Abstract
Primary malignant sacral tumors, including chordoma, chondrosarcoma, and osteosarcoma, are relatively resistant to radiotherapy. Therefore, wide resection with an adequate margin is the only effective way to achieve better local control and cure the patient. Sacrectomy is a major challenge for oncology surgeons, however, due to the complex anatomy and massive bleeding that may occur during the operation. Surgery is generally performed in one or two stages using a combined anterior and posterior approach. To minimize the surgical duration, we initially performed total sacrectomy using a one-stage combined anterior and posterior approach. Based on our accumulated clinical experience and an improved understanding of the pelvic anatomy, we now perform total en bloc sacrectomy using a posterior-only approach. In this chapter, we introduce our experience with sacrectomy using a one-stage combined anterior and posterior approach as well as a posterior-only approach.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Combined Anterior and Posterior Approach
While primary sacral tumors are not common, chordoma and giant cell tumor are the two most common tumor types involving the sacrum. Satisfactory local control of sacral tumors is difficult to achieve due to the anatomic complexity, massive intraoperative bleeding, and challenges realizing adequate margins in this region. Wide resection with a safe margin is the only practical approach to achieve the best local control and cure the disease for patients with primary malignant sacral tumors.
Very few studies have addressed total sacrectomy, for which the most common procedure is a two-stage operation using a combined anterior and posterior approach. In the two-stage operation, the bilateral internal iliac arteries are mobilized from the sacrum by ligating the branches of the iliac vessels, and the soft tissue in front of the tumor is dissected to facilitate resection of the L5–S1 disc using an anterior approach by laparoscopic or open surgery. The total sacrum is then removed using a posterior approach. The two surgical stages are usually performed a few weeks apart. Intra-abdominal surgery often leads to intestinal obstruction. To address these issues, we performed total sacrectomy with a one-stage operation that was achieved using a combined anterior and posterior approach. In this chapter, we describe this surgical procedure carried out in our center.
The indication for one-stage total sacrectomy is malignant sacral tumors invading S1–S2. The relative indication for this procedure is a giant cell tumor extensively invading S1–S5.
Surgical procedure: Bilateral ilioinguinal incisions are made to visualize the retroperitoneal space. The bilateral iliac vessels are mobilized from the sacrum by ligating the branches of the iliac vessels. Soft tissue in front of the tumor is dissected away, and the L5–S1 disc is resected as much as possible. After identifying the upper and lower edge of the sacroiliac joint, two ends of a plastic tube are introduced from anterior to posterior with a thick needle. A wire saw is then passed through the tube to accomplish the osteotomy from the outer edge of the sacroiliac joint via the posterior approach (Fig. 27.1).
(a–c) Schematic diagram of surgical procedure for one-stage total sacrectomy (a) Coronal view revealing the mobilization of the bilateral iliac vessels from the sacrum after ligation of the branches of the iliac vessels. (b) Frontal view revealing application of the silicone tube from the anterior to posterior aspect of the sacrum. (c) Dorsal view showing the passage of the wire saw though the silicone tube
A longitudinal midline incision is made in the posterior approach. The gluteus maximus muscles and parasacral muscles are dissected away, and the lamina and spinal process of L4–L5, posterior aspect of the sacrum, and bilateral sacroiliac joints are visualized. Four transpedicle screws are inserted into the L4 and L5 vertebrae before resection of the sacrum. After visualizing the posterior aspect of the sacrum, the anterior aspect of the sacrum is dissected from the surrounding tissue. The rectum is identified from the posterior approach after resection of the sacrotuberous ligament, sacrospinous ligament, and sacrococcygeal ligament. The rectum is carefully separated and gauze packed into the space between the rectum and anterior aspect of the sacral tumor to push the rectum forward so that the integrity of the rectum is maintained during tumor dissection. The inferior articular process of L5 and the lamina above the tumor are resected, and the bilateral L5 nerve roots and dura sac are carefully preserved. Osteotomies of the bilateral iliac bone are performed along the outer edge of the sacroiliac joints with wire saws passed through the silicone tubes that were placed during the anterior approach. The sacrum is resected at the level of the L5–S1 disc, and then the whole sacrum is removed (Fig. 27.2).
(a–e) A male patient with malignant peripheral nerve sheath tumor involving the sacrum treated with total sacrectomy. (a) Plain film revealing osteolysis in the sacrum. (b) CT image revealing a soft tissue mass and destruction of the sacrum. (c) Abdominal incision used in the patient. (d) Removal of the whole sacrum and L5 vertebra. (e) Plain film revealing reconstruction of lumbosacral stability after resection
After total sacrectomy, four pedical screws are placed into the residual ilium, and two or four rods are applied to connect the screws in the ipsilateral lumbar region and ilium. Complex reconstruction with a screw-rod system and a fibular bone graft is preferred for young patients.
2 The Single Posterior Approach
Before performing total en bloc sacrectomy using a posterior-only approach, the surgeon must consider three major issues: (1) carrying out an osteotomy through the ilium without injuring the viscera, lumbosacral trunk, and bilateral iliac vessels; (2) mobilizing the internal iliac vessels from the soft tissue anterior to the tumor; and (3) excising the L5–S1 disc without injuring the surrounding vital vessels attached tightly to the L5 vertebrae.
