Abstract
Ethanol consumption has effects on the central nervous system (CNS), manifesting as motor incoordination, sleep induction (hypnosis), anxiety, amnesia, and the reinforcement or aversion of alcohol consumption. Acetaldehyde (the direct metabolite of ethanol oxidation) contributes to many aspects of the behavioral effects of ethanol. Given acetaldehyde cannot pass through the blood brain barrier, its concentration in the CNS is primarily determined by local production from ethanol. Catalase and cytochrome P450 2E1 (CYP2E1) represent the major enzymes in the CNS that catalyze ethanol oxidation. CYP2E1 is expressed abundantly within the microsomes of certain brain cells and is localized to particular brain regions. This chapter focuses on the discussion of CYP2E1 in ethanol metabolism in the CNS, covering topics including how it is regulated, where it is expressed and how it influences sensitivity to ethanol in the brain.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Introduction
Excessive alcohol consumption (alcoholism) causes morbidity and mortality in populations of varied ages, regions and ethnicities. Millions of people suffer from alcoholism and billions of dollars are spent annually on alcohol related toxicities (Mokdad et al. 2004; Ginter and Simko 2009; Brust 2010). Excessive alcohol intake leads to extensive tissue damage in organs (such as liver, heart and the respiratory system), as well as promoting disease states, including diabetes mellitus and neuropsychiatric disorders (Brust 2010). The central nervous system (CNS) is particularly susceptible to ethanol where it acts as a depressant. Exposure of the CNS to alcohol may also cause behavioral changes, such as anxiety, aggression, euphoria, poor motion coordination and compromised memory and linguistic proficiency (Vasiliou et al. 2006; Alfonso-Loeches and Guerri 2011).
Alcohol is a class of organic compounds with carbon-bound hydroxyl group(s). The most commonly ingested alcohol is ethanol (CH3CH2OH), an ethane backbone bound by a hydroxyl group. Due to its high affinity for water, once ingested, ethanol is rapidly absorbed from all parts of the gastrointestinal tract largely by simple diffusion into the blood. It is then quickly distributed throughout the body. The majority of ethanol metabolism occurs in the liver. Several distinct pathways contribute to the metabolism of ethanol. Alcohol dehydrogenases (ADHs), catalase and cytochrome P450 2E1 (CYP2E1) are involved in its conversion to acetaldehyde and aldehyde dehydrogenases (ALDHs) convert acetaldehyde to acetate. While ethanol metabolic pathways in the liver are relatively well characterized, considerably less is understood regarding enzymes and pathways involved in ethanol metabolism in the brain. This chapter provides a summary of current knowledge about ethanol metabolism and sensitivity in the CNS, with an emphasis on the role of CYP2E1 in these processes.
8.2 Ethanol Metabolism in the CNS
Three enzymes are responsible for oxidizing ethanol to acetaldehyde: ADH, catalase, and CYP2E1 (Fig. 8.1). Acetaldehyde is further oxidized to acetate by ALDHs (Vasiliou et al. 2006). The mammalian ADH enzyme family has five classes, each with several isoforms (Estonius et al. 1996). Class 1 consists of ADH isoforms 1, 2 and 3; these are responsible for the majority of ethanol metabolism in the liver (Edenberg 1998). The role of ADH enzymes in the brain, once thought to be nonexistent, is now evident but poorly understood. Some isoforms of ADH have been identified in the brain in small quantities. ADH3 was found in the brain but ethanol was shown to be a poor substrate for this particular isoform, with a Km of greater than 2.5 M (Beisswenger et al. 1985). mRNAs for ADH1, a low-Km isoform (Km = 1.4 mM) (Zakhari 2006), has also been detected in the brain (Martinez et al. 2001). Interestingly, ADH activity was not detected in the whole brain homogenate but was found to be localized to granular and Purkinje cells of the cerebellum (Galter et al. 2003). Therefore, if ADHs have a role in the CNS, they appear to be localized to particular brain regions and their function remains to be defined.
