Abstract
Given the rapid spread of economic globalization and technological progress, work and employment have changed significantly. In general, working people are less often exposed to physically strenuous work but more often to psycho-mental stress at work. Despite improved occupational safety measures, occupational hazards and injuries, shift work, overtime work, and adverse psychosocial work environments contribute to a substantial burden of work-related diseases. This burden of disease is unequally distributed between and within countries, leaving socially deprived groups at higher risk of poor health. This chapter presents updated empirical evidence on associations of adverse work and employment conditions with the health of working people. Moreover, it elucidates the contribution of work and employment to social inequalities in adult health. The concluding remarks address policy implications of scientific evidence, with special emphasis on the role of health-promoting national labor and social policies.
Some parts of this contribution were written with close reference to the following document: Siegrist, Rosskam, and Leka (2011). Review of social determinants of health and the health divide in the WHO European Region: Employment and working conditions including occupation, unemployment and migrant workers. Copenhagen: World Health Organization (Unpublished report).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Occupational hazards
- Work stress
- Health inequalities
- Job strain
- Effort-reward imbalance
- Labor and social policies
1 Introduction
Paid work continues to be of critical importance for population health and health inequalities in developed and rapidly developing countries. This is primarily due to the fact that participation in or exclusion from the labor market determines a wide range of life chances that are mediated through regular wages and salaries. Poverty and relative deprivation are widespread among people who lost their job or were prevented from entering the labor market. In addition, long-term unemployment is associated with elevated risks of morbidity and mortality (see below). As work and employment confer social status and related esteem, they may contribute to health-promoting experiences of self-worth, self-efficacy, and a sense of social identity in adult life. Yet, these potentially positive effects are balanced by the adversities and stressors emerging from dangerous and precarious work and employment.
Against this background, this chapter addresses the following questions: (1) What aspects of work and employment affect workers’ health and how?, (2) What is the contribution of work and employment to the development of health inequalities?, (3) Do distinct macro-structural policies related to work and employment matter in this context?, and (4) What are the policy implications of available scientific evidence?
2 Unhealthy Work in a Globalized Economy
With the advent of economic globalization, free market principles in conjunction with technological innovations spread over the world, stimulating large flows of transnational capital, trade, and labor force. Whereas economic globalization is often perceived as enhancing gross national product and increasing national employment rates, particularly in rapidly developing countries undergoing industrialization and urbanization, its adverse consequences are less strongly emphasized. Yet, given growing competition and pressure towards an increase in return on investment, a general intensification of work has been reported in the recent past (Eurostat. European Commission, 2010). This intensification often goes along with an increase in job instability and insecurity, due to threat of job loss or redundancy, downsizing, outsourcing, and the privatization of public services (Landsbergis, 2003). Another consequence of economic globalization concerns segmentation of the labor market and a related increase in income inequality. On the one hand, there is a well-trained, skilled, and flexible workforce with fair promotion prospects and adequate earnings. On the other hand, large parts of the workforce suffer from precarious employment, low wages, exposure to hazards, and low safety at work. At the same time, welfare state policies and trade union activities are weakened, thus augmenting the burden of stressful work among the most vulnerable and deprived groups of national workforces (Landsbergis, 2003; Schnall, Dobson, & Rosskam, 2009).
This process of economic globalization was preceded (and critically accelerated) by profound changes in the nature of employment and work during the past century, manifested by a large expansion of service occupations and professions, a growing impact of automation and information technology, and an unprecedented flexibility of employment arrangements and contracts. Although physically strenuous work and exposure to chemical, biological, and physical hazards continue to pose serious challenges to workers’ health and safety, the threats of a health-adverse psychosocial work environment are now becoming more visible, and they contribute to a growing burden of work-related diseases.
Broadly speaking, three categories of unhealthy work can be distinguished, in addition to the afflictions resulting from job loss and unemployment: (1) physical, biological, and chemical hazards including occupational injuries, (2) work-time related factors with impact on mental and physical health (e.g., shift work, long work hours), and (3) adverse psychosocial work environments affecting workers’ health and well-being either by psychobiological pathways or by health-damaging behaviors. The relevance and impact of these categories on workers’ health varies considerably across countries, and most importantly between economically advanced and developing countries. Here, we briefly summarize some evidence of these three categories of unhealthy work, with an emphasis on studies conducted in advanced Western countries.
