Abstract
A population of multipotent stromal cells exists within bone marrow and other adult tissues, which is able to differentiate into different skeletal tissues such as bone, cartilage and fat. These cells are frequently referred to as mesenchymal stem cells (MSCs) and offer significant therapeutic potential, particularly in orthopaedic applications, but may also have broader roles in regenerative medicine, cancer treatment, as anti-inflammatories, immunosuppressives and vehicles for gene/protein therapy. Much attention has focused on understanding MSC biology and the regulation of differentiation to help realise these clinical aspirations. Here we review some of the key molecular determinants of MSC function, with an emphasis on transcription factor control and the cell-cell signalling pathways that regulate MSC differentiation. The source information comes from a range of different models, including isolated human MSC cultures, animal-derived MSC-like cell lines, animal models and skeletal developmental processes to provide a wide-angled overview of the important players in MSC biology and tri-lineage specification.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
1.1 Origins of MSCs
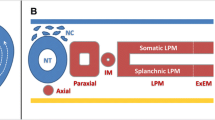
The proposal for the existence of a population of multipotent stromal cells/mesenchymal stem cells (MSCs) was first put forward by Friendenstein and colleagues [1], who reported a population of bone marrow stromal cells capable of generating bone following heterotopic transplantation. The same group later showed that these precursors were a subset of fibroblast like cells capable of forming colonies, termed colony-forming unit fibroblasts (CFU-Fs), when selected by adherence to plastic surfaces [2]. Subsequent work showed the ability of these cultured cells derived from a single CFU-F to proliferate in vitro, whist maintaining their ability to differentiate into osteoblasts, adipocytes and chondrocytes [3]. Together, these data are characteristics of two hallmarks of stemness; the ability to self renew, and to differentiate into multiple lineages, consequently these cells came to be commonly known as mesenchymal stem cells (Fig. 12.1).
Potency of MSCs. MSCs are a multipotent cell capable of self renewal, and differentiation into multiple mesenchymal lineages, including osteoblasts, osteocytes, chondrocytes and adipocytes. MSCs differentiate through a series of committed progenitor cells, and differentiated stages before final maturation into fully committed terminally differentiated cells (Adapted from Caplan and Bruder [106])
Since their discovery MSCs have generated a lot of interest in the biomedical field as a source for stem cell therapies, with their relatively simple ex vivo expansion, multilineage capacity and potential for autologous transplantation. Indeed, clinical trials have been performed in patients with osteogenesis imperfecta, where allogeneic bone marrow-derived MSCs were given to patients after bone marrow transplantation. MSC engraftment was shown and a marked increase in patient recovery was detected [4]. The use of MSCs in tissue engineering is also an area of great scientific interest, with multiple groups generating novel scaffolds and delivery procedures for tissue repair. Tissue engineering involves the generation of a biocompatible scaffold on which cells are cultured before implanting into the patient, and in the case of MSCs this requires a thorough understanding of the differentiation process to ensure correct function of the implanted construct.
The study of MSCs in vivo and the isolation of MSC populations has been hindered by the lack of specific cell surface markers for immuno-phenotype identification. Cultured human mesenchymal stem cells do express a panel of cell surface markers, such as CD105, CD73 and CD90, and lack CD45, CD34 and CD14 [5], however these can be donor-, isolation- and passage-dependent and may not represent the true in vivo MSC population. Due to the difficulty in identifying MSCs in vivo, the majority of work studying the properties of MSCs has been performed using cultured MSCs selected by adherence to culture plastic. However, this generates problems of its own, with different species, isolation techniques, culture conditions and donor sites generating increased complexity in the system. Furthermore, some studies of MSC differentiation have been performed not with primary cells, but with cell lines such as C3H10T1/2 [6, 7] and MC3T3-E1 for osteogenesis, and MC3T3-L1 for adipogenesis, preventing the direct extrapolation of the findings to human MSCs. In addition to the difficulties faced with inter-sample variation, there is the added problem of having highly heterogeneous MSC populations.
MSCs are defined by their ability to adhere to plastic and ability to differentiate into osteoblasts, adipocytes and chondrocytes. MSCs are classically derived from the bone marrow [3], however they have now been isolated from many adult stromal tissues [8], with the more common sources for in vitro differentiation analysis being bone marrow, adipose tissue, and periosteum.
1.2 In Vitro Differentiation of MSCs
MSCs have the ability to differentiate into osteoblasts, adipocytes and chondrocytes by definition, and various methods have been developed to mimic these processes in vitro. Osteoblasts develop through a series of phases, initiated by cellular proliferation, followed by extracellular matrix maturation and matrix mineralisation. These changes in cellular activity correlate with a pattern of maturation of the cells from committed osteoprogenitors to pre- and finally terminally differentiated osteoblasts. This process of cell maturation can be induced in vitro by the addition of bone morphogenetic proteins (BMPs), often BMP-2 [9], or the addition of a differentiation cocktail of dexamethasone, ascorbate and β-glycerophosphate [10]. While both these methods are capable of inducing the osteogenic differentiation of MSCs, it is likely that they act through different mechanisms to generate a comparable response. As with osteoblasts, adipocytes mature though a series of increasingly committed cell types, before becoming terminally differentiated adipocytes, expressing adipocyte specific markers such as FABP4 and 5 [11] and forming lipid vesicles. In vitro adipogenesis can be induced in MSCs by the addition of a differentiation cocktail of dexamethasone, isobutylmethylxanthine (IBMX), indomethacin and insulin. Methods to induce the process of chondrogenesis have also been developed in vitro. Chondrogenic differentiation in vivo requires an initial condensation of the MSCs, which is mimicked in vitro by culturing MSCs as micromass pellets. Chondrogenic differentiation can then be induced by the presence of transforming growth factor-β (TGF-β) resulting in the appearance of a chondrocyte-like phenotype characterised by upregulation of cartilage-specific molecules such as collagen type II and IX, aggrecan, versican, biglycan, and decorin [12]. Differentiating chondrocytes mature through a sequence of defined steps, initially the MSCs differentiate into a proliferative non-hypertrophic stage termed chondroblasts. This stage is characterised by a change from collagen type-I to type-II, IX and XI expression and a highly order columnar organisation. This stage is then followed by a hypertrophic stage, marked by the expression of collagen type-X, which is vital for vascular invasion, osteoblast differentiation, and bone formation.
2 Transcription Factors in MSC Differentiation
2.1 Osteogenesis
A range of transcription factors are known to be involved in the regulation of osteogenesis [13], with two of the more widely studied being Runx2 (Cbfa1) and Osterix. Runx2 is considered the major transcription factor controlling osteoblast commitment and differentiation. Runx2 is a member of the Runt-domain gene family and is expressed in mesenchymal cells early in skeletal development and throughout osteoblast differentiation with molecular and genetic studies indicating its necessity in osteoblast differentiation of mesenchymal cells [14–16]. Runx2 was identified as an important transcription factor in osteogenesis by its binding to a cis-element on the osteocalcin gene and its forced expression in osteoblast precursor cells, MC3T3-E1, caused the transcription of the osteoblast specific genes osteocalcin and collagen 1A1. Further research showed that overexpression of Runx2 can induce osteogenesis in vitro and in vivo. This was demonstrated by increased osteoblastic markers, osteopontin and osteocalcin, increased alkaline phosphatase (ALP) expression and mineralisation in vitro, while in vivo studies showed accelerated healing in critical-sized skull defects [17]. Conversely, Runx2 null mice showed a complete absence of ossification, owing to the maturational arrest of osteoblasts [15]. More recent work has also implicated Runx2 in the trans-differentiation of preadipocytes into osteoblasts. Takahashi (2011), demonstrated that over expression of Runx2 in the preadipocyte cell line, 3T3-E1, resulted in a decrease in the adipocyte markers PPARγ2 and C/EBPα and an increase in osteogenic markers such as ALP, osteocalcin and bone sialoprotein 2 (BSP) [18]. This trans-differentiation was further enhanced by the addition of dexamethasone or the overexpression of the mitogen-activated protein kinase phosphatase-1 (MKP-1). The phosphorylation status of Runx2 is also important. Dexamethasone, a synthetic glucocorticoid, acts to enhance the activity of Runx2 by reducing the amount of Runx2 phosphoserine levels via MKP-1 [19]. While others have demonstrated the phosphorylation of Runx2 on tyrosine, theonine and serine residues increases during dexamethasone induced osteogenesis [20].