Metabolic pathways of ethanol metabolism in the Central Nervous System (CNS). Three enzymes are responsible for oxidizing ethanol to acetaldehyde: alcohol dehydrogenase (ADH), catalase and cytochrome P450 2E1 (CYP2E1). Acetaldehyde is further oxidized to acetate by acetaldehyde dehydrogenase (ALDH). Acetaldehyde is responsible for many of the behavioral effects associated with ethanol consumption. The contribution of each enzyme to total ethanol oxidation occurring in the CNS is as follows: catalase, serving as the primary enzyme, accounts for 60%; CYP2E1 is inducible and accounts for 20%; the remaining 20% is unknown but is thought to involve ADH. Isoforms of ADH present in the CNS have a wide range of affinity for ethanol
There is growing evidence that catalase serves as the primary ethanol metabolizing enzyme in the brain, as well as in the heart and kidney (Vasiliou et al. 2006). Catalase is found primarily in the peroxisome (Fig. 8.1) where it catalyzes the conversion of hydrogen peroxide to oxygen and water. Catalase has a Km of 12 mM for ethanol oxidation (Thurman et al. 1972), which is much lower than that of ADH3, indicating ethanol to be a better substrate for catalase. Catalase accounts for 60% of ethanol oxidation in the brain (Zimatkin et al. 2006) and appears to play a major role in mediating the psychopharmacological effects of ethanol (Vasiliou et al. 2006; Correa et al. 2008). Through the examination of the effect of inhibitors on acetaldehyde production and the use of transgenic mice, Zimatkin and colleagues (2006) verified the importance of catalase in ethanol oxidation in the brain.
Recent studies have also found that CYP2E1 plays a significant role in ethanol oxidation to acetaldehyde in the brain (Vasiliou et al. 2006; Zimatkin et al. 2006). CYP2E1, a membrane-bound protein, catalyzes the oxidation of a variety of endobiotics (such as retinoids and prostaglandins) and xenobiotics (such as drugs and alcohols) (Cheung et al. 2005; Dey and Kumar 2011). It has a relatively high activity towards ethanol oxidation with a Km of 8–10 mM (Zakhari 2006). The CYP2E1 gene is well conserved in mammalian species and CYP2E1 protein is expressed in various tissues and cell types (Lee et al. 1996). While CYP2E1 is most abundantly expressed in hepatocytes, it has been reported in CNS where its expression has been found to be region-, cell type- and organelle- specific (Howard et al. 2003a, b). CYP2E1 has traditionally been considered to be a microsomal protein. However, recent studies indicate that it is also present in the mitochondria through a distinct mitochondrial-import mechanism (Robin et al. 2001, 2002; Knockaert et al. 2011). In this organelle, it promotes oxidative stress during the production of acetaldehyde and thereby has the potential to trigger a series of unfavorable molecular events in neuronal cells (Raza et al. 2004; Bansal et al. 2010).
8.3 Acetaldehyde in Ethanol Sensitivity of the Brain
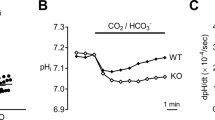
Acetaldehyde is the primary and highly reactive metabolite of ethanol. It has been implicated as a significant contributor to a broad spectrum of adverse physiological and pathophysiological effects of ethanol (Zimatkin et al. 2006). Physiological alterations ascribed to acetaldehyde include changes in glial cell function and differentiation (Sarc et al. 2011). Behavioral alterations include euphoria (intense happiness), anxiolytic (reduced anxiety), hypnotic (also known as sleep time), amnesiac (loss of memory) and aggression, as well as reinforcement or aversion to voluntary ethanol consumption (preference). The contribution of acetaldehyde in each of these distinct ethanol-associated behaviors has been subject to experimental examination. For example, Quertemont and colleagues (2004) examined the role of acetaldehyde in the anxiolytic, hypnotic and amnesiac behavioral effects of ethanol consumption. An association between acetaldehyde and the hypnotic (at higher doses) and amnesiac (dose-dependent) behavioral effects of ethanol were observed. However, acetaldehyde was not involved in the anxiolytic effects of ethanol. These results implicate acetaldehyde in the hypnotic, amnesiac and preferential behaviors of ethanol. Interestingly, data derived from experiments conducted in transgenic animals contradict the theory that acetaldehyde contributes to ethanol’s hypnotic effect. Specifically, in acatalasemic, CYP2E1-null or catalase/CYP2E1 dual-deficient mice, a decrease in blood acetaldehyde levels was accompanied by an increase in ethanol-induced sleep time, especially at high doses of ethanol (Vasiliou et al. 2006).
Acetate is the secondary metabolite of ethanol and, unlike acetaldehyde, can freely cross the BBB. Acetate is metabolized to acetyl-CoA, which can be used in the citric acid cycle or converted into acetylcholine, a neurotransmitter. While the primary source of energy in the brain is glucose, ethanol decreases glucose uptake and potentially switches the source of energy to acetate (Zimatkin et al. 2011). Short sleep or high tolerance rats have been found to have a lower amount of acetyl-CoA in the frontal cortex than long sleep rats, indicating the inborn deficiency of acetyl-CoA is compensated for by ethanol-derived acetate (Zimatkin et al. 2011). It is likely that the tolerance in short sleep rats can be attributed to their ability to use acetate for acetyl-CoA production better than the long sleep rats. Hence, acetate may contribute to the hypnotic effects of ethanol.
