Abstract
Trypanosomatid parasites are a group of flagellated protozoa that includes the genera Leishmania and Trypanosoma, which are the causative agents of diseases (leishmaniases, sleeping sickness and Chagas disease) that cause considerable morbidity and mortality, affecting more than 27 million people worldwide. Today no effective vaccines for the prevention of these diseases exist, whereas current chemotherapy is ineffective, mainly due to toxic side effects of current drugs and to the emergence of drug resistance and lack of cost effectiveness. For these reasons, rational drug design and the search of good candidate drug targets is of prime importance. The search for drug targets requires a multidisciplinary approach. To this end, the completion of the genome project of many trypanosomatid species gives a vast amount of new information that can be exploited for the identification of good drug candidates with a prediction of “druggability” and divergence from mammalian host proteins. In addition, an important aspect in the search for good drug targets is the “target identification” and evaluation in a biological pathway, as well as the essentiality of the gene in the mammalian stage of the parasite, which is provided by basic research and genetic and proteomic approaches. In this chapter we will discuss how these bioinformatic tools and experimental evaluations can be integrated for the selection of candidate drug targets, and give examples of metabolic and signaling pathways in the parasitic protozoa that can be exploited for rational drug design.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Trypanosomatid protozoan parasites of the genera Trypanosoma and Leshmania are infectious agents of important diseases, such as human African trypanosomiasis (HAT or sleeping sickness), Chagas disease and leishmaniases (cutaneous, mucocutaneous and visceral). According to the World Health Organization (WHO), the leishmaniases are endemic in 88 countries, with 350 million people being at risk of acquiring the infection, sleeping sickness occurs in sub-Saharan Africa and threatens more than 60 million people and Chagas disease is prevalent in Latin America and more than 25 million people are at risk of acquiring the infection. Together, these three parasitic diseases represent a huge social and economic burden since approximately 0.5 million people are infected with T. brucei, ten million with T. cruzi and an estimated 12 million with different species of Leishmania (Teixeira et al. 2012), and cause approximately 150,000 deaths annually (Nussbaum et al. 2010).
Since there are no human vaccines yet, the only treatment for these diseases relies solely on chemotherapeutic drugs. For HAT, the first-line treatment for second-stage cases is melarsoprol, a toxic drug in use since 1949. Increase in drug resistance and high therapeutic failure rates have been reported recently in several foci (Robays et al. 2008). Eflornithine is an alternative treatment that is better tolerated, but difficult to administer (Burri and Brun 2003). Nifurtimox, an orally administered cheap drug, has many side effects and is not yet fully validated for use in HAT (Legros et al. 2002). For the treatment of Chagas disease there are two drugs available, benznidazole and nifurtimox, which are highly toxic and ineffective in the chronic phase of infection (Castro and Diaz de Toranzo 1988). For the treatment of leishmaniases, the mostly widely prescribed drug discovered, the pentavalent antimony, was discovered almost a century ago and has various limitations, including serious side effects, prolonged course of treatment and emergence of drug resistance (Croft et al. 2006). Although newer treatments for leishmaniases exist, they are not optimal (Singh et al. 2012). Overall, current chemotherapy for trypanosomatid parasitic diseases has the pre-mentioned serious limitations, including high toxicity, low efficacy, high cost and increasing parasitic resistance. Therefore there is an urgent need to discover new drugs for the treatment of these devastating diseases.
There are several strategies for expanding the repertoire of new antiparasitic agents. Amongst these, one of the most attractive is targeted drug discovery, because in general it requires less investment to develop a molecule against the target. In addition, targeted drug discovery allows lead optimization, which is often essential to make the drug more effective and safer. In this context, identifying a suitable potential target is the first and most important step towards targeted drug discovery.
2 Essential and Desirable Criteria for the Selection of a Trypanosomatid-Specific Drug Target
A good drug target has to meet different criteria. Amongst these criteria some are essential, whereas others are desirable (Fig. 2.1). One of the first essential criteria for drug target selection is its ability to be disease-modifying. For trypanosomatid parasites this means that the target must be essential for the viability of the parasite or its inhibition affects significantly the virulence of the parasite. In this context, it is necessary to select a target that participates in these processes in the “mammalian” forms of the parasite (intracellular amastigote for Leishmania, bloodstream form for T. brucei and trypomastigotes and amastigotes for T. cruzi). Another criterion that is essential for drug target selection is its “druggability”, i.e., the likelihood of small molecule drugs being able to modulate the target. In addition, ideally the target must be either found solely in the parasite, or have differences in the drug binding region/active site that can be exploited for inhibiting more potently the parasitic enzyme, thus allowing the identification of compounds with selective toxicity. The identification of targets for achieving parasite/host selectivity is a less difficult task, as potential molecular targets that are essential for the parasite could be redundant and thus not essential in mammalian cells. Moreover, an assayable target is required for performing drug screening. A simple assay that allows high throughput screening is a desirable criterion for drug target selection, facilitating the screening of a large number of compounds. The necessity of an active recombinant protein to perform screening assays has to be taken into consideration and a desirable criterion would be the feasibility to express the protein in its active form. High molecular weight proteins, or proteins that have transmembrane domains might prove difficult to express in an active form. Furthermore, it is useful if a drug target is found in more than one trypanosomatid species and also shares a function that can be disease-modifying in all trypanosomatid pathogens. Finally the presence of an available three-dimensional structure or a model is useful for drug target selection, as it opens possibilities for the development of structure-activity relationship studies (SARs) for lead optimization and structure-guided drug design.
3 Computational Approaches that Aid Drug Target Prioritization
Prerequisite for the identification of a new drug target is its experimental validation. This process is expensive and time consuming. Thus for the selection of a new drug target, an in silico approach is often essential. To this end, the completion of the genome project of trypanosomatid pathogens (http://www.genedb.org), including Leishmania (L. infantum, L. major and L. braziliensis) and Trypanosoma (T. brucei and T. cruzi) (Berriman et al. 2005; El-Sayed et al. 2005a, b; Ivens et al. 2005) has opened new possibilities for guided drug discovery. These parasites encode from 8,300 to 12,000 protein genes, of which 6,500 are common to L. major, T. brucei and T. cruzi genomes. In addition, another database, the TriTrypDB (Aslett et al. 2010) (http://tritrypdb.org/tritrypdb/), allows the integration of datasets from L. braziliensis, L. infantum, L. major, L. tarentolae, T. brucei and T. cruzi and enables a user to construct complex queries combining multiple data types. The TriTrypDB database gives information on individual genes or chromosomal spans in their genomic context, including syntenic alignments with other kinetoplastid organisms. The TriTrypDB database has allowed in silico metabolic pathway analysis using genome information (Alves-Ferreira et al. 2009). An inventory of predicted metabolic components and integrated metabolic networks of TriTryp is collected in publicly available databases, and a comprehensive review of many of these databases is provided in detail by Myler (Myler 2008). Amongst these, the database BRENDA (Braunschweig Enzyme Database, http://www.brenda-enzymes.org/), contains a plethora of metabolic enzymes that belong to more than 10,000 different organisms, including entries from T. brucei, T. cruzi and L. major. This database includes Enzyme Commission classification, function (including pathways, inhibitors, reaction types and substrates) and structure (including 3D structures), isolation and stability and links to bibliographic references. Another database, the KEGG (Kyoto Encyclopedia of Genes and genomes, http://www.genome.jp/kegg/), is dedicated to the understanding of high-level function utilities and integrates information and maps of metabolic pathways and associated human diseases, including infectious, and prescription drugs. In addition, it contains enzymatic families and reactions from 2,185 organisms including five trypanosomatids (L. infantum, L. major, L. braziliensis, T. cruzi and T. brucei). LeishCyc is a pathway/genome database (http://biocyc.org/LEISH/organism-summary?object=LEISH) that captures information about Leishmania metabolic pathways from genome annotation and literature resources and organizes this information into a structured database supported by a publicly available ontology. It contains 1,027 enzymes, 573 compounds and 143 metabolic pathways and allows the analysis and visualization of Leishmania high-throughput (metabolic ‘omics’ data), including metabolomics and proteomics (Doyle et al. 2009). In addition, pathway tools available in this database allow the identification of reactions that consume unique substrates or participate in unique reactions, the so-called network “chokepoints” (Doyle et al. 2009), which can be particularly useful for drug target selection.
In silico drug target prioritization for major tropical disease pathogens, including the trypanosomatids L. major, T. brucei and T. cruzi, is now possible and can be implemented by TDRtargets.org (http://tdrtargets.org, Crowther et al. 2010). In TDRtargets.org each criterion is assigned a subjective value and targets earn points of each criterion they meet, in a flexible ranking system that allows BOOLEAN intersection of criteria. The criteria used for drug target selection include the availability of structure (PDB structures or ModBased models), phylogeny (for the selection of unique proteins not present in the host), essentiality, druggability, assayabilty (information regarding the availability of recombinant protein) and specific criteria that are applicable in some species, like location, pathway, expression in distinct morphological stages, phenotype and others (Crowther et al. 2010). In addition, the database is not only restricted to drug targets, but also allows the search for compounds (Crowther et al. 2010). Although computational searches may save money and time for drug target identification, experimental validation is always required. The knowledge of important parasitic pathways for virulence or survival will aid this step. Several of these pathways and drug targets are already validated and herein some examples of these are listed.
4 Examples of Putative or Validated Drug Targets in Parasitic Metabolic and Signaling Pathways
Metabolic pathways in trypanosomatids have peculiarities that may be exploited for targeted drug discovery. Since excellent descriptions of these pathways are present (Lakhdar-Ghazal et al. 2002; de Souza and Rodriguez, 2009; Flohe, 2012), herein we will focus only specific points and data that describe validated or potential trypanosomatid drug targets.
4.1 Glycolysis
Glycolysis is an important pathway for drug development in trypanosomatid parasites, not only because it has a critical role for ATP production (the only way for bloodstream T. brucei), but also because it has many unique features reflecting both the peculiar glycosomal compartmentalization and differences in structure-activity relationships (Verlinde et al. 2001) (Fig. 2.2). To this end, the available crystal structures of many trypanosomatid glycolytic enzymes have been resolved, revealing significant differences compared to the corresponding mammalian enzymes. These differences point out the importance of glycolytic enzymes as good drug target candidates (Fig. 2.2).
In this respect, the first enzyme of glycolysis, hexokinase (HK), has been evaluated as a potential drug target. HK is encoded by two very similar enzymes in Leishmania and T. brucei (HK1 and HK2) and one in T. cruzi. The hexokinases from T. brucei (TbHK1 and TbHK2) have distinct C-terminal domains that result in distinct oligomer formation (Morris et al. 2006). The knocking down of TbHK1 by RNA interference (RNAi) revealed that this protein was essential for viability (Chambers et al. 2008a), and this enzyme was inhibited by lonidamine, a drug that killed effectively T. brucei parasites (Chambers et al. 2008b). The hexokinase from T. cruzi (TcHK) displayed significant kinetic differences from its mammalian orthologue, as this enzyme was not inhibited by mammalian HK regulators such as D-glucose-6-phosphate, fructose 1,6 diphosphate, phosphoenolpyruvate, lactate or citrate (Racagni and Machado de Domenech 1983; Urbina and Crespo 1984). In addition, inorganic pyrophosphate (PPi) inhibited this enzyme (Caceres et al. 2003). The synthesis of a series of 42 bisphosphonates confirmed that these compounds could inhibit TcHK, whereby the most potent of which displayed an IC50 of 2.2 μΜ against intracellular amastigotes (Hudock et al. 2006). Another series of non-competitive or mixed TcHK inhibitors, the aromatic arinomethylene biphosphonates, also displayed antiparasitic activity against intracellular amastigotes (Sanz-Rodriguez et al. 2007).
Two other enzymes of the glycolytic pathway, phosphoglucose isomerase (PGI) and phosphofructose kinase (PFK), are promising molecular targets for drug discovery. The crystal structures of PGI from T. brucei (Arsenieva et al. 2009) and L. mexicana (Cordeiro et al. 2004) and the TbPFK (Martinez-Oyanedel et al. 2007; McNae et al. 2009) have been determined and reveal unique features compared to mammalian orthologues. Moreover, the evaluation of a series of 2,5anhydro-D-mannitol derivatives have been described and determined as inhibitors of the T. brucei and L. mexicana PFK (Nowicki et al. 2008).
The crystal structure of L. mexicana and T. brucei fructose 1,6 aldolase (ALD) is also available, and allows the design of specific inhibitors (Chudzik et al. 2000). In this context, selective inhibitors of the trypanosomal over the corresponding mammalian enzyme that belong to the series of 1,6-dihydroxy-2-naphthaldehyde and 2,5 dihydroxybenzaldehyde were designed. However, they displayed low antiparasitic activity, possibly due to their poor potential to cross membranes (Dax et al. 2006).
The trypanosomatid triose-phosphate isomerase (TPI) from T. cruzi (Maldonado et al. 1998), T. brucei (Wierenga et al. 1991a, b) and L. mexicana (Williams et al. 1999) is another glycolytic enzyme with available structure that predicts important differences in the parasitic enzymes compared to the mammalian enzyme. Thus, specific inhibitors of the trypansomatid TPI that are also potent antiparasitics have been developed. More specifically, dithiodianiline and 6,6′-bisbenzothiazole-2,2′ diamine were potent inhibitors of TcTPI and trypanosomatid TPIs respectively, without significantly affecting human TPI (Olivares-Illana et al. 2006, 2007).