Osterix (Osx) is another important transcription factor involved in osteoblast commitment, with Osx-deficient mice showing an absence of osteoblasts and defective bone formation [21]. However, Osx appears to act downstream of Runx2 as Osx is not expressed in Runx2 null mice, but Runx2 expression remains in Osx null mice [21]. The studies into the effects of overexpression of Osx are a little less clear, with multiple groups demonstrating that Osx overexpression is sufficient to induce osteogenesis [22, 23], where as Kurata et al. [24] recorded that Osx overexpression was capable of initiating osteogenesis, shown by early marker expression, but failed to generate terminally differentiated osteoblasts [24].
Other transcription factors of interest in relation to osteogenesis are the Msx/Dlx family of transcription factors. Dlx and Msx are homeodomain transcription factors homologous to the Drosophila Distal-less and muscle specific homeobox genes. Dlx5 and 6 are expressed in very similar patterns throughout almost all of the skeletal elements [25]. Furthermore, overexpression of Dlx5 can accelerate osteoblast differentiation in vitro [26]. Conversely, Dlx5 knockout mice have craniofacial and sensory skeletal defects [27], while double knockouts of Dlx5 and 6 have more severe defects [28], suggesting partial redundancy or compensation between the two transcription factors. Dlx3 is also implicated in osteogeneic differentiation, with expression of Dlx3 in the mouse embryo being associated with new bone formation and regulation of osteoblast differentiation. Furthermore, Dlx3 is expressed in ex vivo osteoblasts, whilst overexpression and RNAi knock down result in increased and decreased osteogenesis respectively [29]. In contrast to the Dlx transcription factors, Msx2 is expressed in the proliferating osteogenic precursors, and not the differentiated cells [29]. Overexpression of Msx2 prevented osteogenic differentiation and mineralisation, while overexpression of the antisense mRNA resulted in decreased proliferation and enhanced osteogenesis [30].
2.2 Adipogenesis
Peroxisome proliferator activated receptor-γ (PPARγ) is a nuclear hormone receptor, thought to be the master regulator of adipogenesis. There are two isoforms of PPARγ, generated by alternate splice sites. PPARγ1 is ubiquitously expressed whilst PPARγ2 is restricted to adipose tissues and appears to be a more potent stimulator of adipogenesis [31]. PPARγ was discovered as key player in adipogenesis through its interaction with the 5′-flanking region of the adipocyte P2 gene, a gene capable of inducing adipocyte specific gene expression. It was subsequently shown to be expressed very early in the differentiation of adipocytes, with forced overexpression of PPARγ inducing adipogenesis in cultured fibroblasts [32]. Interestingly, this induction was not limited to fibroblastic cells; myoblastic cell lines can also be transdifferentiated to adipocytes [33]. Once again complementary experiments have been performed, in which PPARγ was deleted in fibroblasts, resulting in reduced adipogenesis (<2 % efficiency) even with the addition of C/EBPα, another regulator of adipogenesis [34]. These results and others suggest PPARγ is both sufficient and indispensable for adipogenic differentiation. While PPARγ is widely considered the master regulator of adipogenesis, it has also been implicated in the reciprocal regulation of adipogenesis and osteogenesis. Akune et al. [35] showed that embryonic stem cells from homozygous PPARγ-deficient mice would spontaneously differentiate into osteoblasts, while PPARγ haploinsufficiency resulted in enhanced bone formation with increased osteogenesis from bone marrow progenitors both in vivo and ex vivo [35].
CAAT/enhancer binding proteins (C/EBPs) are members of the basic-leucine zipper class of transcription factors, which function as homo- or heterodimers with other C/EBP family members. There are three C/EBPs which play a role in adipogenesis, C/EBPα, β and δ, of which C/EBPα has the most prominent role. A dramatic demonstration of this effect was shown by the overexpression of C/EBPα in fibroblastic cells, resulting in the induction of adipogenesis in up to 50 % of the cells [36]; conversely antisense mRNA knockdown resulted in reduced adipose phenotype in differentiated 3T3-L1 cells [37]. Similar results were obtained in mouse models, in which C/EBPα expression was restricted to the liver, showed reduced adipose tissue [38]. When studying the levels of endogenous C/EBPs, during adipogenesis of cultured cells, it was noted that C/EBPα is expressed late in the differentiation process immediately prior to the activation of the many adipo-specific genes, while C/EBPβ and δ are only transiently expressed, accumulating during the early stages of differentiation, before diminishing prior to terminal differentiation [39]. C/EBPβ and δ act early in the differentiation process to relay the hormonal signals, leading to the activation of C/EBPα [39]. This signal transduction is likely to function through the activation of PPARγ, via C/EBP binding sites in the PPAR promoter. This PPARγ expression is then thought to activate C/EBPα, which then enters a positive feedback loop, increasing the expression of PPARγ (Fig. 12.2). This process is apparent through the generation of PPARγ and C/EBPα null cell lines [40, 41], where PPARγ null cells fail to express C/EBPα despite normal early differentiation [40]. Additionally, C/EBPα null fibroblasts have reduced levels of PPARγ expression, which can be rescued by retroviral transfection and expression of C/EBPα [41]. It is thought that this positive feedback loop maintains the expression of these two important transcription factors through to terminal differentiation of the adipocytes.
Role of Wnt and BMPs in Osteoblast/Adipocyte lineage commitment. Wnt signalling is vital for the commitment decision of MSCs between osteoblasts and adipocytes, acting through the inhibition of PPARγ to prevent adipogenesis and activate osteogenesis via Runx2. BMPs induce the osteogenic differentiation of MSCs via Dlx5 and Runx2. The BMP signalling components SMAD1/5 can also be directed to transcriptional foci by Runx2
Another transcription factor of note for its pro-adipogenic effects is Sterol regulatory binding element protein-1 (SREBP1)/Adipocyte differentiation and determination factor-1 (Add1). Dominant negative expression of SREBP1 in 3T3-L1 (pre-adipocyte line) cells sharply repressed adipogenic differentiation, while overexpression of SREBP1 in the fibroblastic line, NIH-3T3, increased adipogenesis in a synergistic manner with PPARγ overexpression, suggesting its involvement in this pathway [42] (Fig. 12.2). SREBP1 exerts it pro- adipogenic effects through the interaction with E-box domains in the PPARγ promoter regions, allowing further regulation of PPARγ gene expression [43].