In the context of voluntary consumption of ethanol (or ethanol preference), acetaldehyde in the CNS has reinforcing effects. When directly administered to the ventral tegmental area (VTA) of the brain, acetaldehyde reproduces the same activating and reinforcing behavioral effects as ethanol administration (Correa et al. 2003), implicating the role of acetaldehyde in ethanol preference. Supporting this proposal is the observation that inhibition of acetaldehyde formation (by microinjection of a catalase-inhibiting shRNA lentiviral vector directly to the VTA) resulted in a 94% reduction in voluntary ethanol consumption by high alcohol preferring rats (Karahanian et al. 2011). This treatment also eliminated the increased dopamine efflux in the nucleus accumbens normally seen after systemic ethanol administration. However, there was no interruption in normal dopamine pathways as demonstrated by a normal dopamine response to methamphetamines and tyrosine hydroxylase, the enzyme responsible for formation of L-dopa, remained active. Voluntary ethanol consumption was shown to be stimulated by administration of a lentiviral vector encoding ADH that increased acetaldehyde production (Karahanian et al. 2011). These studies strongly support the notion that acetaldehyde produced in the brain mediates the reinforcing effects of ethanol consumption.
There are multiple working theories regarding the involvement of acetaldehyde in ethanol preference (Davis and Walsh 1970; Melchior and Myers 1977; Rodd-Henricks et al. 2002; Vasiliou et al. 2006). Some think acetaldehyde alone may mediate the reinforcing effects attributed to ethanol in the CNS. Others believe acetaldehyde may act as a modulator, augmenting the actions of ethanol. It is also possible that acetaldehyde may react with an endogenous substance (e.g. dopamine) to form another biologically-active compound (e.g. salsolinol), which may serve as the active compound in the reinforcing behavior (McBride et al. 2002). Whatever the mechanism, it is clear that acetaldehyde in the CNS has a reinforcing role in voluntary ethanol consumption. Outside of the CNS, however, acetaldehyde appears to have the opposite effect. Due to metabolism by the abundance of ALDH in the blood brain barrier (BBB), acetaldehyde formed outside of the CNS (i.e., in the periphery) is unable to enter the CNS (Zimatkin 1991). Accordingly, acetaldehyde exists in two physiological compartments separated by the BBB, viz. in the CNS and in the periphery. The effects of acetaldehyde in the periphery are concentration-dependent: reinforcing effects are seen at very low concentrations while mostly aversive affects at normal to high concentrations (McBride et al. 2002). An acetaldehyde “burst” (measured as a spike in blood acetaldehyde levels), occurring as a result of the higher activity of an isoform of ADH, appears to cause reduced voluntary ethanol intake (aversion). Wistar rats conditioned for high ethanol intake were genetically altered to express decreased hepatic ALDH activity (85% reduction). Predictably, this resulted in higher concentrations of circulating acetaldehyde after ethanol consumption (Quintanilla et al. 2007). These animals exhibited a 50% reduction in voluntary ethanol consumption, showing that, contrary to its reinforcing effects in the brain, acetaldehyde outside the CNS tends to have an aversive effect. Future studies quantifying ethanol metabolites, acetaldehyde and acetate, to ensure concordance with normal ethanol intoxication will be vital in investigating the behavioral effects of ethanol with respect to physiological conditions (Deitrich 2004).
8.4 Acetaldehyde Production in the Brain
Before the discovery of ethanol-oxidizing pathways in the brain, research focused on the potential of acetaldehyde to cross into the brain. Ethanol and acetate can freely cross the BBB while acetaldehyde cannot (Deitrich et al. 1989). The observation that acetaldehyde concentrations in the CNS do not correspond to levels in the blood (Tabakoff et al. 1976; Westcott et al. 1980; Deitrich 2011) is consistent with this contention and indicates that acetaldehyde measured in the CNS is produced there.
The discovery of the catalase pathway for acetaldehyde formation in the brain (Aragon et al. 1992; Gill et al. 1992) served as an important first step in our understanding about the role of acetaldehyde in the effects of ethanol in the CNS. Studies using inhibitors of catalase (e.g., aminotriazole or sodium azide) and acatalasemic mice (i.e., have a genetic catalase deficiency that results in ≈ 50% reduction in brain catalase levels) have revealed catalase to be responsible for approximately half of ethanol metabolism occurring the CNS (Zimatkin et al. 2006). This finding indicates the existence of other ethanol metabolizing pathways in the brain. A contender for an alternative pathway is CYP2E1, an isoform of cytochrome P450 which is inducible by ethanol.
