Abstract
The impact of pollen on human health is primarily evident in allergic diseases. Sensitized patients can respond to pollen by symptoms of nose, eyes and bronchi. Pollen threshold levels for sensitization are unknown; instead most studies focus on the prevalence of sensitization for different pollen species. The pollen thresholds for symptom development vary among the different studies. Factors that influence the threshold level of a pollen species for symptom development are discussed. (i) Differences in response are observed among individual patients, but also among (ii) ethnic populations, (iii) changes in response to pollen concentrations during the pollen season occur, (iv) the amount of allergens carried by the pollen grains can differ in per region, from day to day and from year to year, and finally (v) threshold levels are affected by environmental factors, like weather conditions (temperature, pressure and storms), and air pollutants.The diversity of factors that influence the health impact of pollen has hampered the definition of a straight forward relationship between pollen and the severity of symptoms. However, within the public, the policymakers and the pharmaceutical industry there is a need for a definition of threshold pollen levels. A first approach to meet this need could be to define preliminary threshold values for different regions, followed by a validation of these preliminary threshold levels with patient symptom scores that can be collected by using new information and communication technology (ICT).
Finally, the possible role of pollen in non allergic diseases is discussed, especially non-allergic respiratory diseases, cardio- and cerebrovascular diseases, and psychiatric diseases, including suicide and suicide attempt.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
6.1 Introduction
Charles Blackley (1820–1900) was the first to demonstrate that pollen has an impact on human health. He performed the first pollen provocation tests on himself by applying several pollen types to the nostrils, the conjunctiva, the tongue and lips, by inhaling it and by inoculating the upper and lower limbs. Furthermore, he demonstrated that the amount of pollen in the atmosphere was correlated with the severity of his own symptoms (Waite 1995). Nowadays, we know that proteins carried by pollen (allergens) can evoke specific responses in the immune system. First of all, individuals can get sensitized to the allergens (sensitization) and subsequently these IgE-sensitized individuals can respond to the allergens with allergic symptoms. These can consist of nasal symptoms, eye symptoms, or bronchial reactions, or a combination of these. The level of allergen exposure can vary for instance, with the location, the weather or the time of year and it is a relevant determinant for both sensitization and symptom development. This paper focuses on the threshold values of allergen required for sensitization or for the development of symptoms, and on the various factors that can influence these threshold values. Furthermore, allergenic pollen not only appeared to interact with the human immune system to elicit an allergic response in sensitized individuals but it has other effects as well. This is described in the last part of this chapter which focuses on the effect of pollen on non-allergic diseases (Traidl-Hoffmann et al. 2003).
6.1.1 Threshold Values for Sensitization
To our knowledge, studies on threshold values for sensitization are not available and instead of threshold values this paper focuses on the prevalence of sensitization in different areas, which is indicative of the sensitization rate. Prevalence of sensitization is determined by both host genetic factors as well as by environmental factors, like temperature, atmospheric pressure, storms or air-pollution. Environmental factors that are associated with asthma, rhinoconjunctivitis and eczema have been recently discussed by Asher et al. (2010). The effect of pollen exposure on the prevalence of sensitization in a population is not clear: two regional scale studies showed a positive correlation between the pollen exposure and the prevalence of sensitization (Frei and Gassner 2008; Charpin et al. 1993), while a world wide study involving children showed a weak inverse relation, suggesting high exposure to pollen in early life may give some protection against the risk of acquiring respiratory allergy (Burr et al. 2003). Sensitization against inhalant allergens is identified either by a skin prick test or by determination of allergen-specific IgE in peripheral blood. However, a positive result of either of these tests indicates sensitization to a particular allergen, but does not fully correlate with the clinical relevance of this sensitization, i.e. symptom development upon exposure. False positive and false negative results can both occur. The characteristics of an allergen that distinguish it from other pollen components that do not result in sensitization, are incompletely understood (Radauer et al. 2008; Traidl-Hoffmann et al. 2009). Furthermore, pollen exposure is not the only environmental factor that determines sensitization. Other factors include air pollution (Riedl and Diaz-Sanchez 2005), and microbial exposures. Environmental pollution, such as diesel soot particles, can change the immune response in making non-reactive individuals react to an allergen (Diaz-Sanchez et al. 1999). Also non-protein substances derived from pollen for example the “pollen-associated lipid mediators” (PALMS) and adenosine influence the human immune system by making it more prone to trigger a Th2-sensitization response (Traidl-Hoffmann et al. 2005; Gilles et al. 2010). Thus there seems to be more than allergen alone in the sensitization process leading to a Th2-dominated allergy to pollen.
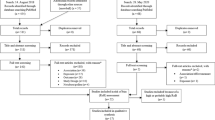
6.1.2 Threshold Levels for Symptom Development
The determination of allergen threshold levels for symptom development is hampered by many factors that influence the outcome. Sensitized patients differ in the extent of exposure to allergen required for symptom development. Furthermore, airborne allergen is thought to be present not only in intact pollen, but also in small respirable particles (Taylor et al. 2004; Spieksma et al. 1995a; Grote et al. 2003). However, whereas most of our knowledge on threshold values and symptom development is based on pollen counts in ambient air determined by a pollen sampler in a certain area, data from monitoring allergen in ambient air are still scarce (Buters et al. 2008). This chapter provides an overview of the current knowledge on pollen threshold values on symptom development and the various factors that influence these threshold values (Fig. 6.1).
6.2 Determination of Threshold Levels for Symptom Development
A large variety of studies has focused on the determination of pollen threshold levels that cause symptoms. Therapeutic intervention studies are especially useful. These deal with the determination of pollen (or allergen) thresholds that cause previously defined symptoms (e.g. “at least five sneezes and/or a symptom score of at least 2 on a scale from 0 to 3”). Although natural exposure to pollen under conditions of daily life is the most relevant, it has several disadvantages (see also Sect. 6.2.3, “Ambient Air Studies”). Therefore more controlled settings have been developed like provocation tests and exposure chambers. These study designs have their own advantages and disadvantages that will be discussed in the following section.
6.2.1 Provocation Tests
In an experimental challenge model the allergen is delivered onto the nasal mucosa by dripping, by paper disc, by pump sprays (Akerlund et al. 2005) or by eye drops on the eyes. In these studies the delivered dose is expressed in arbitrary units such as “Allergen Units” (Abelson et al. 1994), “standardized quantity units” (Korsgren et al. 2007) or “biologic units” (Bonini et al. 1990). These units were defined in most cases for standardization of allergen preparations, and their relation to pollen and/or allergen load is often unclear. Therefore, these studies will not give information on pollen thresholds, but they indicate the different threshold levels to which individual patients will respond. The patients are challenged with standardized increasing concentrations of the allergen until previously defined symptoms develop (Bonini et al. 1990; Abelson et al. 1994; Ahlholm et al. 1998; Ahlstrom-Emanuelsson et al. 2004; Ciprandi et al. 2009). The concentration at which these symptoms develop is the threshold concentration. A drawback of this approach is the repeated challenge of allergen to the nasal mucosa or the conjunctiva, which may prime these tissues and may cause a non-specific increase in the sensitivity and responsiveness (Connell 1968; Canonica and Compalati 2009). Furthermore, whereas these challenge studies will not reveal relevant information on pollen thresholds, they are perfectly suitable for (i) identification of the allergen to which a patient responds; (ii) examining the pathogenesis of allergic rhinitis or conjunctivitis; and (iii) assessing the response of individual patients to therapeutic intervention because of the standardized delivery of the allergen on the surface to be tested. These studies can show clearly that individual patients have different threshold levels for symptom development (Ciprandi et al. 2009).
6.2.2 Pollen Chambers
Special chambers have been developed for controlled human exposure to pollen. These chambers avoid the unpredictable levels of pollen and weather conditions during a study period. Different pollen chambers are developed, either hosting up to 14 persons (Horak et al. 2003), or 160 persons at the same time (Day and Briscoe 1999). The pollen chambers deliver a controlled pollen level over a period and allow assessment of the response throughout the study period. Pollen levels used in these chambers are usually quite high, e.g. 3,500 grains/m3 for ragweed (Day and Briscoe 1999), 4,000 pollen/m3 or 1,500 pollen/m3 for grass pollen (Day and Briscoe 1999; Horak et al. 2003; Krug et al. 2003), to ensure the desired effect of producing a full spectrum of symptom severity in allergic persons without affecting non-allergic participants.
Because of the requirement of high pollen concentrations, the pollen chambers have not yielded good studies on pollen thresholds for symptom development that are relevant in real life. In contrast, the chamber provocations have been very helpful assessing the effect of anti-allergic drugs (Day et al. 2000, 2009).
6.2.3 Ambient Air Studies
Exposure to natural pollen under “real life” conditions is the most relevant situation but also the most difficult to study, since the conditions are not well controlled and the exposure of patients to pollen will be variable due to the fact that they are outdoors during different times at different locations. A study design that tries to control these latter variables are the so-called “park studies” (Georgitis et al. 2000; Akerlund et al. 2005). In these studies, patients are allowed to sit, walk and recreate in a park on a day where at several locations pollen traps monitor the local pollen concentrations. This design has the advantage that parks can be found in almost any city (in contrast to pollen chambers) and patients are in close vicinity to pollen traps during the study period so that exposure can be measured and they can be monitored regularly. The limitations of these park studies are that they are time-consuming to organize and they require effort and time from the patient. Therefore, these studies are often performed on 1 day with high pollen counts to ensure symptom development. For threshold studies the patients should be monitored on subsequent days during the season. Although such daily studies in a park would be valuable for threshold studies, to our knowledge they have never been used for this purpose.
Another method of studying symptoms under natural conditions is to ask patients during their daily life to fill in a record of their symptoms (diary studies). Studies with this kind of approach assess the most relevant situation for the patients, i.e. daily life. However, since there is no general consensus on the method to determine the threshold level under these “real life” conditions, the designs of these studies differ. Furthermore, the “freedom of the patient” leads to variable pollen exposures among individual patients. These aspects are relevant in the interpretation of the results. The local pollen concentration at the patient location is variable and unknown. Often, pollen is monitored by a pollen sampler placed on a central roof top location to give a representative sample of regionally distributed pollen. The results are used as an average estimate of the concentration during the past 24 h in an area defined by a certain vegetation, climate regime and land use. If pollen traps were situated at ground level, the result would be affected by an overrepresentation of pollen produced by sources in the immediate vicinity of the trap. Although the results have been shown to correlate with symptom scores, medication use, and consultations for rhinoconjunctivitis and asthma in several studies, they are not equal to the pollen concentration that individual patients experience during their activities in the street. The difference in the exposure between persons in different parts of a city will vary among pollen types, and is probably more significant for pollen released at low height than for example birch pollen in Scandinavia which is produced in large amounts at tree-top level.
Bi-hourly pollen counts are also possible. These counts reflect the time that the pollen grains arrive at the trap, not the time at which the pollen grains are emitted. Furthermore, these counts will still not give us the pollen levels that the patients encounter. Therefore personal sampling of the environment of the patient is required. Several methods can be used to study the personal exposure to aeroallergens, like battery-operated personal samplers (Fiorina et al. 1997; Mitakakis et al. 2000; Okuda et al. 2005), nasal air samplers (Mitakakis et al. 2000), pollen trapped in nose (Okuda et al. 2005) and hair (Wiltshire 2006). However, to our knowledge none of these methods have been used for threshold studies. The time that the patient is outside and thus exposed to pollen is dependent on the patient’s activities schedule and therefore variable. Furthermore, the activity pattern during the exposed time period will be variable and this will result in a different exposure to pollen (Mitakakis et al. 2000); e.g. a jogger will breathe in more pollen-loaded air than a sun-bather. The size of the group of patients differs between studies and also the criterion of “symptom development” at which the threshold pollen concentration should be determined diverges between different studies. For instance, in one study the pollen threshold level is defined as the pollen count at which 90% of all patients experience their first symptoms (Viander and Koivikko 1978), while another study uses the pollen concentration at which, on a scale from 0 to 3, the mean symptoms score of the whole population exceeds 1 (Florido et al. 1999). Standardization of the method to determine pollen threshold levels (size of the group of patients and of criteria for threshold pollen concentrations) will be necessary for a good evaluation of the threshold concentration in different regions and among different populations.
6.2.4 Clinical Network
In France the assessment of threshold levels for symptom development is not only based on pollen counts but also on the information obtained from a network of allergists. More than 100 allergists from several areas in France provide weekly information on the number of pollinosis patients, the symptom-type, and the severity of the symptoms (Thibaudon et al. 2008). With these clinical data it was possible to draw three areas in France with different threshold levels for the various pollen types (see also Table 6.1). Furthermore, these clinical data have proven to be a tool to study the change in health impact from pollen during a season and to monitor the change in health impact from year to year.
6.3 Allergenic Pollen Species and Their Threshold Values
In the past decades several studies have been published on threshold levels of different pollen types. Studies on the most relevant pollen types in Europe and the Mediterranean countries are discussed in this section.
In aerobiological studies, pollen of species belonging to the same genus or of genera belonging to the same family usually cannot be distinguished under the light microscope as they share the same characteristics (they are stenopalynous). For this reason the different allergenic pollen or spore expositions refer to airborne pollen that represent a family (e.g. Poaceae), a genus (e.g. Plantago), and rarely a single species (e.g. Olea europaea).
