin Genet. 2011;4:1–10.
Walser T, Cui X, Yanagawa J, Lee JM, Heinrich E, Lee G, et al. Smoking and lung cancer: the role of inflammation. Proc Am Thorac Soc. 2008;5(8):811–5.
Yang L, Yang X, Ji W, Deng J, Qiu F, Yang R, et al. Effects of a functional variant c.353T > C in snai1 on risk of two contextual diseases. Chronic obstructive pulmonary disease and lung cancer. Am J Respir Crit Care Med. 2014;189(2):139–48.
Belinsky SA, Palmisano WA, Gilliland FD, Crooks LA, Divine KK, Winters SA, et al. Aberrant promoter methylation in bronchial epithelium and sputum from current and former smokers. Cancer Res. 2002;62(8):2370–7.
Guzman L, Depix MS, Salinas AM, Roldan R, Aguayo F, Silva A, et al. Analysis of aberrant methylation on promoter sequences of tumor suppressor genes and total DNA in sputum samples: a promising tool for early detection of COPD and lung cancer in smokers. Diagn Pathol. 2012;7:87.
Lewis A, Riddoch-Contreras J, Natanek SA, Donaldson A, Man WD, Moxham J, et al. Downregulation of the serum response factor/miR-1 axis in the quadriceps of patients with COPD. Thorax. 2012;67(1):26–34.
Schetter AJ, Heegaard NH, Harris CC. Inflammation and cancer: interweaving microRNA, free radical, cytokine and p53 pathways. Carcinogenesis. 2010;31(1):37–49.
Williams AE, Perry MM, Moschos SA, Larner-Svensson HM, Lindsay MA. Role of miRNA-146a in the regulation of the innate immune response and cancer. Biochem Soc Trans. 2008;36(Pt 6):1211–5.
Makita H, Nasuhara Y, Nagai K, Ito Y, Hasegawa M, Betsuyaku T, et al. Characterisation of phenotypes based on severity of emphysema in chronic obstructive pulmonary disease. Thorax. 2007;62(11):932–7.
Petrache I, Fijalkowska I, Zhen L, Medler TR, Brown E, Cruz P, et al. A novel antiapoptotic role for alpha1-antitrypsin in the prevention of pulmonary emphysema. Am J Respir Crit Care Med. 2006;173(11):1222–8.
de Torres JP, Marin JM, Casanova C, Cote C, Carrizo S, Cordoba-Lanus E, et al. Lung cancer in patients with chronic obstructive pulmonary disease– incidence and predicting factors. Am J Respir Crit Care Med. 2011;184(8):913–9.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Gan WQ, Man SF, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax. 2004;59(7):574–80.
Lee KY, Ho SC, Chan YF, Wang CH, Huang CD, Liu WT, et al. Reduced nuclear factor-kappaB repressing factor: a link toward systemic inflammation in COPD. Eur Respir J. 2012;40(4):863–73.
Ito K, Ito M, Elliott WM, Cosio B, Caramori G, Kon OM, et al. Decreased histone deacetylase activity in chronic obstructive pulmonary disease. N Engl J Med. 2005;352(19):1967–76.
Parimon T, Chien JW, Bryson CL, McDonell MB, Udris EM, Au DH. Inhaled corticosteroids and risk of lung cancer among patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2007;175(7):712–9.
Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–89.
Hussain SP, Hofseth LJ, Harris CC. Radical causes of cancer. Nat Rev Cancer. 2003;3(4):276–85.
Gaziano JM, Glynn RJ, Christen WG, Kurth T, Belanger C, MacFadyen J, et al. Vitamins E and C in the prevention of prostate and total cancer in men: the Physicians’ Health Study II randomized controlled trial. JAMA. 2009;301(1):52–62.