The next enzyme in the glycolytic pathway is glyceraldehyde-3-phosphate dehydrogenase (GD3PDH). Trypanosomatid GD3PDH has been also evaluated as a potential drug target. The structures of GD3PDH from L. mexicana (Kim et al. 1995), T. cruzi (Souza et al. 1998) and T. brucei (Vellieux et al. 1993) are resolved and specific inhibitors based on its structure have been designed. A series of adenosine competitive inhibitors that compete for NAD+ binding with substitutions at the 2′positions of the ribose and N6 position of adenine inhibited the leishmanial enzyme. In particular, one of the analogs [N6-(1-naphthalenemethyl-2′-(3-methoxybenazamido) adenosine] displayed potent antiparasitic activity at the nanomolar range (Suresh et al. 2001). One of the best inhibitors of TbGD3PDH is 3-diethyl (phosphono) propenal, which kills cultured trypanosomes with an LD100 of 300 nM (Willson et al. 1994).
The crystal structure of T. brucei phosphoglycerate kinase (PGK) is also available (Bernstein et al. 1997, 1998), and the comparison with the porcine PGK suggested that the ATP/ADP binding pockets display significant differences. The resolved crystal structures suggest that the ATP/ADP binding pockets between porcine and trypanosomatid PGKs display significant differences. Thus, the adenosine analogue tubercidin, which displays antitrypanosomal activity, has been shown to block the TbPGK (Drew et al. 2003). The trypanosomatid enolase (ENO) crystal structure is available, and the enzyme has a more flexible active site from its mammalian counterpart that might allow the design of specific and potent inhibitors (de AS Navarro et al. 2007).
Pyruvate kinase (PYK) catalyzes the last reaction of glycolysis and the enzyme from L. mexicana has an available crystal structure (Morgan et al. 2010; Tulloch et al. 2008). From this information, unique features of the effector binding site become apparent that could be used for drug design. Stepwise library synthesis and inhibitor design from a rational starting point identified furanose sugar amino amides (Nowicki et al. 2008) and saccharin derivatives as novel inhibitors of trypanosomatid PYK (Morgan et al. 2012). Overall, these data suggest that the glycolytic pathway enzymes are promising drug target candidates for future studies.
4.2 Purine Salvage Pathway
Trypanosomatid parasites are totally deficient in the de novo biosynthesis of purines, and rely on the scavenging from the host (Boitz et al. 2012). Research on purine transport (nucleobase/nucleoside) has focused on the use of purine antimetabolites or specific inhibition of the host nucleoside transporters (de Koning et al. 2005). Moreover the purine transport system can be exploited for the selective transfer of antiparasitic drugs, as in the case of melaminophenyl arsenicals that are efficiently accumulated through the T. b. brucei (De Koning 2008). Other genes involved in the purine salvage pathway include: (i) three phosphoribosyltransferases, hypoxanthine guanine phosphoribosyltransferase (HGPRT), xanthine phosphoribosyltransferase (XPRT), and adenine phosphoribosyltransferase (APRT), which catalyzes purine phosphoribosylation, (ii) adenosine kinase (AK) that phosphorylates adenosine (Datta et al. 1987; Iovannisci and Ullman 1984), and a multitude of interconversion enzymes (LaFon et al. 1982; Looker et al. 1983; Marr et al. 1978) (Fig. 2.3). Although none of the enzymes that convert host purine nucleobases or nucleosides to nucleotides are essential, genes in this pathway display properties that allow their exploitation for targeted drug design.
One such example is HPGPRT, which displays differences from the mammalian homologue with respect to substrate specificity (Monzani et al. 2007). Allopurinol, an effective drug against visceral and cutaneous leishmaniasis (Kager et al. 1981; Martinez and Marr 1992) and Chagas disease, is metabolized more efficiently by parasitic HGPRT than the mammalian homologue (Eakin et al. 1997) and therefore incorporated into RNA during transcription, resulting in its degradation and inhibition of protein synthesis (Marr and Berens 1983). Freymann et al., using a structure-based docking method based on the crystal structure of HGPRT from T. cruzi (TcHGPRT) provided a remarkably efficient path for the identification of HGPRT inhibitors with potent antiparasitic activity against T. cruzi trypomastigotes (Freymann et al. 2000).
Another example involves T. brucei AK. This enzyme activates adenosine antimetabolites, like cordycepin (3′-deoxyadenosine), and consequently contributes to their incorporation into RNA, ceasing protein synthesis (Luscher et al. 2007). In vitro incubation with cordycepin reduced not only the growth of T. brucei but also of T. cruzi, as well as L. major and L. amazonensis, suggesting that cordyceptin is activated by all the corresponding parasitic AKs (Rottenberg et al. 2005). In addition, this drug was active in mouse models of Chagas disease and African trypanosomiasis, when co-administered with deaminase inhibitors (Rottenberg et al. 2005). Thus the purine salvage pathway and the enzymes therein can be “druggable” targets with good potential.
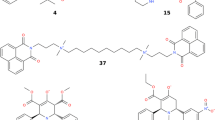
4.3 The Trypanothione System
Trypanothione is a low-molecular mass thiol, unique in trypanosomatids, that adopts the metabolic roles of glutathione (GSH) from other systems. It is implicated in the defense against oxidants, xenobiotics and regulatory proteins and is essential for parasitic survival (Flohe 2012). The biosynthesis and use of trypanothione relies on enzymes that are unique in trypanosomatids and absent from the mammalian host. Trypanothione is known to be synthesized by trypanothione synthetase (TryS) from GSH and spermidine or glutathionylspermidine synthesized by glutathionylspermidine synthase (GSpS). Reduction of oxidized trypanothione is NADPH-dependent and occurs by trypanothione reductase (TryR). Reduced trypanothione then participates in the reduction of glutaredoxin (Ceylan et al. 2010), and dehydroascorbate (Krauth-Siegel and Comini 2008) and tryparedoxin (TXN) (Flohe 2012). The latter mediates the reduction of other regulatory proteins (Flohe 2012). Most of the components of the trypanothione system are essential for parasite viability and allow selective inhibition over the mammalian corresponding enzymes. In addition, the structure of most of the enzymes in this pathway has been determined, making this pathway attractive for therapeutic interventions (Urbina 2010). One of the most attractive targets for drug design is TryR. Numerous reports in the literature exist on the inhibition of TryR, including tricyclic antidepressants and congeners, 2-aminodiphenylsulfides, quaternary alkylammonium, polyamine derivatives and others [reviewed in (Khan 2007)]. However, despite the multitude of TryR inhibitors, only a few were efficacious in animal models of leishmaniasis and trypanosomiasis (Flohe 2012). The differences observed between in vitro and in vivo antiparasitic effects of TryR inhibitors can be attributed to the pleiotropic effects of these inhibitors (Urbina 2010), to their metabolic instability (Khan 2007) and finally to the fact that redox metabolism of trypanosomatids is normal unless the residual activity of TryR is below 5 % of wild-type activity (Krieger et al. 2000). Apart from TryR, TryS, the enzyme that catalyzes the synthesis of trypanothione, has been validated as a drug target. Interestingly, compounds that inhibit this enzyme proved to effectively killT. brucei parasites (Torrie et al. 2009). Thus, it is clear that the unique trypanothione system provides opportunities for the development of novel inhibitors with limited “off-target” activity to the host.
4.4 Sterol Biosynthesis
The abundant supply of cholesterol present in their mammalian hosts cannot be used by trypanosomatid protozoa. Instead, Trypanosoma and Leishmania parasites have a strict requirement for specific endogenous sterols (ergosterol and other sterols) for survival and growth. The main sterols of trypanosomatids belong to the C28-ergostane or C29-stigmastane [reviewed in (de Souza and Rodrigues 2009)]. An exception to this rule is the membrane composition of bloodstream T. brucei parasites, which contains predominantly cholesterol, incorporated through a receptor-mediated endocytic process by suppressing the de novo ergosterol biosynthesis (Coppens et al. 1988). The sterol biosynthesis pathway is a promising target for the development of new anti-trypanosomatid drugs. Several drugs available today are known to interfere with the sterol biosynthesis pathway (Fig. 2.4).
Amongst these are quinuclidines that target squalene synthase (SQS, E.C. 2.5.1.21), the enzyme that catalyzes the first committed step in sterol biosynthesis (Fig. 2.4). This enzyme is a very attractive target and has been validated not only for treating hypercholesterolhaemia in humans but also for treating trypanosomatid diseases (Suckling 2006; Urbina et al. 2002). Two quinuclidines, ER-119884 and E5700, had potent in vitro anti-Leishmania (Fernandes Rodrigues et al. 2008) and anti-T. cruzi activity and the latter compound provided full protection against death in an in vivo murine model of Chagas disease (Urbina et al. 2004). Despite the fact that most SQS inhibitors tested in the parasite also block the mammalian host enzyme, this inhibition is tolerable in mammals. In addition, it has been possible to develop specific antiparasitic SQS inhibitors (Orenes Lorente et al. 2005; Sealey-Cardona et al. 2007), such as aryloxylethyl thiocyanates (WC-9) (Elhalem et al. 2002; Urbina et al. 2003) and 2-alkylaminoethyl-1,1-bisphosphonic acids (Rodrigues-Poveda et al. 2012). Another enzyme in the parasitic sterol biosynthesis pathway is squalene epoxidase (EC1.4.99.7) that converts squalene to 2,3 oxidosqualene. The antifungal drug terbinafine displayed potent antileishmanial activity against promastigotes and intracellular amastigotes by inhibiting this enzyme (Goad et al. 1985; Vannier-Santos et al. 1995). This drug displayed a synergistic effect with ketoconazole, another antifungal drug that also interferes with ergosterol biosynthesis (Vannier-Santos et al. 1995). The same drug combination also displayed a synergistic antiproliferative effect against epimastigotes and amastigotes of T. cruzi (Urbina et al. 1988). Lanosterol synthase (or oxidosqualene cyclase) is a key enzyme in sterol biosynthesis as it catalyzes the cyclization of 2,3 oxidosqualene (Fig. 2.4). This enzyme has already been validated as a chemotherapeutic target against T. brucei and T. cruzi (Buckner et al. 2001, 2000; Urbina and Docampo 2003).
Another reaction in sterol biosynthesis is the formation of zimosterol from lanosterol. This reaction is catalyzed by C14-demethylase (CYP51), a very diverse enzyme amongst kingdoms that is known to be inhibited by azoles (Urbina 2010). Several studies have shown that commercial inhibitors of yeast CYP51 available for the treatment of fungal infections (like ketoconazole, itraconazole) have a suppressive effect against Chagas disease in humans or in animals (Urbina 2002; Urbina and Docampo 2003). More potent and specific fungal and parasitic CYP51 inhibitors such as D0870 and posaconazole (POS) (Molina et al. 2000), a structural analogue of itraconazole, could completely cure experimental acute and chronic Chagas disease (Urbina et al. 1996a). Posoconazole is now poised to enter clinical trials to evaluate the effectiveness in treatment of Chagas disease (Robertson and Renslo 2011). POS has been tested in leishmaniasis in experimental murine models of leishmaniasis, showing a good efficacy against cutaneous leishmaniasis and to a lesser extent against visceral leishmaniasis due to L. donovani infection (Al-Abdely et al. 1999). Other triazoles like TAK-187, UR-9825 and ravuconazole displayed potent antiparasitic activity (Urbina 2010).
Finally, another important enzyme that catalyzes the C24 transmethylation reaction in the sterol biosynthesis is Δ24(25)-sterol methyltransferase (SMT) (EC 2.1.41), which is unique in trypanosomatids, but absent in the mammalian host. This enzyme has been shown to be inhibited by various azasterols, leading to in vitro antiproliferative effects against L. amazonensis and T. cruzi parasites (Lorente et al. 2004; Magaraci et al. 2003; Rodrigues et al. 2002; Urbina et al. 1995). One of the most potent inhibitors of SMT, 22,26 azasterol, displays selective antiparasitic activity in a murine model of acute Chagas disease (Urbina et al. 1996b). Overall, the data presented here suggests that the enzymes within the sterol biosynthesis pathway may be utilized for the design of potent and specific antitrypanosomatid inhibitors.
4.5 Pteridine Metabolism
Trypanosomatid parasites lack a de novo pathway for the synthesis of pteridines (folate and pteridines) and rely on salvage from the host (Beck and Ullman 1990). Among the key proteins of the pteridine salvage network that mediates the accumulation and reduction of pteridines, there is a bifunctional enzyme (DHFR-TS) that has activities of dihydrofolate reductase (DHFR) and thymidylate synthase (TS) -unlike the monofunctional enzyme of mammalian hosts-, and pteridine reductase (PTR1) that reduces both folate and biopterin (Fig. 2.5). These two enzymes have been proposed as drug targets in trypanosomatids, since they participate in essential pathways for the parasite metabolism, like thymidylate production by folates and oxidant resistance by the reduction of pterins (Moreira et al. 2009; Nare et al. 2009). Drugs that have been used to inhibit DHFR have proven ineffective in Leishmania (Neal and Croft 1984). This observation can be explained by the emergence of drug resistance. As PTR1 may reduce both, pterins and folates, this enzyme can act to override the inhibition of DHFR-TS (Nare et al. 1997). Thus, in L. major resistant strains, the amplification of PTR1 was observed (Nare et al. 1997). On the other hand, DHFR-TS is a validated drug target in T. brucei (Sienkiewicz et al. 2008), as null mutants had an absolute requirement for thymidine. Removal of thymidine from the medium resulted in growth arrest, followed by cell death and PTR1 was not able to compensate for loss of DHFR activity (Sienkiewicz et al. 2008). Mice infected with DHFR-TS null mutants were incapable of establishing infections (Sienkiewicz et al. 2008). The above suggests that both DHFR and TS activities in T. brucei are required for thymidylate synthesis and that thymidine concentrations in the host are limiting. Thus, the targeting of this enzyme could prove fruitful for improving/curing HAT.