Furthermore it is important to note that when we try to define the pollen risk threshold, the definition depends on the methodology used for pollen monitoring, i.e. the sampler type or the sampler height position. For instance, most threshold studies in ambient air determine pollen levels using a pollen sampler on a roof top, usually at a different height from personal exposure. This is one of the reasons why threshold values differ among the different studies (Table 6.1). Greater differences can be observed when comparing both daily and intradiurnal pollen content in the air at human height or roof top height, showing higher or lower differences depending on pollen size, meteorological conditions and atmospheric stability during the sampling period (Rantio-Lehtimäki et al. 1991; Galán et al. 1995; Alcázar et al. 1998, 1999a, b). The various pollen types will be discussed in alphabetical order and studies on the threshold values and the prevalence are summarized in Tables 6.1 and 6.2, respectively.
6.3.1 Alnus, Betulaceae Family
Alder is a rather common tree in all temperate climatic regions, mainly restricted to wet soil conditions. Predominant species of the genus are black alder (A. glutinosa) and grey alder (A. incana). The flowering period occurs from winter to early spring, depending on the climatic characteristic of the region. Patients sensitive to alder pollen may exhibit reactions towards other pollen of the Fagales order, although the cross reactions appear to be strongest among the species belonging to the same family e.g. within the family of Betulaceae, e.g. alder/birch. The major allergen of alder Aln g 1 is closely related to the major allergens of birch (Bet v 1), hazel (Cor a 1), hornbeam (Car b 1) and oak (Que a 1) (Matthiessen et al. 1991). The alder pollen season precedes the season of birch pollen and may act as a primer making patients more sensitive to birch pollen (Emberlin et al. 2007).
6.3.2 Ambrosia, Asteraceae (Compositae) Family
Although this genus comprises up to 45 species worldwide, the species that is spreading in Europe and Eastern North-America is essentially Ambrosia artemisiifolia or common ragweed. Ragweed established itself in Europe at the beginning of the twentieth century, resulting in highly infested areas like the Balkan area, the Rhône valley in France and Northern Italy. In areas heavily infested with these plants ragweed pollen is considered as the major pollen allergen (e.g. Vitányi et al. 2003).
Ragweed pollen is often nearly the only pollen type in the air except for a very short period in the beginning of the flowering season when mugwort pollen (Artemisia vulgaris) is also airborne. Although the allergens present in mugwort and ragweed pollen show cross reactivity (Hirschwehr et al. 1998; Asero et al. 2006), this does not interfere with the diagnosis for ragweed pollinosis, since the flowering season of these two species only partly overlaps. If sufferers keep a daily symptom diary it is easy to know if symptoms correlate with the presence of either ragweed or mugwort pollen in the air.
European studies on the ragweed pollen threshold for symptom development are rare. This is most likely to be due to the fact that ragweed is an invasive weed that was not known in Europe two centuries ago and was introduced from the new World. Its spread is now intensive due to several factors such as (i) changes in lifestyle and land use, (ii) increases in suburbs resulting in the decrease of arable lands (iii) some bylaws of Common Agricultural Policy established in 1993–1994 (Déchamp et al. 2001) and recently (iv) possible effects of climate change.
A relevant paper on ragweed thresholds comes from Quebec, in the Eastern part of Canada (Comtois and Gagnon 1988). This study, which was conducted over two pollen seasons showed that symptoms appear at 1–3 pollen/m3 of air. In France, many ragweed pollen allergic patients ask for treatment when the first pollen grains appear in the pollen monitoring trap (Déchamp et al. 1995).
Ragweed pollen is prevalent between 42° and 50° Northern latitude and rare in most countries around the Mediterranean coast and Portugal. Recent studies on the prevalence of ragweed sensitization in Europe show an increasing trend (Burbach et al. 2009). In contrast to other pollen types, ragweed pollinosis tends to be more prevalent in suburbs than in towns (Harf and Déchamp 2001).
6.3.3 Artemisia, Asteraceae (Compositae) Family
Mugwort is an unsuspicious weed, which looks very similar to Ambrosia. The major allergen of the mugwort pollen, Art v 1, is homologous to Amb a 4 of Ambrosia pollen and may cause cross reactivity in patients (Wopfner et al. 2005).
The weed is spread all over Europe. The most common species in Europe is A. vulgaris and it flowers in late summer (at the end of July, August and September). Two species which are common in Southern Europe A. annua and A. verlotorum flower even later (late summer to autumn). For this pollen type it was shown that street level counts are usually higher than the counts from rooftop samplers (Rantio-Lehtimäki et al. 1991). This may also hold for other pollen types due to the fact that these pollen grains are released during the early morning, when there is hardly any convection or turbulence in the air, preventing them from being lifted up to rooftop levels.
6.3.4 Betula, Betulaceae Family
Birch is the major pollen allergen producing tree in Northern Europe. The flowering season varies depending on the area. In Western Europe flowering starts by the end of March while in Central and Eastern Europe pollen grains appear in the air from the beginning to mid-April. Northward flowering starts, depending on the latitude, from late April to late May. Towards the South the number of birch trees is reduced and in Spain they are found mostly in mountainous areas and in zones in the interior of the North of the Peninsula with maximum values being detected during February and March (Hernandez et al. 1998).
Some allergens of these pollen grains show cross reactivity with other species belonging to this family. For example, the major allergen of birch Bet v 1 and Bet v 2 share IgE epitopes with the allergens in hazel and alder (Niederberger et al. 1998). Due to this cross reactivity the sequential flowering of the Betulaceae species may cause a prolonged hay fever season for sensitive patients.
6.3.5 Castanea, Fagaceae Family
There are no threshold studies published for Castanea pollen. This may be due to the fact that chestnut allergy (a) is strongly associated with latex-fruit syndrome and some other fruits (Raulf-Heimsoth et al. 2007), (b) has cross-reactivity with many other tree species like birch, walnut or Quercus (Cosmes et al. 2005; Teuber et al. 2003), (c) scores very low in monosensitization in positive skin prick-tested patients to Castanea (Lee et al. 2005; Laurent et al. 1993). Flowers bloom in late spring.
6.3.6 Casuarina, Casuarinaceae Family
The genus Casuarina (Australian pine) comprises nearly 60 species mainly natives to Australia. Some species are represented in warm regions forming part of the green urban spaces. It is an anemophilous tree that flowers during autumn, from September to November depending on the climatic characteristic of the region. Casuarina pollen allergenicity has been cited by various researchers (i.e. Agashe et al. 1994; García et al. 1997), but there are no studies on the pollen threshold for sensitized patients. Trigo et al. (1999) describes the presence of this pollen type in Spain. Although in most locations the daily average concentration of Casuarina pollen did not exceed 5 pollen/m3 of air, in some locations in Andalusia Region and especially in Malaga (Sun Coast), 30 and 500 pollen/m3 of air were reached, respectively. For this reason it is important to consider this tree as responsible of autumnal allergies in the Mediterranean Region.
6.3.7 Corylus, Betulaceae Family
Hazel is widely distributed in Europe and it typically has a number of shoots or trunks branching out at ground level. Due to this growth habit, it has been referred to as a bush rather than a tree. Flowering occurs from winter to early spring, depending on the climatic characteristics of the region.
The major allergen of hazel pollen, Cor a 1, is cross reactive with Bet v 1. Mari et al. (2003) showed that exposure to a high amount of hazel pollen in an intensively cultivated hazel area north of Rome (Italy) seems to lead to an IgE sensitization to allergenic molecules that are present only in hazel or hazel-related pollen.
6.3.8 Cupressaceae Family
Cupressaceae are the most widely distributed conifer family with a global range of nearly all continents except for Antarctica. In Europe, trees of the genus Cupressus are spread widely over the East Mediterranean e.g. C. sempervirens (native) and C. arizonica (introduced). Many species or genera of this family (e.g. Cupressus, Juniperus, Thuya) release pollen almost all year round and their pollen cannot be distinguished morphologically from each other. Daily concentrations can reach record peaks in the Mediterranean region during winter or early spring (Hidalgo et al. 2003; Charpin et al. 2005; Perez-Badia et al. 2010) although the pollen production shows a large variation from year to year. A gradual increase in the annual amounts of Cupressaceae pollen in the Mediterranean was observed since the 1980s, which in some cases was attributed to the increased planting of these trees (Calleja and Farrera 2000; Damialis et al. 2007).
Since reliable extracts to test the sensitization to Cupressaceae allergy have only been available since the last decade, the epidemiology of this allergy is poorly understood (Charpin et al. 2005). In Europe, allergy to Cupressaceae pollen was considered a rarity until 1975. Since then, considerable increases in the number of cases has been observed in Spain, France, Italy and Israel (Guerra et al. 1996; Papa et al. 2001; Charpin et al. 2005). An Italian multicentre study showed that 14.7% of the Cupressaceae allergic patients were monosensitized and that their average age was higher than that of the polysensitized patients (Italian Association of Aerobiology 2002). This may suggest that at least in some of the Cupressaceae allergic patients the sensitization may be caused by a long lasting exposure to the pollen, without being a typical atopic patient (Charpin et al. 2005).
6.3.9 Fagus, Fagaceae Family
Fagus is a tree of temperate South-West and Central Europe, extending to South Sweden. No threshold values for Fagus (beech) pollen can be found in the literature. Also studies on prevalence rates are not very conclusive. In Germany, 12% of all hay fever patients react to it (Horak et al. 1979). Reactions against beech pollen allergen occurred in 87% of all persons allergic to birch pollen in a Swedish multicentre study (Eriksson et al. 1984). The rate was the same in all Sweden, even in parts of the country where Fagus does not occur. It was concluded that the reactions against Fagus allergens resulted from of primary sensitization to Betula pollen. According to Horak et al. (1979), approximately 50% of all beech pollen allergies are due to cross-reactions with pollen from other species of Fagales. In a study from Swiss and Austrian birch pollen allergic patients, sera exhibited similar IgE reactivity profiles to birch, beech and oak pollen extracts due to beech and oak allergens that cross-react with the birch pollen allergens Bet v 1, 2 and 4 (Egger et al. 2008). In Sweden, the correlation coefficient between reactions to birch and beech pollen was 0.75 (Eriksson et al. 1987). The beech-specific IgE-levels were 0.063 in patients from Basel and 0.081 in patients from Vienna, respectively, as compared to 0.481 and 0.668 for birch (Egger et al. 2008). Beech is considered to be an early spring flowering tree.
6.3.10 Fraxinus, Oleaceae Family
In central Europe, Fraxinus pollen concentrations are considerably high. In Switzerland, for example, the concentrations are comparable with the amounts of birch pollen. Most of these pollen grains originate from Fraxinus excelsior, while other species with a more southern European distribution like Fraxinus ornus or Fraxinus angustifolia are represented with distinctly less pollen in the pollen traps (Guerra et al. 1996). Several studies show that ash pollen should be considered as a relevant allergen of spring pollinosis (Schmid-Grendelmeier et al. 1994; Hemmer et al. 2000). Sensitization to Fraxinus pollen is common in Switzerland and is also of clinical relevance as shown by nasal provocation tests (Schmid-Grendelmeier et al. 1994). The prevalence of Fraxinus sensitization in groups of pollen allergic patients varied from 17.6% in Vienna (Hemmer et al. 2000), 51.8% in Locarno and Lugano, Switzerland (Colombo 2010) to 56% in Zurich, Switzerland (Schmid-Grendelmeier et al. 1994).
The main ash allergen Fra e 1 is a homolog of Ole e 1, the highly allergenic olive pollen allergen. Fra e 1 has only a limited cross reactivity to birch pollen. Additionally this cross reactivity is confined to minor birch allergens (Wahl et al. 1996). Concerning thresholds for the development of symptoms, the study of Horak et al. (1979) gives a level of 167 pollen/m3. In this study patients’ symptoms were compared with the pollen measurements of the pollen trap in Vienna. The threshold is defined as the value for causing symptoms in the average patient. Thresholds for high pollen concentrations in Switzerland and Austria are 100 and 90 pollen/m3 respectively, but these values are not based on symptom studies. Fraxinus is considered to be a late winter or spring flowering tree, depending on the species and the geographical area.
6.3.11 Ligustrum, Oleaeceae Family
The genus Ligustrum (privet) comprises about 20 species, subspecies and varieties. They are frequently found in urban environments in the Mediterranean Region, both as ornamental trees or hedges in parks and gardens. Privet is considered to be an entomophilous plant with large and heavy pollen grains which are not well collected by samplers located on the building roof tops. However, Cariñanos et al. (2002) have observed higher pollen counts in samplers situated at human height, where this plant is observed frequently in the urban green space.
Being a member of the Oleaceae family, privet pollen carries a homologue of Ole e 1. Since the flowering period occurs at the end of spring, coinciding with the post-peak olive pollen curve, for people suffering from olive pollen allergy the period with symptoms can be extended. For this reason privet pollen should be considered as a potential causative agent of local allergy problems (Cariñanos et al. 2002).
6.3.12 Olea Europaea, Oleaeceae Family
Olive is a cultivated evergreen tree native to the Mediterranean region. It is an ambophilous species, i.e. pollinated by both insects and the wind. Due to the selection through time of varieties with high flower and pollen production, nowadays the anemophilous character is more pronounced. Although the olive tree showed an entomophilous character in origin, today it is considered to be an anemophilous species due to the selection through time of varieties with high flower and pollen production. Although Ole e 1 was the first major allergen described and characterized, it has been demonstrated since that there are at least, 20 proteins present with allergic activity. Ten of these have been characterized, cloned and expressed (Cárdaba et al. 2007) (see paragraph 6.4.2). This tree flowers during the spring so that the olive and grass pollen seasons usually coincide. Although many studies support the role of olive pollen as one of the main causes of allergic disease in the Mediterranean area, only a few studies cite a specific risk threshold for sensitized patients (Table 6.1). As it has been mentioned before, the methodology used for pollen monitoring is an important issue to take into consideration when trying to define the pollen risk threshold. In these two studies (Table 6.1) a Hirst designed spore trap, located on a roof top, was used in Spain, while a Rotorod sampler located at a height of 80 cm was used in Israel.