Lee IM, Cook NR, Gaziano JM, Gordon D, Ridker PM, Manson JE, et al. Vitamin E in the primary prevention of cardiovascular disease and cancer: the Women’s Health Study: a randomized controlled trial. JAMA. 2005;294(1):56–65.
van Zandwijk N, Dalesio O, Pastorino U, de Vries N, van Tinteren H. EUROSCAN, a randomized trial of vitamin A and N-acetylcysteine in patients with head and neck cancer or lung cancer. For the EUropean Organization for Research and Treatment of Cancer Head and Neck and Lung Cancer Cooperative Groups. J Natl Cancer Inst. 2000;92(12):977–86.
Jackson AL, Zhou B, Kim WY. HIF, hypoxia and the role of angiogenesis in non-small cell lung cancer. Expert Opin Ther Targets. 2010;14(10):1047–57.
Giatromanolaki A, Koukourakis MI, Sivridis E, Turley H, Talks K, Pezzella F, et al. Relation of hypoxia inducible factor 1 alpha and 2 alpha in operable non-small cell lung cancer to angiogenic/molecular profile of tumours and survival. Br J Cancer. 2001;85(6):881–90.
Kim WY, Perera S, Zhou B, Carretero J, Yeh JJ, Heathcote SA, et al. HIF2alpha cooperates with RAS to promote lung tumorigenesis in mice. J Clin Invest. 2009;119(8):2160–70.
Kaya A, Ciledag A, Gulbay BE, Poyraz BM, Celik G, Sen E, et al. The prognostic significance of vascular endothelial growth factor levels in sera of non-small cell lung cancer patients. Respir Med. 2004;98(7):632–6.
Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355(24):2542–50.
Kasahara Y, Tuder RM, Taraseviciene-Stewart L, Le Cras TD, Abman S, Hirth PK, et al. Inhibition of VEGF receptors causes lung cell apoptosis and emphysema. J Clin Invest. 2000;106(11):1311–9.
Kranenburg AR, de Boer WI, Alagappan VK, Sterk PJ, Sharma HS. Enhanced bronchial expression of vascular endothelial growth factor and receptors (Flk-1 and Flt-1) in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(2):106–13.
Punturieri A, Szabo E, Croxton TL, Shapiro SD, Dubinett SM. Lung cancer and chronic obstructive pulmonary disease: needs and opportunities for integrated research. J Natl Cancer Inst. 2009;101(8):554–9.
Houghton AM, Rzymkiewicz DM, Ji H, Gregory AD, Egea EE, Metz HE, et al. Neutrophil elastase-mediated degradation of IRS-1 accelerates lung tumor growth. Nat Med. 2010;16(2):219–23.
Vignola AM, Riccobono L, Mirabella A, Profita M, Chanez P, Bellia V, et al. Sputum metalloproteinase-9/tissue inhibitor of metalloproteinase-1 ratio correlates with airflow obstruction in asthma and chronic bronchitis. Am J Respir Crit Care Med. 1998;158(6):1945–50.
Linder R, Ronmark E, Pourazar J, Behndig A, Blomberg A, Lindberg A. Serum metalloproteinase-9 is related to COPD severity and symptoms – cross-sectional data from a population based cohort-study. Respir Res. 2015;16:28.
Nozawa H, Chiu C, Hanahan D. Infiltrating neutrophils mediate the initial angiogenic switch in a mouse model of multistage carcinogenesis. Proc Natl Acad Sci U S A. 2006;103(33):12493–8.
Minn AJ, Gupta GP, Siegel PM, Bos PD, Shu W, Giri DD, et al. Genes that mediate breast cancer metastasis to lung. Nature. 2005;436(7050):518–24.
D’Armiento J, Dalal SS, Okada Y, Berg RA, Chada K. Collagenase expression in the lungs of transgenic mice causes pulmonary emphysema. Cell. 1992;71(6):955–61.
Joos L, He JQ, Shepherdson MB, Connett JE, Anthonisen NR, Pare PD, et al. The role of matrix metalloproteinase polymorphisms in the rate of decline in lung function. Hum Mol Genet. 2002;11(5):569–76.
Hunninghake GM, Cho MH, Tesfaigzi Y, Soto-Quiros ME, Avila L, Lasky-Su J, et al. MMP12, lung function, and COPD in high-risk populations. N Engl J Med. 2009;361(27):2599–608.