2.1 Occupational Hazards and Injuries
The European-wide panel survey on working conditions indicated that, in 2005, every sixth worker in Europe was exposed to toxic substances at the workplace, and almost one third was exposed to noise at work, at least intermittently. Moreover, 24 % reported exposure to vibrations, 45 % were working in painful, tiring positions, and more than half were confined to repetitive hand or arm movements, mainly due to computer work (Parent-Thirion, Macias, Hurley, & Vermeylen, 2007). Findings from the latest panel wave by and large confirm these trends (Eurostat. European Commission, 2010). It is evident that physical and chemical stressors at work make a significant contribution to the burden of work-related diseases and injuries (Verma, Purdham, & Roels, 2002). Specifically, occupational groups with a high percentage of workers in lower socio-economic positions are at elevated risk of occupational injuries and accidents, such as construction workers, agricultural workers, transport workers, or miners (Arndt et al., 2005). Moreover, unhealthy or restricted posture at work, repetitive movements, and heavy lifting are more prevalent among lower status workers, and these conditions increase the risk of musculoskeletal disorders (Bernard, 1997). Workers exposed to these physically stressful conditions are less likely to be able to work until retirement age (Parent-Thirion et al., 2007), and their risk of needing disability pension is increased by 50–100 % compared to unexposed workers (Blekesaune & Solem, 2005). In addition to unhealthy posture at work, sedentary work was shown to be a risk factor of reduced health, with particular importance for cardiovascular disease (Olsen & Kristensen, 1991).
Apart from asbestos and related lung diseases and certain carcinogenic substances, a majority of investigations in the field of occupational medicine explored toxic effects at work on the cardiovascular system. Toxic effects include carbon monoxide, nitrates, carbon disulfide (CS2), and nanoparticles and fine particles (PM 2,5) among others. In addition to these chemical factors, physical factors such as cold, heat, vibration, and noise matter for cardiovascular health. Noise is a special case, as it is difficult to disentangle its sound-related physiological effects from the biological effects elicited by emotionally stressful experience (Steenland, 2000). Physical, ergonomic, and chemical hazards at work are often combined with an adverse psychosocial work environment, thus multiplying health risks among exposed people. Few studies have documented the long-term health effects of these cumulative exposures in any detail (Devereux, Vlachonikolis, & Buckle, 2002; Dragano, 2007).
Fewer scientific studies are available on health-adverse effects of these occupational hazards and injuries in less developed, rapidly growing countries, but there is reason to believe that the respective burden of disease is much larger, given generally lower levels of occupational safety and health monitoring, lower investments in the proliferation of occupational health services, and deficiencies in implementing laws, regulations, and protective devices at national, regional, and local levels (Rantanen, 2010).
2.2 Work-Time Related Health Risks
In addition to the physical environment, the organization of work, and specifically of work time, plays an important role in triggering occupational health risks, physical and chemical hazards and injuries, and psychosocial adversity. Work-time arrangements differ between occupational groups, and some of these arrangements were shown to have adverse consequences for the health and well-being of workers. This holds particularly true for shift work and long work hours. Globally, there is a high prevalence of overtime work, irregular work, and periods of commitment to extensive work hours. Within European countries, about every tenth male worker reported working regularly more than 60 h per week (Parent-Thirion et al., 2007). For special service occupations and professions, persons performing on-call jobs, freelancers, and several groups having ‘modern,’ less formalized, atypical jobs, it has become increasingly difficult to clearly distinguish work from non-work periods in their daily life. Another frequent work-time related problem concerns shift work. Shift work is frequent in the production sector and in some service occupations and professions. Overall, in the 27 member countries of the European Union, the prevalence of shift work is 17 % (Eurostat. European Commission, 2010). A strong social gradient of shift work is obvious. Twenty-six per cent of low skilled manual workers in the survey, compared to 12 % of skilled manual workers, reported performing regular shift work. Shift work and long work hours are the two conditions that have been the most widely studied with respect to adverse health effects. Results suggest that the risk of cardiovascular disease in shift workers is about 40 % higher than that risk in daytime workers (Härmä, 2006). Similarly, an increased risk of developing metabolic syndrome was observed among shift workers, with a relative risk of about 1.7 (De Bacquer et al., 2009). Additional investigations demonstrate an elevated risk of accidents, particularly amongst evening and night shift workers (Bambra, Whitehead, Sowden, Akers, & Petticrew, 2008). Reported health effects are contingent on duration of shift work, with marked increases after more than 10 years of continued exposure (Steenland, 2000). Night shifts are particularly relevant as a potential source of work accidents, cardiovascular and gastro-intestinal problems, and eventually cancer (Swerdlow, 2003). Combined effects of shift work and chronic psychosocial stress at work were observed for coronary heart disease and for poor mental health (Bøggild, Burr, Tüchsen, & Jeppesen, 2001; Peter, Alfredsson, Knutsson, Siegrist, & Westerholm, 1999).