Pteridine metabolism in trypanosomatids. (a) Thymidylate synthesis. The figure shows the thymidilate cycle in which thymidilate is synthesized by DHFR-TS, with the use of methylene tetrahydrofolate and its convertion to dihydrofolate. The same enzyme converts dihydrofolate to tetrahydrofolate. (b) Contribution of PTR1 to the reduction of pterins and folates and known inhibitors of this enzyme
On the other hand, research on the inhibition of trypanosomatid PTR1 has been more intense. PTR1 is an essential enzyme for viability, as PTR1 null mutants in T. brucei are not viable (Sienkiewicz et al. 2008). Virtual screening identified aminothiazole and aminobenzimidazole inhibitors as potent and selective TbPTR1 inhibitors (Fig. 2.5). Despite the good potency against PTR1 and favorable physicochemical properties, representative members of the scaffolds were not trypanocidal (Mpamhanga et al. 2009). The reason for this lack of correlation between enzymatic inhibition and antitrypanosomal activity is currently under investigation (Mpamhanga et al. 2009). As both PTR1 and DHFR-TS catalyze the same reactions, an attempt to inhibit both of these enzymes would be desirable. A screen against L. major PTR1 identified a number of compounds inhibiting both PTR1 and DHFR-TS. Four of these compounds displayed antiparasitic activity, suggesting that the inhibition of both of these enzymes is required for the efficacy of new drug candidates (Hardy et al. 1997).
4.6 Drug Targets in Signaling and Other Pathways Essential for Parasitic Survival
4.6.1 Topoisomerases
Topoisomerases use DNA strand scission, manipulation and rejoining activities to deal with DNA torsional stress, which makes them potential targets for treating parasitic diseases. As topoisomerases are involved in replication, transcription, chromosomal condensation and segregation, inhibitors of these enzymes have a drastic inhibitory effect on the growth of trypanosomatid parasites (Balana-Fouce et al. 2006; Das et al. 2006a; De Sousa et al. 2003; Deterding et al. 2005; Douc-Rasy et al. 1988). These enzymes are grouped into type I and II, depending on their ability to cleave single- and double-stranded DNA, respectively. Trypanosomatid parasites possess both types of topoisomerases (Bakshi and Shapiro 2004; Balana-Fouce et al. 2006; Das et al. 2006b; De Sousa et al. 2003; Douc-Rasy et al. 1988; Strauss and Wang 1990). Type I topoisomerases include type IA and IB subclasses, which are grouped on the basis of differences in their aminoacid sequences and mechanism of action (Champoux and Dulbecco 1972). Topoisomerase IB in trypanosomatids acts as an unusual bi-subunit enzyme, and it is localized in both the nucleus and the kinetoplast (Bakshi and Shapiro 2004; Das et al. 2004).
Topoisomerase inhibitors are often used as anticancer drugs in mammalian cells. These drugs may inhibit topoisomerases via two distinct mechanisms. The first type of inhibition includes the covalent stabilization of DNA-topoisomerase complexes, and the drugs that have this action are referred to as topoisomerase poisons. The second type of inhibition is mediated by drugs that interfere with the active site of the enzyme, and are termed topoisomerase inhibitors (Steverding and Wang 2009). Camptothecins, anthracyclins, epipodophyllotoxins and quinolones are classified as topoisomerase poisons, whereas coumarin antibiotics and forstriecin analogues are topoisomerase inhibitors (Steverding and Wang 2009). Topoisomerases are essential proteins for parasite viability. Thus, topoisomerase inhibitors or poisons have been shown to have activity against trypanosomatid protozoa, mediating apoptosis-like death (Smirlis et al. 2010). Moreover, the antileishmanial compounds sodium stibogluconate and urea stibamine have been shown to act via the inhibition of type I topoisomerase (Chawla and Madhubala 2010). Camptothecin, a drug that acts as a poison against leishmanial topoisomerase I (Das et al. 2006a), has been found to block L. donovani, T. cruzi and T. brucei proliferation, whereas analogues have been screened against T. brucei bloodstream parasites and different substitutions have been identified (9,10,11-methylenedioxy analogs) that display a selectivity over the T. brucei parasites (Bodley et al. 1995). In addition, the flavones baicalein, quercetin and luteolinhave been shown to stabilize the DNA- L. donovani bi-subunit topoisomerase I cleavage complex by a differential mechanism, providing in this way additional insights into the ligand-binding properties of L. donovani topoisomerase I (Das et al. 2006b). Besides the abovementioned flavones, three isoflavanoids, 8-prenylmucronulatol, lyasperin H and smiranicin display antileishmanial activity correlated with topoisomerase II inhibition and kinetoplast DNA (kDNA) linearization (Salem and Werbovetz 2005). Acridine compounds, such as 9-anilinoacridine derivatives, display antiparasitic activity against Leishmania and Trypanosoma and their mode of action is via the inhibition of topoisomerase II (Figgitt et al. 1992). The topoisomerase II poisons, belonging to the family of anthracycline antibiotics daunomycin and its hydroxyl derivative doxorubicin, had activity against T. b. rhodesiense affecting parasite motility and infectivity to mice (Williamson and Scott-Finnigan 1978). Moreover, doxorubicin has been shown to be highly active in an in vivo model of visceral leishmaniasis (Sett et al. 1992), its mechanism of action being the inhibition of leishmanial topoisomerase II (Singh and Dey 2007). Another set of topoisomerase II poisons, the fluoroquinolones like KB5426, ofloxacin and ciprofloxacin have been shown to have activity against T. brucei (Nenortas et al. 1999, 2003). Finally, aclarubicin, an anthracenedionemotoxantrone derivative that acts as a catalytic inhibitor of topoisomerase II, exhibited potent antiparasitic activity against T. brucei bloodstream parasites and a 1,000 fold selectivity index, making this drug a good drug candidate for the treatment of trypanosomiasis (Deterding et al. 2005). Despite the fact that parasitic topoisomerases are essential for survival, and that a multitude of compounds that target these enzymes are available, up to date most of the known topoisomerase inhibitors lack selectivity over the host cells. To this end it is essential to exploit differences between parasite and mammalian topoisomerases.
4.6.2 Proteases
Proteases in trypanosomatid protozoa have been shown to be involved in many important signaling processes, including cell-cycle progression, stage differentiation, autophagy, apoptosis and others (Abdulla et al. 2008; Ambit et al. 2008; Boukai et al. 2000; Galvao-Quintao et al. 1990; Leon et al. 1994; Smirlis and Soteriadou 2011). Amongst the multitude of proteases in parasitic protozoan, cathepsin-like cysteine proteases have been the focus of attention. The cathepsin L-like proteases include CPA and CPB in Leishmania, and cruzipain and brucipain (or rhodesain) in T. cruzi and T. brucei, respectively. On the other hand, the cathepsin B-like proteases are termed CPC in Leishmania and TbCatB in T. brucei. CPB deletion mutants in L. mexicana displayed reduced virulence in BALB/c mice, suggesting that the pharmacological inhibition of this protease may compromise the progression of leishmaniasis (Alexander et al. 1998). Indeed, a peptide that has been characterized as a natural inhibitor of cysteine proteases and a potent inhibitor of CPB led to a reduced virulence and a Th1 response (Bryson et al. 2009). In L. major, a class of cathepsin inhibitors, known as aziridine-2,3-dicarboxylate derivatives, induced cell death correlated with the presence of autophagy-related lysosome-like vacuoles (Schurigt et al. 2010).
In T. brucei, downregulation of brucipain by RNAi showed that this protease is not essential for growth. However, a vinyl-sulfone inhibitor (K11777, see below) of this protease limited the ability of T. b. rhodesiense to cross the blood brain barrier in brain endothelial cells in vitro, suggesting its potential role ameliorating central nervous system (CNS) damage during T. brucei infection. Despite the fact that brucipain was not proven to be essential for T. brucei viability, TbCatB was required for parasite growth, participating in iron acquisition by degrading host transferrin (Abdulla et al. 2008; O’Brien et al. 2008). Thus, a series of selective purine nitrile inhibitors with enhanced potency for TbCatB were developed via structure-guided optimization. These compounds were trypanocidal, reaffirming the potential of TbCatB as a therapeutic target, whereas a lead compound of the series significantly prolonged the life of infected mice with T. brucei (Mallari et al. 2009, 2010).
In T. cruzi, cruzipain is required for all the major proteolytic activities of the parasite life cycle (Cazzulo 2002; Urbina and Docampo 2003). Inhibition of this protease by K-11777 resulted in cessation of proliferation in epimastigotes and intracellular amastigotes and arrested metacyclogenesis. In murine models of acute and chronic Chagas disease, the inhibitor significantly reduced parasitemia and prolonged survival, conferring minimal toxicity to the host (Engel et al. 1998). In addition, the same compound displayed therapeutic activities in an immunodeficient mouse model of Chagas disease (Doyle et al. 2007). In a canine model of acute Chagas disease, K-11777 significantly reduced cardiac damage (Barr et al. 2005). Following these promising results in animal models of Chagas disease, the development of K-11777 as a new treatment for Chagas diseases was initiated. Despite the hepatotoxicity and other serious problems with this compound that resulted in terminating the project, this effort demonstrated that cruzipain inhibitors could prove promising drugs for the treatment of Chagas disease. Thus, attempts to identify potent and specific inhibitors of cruzipain were initiated (Brak et al. 2008; Caffrey et al. 2000; Du et al. 2002). Structure-activity relationship studies (SARs) demonstrated that thiosemicrbazone and semicarbazone scaffolds are potent and selective cruzipain inhibitors (Du et al. 2002; Guido et al. 2008). Moreover, several other classes of non-peptidic inhibitors have been identified, including vinyl-sulphone containing macrocycles (Brak et al. 2008), aryl oxymethyl-ketone inhibitors (Brak et al. 2008) and quinoxaline-N-acyl hydrazone inhibitors (Romeiro et al. 2009). Thus, cruzipain is a confirmed drug target, and research for the identification of a good cruzipain inhibitor suitable for future drug development is ongoing.
Overall, parasitic proteases are enzymes with a potential to be good drug target candidates and thus further investigation on their role in the parasitic life-cycle, essentiality and druggability is required.
4.6.3 Kinases
In view of the success in targeting eukaryotic protein kinases (PKs) in other disease contexts (notably cancer), parasitic kinases are considered attractive drug targets. Moreover, additional reasons exist that justify the selection of parasitic kinases as ideal drug targets. These include the fundamental role of parasitic kinases and phosphorylation cascades in critical parasite pathways for survival and virulence, such as cell-cycle progression, differentiation and others and the divergence between the kinomes of the parasites and of their human hosts, which allows the design of drugs that may specifically target the parasitic kinase (Naula et al. 2005). Despite the pharmaceutical interest on host protein kinases, protozoan PKs remain largely underexplored as targets for neglected diseases. Interestingly, tryapanosomatids have a significant number of PK genes, with 179 genes present in L. major, 156 in T. brucei and 171 in T. cruzi (Naula et al. 2005). Several of these kinases, notably members of the CMGC group of kinases, have already been validated as drug targets for the treatment of parasitic diseases. Amongst these are the cyclin-dependent kinases (CDKs), mitogen-activated protein kinases (MPK) and glycogen synthase kinase 3(GSK-3) (Grant et al. 1998; Hassan et al. 2001; Tu and Wang 2004; Wang et al. 1998, 2005; Wiese 1998, 2007; Ojo et al. 2008; Xingi et al. 2009).
The number of MPK homologues in Leishmania is rather large, with 15 putative mitogen activated protein kinases (MPK) identified, along with 13 in T. brucei, several of which are two-copy genes (Wiese 2007). Several of these kinases are characterized, including TbECK1 (the homologue of LmxMPK6) (Ellis et al. 2004), LmxMPK11 and LmxMPK13 (Marshall and Rosenbaum 2001; Bengs et al. 2005), with no evidence up to date that they could serve as molecular targets for the treatment of trypanosomatid diseases. On the other hand, MPK5 is a validated drug target, since a null LmxMPK5 mutant displayed an impaired ability to cause lesions in BALB/c mice infected with L. mexicana (Wiese 2007). The LmxMPK5 homologue in T. brucei,TbMPK5, has been found to be involved in the differentiation of bloodstream forms to stumpy forms, and a null mutant of this kinase displayed a massive reduction of parasitemia (16-fold lower) in immunosuppressed mice (Domenicali Pfister et al. 2006). Moreover, a null LmxMPK5 mutant displayed an impaired ability to cause lesions in BALB/c mice infected with L. mexicana. Thus, these data suggest that trypanosomatid MPK5 might be exploitable as a target for chemotherapy against human sleeping sickness and leishmaniases. Another MPK, LmxMPK1, has been shown to be essential for cell-cycle progression and survival in L. mexicana amastigotes in a murine model of leishmaniasis, representing thus a functionally validated drug target (Wiese 1998). In addition, the related kinase LmxMPK2 also represents a putative drug target, as it is shown that it is required for the establishment of infection and in important processes in the mammalian amastigote stage (Wiese 2007). One of the most studied and validated target that belongs to this group of kinases is LmxMPK4. This enzyme is essential for viability in L. mexicana, as LmxMPK4 null mutants could not be generated (Wang et al. 2005). The same kinase displays enhanced activity upon exposure to pH 5.5 and 37°C in L. major promastigotes and L. donovani axenic amastigotes, the natural stress signals that occur during the differentiation of the parasite from the insect to the mammalian stage (Morales et al. 2007). In addition, a new E. coli based expression system was generated for LmxMPKK5 that included a STE7-like protein kinase from L. mexicana, required for its activation. This effort is the basis for the development of drug screening assays of LmxMPK4 (John von Freyend et al. 2010).