6.3.13 Parietaria, Urticaceae Family
Pellitory-of-the-wall (Parietaria) is a typical allergenic pollen producing plant in the Mediterranean area. Par j 1 and Par j 2 are the two major allergens, with similar IgE epitopes, in Parietaria judaica (Asturias et al. 2003). Parietaria belongs to the Urticaceae family together with Urtica (nettle) which is allergenically of little importance. The pollen of these two genera cannot be distinguished microscopically. Only the species Urtica membranaceae has a distinct pollen type, allowing the study of its individual pollen behaviour in the air (Galán et al. 2000). In the Mediterranean area the pollen season extends from spring to early summer and even autumn (Fotiou et al. 2011), depending on the species and the geographical area.
6.3.14 Plantago, Plantaginaceae Family
Plantain (Plantago) pollen is considered to be a minor cause of pollinosis in Europe (D’Amato et al. 1998). Mono allergy to plantain is unusual and often patients that are positive in a skin prick test for plantain pollen extract are also sensitized for grass pollen (Watson and Constable 1991; D’Amato et al. 1998). This is probably due to cross reactivity among these pollen species. Group 5 grass pollen allergen appeared to be responsible for most grass/plantain cross reactivity (Asero et al. 2000). The flowering season of plantain largely overlaps with the grass flowering period. Therefore the symptoms caused by Plantago cannot always be attributed to Plantago pollen.
6.3.15 Platanus, Platanaceae Family
Plane trees are widely grown as street and shade trees in European cities, especially in France, Spain, Italy and Greece. London Plane tree (P. acerifolia or P. hybrida) is the most common cultivated species. A high prevalence of positive skin prick tests has been recorded for Platanus hybrida in Madrid (Varela et al. 1997). In Córdoba (South Spain) 17% of the population is sensitive to Platanus pollen and patients presented symptoms almost immediately after the Platanus pollen season started, as this pollen type appears abruptly in high concentrations in the air. Patients suffer from symptoms at pollen concentrations of 51–200 pollen/m3 during less than a month (Alcázar et al. 2004). Platanus pollen is produced at high levels in the southern European countries, where it is a relevant allergenic pollen species. Plane trees flower during early spring.
6.3.16 Poaceae Family
Poaceae, grasses, comprise a high number of species flowering from winter to the end of summer, depending on the species and on the geographical area. Although knowledge about the differences in the allergenic potency of the various species is scarce, most species are considered to be allergenic. A recent study showed that within the Pooidae subfamily 12 grass species which are common in the temperate and subtropical zones appeared to share similar IgE determinants (Andersson and Lidholm 2003). Threshold studies discussed here deal with the mixture of grass pollen that is produced in the particular area under study. Most threshold studies in ambient air determine pollen levels using a pollen sampler on a roof top, except for a study from Israel, but the criteria at which the threshold levels are determined differ among the different studies (Table 6.1). Recent European studies show that the prevalence of sensitization to grass pollen is significantly higher than that to other pollen species (Bauchau and Durham 2004; Bousquet et al. 2007) except for ragweed pollen in highly infested regions (Vitányi et al. 2003). The prevalence of grass pollen allergy differs among different European countries and among different studies (Table 6.2) and appears to be inversely associated with pollen exposure (Burr et al. 2003). This inverse association is very weak, but this study cautions us to conclude that high exposure to pollen increases the risk of rhinoconjunctivitis or/and asthma.
6.3.17 Rumex, Polygonaceae Family
Sorrel flowers from late May until August, which largely overlaps with the flowering seasons of Plantago and grass pollen. The clinical relevance of sorrel pollen cannot easily be defined. Allergy to sorrel may be overlooked, because it is not thought of during the grass pollen season. From a group of 96 grass pollen allergic patients in Austria, 70% of randomly selected sera tested positively for sorrel specific IgE. Relevant cross-reactivity between grass and sorrel pollen was excluded (Frank et al. 1991).
6.3.18 Salix, Salicaceae Family
Salix species (willow, sallow) are both insect- and wind pollinated, but the proportions of the two pollination modes differ between species. Pollen grains often tend to stick together (Dobson 1988; Karrenberg et al. 2002) and regional levels of airborne pollen are often low (Jones and Harrison 2004; Zeghnoun et al. 2005). No published threshold values of Salix are available from Europe and a Canadian study showed that the impact of an interquartile increase in daily Salix pollen levels upon asthma admissions was insignificant (Dales et al. 2008). The prevalence of Salix sensitization has been addressed in a Swedish multi-centre study (Eriksson et al. 1984). Positive skin prick reactions against Salix allergens occurred in 37% of people with birch pollen allergy, but they were strong (>2+) in only 12%. In patients reacting to other pollen types, only 6% showed mild positive results in prick tests (SPT = 1+), and no one had a stronger reaction. Positive IgE tests against Salix allergens were found in 40% of the birch pollen sensitive people, but only 6% reacted with RAST class > 2. In Eskisehir, Turkey, 24.9% of the hay fever patients reacted to Salix pollen. Of these, the allergy was considered severe in 16.9% (Egger et al. 2008).
6.3.19 Spore Types: Alternaria and Cladosporium
Epidemiological studies on mould allergy in Europe show that Alternaria and Cladosporium are the most important sources of fungal allergens; Cladosporium seems to be most prevalent in Northern Europe and Alternaria, especially in children, is most common in Southern Europe (D’Amato et al. 1997). A multicenter study in Europe showed that the prevalence of positive skin prick tests to these moulds varies from 3% in Portugal to 20% in Spain (D’Amato et al. 1997). Studies on the threshold level that induces symptoms are scarce for these spores. A study from 1979 mentions 100 spores/m3 for Alternaria and 3,000 spores/m3 for Cladosporium (Gravesen 1979) but no details on the determination are given.
In Europe, the main season for the occurrence of Alternaria spores is from June until October (Kasprzyk 2008), thus overlapping with the grass pollen season. The variation in annual totals is large, for instance concentrations from 10,000 to 25,000 spores/m3/year have been described (Thibaudon and Lachasse 2006).
6.4 Factors Affecting the Threshold
6.4.1 Differences Among Individuals
6.4.1.1 Nonspecific and Allergen-Specific Hyperreactivity as Basis for Symptoms
The physiological background for symptom development in allergic individuals is the increased sensitivity of their mucosa after allergen exposure. This may result in an hyperreactivity (or hyperresponsiveness) of the mucosa of eyes, nose or bronchi. There are two types of hyperreactivity (or hyperresponsiveness) of the mucosa in eyes, noses, and bronchi which determine the severity of the clinical response (symptoms) in pollen allergic individuals following exposure to pollen allergens: the non-specific and the allergen-specific hyperreactivity. Since there are more data on the hyperreactivity of the airways than for nose and eyes, this part will focus primarily on bronchial hyperresponsiveness.
Airway or bronchial hyperresponsiveness (BHR) is defined as excessive bronchial narrowing and manifests itself as an exaggerated bronchoconstrictor response of the airways to various inhaled stimuli, including pollen (Sterk et al. 1993). BHR is determined at least in part by airway inflammation and airway structural remodeling (Busse 2010). The severity of BHR in non-asthmatic patients changes with pollen-induced rhinitis during the season and evidence suggests that during the pollen season, and even after the cessation of exposure to pollen, BHR is increased for weeks (Prieto et al. 1994).
The severity of allergic BHR is often measured as the provocative dose or concentration causing a 20% fall in the FEV1 (=forced expiratory volume in 1 s) (Sterk et al. 1993). Non-specific BHR can be measured by using non-specific bronchoconstrictor stimuli such as histamine and methacholine that are well standardized and frequently used in clinical settings. Methacholine and histamine act directly on smooth muscle, while other stimuli can act indirectly by stimulating the release of inflammatory mediators and/or by stimulating neural pathways (Sterk et al. 1993).
6.4.1.2 Factors Influencing Hyperreactivity and Threshold
It is a well-known fact that the same amount of pollen does not cause the same intensity of complaints among individual patients with hay fever. Different factors or exposures have been implicated in temporary changes in nasal and airway reactivity. BHR may be variable over time because of several reasons.
6.4.1.3 Atopy
The most important and independent risk factors for BHR are lung function and atopy. Lower FEV1, a lower Tiffeneau ratio (FEV1 as a percentage of FVC), and the presence of atopy are associated with an increased occurrence of BHR (Britton et al. 1994).
The association between atopy and BHR is complex. Both skin prick test positivity as well as serum IgE are positively associated with BHR (Peat et al. 1996; Sunyer et al. 1995). Also it has been shown that BHR is frequently present in subjects without asthma but with allergic rhinitis. Moreover, BHR worsens during the allergen season in subjects with rhinitis who are atopic to pollen (Riccioni et al. 2002).
6.4.1.4 Gender and Age
Several studies have shown a relationship between BHR and gender. In children without asthma, BHR is approximately twice as frequent in boys as in girls (Ernst et al. 2002). On the other hand, the occurrence of BHR is more frequent among female than among male adults (Britton et al. 1994). This switch in prevalence among males and females seems to occur during and/or after puberty. The relationship between BHR and age is unclear: BHR is either not influenced by age or subjects of older age have a lower risk for BHR after correction for lung function or those of older age are more likely to have increased BHR (Hopp et al. 1985).
6.4.1.5 Influence of Smoking
Although smoking has been significantly associated with BHR, cigarette smoking appears less important than atopic status after correction for other risk factors (Britton et al. 1994). Smoking may increase BHR in part by increasing inflammatory cell numbers in the airways (Amin et al. 2003).
6.4.1.6 Allergen Exposure
Experimental exposure to allergen is associated with an increase in BHR the following day (Sterk et al. 1993). Seasonal variations in the allergen load and air pollution are paralleled by fluctuations in BHR, with higher allergen exposure levels being associated with increased responsiveness (van der Heide et al. 1994).
In subjects with asthma, a worsening in indices of BHR has been observed after respiratory infections (Cheung et al. 1995).
6.4.1.7 Effects of Lifestyle
Pollen counts show the pollen concentrations in the outside environment. However, most people spend most of their time indoors. Farrera et al. (2002), using a Cour’s pollen trap inside and outside a house in the Rhône Valley (France), showed that 60% of the taxa found in the environment close to the house were also present inside the house during the same period. Ragweed pollen was the most prevalent species. It would be interesting to investigate the factors that are responsible for transfer the pollen grains inside the house.
Furthermore, the patient’s personal agenda is relevant for the exposure to pollen. A person can sit inside a house all day or cycle through meadows. Also the traveling history of a person is relevant for the specific exposure to pollen. This was nicely demonstrated by Penel et al. (2009) who collected the hairwashing of volunteers in Valence and subsequently identified the pollen in these washings. In a period without any Pinus pollen on the trap he found that 36% of the pollen from the hair washing was Pinus pollen. This person arrived from Spain where Pinus was flowering. This study showed that hair can function as a pollen trap that is indicative for the site of life for a person.
6.4.1.8 Effects of Viral and Bacterial Infections
Transmissible viral infections occurring in the general population are also an environmental factor which can potentially modify the allergic response and asthma attacks. Viral infections and immunodeficiency (e.g. HIV) might be problematic, for instance, in immunotherapy. Depending on the virus and the person’s state of health, various viruses can infect almost any type of body tissue, from the brain to the skin. Viral infections cannot be treated with antibiotics.
Busse (1989) summarizes the important role that viral illnesses could play in the allergic diathesis. Respiratory infections precipitate wheezing in many patients with asthma. A number of important conclusions in this relationship has come from detailed epidemiological studies. First, viral, not bacterial, respiratory infections provoke asthma in children and adults. Second, although many respiratory viruses trigger asthma, the prevalent organism responsible for increased wheezing varies with the age of the affected patient. For example, respiratory syncytial virus (RSV) infections predominate in infants and young children, whereas rhinovirus, influenza and para-influenza emerge with greater frequency as age increases. It is, however, unlikely that mechanisms of virus-induced wheezing are different for each respiratory virus. Rather, a common mode of asthma exacerbation should prove to be the rule. Third, the likelihood of increased wheezing with colds is greater when patients have severe symptoms such as malaises, fever, coryza, etc. Greiff et al. (2002) suggest that common colds in part through stimulation of granulocyte activity potentiate the airway inflammation in allergic diseases.
6.4.2 Differences Among Different Ethnic Populations
Different studies have shown that the pollen threshold levels for symptom development depend not only on allergy potency, but also on other environmental, genetic and socio-economic characteristics, e.g. ethnic population. This will be illustrated by studies on olive pollen, one of the main causes of allergic disease in the Mediterranean area. Olive allergy represents a unique allergy model where a sharp exposure gradient leads to different clinical allergy profiles (Barber et al. 2007). First of all, it is important to present the different proteins which have allergenic activity. Taking into account that major allergens are defined as those recognized by more than 50% of the patients allergic to a particular source (King et al. 1994), Ole e 1 was the first major allergen described and characterized (Blanca et al. 1983; Lauzurica et al. 1988a, b), being recognized by more than 70% of patients. Nowadays the presence of, at least, 20 proteins with allergenic activity has been demonstrated, and 10 of them have been characterized, cloned and expressed (Cárdaba et al. 2007), including Ole e 1 as the major allergen and other minor allergens (Lauzurica et al. 1988a, b; Villalba et al. 1994; Asturias et al. 1997; Ledesma et al. 1998; Barral et al. 2004, 2006). Recently, the 11th has been described (R. Rodriguez, personal communication).
