Abstract
En bloc resection of iliosacral sarcomas is a surgical challenge. Eight percent to 25% of posterior pelvic tumors may have sacral extension [1–3]. Tumors extending slightly into the sacrum or tumor mass covering IS joint may be excised with an osteotomy through the lateral sacral mass, whereas resection of tumors involving sacral nerves and vertebrae or the lumber spine is more complex. The complex local anatomy and the surgeon’s desire to protect neural function may increase the likelihood of inadvertent tumor penetration [4, 5].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
En bloc resection of iliosacral sarcomas is a surgical challenge. Eight percent to 25% of posterior pelvic tumors may have sacral extension [1,2,3]. Tumors extending slightly into the sacrum or tumor mass covering IS joint may be excised with an osteotomy through the lateral sacral mass, whereas resection of tumors involving sacral nerves and vertebrae or the lumber spine is more complex. The complex local anatomy and the surgeon’s desire to protect neural function may increase the likelihood of inadvertent tumor penetration [4, 5].
Detailed surgical planning is extremely important for iliosacral tumor resection. A multidisciplinary approach should be considered due to visceral involvement. Despite the emphasis on individualized surgical planning, a standardization in surgical management can facilitate surgical planning and procedures. The conventional Enneking classification of pelvic tumors has been useful for the resection of tumors located in the innominate bone. Based on the tumor location and the planned osteotomy site, the authors’ institution proposes a novel categorization system for pelvic tumors with sacral invasion, standardized surgical procedures, as well as reconstructive methods.
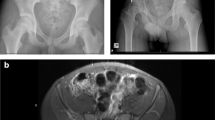
Differing from the classification designed for tumors localized in the sacrum, the system (Table 9.1 and Fig. 9.1) was devised based on the sagittal extent of sacral invasion rather than the transverse level of sacral invasion of the tumor. Type P-s (abbreviation for “pelvic tumor with sacral invasion”) I resection refers to osteotomy through the ipsilateral sacral wing when the tumor only invades the adjacent sacroiliac joint. Type P-s II resection refers to osteotomy through the sacral midline when the tumor invades the ipsilateral sacral foramina. Type P-s III resection refers to osteotomy through the contralateral sacral wing when the tumor invades the contralateral sacral foramina. And type P-s IV resection refers to osteotomy through the contralateral iliac wing when the tumor invades the contralateral sacroiliac joint. Meanwhile, the extent of invasion to the innominate bone is categorized as type “a” when confined to the iliac wing or type “b” when there is invasion in the periacetabular region. The combined approach is usually planned for type P-s II, III, and IV resection (Fig. 9.2).
Depending on whether the ipsilateral sacral nerve foramen is involved, combined approaches or single lateral approach is used. The margin on sacral side is technique demanding and paramount in type IV resection. For the cases in which the sacral foramen or sacral canal is free of tumor invading, the tumor resection can be completed through one semimobile lateral decubitus position. Extended ilioinguinal incision is normally used, and the retroperitoneal space is first exposed. The plane between the iliacus and psoas muscle is developed. The iliacus muscle is transected through its substance. A large posterior gluteal myocutaneous flap is developed, and this allows exposure of the sciatic notch. A Gigli saw is then introduced through the sciatic notch, and ilium osteotomy is performed. Another Gigli saw is placed medial to the iliosacral joint. The lumbosacral trunk, iliac vessels, and ureter should be retracted medially and carefully protected. The osteotomy is then performed through ipsilateral sacral ala lateral to sacral foramen. Part of ilium and whole iliosacral joint is then resected, similar margin on sacral side as that of extended hemipelvectomy. In the circumstance of sacral foramen being involved, single-stage combined approaches should be used (Fig. 9.3). First, the prone position is adopted. A midline incision with one or two caudal branches extending along gluteal maximum is shaped into a curve or reversed Y for the posterior approach to lower lumbar spine and sacrum. The gluteus maximus myocutaneous is developed, and erector spinae are detached from the insertion on sacrum. The sacral nerve roots and dura within the sacral canal are exposed by a laminectomy. Ligation of the ipsilateral S1–S3 nerve roots is obligatory, while the contralateral nerve roots are preferably preserved. The ipsilateral facet joint and accessory articulation of L5–S1 are resected, along with partial intervertebral disc resection. The presacral space is packed with moist gauze so that the vessels and rectum can be pushed away from the anterior surface of the sacrum. By retracting the severed nerve roots and ligated dural sac to the counter lateral side, sagittal vertebrectomy can be performed posteriorly. The wound is closed temporally with continuous suture. Then the patient is placed in lateral decubitus position. Similar procedure is performed as that of standard type IV resection. The ipsilateral half-discectomy of L5–S1 is performed, and sagittal sacral osteotomy through midline is carried out to complete osteotomy. Then the extended type IV resection is completed.