As with osteogenesis, there are also transcription factors involved in the inhibition of adipogenesis. C/EBP homologous proteins (CHOPs) negatively regulate adipogenesis through interactions with C/EBPs. CHOP10 for example binds to C/EBPβ early during differentiation, preventing it from binding PPARγ, thereby delaying the terminal differentiation of adipocytes, allowing for the initial clonal expansion step [44]. The activity of SREBP1 is also negatively regulated during adipogenesis, by the binding of Inhibitor of DNA binding (Id) proteins which prevent SREBP1 from binding to the E-box DNA regulatory sequences [45]. Another transcription factor important in the negative regulation of adipogenesis is GATA binding transcription factor (GATAs) family. GATA2 and 3 have been shown to be expressed in pre-adipocytes, and their down regulation leads to enhanced adipogenesis. Forced expression of GATA2 and 3 prevents the switch from pre-adipocytes to mature adipocytes, in part through binding directly to PPARγ [46], but also through the formation of protein complexes with C/EBPα or β [47].
2.3 Chondrogenesis
As with both adipogenesis and osteogenesis, there is an apparent master regulator of chondrogenesis, Sox9. Sox9 is a member of a family of transcription factors that contain a HMG-type DNA binding domain, and is expressed throughout chondrogenic differentiation until the cells become hypertrophic, where it is rapidly shut off [48]. The requirement for Sox9 is clearly demonstrated in the work by Akiyama et al. [49], where deletion of Sox9 expression in the mesenchymal cells of limb buds lead to the complete absence of chondrogenic mesenchymal condensations in the developing limbs, while deletion of the Sox9 gene in mesenchymal condensations lead to the arrest of chondrogenesis at this stage [49]. These results clearly demonstrated that Sox9 was vital for chondrogenesis, and plays important roles in both mesenchymal condensation and for chondrogenic progression.
Furthermore, Sox9 was identified as part of a triad of Sox genes which are sufficient for the induction of chondrogenesis in embryonic stem cells [50]. Two other members of the Sox family of transcription factors also play a role in chondrogenesis L-Sox5 and Sox6. L-Sox5 and Sox6 differ from Sox9 in that they do not possess a transactivation domain and therefore do not affect gene expression directly, but are thought to alter gene expression through the recruitment of other transcriptional activators [51]. L-Sox5 and Sox6 are coexpressed with Sox9 during chondrogenesis and therefore share expression patterns with the chondrogenic marker Col2A1, prompting further studies into the role of these transcription factors in chondrogenesis. L-Sox5- and Sox6-deficient mice present chondrogenic defects, with the dual knockout generating a more severe phenotype, suggesting some redundancy. However, in contrast to Sox9-deficient mice, Sox5/6-deficient mice do develop chondrogenic mesenchymal condensations [52], implicating their role as being later in the differentiation process. It is thought that these three Sox transcription factors work in collaboration to activate chondrocyte-specific markers, with enhanced Col2A1 reporter expression when all three Sox genes are coexpressed in non-chondrogenic cells [53]. Similarly the three Sox proteins have been shown to cooperatively activate the chondrocyte marker Col11A2 [54]. As discussed above, Sox transcription factors are required for the progression of chondrogenesis, but over expression of the Sox triad also causes chondrogenesis arrest in the pre-hypertrophic cells preventing terminal differentiation [50]. It is thought that this terminal differentiation inhibition is at least in part due to the action of two genes, S110A1 and S100B, members of the S100 protein family which carry the Ca2+-binding EF-hand motif. These proteins are expressed during the late proliferative and pre-hypertrophic stages of chondrogenesis, and when overexpressed in chondrogenesis inhibited the terminal differentiation step. Furthermore, S100B protein expression is responsive to the Sox triad through enhancer elements in the 5′ flanking region [55].
As described above, Runx2 is a master regulator of osteogenesis, but it also has important roles in regulating chondrogenesis. The initial evidence for this was presented in the Runx2 null mice used to identify its function in osteogenesis. It was noted that these mice also had cartilage defects as well as the more obvious bone defects [56]. Runx2 null mice had a lack of hypertrophic chondrocytes, implying an important role for Runx2 in this step. The expression levels of Runx2 are at their highest in chondrocytes during the hypertrophic stage [56], and overexpression of Runx2 during hypertrophy caused enhanced maturation and increased endochondral ossification [57].
3 Signalling Pathways Controlling MSC Differentiation
Multiple signalling pathways have also been found to be involved in lineage commitment and MSC behaviour. For example, studies have identified the involvement of bone morphogenetic proteins (BMPs), Hedgehog (Hh) and Wnt signalling (Fig. 12.3) in the regulation of MSC differentiation [58–60].
Signalling pathways. (a) The Canonical Wnt signalling cascade. Canonical Wnt signalling mediates its effect by binding to their receptors frizzled (Fzd) and co-receptors, LRP 5/6. This causes activation of intracellular Dishevelled (Dvl) which, in turn, inhibits glycogen synthase kinase-3 β (GSK3β). This results in the stabilisation and nuclear translocation of β-catenin, inducing gene transcription via the LEF/TCF family of transcription factors. In the absence of Wnt signalling, a complex containing GSK3β phophorylates β-catenin, leading to degradation by ubiquitination. (b) The Hedgehog signalling cascade. In the absence of any Hedgehog ligand the Hedgehog signalling complex phosphorylates the Gli family of transcription factors, leading to degradation or proteolytic cleavage to transcriptional repressors. In the presence of Hedgehog ligand, signalling is mediated through the binding of Hedgehog to their receptor Patched (Ptc). This causes the inhibition of a second transmembrane protein, Smoothened (Smo), to be relieved. Smo is then able to inhibit the Hedgehog signalling complex preventing the phosphorylation of the Gli proteins, priming them for transcriptional activation. (c) TGFβ/BMP signalling cascade. TGFβ/BMPs signal through their receptors on the cell surface which phosphorylate and activate their respective R-SMADs, which in turn can then bind to the Co-SMAD (SMAD 4). This R-SMAD/Co-SMAD complex can then enter the nucleus where it interacts with transcription factors to induce gene expression
3.1 Wnt Signalling Pathway
Wnt signalling has been implicated by multiple studies to play an important role in the regulation of skeletal function, and in particular osteoblast differentiation and activity. Wnt molecules are a family of cysteine-rich secreted glyco-lipoproteins that regulate many processes including development, cell proliferation and cell fate [61]. Wnt signalling acts through two known pathways, the canonical pathway involving β-catenin, and the β-catenin-independent pathway termed the non-canonical pathway. Canonical Wnt ligands mediate their effects by binding to their receptors frizzled (Fzd) and co-receptors, low-density lipoprotein receptor related protein (LRP) 5 and 6. This causes activation of intracellular Dishevelled which in turn inhibits a protein destruction complex. This results in the stabilisation and nuclear translocation of β-catenin, inducing gene transcription via the LEF/TCF family of transcription factors. In the absence of Wnt signalling, the destruction complex is not inhibited and can therefore perform its function to phosphorylate β-catenin, through glycogen synthase kinase 3β (GSK3β) leading to degradation by ubiquitination (Fig. 12.3a).
3.2 Wnt Signalling in Lineage Commitment
The role of Wnt signalling in bone regulation was first identified in osteoporosis pseudoglioma syndrome patients (characterised by low bone mineral density) with loss of function mutations in the co-receptor LRP5 [62]. Conversely, mutations in the N-terminus of LRP5 that reduce the affinity with the Wnt signalling inhibitor Dkk1 are associated with high bone mass [58]. These observations have been reinforced by using mouse models in which LRP5 overexpression [63] and reduced inhibition of Wnt signalling by sFRP1 knock down [64] resulted in similar results with increase bone mass and density.