In the case of olive pollen exposure, it has been demonstrated in several studies that high levels of pollen exposure can cause minor allergens to become major allergens for allergic patients that live in areas with high exposure to the respective pollen. For example, some minor allergens have been defined as major allergens, i.e. Ole e 4 and Ole e 7, by Rodríguez et al. (2001). Cárdaba et al. (2007) described a more complex IgE response to the various olive allergens in allergic patients from areas with extremely high pollen counts. They showed that not only Ole e 1 but also 2, 7 and 10 were major allergens in highly exposed populations, but not in populations with a lower antigenic exposure. On the other hand, Barber et al. (2007, 2008) defined next to Ole e 1, also Ole e 7 and Ole e 9 to be major allergens. Ole e 7 sensitization has been described with an average prevalence of about 47% in patients with olive allergy by Tejera et al. (1999). These authors show that high exposure to olive pollen can lead to different sensitization rates to this “minor allergen” Ole 7. In Jaen (South of Spain) up to 60% of the patients were sensitized to Ole 7, compared to less than 20% of the patients in the Madrid area (Central Spain) (Tejera et al. 1999).
Moreover, in a high olive pollen exposed area in the Andalusia Region, Spain (Jaen, Córdoba, Granada and Malaga provinces), it has been observed that 50% of the patients reacted only to Ole e 1, which is normal in areas with lower pollen counts. On the other hand, Ole e 9 sensitization always coincided with Ole e 1; however, Ole e 7 cases were Ole e 1 independent, 40% of Ole e 1-negative patients were sensitized to Ole e 7 (Barber et al. 2007, 2008). In this well exposed area of Andalusia it is important to consider not only Ole e 1, but also Ole e 9 and, particularly, Ole e 7. In other areas which are less exposed to olive pollen, Ole e 7 sensitization always coincided with Ole e 1. Clearly, new approaches to allergen standardization, diagnosis, and vaccination are necessary in different geographical areas.
Although it is generally believed that allergic sensitization to aeroallergens reflects the degree of exposure, and this also applies to pollen sensitivity, some studies show different results (Cárdaba et al. 2007). Geller-Bernstein et al. (1996) have observed different sensitization prevalences to olive pollen, in ethnically different populations of Israel. Geller-Bernstein et al. (2002) have observed very low prevalence of sensitization to olive pollen in the Druse Arab, (12%), Christian Arab (27%) and Muslim Arab (35%) populations, as compared to the Jewish population (66%). The Druse, the Christian and part of the Muslim Arabs have lived in the study region for several centuries. In this area, olive trees have been cultivated as a crop for centuries, so that the residents are massively exposed to olive pollen from birth. However their sensitization prevalence to olive pollen is lower than that of the Jewish population that has lived in the same region only for about 150 years. This interesting observation might indicate that a population exposed to a type of pollen (allergen) from birth onwards, for centuries, might lead to tolerance, rather than to sensitization – possibly another aspect of the “hygiene hypothesis” (Geller-Bernstein et al. 2002; Cárdaba et al. 2007).
Geller-Bernstein et al. (2002) compared the Israeli Druse population and the Andalusia population. Both populations are exposed to massive amounts of olive pollen in the air from birth. Such a continuous exposure has apparently lowered their possible sensitization to olive allergens. Finally, in studies comparing pollen thresholds for symptom development in different geographical areas, only a few papers focus on olive pollen, i.e. Jaen (Andalusia Region, Spain) (Florido et al. 1999) and Netzer Sireni (Coastal Plain of Israel, Israel) (Waisel et al. 2004). Florido et al. (1999) have published a pollen risk threshold of 400 olive pollen/m3 for Jaen patients, the province with the biggest number of olive groves in the world. However, lower pollen counts in the air (2–4 pollen/m3) seem to cause allergy among the Israeli population living in Netzer Sireni, with a smaller number of olive trees. The olive pollen threshold level for symptom development may differ in different geographical areas, depending upon amount of exposure and/or ethnic origins.
In general, different studies on migration offer information about the role of the environmental and genetic factors in the development of atopy and asthma under different scenarios (Hjern et al. 1999; Brabäck et al. 2004). These studies show that both the way of life and the environmental factors of industrialized countries play a role in the case of atopy and asthma. Furthermore, it appeared that in the beginning of respiratory allergies environmental factors play a more important role than genetic ones (Hjern et al. 2000; Rottem et al. 2005; Lombardi et al. 2008). The epidemiological information reveals that the prevalence of asthma and atopy depends on the age in which the migration occurs and is increased by the duration of the residence in the countries of destination.
All these studies demonstrate how difficult it is to define risk thresholds for sensitization to olive pollen in a particular geographical area.
6.4.3 Seasonal Variations in Threshold Level
Regarding the seasonal variations in threshold level, lower pre- and post-season exposure to relatively smaller pollen concentrations may cause allergic responses at a lower threshold. In the case of olive, Ole e 1 is also present in other trees belonging to the Oleaceae family, such as Fraxinus and Ligustrum. In the Andalusia region (Spain) different Fraxinus species flower at different periods of time. F. angustifolia, flowering in early spring, coincides with pre-season olive pollen exposure and F. ornus, flowering in late spring, coincides with high olive pollen exposure (Guerra et al. 1996). On the other hand, privet (Ligustrum) is an ornamental tree that flowers later, in June, coinciding with post-season olive exposure. This pollen appears in the air after the patients have been suffering from olive pollen allergy for a long time (Cariñanos et al. 2002). Privet pollen grains are very heavy and they are not transported easily by air. However, it has been demonstrated that people living near large areas with this ornamental tree suffer from allergy. For this reason, these homologous pollen types can be responsible in a percentage of olive allergic responses at the beginning and end of the olive pollen season.
It is also important to take into consideration pan-allergens (i.e. profilins, lipid-transfer, proteins, polcalcins, etc.) when trying to understand the seasonal variations in threshold levels (Barber et al. 2008; Quiralte et al. 2007). Homologous allergens in Oleaceae and non-Oleaceae species could account for cross-reactivity between different pollen (Quiralte et al. 2007). This is important especially in patients living in south Europe, where olive and grass pollen seasons usually coincide. Profilin sensitizations are mainly associated with grasses. Moreover other different allergenic pollen seasons usually overlap, i.e. Rumex, Plantago, Artemisia, Ambrosia or Amaranthaceae/Chenopodiaceae (nowadays both of them are included in the Amaranthaceae family) (Barber et al. 2008).
Another variation in symptom development during the season is observed in the grass pollen season in a Dutch grass pollen sensitive patient group. Patients seem to respond with more severe symptoms to the relatively low grass pollen concentrations in the early part of the season, while at the end of the season when the grass pollen concentrations were still relatively high, symptom scores were reduced (de Weger et al. 2008).
6.4.4 Pollen Allergens in the Air
Most pollen allergens in the air are carried by pollen grains, but the presence of airborne small respirable particles containing pollen allergens has also been reported (Spieksma et al. 1995a; Schäppi et al. 1997). The total amount of allergen in the air we breathe needs to be considered in the assessment of thresholds for symptom development.
6.4.4.1 Small Respirable Particles
Pollen is the carrier of the airborne allergens. Although the existence of non-pollen, small respirable particles that contain allergen is still debated, for birch for instance the only source of the main allergen Bet v 1 is the pollen. Even anatomically closely situated parts of the catkin to pollen, such as orbicules (anatomic part inside anthers to which developing pollen are attached) do not contain allergen Bet v 1 (Vinckier et al. 2006). At first this may seem surprising, but closer investigation showed that no Bet v 1 allergen is present in birch pollen until about 1 week before pollination (Buters et al. 2010). The Bet v 1 allergen was found only inside the pollen. Because orbicles were shown to be devoid of this allergen, there is apparently no transfer of Bet v 1 inside catkins, and separate parts of a birch tree including catkins must produce their own Bet v 1. So far Bet v1 has not been found in any plant parts studied (except one report on the presence of low levels of Bet v 1 in birch leaves) (Grote and Fromme 1986). Even if other parts of the tree such as leaves, bark or catkins contain some Bet v 1, they must become airborne which is unlikely. Thus, small respirable particles containing allergen must come from pollen from processes during or after pollen release, for example, rupture of pollen from birch (Schäppi et al. 1999b; Grote et al. 2003; Taylor et al. 2004; Namork et al. 2006) or grass (Rantio-Lehtimäki et al. 1994; Schumacher et al. 1988; Motta et al. 2006; Namork et al. 2006), or transfer of allergen after extraction by rain water to other environmental particles (Behrendt and Becker 2001). In Munich, Germany, during the last 5 years of continuous allergen monitoring in ambient air during the pollen season, Buters et al. (2010) did not find any birch allergen in the respirable fraction containing PM < 2.5 μm. The discrepancy between their results and other authors could be due either to specific climatic conditions not present in Munich, Germany, or to the difference between grass and birch pollen (Namork et al. 2006). Finding these small respirable particles is challenging as they occur in the same respirable fraction PM < 2.5 μm as diesel soot particles. Diesel soot adsorbs the allergen Bet v 1 and consequently no allergen can be detected anymore in the sampled fraction. It is also unclear if allergen-coated diesel particles release the allergen once inhaled, or if that the allergen is no longer bioavailable for interactions with the immune system (see Fig. 6.2).
Pollen releases several substances, such as lipid mediators (PALMS) and larger quantities of adenosine; factors which seem to influence the sensitization reaction of the immune system. Once sensitized, the allergen seems to govern the observed patient symptoms (environmental pollutants influence the extent of the immune reaction too (Lubitz et al. 2010), but these compounds do not originate from pollen). The discussion concerning the threshold value then becomes the question of whether pollen releases a constant amount of allergen. If the pollen were constant in allergen release, then the pollen count would be a good surrogate marker for allergen exposure and a pollen-symptom threshold could be determined. If pollen release a variable amount of allergen, then an allergen-symptom threshold is perhaps possible.
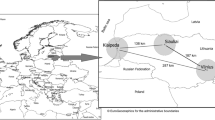
6.4.4.2 Regional Variation in Allergen Release
There are very few studies concerning the regional variability of allergen release from the same amount of pollen. Buters et al. (2008) showed that two regions in Germany, about 600 km apart, varied three-fold in allergen release from the same amount of pollen of the same species, and that this difference remained similar during the 3 years studied (see Fig. 6.3). Also, Ambrosia artimisiifolia plants exposed to higher CO2 values gave rise to higher pollen production but less allergen release per pollen (Ziska et al. 2003; Rogers et al. 2006). CO2 varies among regions, although the differences are small, except for inner cities (Ziska et al. 2003). Interestingly, more individuals living in inner cities with a higher environmental pollution are sensitized than city-inhabitants that live in less polluted areas (Morgenstern et al. 2008).
Differences in Bet v 1 release from the same amount of pollen collected directly from trees in Munich and Nordrheinwestphalia (NRW) and from different years. The figure shows the median and the 90 and 75% confidence interval (with permission from Buters and Behrendt (2008))
6.4.4.3 Day-to-Day Variability in Allergen Release
For birch, several authors monitored the allergen release from pollen collected from ambient air (see Fig. 6.4) (Buters et al. 2010).
(a) Daily variation in birch pollen allergen in different fractions of ambient air (-● - PM > 10 μm, - ▲ - 10 μm > PM > 2.5 μm: not shown 2.5 μm > PM > 0.12 μm, since all fractions resulted in baseline values) and pollen (grey bars) in ambient air from Munich, Germany in 2006. At the end of the birch pollen season pollen counts decline, but Bet v 1 does not. (b) Concomitant humidity (■) and temperature (▼) at the sampling site. Adapted from Buters et al. (2010).
After rainfall (recognized by a very high humidity) both pollen and the allergen are greatly reduced. In the 1990s Rantio-Lehtimäki in Finland (Pehkonen and Rantio-Lehtimaki 1994; Jensen et al. 1989) had shown that allergen and pollen flight were not congruent, suggesting that the release of allergen per pollen is not constant and varied per day. Schäppi and colleagues, first in Switzerland and later also in Australia, showed the same results (Schäppi et al. 1996, 1997, 1999a,b). Riediker et al. (2000) confirmed this finding but also cautioned that allergen present in other fractions of ambient air might be due to sampling artefacts. The same was described for olive pollen (De Linares et al. 2007) although surprisingly most olive allergen was detected in those fractions that do not contain pollen. For grass pollen the differences in release is to be expected as the pollen from different grass species cannot be discriminated in a Hirst-type pollen trap, as microscopically the main species of grass pollen (such as Lolium perenne, Dactylis glomerata or Phleum pratense) show the same morphology (Winkler et al. 2001).
The allergen release per fixed amount of grass pollen varied (Schumacher et al. 1988). In addition, it can be demonstrated that, Phl p 5 was only partly congruent to grass pollen counts over Europe (Buters et al. unpublished observation).