Extended or irregular work hours provide an additional occupational health risk. For instance, working more than 11 h a day is associated with a threefold risk of myocardial infarction (Van der Hulst, 2003), and a fourfold increased risk of type 2 diabetes (Kawakami, Araki, Takatsuka, Shimizu, & Ishibashi, 1999). Moreover, in jobs with an overtime schedule the risk of injury is increased by 61 % amongst American workers (Dembe, Erickson, Delbos, & Banks, 2006). In an 11-year longitudinal study with Finnish workers, atherosclerotic plaque growth in the carotid was proportional to number of days worked per week and to annual work hours (Krause et al., 2009). Finally, the risk of coronary heart disease was increased by about 70 % among British civil servants who worked 3–4 h overtime each day for a period of about 10 years, compared to study participants working normal hours (Kivimäki et al., 2011).
Again, the conditions of shift work, irregular work hours, and overtime work are highly prevalent in developing countries, and there are large discrepancies concerning their regulation and control between the most advanced and less developed countries (Rantanen, 2010).
2.3 Health-Adverse Psychosocial Work Environments
Psychosocial risks contributing to the experience of stressful work are widely recognized as major challenges to current occupational health. As explained, economic globalization induces work intensification among many occupational groups, often in combination with threats to job security, promotion prospects, and fair pay. Being repeatedly challenged or overtaxed by demands, losing control over one’s own tasks, being treated unfairly, and suffering from threats to one’s legitimate rewards at work are major conditions that evoke recurrent stressful experiences with adverse long-term effects on physical and mental health. To identify these conditions, which are often embedded in complex and variable work environments, a theoretical model is needed. Whereas several such models have been developed (Cartwright & Cooper, 2009), only few concepts have been repeatedly tested with rigorous study designs. Among these, three models have received special attention in international research, the demand-control (or job strain) model, the effort-reward imbalance model, and the model of organizational injustice.
The demand-control (or job strain) model identifies stressful work in terms of job task profiles defined by high psychological demands and a low degree of control or decision latitude (Karasek & Theorell, 1990). Stressful experience resulting from this exposure is due to limited experience of personal control and self-efficacy in combination with continued high work pressure. ‘Effort-reward imbalance’ was developed as a complementary model with a primary focus on the work contract; at the core of the model is the principle of social reciprocity (Siegrist, 1996). Rewards received in return for efforts expended at work include money, esteem, and career opportunities (promotion, job security). The model asserts that lack of reciprocity (high effort in combination with low reward) occurs frequently and generates strong negative emotions and psychobiological stress responses with adverse long-term effects on health. More recently, the concept of organizational justice was introduced, proposing adverse health effects of three aspects of injustice (distributive, i.e., perceived fairness of the distribution of valued resources; procedural, i.e., perceived fairness of decision making; interactional, i.e., perceived fairness of being treated by superiors and colleagues) (Greenberg, 2010; Elovainio, Kivimäki, & Vahtera, 2002).
Several systematic reviews summarized the current state of the art in this rapidly expanding field of occupational health research (Eller et al., 2009; Greenberg, 2010; Kivimäki et al., 2006; Leka & Jain, 2010; Nieuwenhuijsen, Bruinvels, & Frings-Dresen, 2010; Stansfeld & Candy, 2006; Tsutsumi & Kawakami, 2004). A majority of prospective observational cohort studies tested these work stress models with regard to cardiovascular diseases and poor mental health (mainly depression), given their significant contribution to the worldwide burden of disease (for detailed review, see Siegrist et al., 2011). Concerning cardiovascular disease, a majority of at least 30 reports derived from prospective studies document elevated odds ratios of fatal or non-fatal cardiovascular events among persons reporting job strain, effort-reward imbalance, or organizational injustice. Overall, risks are 40 % to 50 % higher among persons suffering from psychosocial stress at work compared to persons who are free of stress at work. Effects are stronger in men than in women and more pronounced in middle-aged than in older working populations. Similar effects are observed in case of re-infarction after survived first coronary heart disease.
In addition, several cardiovascular risk factors are associated with an adverse psychosocial work environment, in particular metabolic syndrome (Chandola, Brunner, & Marmot, 2006), type 2 diabetes (Kumari, Head, & Marmot, 2004), hypertension (Schnall, Belkić, Landsbergis, & Baker, 2000), and health-adverse behaviors (Siegrist & Rödel, 2006). With respect to mental health, major results from prospective investigations confirm elevated risks of depression among employees with work-related stress in terms of these models, and odds ratios vary between 1.5 and 3.6, depending on type of measure, gender, and occupational group under study (Bonde, 2008; Nieuwenhuijsen et al., 2010).