In an attempt to elucidate the molecular basis for this response to Wnt, many studies have been carried out using various activators and inhibitors of the Wnt signalling pathway both in vivo and vitro. One process by which Wnt signalling may act to increase bone formation is through the stimulation of osteoblast development. Inhibition of GSK3β enzyme activity using LiCl or small molecules, caused increased β-catenin nuclear translocation, stimulated mouse mesenchymal precursors to differentiate into osteoblasts [6, 7]. GSK3β is involved in other pathways and may therefore cause these effects through means other than the Wnt pathway, however Wnt3a, Wnt1, Wnt10 [65] and constitutively active β-catenin also stimulate osteoblastogenesis, while Dkk1 reduces osteoblast differentiation [66]. Further to this, in vivo work has shown that administration of LiCl, a GSK3β inhibitor, to C57BL/6 mice for 4 weeks dramatically increased bone formation rate [67]. One route by which Wnt is thought to promote osteogenesis is through the direct stimulation of Runx2 expression [68] (Fig. 12.2). Gaur et al. [68] identified a TCF binding site in the promoter of Runx2 and demonstrated an increase in Runx2 expression in response to co-expression of TCF and canonical Wnt proteins.
However, while there is a good deal of evidence in mouse in vivo and vitro for the role of Wnt in inducing osteogenic differentiation, the research in human MSCs is much less conclusive and straightforward. This difference is clearly demonstrated by the work carried out by Boland et al. [69], which demonstrated that Wnt3a conditioned media, leading to canonical Wnt signalling, caused inhibition of osteogenic differentiation demonstrated by reduced ALP mRNA and activity and decreased mineralisation [69]. Induced Wnt signalling did however appear to increase the proliferation rate of human MSCs, whilst at the same time reducing apoptosis (Fig. 12.2). Similar results have been shown in human MSCs by inducing Wnt signalling at different stages of the canonical pathway, including LRP5 and TCF1 [70]. Interestingly these studies also identify the non-canonical Wnt signalling pathway, induced by Wnt5a, as an activator of osteogenesis in human MSCs, capable of inhibiting the effect of Wnt3a activity.
More recently, research has focused on deciphering these apparent variations in response to canonical Wnt signalling. Eijken et al. [71] used a human foetal osteoblastic cell line, with which they generated a non-differentiating and differentiating population, through the addition of the synthetic glucocorticoid dexamethasone [71], while Quarto et al. [72] used a range of human and mouse multipotent and pre-osteoblastic cells to study the effect of Wnt manipulation on osteogenic differentiation [72]. These studies, amongst others [73] have demonstrated that the response to Wnt signalling is dependent on the level of activation and the differentiation state of the target cells. Collectively it seems that canonical Wnt stimulates differentiation of cells committed to the osteogenic lineage, but can inhibit the differentiation of multipotent cells, and prevent the terminal differentiation of mature osteoblasts.
Canonical Wnt signalling is also well studied with relation to adipogenic differentiation, with multiple studies showing reduced adipogenesis with Wnt signalling [74], both in vivo and in vitro. Upon canonical Wnt stimulation, adipogenesis of 3T3-L1 cells is completely inhibited. Canonical Wnt activation does not affect the expression of the early adipocyte transcription factors, C/EBPβ and δ, but blocks C/EBPα and PPARγ and the downstream gene aP2 [75] (Fig. 12.2). The inhibition of PPARγ is thought to be via the activation of chicken ovalbumin upstream promoter transcription factor II, leading to the recruitment of the silencing mediator of retinoid and thyroid hormone receptors co-repressor complex. This binds to the PPARγ gene, maintaining the chromatin in a hypoacetylated state repressing its expression [76]. Conversely, the expression of Wnt inhibitors, reducing endogenous Wnt, causes the spontaneous adipogenic differentiation of pre-adipocytes [75]. This work, along with related findings, identifies canonical Wnt as an important switch in the lineage decisions of MSCs, with canonical Wnt maintaining the cells in a multipotent state until its coordinated removal results in adipogenesis. Recently, work has been carried out studying the relationship between adipogenesis and osteogenesis in response to canonical Wnt signalling [77]. Liu et al. [77] were able to show that human MSCs under dual osteogenic and adipogenic conditions, preferentially formed osteoblasts in response to Wnt3a administration. This response was shown to be due to differential inhibition of the two differentiation processes, where adipogenesis is totally inhibited at low Wnt stimulation, and osteogenesis is only partially inhibited. This suggests that under dual lineage differentiation conditions, differences in sensitivity to Wnt inhibition may alter the equilibrium and shift the commitment from adipocytes toward osteoblasts. This work correlates with that discussed earlier, in which PPARγ-deficient embryonic stem cells would spontaneously differentiate into osteoblasts [35], again implicating Wnt signalling as important regulatory element of lineage decision and commitment.
Canonical Wnt signalling is also influential in the differentiation of MSCs into chondrocytes. This was demonstrated by Day et al. [78] who generated mice with ectopic induction of canonical Wnt signalling in the developing limb bud. These mice showed enhanced ossification and reduced chondrocyte formation. Furthermore, inactivation of β-catenin, therefore preventing canonical Wnt, created the opposite phenotype, with ectopic chondrocyte differentiation, and reduced osteogenesis [78]. In vitro work also confirms a role for Wnt signalling in chondrogenesis, with the overexpression of Wnt8c, 9a or β-catenin causing enhanced chondrocyte hypertrophy in chick upper sternal chondrocytes. Canonical Wnt activation led to decreased Sox9 and Col2A1 expression, whist increasing the hypertrophic markers Col10A1 and Runx2. Canonical Wnt exerts these effects, at least in part, through the LEF/TCF activation of Runx2 and in turn induces the expression of Col10A1 [79]. These findings correlate with those in human MSC culture, where inhibition of canonical Wnt signalling by secreted frizzled-related proteins and Dickkopf overexpression causes enhanced chondrogenesis, with up regulation of Col2A1, Sox9 and glycosaminoglycan expression, and a decrease in Col1A1. However, Wnt inhibition does not induce the expression of Col10A1 [80], suggesting Wnt inhibition can induce early chondrocyte differentiation, but has no effect of final maturation and hypertrophy (Fig. 12.4).
Chondrogenic differentiation of MSCs. Shh and BMPs act together to generate positive feedback loop with Sox9 and Nkx3.2, stimulating the differentiation of MSCs into prehypertrophic chondrocytes, while Wnt signalling inhibits the initiation of chondrogenic differentiation. Wnt signalling is however required for the switch between prehypertrophic and hypertrophic chondrocytes leading to reduced Sox9 expression and increased Col10A1. Ihh expression in prehypertrophic chondrocytes stimulates the switch to hypertrophic chondrocytes, yet also causes PTHrP expression in the surrounding perichondrium, which in turn inhibits hypertrophy in the leading edge of the developing limb, generating a positional negative feedback loop
3.3 Hedgehog Signalling Pathway
Another well studied signalling pathway shown to be involved in bone development is the hedgehog (Hh) pathway [81–83]. Hedgehog was first discovered in Drosophila as a single gene that regulates many diverse aspects of embryonic and adult patterning. Hh signalling has since been found to be present in mammalian cells, but differs initially in that there are three Hh proteins; Sonic hedgehog (Shh), Desert hedgehog (Dhh), and Indian hedgehog (Ihh). Some functional redundancy can be seen between these types, however they do express distinct expression profiles with little overlap [84].
All Hh proteins signal through the same receptors and signalling pathway. The Hh pathway is triggered by the binding of Hedgehog to its receptor, Patched (Ptc). In the absence of any Hh interaction, Ptc acts to inhibit the activity of a 7-transmembrane protein, Smoothened (Smo). In contrast, in the presence of Hh binding to Ptc, Smo repression is alleviated leading to signal transduction and the conversion of the Gli family of transcription factors to an activating state. There are three Gli proteins in mammals, Gli1, 2 and 3, compared to the single transcription factor, Ci, in Drosophila [85].