Despite the promising results that suggest that targeting MPKs in trypanosomatid parasites could provide a disease-modifying mechanism, another group of CMGC kinases, namely the CDKs, has attracted more attention towards the validation of its members as potential drug targets. This family is well represented in trypanosomatids, with 11 members in L. major and T. brucei and 10 members in T. cruzi (Naula et al. 2005). Trypanosomatid CDKs contain cyclin-binding regions as anticipated (Naula et al. 2005), whereas the presence of a cyclin (CYC2, CYC3, CYC6 for T. brucei, and CYC1, CYCA and CYC6 for Leishmania) for the activity of the trypanosomatid homologue of mammalian CDK1 (CRK3) has been shown (Wang et al. 1998; Van Hellemond et al. 2000; Li and Wang 2003; Hammarton et al. 2003, 2004; Tu and Wang 2004; Banerjee et al. 2006; Gomes et al. 2010). The function of two kinases from L. mexicana and T. brucei, namely CRK1 and CRK3, have been analysed in detail. In L. mexicana, the activity of LmxCRK1 was shown to be restricted to the promastigote stage, whereas its role in amastigotes has not been investigated in detail (Grant et al. 2004). In T. brucei, downregulation of CRK1 by RNAi in bloodstream and procyclic forms led to reduced growth and increase in the number of cells in the G1 phase of the cell-cycle, demonstrating the importance of this kinase in regulating the G1→S transition (Tu and Wang 2004). Despite these results, the validation of this kinase as a drug target in both Leishmania and Trypanosoma still remains an open issue.
On the other hand, CRK3 has been validated as a drug target in trypanosomatid parasites and has been studied in great detail compared to other parasitic CDK kinases. As mentioned above, CRK3 is considered to be the functional homologue of mammalian CDK1. Initially, the functional homology of the L. major CDK, CRK3 to Schizosaccharomyces pombe CDKs was demonstrated by the functional complementation of this kinase in a temperature-sensitive S. pombe cdc2/CDK1 null mutant (Wang et al. 1998). The gene for L. mexicana CRK3 was shown to be essential for viability, as it is a crucial regulator of cell division. CRK3 activity was found to peak in the G2/M phase of the cell cycle, and inhibition of CRK3 in vivo resulted in cell cycle arrest (Hassan et al. 2001). The same effect on cell-cycle progression was observed upon the downregulation of TbCRK3 in T. brucei procyclics and bloodstream parasites (Tu and Wang 2004). Grant et al. previously described the screening of a diverse chemical library of antimitotic compounds for potential inhibitors of Leishmania CRK3 (Grant et al. 1998). However, despite the potent effect of these inhibitors on the leishmanial kinase, they failed to show selectivity over the mammalian CDK1–CYCB complex (Grant et al. 2004). Recent studies identified Leishmania CRK3–CYC6 inhibitors belonging to the class of azapurines, with micromolar potency, following a high-throughput screen with heterocyclic and kinase libraries (Walker et al. 2011). However, potent inhibitors of CRK3-CYC6 did not always display antiparasitic activity (Cleghorn et al. 2011). This suggests that CYC6 might not be the cyclin that in vivo is required for the function of CRK3 (Cleghorn et al. 2011). Further work is required to delineate the discrepancy between the drug inhibition of CRK3 and the lack of antiparasitic activity of certain inhibitors.
Apart from the MPK and CDKs of the CMGC kinase family, as mentioned above, GSK-3 has attracted attention, constituting a model candidate for drug target selection. GSK-3 is a multifunctional serine/threonine kinase of the CMGC family, found in all eukaryotes. This enzyme is known to play a key role in many cellular and physiological events, including Wnt[Int and Wg (wingless) in Drosophila] signaling, transcription, cell-cycle and differentiation, neuronal functions and circadian rhythm (Phukan et al. 2010). These functions of GSK-3 and its implication in many human diseases, such as Alzheimer’s disease, non-insulin-dependent diabetes mellitus and cancer, have stimulated an active search for potent and selective GSK-3 inhibitors (Phukan et al. 2010). Two GSK-3 genes, GSK-3s (short) and GSK-3l (long), are encoded in the T. brucei and the leishmanial genome. Of the two isoforms, the short isoform has been analysed in both T. brucei and L. donovani (Ojo et al. 2008; Xingi et al. 2009). Previous studies demonstrated that leishmanial GSK-3s was essential for parasitic viability, and its inhibition causes cell-cycle defects and apoptosis-like death (Xingi et al. 2009). Moreover, RNAi experiments showed that TbGSK-3s is essential for viability in bloodstream forms of T. brucei (Ojo et al. 2008). These results validate this kinase as a drug target for the treatment of leishmaniasis and HAT. Apart from the essentiality in the life-cycle of trypanosomatid parasites, parasitic GSK-3s has many desirable characteristics that justify its selection as a drug target. More importantly, inhibitor scaffolds and inhibitors of parasitic GSK-3 have been identified that also show good antiparasitic activity (Oduor et al. 2011; Ojo et al. 2011, 2008; Xingi et al. 2009). Indirubins, a class of bis-indole compounds known for over a century as a minor constituent of plant, animal and microorganism-derived indigo, represent inhibitory scaffolds targeting LdGSK-3s (Xingi et al. 2009). More specifically, a series of 6- and 5- halogen substituted indirubins, were tested against promastigotes and intracellular amastigotes (Xingi et al. 2009). Four of these compounds displayed antileishmanial activity against L. donovani promastigotes and intracellular amastigotes. All of the analogues with antiparasitic activity inhibited both CRK3 and LdGSK-3s. Of these, 6-Br-5methylindirubin-3′oxime inhibited 7 times more potently LdGSK-3s (IC50 90 nM) and killed effectively promastigotes and intracellular amastigotes (IC50 < 1.2 μΜ). Interestingly, although 6 bromo-substituted indirubins are powerful ATP competitive inhibitors of mammalian GSK-3 (Polychronopoulos et al. 2004), they displayed a high selectivity index because the inhibition of host kinase is tolerable in adult mammals (Henriksen et al. 2003; Kaidanovich-Beilin and Eldar-Finkelman 2006). Furthermore, since GSK-3 has also been pursued as a human drug target, a large number of inhibitors are available for screening against parasites. To this end, a collaborative industrial/academic partnership facilitated by the World Health Organization Tropical Diseases Research division (WHO TDR) was initiated, to stimulate research aimed at identifying new drugs for treating HAT. In this context, a subset of 16,000 inhibitors that target human GSK-3β from the Pfizer compound collection were screened, and potent and selective inhibitors of TbGSK-3s were identified (Oduor et al. 2011).
The continuation of a drug discovery program by the synthesis of more potent and selective inhibitors of parasitic GSK-3s is possible because critical differences exist in the ATP-binding pocket between parasite and human GSK-3 (Ojo et al. 2011; Xingi et al. 2009). More specifically, the two major differences in the leishmanial enzyme that are conserved in T. brucei are the replacement of Gln185hGSK-3β by His155LdGSK-3s in the sugar-binding region, and the replacement of the “gatekeeper”Leu132hGSK-3β by Met100LdGSK-3s (Xingi et al. 2009). In addition, the crystal structure of L. major GSK-3s is now available that allows more accurate structure-activity relationship studies for future drug design.
Thus, with respect to parasite essentiality, assayability for high throughput screening, the availability of crystal structure, the existence of differences in the active site in comparison to its mammalian homologues, the redundancy of mammalian GSK-3β function in the mammalian host and the tolerance of its inhibition, and finally the presence of a multitude of compounds known to inhibit parasitic GSK-3s, make this enzyme an excellent “model for drug target selection”. Research into parasitic GSK-3s kinases provides an excellent opportunity to develop a targeted drug therapy for leishmaniases and HAT.
5 Investigating Drug Repurposing Opportunities for Drug Target Identification and for Antiparasitic Drug Discovery
The process of finding new uses for existing drugs (marketed drugs and failed or idle compounds, or drugs whose mammalian targets are known) outside the scope of the original indication is variously referred to as repositioning, redirecting, repurposing, and reprofiling. Nowadays, as more and more pharmaceutical companies are exploring the existing arsenal of known drugs for repositioning candidates, the number of repositioning successful stories is steadily increasing (Padhy and Gupta 2011).
Thus, the exploitation of drugs whose targets have already been discovered in other systems can offer advantages for both drug target identification and antiparasitic drug discovery. For drug repositioning strategy, in order to facilitate the access of information concerning therapeutic targets, there are publicly accessible databases, such as DrugBank, Potential Drug Target Database, Therapeutic Target Database, and SuperTarget. These databases complement each other to provide target and drug profiles (Zhu et al. 2010). Moreover, it is now possible to reposition marketed drugs to novel targets and vice-versa. This can be achieved by a java-based software called IDMap (Ha et al. 2008). The next step is to gain access to compound libraries.
This step is challenging and the choice of a compound library is critical for the discovery of a potential drug target in protozoa. Despite the fact that genetic validation will be required for assessing the essentiality for viability or virulence of a potential drug target, this approach saves time and aids researchers to avoid laborious and high-cost techniques, like genetic manipulation (i.e. targeted gene deletion) over targets that are not essential for parasite viability (Fig. 2.1). This approach has been used to validate LdGSK-3s as a drug target for the treatment of leishmaniasis by using known inhibitors of mammalian GSK-3. These inhibitors displayed both antiparasitic activity and activity against LdGSK-3s. The inhibitory activity of LdGSK-3s, as the leishmanicidal mechanism of action, was further validated by the over-expression of LdGSK-3s in L. donovani promastigotes, and the demonstration that L. donovani over-expressing LdGSK-3s were protected from the leishmanicidal effects of indirubins (Xingi et al. 2009).
Drug repositioning can be also a good strategy once a target is selected (Fig. 2.1), for identifying compounds that represent potential attractive starting points for a drug discovery program. The T. brucei GSK-3s has provided an excellent example for this strategy and the screening of a compound library from the Pfizer compound collection as mentioned above, known to target mammalian GSK-3β,resulted in the identification of inhibitors that target better the parasitic TbGSK-3s (Oduor et al. 2011).
Finally, drug repurposing offers an additional advantage for the choice of drugs that are marketed. For these drugs, information already exists concerning their clinical safety data, pharmacokinetics, and viable dose range are available at the start of a development project, and the risks associated with clinical development are significantly reduced with fewer failures in the later stages. One such example is amphotericin B, an antifungal agent that creates membrane leaks by binding to ergosterol used to treat thrush, and is used today as an antileishmanial agent (Hartsel and Bolard 1996). Commercial inhibitors of yeast CYP51, an enzyme that is also present in trypanosomatids, have proved to have antiparasitic effects. One such example is posaconazole (Noxafil) a broad spectrum antifungal, is also a prime candidate for clinical trials in patients with Chagas disease (Robertson and Renslo 2011).
6 Concluding Remarks
There are many opportunities for the selection and/or identification of novel drug targets for drug development against diseases caused by trypanosomatid parasites. These include methods, like systems biology and network analysis, which integrate biochemistry and cell biology with genetics, as well as bioinformatics and computational biology to obtain holistic descriptions at the organism level. A good drug target gives the opportunity to develop safer drugs at a lower cost. Today the process to predict and validate drug targets is faster than before. This is due to the advances in in silico drug target prediction, in the completion of the genome project of trypanosomatid pathogens, and in systems biology. Despite this, researchers that are new to the field have to have in mind that a multitude of trypanosomatid (potential) drug targets are already validated or close to validation. In addition to these molecular targets, a variety of attractive drugs that inhibit many of these enzymes exists, which could serve as promising scaffolds for the synthesis of more potent and selective antiparasitic agents. However, despite these advances, there seems to be little interest to make new drugs for the neglected diseases caused by trypanosomatid parasites. This cannot be attributed to a lack of scientific knowledge. It is more likely that the lack of interest to develop antiparasitic drugs is attributed to the low probability of pharmaceutical companies to have a profitable financial return. Thus, a targeted response is required for an adequately funded, needs-driven priority R&D agenda to combat these devastating diseases.