6.4.4.4 Year-to-Year Variability in Allergen Release
Currently, to our knowledge only one study has examined the effect of different seasons on the allergen release of birch pollen. The authors reported an up to five-fold difference in allergen release between the same amount of pollen sampled from the same trees in different years (Buters et al. 2008). Although day of sampling will influence the allergenicity of pollen due to the rapid increase of allergen just before pollination, the year-to-year differences remained between all years studied. Indeed, pollen sampled from ambient air from the same location varied up to ten-fold in allergen release potency between different years (Buters et al. 2010). Thus allergen release from the same amount of birch pollen is variable. Also, the high variability among individual birch trees was not constant between years, although a few trees constantly remained in the lower percentile (Buters et al. 2008) A Europe-wide project was initiated that studies these questions in detail for birch, grass and olive pollen (see www.hialine.com).
6.4.4.5 Allergen Release from Different Pollen Species
Differences in allergen release from the same amount of pollen was best studied for birch (see above) but was also reported for grass, olive and ragweed pollen (Namork et al. 2006; Buters et al. 2008, 2010). The phenomenon seems to be present in all the pollen species studied. This phenomenon is likely to be a general natural characteristic of plants since it has been known for a long time that the specific contents of certain ingredients vary also in non-allergenic species (Stahl and Jork 1964; Filipowicz et al. 2006). Pollen is thus no exception.
Although previous findings suggest that airborne allergen measurements correlate with pollen counts (Marsh et al. 1987; Spieksma et al. 1995a), the recent studies discussed above suggest that it is likely that pollen contain different amounts of allergen per pollen grain. The question remains, if the differences observed result in differences in patient symptoms. An additional advantage of allergen monitoring could be that automation and on-line monitoring of allergen is less complicated than pollen counting, as the current techniques have difficulties discriminating optically similar but allergenically different pollen species (Delaunay et al. 2007).
Pollen grains release more than allergen alone (Traidl-Hoffmann et al. 2005) and the allergens themselves are a mixture of several different proteins, each protein again consisting of a mix of different isoforms. Thus birch pollen releases a mixture consisting of at least PALMs, adenosine, Bet v 1, Bet v 2, and Bet v 4. Bet v 1 consists of 37 reported isoforms, of which 6 are commonly present in European samples.
The major isoform of Bet v 1 is Bet v 1.0101. About >90% of European sensitized individuals are sensitized to Bet v 1 (Moverare et al. 2002), and >50% of Bet v 1 is made up by the isoform Bet v 1.0101 (Swoboda et al. 1995). The other isoforms of Bet v 1 are close homologues of Bet v 1.0101 and birch pollen sensitized individuals react to all these isoforms equally, except for the hypoallergenic isoform Bet v 1.0401 (Bet v 1d), which is a minor isoform (Hartl et al. 1999). Patients sensitized to the minor allergen Bet v 2 or Bet v 4 are often simultaneously sensitized to Bet v 1 (Moverare et al. 2002).
The major allergen in grass pollen is Phl p 5. Phl p 1 is a major allergen too and often sensitization to both occurs simultaneously (Moverare et al. 2006). ELISA, the technique used to determine the allergen content of ambient air in all published studies, is mostly designed to recognize only one allergen, of which it then recognizes the isoform mix relevant for patients. For Bet v 1 the antibodies used in the ELISA recognized all isoforms (except the hypoallergenic Bet v 1.0104) of Bet v 1, and the ELISA used predicted patient reactivity. Therefore, this technique is suitable for determining allergen exposure.
6.4.4.6 Allergen Release from Other Plant Parts
Allergen specific IgE binding activity appeared to be present in other plant parts than pollen of e.g. ragweed (Agarwal et al. 1984) and birch (Fountain et al. 1992). It is not known whether leaves, stems, seeds and roots can release relevant amounts of allergens into the air under general conditions. However, release of allergens from other plant parts than pollen may be relevant during the annual campaigns to draw ragweed in the Rhône valley. During these campaigns which take place before the flowering season of ragweed, plants are being broken and snapped and during these actions some of the voluntary workers suffered from sudden attacks of asthma, conjunctivitis and/or urticaria (C. Déchamp, personal communication).
6.4.5 Environmental Aspects
6.4.5.1 Temperature and CO2
Temperature is the primary determinant of the metabolic rate of plants, and therefore it is an important determinant of phenology including that of allergenic plants (Linderholm 2006). Higher CO2 concentrations stimulate photosynthesis in many plants especially when enough nutrients such as nitrogen are available (Bazzaz 1990). Therefore increasing temperature and high CO2 may affect the pollen load in a region.
Spieksma et al. (1995b) examined atmospheric birch (Betula) pollen data from five European stations (Basel, Vienna, London, Leiden, and Stockholm) between 1961 and 1993 (records from 18 to 30 years). They found weakly rising trends of annual sums of daily concentrations at all five stations. More recent European studies, in Denmark (Rasmussen 2002) and Switzerland (Frei 1998) found trends of increasing amounts of pollen over the latter decades of the 1900s that were related to climate change. Teranishi et al. (2000) studied the association between Japanese cedar (Cryptomeria japonica) pollen and temperature from 1983 to 1998 in Japan. They found a significant positive correlation between total pollen count in a year and temperature in July the previous year. In North America, Levetin (2001) has found statistically significant increases in a number of taxa, including Juniperus, Quercus, Carya, and Betula, since 1987. There is some evidence that these increases have been associated with increases in average winter temperature.
Rising CO2 concentrations may affect the amount of pollen produced per plant as well as the allergenic content of the pollen grains itself. Greenhouse experiments with ragweed plants showed that plants exposed to elevated levels of CO2 increased their ragweed pollen production (Ziska and Caulfield, 2000) as well as the Amb a 1 content per pollen grain (Singer et al. 2005).
6.4.5.2 Atmospheric Pressure
Although only a few studies on the importance of atmospheric pressure have been carried out, the effects of pressure on the threshold levels can be very diverse. (i) In connection with the NAO (North Atlantic Oscillation)-studies it has been shown that that pressure is a much more important factor causing changes in pollen concentrations than has been realized thus far (e.g. Smith et al. 2009). The role of pressure is revealed in long-distance pollen transport. Emberlin (1994) suggested that an increase in the strength of the Atlantic westerlies over north-west Europe would enhance the long distance transport of pollen from northern and central Europe to Scandinavia. This aspect should be taken into account for pollen forecast, since it may affect the expected pollen load for the coming day(s) considerably. (ii) Although the role of climatic factors in exacerbating asthma is poorly understood (D’Amato et al. 2001), high and low atmospheric pressures have been linked to asthma attacks (Garty et al. 1998; Celenza et al. 1996). There is evidence that changes in temperature, barometric pressure and relative humidity have some influence on the worsening of asthmatic symptoms (e.g. Hashimoto et al. 2004). (iii) Differences in atmospheric pressure can cause remarkable error in the function of pollen trap; for instance, in Switzerland at an altitude of about 2,300 m at Gütsch where the mean air pressure is 770 hPa this causes a 10% error compared to sampling in Basel where the air pressure is 979 hPa on an average (Gehrig and Peeters 2000).
6.4.5.3 Thunderstorms
Thunderstorms have been linked to asthma epidemics, especially during the pollen seasons, and there are descriptions of asthma outbreaks associated with thunderstorms. This is mainly because pollen grains release allergenic particles when they get in to contact with rainwater in combination with an electric field.
Grass pollen has been responsible for triggering allergic asthma, gaining impetus as a result of the 1987/1989 Melbourne and 1994 London thunderstorm-associated asthma epidemics (Suphioglu 1998). Ryegrass pollen ruptures upon contact with water releasing about 700 starch granules which not only contain the major allergen Lol p 5, but have been shown to trigger both in vitro and in vivo IgE-mediated responses. Starch granules have been isolated in Melbourne atmosphere with 50-fold increase following rainfall. Free grass pollen allergen molecules have been shown to interact with other particles including diesel exhaust carbon particles, providing a further transport mechanism for allergens to gain access into lower airways (Suphioglu 1998). Taylor et al. (2007) also suggested that thunderstorm asthma epidemics may be triggered by grass pollen rupture in the atmosphere and the entrainment of respirable-sized particles in the outflows of air masses at ground level. Pollen contains nicotinamide adenine dinucleotide phosphate (reduced) oxidases and bioactive lipid mediators which likely contribute to the inflammatory response.
Vaidyanathan et al. (2006) decided to determine whether the potential for pollen fragmentation is increased during thunderstorms by exploring the effects of electric fields, with magnitude as found in the outdoor environment. Fresh pollen grains were collected from Bermuda grass flowers. Water was added to test for pollen rupture and to assess pollen viability. Bermuda grass pollen did not rupture within 1 h of contact with water. Only after exposure to an electric field the Bermuda grass pollen showed a considerable amount of rupturing immediately upon immersion in water. The higher the voltage the pollen is exposed to before coming into contact with water, the higher the percentage of rupture of the pollen. Electric fields, generated in the laboratory and of magnitude found during thunderstorms, affected the pollen after as little as a 5 s exposure. Thunderstorms regularly generate electric fields up to 5 kV/m in strength, can reach 10 kV/m and cover several km in distance.
6.4.5.4 Ozone
Exposure to increased atmospheric levels of O3 causes increased airway reactivity to pollen and is related to an increased risk of asthma exacerbation (Chen et al. 2004). It has been observed that O3 exposure has a priming effect on allergen-induced responses as well as an intrinsic inflammatory effect in the airways of allergic asthmatics (Molfino et al. 1991; Kehrl et al. 1999). Exposure to O3 may increase the risk of allergic sensitization in predisposed subjects. Indeed, by lowering the threshold concentration of allergen able to induce clinical symptoms, O3 can enhance the airway responsiveness of sensitized subjects. Molfino et al. (1991) reported that a 1-h exposure to 0.12 ppm O3 while at rest caused a two-fold reduction in the provocation concentration of inhaled antigen required to cause early bronchoconstriction in specifically sensitized asthmatic subjects. The mean provocation dose of ragweed pollen necessary to reduce FEV1 by 20% in sensitized asthmatic subjects was significantly reduced to about one-half the dose of ragweed allergen when the patients were pre-exposed to 0.12 ppm O3 for 1 h versus pre-exposure to air. Jörres et al. (1996) using a higher effective dose (0.25 ppm inhaled through a mouthpiece with intermittent exercise) and a longer duration of exposure (3 h), found that 23 of 24 mild asthmatic subjects required a lower provocation dose of allergen to cause a 20% decrease in FEV1 (PD20) after O3 exposure. The previous exposure to O3 (and NO2) on subsequent pollen allergen significantly increases the allergen-induced release of eosinophil cationic protein in nasal lavage of patients with seasonal allergic rhinitis (Devalia et al. 1998).
Rogerieux et al. (2007) exposed timothy grass pollen to ozone (O3), nitrogen dioxide (NO2) and sulphur dioxide (SO2) alone or in combination. For O3-treated pollen, tests with patients’ sera showed an acidification of allergens Phl p 1b, Phl p 4, Phl p 5 and Phl p 6. Moreover, samples treated with a mix of NO2/O3 or NO2/SO2 showed a higher decrease in allergen content, compared with samples treated with only one pollutant.
6.4.5.5 Nitrogen Dioxide (NO2) and Sulphur Dioxide (SO2)
Automobile exhaust is the most significant source of NO2 which is an oxidant pollutant. It is less chemically reactive than O3 and thus the inhalation of NO2 is usually not associated with significant changes in bronchial function of asthmatic patients but it has an obstructive influence on bronchi during exercise (Roger et al. 1990). Tunnicliffe et al. (1994) demonstrated a greater allergen-induced early bronchoconstriction by a combined inhalation of allergen and NO2 for 1 h, while at rest, than after sham exposure. SO2 is generated primarily from burning of sulphur-containing fossil fuel. It has been shown to induce bronchial obstruction very rapidly (within 2–5 min) in asthmatic patients at low concentrations (Riedel et al. 1988). O3, NO2 and SO2 have been found to interact with allergenic pollen in the ambient air to aggravate symptoms of asthma (Feo Brito et al. 2007).
Rogerieux et al. (2007) showed that exposure of grass pollen to nitrogen dioxide (NO2) and sulphur dioxide (SO2) induced a decrease of grass allergen recognition by patients’ sera. This decrease could be due to a mechanical loss of allergens from the altered pollen grains and/or post-translational modifications affecting allergen recognition by IgE.
6.4.5.6 Particulate Matter
Particulates, alternatively referred to as particulate matter (PM) or fine particles, are tiny particles of solid or liquid suspended in a gas. Sources of particulate matter can be man made or natural. Some particulates occur naturally, originating from volcanoes, dust storms, forest and grassland fires, living vegetation, and sea spray. Human activities, such as the burning of fossil fuels in vehicles, power plants and various industrial processes also generate significant amounts of aerosols. Increased levels of fine particles in the air are linked to health hazards such as heart disease, altered lung function and lung cancer. Fernvik et al. (2002) studied health effects due to air pollution arising from motor vehicles, a major public and political concern world-wide. Epidemiological studies have shown that the manifestations of asthma are increased by air pollution in individuals who are already affected, e.g., the interaction between ambient PM10 and pollen in studies of short-term effects (Lierl and Hornung 2003; Feo Brito et al. 2007) To investigate the potential role of traffic particulate matter, TPM, or pure carbon core particles in the initiation and persistence of experimental allergic inflammation, mice were immunized with birch pollen alone, or pollen together with TPM, or with birch pollen and Al(OH)3, or with birch pollen and carbon core particles. Mice immunized with birch pollen alone and challenged intranasally with pollen or a mixture of pollen and TPM demonstrated the highest levels of IL-4 and IL-5 (Fernvik et al. 2002). These results highlight the importance of the exposure to a combination of particulate matters and pollen allergens. The results strongly suggest that it is most likely to be the organic phase bound to the carbon core of the diesel exhaust particles (DEP) that might have an important adjuvant effect in the induction of experimental allergy.