8.5 CYP2E1 Expression in the Brain
Although the presence of CYP2E1 in the brain had been established, early research using brain homogenates argued against CYP2E1 participating in ethanol oxidation (Gill et al. 1992). There are several explanations for these negative data: First, the cytochrome P450 inhibitor used, metyrapone, displays specificity for the isozyme CYP2B rather than CYP2E1. Second, the agents used to inhibit catalase can, at high doses, also inhibit CYP2E1 (Zimatkin et al. 2006), leading to an overestimation of the role of catalase in the brain. Third, the presence of ADH in the brain, specifically some isoforms of ADH such as ADH3 (Beisswenger et al. 1985; Kerr et al. 1989) may account for the discrepancy seen upon catalase inhibition rather than it being attributed to CYP2E1.
In a three part experiment by Zimatkin and colleagues (2006), ethanol oxidation was studied by measuring the concentration of acetaldehyde and acetate in perfused mouse brains and brain homogenates. Catalase was found to mediate 60% of ethanol metabolism in the brain. Inhibition of ADH decreased acetate levels, but had no effect on acetaldehyde levels, likely due to non-specific inhibition of ALDH by the ADH inhibitor used in the experiments (although this has not been confirmed). Inhibition of CYP2E1 (using dallyl sulfide (DAS) or beta-phenethyl-isothiocyanate) led to a significant decrease in both acetaldehyde and acetate (Deitrich 2004). Experiments using animal models harboring genetic deficiencies in CYP2E1 and/or catalase indicate that CYP2E1 is responsible for approximately 20% of ethanol metabolism in the brain (Zimatkin et al. 2006). After considering the combined contributions of catalase and CYP2E1 to ethanol oxidation in the brain, there remains 20% of ethanol oxidation unaccounted for; this is speculated to be attributable to ADH and/or other enzymes (Person et al. 2000; Zimatkin et al. 2006).
The metabolism of ethanol by the prenatal brain has been of great interest, particularly given the impact ethanol consumption by pregnant women may have on the developing CNS of the fetus. Prenatal brain homogenates are capable of generating acetaldehyde from ethanol (Person et al. 2000). While CYP2E1 activity was shown to be present in the prenatal brain of humans, acetaldehyde formation appeared to occur by a mechanism independent of CYP2E1, catalase or ADH (Person et al. 2000). However, at birth (and in states of starvation) CYP2E1 induction by ethanol is rapid (Abdulla et al. 2006). While experiments using whole brain homogenates to investigate CYP2E1 metabolism of ethanol have often been equivocal, examination of specific brain locations have provided evidence of oxidation of ethanol by CYP2E1. This apparent disparity may be a consequence of whole brain enzymatic systems overshadowing discrete systems of specific brain regions and/or interference by fatty tissue that is abundant in the brain. Brain region-specific metabolism of ethanol may be extremely important. It is well established that specific brain regions are responsible for different CNS functions. Accordingly, the generation of different levels of ethanol metabolites depending on the enzyme present and the region could be responsible for different effects of ethanol on CNS function. For example, the presence of catalase and CYP2E1 ensure local formation of acetaldehyde, which mediates the positive reinforcing, motor disorder and local neurotoxic effects of alcohol (Zimatkin et al. 2006). Local metabolism results in local accumulation of ethanol metabolites and its condensation products (acetaldehyde, salsolinol, acetate) that would mediate the selective disturbances in certain brain structures and their involvement inthe behavioral effects of alcohol (Zimatkin et al. 2006). Ethanol treatment of male rats induced 1.7–2-fold increases in CYP2E1 protein and activity in olfactory bulbs, the frontal cortex, the hippocampus and the cerebellum (Howard et al. 2003a, b). In this same study, nicotine administration was shown to also induce CYP2E1 in the same CNS locations. These findings offer an explanation for the frequent co-addiction seen between ethanol and nicotine. Further, they underscore how the metabolism of ethanol is up-regulated upon co-treatment with nicotine and the corresponding CYP2E1 induction. In other animal studies, higher concentrations of CYP2E1 have been found in the hippocampus, medulla and substantia nigra (Howard et al. 2003a, b), brain regions responsible for memory and potentiation, autonomic functions, and dopamine regulation, respectively. By influencing acetaldehyde production at these sites, CYP2E1 may play a critical role in mediating the effects of ethanol.
CYP2E1 mRNA, protein, enzyme activity and induction by ethanol have been found in neural and glial cells of the CNS (Howard et al. 2003a, b). In a study of human brains obtained from smoking and non-smoking alcoholics, increased expression of CYP2E1 protein was found in granular cells of the dentate gyrus and pyramidal cells of the hippocampus (Howard et al. 2003a, b). Animal studies have found a higher concentration of CYP2E1 protein in astrocytes and glial cells following inflammatory induction (Sarc et al. 2011). The identification of CYP2E1 in dopaminergic neurons of the substantia nigra suggests that it may be involved in dopamine regulation (Howard et al. 2003a, b) and have potential implications in Parkinson disease.