Other health outcomes significantly related to job strain, effort-reward imbalance, or organizational injustice concern reduced physical and mental functioning (Stansfeld, Bosma, Hemingway, & Marmot, 1998), musculoskeletal disorders (Rugulies & Krause, 2008), and disability pension (Dragano, 2007).
It is clear from this brief summary that effects of an adverse psychosocial work environment on health have mainly been studied in advanced Western countries. However, importantly, several recent findings from rapidly developing countries, mainly China (Xu, Zhao, Guo, Guo, & Gao, 2009) and Brazil (Harter Griep, Rotenberg, Chor, Toivanen, & Landsbergis, 2010), are confirming the relevance of these models in explaining occupational health in these countries as well.
In summary, three pathways leading from occupational exposures to physical and mental disorders were described, acting as toxic chemical, physical, or biological stressors, as psychosocial stressors eliciting psychobiological stress reactions in the organism, or as determinants of risk behavior. In many workplaces multiple interactions between these pathways are observed. The prevalence of these pathways differs between economically advanced and rapidly developing countries, and much more scientific evidence and preventive practice is established in advanced countries. Yet, given the universality of underlying mechanisms, there is reason to believe that the burden of unhealthy work in rapidly developing countries in the long run will be similar to the burden observed in Western countries.
3 Employment, Work, and Health Inequalities
It is evident from the reported findings that the quality of work and employment follows a social gradient, leaving persons in lower socioeconomic positions in more deprived conditions. This has been documented for risk of long-term unemployment, precarious work (defined by job insecurity, poor safety at work, exposure to multiple stressors, low wage, and lack of control), physical work, shift work, job strain, and effort-reward imbalance (Johnson, 2009; Siegrist & Theorell, 2006). Adverse health effects of unemployment are probably the strongest single determinant of work-related social inequalities in health, at least in a global perspective. This is due to the fact that the risk of job loss and long-term unemployment increases with each step a person moves down the ladder of educational qualifications, with highest risks among unskilled and semi-skilled workers and among less qualified migrant workers. A substantial body of evidence indicates an elevated burden of disease due to long-term unemployment (for a review, see Schnall et al., 2009; Siegrist et al., 2011). More specifically, risks of fatal or non-fatal cardiovascular or cerebrovascular events and risks of all-cause mortality are twice as high. Similar effects were observed for depression, suicide, functional limitations and health-adverse behaviors, especially heavy drinking. In this context, the mortality crisis of men in Russia and other post-communist countries in Eastern Europe deserves special attention, as it is likely that the sudden loss of core social roles in the lives of large numbers of men contributed to stress-associated morbidity and mortality (Stuckler, Basu, Suhrcke, Coutts, & McKee, 2009).
Among working people in lower social positions, occupational injuries and the majority of traditional occupational diseases are more prevalent than among people in more privileged positions. Major chronic diseases in midlife and early old age, in particular cardiovascular diseases, depression, metabolic disorders, pulmonary disease, and certain cancers, were additionally shown to follow a social gradient, with higher burden of disease among the less privileged segments of working populations (Marmot, 2004). Clearly, only a minor part of this burden of chronic disease is attributable to adverse working conditions, but in view of the frequency of unhealthy working conditions and the elevated risks of incidence following exposure to stressful work, their impact is nevertheless considerable (Siegrist & Theorell, 2006).
To analyze more precisely the contribution of an adverse psychosocial work environment to explaining social inequalities in health, two strategies are applied – the mediation hypothesis and the effect modification hypothesis. The mediation hypothesis claims that a substantial part of the strength of the association between socioeconomic position and health is due to the impact of adverse working conditions on health. In this view, stressful work and employment are considered core determinants of social inequalities of health in midlife and early old age. The effect modification hypothesis posits that susceptibility to an exposure (such as health-adverse work and employment) is higher among employees in lower socioeconomic positions compared to higher status people and, therefore, that the effect size produced by the exposure is higher. This hypothesis is based on evidence of poorer material and psychosocial coping resources among persons with lower status, whose exposure to adversities and threats is particularly high.