Diaz-Sanchez et al. (1996) studied the effect of DEP on antigen in ragweed-sensitive subjects challenged (nasal provocation test) with DEP, Amb a1 (the major ragweed allergen) and a combination of DEP and Amb a 1. Provocation with ragweed led to an increase in both total and ragweed-specific IgE in nasal lavage fluid measured at 18 h, 4 and 8 days post challenge. The DEP challenge increased the concentration of ragweed-specific IgE 16-fold versus concentrations observed after challenge with ragweed allergen alone. Combination of DEP and ragweed allergen challenge markedly enhances human in vivo nasal ragweed-specific IgE and skews cytokine production to a T-helper cell type-2 (Th2) pattern. These results indicate that DEP plays a role in the enhanced allergic inflammatory response thus decreasing the threshold value (Rudell et al. 1994).
6.5 Impact of Allergenic Pollen on Non-allergic Diseases
Recent observations draw attention to rather consistent relationships between daily variations in both pollen counts and the incidence or prevalence of various non-allergic diseases. This applies especially to three groups of diseases: non-allergic respiratory diseases, cardio- and cerebrovascular diseases, and psychiatric diseases including suicide and suicide attempt.
6.5.1 Effects on Non-allergic Respiratory Diseases
An impressive amount of data supports the effects of air pollution on respiratory diseases both in terms of mortality and morbidity (Schwela 2000; Baldacci and Viegi 2002; Pascal 2009). However, pollen and spores have been included rarely among pollutants and their possible effects are often neglected. Brunekreef et al. (2000) were the first in 2000 to report an association between pollen concentrations and mortality. The authors evaluated daily non-accidental deaths due to cardiovascular and respiratory diseases and pneumonia between 1986 and 1994 in the Netherlands, and daily pollen levels for Poaceae, Betula, Quercus, Fraxinus, Artemisia, and Rumex from two stations (Leiden, west and Helmond, south). Results were also adjusted for long-term and seasonal trends, temperature, relative humidity, influenza morbidity, day of the week and holidays. Furthermore, lag (−7, −2, −1, 0) effect was evaluated. The main findings were that (i) Weekly concentrations of Poaceae were associated particularly with daily deaths due to chronic obstructive pulmonary disease (COPD) and pneumonia (ii) there was a consistent dose–response relationship and (iii) Betula and Rumex were positively associated with mortality. None of these findings were confounded by air pollution.
More recently, several papers confirmed and clarified Brunekreef’s (Brunekreef et al. 2000) study. A symmetric case-crossover analysis, including pollen levels of Asteraceae, Betulaceae, Cupressaceae, Chenopodiaceae, Ericaceae, Fagaceae, Myrtaceae, Oleaceae, Pinaceae, Plantaginaceae, Platanaceae, Poaceae, Polygonaceae, Salicaceae and Urticaceae, performed in the city of Vigo (Spain) provided confirmation of a short-term relationship between pollen levels of Betula, Chenopodiaceae, Corylus and Alnus and the medical emergency calls for respiratory and cardiovascular causes in the period 1996–1999, even though there was no evident interaction between pollen and chemical air pollutants (Carracedo-Martinez et al. 2008). Interestingly, this association was statistically significant at lag 0 for Chenopo-diaceae, at lag 2 for Corylus and Alnus and at lag 3 for Betula, whereas no relationships were found at lag 1.
In Darwin (Australia), positive linear associations were shown between hospital admissions for total respiratory diseases and COPD in the period April 2004–November 2005 and total pollen counts, without lag effect. But no convincing evidence was found for relationships between total pollen and asthma or respiratory infections. The finding of an association between pollen concentrations and respiratory hospital admissions that could not be explained by asthma admissions suggests that ambient airborne pollen grains might have a wider public health impact than previously recognized. When individual taxa were investigated, associations were the strongest in relation to Myrtaceae pollen (the dominant tree taxon in the region), while positive associations not attaining statistical significance were observed for Poaceae, Cyperaceae and Arecaceae. On the other hand, no associations were evident for any conditions with fungal spores (Hanigan and Johnston 2004).
Another study, published by Burney et al. (2008), shed new light on intrinsic (i.e. non-allergic) asthma. A cohort of 297 patients using bronchodilators aged 18–64 years was extensively evaluated with skin tests in London and they were asked to report any acute respiratory event over the coming months. Small particles with a mean aerodynamic diameter <10 μm (PM10) were collected and the ability of airborne particles to bind IgE from the patients was compared with particles sampled on the weekend before their reported exacerbation and with particles sampled on the weekend 2 weeks before or after. A highly significant association (p = 0.00089) between exacerbations and a 25% increase in IgE binding to particles collected on the previous weekend compared with the control weekends was found, even in patients with negative skin prick tests to grass or tree pollen. This observation indicates a role of unidentified allergens in asthma diagnosed as intrinsic, suggesting limits in current allergy diagnostics.
6.5.2 Effects on Cardio- and Cerebrovascular Diseases
The study in the Netherlands by Brunekreef et al. (2000) does not allow any conclusions on the possible effects on mortality from cardiovascular diseases to be drawn. The association between pollen and mortality was seen only for two taxa, Betula and Rumex, and the authors did not show results by disease type. On the other hand, high Poaceae pollen counts were not associated with mortality from cardiovascular diseases. Similarly, in the study with patients who made medical emergency calls in Vigo (Carracedo-Martinez et al. 2008), elevations in pollen levels did not increase medical emergency calls because of cardiovascular causes.
However, Low et al. (2006) analyzed the effects of numerous environmental variables, including pollen and spore counts, on hospital admissions for stroke in New York. Using a statistical time series modelling technique, the authors found a relatively small, but significant independent association (p = 0.0341), between stroke events and grass pollen concentration. It is a pity that they did not provide any hypothesis supporting this observation, apart from the fact that alveolar inflammation is proposed as the mechanistic link.
Similarly, according to Matheson et al. (2008), hay fever seems to be a risk factor for stroke during a 4.4 year period in South Carolina. Patients with a history of allergic rhinitis had an unadjusted hazard ratio of 1.72 (95% CI, 1.08–2.27) for stroke versus patients without allergic rhinitis. Risk of stroke remained significant (hazard ratio, 1.87 [95% CI, 1.17–2.99]) after controlling for age, sex, race, smoking status, body mass index, diabetes, hypertension, alcohol use, and hyperlipidemia. The authors suggested the mechanism to be the systemic inflammation found in those with allergic rhinitis. Yet, Ng et al. (2008) put forward an additional explanation, i.e. obstructive sleep apnea (OSA), for the increased risk. It is now well accepted that allergic rhinitis is associated with an increased risk of OSA in adults and children and that adults with OSA have an increased risk of cerebrovascular disease independent of atherosclerotic risk factors.
6.5.3 Effects on Psychiatric Diseases
The seasonal trend of some psychiatric diseases has been reported consistently, but its causality is still poorly understood. In this view, several papers investigated the possible role of the pollen season which overlaps with the seasonality of some psychiatric diseases. An experimental study showed a regression in children with autistic spectrum disorders (ASD) or with attention deficit hyperactive disorder (ADHD) after nasal challenge with oak, timothy grass and ragweed pollen. During natural pollen exposure, 15 of 29 (52%) children with ASD and 10 of 18 (56%) children with ADHD demonstrated neurobehavioral regression. There was no correlation with the child’s allergic status (IgE, skin tests and RAST) or allergy symptoms. The same effect was observed in allergic and non-allergic children (Boris and Goldblatt 2004). The authors suggested that, although they had not conducted an empirically test, an unknown non IgE-mediated mechanism underlined this relationship.
The most numerous studies are about suicide or suicide attempt, including those done at the University of Maryland School of Medicine at Baltimore. A strong and highly replicated seasonality of suicide in late spring and, less consistent, in late summer and early fall is well known (Hakko et al. 1998). For this reason, Postolache et al. (2005) performed an epidemiologic study analyzing 2,417 suicides in the tree pollen season and 1,811 in the ragweed season for the continental US and Canada in the period 1995–1998. They found a two-fold increase in the rate of non-violent suicides among younger females during the period with high tree pollen, in comparison to similar periods with low tree pollen (95% CI, 1.3–3.0). There was no difference between the post pollen period and the pre pollen period. The association was thus found only for non-violent suicides, only in females, and only for tree pollen (and not also for ragweed pollen). While these results may have been confounded by a number of biological and psychosocial factors (such as impact of feeling sick), acting during the allergy season on individuals and their social support systems, two possible explanations were proposed. These were the side-effect of anti-allergic drugs (pseudoephedrine, antihistamines and corticosteroids), which may worsen prosuicidal factors such as night-insomnia, day-somnolence, agitation, anxiety, impulsivity, and cognitive disturbance (Pretorius 2004); or a mechanism linked to an increased expression of cytokines during the immune activation. Both hypotheses appear rather weak. Nevertheless, three points require careful thought: (i) If there is insufficient data to prove any link between the other medications used to treat allergy and suicidality, systemic (but not topical) corticosteroids used for severe symptoms have been really associated with manic and depressive episodes and mixed mood states (Postolache et al. 2008). On June 12, 2009 the US Food and Drug Administration issued a warning raising concerns about the suicidality potential of montelukast (trade name Singulair®) and other leukotriene receptor antagonists (LTRA) (Manalai et al. 2009). (ii) Another mechanism linking allergic inflammation, depression, and suicide has been demonstrated. Reeves et al. (2007) outlined the role of alcohol, that is a well-established risk factor for adolescent suicide, in inducing phosphorylation and rearrangement of tight junction proteins of the blood–brain barrier (BBB) resulting in increased “leakiness”, i.e. passage of cells and molecules. Many authors have proposed for a long time that allergic inflammation influences depression-related brain function via molecular and cellular mediators, but those mediators have a very limited access to the brain when the BBB is intact. Alcohol intake disrupts BBB, allowing increased brain exposure to cellular mediators of allergy, especially in youth when alcohol use starts. (iii) It has also been shown in Brown Norway rats that sensitization and exposure to aeroallergens induces anxiety-like and aggressive behaviours as well as allergy-related helper T-cell type 2 (Th2) cytokine gene expression in the prefrontal cortex. Thus, it is possible that sensitization and exposure to aeroallergens, which peak in spring, may be conducive to seasonal exacerbation of suicide risk factors such as anxiety, depression, hostility/aggression, and sleep disturbance. The recent report of Th2 (allergy-mediating) cytokine expression in the orbitofrontal cortex of suicide victims should lead to future studies to test the hypothesis that mediators of allergic inflammation in the nasal cavities may result in Th2 cytokine expression in the brain, influencing affect and behavioural modulation (Postolache et al. 2008).
Other studies showed a significant relationship (p < 0.001) between high pollen season and self-reported non-winter seasonal affective disorder (SAD), distinguished by depression in summer and remission in fall and winter (Guzman et al. 2007). The survey was conducted among college students at local universities in Washington, DC. However, the sample included only African American and African students and, therefore, the results may not be applicable to the entire population. The study was based only on a questionnaire and patients were not tested for pollen sensitization. No direct measures of depression scores or pollen counts were collected. It is nevertheless a fact that the findings confirm certain results of the oldest study about this question that used an ethnically diverse sample (Bartko and Kasper 1989).
Postolache et al. (2008) stated that (i) the rates of depression, anxiety, and sleep disturbance (suicide risk factors) are greater in patients with allergic rhinitis than in the general population, (ii) that the rate of allergy is greater in patients with depression and (iii) finally that patients with a history of allergy may have an increased rate of suicide. However, it remains unknown if these associations are true or spurious, and if true, if they represent trait (vulnerability) – level relationship or if mood-states are involved, i.e. if there is adequate evidence to suggest that exposure to allergens might trigger mood changes in vulnerable individuals. In another study, confirming the relationship between tree pollen and changes in mood in patients sensitized to that pollen, Postolache et al. (2007) suggested a connection between allergy and depression decompensation rather than between pollen and depression.
To sum up, allergy can influence mood by several potential mechanisms. There may be somatic changes, such as discomfort caused by allergic inflammatory processes in the upper airway that may affect well being. This situation may lead to other possible mediators affecting mood, such as the use of medications like corticosteroids or LTRA, or disturbance of sleep caused by multiple factors including obstruction of the airways. The release of inflammatory mediators including cytokines is one likely mechanism that may promote the worsening in mood. This mood worsening can occur by either acting directly in the brain or through other pathways, such as interactions with the HPA-axis and/or the IDO enzyme. Cytokines have been shown to induce depression and anxiety. The findings of Postolache et al. (2007) relating allergic symptoms with depression scores may be explained in part by the release of cytokines during allergic reactions. In vitro studies have also shown that certain human polymorphisms increase the expression of cytokines including TNF-α, IL-13, and IFN-γ. In addition, certain cytokine polymorphisms increase susceptibility to allergic disease such as asthma. Moreover, allergic symptoms have been correlated with the amount of cytokines released during some allergic reactions. It is possible that depression scores in some individuals may reflect the increased amount of cytokine release during allergic processes. This issue is a matter to be clarified with future investigations.