Astroglial cells represent the majority of the brain cell population. They play an important role in the (i) developmental guidance of migrating neurons, (ii) regulation of neurotransmitter and ion levels, (iii) nutrition of neurons, and (iv) production of neurotrophic factors (Sarc et al. 2011). Astrocytes also represent a major site for the detoxification or bioactivation of neurotoxins and they are important contributors to the creation of the immune response in the brain (Sarc et al. 2011). Ethanol exposure changes growth, differentiation and function of neuronal and astroglial cells (Vemuri and Chetty 2005; Vangipuram and Lyman 2010; Sarc et al. 2011). For example, in rat primary cultures of astroglial cells, ethanol and acetaldehyde were both shown to be able to modulate TNF-alpha and IL6 production (Sarc et al. 2011). Therefore, alterations in acetaldehyde concentration through CYP2E1 induction have the potential to directly modulate astroglial cell function; however, more research is needed.
The intracellular processing of ethanol and its metabolites are important when considering how ethanol can influence cellular function. As noted, catalase is found primarily in the peroxisome and CYP2E1 is found primarily in the endoplasmic reticulum or microsomes of the cell (Fig. 8.1). As such, it is likely that the majority of ethanol is metabolized to acetaldehyde in these parts of the cell. Acetaldehyde must then diffuse to the mitochondria where it would be oxidized by ALDH2 to acetate (Deitrich et al. 2006). En route, acetaldehyde can interact with other molecules in the intracellular milieu and thereby alter cellular function.
Study of enzyme activities have been conducted in subcellular fractions of homogenates from mouse and rat brains (Zimatkin et al. 2006). These studies confirmed highest ethanol metabolizing activities of catalase and CYP2E1 to be present in the peroxisomal and microsomal fractions, respectively. Ethanol oxidation in the microsomal fraction increased with the addition of NADPH (a known CYP2E1 cofactor) and was decreased by CYP2E1 inhibitors, strengthening the contention that CYP2E1 is an essential enzyme in ethanol metabolism in the microsomal fraction. Ethanol oxidation was decreased in the microsomal fraction of CYP2E1-null mice (Vasiliou et al. 2006). The failure of CYP2E1 absence (in the CYP2E1-null mice) to prevent oxidation of ethanol by the microsomal fraction suggests that other enzymatic pathways may play a role (Vasiliou et al. 2006). Given the apparent specific subcellular locations of the ethanol-metabolizing enzymes, there is the potential that acetaldehyde could cause elicit cellular effects during its passage to the mitochondria where it is converted to acetate.
8.6 Regulation of CYP2E1 in the CNS
CYP2E1 can activate small, low molecular weight compounds. Some endogenous substrates for CYP2E1 include acetone and fatty acids (which are abundant in the brain) (Lieber 1999). CYP2E1 can also activate toxic compounds and procarcinogens found in tobacco smoke, such as nitrosamine compounds (Lieber 1999). Accordingly, induction of CYP2E1 by ethanol can promote bioactivation of these compounds (Howard et al. 2003a, b). As noted, CYP2E1 can also be induced by nicotine (found in cigarette smoke), which can result in bioactivation of the above compounds and in increased ethanol oxidation. Indeed, Howard and colleagues (2003a, b) determined that CYP2E1 was induced by nicotine, which offers an explanation for the increased self-administration of ethanol after exposure of rats to nicotine (Hauser et al. 2012). Induction of CYP2E1 in the CNS by nicotine likely increases the metabolism of ethanol to acetaldehyde, a result consistent with the theory that increases in CNS acetaldehyde causes reinforcement in ethanol preference.
In addition to chemical activation, CYP2E1 is differentially regulated by inflammation and infectious conditions (Abdulla et al. 2006). In this study, peripheral and central nervous system inflammation was induced in rats by lipopolysaccharide (LPS; an endotoxin that induces an inflammatory response in most animals) via intraperitoneal and intracerebroventricular administration, respectively. Under both conditions, inflammation caused an initial increase in hepatic CYP2E1 mRNA levels following by a decrease in CYP2E1 activity. The discovery of this regulatory mechanism in the liver in response to CNS inflammation led to the hypothesis that astroglial cells may have the potential to regulate CYP2E1 under similar circumstances (Abdulla et al. 2006). In another study in rat primary cortical glial cells, LPS was shown to induce the expression of catalytically-active CYP2E1, with a maximum induction occurring at 24 h (Tindberg et al. 1996). Clearly, the effects of inflammation on CYP2E1 regulation in the CNS are complex and differ greatly from cell culture models to in vivo studies.