Houghton AM, Grisolano JL, Baumann ML, Kobayashi DK, Hautamaki RD, Nehring LC, et al. Macrophage elastase (matrix metalloproteinase-12) suppresses growth of lung metastases. Cancer Res. 2006;66(12):6149–55.
Magnussen H, Watz H, Kirsten A, Wang M, Wray H, Samuelsson V, et al. Safety and tolerability of an oral MMP-9 and −12 inhibitor, AZD1236, in patients with moderate-to-severe COPD: a randomised controlled 6-week trial. Pulm Pharmacol Ther. 2011;24(5):563–70.
Shepherd FA, Sridhar SS. Angiogenesis inhibitors under study for the treatment of lung cancer. Lung Cancer. 2003;41 Suppl 1:S63–72.
Hirsh L, Dantes A, Suh BS, Yoshida Y, Hosokawa K, Tajima K, et al. Phosphodiesterase inhibitors as anti-cancer drugs. Biochem Pharmacol. 2004;68(6):981–8.
Greenhough A, Smartt HJ, Moore AE, Roberts HR, Williams AC, Paraskeva C, et al. The COX-2/PGE2 pathway: key roles in the hallmarks of cancer and adaptation to the tumour microenvironment. Carcinogenesis. 2009;30(3):377–86.
Mao JT, Roth MD, Fishbein MC, Aberle DR, Zhang ZF, Rao JY, et al. Lung cancer chemoprevention with celecoxib in former smokers. Cancer Prev Res (Phila). 2011;4(7):984–93.
Reckamp KL, Koczywas M, Cristea MC, Dowell JE, Wang HJ, Gardner BK, et al. Randomized phase 2 trial of erlotinib in combination with high-dose celecoxib or placebo in patients with advanced non-small cell lung cancer. Cancer. 2015;121(18):3298–306.
Roh GS, Yi CO, Cho YJ, Jeon BT, Nizamudtinova IT, Kim HJ, et al. Anti-inflammatory effects of celecoxib in rat lungs with smoke-induced emphysema. Am J Physiol Lung Cell Mol Physiol. 2010;299(2):L184–91.
Keith RL, Miller YE, Hudish TM, Girod CE, Sotto-Santiago S, Franklin WA, et al. Pulmonary prostacyclin synthase overexpression chemoprevents tobacco smoke lung carcinogenesis in mice. Cancer Res. 2004;64(16):5897–904.
Lange A, Gustke H, Glassmeier G, Heine M, Zangemeister-Wittke U, Schwarz JR, et al. Neuronal differentiation by indomethacin and IBMX inhibits proliferation of small cell lung cancer cells in vitro. Lung Cancer. 2011;74(2):178–87.
Schuller HM, Plummer 3rd HK, Bochsler PN, Dudric P, Bell JL, Harris RE. Co-expression of beta-adrenergic receptors and cyclooxygenase-2 in pulmonary adenocarcinoma. Int J Oncol. 2001;19(3):445–9.
Lee SU, Ahn KS, Sung MH, Park JW, Ryu HW, Lee HJ, et al. Indacaterol inhibits tumor cell invasiveness and MMP-9 expression by suppressing IKK/NF-kappaB activation. Mol Cells. 2014;37(8):585–91.
Zhao Q, Gu X, Zhang C, Lu Q, Chen H, Xu L. Blocking M2 muscarinic receptor signaling inhibits tumor growth and reverses epithelial-mesenchymal transition (EMT) in non-small cell lung cancer (NSCLC). Cancer Biol Ther. 2015;16(4):634–43.
Zhao Q, Yue J, Zhang C, Gu X, Chen H, Xu L. Inactivation of M2 AChR/NF-kappaB signaling axis reverses epithelial-mesenchymal transition (EMT) and suppresses migration and invasion in non-small cell lung cancer (NSCLC). Oncotarget. 2015;6(30):29335–46.