Abbreviations
- AK:
-
Adenosine kinase
- ALD:
-
Fructose 1,6 aldolase
- APRT:
-
Adenine phopsphoribosyltransferase
- CatB:
-
Cathepsin B
- CDK:
-
Cyclin dependent kinase
- CNS:
-
Central Nervous System
- CPA:
-
Cysteine proteinase A
- CPB:
-
Cysteine proteinase B
- CRK:
-
cdc2 related kinase
- CYC:
-
Cyclin
- CYP51:
-
Cytochrome P-450 51
- DHFR:
-
Dihydrofolate reductase
- ECK1:
-
ERK-like, CRK-like Kinase-1
- ENO:
-
Enolase
- G3DPH:
-
Glycerol-3-phosphate dehydrogenase
- GD3DPH:
-
Glyceraldehyde 3-phosphate dehydrogenase
- GK:
-
Glycerol kinase
- GSH:
-
Glutathione
- GSK-3:
-
Glycogen synthase kinase 3
- GSpS:
-
Glutathionylspermidine
- HAT:
-
Human African trypanosomiasis
- HGPRT:
-
Hypoxanthine guanine phopsphoribosyltransferase
- HK:
-
Hexokinase
- kDNA:
-
Kinetoplast DNA
- MPK:
-
Mitogen activated kinase
- PFK:
-
Phosphofructose kinase
- PGI:
-
Phosphoglucose isomerase
- PGK:
-
Phosphoglycerate kinase
- PGM:
-
Phosphoglycerate mutase
- PK:
-
Protein kinase
- POS:
-
Posaconazole
- PTR:
-
Pteridine reductase
- PYK:
-
Pyruvate kinase
- SMT:
-
Δ24(15)-sterol methyltransferase
- SQS:
-
Squalene synthatase
- STE7:
-
Signaling terminal 7 extension
- TPI:
-
Triose phosphate isomerase
- TryR:
-
Trypanothione reductase
- TryS:
-
Trypanothione synthatase
- TS:
-
Thymidylate synthase
- TXN:
-
Tryparedoxin
- WHO:
-
World Health Organization
- XPRT:
-
Xanthine phopsphoribosyltransferase
References
Abdulla MH, O’Brien T, Mackey ZB, Sajid M, Grab DJ, McKerrow JH (2008) RNA interference of Trypanosoma brucei cathepsin B and L affects disease progression in a mouse model. PLoS Negl Trop Dis 2:e298
Al-Abdely HM, Graybill JR, Loebenberg D, Melby PC (1999) Efficacy of the triazole SCH 56592 against Leishmania amazonensis and Leishmania donovani in experimental murine cutaneous and visceral leishmaniases. Antimicrob Agents Chemother 43:2910–2914
Alexander J, Coombs GH, Mottram JC (1998) Leishmania mexicana cysteine proteinase-deficient mutants have attenuated virulence for mice and potentiate a Th1 response. J Immunol 161:6794–6801
Alves-Ferreira M, Guimaraes AC, Capriles PV, Dardenne LE, Degrave WM (2009) A new approach for potential drug target discovery through in silico metabolic pathway analysis using Trypanosoma cruzi genome information. Mem Inst Oswaldo Cruz 104:1100–1110
Ambit A, Fasel N, Coombs GH, Mottram JC (2008) An essential role for the Leishmania major metacaspase in cell cycle progression. Cell Death Differ 15:113–122
Arsenieva D, Appavu BL, Mazock GH, Jeffery CJ (2009) Crystal structure of phosphoglucose isomerase from Trypanosoma brucei complexed with glucose-6-phosphate at 1.6 A resolution. Proteins 74:72–80
Aslett M, Aurrecoechea C, Berriman M, Brestelli J, Brunk BP, Carrington M, Depledge DP, Fischer S, Gajria B, Gao X, Gardner MJ, Gingle A, Grant G, Harb OS, Heiges M, Hertz-Fowler C, Houston R, Innamorato F, Iodice J, Kissinger JC, Kraemer E, Li W, Logan FJ, Miller JA, Mitra S, Myler PJ, Nayak V, Pennington C, Phan I, Pinney DF, Ramasamy G, Rogers MB, Roos DS, Ross C, Sivam D, Smith DF, Srinivasamoorthy G, Stoeckert CJ Jr, Subramanian S, Thibodeau R, Tivey A, Treatman C, Velarde G, Wang H (2010) TriTrypDB: a functional genomic resource for the Trypanosomatidae. Nucleic Acids Res 38:D457–462
Bakshi RP, Shapiro TA (2004) RNA interference of Trypanosoma brucei topoisomerase IB: both subunits are essential. Mol Biochem Parasitol 136:249–255
Balana-Fouce R, Redondo CM, Perez-Pertejo Y, Diaz-Gonzalez R, Reguera RM (2006) Targeting atypical trypanosomatid DNA topoisomerase I. Drug Discov Today 11:733–740
Banerjee S, Sen A, Das P, Saha P (2006) Leishmania donovani cyclin 1 (LdCyc1) forms a complex with cell cycle kinase subunit CRK3 (LdCRK3) and is possibly involved in S-phase-related activities. FEMS Microbiol Lett 256:75–82
Barr SC, Warner KL, Kornreic BG, Piscitelli J, Wolfe A, Benet L, McKerrow JH (2005) A cysteine protease inhibitor protects dogs from cardiac damage during infection by Trypanosoma cruzi. Antimicrob Agents Chemother 49:5160–5161
Beck JT, Ullman B (1990) Nutritional requirements of wild-type and folate transport-deficient Leishmania donovani for pterins and folates. Mol Biochem Parasitol 43:221–230
Bengs F, Scholz A, Kuhn D, Wiese M (2005) LmxMPK9, a mitogen-activated protein kinase homologue affects flagellar length in Leishmania mexicana. Mol Microbiol 55:1606–1615
Bernstein BE, Michels PA, Hol WG (1997) Synergistic effects of substrate-induced conformational changes in phosphoglycerate kinase activation. Nature 385:275–278
Bernstein BE, Michels PA, Kim H, Petra PH, Hol WG (1998) The importance of dynamic light scattering in obtaining multiple crystal forms of Trypanosoma brucei PGK. Protein Sci 7:504–507
Berriman M, Ghedin E, Hertz-Fowler C, Blandin G, Renauld H, Bartholomeu DC, Lennard NJ, Caler E, Hamlin NE, Haas B, Bohme U, Hannick L, Aslett MA, Shallom J, Marcello L, Hou L, Wickstead B, Alsmark UC, Arrowsmith C, Atkin RJ, Barron AJ, Bringaud F, Brooks K, Carrington M, Cherevach I, Chillingworth TJ, Churcher C, Clark LN, Corton CH, Cronin A, Davies RM, Doggett J, Djikeng A, Feldblyum T, Field MC, Fraser A, Goodhead I, Hance Z, Harper D, Harris BR, Hauser H, Hostetler J, Ivens A, Jagels K, Johnson D, Johnson J, Jones K, Kerhornou AX, Koo H, Larke N, Landfear S, Larkin C, Leech V, Line A, Lord A, Macleod A, Mooney PJ, Moule S, Martin DM, Morgan GW, Mungall K, Norbertczak H, Ormond D, Pai G, Peacock CS, Peterson J, Quail MA, Rabbinowitsch E, Rajandream MA, Reitter C, Salzberg SL, Sanders M, Schobel S, Sharp S, Simmonds M, Simpson AJ, Tallon L, Turner CM, Tait A, Tivey AR, Van Aken S, Walker D, Wanless D, Wang S, White B, White O, Whitehead S, Woodward J, Wortman J, Adams MD, Embley TM, Gull K, Ullu E, Barry JD, Fairlamb AH, Opperdoes F, Barrell BG, Donelson JE, Hall N, Fraser CM, Melville SE, El-Sayed NM (2005) The genome of the African trypanosome Trypanosoma brucei. Science 309:416–422
Bodley AL, Wani MC, Wall ME, Shapiro TA (1995) Antitrypanosomal activity of camptothecin analogs. Structure-activity correlations. Biochem Pharmacol 50:937–942
Boitz JM, Ullman B, Jardim A, Carter NS (2012) Purine salvage in Leishmania: complex or simple by design? Trends Parasitol 28:345–352
Boukai LK, da Costa-Pinto D, Soares MJ, McMahon-Pratt D, Traub-Cseko YM (2000) Trafficking of cysteine proteinase to Leishmania lysosomes: lack of involvement of glycosylation. Mol Biochem Parasitol 107:321–325
Brak K, Doyle PS, McKerrow JH, Ellman JA (2008) Identification of a new class of nonpeptidic inhibitors of cruzain. J Am Chem Soc 130:6404–6410
Bryson K, Besteiro S, McGachy HA, Coombs GH, Mottram JC, Alexander J (2009) Overexpression of the natural inhibitor of cysteine peptidases in Leishmania mexicana leads to reduced virulence and a Th1 response. Infect Immun 77:2971–2978
Buckner FS, Griffin JH, Wilson AJ, Van Voorhis WC (2001) Potent anti-Trypanosoma cruzi activities of oxidosqualene cyclase inhibitors. Antimicrob Agents Chemother 45:1210–1215
Buckner FS, Nguyen LN, Joubert BM, Matsuda SP (2000) Cloning and heterologous expression of the Trypanosoma brucei lanosterol synthase gene. Mol Biochem Parasitol 110:399–403
Burri C, Brun R (2003) Eflornithine for the treatment of human African trypanosomiasis. Parasitol Res 90(Supp 1):S49–52
Caceres AJ, Portillo R, Acosta H, Rosales D, Quinones W, Avilan L, Salazar L, Dubourdieu M, Michels PA, Concepcion JL (2003) Molecular and biochemical characterization of hexokinase from Trypanosoma cruzi. Mol Biochem Parasitol 126:251–262
Caffrey CR, Scory S, Steverding D (2000) Cysteine proteinases of trypanosome parasites: novel targets for chemotherapy. Curr Drug Targets 1:155–162
Castro JA, Diaz de Toranzo EG (1988) Toxic effects of nifurtimox and benznidazole, two drugs used against American trypanosomiasis (Chagas’ disease). Biomed Environ Sci 1:19–33
Cazzulo JJ (2002) Proteinases of Trypanosoma cruzi: potential targets for the chemotherapy of Chagas disease. Curr Top Med Chem 2:1261–1271
Ceylan S, Seidel V, Ziebart N, Berndt C, Dirdjaja N, Krauth-Siegel RL (2010) The dithiol glutaredoxins of African trypanosomes have distinct roles and are closely linked to the unique trypanothione metabolism. J Biol Chem 285:35224–35237
Chambers JW, Kearns MT, Morris MT, Morris JC (2008a) Assembly of heterohexameric trypanosome hexokinases reveals that hexokinase 2 is a regulable enzyme. J Biol Chem 283:14963–14970
Chambers JW, Fowler ML, Morris MT, Morris JC (2008b) The anti-trypanosomal agent lonidamine inhibits Trypanosoma brucei hexokinase 1. Mol Biochem Parasitol 158:202–207
Champoux JJ, Dulbecco R (1972) An activity from mammalian cells that untwists superhelical DNA–a possible swivel for DNA replication (polyoma-ethidium bromide-mouse-embryo cells-dye binding assay). Proc Natl Acad Sci USA 69:143–146
Chawla B, Madhubala R (2010) Drug targets in Leishmania. J Parasit Dis 34:1–13
Chudzik DM, Michels PA, de Walque S, Hol WG (2000) Structures of type 2 peroxisomal targeting signals in two trypanosomatid aldolases. J Mol Biol 300:697–707
Cleghorn LA, Woodland A, Collie IT, Torrie LS, Norcross N, Luksch T, Mpamhanga C, Walker RG, Mottram JC, Brenk R, Frearson JA, Gilbert IH, Wyatt PG (2011) Identification of inhibitors of the Leishmania cdc2-related protein kinase CRK3. ChemMedChem 6:2214–2224
Coppens I, Baudhuin P, Opperdoes FR, Courtoy PJ (1988) Receptors for the host low density lipoproteins on the hemoflagellate Trypanosoma brucei: purification and involvement in the growth of the parasite. Proc Natl Acad Sci USA 85:6753–6757
Cordeiro AT, Michels PA, Delboni LF, Thiemann OH (2004) The crystal structure of glucose-6-phosphate isomerase from Leishmania mexicana reveals novel active site features. Eur J Biochem 271:2765–2772
Croft SL, Sundar S, Fairlamb AH (2006) Drug resistance in leishmaniasis. Clin Microbiol Rev 19:111–126
Crowther GJ, Shanmugam D, Carmona SJ, Doyle MA, Hertz-Fowler C, Berriman M, Nwaka S, Ralph SA, Roos DS, Van Voorhis WC, Aguero F (2010) Identification of attractive drug targets in neglected-disease pathogens using an in silico approach. PLoS Negl Trop Dis 4:e804
Das BB, Sen N, Dasgupta SB, Ganguly A, Das R, Majumder HK (2006a) Topoisomerase research of kinetoplastid parasite Leishmania, with special reference to development of therapeutics. Indian J Med Res 123:221–232
Das BB, Sen N, Ganguly A, Majumder HK (2004) Reconstitution and functional characterization of the unusual bi-subunit type I DNA topoisomerase from Leishmania donovani. FEBS Lett 565:81–88
Das BB, Sen N, Roy A, Dasgupta SB, Ganguly A, Mohanta BC, Dinda B, Majumder HK (2006b) Differential induction of Leishmania donovani bi-subunit topoisomerase I-DNA cleavage complex by selected flavones and camptothecin: activity of flavones against camptothecin-resistant topoisomerase I. Nucleic Acids Res 34:1121–1132
Datta AK, Bhaumik D, Chatterjee R (1987) Isolation and characterization of adenosine kinase from Leishmania donovani. J Biol Chem 262:5515–5521