8.7 Genetic Variation of CYP2E1 in Ethanol Sensitivity
The gene encoding the CYP2E1 enzyme is highly conserved among species, indicating its evolutionary importance. Genetic factors influence sensitivity and tolerance to ethanol in laboratory animals and humans (Bhave et al. 2006). Genetic factors influence sensitivity and tolerance to ethanol in laboratory animals and humans (Bhave et al. 2006). Genetic manipulation of enzyme expression has permitted mechanistic investigation of the roles of specific enzymes in ethanol oxidation. For example, acetaldehyde production following ethanol consumption is reduced in acatalasemic mice (Vasiliou et al. 2006). Acetaldehyde production by brain homogenates from CYP2E1-null mice was not affected by the absence of CYP2E1 (Vasiliou et al. 2006), bringing into question the importance of this enzyme in ethanol oxidation. However, acetaldehyde production in CYP2E1-null/acatalasemic mice was significantly lower than the already reduced levels observed in acatalasemic mice. The difference between the levels confirms the significance of the CYP2E1 enzyme (Vasiliou et al. 2006).
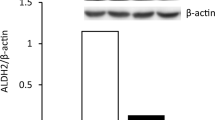
A role for genetic polymorphisms in the genes coding for the enzymes in ethanol metabolism was proposed to explain ethanol preference between inbred C57BL/6 (high preference) and DBA/2 (low preference) strains of mice (Bhave et al. 2006). There are nine known ADH-coding genes and three catalase-coding genes in the mouse (Bhave et al. 2006). The genes encoding cytochrome P450 families range from 82 to 102, depending on the source (Bhave et al. 2006). A gene array allowed the comparison of genes from the two mouse lines bred for different preferences for ethanol but naïve to ethanol exposure. As quantified by the array, the intensity for CYP2E1 was low or undetectable in ethanol naïve mice (Bhave et al. 2006). The failure to observe any increase could be due to testing the whole brain tissue rather than specific locations, cells or subcellular fractionations. The main result of this study was that ethanol preference was due to genetic differences in ALDH2, the enzyme responsible for metabolizing acetaldehyde to acetate. The low preferring DBA2 strain had higher amounts of ALDH mRNA in the CNS and the high preferring C57BL/6 had lower levels of ALDH (Bhave et al. 2006). Low levels of ALDH would potentially cause increased concentrations of acetaldehyde, providing additional evidence that acetaldehyde in the CNS is reinforcing.
There is the potential that induction of CYP2E1 by nicotine could contribute to metabolic tolerance in smoking alcoholics. This possibility led to research into the impact of polymorphisms that induce CYP2E1 on alcohol dependence. Specifically, the CYP2E1*1D polymorphism was found to occur with greater frequency in nicotine- or alcohol- dependent populations and it showed an association with nicotine- and alcohol- dependence (Howard et al. 2003a, b). The greater inducibility of CYP2E1 associated with this polymorphism is likely to contribute to the development of nicotine and ethanol co-dependencies (Howard et al. 2003a, b), because of increased metabolism of ethanol and nicotine. Other polymorphisms for CYP2E1 exist in different populations; however, correlations between genotype (polymorphism) and phenotype (ethanol preference or dependence) are yet to be conducted.
8.8 Conclusion
The discovery of ethanol metabolizing enzymes in the CNS has led to much research into the effect of ethanol and its metabolic products on behavior and addiction. Because CYP2E1 can be induced by ethanol and nicotine, it has been the focus of major studies in addiction and co-addiction involving ethanol. Some studies investigating ethanol sensitivity focus on the primary product of ethanol oxidation, acetaldehyde, while others examine both acetaldehyde and its final product, acetate. To determine ethanol effects in response to the presence and quantity of ethanol and its metabolites, behavioral, locomotor or preferential tests are usually conducted in animals. Through the use of inhibitors or inducers of the main ethanol-metabolizing agents, as well as genetic manipulation of enzyme expression, the importance of CYP2E1 in the CNS and in regulating sensitivity to ethanol is beginning to be revealed.