Smo exerts its effect on signal transduction by inhibiting the hedgehog signalling complex, primarily consisting of glycogen synthase kinase, protein kinase A and casein kinase (GSK3β, PKA and CSK, respectively). Under inactive conditions, when Smo activity is inhibited by Ptc, this complex acts to phosphorylate the Gli transcription factors, priming the Gli proteins for degradation or proteolytic cleavage. This has the overall effect of increasing the transcriptional repressor forms of the Gli proteins, preventing target gene transcription. Conversely, the release of inhibition of Smo, by Hh binding to Ptc, results in inhibition of the Hedgehog signalling complex, and therefore prevents phosphorylation of the Gli proteins. The predominant Gli state is therefore converted to activatory, leading to the transcription of target genes (Fig. 12.3b).
3.4 Hh Signalling in Lineage Commitment
Indian hedgehog (Ihh) signalling is indispensable for osteoblast development during endochondral ossification. This was strikingly shown in Ihh−/− mice, which demonstrated a complete failure of osteoblast development in endochondral bones [82]. Further to this, genetic manipulation of Smo, resulting in removal of Smo from the perichondral cells using a Cre-LoxP system, resulted in the failure of osteoblast differentiation [81]. In addition to these in vivo experiments, the role of Hh signalling in mesenchymal commitment has been studied in vitro. The induction of the hedgehog pathway, by addition of recombinant Hh protein, in C3H10T1/2 cells, induced osteogenesis, with ALP activity detectable after just 2 days of treatment [83].
There is now also evidence for interactions between the Hh and Wnt pathways in relation to osteogenesis. Ihh−/− mice showed a disrupted Wnt signalling phenotype at E14.5 and E16.5, with an absence of nuclear β-catenin staining in the perichondral cells, as compared to the positive staining of the wild type mice [83]. To investigate the functional relationship between Hh and Wnt signalling as inferred by the Ihh−/− mice, the same group used an in vitro C3H10T1/2 differentiation model, in which Ihh overexpression led to ALP expression in the Ihh-expressing cells. This osteogenic differentiation was however reduced by ∼50 % when the cells were co-transfected with either Dkk or double negative Tcf4 constructs. In addition to this, Wnt5a, Wnt7b and Wnt 9a mRNA levels were significantly induced over controls in response to 24–48 h of Hh treatment. This body of work suggests that Hh signalling acts upstream of Wnt signalling and that Wnt signalling is required, at least in part, for the osteogenic inducing potential of Hh.
Ihh is also implicated in the switch between pre- and hypertrophic differentiation, where it is thought to act with parathyroid hormone-related protein (PTHrP) to generate a negative feedback loop regulating the onset of hypertrophy. Ihh signalling by the developing chondrocytes, targets the surrounding perichondrium, where it leads to PTHrP expression. PTHrP then signals to the pre-hypertrophic chondrocytes preventing the initiation of hypertrophic differentiation [86]. It is postulated that the level of Ihh/PTHrP signalling regulated the distance between the joint region and the onset of hypertrophy (Fig. 12.4).
3.5 TGFβ-Superfamily Signalling Pathways
The TGFβ-superfamily contains many transcription factors and morphogens, including two families involved in MSC differentiation, TGFβ and BMPs. As members of the TGFβ-superfamily, both TGFβ and BMPs are dimeric secreted ligands, which generally exist as homodimers. Binding of these ligands to their corresponding receptors, leads to the phosphorylation of the receptor SMADs (R-SMADs). This in turn leads to the interaction of the R-SMADs with SMAD4 (Co-SMAD), and translocation to the nucleus. Here the SMADs interact with transcription factors to activate gene expression. The R-SMADs are specific to either TGFβ signalling or BMP signalling, with SMADs 2/3 for TGFβ and SMADs 1/5/8 for BMPs, generating specificity between the two pathways. Inhibitor SMADS (I-SMADs) also play a role in this pathway by generating a feedback control loop (Fig. 12.3c).
3.6 TGFβ- Superfamily Signalling in Lineage Commitment
BMPs were first identified as proteins that were capable of inducing endochondral bone formation and increasing osteoblast differentiation in vitro [87]. However it is now known that BMPs play vital roles in a wide variety of embryonic processes, including gastrulation, neural development and endothelial cell function [88, 89]. This review will concentrate on the roles of BMPs on the differentiation of MSCs. As stated above, the application of recombinant BMPs to in vitro pre-osteoblast cultures results in increased osteoblastogenesis, demonstrated by increased ALP, osteocalcin expression and matrix mineralisation [87], while the blocking of BMP signalling both arrests osteogenesis and prevents the programmed cell death of mature osteoblasts. BMPs are thought to induce osteoblast differentiation through the activation of Runx2 [90]. Recent work in multiple mouse cell lines has demonstrated that this increase in Runx2 activity in response to BMPs is indirect and acts through Dlx5 [91]. Runx2 is also thought to interact with SMAD1 and 5. These SMAD-Runx2 complexes are directed by the Runx2 targeting signals to sub-nuclear foci where gene targets for both transcription factors are present. This suggests that SMAD transcriptional activation is at least in part dependent on the targeting factors of Runx2 [92]. It is interesting to note that BMP2 stimulation of Dlx5 stimulates the expression of osterix independently of Runx2, implicating Dlx2 as an important regulator of early and late BMP-induced osteogenesis [93].
BMPs not only induce osteoblast differentiation, but also have pro-chondrogenic characteristics, and have been shown to increase the expression of type II and X collagen in growth plate cultures [94]. BMPs exert their effect on chondrogenesis through the chondrogenic master regulator Sox9. Beads soaked in BMP4 implanted into mouse mandibular explants induced ectopic cartilage formation in the proximal position of the explants. These same areas also had upregulation of the Sox9 transcription factor, implicating its role in BMP induced chondrogenesis. Interestingly, BMP4-soaked beads did not induce chondrogenesis in the rostral position, despite similar up regulation of Sox9. However, upregulation of the homeodomain transcription factor Msx2 was also seen in the areas surrounding the beads, and to a much greater degree in rostral region of the explants. Furthermore, ectopic expression of Msx2 prevented the BMP4 induced chondrogenesis, and reduced endogenous chondrogenesis [95]. This body of work demonstrates that BMP induction of chondrogenesis via Sox9, is also dependent on the expression of Msx2, generating a threshold for chondrogenesis, thereby providing a means for positional regulation of chondrogenesis in vivo.
Chondrogenesis is also reliant on the complex cross-talk between BMPs and the Shh/Ihh signalling pathways. One transcription factor of interest in the regulation of chondrogenesis is the homeobox protein, Nkx3.2. Shh signalling initiates the expression of Nkx3.2, while BMP signals act to maintain its expression [96], allowing the transcription repressor activity of Nkx3.2 to block the activity of inhibitors of BMP-induced chondrogenesis. Interestingly, Nkx3.2 also acts to repress Runx2 activity which prevents the onset of differentiation [97]. Furthermore, Nkx3.2 can induce the expression of Sox9 [98], which in turn can increase expression of Nkx3.2, generating a positive feedback loop maintaining the expression of pro-chondrogenic factors. In summary, BMP acts to induce Runx2, stimulating osteogenic differentiation, yet acting alongside Shh signalling during chondrogenesis, generates and maintains high levels of Nkx3.2 leading to the down regulation of Runx2 and increased Sox9, allowing the onset of chondrogenesis (Fig. 12.4).