Currently, there is limited evidence supporting either hypothesis. For instance, using multivariate regression analysis to test the mediation hypothesis, low control at work was independently associated with incidence of coronary disease and with low socioeconomic status in the Whitehall II Study (Marmot, Bosma, Hemingway, Brunner, & Stansfeld, 1997). In a multivariate analysis, low control in the workplace accounted for about half the social gradient of coronary heart disease. Additional studies reviewed elsewhere (Siegrist & Theorell, 2006) were conducted along these lines. An investigation that analyzed hospital injury rates in relation to socioeconomic status and working conditions in different occupational groups of two private hospitals in Massachusetts deserves special attention (D’Errico et al., 2007). Whereas a strong social gradient of injury rates was found, this gradient was greatly attenuated when controlling for psychosocial and ergonomic workplace exposures. These exposures were decision latitude, reward (psychosocial), bending, kneeling, and forceful exertion (ergonomic).
The effect modification hypothesis was tested in several studies, where the effect of job strain and of high effort and low reward at work on health was found to be greater in lower than in higher socioeconomic groups (Johnson & Hall, 1988; Wege et al., 2008). For instance, in a German study, depressive symptoms were almost seven times more frequent in the lowest occupational group scoring high on effort-reward imbalance than in the highest occupational group scoring low on effort-reward imbalance (Wege et al., 2008).
In conclusion, given a powerful social gradient of morbidity and mortality in working age populations and given a clear-cut social gradient of the quality of work and employment, it is obvious that this latter condition has direct impact on health, as analyzed by the mediation and the effect modification hypotheses.
So far, our analysis has been restricted to organizational contexts of unequal work and its effects on unequal health. However, it is important to know whether also the wider macro-political context has an impact on quality of work and employment and thus may indirectly affect workers’ health. This question is discussed in brief in the following section.
4 Macro-Structural Aspects
National labor and social policies can influence the quality of work and employment within respective workforces by setting rules and regulations which protect workers’ health, by investing in active labor market policies including rehabilitation services, and by offering financial support in case of job loss and other income shocks. It is therefore assumed that the mean quality of work and employment is more favorable in countries that developed welfare state measures than in countries with poor welfare state investments.
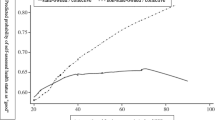
In a cross-national comparative study, the Survey of Health, Ageing and Retirement in Europe (SHARE), these associations were tested in a sample of 6,619 men and 7,688 women in 13 European countries. Data on mean perceived quality of the psychosocial work environment (low control, low reward) in each country were correlated with the country’s performance in terms of three labor policy indicators available from OECD statistics: (a) the percentage of persons aged 25–64 who stated that they received education or training in the last month, (b) the amount of expenditures in favor of education or training, measured as percentage of the gross domestic product, (c) the amount of expenditures in favor of rehabilitation services for people with limited working capacity, again measured as percentage of the gross domestic product (for details, see Siegrist & Wahrendorf, 2011). As Fig. 2.1 shows, consistent ecological correlations are observed between mean quality of work, measured as the percentage of persons reporting poor control (upper part) and poor reward, respectively (lower part in Fig. 2.1), and the amount of the country’s labor and social policy investment. Associations are particularly strong with regard to the first and the third macro-policy indicator. In general, the Nordic countries, Switzerland, and the Netherlands display more favorable conditions than southern and eastern European countries, indicating that higher investments in social and labor policies go along with higher mean quality of work. Furthermore, preliminary evidence suggests that mean odds ratios of experiencing poor mental health as a function of low quality of work are higher in countries with low policy investments as compared to odds ratios in countries with substantial policy investments (Dragano, Siegrist, & Wahrendorf, 2011).
Macro indicators and poor quality of work (based on weighted data) (Siegrist & Wahrendorf, 2011, p. 174). Exp expenditure. Note. Based on weighted data
These preliminary results support the notion that the analysis of work and employment in the context of health inequalities needs to be broadened beyond organization-level characteristics to include distinct national labor and social policies. Broadening the frames of reference has important policy implications, as will be briefly discussed in the final section.
5 Policy Implications
An obvious conclusion from the empirical evidence presented in the previous sections points to the need to supplement organization-level and interpersonal-level measures of worksite health promotion by distinct macro-structural policies. To reduce the social gradient of health in working age populations effectively, national level policies are needed that target the country’s overall protection system. These policies should serve as a mandate to individual organizations and workplaces to implement interventions where problems exist. Therefore, national budget and tax policies are recommended that allow the maintenance and further development of active labor market policies. In this process, improved monitoring and risk management systems with regard to occupational health hazards are instrumental. The same holds true for best practice models that may be available from some pioneering countries. Furthermore, international organizations can provide useful support, such as initiatives from EU agencies, the International Labor Organization (ILO), and the World Health Organization (WHO).