References
Abdulla D, Goralski KB et al (2006) The regulation of cytochrome P450 2E1 during LPS-induced inflammation in the rat. Toxicol Appl Pharmacol 216(1):1–10
Alfonso-Loeches S, Guerri C (2011) Molecular and behavioral aspects of the actions of alcohol on the adult and developing brain. Crit Rev Clin Lab Sci 48(1):19–47
Aragon CM, Rogan F et al (1992) Ethanol metabolism in rat brain homogenates by a catalase-H2O2 system. Biochem Pharmacol 44(1):93–98
Bansal S, Liu CP et al (2010) Mitochondria-targeted cytochrome P450 2E1 induces oxidative damage and augments alcohol-mediated oxidative stress. J Biol Chem 285(32):24609–24619
Beisswenger TB, Holmquist B et al (1985) chi-ADH is the sole alcohol dehydrogenase isozyme of mammalian brains: implications and inferences. Proc Natl Acad Sci USA 82(24):8369–8373
Bhave SV, Hoffman PL et al (2006) Gene array profiles of alcohol and aldehyde metabolizing enzymes in brains of C57BL/6 and DBA/2 mice. Alcohol Clin Exp Res 30(10):1659–1669
Brust JC (2010) Ethanol and cognition: indirect effects, neurotoxicity and neuroprotection: a review. Int J Environ Res Public Health 7(4):1540–1557
Cheung C, Yu AM et al (2005) The cyp2e1-humanized transgenic mouse: role of cyp2e1 in acetaminophen hepatotoxicity. Drug Metab Dispos 33(3):449–457
Correa M, Arizzi MN et al (2003) Open field locomotor effects in rats after intraventricular injections of ethanol and the ethanol metabolites acetaldehyde and acetate. Brain Res Bull 62(3):197–202
Correa M, Manrique HM et al (2008) Reduction in the anxiolytic effects of ethanol by centrally formed acetaldehyde: the role of catalase inhibitors and acetaldehyde-sequestering agents. Psychopharmacology (Berl) 200(4):455–464
Davis VE, Walsh MJ (1970) Alcohol, amines, and alkaloids: a possible biochemical basis for alcohol addiction. Science 167(3920):1005–1007
Deitrich RA (2004) Acetaldehyde: Deja vu du jour. J Stud Alcohol 65(5):557–572
Deitrich R (2011) Ethanol as a prodrug: brain metabolism of ethanol mediates its reinforcing effects–a commentary. Alcohol Clin Exp Res 35(4):581–583
Deitrich RA, Dunwiddie TV et al (1989) Mechanism of action of ethanol – initial central-nervous-system actions. Pharmacol Rev 41(4):489–537
Deitrich R, Zimatkin S et al (2006) Oxidation of ethanol in the brain and its consequences. Alcohol Res Health 29(4):266–273
Dey A, Kumar SM (2011) Cytochrome P450 2E1 and hyperglycemia-induced liver injury. Cell Biol Toxicol 27(4):285–310
Edenberg HJ (1998) Genetics of alcoholism. Science 282(5392):1269
Estonius M, Svensson S et al (1996) Alcohol dehydrogenase in human tissues: localisation of transcripts coding for five classes of the enzyme. FEBS Lett 397(2–3):338–342
Galter D, Carmine A et al (2003) Distribution of class I, III and IV alcohol dehydrogenase mRNAs in the adult rat, mouse and human brain. Eur J Biochem 270(6):1316–1326
Gill K, Menez JF et al (1992) Enzymatic production of acetaldehyde from ethanol in rat brain tissue. Alcohol Clin Exp Res 16(5):910–915
Ginter E, Simko V (2009) Alcoholism: recent advances in epidemiology, biochemistry and genetics. Bratisl Lek Listy 110(5):307–311
Hauser SR, Getachew B et al (2012) Nicotine modulates alcohol-seeking and relapse by alcohol-preferring (P) rats in a time-dependent manner. Alcohol Clin Exp Res 36(1):43–54
Howard LA, Ahluwalia JS et al (2003a) CYP2E1*1D regulatory polymorphism: association with alcohol and nicotine dependence. Pharmacogenetics 13(6):321–328
Howard LA, Miksys S et al (2003b) Brain CYP2E1 is induced by nicotine and ethanol in rat and is higher in smokers and alcoholics. Br J Pharmacol 138(7):1376–1386
Karahanian E, Quintanilla ME et al (2011) Ethanol as a prodrug: brain metabolism of ethanol mediates its reinforcing effects. Alcohol Clin Exp Res 35(4):606–612
Kerr JT, Maxwell DS et al (1989) Immunocytochemistry of alcohol dehydrogenase in the rat central nervous system. Alcohol Clin Exp Res 13(6):730–736
Knockaert L, Fromenty B et al (2011) Mechanisms of mitochondrial targeting of cytochrome P450 2E1: physiopathological role in liver injury and obesity. FEBS J 278(22):4252–4260
Lee SS, Buters JT et al (1996) Role of CYP2E1 in the hepatotoxicity of acetaminophen. J Biol Chem 271(20):12063–12067
Lieber CS (1999) Microsomal ethanol-oxidizing system (MEOS): the first 30 years (1968–1998)–a review. Alcohol Clin Exp Res 23(6):991–1007