TGFβ signalling also plays a role in the regulation of MSC differentiation. Unlike BMP-specific SMADs, TGFβ SMADs do not induce osteogenesis, but in fact act to repress the pro-osteogenic effects of BMPs. This inhibition is mediated through SMAD3, which interacts with Runx2 repressing its transcriptional activity [99]. In contrast to this inhibitory effect on osteogenesis, TGFβ is required for the in vitro chondrogenic differentiation of multipotent mesenchymal cells, acting through the p38, ERK-1, and JNK MAP Kinases [100].
4 Additional Regulators of MSC Differentiation
4.1 miRNAs in MSC Differentiation
The discovery of microRNAs (miRNAs) as a mechanism for regulating gene expression in the early 2000s [101] opened up a new avenue of investigation in the hunt for regulators of MSC differentiation. miRNAs are small non-coding RNAs that regulate the translation of protein coding genes by binding to the 3′ untranslated region and in most cases causing degradation of the mRNA. Li et al. [102] found that following BMP-induced osteoblast differentiation, 22 miRNAs could be detected as downregulated [102]. They then showed that two of these downregulated miRNAs acted directly on genes important in osteoblast differentiation. MiR-133 directly targets Runx2, the master regulator of osteogenesis, while miR-135 acts upon SMAD5, an important transducer of the BMP signal. Similarly, Hassan et al. [103] showed that Runx2 negatively regulates a cluster of miRNAs, 23a ∼ 27a ∼ 24-2, and that these miRNAs act to suppress osteogenesis by suppression of SATB2, a protein that acts synergistically with Runx2 during osteogenesis [103]. It is thought that this generates a feed forward loop, whereby Runx2 expression can de-repress SATB2, enhancing osteogenic progression.
4.2 Mechanical Stimulation in MSC Differentiation
The effect of mechanical stimuli on the differentiation of MSCs is another growing area of research. McMahon et al. [104] demonstrated that MSCs grown in a 3D collagen type I-glycosaminoglycan (GAG) scaffold could differentiate into chondrocytes when supplemented with inductive medium. This differentiation could then be enhanced by the application of 10 % cyclic tensile loading for 7 days, measured by increased GAG synthesis [104]. Similarly, Sim et al. [105] created a novel micro cell chip system to apply compressive pressures to MSCs. MSCs grown in this system could differentiate into osteoblasts when treated with an osteogenic cocktail, measured by ALP expression, and this was further enhanced by intermittent cyclic compression for 1 week [105].
5 Summary
The regulation of MSC differentiation is complex and multilayered, comprising an interwoven combination of genetic, bio-chemical and mechanical influences. Since the early work of Friedenstein and colleagues [1, 2], great advances have been made in the molecular description of MSC control, but challenges do remain. There is a lack of consensus in the field on appropriate MSC isolation techniques, caused largely by the absence of a truly selective and universally adopted MSC marker. Much work therefore relies on the use of heterogeneous MSC-like populations of cells, sorted, somewhat crudely perhaps, by their adherence to a plastic surface. Transgenic models have given a penetrating insight into the genetic determinants of skeletal tissue development and organisation, but inter-species variations in MSCs persist in mouse and man. However, there is a common belief, supported by an admirable resolve and talented research, that these obstacles and others will be overcome, and that the information gathered on MSC biology will continue to add to the scientific and clinical appeal of these precious cells.
References
Friedenstein AJ, Piatetzky S II, Petrakova KV (1966) Osteogenesis in transplants of bone marrow cells. J Embryol Exp Morphol 16(3):381–390
Friedenstein AJ, Chailakhjan RK, Lalykina KS (1970) The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet 3(4):393–403
Pittenger MF et al (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284(5411):143–147
Horwitz EM et al (2002) Isolated allogeneic bone marrow-derived mesenchymal cells engraft and stimulate growth in children with osteogenesis imperfecta: implications for cell therapy of bone. Proc Natl Acad Sci USA 99(13):8932–8937
Dominici M et al (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The international society for cellular therapy position statement. Cytotherapy 8(4):315–317
Jackson A et al (2005) Gene array analysis of Wnt-regulated genes in C3H10T1/2 cells. Bone 36(4):585–598
Kulkarni NH et al (2006) Orally bioavailable GSK-3alpha/beta dual inhibitor increases markers of cellular differentiation in vitro and bone mass in vivo. J Bone Miner Res 21(6):910–920
da Silva Meirelles L, Chagastelles PC, Nardi NB (2006) Mesenchymal stem cells reside in virtually all post-natal organs and tissues. J Cell Sci 119(Pt 11):2204–2213
Banerjee C et al (2001) Differential regulation of the two principal Runx2/Cbfa1 n-terminal isoforms in response to bone morphogenetic protein-2 during development of the osteoblast phenotype. Endocrinology 142(9):4026–4039
Jaiswal N et al (1997) Osteogenic differentiation of purified, culture-expanded human mesenchymal stem cells in vitro. J Cell Biochem 64(2):295–312
Samulin J et al (2008) Differential gene expression of fatty acid binding proteins during porcine adipogenesis. Comp Biochem Physiol B Biochem Mol Biol 151(2):147–152
Pelttari K, Steck E, Richter W (2008) The use of mesenchymal stem cells for chondrogenesis. Injury 39(suppl 1):S58–S65
Marie PJ (2008) Transcription factors controlling osteoblastogenesis. Arch Biochem Biophys 473(2):98–105
Ducy P et al (1997) Osf2/Cbfa1: a transcriptional activator of osteoblast differentiation. Cell 89(5):747–754
Komori T et al (1997) Targeted disruption of Cbfa1 results in a complete lack of bone formation owing to maturational arrest of osteoblasts. Cell 89(5):755–764
Xiao ZS et al (1998) Genomic structure and isoform expression of the mouse, rat and human Cbfa1/Osf2 transcription factor. Gene 214(1–2):187–197
Zheng H et al (2004) Cbfa1/osf2 transduced bone marrow stromal cells facilitate bone formation in vitro and in vivo. Calcif Tissue Int 74(2):194–203
Takahashi T (2011) Overexpression of Runx2 and MKP-1 stimulates transdifferentiation of 3T3-L1 preadipocytes into bone-forming osteoblasts in vitro. Calcif Tissue Int 88(4):336–347
Phillips JE et al (2006) Glucocorticoid-induced osteogenesis is negatively regulated by Runx2/Cbfa1 serine phosphorylation. J Cell Sci 119(Pt 3):581–591
Shui C et al (2003) Changes in Runx2/Cbfa1 expression and activity during osteoblastic differentiation of human bone marrow stromal cells. J Bone Miner Res 18(2):213–221
Nakashima K et al (2002) The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell 108(1):17–29
Wu L et al (2007) Osteogenic differentiation of adipose derived stem cells promoted by overexpression of osterix. Mol Cell Biochem 301(1–2):83–92