Dax C, Duffieux F, Chabot N, Coincon M, Sygusch J, Michels PA, Blonski C (2006) Selective irreversible inhibition of fructose 1,6-bisphosphate aldolase from Trypanosoma brucei. J Med Chem 49:1499–1502
de AS Navarro MV, Gomes Dias SM, Mello LV, da Silva Giotto MT, Gavalda S, Blonski C, Garratt RC, Rigden DJ (2007) Structural flexibility in Trypanosoma brucei enolase revealed by X-ray crystallography and molecular dynamics. FEBS J 274:5077–5089
de Koning HP, Bridges DJ, Burchmore RJ (2005) Purine and pyrimidine transport in pathogenic protozoa: from biology to therapy. FEMS Microbiol Rev 29:987–1020
De Koning HP (2008) Ever increasing complexities of diamidine and arsenical cross resistance in African trypanosomes. Trends Parasitol 24:345–349
De Sousa JM, Lareau SM, Pearson RD, Carvalho EM, Mann BJ, Jeronimo SM (2003) Characterization of Leishmania chagasi DNA topoisomerase II: a potential chemotherapeutic target. Scand J Infect Dis 35:826–829
de Souza W, Rodrigues JC (2009) Sterol biosynthesis pathway as target for anti-trypanosomatid drugs. Interdiscip Perspect Infect Dis 2009:642502
Deterding A, Dungey FA, Thompson KA, Steverding D (2005) Anti-trypanosomal activities of DNA topoisomerase inhibitors. Acta Trop 93:311–316
Domenicali Pfister D, Burkard G, Morand S, Renggli CK, Roditi I, Vassella E (2006) A mitogen-activated protein kinase controls differentiation of bloodstream forms of Trypanosoma brucei. Eukaryot Cell 5:1126–1135
Douc-Rasy S, Riou JF, Ahomadegbe JC, Riou G (1988) ATP-independent DNA topoisomerase II as potential drug target in trypanosomes. Biol Cell 64:145–156
Doyle MA, MacRae JI, De Souza DP, Saunders EC, McConville MJ, Likic VA (2009) LeishCyc: a biochemical pathways database for Leishmania major. BMC Syst Biol 3:57
Doyle PS, Zhou YM, Engel JC, McKerrow JH (2007) A cysteine protease inhibitor cures Chagas’ disease in an immunodeficient-mouse model of infection. Antimicrob Agents Chemother 51:3932–3939
Drew ME, Morris JC, Wang Z, Wells L, Sanchez M, Landfear SM, Englund PT (2003) The adenosine analog tubercidin inhibits glycolysis in Trypanosoma brucei as revealed by an RNA interference library. J Biol Chem 278:46596–46600
Du X, Guo C, Hansell E, Doyle PS, Caffrey CR, Holler TP, McKerrow JH, Cohen FE (2002) Synthesis and structure-activity relationship study of potent trypanocidal thio semicarbazone inhibitors of the trypanosomal cysteine protease cruzain. J Med Chem 45:2695–2707
Eakin AE, Guerra A, Focia PJ, Torres-Martinez J, Craig SP 3rd (1997) Hypoxanthine phosphoribosyltransferase from Trypanosoma cruzi as a target for structure-based inhibitor design: crystallization and inhibition studies with purine analogs. Antimicrob Agents Chemother 41:1686–1692
El-Sayed NM, Myler PJ, Bartholomeu DC, Nilsson D, Aggarwal G, Tran AN, Ghedin E, Worthey EA, Delcher AL, Blandin G, Westenberger SJ, Caler E, Cerqueira GC, Branche C, Haas B, Anupama A, Arner E, Aslund L, Attipoe P, Bontempi E, Bringaud F, Burton P, Cadag E, Campbell DA, Carrington M, Crabtree J, Darban H, da Silveira JF, de Jong P, Edwards K, Englund PT, Fazelina G, Feldblyum T, Ferella M, Frasch AC, Gull K, Horn D, Hou L, Huang Y, Kindlund E, Klingbeil M, Kluge S, Koo H, Lacerda D, Levin MJ, Lorenzi H, Louie T, Machado CR, McCulloch R, McKenna A, Mizuno Y, Mottram JC, Nelson S, Ochaya S, Osoegawa K, Pai G, Parsons M, Pentony M, Pettersson U, Pop M, Ramirez JL, Rinta J, Robertson L, Salzberg SL, Sanchez DO, Seyler A, Sharma R, Shetty J, Simpson AJ, Sisk E, Tammi MT, Tarleton R, Teixeira S, Van Aken S, Vogt C, Ward PN, Wickstead B, Wortman J, White O, Fraser CM, Stuart KD, Andersson B (2005a) The genome sequence of Trypanosoma cruzi, etiologic agent of Chagas disease. Science 309:409–415
El-Sayed NM, Myler PJ, Blandin G, Berriman M, Crabtree J, Aggarwal G, Caler E, Renauld H, Worthey EA, Hertz-Fowler C, Ghedin E, Peacock C, Bartholomeu DC, Haas BJ, Tran AN, Wortman JR, Alsmark UC, Angiuoli S, Anupama A, Badger J, Bringaud F, Cadag E, Carlton JM, Cerqueira GC, Creasy T, Delcher AL, Djikeng A, Embley TM, Hauser C, Ivens AC, Kummerfeld SK, Pereira-Leal JB, Nilsson D, Peterson J, Salzberg SL, Shallom J, Silva JC, Sundaram J, Westenberger S, White O, Melville SE, Donelson JE, Andersson B, Stuart KD, Hall N (2005b) Comparative genomics of trypanosomatid parasitic protozoa. Science 309:404–409
Elhalem E, Bailey BN, Docampo R, Ujvary I, Szajnman SH, Rodriguez JB (2002) Design, synthesis, and biological evaluation of aryloxyethyl thiocyanate derivatives against Trypanosoma cruzi. J Med Chem 45:3984–3999
Ellis J, Sarkar M, Hendriks E, Matthews K (2004) A novel ERK-like, CRK-like protein kinase that modulates growth in Trypanosoma brucei via an autoregulatory C-terminal extension. Mol Microbiol 53:1487–1499
Engel JC, Doyle PS, Palmer J, Hsieh I, Bainton DF, McKerrow JH (1998) Cysteine protease inhibitors alter golgi complex ultrastructure and function in Trypanosoma cruzi. J Cell Sci 111(Pt 5):597–606
Fernandes Rodrigues JC, Concepcion JL, Rodrigues C, Caldera A, Urbina JA, de Souza W (2008) In vitro activities of ER-119884 and E5700, two potent squalene synthase inhibitors, against Leishmania amazonensis: antiproliferative, biochemical, and ultrastructural effects. Antimicrob Agents Chemother 52:4098–4114
Figgitt D, Denny W, Chavalitshewinkoon P, Wilairat P, Ralph R (1992) In vitro study of anticancer acridines as potential antitrypanosomal and antimalarial agents. Antimicrob Agents Chemother 36:1644–1647
Flohe L (2012) The trypanothione system and the opportunities it offers to create drugs for the neglected kinetoplast diseases. Biotechnol Adv 30:294–301
Freymann DM, Wenck MA, Engel JC, Feng J, Focia PJ, Eakin AE, Craig SP (2000) Efficient identification of inhibitors targeting the closed active site conformation of the HPRT from Trypanosoma cruzi. Chem Biol 7:957–968
Galvao-Quintao L, Alfieri SC, Ryter A, Rabinovitch M (1990) Intracellular differentiation of Leishmania amazonensis promastigotes to amastigotes: presence of megasomes, cysteine proteinase activity and susceptibility to leucine-methyl ester. Parasitology 101(Pt 1):7–13
Goad LJ, Holz GG Jr, Beach DH (1985) Effect of the allylamine antifungal drug SF 86-327 on the growth and sterol synthesis of Leishmania mexicana mexicana promastigotes. Biochem Pharmacol 34:3785–3788
Gomes FC, Ali NO, Brown E, Walker RG, Grant KM, Mottram JC (2010) Recombinant Leishmania mexicana CRK3: CYCA has protein kinase activity in the absence of phosphorylation on the T-loop residue Thr178. Mol Biochem Parasitol 171:89–96
Grant KM, Dunion MH, Yardley V, Skaltsounis AL, Marko D, Eisenbrand G, Croft SL, Meijer L, Mottram JC (2004) Inhibitors of Leishmania mexicana CRK3 cyclin-dependent kinase: chemical library screen and antileishmanial activity. Antimicrob Agents Chemother 48:3033–3042
Grant KM, Hassan P, Anderson JS, Mottram JC (1998) The crk3 gene of Leishmania mexicana encodes a stage-regulated cdc2-related histone H1 kinase that associates with p12. J Biol Chem 273:10153–10159
Guido RV, Trossini GH, Castilho MS, Oliva G, Ferreira EI, Andricopulo AD (2008) Structure-activity relationships for a class of selective inhibitors of the major cysteine protease from Trypanosoma cruzi. J Enzyme Inhib Med Chem 23:964–973
Ha S, Seo YJ, Kwon MS, Chang BH, Han CK, Yoon JH (2008) IDMap: facilitating the detection of potential leads with therapeutic targets. Bioinformatics 24:1413–1415
Hammarton TC, Clark J, Douglas F, Boshart M, Mottram JC (2003) Stage-specific differences in cell cycle control in Trypanosoma brucei revealed by RNA interference of a mitotic cyclin. J Biol Chem 278:22877–22886
Hammarton TC, Engstler M, Mottram JC (2004) The Trypanosoma brucei cyclin, CYC2, is required for cell cycle progression through G1 phase and for maintenance of procyclic form cell morphology. J Biol Chem 279:24757–24764
Hardy LW, Matthews W, Nare B, Beverley SM (1997) Biochemical and genetic tests for inhibitors of Leishmania pteridine pathways. Exp Parasitol 87:157–169
Hartsel S, Bolard J (1996) Amphotericin B: new life for an old drug. Trends Pharmacol Sci 17:445–449
Hassan P, Fergusson D, Grant KM, Mottram JC (2001) The CRK3 protein kinase is essential for cell cycle progression of Leishmania mexicana. Mol Biochem Parasitol 113:189–198
Henriksen EJ, Kinnick TR, Teachey MK, O’Keefe MP, Ring D, Johnson KW, Harrison SD (2003) Modulation of muscle insulin resistance by selective inhibition of GSK-3 in Zucker diabetic fatty rats. Am J Physiol Endocrinol Metab 284:E892–900
Hudock MP, Sanz-Rodriguez CE, Song Y, Chan JM, Zhang Y, Odeh S, Kosztowski T, Leon-Rossell A, Concepcion JL, Yardley V, Croft SL, Urbina JA, Oldfield E (2006) Inhibition of Trypanosoma cruzi hexokinase by bisphosphonates. J Med Chem 49:215–223
Iovannisci DM, Ullman B (1984) Characterization of a mutant Leishmania donovani deficient in adenosine kinase activity. Mol Biochem Parasitol 12:139–151
Ivens AC, Peacock CS, Worthey EA, Murphy L, Aggarwal G, Berriman M, Sisk E, Rajandream MA, Adlem E, Aert R, Anupama A, Apostolou Z, Attipoe P, Bason N, Bauser C, Beck A, Beverley SM, Bianchettin G, Borzym K, Bothe G, Bruschi CV, Collins M, Cadag E, Ciarloni L, Clayton C, Coulson RM, Cronin A, Cruz AK, Davies RM, De Gaudenzi J, Dobson DE, Duesterhoeft A, Fazelina G, Fosker N, Frasch AC, Fraser A, Fuchs M, Gabel C, Goble A, Goffeau A, Harris D, Hertz-Fowler C, Hilbert H, Horn D, Huang Y, Klages S, Knights A, Kube M, Larke N, Litvin L, Lord A, Louie T, Marra M, Masuy D, Matthews K, Michaeli S, Mottram JC, Muller-Auer S, Munden H, Nelson S, Norbertczak H, Oliver K, O’Neil S, Pentony M, Pohl TM, Price C, Purnelle B, Quail MA, Rabbinowitsch E, Reinhardt R, Rieger M, Rinta J, Robben J, Robertson L, Ruiz JC, Rutter S, Saunders D, Schafer M, Schein J, Schwartz DC, Seeger K, Seyler A, Sharp S, Shin H, Sivam D, Squares R, Squares S, Tosato V, Vogt C, Volckaert G, Wambutt R, Warren T, Wedler H, Woodward J, Zhou S, Zimmermann W, Smith DF, Blackwell JM, Stuart KD, Barrell B, Myler PJ (2005) The genome of the kinetoplastid parasite, Leishmania major. Science 309:436–442
John von Freyend S, Rosenqvist H, Fink A, Melzer IM, Clos J, Jensen ON, Wiese M (2010) LmxMPK4, an essential mitogen-activated protein kinase of Leishmania mexicana is phosphorylated and activated by the STE7-like protein kinase LmxMKK5. Int J Parasitol 40:969–978
Kager PA, Rees PH, Wellde BT, Hockmeyer WT, Lyerly WH (1981) Allopurinol in the treatment of visceral leishmaniasis. Trans R Soc Trop Med Hyg 75:556–559
Kaidanovich-Beilin O, Eldar-Finkelman H (2006) Long-term treatment with novel glycogen synthase kinase-3 inhibitor improves glucose homeostasis in ob/ob mice: molecular characterization in liver and muscle. J Pharmacol Exp Ther 316:17–24
Khan MO (2007) Trypanothione reductase: a viable chemotherapeutic target for antitrypanosomal and antileishmanial drug design. Drug Target Insights 2:129–146
Kim H, Feil IK, Verlinde CL, Petra PH, Hol WG (1995) Crystal structure of glycosomal glyceraldehyde-3-phosphate dehydrogenase from Leishmania mexicana: implications for structure-based drug design and a new position for the inorganic phosphate binding site. Biochemistry 34:14975–14986