Indications for total en bloc sacrectomy using a posterior-only approach in our center are (1) primary malignant sacral tumor with S1–S2 involvement; (2) tumor not involving the internal iliac vessels and bowel, evaluated by imaging studies and digital rectal examination; and (3) recurrent sacral tumors without a history of an anterior procedure.
Surgical procedure: Prior to surgery, the main arteries feeding the sacral tumor are selectively embolized by the radiologist. The arteries are embolized based on the blood supply to the sacrum to occlude the middle sacral, iliolumbar, and lateral sacral arteries. The bilateral internal iliac arteries are not commonly embolized. After preoperative embolization, the patient is taken directly to the operation room, receives general anesthesia, and is placed in a supine position, and an aortic balloon is inserted into the abdominal aorta by femoral access. The aortic balloon is inflated during the tumor resection to reduce intraoperative blood loss. We recently described this technique, and it is performed in patients with large sacral tumors requiring extensive dissection. The patient is then moved into a prone position. An inverted “Y” incision is applied to reveal the posterior aspect of the sacrum and the adjacent ilium. A posterior longitudinal midline incision is made in the lumbosacral region, and two other incisions are made beginning from the end of the midline incision and going along the fibers of the gluteus maximus muscle. To reveal the posterior aspect of the bilateral ilium and the sacrum, and the spinal process and lamina of L4–L5, the gluteus and the parasacral muscles are carefully dissected away. Before resection of the sacrum tumor, four pedicle screws are placed into the L4 and L5 pedicles. After revealing the posterior aspect of the sacrum, the anterior aspect is separated. Visualization of the rectum is achieved after resecting the sacrotuberous, the sacrospinous, and the sacrococcygeal ligaments. The rectum is carefully separated, and gauze is packed into the space between the rectum and anterior aspect of the sacral tumor to push the rectum forward to maintain the integrity of the rectum during the tumor dissection (Fig. 27.3). The inferior articular process of L5 and the lamina above the tumor are resected, and the bilateral L5 nerve roots and dura sac are carefully preserved. Ligation and division of the dura sac below L5 are then performed. Resection of the L5–S1 disc is carried out using a posterior approach. Excision of the bilateral transverse processes of L5 is necessary so that blunt dissection from the lower and upper edge of the sacroiliac joints can be achieved. To maintain the integrity of the internal iliac vessels and lumbosacral trunks during the osteotomy, the internal iliac vessels and lumbosacral trunks are pushed away from the iliac osteotomy lines by packing gauze in front of the sacroiliac joints. After identifying the lower and upper edges of the sacroiliac joint, a silicone tube is placed in the anterior aspect of the sacroiliac joint. A wire saw is passed through the tube to achieve the osteotomy along the outer edge of the sacroiliac joints with an adequate margin. After osteotomy of the bilateral ilium, the sacrum can be easily lifted up, which may facilitate the visualization of the sacral nerves, lumbosacral trunks, rectum, and iliac vessels. The branches of the internal iliac vessels to the sacrum and the middle sacral artery are identified and ligated. The anterior aspect of the tumor is carefully dissected, and the sacral nerve roots are resected. The total sacrum is then removed (Fig. 27.4).
(a and b) Schematic diagram of the operation procedure for total en bloc sacrectomy. (a) Blunt dissection by fingers from the lower and upper edge of the sacroiliac joint. (b) Application of the silicone tube in the anterior space of the sacroiliac joint and passage of the wire saw though the silicone tube
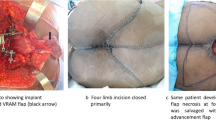
A female patient with sacral osteosarcoma involving S1–S5 treated with total sacrectomy. (a) The patient was placed on the supine position and an inverted “Y” incision was used. (b) Magnetic resonance image showing low signal intensity on T1WI in the sacrum. (c) CT image showing a soft tissue mass resulting in the destruction of the sacrum. (d) Image of the entire sacrum. (e) Plain film showing the reconstruction of the lumbosacral stability after total sacrectomy
After total sacrectomy, four pedical screws are placed into the residual ilium, and two or four rods are applied to connect the screws in the ipsilateral lumbar region and ilium. Complex reconstruction with a screw-rod system and a fibular bone graft is preferred for young patients. We recently performed reconstruction with a 3D-printed custom-made prosthesis after the tumor resection (Fig. 27.5).
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature B.V.
About this chapter
Cite this chapter
Zang, J., Guo, W. (2020). One-Stage Total Sacrectomy. In: Guo, W., Hornicek, F., Sim, F. (eds) Surgery of the Pelvic and Sacral Tumor. Springer, Dordrecht. https://doi.org/10.1007/978-94-024-1945-0_27
Download citation
DOI: https://doi.org/10.1007/978-94-024-1945-0_27
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-024-1943-6
Online ISBN: 978-94-024-1945-0
eBook Packages: MedicineMedicine (R0)