Tu Q, Valverde P, Chen J (2006) Osterix enhances proliferation and osteogenic potential of bone marrow stromal cells. Biochem Biophys Res Commun 341(4):1257–1265
Kurata H et al (2007) Osterix induces osteogenic gene expression but not differentiation in primary human fetal mesenchymal stem cells. Tissue Eng 13(7):1513–1523
Chen X et al (1996) Dlx5 and Dlx6: an evolutionary conserved pair of murine homeobox genes expressed in the embryonic skeleton. Ann N Y Acad Sci 785:38–47
Tadic T et al (2002) Overexpression of Dlx5 in chicken calvarial cells accelerates osteoblastic differentiation. J Bone Miner Res 17(6):1008–1014
Depew MJ et al (1999) Dlx5 regulates regional development of the branchial arches and sensory capsules. Development 126(17):3831–3846
Robledo RF et al (2002) The Dlx5 and Dlx6 homeobox genes are essential for craniofacial, axial, and appendicular skeletal development. Genes Dev 16(9):1089–1101
Hassan MQ et al (2004) Dlx3 transcriptional regulation of osteoblast differentiation: temporal recruitment of Msx2, Dlx3, and Dlx5 homeodomain proteins to chromatin of the osteocalcin gene. Mol Cell Biol 24(20):9248–9261
Dodig M et al (1999) Ectopic Msx2 overexpression inhibits and Msx2 antisense stimulates calvarial osteoblast differentiation. Dev Biol 209(2):298–307
Mueller E et al (2002) Genetic analysis of adipogenesis through peroxisome proliferator-activated receptor gamma isoforms. J Biol Chem 277(44):41925–41930
Tontonoz P et al (1994) mPPAR gamma 2: tissue-specific regulator of an adipocyte enhancer. Genes Dev 8(10):1224–1234
Hu E, Tontonoz P, Spiegelman BM (1995) Transdifferentiation of myoblasts by the adipogenic transcription factors PPAR gamma and C/EBP alpha. Proc Natl Acad Sci U S A 92(21):9856–9860
Rosen ED et al (2002) C/EBPalpha induces adipogenesis through PPARgamma: a unified pathway. Genes Dev 16(1):22–26
Akune T et al (2004) PPARgamma insufficiency enhances osteogenesis through osteoblast formation from bone marrow progenitors. J Clin Invest 113(6):846–855
Freytag SO, Paielli DL, Gilbert JD (1994) Ectopic expression of the CCAAT/enhancer-binding protein alpha promotes the adipogenic program in a variety of mouse fibroblastic cells. Genes Dev 8(14):1654–1663
Lin FT, Lane MD (1992) Antisense CCAAT/enhancer-binding protein RNA suppresses coordinate gene expression and triglyceride accumulation during differentiation of 3T3-L1 preadipocytes. Genes Dev 6(4):533–544
Linhart HG et al (2001) C/EBPalpha is required for differentiation of white, but not brown, adipose tissue. Proc Natl Acad Sci U S A 98(22):12532–12537
Yeh WC et al (1995) Cascade regulation of terminal adipocyte differentiation by three members of the C/EBP family of leucine zipper proteins. Genes Dev 9(2):168–181
Rosen ED et al (1999) PPAR gamma is required for the differentiation of adipose tissue in vivo and in vitro. Mol Cell 4(4):611–617
Wu Z et al (1999) Cross-regulation of C/EBP alpha and PPAR gamma controls the transcriptional pathway of adipogenesis and insulin sensitivity. Mol Cell 3(2):151–158
Kim JB, Spiegelman BM (1996) ADD1/SREBP1 promotes adipocyte differentiation and gene expression linked to fatty acid metabolism. Genes Dev 10(9):1096–1107
Fajas L et al (1999) Regulation of peroxisome proliferator-activated receptor gamma expression by adipocyte differentiation and determination factor 1/sterol regulatory element binding protein 1: implications for adipocyte differentiation and metabolism. Mol Cell Biol 19(8):5495–5503
Tang QQ, Lane MD (2000) Role of C/EBP homologous protein (CHOP-10) in the programmed activation of CCAAT/enhancer-binding protein-beta during adipogenesis. Proc Natl Acad Sci U S A 97(23):12446–12450
Moldes M et al (1999) Functional antagonism between inhibitor of DNA binding (Id) and adipocyte determination and differentiation factor 1/sterol regulatory element-binding protein-1c (ADD1/SREBP-1c) trans-factors for the regulation of fatty acid synthase promoter in adipocytes. Biochem J 344(Pt 3):873–880
Tong Q et al (2000) Function of GATA transcription factors in preadipocyte-adipocyte transition. Science 290(5489):134–138
Tong Q et al (2005) Interaction between GATA and the C/EBP family of transcription factors is critical in GATA-mediated suppression of adipocyte differentiation. Mol Cell Biol 25(2):706–715
Zhao Q et al (1997) Parallel expression of Sox9 and Col2a1 in cells undergoing chondrogenesis. Dev Dyn 209(4):377–386
Akiyama H et al (2002) The transcription factor Sox9 has essential roles in successive steps of the chondrocyte differentiation pathway and is required for expression of Sox5 and Sox6. Genes Dev 16(21):2813–2828
Ikeda T et al (2004) The combination of SOX5, SOX6, and SOX9 (the SOX trio) provides signals sufficient for induction of permanent cartilage. Arthritis Rheum 50(11):3561–3573
Frith J, Genever P (2008) Transcriptional control of mesenchymal stem cell differentiation. Transfus Med Hemother 35(3):216–227
Smits P et al (2001) The transcription factors L-Sox5 and Sox6 are essential for cartilage formation. Dev Cell 1(2):277–290
Lefebvre V, Behringer RR, de Crombrugghe B (2001) L-Sox5, Sox6 and Sox9 control essential steps of the chondrocyte differentiation pathway. Osteoarthr Cartil 9(suppl A):S69–S75
Bridgewater LC, Lefebvre V, de Crombrugghe B (1998) Chondrocyte-specific enhancer elements in the Col11a2 gene resemble the Col2a1 tissue-specific enhancer. J Biol Chem 273(24):14998–15006
Saito T et al (2007) S100A1 and S100B, transcriptional targets of SOX trio, inhibit terminal differentiation of chondrocytes. EMBO Rep 8(5):504–509
Kim IS et al (1999) Regulation of chondrocyte differentiation by Cbfa1. Mech Dev 80(2):159–170
Enomoto-Iwamoto M et al (2001) Participation of Cbfa1 in regulation of chondrocyte maturation. Osteoarthr Cartil 9(suppl A):S76–S84
Boyden LM et al (2002) High bone density due to a mutation in LDL-receptor-related protein 5. N Engl J Med 346(20):1513–1521
Yamaguchi A, Komori T, Suda T (2000) Regulation of osteoblast differentiation mediated by bone morphogenetic proteins, hedgehogs, and Cbfa1. Endocr Rev 21(4):393–411
Shimoyama A et al (2007) Ihh/Gli2 signaling promotes osteoblast differentiation by regulating Runx2 expression and function. Mol Biol Cell 18(7):2411–2418
Ling L, Nurcombe V, Cool SM (2009) Wnt signaling controls the fate of mesenchymal stem cells. Gene 433(1–2):1–7
Gong Y et al (2001) LDL receptor-related protein 5 (LRP5) affects bone accrual and eye development. Cell 107(4):513–523
Babij P et al (2003) High bone mass in mice expressing a mutant LRP5 gene. J Bone Miner Res 18(6):960–974
Bodine PV et al (2004) The Wnt antagonist secreted frizzled-related protein-1 is a negative regulator of trabecular bone formation in adult mice. Mol Endocrinol 18(5):1222–1237
Bennett CN et al (2005) Regulation of osteoblastogenesis and bone mass by Wnt10b. Proc Natl Acad Sci U S A 102(9):3324–3329
Krishnan V, Bryant HU, Macdougald OA (2006) Regulation of bone mass by Wnt signaling. J Clin Invest 116(5):1202–1209