Priorities of national regulations that aim at promoting healthy work and reducing health inequalities concern the protection of workers from job instability and redundancy, the control of long work hours, shift work, and exposure to hazardous chemical, physical, and psychosocial exposures, and the provision of comprehensive occupational health and safety services that also meet prevention and rehabilitation needs of occupational risk groups. Next, at the level of single organizations, companies, or branches, at least the following policy recommendations can be proposed in view of currently available scientific evidence:
-
Increase the flexibility of work-time arrangements, including broader opportunities for part-time work and continued training, as well as ‘flexicurity’ models of occupational careers
-
Secure fair pension and retirement arrangements in relation to both lifetime contributions to the labor market and major shocks (long-term unemployment, forced early retirement, disability pension)
-
Implement measures of organizational and personnel development that are instrumental in increasing control at work and in providing fair rewards in return for effort expended; these measures concern separate organizations as well as larger bodies of branches, stakeholder associations, trade unions, or even national and transnational legislation.
This latter recommendation could be further specified by pointing to models of good practice that are already available in the context of European-wide initiatives (Siegrist & Wahrendorf, 2011). Measures include the reorganization of division of work, with the aim of developing more complete job task profiles (job enlargement, job enrichment, for example) and more adequate promotion prospects (including job security, more flexible forms of remuneration and non-monetary gratification, enhanced leadership training, and the development of a culture of trust, fairness, and transparency at organizational level). These measures should specifically target lower status occupational groups with an effort to reduce their work-related burden of disease.
In conclusion, within a globalized economy the reduction of poor quality of employment and work and the reduction of their adverse effects on workers’ health provide substantial challenges to international occupational public health. But over the past two or three decades we have witnessed a substantial increase of scientific evidence on causes and consequences of unhealthy work, and enhanced policy efforts to tackle these challenges are emerging at international, national, and local levels. Therefore, there is hope that these efforts will ultimately result in a sizeable reduction of health inequalities and the growth of sustainable and healthy work.
References
Arndt, V., Rothenbacher, D., Daniel, U., Zschenderlein, B., Schuberth, S., & Brenner, H. (2005). Construction work and risk of occupational disability: A ten year follow up of 14,474 male workers. Occupational and Environmental Medicine, 62, 559–566.
Bambra, C. L., Whitehead, M. M., Sowden, A. J., Akers, J., & Petticrew, M. P. (2008). Shifting schedules: The health effects of reorganizing shift work. American Journal of Preventive Medicine, 34, 427–434.
Bernard, B. P. (Ed.). (1997). Musculoskeletal disorders and workplace factors: A critical review of epidemiological evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. DHHS (NIOSH) publication no. 97B141. Cincinnati, OH: National Institute for Occupational Safety and Health. Retrieved from http://www.cdc.gov/niosh/97-141pd.html
Blekesaune, M., & Solem, P. E. (2005). Working conditions and early retirement: A prospective study of retirement behavior. Research on Aging, 27, 3–30.
Bøggild, H., Burr, H., Tüchsen, F., & Jeppesen, H. J. (2001). Work environment of Danish shift and day workers. Scandinavian Journal of Work, Environment & Health, 27, 97–105.
Bonde, J. P. E. (2008). Psychosocial factors at work and risk of depression: A systematic review of the epidemiological evidence. Occupational and Environmental Medicine, 65, 438–445.
Cartwright, S., & Cooper, C. L. (Eds.). (2009). The Oxford handbook of organizational well-being. Oxford, England: Oxford University Press.
Chandola, T., Brunner, E., & Marmot, M. (2006). Chronic stress at work and the metabolic syndrome: Prospective study. BMJ, 332, 521–525.
De Bacquer, D., van Risseghem, M., Clays, E., Kittel, F., De Backer, G., & Braeckman, L. (2009). Rotating shift work and the metabolic syndrome: A prospective study. International Journal of Epidemiology, 38, 848–854.
Dembe, A., Erickson, J. B., Delbos, R. G., & Banks, S. M. (2006). Nonstandard shift schedules and the risk of job-related injuries. Scandinavian Journal of Work, Environment & Health, 32, 232–240.
D’Errico, A., Punnett, L., Cifuentes, M., Boyer, J., Tessler, J., Gore, R., et al. (2007). Hospital injury rates in relation to socioeconomic status and working conditions. Occupational and Environmental Medicine, 64, 325–333. doi:10.1136/oem.2006.027839.
Devereux, J. J., Vlachonikolis, I. G., & Buckle, P. W. (2002). Epidemiological study to investigate potential interaction between physical and psychosocial factors at work that may increase the risk of symptoms of musculoskeletal disorder of the neck and upper limb. Occupational and Environmental Medicine, 59, 269–277.