6.6 Conclusion
Pollen has a substantial impact on human health. Besides the role of pollen and fungal spores in allergic diseases, recent research also suggests an effect of allergenic pollen on non-allergic diseases. Current knowledge is insufficient to draw a conclusion on these effects. Experimental studies showing a proinflammatory and immunomodulatory activity of pollen support the hypothesis of a non-IgE mediated effect on human health, even if with several limitations, some epidemiological observations are consistent with the experimental data. Other indications come from studies on respiratory and psychiatric diseases which present some diagnostic difficulties and limitations. However, all these findings have not been sufficiently reproduced so far. Consequently, further research is needed at clinical, epidemiological, animal and postmortem tissue levels to clarify the complex role of pollen on human health, which probably goes beyond allergic diseases. Experimental studies should identify the role of pollen-derived particles in airborne particulate matter (e.g.PM10) and their effects on human health. Moreover, epidemiological studies should be specifically designed by a multidisciplinary research team, with the aim of confirming the association between pollen counts and diseases. The advances in the field of detection of airborne allergens could contribute to distinguishing the effects of allergens from those of other non-allergenic proteins of pollen (Thibaudon and Sindt 2008).
Most knowledge on the impact of pollen on human health deals with the allergic sensitization upon pollen exposure causing IgE-mediated responses in susceptible individuals. These responses, resulting in respiratory diseases and allergic eye irritation, have a marked impact not only on clinical parameters, but also on functional status as shown by a study demonstrating a reduction in productivity of 11–40% (Vandenplas et al. 2008). This impact of pollen on health status differs among patients, both on an individual as well as on a population level. It is dependent on weather conditions (e.g. temperature, thunderstorms), presence of air pollutants (e.g. O3, NO2, SO2, particulate air pollution [PM]) and the impact may change during the season. Furthermore, the amount of allergen per pollen grain can differ which may affect the impact of pollen.
The diversity of factors that influence the health impact of pollen has hampered the definition of a straightforward relationship between pollen and the severity of symptoms. Several studies report pollen levels at which symptoms develop, but there is still no consensus on these threshold levels. The various factors discussed in this overview that influence the interactions between pollen and patients, are responsible for the fact that threshold values not only vary by pollen type, but also by region, population, year, time of the season, and landscape architecture (e.g. urban or rural). However, there is a need for definition of threshold pollen levels, not only for scientists and physicians, but also for patients that want to know at which pollen concentration they are at risk for symptom development, and for policymakers that want to create distinct rules for public information services. At this moment, science cannot formulate a validated solution. However, one first approach to tackle this problem could be to define preliminary threshold values for different regions. Whereas this is inevitably an oversimplification, such preliminary threshold values could be validated using symptoms scores of patients that can be entered by special websites (e.g. www.allergieradar.nl or www.polleninfo.org). Such websites may reach a wide audience and symptoms scores can be collected including GPS coordinates. The combination of geographical coordinates and symptoms scores will result in relevant new information which can teach us whether these preliminary threshold values are correct or whether they should be adjusted based on interacting mechanisms.
References
Abelson, M. B., George, M. A., Schaefer, K., & Smith, L. M. (1994). Evaluation of the new ophthalmic antihistamine, 0.05% levocabastine, in the clinical allergen challenge model of allergic conjunctivitis. Journal of Allergy and Clinical Immunology, 94, 458–464.
Agarwal, M. K., Swanson, M. C., Reed, C. E., & Yunginger, J. W. (1984). Airborne ragweed allergens: Association with various particle sizes and short ragweed plant parts. Journal of Allergy and Clinical Immunology, 74, 687–693.
Agashe, S. N., Bapat, B. N., Bapat, H. N., & Philip, E. (1994). Aerobiology of Casuarina pollen and its significance as a potential aeroallergen. Aerobiologia, 10, 123–128.
Ahlholm, J. U., Helander, M. L., & Savolainen, J. (1998). Genetic and environmental factors affecting the allergenicity of birch (Betula pubescens ssp. czerepanovii [Orl.] Hamet-ahti) pollen. Clinical and Experimental Allergy, 28(11), 1384–1388.
Ahlstrom-Emanuelsson, C., Andersson, M., Persson, C., Schrewelius, C., & Greiff, L. (2004). Topical treatment with aqueous solutions of rofleponide palmitate and budesonide in a pollen-season model of allergic rhinitis. Clinical and Experimental Allergy, 34(5), 731–735.
Akerlund, A., Andersson, M., Leflein, J., Lildholdt, T., & Mygind, N. (2005). Clinical trial design, nasal allergen challenge models, and considerations of relevance to pediatrics, nasal polyposis, and different classes of medication. Journal of Allergy and Clinical Immunology, 115(3 Suppl. 1), 460–482.
Alcázar, P., Galán, C., Cariñanos, P., & Domínguez, E. (1998). Vertical variation in Urticaceae airborne pollen concentration. Aerobiologia, 14, 131–134.
Alcázar, P., Galán, C., Cariñanos, P., & Domínguez, E. (1999a). Diurnal variations of airborne pollen at two different heights. Journal of Investigational Allergology and Clinical Immunology, 9, 89–95.
Alcázar, P., Galán, C., Cariñanos, P., & Domínguez, E. (1999b). Effects of sampling height and climatic conditions in aerobiological studies. Journal of Investigational Allergology and Clinical Immunology, 9, 253–261.
Alcázar, P., Cariñanos, P., De Castro, C., Guerra, F., Moreno, C., Domínguez-Vilches, E., & Galán, C. (2004). Airborne plane-tree (Platanus hispanica) pollen distribution in the city of Córdoba, South-western Spain, and possible implications on pollen allergy. Journal of Investigational Allergology and Clinical Immunology, 14(3), 238–243.
Amin, K., Ekberg-Jansson, A., Lofdahl, C. G., & Venge, P. (2003). Relationship between inflammatory cells and structural changes in the lungs of asymptomatic and never smokers (a biopsy study). Thorax, 58, 135–142.
Andersson, K., & Lidholm, J. (2003). Characteristics and immunobiology of grass pollen allergens. International Archives of Allergy and Immunology, 130, 87–107.
Antepara, I., Fernandez, J. C., Gamboa, P., Jauregui, I., & Miguel, F. (1995). Pollen allergy in the Bilbao area (European Atlantic seaboard climate): Pollination forecasting methods. Clinical and Experimental Allergy, 25, 133–140.
Asero, R., Mistrello, G., Roncarolo, D., & Casarini, M. (2000). Detection of allergens in plantain (Plantago lanceolata) pollen. Allergy, 55, 1059–1062.
Asero, R., Wopfner, N., Gruber, P., Gadermaier, G., & Ferreira, F. (2006). Artemisia and Ambrosia hypersensitivity: Co-sensitization or co-recognition? Clinical and Experimental Allergy, 36, 658–665.
Asher, M. I., Stewart, A. W., Mallol, J., Montefort, S., Lai, C. K., Aït-Khaled, N., & Odhiambo, J. (2010). Which population level environmental factors are associated with asthma, rhinoconjunctivitis and eczema? Review of the ecological analyses of ISAAC Phase One. Respiratory Research, 11, 8.
Asturias, J. A., Arilla, M. C., Gomez-Bayon, N., Martinez, A., Martinez, J., & Palacios, R. (1997). Cloning and expression of the panallergen profilin and the major allergen (Ole e 1) from olive tree pollen. Journal of Allergy and Clinical Immunology, 100, 365–372.
Asturias, J. A., Gómez-Bayón, N., Eseverri, J. L., & Martínez, A. (2003). Par j 1 and Par j 2, the major allergens from Parietaria judaica pollen, have similar immunoglobulin E epitopes. Clinical and Experimental Allergy, 33, 518–524.
Baldacci, S., & Viegi, G. (2002). Respiratory effects of environmental pollution: Epidemiological data. Monaldi Archives for Chest Disease, 57(3–4), 156–160.
Banken, R., & Comtois, P. (1990). Concentration de l’herbe à poux et prévalence de la rhinite allergique dans deux municipalités des Laurentides. L’Unión Médicale du Canada, 119, 178–182.
Barber, D., Moreno, C., Ledesma, A., Serrano, P., Galán, A., Villalba, M., Guerra, F., Lombardero, M., & Rodríguez, R. (2007). Degree of olive pollen exposure and sensitization patterns. Clinical implications. Journal of Investigational Allergology and Clinical Immunology, 17(Suppl. 1), 63–68.
Barber, D., de la Torre, F., Feo, F., Florido, F., Guardia, P., Moreno, C., Quiralte, J., Lombardero, M., Villalba, M., & Salcedo, G. (2008). Understanding patient sensitization profiles in complex pollen areas: A molecular epidemiological study. Allergy, 63, 1550–1558.
Barral, P., Tejera, M. L., Treviño, M. A., Batanero, E., Villalba, M., Bruix, M., & Rodríguez, R. (2004). Recombinant expression of Ole e 6, a Cysenriched pollen allergen, in Pichia pastoris yeast. Detection of partial oxidation of methionine by NMR. Protein Expression and Purification, 37, 336–343.
Barral, P., Serrano, A. G., Batanero, E., Pérez-Gil, J., Villalba, M., & Rodríguez, R. (2006). A recombinant functional variant of the olive pollen allergen Ole e 10 expressed in baculovirus system. Journal of Biotechnology, 121, 402–409.
Bartko, J. J., & Kasper, S. (1989). Seasonal changes in mood and behavior: A cluster analytic approach. Psychiatry Research, 28(2), 227–239.
Bauchau, V., & Durham, S. R. (2004). Prevalence and rate of diagnosis of allergic rhinitis in Europe. European Respiratory Journal, 24(5), 758–764.
Bazzaz, F. A. (1990). The response of natural ecosystems to the rising global CO2 levels. Annual Review of Ecology and Systematics, 21, 167–196.
Behrendt, H., & Becker, W. M. (2001). Localization, release and bioavailability of pollen allergens: The influence of environmental factors. Current Opinion in Immunology, 13, 709–715.
Belchi-Hernandez, J., Moreno-Grau, S., Bayo, J., Rendueles, B. E., Moreno, J., Angosto, J. M., Iniesta-Perez, B., & Gonzalez, A. M. (2001). Pollinosis related to Zygophyllum fabago in a Mediterranean area. Aerobiologia, 17, 241–246.
Blanca, M., Boulton, P., Brostoff, J., & Gonzalez-Reguera, I. (1983). Studies of the allergens of Olea europea pollen. Clinical Allergy, 13(5), 473–478.
Bonini, S., Bonini, S., Bucci, M. G., Berruto, A., Adriani, E., Balsano, F., & Allansmith, M. R. (1990). Allergen dose response and late symptoms in a human model of ocular allergy. Journal of Allergy and Clinical Immunology, 86, 869–876.
Boris, M., & Goldblatt, A. (2004). Pollen exposure as a cause for the deterioration of neurobehavioral function in children with autism and attention deficit hyperactive disorder: Nasal pollen challenge. Journal of Nutritional and Environmental Medicine, 14(1), 47–54.
Bousquet, P. J., Chinn, S., Janson, C., Kogevinas, M., Burney, P., & Jarvis, D. (2007). Geographical variation in the prevalence of positive skin tests to environmental aeroallergens in the European Community Respiratory Health Survey I. Allergy, 62(3), 301–309.
Brabäck, L., Hjernwz, A., & Rasmussen, F. (2004). Trends in asthma, allergic rhinitis and eczema among Swedish conscripts from farming and non-farming environments. A nationwide study over three decades. Clinical and Experimental Allergy, 34, 38–43.
Britton, J., Pavord, I., Richards, K., Knox, A., Wisniewski, A., Wahedna, I., Kinnear, W., Tattersfield, A., & Weiss, S. (1994). Factors influencing the occurrence of airway hyperreactivity in the general population: The importance of atopy and airway calibre. European Respiratory Journal, 7, 881–887.
Brunekreef, B., Hoek, G., Fischer, P., & Spieksma, F. T. (2000). Relation between airborne pollen concentrations and daily cardiovascular and respiratory-disease mortality. The Lancet, 355(9214), 1517–1518.
Burbach, G. J., Heinzerling, L. M., Edenharter, G., Bachert, C., Bindslev-Jensen, C., Bonini, S., Bousquet, J., Bousquet-Rouanet, L., Bousquet, P. J., & Bresciani, M. (2009). GA(2)LEN skin test study II: Clinical relevance of inhalant allergen sensitizations in Europe. Allergy, 64, 1507–1515.
Burney, P. G., Newson, R. B., Burrows, M. S., & Wheeler, D. M. (2008). The effects of allergens in outdoor air on both atopic and nonatopic subjects with airway disease. Allergy, 63(5), 542–546.
Burr, M. L., Emberlin, J. C., Treu, R., Cheng, S., & Pearce, N. E. (2003). Pollen counts in relation to the prevalence of allergic rhinoconjunctivitis, asthma and atopic eczema in the International Study of Asthma and Allergies in Childhood (ISAAC). Clinical and Experimental Allergy, 33(12), 1675–1680.
Busse, W. W. (1989). The relationship between viral infections and onset of allergic diseases and asthma. Clinical and Experimenal Allergy, 19, 1–9.
Busse, W. W. (2010). The relationship of airway hyperresponsiveness and airway inflammation: Airway hyperresponsiveness in asthma: Its measurement and clinical significance. Chest, 138, 4–10.