Clement-Lacroix P et al (2005) Lrp5-independent activation of Wnt signaling by lithium chloride increases bone formation and bone mass in mice. Proc Natl Acad Sci U S A 102(48):17406–17411
Gaur T et al (2005) Canonical WNT signaling promotes osteogenesis by directly stimulating Runx2 gene expression. J Biol Chem 280(39):33132–33140
Boland GM et al (2004) Wnt 3a promotes proliferation and suppresses osteogenic differentiation of adult human mesenchymal stem cells. J Cell Biochem 93(6):1210–1230
Baksh D, Boland GM, Tuan RS (2007) Cross-talk between Wnt signaling pathways in human mesenchymal stem cells leads to functional antagonism during osteogenic differentiation. J Cell Biochem 101(5):1109–1124
Eijken M et al (2008) Wnt signaling acts and is regulated in a human osteoblast differentiation dependent manner. J Cell Biochem 104(2):568–579
Quarto N, Behr B, Longaker MT (2010) Opposite spectrum of activity of canonical Wnt signaling in the osteogenic context of undifferentiated and differentiated mesenchymal cells: implications for tissue engineering. Tissue Eng Part A 16(10):3185–3197
Kahler RA et al (2006) Lymphocyte enhancer-binding factor 1 (Lef1) inhibits terminal differentiation of osteoblasts. J Cell Biochem 97(5):969–983
Prestwich TC, Macdougald OA (2007) Wnt/beta-catenin signaling in adipogenesis and metabolism. Curr Opin Cell Biol 19(6):612–617
Bennett CN et al (2002) Regulation of Wnt signaling during adipogenesis. J Biol Chem 277(34):30998–31004
Okamura M et al (2009) COUP-TFII acts downstream of Wnt/beta-catenin signal to silence PPARgamma gene expression and repress adipogenesis. Proc Natl Acad Sci U S A 106(14):5819–5824
Liu G et al (2009) Canonical Wnts function as potent regulators of osteogenesis by human mesenchymal stem cells. J Cell Biol 185(1):67–75
Day TF et al (2005) Wnt/beta-catenin signaling in mesenchymal progenitors controls osteoblast and chondrocyte differentiation during vertebrate skeletogenesis. Dev Cell 8(5):739–750
Dong YF et al (2006) Wnt induction of chondrocyte hypertrophy through the Runx2 transcription factor. J Cell Physiol 208(1):77–86
Im GI, Lee JM, Kim HJ (2011) Wnt inhibitors enhance chondrogenesis of human mesenchymal stem cells in a long-term pellet culture. Biotechnol Lett 33(5):1061–1068
Long F et al (2004) Ihh signaling is directly required for the osteoblast lineage in the endochondral skeleton. Development 131(6):1309–1318
St-Jacques B, Hammerschmidt M, McMahon AP (1999) Indian hedgehog signaling regulates proliferation and differentiation of chondrocytes and is essential for bone formation. Genes Dev 13(16):2072–2086
Hu H et al (2005) Sequential roles of Hedgehog and Wnt signaling in osteoblast development. Development 132(1):49–60
Bitgood MJ, McMahon AP (1995) Hedgehog and Bmp genes are coexpressed at many diverse sites of cell-cell interaction in the mouse embryo. Dev Biol 172(1):126–138
Deschaseaux F, Sensebe L, Heymann D (2009) Mechanisms of bone repair and regeneration. Trends Mol Med 15(9):417–429
Vortkamp A et al (1996) Regulation of rate of cartilage differentiation by Indian hedgehog and PTH-related protein. Science 273(5275):613–622
Sampath TK et al (1992) Recombinant human osteogenic protein-1 (hOP-1) induces new bone formation in vivo with a specific activity comparable with natural bovine osteogenic protein and stimulates osteoblast proliferation and differentiation in vitro. J Biol Chem 267(28):20352–20362
Valcourt U, Moustakas A (2005) BMP signaling in osteogenesis, bone remodeling and repair. Eur J Trauma 31(5):464–479
Gitelman SE et al (1995) Vgr-1/BMP-6 induces osteoblastic differentiation of pluripotential mesenchymal cells. Cell Growth Differ 6(7):827–836
Lee KS et al (2000) Runx2 is a common target of transforming growth factor beta1 and bone morphogenetic protein 2, and cooperation between Runx2 and Smad5 induces osteoblast-specific gene expression in the pluripotent mesenchymal precursor cell line C2C12. Mol Cell Biol 20(23):8783–8792
Lee MH et al (2003) BMP-2-induced Runx2 expression is mediated by Dlx5, and TGF-beta 1 opposes the BMP-2-induced osteoblast differentiation by suppression of Dlx5 expression. J Biol Chem 278(36):34387–34394
Zaidi SK et al (2002) Integration of Runx and Smad regulatory signals at transcriptionally active subnuclear sites. Proc Natl Acad Sci USA 99(12):8048–8053
Lee MH et al (2003) BMP-2-induced Osterix expression is mediated by Dlx5 but is independent of Runx2. Biochem Biophys Res Commun 309(3):689–694
De Luca F et al (2001) Regulation of growth plate chondrogenesis by bone morphogenetic protein-2. Endocrinology 142(1):430–436
Semba I et al (2000) Positionally-dependent chondrogenesis induced by BMP4 is co-regulated by Sox9 and Msx2. Dev Dyn 217(4):401–414
Murtaugh LC et al (2001) The chick transcriptional repressor Nkx3.2 acts downstream of Shh to promote BMP-dependent axial chondrogenesis. Dev Cell 1(3):411–422
Lengner CJ et al (2005) Nkx3.2-mediated repression of Runx2 promotes chondrogenic differentiation. J Biol Chem 280(16):15872–15879
Zeng L et al (2002) Shh establishes an Nkx3.2/Sox9 autoregulatory loop that is maintained by BMP signals to induce somitic chondrogenesis. Genes Dev 16(15):1990–2005
Alliston T et al (2001) TGF-beta-induced repression of CBFA1 by Smad3 decreases cbfa1 and osteocalcin expression and inhibits osteoblast differentiation. EMBO J 20(9):2254–2272
Lutz M, Knaus P (2002) Integration of the TGF-beta pathway into the cellular signalling network. Cell Signal 14(12):977–988
Benfey PN (2003) Molecular biology: microRNA is here to stay. Nature 425(6955):244–245
Li Z et al (2008) A microRNA signature for a BMP2-induced osteoblast lineage commitment program. Proc Natl Acad Sci U S A 105(37):13906–13911
Hassan MQ et al (2010) A network connecting Runx2, SATB2, and the miR-23a ∼ 27a ∼ 24-2 cluster regulates the osteoblast differentiation program. Proc Natl Acad Sci USA 107(46):19879–19884
McMahon LA et al (2008) Regulatory effects of mechanical strain on the chondrogenic differentiation of MSCs in a collagen-GAG scaffold: experimental and computational analysis. Ann Biomed Eng 36(2):185–194
Sim WY et al (2007) A pneumatic micro cell chip for the differentiation of human mesenchymal stem cells under mechanical stimulation. Lab Chip 7(12):1775–1782
Caplan AI, Bruder SP (2001) Mesenchymal stem cells: building blocks for molecular medicine in the 21st century. Trends Mol Med 7(6):259–264
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Cook, D., Genever, P. (2013). Regulation of Mesenchymal Stem Cell Differentiation. In: Hime, G., Abud, H. (eds) Transcriptional and Translational Regulation of Stem Cells. Advances in Experimental Medicine and Biology, vol 786. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-6621-1_12
Download citation
DOI: https://doi.org/10.1007/978-94-007-6621-1_12
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-6620-4
Online ISBN: 978-94-007-6621-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)