Lin G, Sun L, Wang R, Guo Y, Xie C. Overexpression of muscarinic receptor 3 promotes metastasis and predicts poor prognosis in non-small-cell lung cancer. J Thorac Oncol. 2014;9(2):170–8.
Xu R, Shang C, Zhao J, Han Y, Liu J, Chen K, et al. Activation of M3 muscarinic receptor by acetylcholine promotes non-small cell lung cancer cell proliferation and invasion via EGFR/PI3K/AKT pathway. Tumour Biol. 2015;36(6):4091–100.
Zhang S, Togo S, Minakata K, Gu T, Ohashi R, Tajima K, et al. Distinct roles of cholinergic receptors in small cell lung cancer cells. Anticancer Res. 2010;30(1):97–106.
Hua N, Wei X, Liu X, Ma X, He X, Zhuo R, et al. A novel muscarinic antagonist R2HBJJ inhibits non-small cell lung cancer cell growth and arrests the cell cycle in G0/G1. PLoS One. 2012;7(12), e53170.
Hashimoto N, Matsuzaki A, Okada Y, Imai N, Iwano S, Wakai K, et al. Clinical impact of prevalence and severity of COPD on the decision-making process for therapeutic management of lung cancer patients. BMC Pulm Med. 2014;14:14.
Lugg ST, Agostini PJ, Tikka T, Kerr A, Adams K, Bishay E, et al. Long-term impact of developing a postoperative pulmonary complication after lung surgery. Thorax. 2016;71(2):171–6.
Kobayashi S, Suzuki S, Niikawa H, Sugawara T, Yanai M. Preoperative use of inhaled tiotropium in lung cancer patients with untreated COPD. Respirology. 2009;14(5):675–9.
Sekine Y, Suzuki H, Yamada Y, Koh E, Yoshino I. Severity of chronic obstructive pulmonary disease and its relationship to lung cancer prognosis after surgical resection. Thorac Cardiovasc Surg. 2013;61(2):124–30.
Kuo CH, Wu CY, Lee KY, Lin SM, Chung FT, Lo YL, et al. Chronic obstructive pulmonary disease in stage I non-small cell lung cancer that underwent anatomic resection: the role of a recurrence promoter. COPD. 2014;11(4):407–13.
Putila J, Guo NL. Combining COPD with clinical, pathological and demographic information refines prognosis and treatment response prediction of non-small cell lung cancer. PLoS One. 2014;9(6), e100994.
Izquierdo JL, Resano P, El Hachem A, Graziani D, Almonacid C, Sanchez IM. Impact of COPD in patients with lung cancer and advanced disease treated with chemotherapy and/or tyrosine kinase inhibitors. Int J Chron Obstruct Pulmon Dis. 2014;9:1053–8.
Lim JU, Yeo CD, Rhee CK, Kim YH, Park CK, Kim JS, et al. Chronic obstructive pulmonary disease-related non-small-cell lung cancer exhibits a low prevalence of EGFR and ALK driver mutations. PLoS One. 2015;10(11), e0142306.
Schiavon M, Marulli G, Nannini N, Pasello G, Lunardi F, Balestro E, et al. COPD-related adenocarcinoma presents low aggressiveness morphological and molecular features compared to smoker tumours. Lung Cancer. 2014;86(3):311–7.
de Boer WI, Hau CM, van Schadewijk A, Stolk J, van Krieken JH, Hiemstra PS. Expression of epidermal growth factors and their receptors in the bronchial epithelium of subjects with chronic obstructive pulmonary disease. Am J Clin Pathol. 2006;125(2):184–92.
Woodruff PG, Wolff M, Hohlfeld JM, Krug N, Dransfield MT, Sutherland ER, et al. Safety and efficacy of an inhaled epidermal growth factor receptor inhibitor (BIBW 2948 BS) in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;181(5):438–45.
Inoue T, Shiomi H, Oh RJ. Stereotactic body radiotherapy for Stage I lung cancer with chronic obstructive pulmonary disease: special reference to survival and radiation-induced pneumonitis. J Radiat Res. 2015;56(4):727–34.