Dragano, N. (2007). Arbeit, Stress und krankheitsbedingte Frührenten: Zusammenhänge aus theoretischer und empirischer Sicht. Wiesbaden, Germany: VS Verlag.
Dragano, N., Siegrist, J., & Wahrendorf, M. (2011). Welfare regimes, labour policies and unhealthy psychosocial working conditions: A comparative study with 9917 older employees from 12 European countries. Journal of Epidemiology & Community Health, 65, 793–799. doi:10.1136/jech.2009.098541.
Eller, N. H., Netterstrøm, B., Gyntelberg, F., Kristensen, T. S., Nielsen, F., Steptoe, A., et al. (2009). Work-related psychosocial factors and the development of ischemic heart disease: A systematic review. Cardiology in Review, 17, 83–97.
Elovainio, M., Kivimäki, M., & Vahtera, J. (2002). Organizational justice: Evidence of a new psychosocial predictor of health. American Journal of Public Health, 92, 105–108.
Eurostat. European Commission. (2010). Europe in figures: Eurostat yearbook. Luxembourg, Luxembourg: Publications Office of the European Union.
Greenberg, J. (2010). Organizational injustice as an occupational health risk. The Academy of Management Annals, 4, 205–243.
Härmä, M. (2006). Workhours in relation to work stress, recovery and health. Scandinavian Journal of Work, Environment & Health, 32, 502–514.
Harter Griep, R., Rotenberg, L., Chor, D., Toivanen, S., & Landsbergis, P. (2010). Beyond simple approaches to studying the associations between work characteristics and absenteeism: Combining the DCS and ERI models. Work & Stress, 24, 179–195.
Johnson, J. V. (2009). The growing imbalance: Class, work, and health in an era of increasing inequality. In P. L. Schnall, M. Dobson, & E. Rosskam (Eds.), Unhealthy work: Causes, consequences, cures (pp. 37–59). Amityville, NY: Baywood.
Johnson, J. V., & Hall, E. M. (1988). Job strain, workplace social support and cardiovascular disease: A cross sectional study of a random sample of the Swedish working population. American Journal of Public Health, 78, 1336–1342.
Karasek, R. A., & Theorell, T. (1990). Healthy work. New York: Basic Books.
Kawakami, N., Araki, S., Takatsuka, N., Shimizu, H., & Ishibashi, H. (1999). Overtime, psychosocial working conditions, and occurrence of non- insulin dependent diabetes mellitus in Japanese men. Journal of Epidemiology & Community Health, 53, 359–363.
Kivimäki, M., Batty, G. D., Hamer, M., Ferrie, J. E., Vahtera, J., Virtanen, M., et al. (2011). Using additional information on working hours to predict coronary heart disease: A cohort study. Annals of Internal Medicine, 154, 457–463.
Kivimäki, M., Virtanen, M., Elovainio, M., Kouvonen, A., Väänänen, A., & Vahtera, J. (2006). Work stress in the etiology of coronary heart disease – a meta-analysis. Scandinavian Journal of Work, Environment & Health, 32, 431–442.
Krause, N., Brand, R. J., Kauhanen, J., Kaplan, G. A., Syme, S. L., Wong, C. C., et al. (2009). Work time and 11-year progression of carotid atherosclerosis in middle-aged Finnish men. Preventing Chronic Disease, 6, 1–20.
Kumari, M., Head, J., & Marmot, M. (2004). Prospective study of social and other risk factors for incidence of type II diabetes in the Whitehall II Study. Archives of Internal Medicine, 164, 1873–1880.
Landsbergis, P. A. (2003). The changing organization of work and the safety and health of working people: a commentary. Journal of Occupational and Environmental Medicine, 45, 61–72.
Leka, S., & Jain, A. (2010). Health impact of psychosocial hazards at work: An overview. Geneva, Switzerland: World Health Organization.
Marmot, M. (2004). Status syndrome. London: Bloomsbury.
Marmot, M. G., Bosma, H., Hemingway, H., Brunner, E., & Stansfeld, S. (1997). Contribution of job control and other risk factors to social variations in coronary heart disease incidence. The Lancet, 350, 235–239.
Nieuwenhuijsen, K., Bruinvels, D., & Frings-Dresen, M. (2010). Psychosocial work environment and stress-related disorders: A systematic review. Occupational Medicine, 60, 277–286.
Olsen, O., & Kristensen, T. S. (1991). Impact of work environment on cardiovascular diseases in Denmark. Journal of Epidemiology and Community Health, 45, 4–10.
Parent-Thirion, A., Macias, E. F., Hurley, J., & Vermeylen, G. (2007). European foundation for the improvement of living and working conditions: Fourth European working conditions survey. Luxemburg, Luxembourg: Office for Official Publications of the European Communities.