Krauth-Siegel RL, Comini MA (2008) Redox control in trypanosomatids, parasitic protozoa with trypanothione-based thiol metabolism. Biochim Biophys Acta 1780:1236–1248
Krieger S, Schwarz W, Ariyanayagam MR, Fairlamb AH, Krauth-Siegel RL, Clayton C (2000) Trypanosomes lacking trypanothione reductase are avirulent and show increased sensitivity to oxidative stress. Mol Microbiol 35:542–552
LaFon SW, Nelson DJ, Berens RL, Marr JJ (1982) Purine and pyrimidine salvage pathways in Leishmania donovani. Biochem Pharmacol 31:231–238
Lakhdar-Ghazal F, Blonski C, Willson M, Michels P, Perie J (2002) Glycolysis and proteases as targets for the design of new anti-trypanosome drugs. Curr Top Med Chem 2:439–56
Legros D, Ollivier G, Gastellu-Etchegorry M, Paquet C, Burri C, Jannin J, Buscher P (2002) Treatment of human African trypanosomiasis–present situation and needs for research and development. Lancet Infect Dis 2:437–440
Leon LL, Temporal RM, Soares MJ, Grimaldi Junior G (1994) Proteinase activities during temperature-induced stage differentiation of species complexes of Leishmania. Acta Trop 56:289–298
Li Z, Wang CC (2003) A PHO80-like cyclin and a B-type cyclin control the cell cycle of the procyclic form of Trypanosoma brucei. J Biol Chem 278:20652–20658
Looker DL, Berens RL, Marr JJ (1983) Purine metabolism in Leishmania donovani amastigotes and promastigotes. Mol Biochem Parasitol 9:15–28
Lorente SO, Rodrigues JC, Jimenez Jimenez C, Joyce-Menekse M, Rodrigues C, Croft SL, Yardley V, de Luca-Fradley K, Ruiz-Perez LM, Urbina J, de Souza W, Gonzalez Pacanowska D, Gilbert IH (2004) Novel azasterols as potential agents for treatment of leishmaniasis and trypanosomiasis. Antimicrob Agents Chemother 48:2937–2950
Luscher A, Onal P, Schweingruber AM, Maser P (2007) Adenosine kinase of Trypanosoma brucei and its role in susceptibility to adenosine antimetabolites. Antimicrob Agents Chemother 51:3895–3901
Magaraci F, Jimenez CJ, Rodrigues C, Rodrigues JC, Braga MV, Yardley V, de Luca-Fradley K, Croft SL, de Souza W, Ruiz-Perez LM, Urbina J, Gonzalez Pacanowska D, Gilbert IH (2003) Azasterols as inhibitors of sterol 24-methyltransferase in Leishmania species and Trypanosoma cruzi. J Med Chem 46:4714–4727
Maldonado E, Soriano-Garcia M, Moreno A, Cabrera N, Garza-Ramos G, de Gomez-Puyou M, Gomez-Puyou A, Perez-Montfort R (1998) Differences in the intersubunit contacts in triosephosphate isomerase from two closely related pathogenic trypanosomes. J Mol Biol 283:193–203
Mallari JP, Shelat AA, Kosinski A, Caffrey CR, Connelly M, Zhu F, McKerrow JH, Guy RK (2009) Structure-guided development of selective TbcatB inhibitors. J Med Chem 52:6489–6493
Mallari JP, Zhu F, Lemoff A, Kaiser M, Lu M, Brun R, Guy RK (2010) Optimization of purine-nitrile TbcatB inhibitors for use in vivo and evaluation of efficacy in murine models. Bioorg Med Chem 18:8302–8309
Marr JJ, Berens RL (1983) Pyrazolopyrimidine metabolism in the pathogenic trypanosomatidae. Mol Biochem Parasitol 7:339–356
Marr JJ, Berens RL, Nelson DJ (1978) Purine metabolism in Leishmania donovani and Leishmania braziliensis. Biochim Biophys Acta 544:360–371
Marshall WF, Rosenbaum JL (2001) Intraflagellar transport balances continuous turnover of outer doublet microtubules: implications for flagellar length control. J Cell Biol 155:405–414
Martinez-Oyanedel J, McNae IW, Nowicki MW, Keillor JW, Michels PA, Fothergill-Gilmore LA, Walkinshaw MD (2007) The first crystal structure of phosphofructokinase from a eukaryote: Trypanosoma brucei. J Mol Biol 366:1185–1198
Martinez S, Marr JJ (1992) Allopurinol in the treatment of American cutaneous leishmaniasis. N Engl J Med 326:741–744
McNae IW, Martinez-Oyanedel J, Keillor JW, Michels PA, Fothergill-Gilmore LA, Walkinshaw MD (2009) The crystal structure of ATP-bound phosphofructokinase from Trypanosoma brucei reveals conformational transitions different from those of other phosphofructokinases. J Mol Biol 385:1519–1533
Molina J, Martins-Filho OA, Brener Z, Romanha AJ, Loebenberg D, Urbina JA (2000) Activities of the triazole derivative SCH 56592 (posaconazole) against drug-resistant strains of the protozoan parasite Trypanosoma (Schizotrypanum) cruzi in immunocompetent and immunosuppressed murine hosts. Antimicrob Agents Ch 44:150–155
Monzani PS, Trapani S, Thiemann OH, Oliva G (2007) Crystal structure of Leishmania tarentolae hypoxanthine-guanine phosphoribosyltransferase. BMC Struct Biol 7:59
Morales MA, Renaud O, Faigle W, Shorte SL, Spath GF (2007) Over-expression of Leishmania major MAP kinases reveals stage-specific induction of phosphotransferase activity. Int J Parasitol 37:1187–1199
Moreira W, Leblanc E, Ouellette M (2009) The role of reduced pterins in resistance to reactive oxygen and nitrogen intermediates in the protozoan parasite Leishmania. Free Radic Biol Med 46:367–375
Morgan HP, McNae IW, Hsin KY, Michels PA, Fothergill-Gilmore LA, Walkinshaw MD (2010) An improved strategy for the crystallization of Leishmania mexicana pyruvate kinase. Acta Crystallogr Sect F Struct Biol Cryst Commun 66:215–218
Morgan HP, Walsh MJ, Blackburn EA, Wear MA, Boxer MB, Shen M, Veith H, McNae IW, Nowicki MW, Michels PA, Auld DS, Fothergill-Gilmore LA, Walkinshaw MD (2012) A new family of covalent inhibitors block nucleotide binding to the active site of pyruvate kinase. Biochem J 448:62–72
Morris MT, DeBruin C, Yang Z, Chambers JW, Smith KS, Morris JC (2006) Activity of a second Trypanosoma brucei hexokinase is controlled by an 18-amino-acid C-terminal tail. Eukaryot Cell 5:2014–2023
Mpamhanga CP, Spinks D, Tulloch LB, Shanks EJ, Robinson DA, Collie IT, Fairlamb AH, Wyatt PG, Frearson JA, Hunter WN, Gilbert IH, Brenk R (2009) One scaffold, three binding modes: novel and selective pteridine reductase 1 inhibitors derived from fragment hits discovered by virtual screening. J Med Chem 52:4454–4465
Myler PJ (2008) Searching the Tritryp genomes for drug targets. Adv Exp Med Biol 625:133–140
Nare B, Garraway LA, Vickers TJ, Beverley SM (2009) PTR1-dependent synthesis of tetrahydrobiopterin contributes to oxidant susceptibility in the trypanosomatid protozoan parasite Leishmania major. Curr Genet 55:287–299
Nare B, Hardy LW, Beverley SM (1997) The roles of pteridine reductase 1 and dihydrofolate reductase-thymidylate synthase in pteridine metabolism in the protozoan parasite Leishmania major. J Biol Chem 272:13883–13891
Naula C, Parsons M, Mottram JC (2005) Protein kinases as drug targets in trypanosomes and Leishmania. Biochim Biophys Acta 1754:151–159
Neal RA, Croft SL (1984) An in-vitro system for determining the activity of compounds against the intracellular amastigote form of Leishmania donovani. J Antimicrob Chemother 14:463–475
Nenortas E, Burri C, Shapiro TA (1999) Antitrypanosomal activity of fluoroquinolones. Antimicrob Agents Chemother 43:2066–2068
Nenortas E, Kulikowicz T, Burri C, Shapiro TA (2003) Antitrypanosomal activities of fluoroquinolones with pyrrolidinyl substitutions. Antimicrob Agents Chemother 47:3015–3017
Nowicki MW, Tulloch LB, Worralll L, McNae IW, Hannaert V, Michels PA, Fothergill-Gilmore LA, Walkinshaw MD, Turner NJ (2008) Design, synthesis and trypanocidal activity of lead compounds based on inhibitors of parasite glycolysis. Bioorg Med Chem 16:5050–5061
Nussbaum K, Honek J, Cadmus CM, Efferth T (2010) Trypanosomatid parasites causing neglected diseases. Curr Med Chem 17:1594–1617
O’Brien TC, Mackey ZB, Fetter RD, Choe Y, O’Donoghue AJ, Zhou M, Craik CS, Caffrey CR, McKerrow JH (2008) A parasite cysteine protease is key to host protein degradation and iron acquisition. J Biol Chem 283:28934–28943
Oduor RO, Ojo KK, Williams GP, Bertelli F, Mills J, Maes L, Pryde DC, Parkinson T, Van Voorhis WC, Holler TP (2011) Trypanosoma brucei glycogen synthase kinase-3, a target for anti-trypanosomal drug development: a public-private partnership to identify novel leads. PLoS Negl Trop Dis 5:e1017
Ojo KK, Arakaki TL, Napuli AJ, Inampudi KK, Keyloun KR, Zhang L, Hol WG, Verlinde CL, Merritt EA, Van Voorhis WC (2011) Structure determination of glycogen synthase kinase-3 from Leishmania major and comparative inhibitor structure-activity relationships with Trypanosoma brucei GSK-3. Mol Biochem Parasitol 176:98–108
Ojo KK, Gillespie JR, Riechers AJ, Napuli AJ, Verlinde CL, Buckner FS, Gelb MH, Domostoj MM, Wells SJ, Scheer A, Wells TN, Van Voorhis WC (2008) Glycogen synthase kinase 3 is a potential drug target for African trypanosomiasis therapy. Antimicrob Agents Chemother 52:3710–3717
Olivares-Illana V, Perez-Montfort R, Lopez-Calahorra F, Costas M, Rodriguez-Romero A, Tuena de Gomez-Puyou M, Gomez Puyou A (2006) Structural differences in triosephosphate isomerase from different species and discovery of a multitrypanosomatid inhibitor. Biochemistry 45:2556–2560
Olivares-Illana V, Rodríguez-Romero A, Becker I, Berzunza M, García J, Pérez-Montfort R, Cabrera N, López-Calahorra F, de Gómez-Puyou MT, Gómez-Puyou A (2007) Perturbation of the dimer interface of triosephosphate isomerase and its effect on Trypanosoma cruzi. PLoS Negl Trop Dis 1(1):e01
Orenes Lorente S, Gomez R, Jimenez C, Cammerer S, Yardley V, de Luca-Fradley K, Croft SL, Ruiz Perez LM, Urbina J, Gonzalez Pacanowska D, Gilbert IH (2005) Biphenylquinuclidines as inhibitors of squalene synthase and growth of parasitic protozoa. Bioorg Med Chem 13:3519–3529
Padhy BM, Gupta YK (2011) Drug repositioning: re-investigating existing drugs for new therapeutic indications. J Postgrad Med 57:153–160
Phukan S, Babu VS, Kannoji A, Hariharan R, Balaji VN (2010) GSK3beta: role in therapeutic landscape and development of modulators. Br J Pharmacol 160:1–19
Polychronopoulos P, Magiatis P, Skaltsounis AL, Myrianthopoulos V, Mikros E, Tarricone A, Musacchio A, Roe SM, Pearl L, Leost M, Greengard P, Meijer L (2004) Structural basis for the synthesis of indirubins as potent and selective inhibitors of glycogen synthase kinase-3 and cyclin-dependent kinases. J Med Chem 47:935–946
Racagni GE, Machado de Domenech EE (1983) Characterization of Trypanosoma cruzi hexokinase. Mol Biochem Parasitol 9:181–188
Robays J, Nyamowala G, Sese C, Betu Ku Mesu Kande V, Lutumba P, Van der Veken W, Boelaert M (2008) High failure rates of melarsoprol for sleeping sickness, Democratic Republic of Congo. Emerg Infect Dis 14:966–967
Robertson SA, Renslo AR (2011) Drug discovery for neglected tropical diseases at the Sandler Center. Future Med Chem 3:1279–1288
Rodrigues-Poveda CA, Gonzalez-Pacanowska D, Szajnman SH, Rodriguez JB (2012) 2-Alkylaminoethyl-1,1-Bisphosphonic acids are potent inhibitors of the enzymatic activity of Trypanosoma cruzi squalene synthase. Antimicrob Agents Chemother 56:4483–4486
Rodrigues JC, Attias M, Rodriguez C, Urbina JA, Souza W (2002) Ultrastructural and biochemical alterations induced by 22,26-azasterol, a delta(24(25))-sterol methyltransferase inhibitor, on promastigote and amastigote forms of Leishmania amazonensis. Antimicrob Agents Chemother 46:487–499