Farid [4] introduced a method to improve the accuracy of osteotomy for iliosacral tumor resection. High-speed burr was used to perform the osteotomy. At the authors’ institution, an ultrasonic osteotome was usually used to perform precise osteotomies. In the prone position, a midline posterior incision and sacral laminectomy allow exposure of sacral roots. The ventral foramina are located directly anterior to the dorsal foramina. A sacral osteotomy begins by dividing the posterior sacral cortex using Kerrison rongeur. The dura and involved nerve roots were ligated. Division of involved roots allows dural retraction and facilitates the vertical osteotomy. This is followed by the cranial osteotomy. If tumor extension spares the upper part of the lateral mass of S1 and the base of the articular process, an oblique cranial osteotomy is performed to preserve lumbosacral stability. Ultrasonic osteotome is used to finalize the osteotomy down to the anterior cortex. Sacral depth substantially increases in the midline in S1 particularly in the promontory. If the tumor extends into the body of S1, the vertical osteotomy should extend cranially to the tip of the sacral promontory. Then transverse division of the L5–S1 disc and the facet joint is performed. The superior end plate of S1 is divided vertically to join the vertical osteotomy at the promontory. This osteotomy destabilizes the lumbosacral articulation and may require instrumentation and fusion. Finally, the osteotomy surrounds the tumor caudally.
References
Aydinli U, Akesen B, Yalcinkaya U, Hakyemez B, Serifoglu R. Iliosacral fixation after type-1 hemipelvectomy: a novel technique. Acta Orthop Belg. 2012;78(3):393–7.
Guo W, Sun X, Ji T, Tang X. Outcome of surgical treatment of pelvic osteosarcoma. J Surg Oncol. 2012;106(4):406–10.
Ieguchi M, Hoshi M, Takada J, Hidaka N, Nakamura H. Navigation-assisted surgery for bone and soft tissue tumors with bony extension. Clin Orthop Relat Res. 2012;470(1):275–83.
Farid YR. Decancellation sacral osteotomy in iliosacral tumor resection: a technique for precise sacral margins. Clin Orthop Relat Res. 2010;468(5):1362–72.
Witte D, Bernd L, Bruns J, Gosheger G, Hardes J, Hartwig E, et al. Limb-salvage reconstruction with MUTARS hemipelvic endoprosthesis: a prospective multicenter study. Eur J Surg Oncol. 2009;35(12):1318–25.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature B.V.
About this chapter
Cite this chapter
Ji, T., Guo, W. (2020). Combined Approach for Iliosacral Tumor Resection. In: Guo, W., Hornicek, F., Sim, F. (eds) Surgery of the Pelvic and Sacral Tumor. Springer, Dordrecht. https://doi.org/10.1007/978-94-024-1945-0_9
Download citation
DOI: https://doi.org/10.1007/978-94-024-1945-0_9
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-024-1943-6
Online ISBN: 978-94-024-1945-0
eBook Packages: MedicineMedicine (R0)