Peter, R., Alfredsson, L., Knutsson, A., Siegrist, J., & Westerholm, P. (1999). Does a stressful psychosocial work environment mediate the effects of shift work on cardiovascular risk factors in men? Scandinavian Journal of Work, Environment & Health, 25, 376–381.
Rantanen, J. (2010). Occupational health service systems in the south-eastern European subregion. Copenhagen, Denmark: WHO Regional Office for Europe.
Rugulies, R., & Krause, N. (2008). Effort-reward imbalance and incidence of low back and neck injuries in San Francisco transit operators. Occupational and Environmental Medicine, 65, 525–533.
Schnall, P., Dobson, M., & Rosskam, E. (Eds.). (2009). Unhealthy work: Causes, consequences, cures. New York: Baywood.
Schnall, P., Belkić, K., Landsbergis, P., & Baker, D. (2000). The workplace and cardiovascular disease. Occupational Medicine, 15, 1–6.
Siegrist, J. (1996). Adverse health effects of high-effort/low-reward conditions. Journal of Occupational Health Psychology, 1, 27–41.
Siegrist, J., & Rödel, A. (2006). Work stress and health risk behavior. Scandinavian Journal of Work, Environment & Health, 32, 473–481.
Siegrist, J., Rosskam, E., & Leka, S. (Eds.). (2011). Review of social determinants of health and the health divide in the WHO European Region: Employment and working conditions including occupation, unemployment and migrant workers. Unpublished report. Copenhagen, Denmark: World Health Organization.
Siegrist, J., & Theorell, T. (2006). Socio-economic position and health: The role of work and employment. In J. Siegrist & M. Marmot (Eds.), Social inequalities in health: New evidence and policy implications (pp. 73–100). Oxford, Englad: Oxford University Press.
Siegrist, J., & Wahrendorf, M. (2011). Quality of work, health and early retirement: European comparisons. In A. Börsch-Supan, M. Brandt, K. Hank, & M. Schröder (Eds.), The individual and the welfare state: Life histories in Europe (pp. 169–177). Heidelberg, Germany: Springer.
Stansfeld, S. A., Bosma, H., Hemingway, H., & Marmot, M. G. (1998). Psychosocial work characteristics and social support as predictors of SF-36 functioning: The Whitehall II Study. Psychosomatic Medicine, 60, 247–255.
Stansfeld, S., & Candy, B. (2006). Psychosocial work environment and mental health: A meta-analytic review. Scandinavian Journal of Work, Environment & Health, 32, 443–462.
Steenland, K. (2000). Shift work, long hours, and cardiovascular disease: A review. Occupational Medicine, 15, 7–17.
Stuckler, D., Basu, S., Suhrcke, M., Coutts, A., & McKee, M. (2009). The public health effect of economic crises and alternative policy responses in Europe: An empirical analysis. The Lancet, 374, 315–323.
Swerdlow, A. (2003). Shift work and breast cancer: A critical review of the epidemiological evidence. Research Report 132, Prepared by The Institute of Cancer Research for the Health and Safety Executive. London: Health and Safety Executive. Retrieved from http://www.hse.gov.uk/research/rrpdf/rr132.pdf
Tsutsumi, A., & Kawakami, N. (2004). A review of empirical studies on the model of effort-reward imbalance at work: Reducing occupational stress by implementing a new theory. Social Science & Medicine, 59, 2335–2359.
Van der Hulst, M. (2003). Long work hours and health. Scandinavian Journal of Work, Environment & Health, 29, 171–188.
Verma, D. K., Purdham, J. T., & Roels, H. A. (2002). Translating evidence about occupational conditions into strategies for prevention. Occupational and Environmental Medicine, 59, 205–214.
Wege, N., Dragano, N., Erbel, R., Jockel, K. H., Moebus, S., Stang, A., et al. (2008). When does work stress hurt? Testing the interaction with socioeconomic position in the Heinz Nixdorf Recall Study. Journal of Epidemiology & Community Health, 62, 338–341.
Xu, W., Zhao, Y., Guo, L., Guo, Y., & Gao, W. (2009). Job stress and coronary heart disease: A case–control study using a Chinese population. Journal of Occupational Health, 51, 107–113.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Siegrist, J. (2014). Social Inequalities in Work and Health in a Globalized Economy. In: Bridging Occupational, Organizational and Public Health. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-5640-3_2
Download citation
DOI: https://doi.org/10.1007/978-94-007-5640-3_2
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-5639-7
Online ISBN: 978-94-007-5640-3
eBook Packages: MedicineMedicine (R0)