Romeiro NC, Aguirre G, Hernandez P, Gonzalez M, Cerecetto H, Aldana I, Perez-Silanes S, Monge A, Barreiro EJ, Lima LM (2009) Synthesis, trypanocidal activity and docking studies of novel quinoxaline-N-acylhydrazones, designed as cruzain inhibitors candidates. Bioorg Med Chem 17:641–652
Rottenberg ME, Masocha W, Ferella M, Petitto-Assis F, Goto H, Kristensson K, McCaffrey R, Wigzell H (2005) Treatment of African trypanosomiasis with cordycepin and adenosine deaminase inhibitors in a mouse model. J Infect Dis 192:1658–1665
Salem MM, Werbovetz KA (2005) Antiprotozoal compounds from Psorothamnus polydenius. J Nat Prod 68:108–111
Sanz-Rodriguez CE, Concepcion JL, Pekerar S, Oldfield E, Urbina JA (2007) Bisphosphonates as inhibitors of Trypanosoma cruzi hexokinase: kinetic and metabolic studies. J Biol Chem 282:12377–12387
Schurigt U, Schad C, Glowa C, Baum U, Thomale K, Schnitzer JK, Schultheis M, Schaschke N, Schirmeister T, Moll H (2010) Aziridine-2,3-dicarboxylate-based cysteine cathepsin inhibitors induce cell death in Leishmania major associated with accumulation of debris in autophagy-related lysosome-like vacuoles. Antimicrob Agents Chemother 54:5028–5041
Sealey-Cardona M, Cammerer S, Jones S, Ruiz-Perez LM, Brun R, Gilbert IH, Urbina JA, Gonzalez-Pacanowska D (2007) Kinetic characterization of squalene synthase from Trypanosoma cruzi: selective inhibition by quinuclidine derivatives. Antimicrob Agents Chemother 51:2123–2129
Sett R, Basu N, Ghosh AK, Das PK (1992) Potential of doxorubicin as an antileishmanial agent. J Parasitol 78:350–354
Sienkiewicz N, Jaroslawski S, Wyllie S, Fairlamb AH (2008) Chemical and genetic validation of dihydrofolate reductase-thymidylate synthase as a drug target in African trypanosomes. Mol Microbiol 69:520–533
Singh G, Dey CS (2007) Induction of apoptosis-like cell death by pentamidine and doxorubicin through differential inhibition of topoisomerase II in arsenite-resistant L. donovani. Acta Trop 103:172–185
Singh N, Kumar M, Singh RK (2012) Leishmaniasis: current status of available drugs and new potential drug targets. Asian Pac J Trop Med 5:485–497
Smirlis D, Duszenko M, Ruiz AJ, Scoulica E, Bastien P, Fasel N, Soteriadou K (2010) Targeting essential pathways in trypanosomatids gives insights into protozoan mechanisms of cell death. Parasit Vectors 3:107
Smirlis D, Soteriadou K (2011) Trypanosomatid apoptosis: ‘apoptosis’ without the canonical regulators. Virulence 2:253–256
Souza DH, Garratt RC, Araujo AP, Guimaraes BG, Jesus WD, Michels PA, Hannaert V, Oliva G (1998) Trypanosoma cruzi glycosomal glyceraldehyde-3-phosphate dehydrogenase: structure, catalytic mechanism and targeted inhibitor design. FEBS Lett 424:131–135
Steverding D, Wang X (2009) Evaluation of anti-sleeping-sickness drugs and topoisomerase inhibitors in combination on Trypanosoma brucei. J Antimicrob Chemother 63:1293–1295
Strauss PR, Wang JC (1990) The TOP2 gene of Trypanosoma brucei: a single-copy gene that shares extensive homology with other TOP2 genes encoding eukaryotic DNA topoisomerase II. Mol Biochem Parasitol 38:141–150
Suckling KE (2006) The return of two old targets? Expert Opin Ther Targets 10:785–788
Suresh S, Bressi JC, Kennedy KJ, Verlinde CL, Gelb MH, Hol WG (2001) Conformational changes in Leishmania mexicana glyceraldehyde-3-phosphate dehydrogenase induced by designed inhibitors. J Mol Biol 309:423–435
Teixeira SM, de Paiva RM, Kangussu-Marcolino MM, Darocha WD (2012) Trypanosomatid comparative genomics: contributions to the study of parasite biology and different parasitic diseases. Genet Mol Biol 35:1–17
Torrie LS, Wyllie S, Spinks D, Oza SL, Thompson S, Harrison JR, Gilbert IH, Wyatt PG, Fairlamb AH, Frearson JA (2009) Chemical validation of trypanothione synthetase: a potential drug target for human trypanosomiasis. J Biol Chem 284:36137–36145
Tu X, Wang CC (2004) The involvement of two cdc2-related kinases (CRKs) in Trypanosoma brucei cell cycle regulation and the distinctive stage-specific phenotypes caused by CRK3 depletion. J Biol Chem 279:20519–20528
Tulloch LB, Morgan HP, Hannaert V, Michels PA, Fothergill-Gilmore LA, Walkinshaw MD (2008) Sulphate removal induces a major conformational change in Leishmania mexicana pyruvate kinase in the crystalline state. J Mol Biol 383:615–626
Urbina JA (2002) Chemotherapy of Chagas disease. Curr Pharm Des 8:287–295
Urbina JA (2010) Specific chemotherapy of Chagas disease: relevance, current limitations and new approaches. Acta Trop 115:55–68
Urbina JA, Concepcion JL, Caldera A, Payares G, Sanoja C, Otomo T, Hiyoshi H (2004) In vitroand in vivo activities of E5700 and ER-119884, two novel orally active squalene synthase inhibitors, against Trypanosoma cruzi. Antimicrob Agents Chemother 48:2379–2387
Urbina JA, Concepcion JL, Montalvetti A, Rodriguez JB, Docampo R (2003) Mechanism of action of 4-phenoxyphenoxyethyl thiocyanate (WC-9) against Trypanosoma cruzi, the causative agent of Chagas’ disease. Antimicrob Agents Chemother 47:2047–2050
Urbina JA, Concepcion JL, Rangel S, Visbal G, Lira R (2002) Squalene synthase as a chemotherapeutic target in Trypanosoma cruzi and Leishmania mexicana. Mol Biochem Parasitol 125:35–45
Urbina JA, Crespo A (1984) Regulation of energy metabolism in Trypanosoma (Schizotrypanum) cruzi epimastigotes. I. Hexokinase and phosphofructokinase. Mol Biochem Parasitol 11:225–239
Urbina JA, Docampo R (2003) Specific chemotherapy of Chagas disease: controversies and advances. Trends Parasitol 19:495–501
Urbina JA, Lazardi K, Aguirre T, Piras MM, Piras R (1988) Antiproliferative synergism of the allylamine SF 86-327 and ketoconazole on epimastigotes and amastigotes of Trypanosoma (Schizotrypanum) cruzi. Antimicrob Agents Chemother 32:1237–1242
Urbina JA, Payares G, Molina J, Sanoja C, Liendo A, Lazardi K, Piras MM, Piras R, Perez N, Wincker P, Ryley JF (1996a) Cure of short- and long-term experimental Chagas’ disease using D0870. Science 273:969–971
Urbina JA, Vivas J, Lazardi K, Molina J, Payares G, Piras MM, Piras R (1996b) Antiproliferative effects of delta 24(25) sterol methyl transferase inhibitors on Trypanosoma (Schizotrypanum) cruzi: in vitro and in vivo studies. Chemotherapy 42:294–307
Urbina JA, Vivas J, Visbal G, Contreras LM (1995) Modification of the sterol composition of Trypanosoma (Schizotrypanum) cruzi epimastigotes by delta 24(25)-sterol methyl transferase inhibitors and their combinations with ketoconazole. Mol Biochem Parasitol 73:199–210
Van Hellemond JJ, Neuville P, Schwarz RT, Matthews KR, Mottram JC (2000) Isolation of Trypanosoma brucei CYC2 and CYC3 cyclin genes by rescue of a yeast G(1) cyclin mutant. Functional characterization of CYC2. J Biol Chem 275:8315–8323
Vannier-Santos MA, Urbina JA, Martiny A, Neves A, de Souza W (1995) Alterations induced by the antifungal compounds ketoconazole and terbinafine in Leishmania. J Eukaryot Microbiol 42:337–346
Vellieux FM, Hajdu J, Verlinde CL, Groendijk H, Read RJ, Greenhough TJ, Campbell JW, Kalk KH, Littlechild JA, Watson HC et al (1993) Structure of glycosomal glyceraldehyde-3-phosphate dehydrogenase from Trypanosoma brucei determined from Laue data. Proc Natl Acad Sci USA 90:2355–2359
Verlinde CL, Hannaert V, Blonski C, Willson M, Perie JJ, Fothergill-Gilmore LA, Opperdoes FR, Gelb MH, Hol WG, Michels PA (2001) Glycolysis as a target for the design of new anti-trypanosome drugs. Drug Resist Updat 4:50–65
Walker RG, Thomson G, Malone K, Nowicki MW, Brown E, Blake DG, Turner NJ, Walkinshaw MD, Grant KM, Mottram JC (2011) High throughput screens yield small molecule inhibitors of Leishmania CRK3: CYC6 cyclin-dependent kinase. PLoS Negl Trop Dis 5:e1033
Wang Q, Melzer IM, Kruse M, Sander-Juelch C, Wiese M (2005) LmxMPK4, a mitogen-activated protein (MAP) kinase homologue essential for promastigotes and amastigotes of Leishmania mexicana. Kinetoplastid Biol Dis 4:6
Wang Y, Dimitrov K, Garrity LK, Sazer S, Beverley SM (1998) Stage-specific activity of the Leishmania major CRK3 kinase and functional rescue of a Schizosaccharomyces pombe cdc2 mutant. Mol Biochem Parasitol 96:139–150
Wierenga RK, Noble ME, Postma JP, Groendijk H, Kalk KH, Hol WG, Opperdoes FR (1991a) The crystal structure of the “open” and the “closed” conformation of the flexible loop of trypanosomal triosephosphate isomerase. Proteins 10:33–49
Wierenga RK, Noble ME, Vriend G, Nauche S, Hol WG (1991b) Refined 1.83 a structure of trypanosomal triosephosphate isomerase crystallized in the presence of 2.4 M-ammonium sulphate. A comparison with the structure of the trypanosomal triosephosphate isomerase-glycerol-3-phosphate complex. J Mol Biol 220:995–1015
Wiese M (1998) A mitogen-activated protein (MAP) kinase homologue of Leishmania mexicana is essential for parasite survival in the infected host. EMBO J 17:2619–2628
Wiese M (2007) Leishmania MAP kinases–familiar proteins in an unusual context. Int J Parasitol 37:1053–1062
Williams JC, Zeelen JP, Neubauer G, Vriend G, Backmann J, Michels PA, Lambeir AM, Wierenga RK (1999) Structural and mutagenesis studies of leishmania triosephosphate isomerase: a point mutation can convert a mesophilic enzyme into a superstable enzyme without losing catalytic power. Protein Eng 12:243–250
Williamson J, Scott-Finnigan TJ (1978) Trypanocidal activity of antitumor antibiotics and other metabolic inhibitors. Antimicrob Agents Chemother 13:735–744
Willson M, Lauth N, Perie J, Callens M, Opperdoes FR (1994) Inhibition of glyceraldehyde-3-phosphate dehydrogenase by phosphorylated epoxides and alpha-enones. Biochemistry 33:214–220
Xingi E, Smirlis D, Myrianthopoulos V, Magiatis P, Grant KM, Meijer L, Mikros E, Skaltsounis AL, Soteriadou K (2009) 6-Br-5methylindirubin-3′oxime (5-Me-6-BIO) targeting the leishmanial glycogen synthase kinase-3 (GSK-3) short form affects cell-cycle progression and induces apoptosis-like death: exploitation of GSK-3 for treating leishmaniasis. Int J Parasitol 39:1289–1303
Zhu F, Han B, Kumar P, Liu X, Ma X, Wei X, Huang L, Guo Y, Han L, Zheng C, Chen Y (2010) Update of TTD: therapeutic target database. Nucleic Acids Res 38:D787–791
Acknowledgements
The authors wish to thank the FP7-PEOPLE-2010-IRSES program “ChemBioFight” (Exploring chemical biodiversity with innovative approaches for fighting Chagas and leishmaniasis, grant number 269031) for financial support.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Smirlis, D., Soares, M.B.P. (2014). Selection of Molecular Targets for Drug Development Against Trypanosomatids. In: Santos, A., Branquinha, M., d’Avila-Levy, C., Kneipp, L., Sodré, C. (eds) Proteins and Proteomics of Leishmania and Trypanosoma. Subcellular Biochemistry, vol 74. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-7305-9_2
Download citation
DOI: https://doi.org/10.1007/978-94-007-7305-9_2
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-7304-2
Online ISBN: 978-94-007-7305-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)