Martinez SE, Vaglenova J et al (2001) Distribution of alcohol dehydrogenase mRNA in the rat central nervous system. Consequences for brain ethanol and retinoid metabolism. Eur J Biochem 268(19):5045–5056
McBride WJ, Li TK et al (2002) Involvement of acetaldehyde in alcohol addiction. Alcohol Clin Exp Res 26(1):114–119
Melchior CL, Myers RD (1977) Preference for alcohol evoked by tetrahydropapaveroline (THP) chronically infused in the cerebral ventricle of the rat. Pharmacol Biochem Behav 7(1):19–35
Mokdad AH, Marks JS et al (2004) Actual causes of death in the United States, 2000. JAMA 291(10):1238–1245
Person RE, Chen H et al (2000) Enzymic catalysis of the accumulation of acetaldehyde from ethanol in human prenatal cephalic tissues: Evaluation of the relative contributions of CYP2E1, alcohol dehydrogenase, and catalase/peroxidases. Alcohol Clin Exp Res 24(9):1433–1442
Quertemont E, Tambour S et al (2004) Behavioral characterization of acetaldehyde in C57BL/6J mice: locomotor, hypnotic, anxiolytic and amnesic effects. Psychopharmacology (Berl) 177(1–2):84–92
Quintanilla ME, Tampier L et al (2007) Sex differences, alcohol dehydrogenase, acetaldehyde burst, and aversion to ethanol in the rat: a systems perspective. Am J Physiol Endocrinol Metab 293(2):E531–E537
Raza H, Prabu SK et al (2004) Elevated mitochondrial cytochrome P450 2E1 and glutathione S-transferase A4-4 in streptozotocin-induced diabetic rats: tissue-specific variations and roles in oxidative stress. Diabetes 53(1):185–194
Robin MA, Anandatheerthavarada HK et al (2001) Mitochondrial targeted cytochrome P450 2E1 (P450 MT5) contains an intact N terminus and requires mitochondrial specific electron transfer proteins for activity. J Biol Chem 276(27):24680–24689
Robin MA, Anandatheerthavarada HK et al (2002) Bimodal targeting of microsomal CYP2E1 to mitochondria through activation of an N-terminal chimeric signal by cAMP-mediated phosphorylation. J Biol Chem 277(43):40583–40593
Rodd-Henricks ZA, Melendez RI et al (2002) The reinforcing effects of acetaldehyde in the posterior ventral tegmental area of alcohol-preferring rats. Pharmacol Biochem Behav 72(1–2):55–64
Sarc L, Wraber B et al (2011) Ethanol and acetaldehyde disturb TNF-alpha and IL-6 production in cultured astrocytes. Hum Exp Toxicol 30(9):1256–1265
Tabakoff B, Anderson RA et al (1976) Brain acetaldehyde after ethanol administration. Biochem Pharmacol 25(11):1305–1309
Thurman RG, Ley HG et al (1972) Hepatic microsomal ethanol oxidation. Hydrogen peroxide formation and the role of catalase. Eur J Biochem 25(3):420–430
Tindberg N, Baldwin HA et al (1996) Induction of cytochrome P450 2E1 expression in rat and gerbil astrocytes by inflammatory factors and ischemic injury. Mol Pharmacol 50(5):1065–1072
Vangipuram SD, Lyman WD (2010) Ethanol alters cell fate of fetal human brain-derived stem and progenitor cells. Alcohol Clin Exp Res 34(9):1574–1583
Vasiliou V, Ziegler TL et al (2006) CYP2E1 and catalase influence ethanol sensitivity in the central nervous system. Pharmacogenet Genomics 16(1):51–58
Vemuri MC, Chetty CS (2005) Alcohol impairs astrogliogenesis by stem cells in rodent neurospheres. Neurochem Int 47(1–2):129–135
Westcott JY, Weiner H et al (1980) In vivo acetaldehyde in the brain of the rat treated with ethanol. Biochem Pharmacol 29(3):411–417
Zakhari S (2006) Overview: how is alcohol metabolized by the body? Alcohol Res Health 29(4):245–254
Zimatkin SM (1991) Histochemical study of aldehyde dehydrogenase in the rat CNS. J Neurochem 56(1):1–11
Zimatkin SM, Pronko SP et al (2006) Enzymatic mechanisms of ethanol oxidation in the brain. Alcohol Clin Exp Res 30(9):1500–1505
Zimatkin SM, Oganesian NA et al (2011) Acetate-dependent mechanisms of inborn tolerance to ethanol. Alcohol Alcohol 46(3):233–238
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Heit, C., Dong, H., Chen, Y., Thompson, D.C., Deitrich, R.A., Vasiliou, V.K. (2013). The Role of CYP2E1 in Alcohol Metabolism and Sensitivity in the Central Nervous System. In: Dey, A. (eds) Cytochrome P450 2E1: Its Role in Disease and Drug Metabolism. Subcellular Biochemistry, vol 67. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-5881-0_8
Download citation
DOI: https://doi.org/10.1007/978-94-007-5881-0_8
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-5880-3
Online ISBN: 978-94-007-5881-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)