Kimura T, Togami T, Takashima H, Nishiyama Y, Ohkawa M, Nagata Y. Radiation pneumonitis in patients with lung and mediastinal tumours: a retrospective study of risk factors focused on pulmonary emphysema. Br J Radiol. 2012;85(1010):135–41.
Takeda A, Kunieda E, Ohashi T, Aoki Y, Oku Y, Enomoto T, et al. Severe COPD is correlated with mild radiation pneumonitis following stereotactic body radiotherapy. Chest. 2012;141(4):858–66.
Ishijima M, Nakayama H, Itonaga T, Tajima Y, Shiraishi S, Okubo M, et al. Patients with severe emphysema have a low risk of radiation pneumonitis following stereotactic body radiotherapy. Br J Radiol. 2015;88(1046):20140596.
Grumelli S, Corry DB, Song LZ, Song L, Green L, Huh J, et al. An immune basis for lung parenchymal destruction in chronic obstructive pulmonary disease and emphysema. PLoS Med. 2004;1(1), e8.
Mantovani A, Sozzani S, Locati M, Allavena P, Sica A. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol. 2002;23(11):549–55.
Whiteside TL. Immune suppression in cancer: effects on immune cells, mechanisms and future therapeutic intervention. Semin Cancer Biol. 2006;16(1):3–15.
Calles A, Liao X, Sholl LM, Rodig SJ, Freeman GJ, Butaney M, Lydon C, Dahlberg SE, Hodi FS, Oxnard GR, Jackman DM, Jänne PA. Expression of PD-1 and Its Ligands, PD-L1 and PD-L2, in smokers and never smokers with KRAS-Mutant Lung Cancer. J Thorac Oncol. 2015;10(12):1726–35. doi:10.1097/JTO.0000000000000687.
Yang Y, Pang Z, Ding N, Dong W, Ma W, Li Y, Du J, Liu Q. The efficacy and potential predictive factors of PD-1/PD-L1 blockades in epithelial carcinoma patients: a systematic review and meta analysis. Oncotarget. 2016. doi:10.18632/oncotarget.11291.
Kalathil SG, Lugade AA, Pradhan V, Miller A, Parameswaran GI, Sethi S, et al. T-regulatory cells and programmed death 1+ T cells contribute to effector T-cell dysfunction in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2014;190(1):40–50.
Yap KL, Ada GL, McKenzie IF. Transfer of specific cytotoxic T lymphocytes protects mice inoculated with influenza virus. Nature. 1978;273(5659):238–9.
Topham DJ, Tripp RA, Doherty PC. CD8+ T cells clear influenza virus by perforin or Fas-dependent processes. J Immunol. 1997;159(11):5197–200.
Diel R, Loddenkemper R, Meywald-Walter K, Niemann S, Nienhaus A. Predictive value of a whole blood IFN-gamma assay for the development of active tuberculosis disease after recent infection with Mycobacterium tuberculosis. Am J Respir Crit Care Med. 2008;177(10):1164–70.
Mylonaki E, Manika K, Zarogoulidis P, Domvri K, Voutsas V, Zarogoulidis K, et al. In vivo synergistic cytogenetic effects of aminophylline on lymphocyte cultures from patients with lung cancer undergoing chemotherapy. Mutat Res. 2012;740(1–2):1–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media Singapore
About this chapter
Cite this chapter
Togo, S., Namba, Y., Takahashi, K. (2017). Association of COPD and Lung Cancer: How Does COPD Management Change the Outcome of Treatment of Lung Cancer?. In: Nakamura, H., Aoshiba, K. (eds) Chronic Obstructive Pulmonary Disease. Respiratory Disease Series: Diagnostic Tools and Disease Managements. Springer, Singapore. https://doi.org/10.1007/978-981-10-0839-9_18
Download citation
DOI: https://doi.org/10.1007/978-981-10-0839-9_18
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-0838-2
Online ISBN: 978-981-10-0839-9
eBook Packages: MedicineMedicine (R0)