Buters, J. T., & Behrendt, H. (2008). Kombinationswirkungen: Pollen und Schadstoffe. Rundgesprache der Kommission für Ökologie, Bd 38. Bioaerosole und ihre Bedeutung für die Gesundheit (pp. 97–105). München: Verlag Dr. Friedrich Pfeil.
Buters, J. T., Kasche, A., Weichenmeier, I., Schober, W., Klaus, S., Traidl-Hoffmann, C., Menzel, A., Huss-Marp, J., Kramer, U., & Behrendt, H. (2008). Year-to-year variation in release of Bet v 1 allergen from birch pollen: Evidence for geographical differences between West and South Germany. International Archives of Allergy and Immunology, 145, 122–130.
Buters, J. T., Weichenmeier, I., Ochs, S., Pusch, G., Kreyling, W., Boere, A. J., Schober, W., & Behrendt, H. (2010). The allergen Bet v 1 in fractions of ambient air deviates from birch pollen counts. Allergy, 65, 850–858.
Calleja, M., & Farrera, I. (2000). Le Cyprès:un nouveau fléau pour la région Rhône-Alpes? Allergy and Immunology, 32, 125–127.
Camacho, J. L., Cano, D., Cervigón, P., Gutiérrez, A. M., & Subiza, J. (2008). Forecasting climate and health related events on plane tree pollen and grass pollen seasons in Madrid region (Spain). Climate prediction applications science workshop, Chapel Hill, NC March 4–7 (poster session).
Canonica, G. W., & Compalati, E. (2009). Minimal persistent inflammation in allergic rhinitis: Implications for current treatment strategies. Clinical and Experimental Immunology, 156, 260–271.
Cárdaba, B., Llanes, E., Chacártegui, M., Sastre, B., López, E., Mollá, R., del Pozo, V., Florido, F., Quiralte, J., Palomino, P., & Lahoz, C. (2007). Modulation of allergic response by gene–environment interaction: Olive pollen Allergy. Journal of Investigational Allergology and Clinical Immunology, 17(Suppl 1), 83–87.
Cariñanos, P., Alcázar, P., Galán, C., & Domínguez, E. (2002). Privet pollen (Ligustrum sp.) as potential cause of pollinosis in the city of Cordoba, south-west Spain. Allergy, 57, 92–97.
Carracedo-Martinez, E., Sanchez, C., Taracido, M., Saez, M., Jato, V., & Figueiras, A. (2008). Effect of short-term exposure to air pollution and pollen on medical emergency calls: A case-crossover study in Spain. Allergy, 63(3), 347–353.
Celenza, A., Fothergill, J., Kupek, E., & Shaw, R. J. (1996). Thunderstorm associated asthma: A detailed analysis of environmental factors. British Medical Journal, 312, 604–607.
Charpin, D., Hughes, B., Mallea, M., Sutra, J. P., Balansard, G., & Vervloet, D. (1993). Seasonal allergic symptoms and their relation to pollen exposure in south-east France. Clinical and Experimental Allergy, 23, 435–439.
Charpin, D., Calleja, M., Lahoz, C., Pichot, C., & Waisel, Y. (2005). Allergy to cypress pollen. Allergy, 60, 293–301.
Chen, L. L., Tager, I. B., Peden, D. B., Christian, D. L., Ferrando, R. E., Welch, B. S., & Balmes, J. R. (2004). Effect of ozone exposure on airway responses to inhaled allergen in asthmatic subjects. Chest, 125(6), 2328–2335.
Cheung, D., Dick, E. C., Timmers, M. C., de Klerk, E. P., Spaan, W. J., & Sterk, P. J. (1995). Rhinovirus inhalation causes long-lasting excessive airway narrowing in response to methacholine in asthmatic subjects in vivo. American Journal of Respiratory and Critical Care Medicine, 152, 1490–1496.
Ciprandi, G., Filaci, G., Negrini, S., De, A. M., Fenoglio, D., & Marseglia, G. (2009). Serum leptin levels in patients with pollen-induced allergic rhinitis. International Archives of Allergy and Immunology, 148(3), 211–218.
Colombo, V. (2010). Zum Sensibilisierungsspektrum von Pollenallergikern im Kanton Tessin. Eine prospektive Studie in Locarno und Lugano 2009. Thesis. Zurich: University of Zurich.
Comtois, P., & Gagnon, L. (1988). Pollen concentration and frequency of pollinosis symptoms: Method of determination of the clinical threshold. Revue Française d’Allergologie, 28, 279–286.
Connell, J. T. (1968). Quantitative intranasal pollen challenge. II. Effect of daily pollen challenge, environmental pollen exposure, and placebo challenge on the nasal membrane. Journal of Allergy, 41(3), 123–139.
Cosmes, M. P., Moreno, A. A., Dominguez, N. C., Gutierrez, V. A., Belmonte, S. J., & Roure, N. J. (2005). Sensitization to Castanea sativa pollen and pollinosis in northern Extremadura (Spain). Allergologia et immunopathologia, 33(3), 145–150.
D’Amato, G., Ruffilli, A., & Ortolani, C. (1991). Allergenic significance of Parietaria. In G. D’Amato, F. Th. M. Spieksma, & S. Bonini (Eds.), Allergenic pollen and pollinosis in Europe (pp. 113–118). Oxford: Blackwell Scientific Publishers.
D’Amato, G., Chatzigeorgiou, G., Corsico, R., Gioulekas, D., Jager, L., Jager, S., Kontou-Fili, K., Kouridakis, S., Liccardi, G., Meriggi, A., Palma-Carlos, A., Palma-Carlos, M. L., Pagan Aleman, A., Parmiani, S., Puccinelli, P., Russo, M., Spieksma, F. T., Torricelli, R., & Wuthrich, B. (1997). Evaluation of the prevalence of skin prick test positivity to Alternaria and Cladosporium in patients with suspected respiratory allergy. A European multicenter study promoted by the Subcommittee on Aerobiology and Environmental Aspects of Inhalant Allergens of the European Academy of Allergology and Clinical Immunology. Allergy, 52(7), 711–716.
D’Amato, G., Spieksma, F., Liccardi, G., Jäger, S., Russo, M., Kontou-Fili, K., Nikkels, H., Wüthrich, B., & Bonini, S. (1998). Pollen-related allergy in Europe. Allergy, 53, 567–578.
D’Amato, G., Liccardi, M., & Cazzola, M. (2001). The role of outdoor air pollution and climatic changes on the rising trends in respiratory allergy. Respiratory Medicine, 95, 606–611.
Dales, R. E., Cakmak, S., Judek, S., & Coates, F. (2008). Tree pollen and hospitalization for asthma in urban Canada. International Archives of Allergy and Immunology, 146(3), 241–247.
Damialis, A., Halley, J. M., Giouleka, D., & Vokou, D. (2007). Long-term trends in atmospheric pollen levels in the city of Thessaloniki, Greece. Atmospheric Environment, 41, 7011–7021.
Davies, R. R., & Smith, L. P. (1973). Forecasting the start and severity of the hay fever season. Clinical Allergy, 3(3), 263–267.
Day, J. H., & Briscoe, M. P. (1999). Environmental exposure unit: A system to test anti-allergic treatment. Annals of Allergy, Asthma & Immunology, 83(2), 83–89.
Day, J. H., Briscoe, M. P., Rafeiro, E., Ellis, A. K., Pettersson, E., & Akerlund, A. (2000). Onset of action of intranasal budesonide (Rhinocort aqua) in seasonal allergic rhinitis studied in a controlled exposure model. Journal of Allergy and Clinical Immunology, 105(3), 489–494.
Day, J. H., Briscoe, M. P., Ratz, J. D., Ellis, A. K., Yao, R., & Danzig, M. (2009). Onset of action of loratadine/montelukast in seasonal allergic rhinitis subjects exposed to ragweed pollen in the Environmental Exposure Unit. Allergy and Asthma Proceedings, 30(3), 270–276.
Déchamp, C., Legal, M., & Deviller, P. (1995). Prevalence of ragweed pollinosis in the South and Eastern suburbs of Lyon in 1993. Allergie et Immunologie, 27, 320–325.
Déchamp, C., Rimet, M. L., Méon, H., & Deviller, P. (1997). Parameters of ragweed pollination in the LYON’s area (France) from fourteen years of pollen counts. Aerobiologia, 13, 275–279.
Déchamp, C., Calleja, M., Deviller, P., Harf, R., & Méon, H. (2001). L’ambroisie dans le Rhône et la Politique Agricole Commune. Le rôle des jachères européennes et des cultures de tournesol sur la pollution biologique aéroportée par le pollen d’ambroisie. Phytoma, 538, 13–16.
Delaunay, J. J., Sasajima, H., Okamoto, Y., & Yokota, M. (2007). Side-by-side comparison of automatic pollen counters for use in pollen information systems. Annals of Allergy, Asthma & Immunology, 98, 553–558.
De Linares, C., Nieto-Lugilde, D., Alba, F., Diaz de la Guardia, C., Galán, C., & Trigo, M. M. (2007). Detection of airborne allergen (Ole e 1) in relation to Olea europaea pollen in S Spain. Clinical and Experimental Allergy, 37, 125–132.
Devalia, J. L., Rusznak, C., & Davies, R. J. (1998). Allergen/irritant interaction – Its role in sensitization and allergic disease. Allergy, 53, 335–345.
De Weger, L. A., Beerthuizen, T., Gast-Strookman, J. M., van der Plas, D. T., Hiemstra, P. S., Terreehorst, I., & Sont, J. K. (2008). Seasonal variability in the relationship between grass pollen counts and ICT-based daily hay fever symptom scores in patients with allergic rhinitis: Implications for hay fever forecasts. EAACI 2008, Barcelona, Spain.
Diaz-Sanchez, D., Tsien, A., Casillas, A., Dotson, A. R., & Saxon, A. (1996). Enhanced nasal cytokine production in human beings after in vivo challenge with diesel exhaust particles. Journal of Allergy and Clinical Immunology, 98(1), 114–123.
Diaz-Sanchez, D., Garcia, M. P., Wang, M., Jyrala, M., & Saxon, A. (1999). Nasal challenge with diesel exhaust particles can induce sensitization to a neoallergen in the human mucosa. Journal of Allergy and Clinical Immunology, 104, 1183–1188.
Dobson, H. E. M. (1988). Survey of pollen and pollenkitt lipids – Chemical cues to flower visitors? American Journal of Botany, 75(2), 170–182.
Egger, C. M., Focke, C., Bircher, A. J., Scherer, K., Mothes-Luksch, N., Horak, F., & Valenta, R. (2008). The allergen profile of beech and oak pollen. Clinical and Experimental Allergy, 38(10), 1688–1696.
Emberlin, J. (1994). The effects of patterns in climate and pollen abundance on allergy. Allergy, 49, 15–20.
Emberlin, J., Smith, M., Close, R., & Adams-Groom, B. (2007). Changes in the pollen seasons of the early flowering trees Alnus spp. and Corylus spp. in Worcester, United Kingdom, 1996–2005. International Journal of Biometeorology, 51, 181–191.
Eriksson, N. E., Wihl, J.-Å., Arrendal, H., & Strandhede, S.-O. (1984). Tree Pollen Allergy. Allergy, 39(8), 610–617.
Eriksson, N. E., Wihl, J.-Å., Arrendal, H., & Strandhede, S.-O. (1987). Tree pollen allergy. III. Cross reactions based on results from skin prick tests and the RAST in hay fever patients. A multi-centre study. Allergy, 42(3), 205–214.
Erkara, I. P., Cingi, C., Ayranci, U., Gurbuz, K. M., Pehlivan, S., & Tokur, S. (2009). Skin prick test reactivity in allergic rhinitis patients to airborne pollens. Environmental Monitoring, 151, 401–412.
Ernst, P., Ghezzo, H., & Becklake, M. R. (2002). Risk factors for bronchial hyper responsiveness in late childhood and early adolescence. European Respiratory Journal, 20, 635–639.
Farrera, I., Calleja, M., & Déchamp, C. (2002). Indoor and outdoor sedimentation in the Rhône-Alpes region during the ragweed pollen season. Revue française d’allergologie et d’immunologie Clinique, 42(7), 750–753.
Feo Brito, F., Mur Gimeno, P., Martinez, C., Tobias, A., Suarez, L., Guerra, F., Borja, J. M., & Alonso, A. M. (2007). Air pollution and seasonal asthma during the pollen season. A cohort study in Puertollano and Ciudad Real (Spain). Allergy, 62(10), 1152–1157.
Fernvik, E., Scharnweber, T., Knopp, D., Niessner, R., Vargaftig, B. B., & Peltre, G. (2002). Effects of fractions of traffic particulate matter on TH2-cytokines, IgE levels, and bronchial hyperresponsiveness in mice. Journal of Toxicology and Environmental Health. Part A, 65, 1025–1045.
Filipowicz, N., Piotrowski, A., Ochocka, J. R., & Asztemborska, M. (2006). The phytochemical and genetic survey of common and dwarf juniper (Juniperus communis and Juniperus nana) identifies chemical races and close taxonomic identity of the species. Planta Medica, 72, 850–853.
Fiorina, A., Scordamaglia, A., Mincarini, M., Fregonese, L., & Canonica, G. W. (1997). Aerobiologic particle sampling by a new personal collector (Partrap FA52) in comparison to the Hirst (Burkard) sampler. Allergy, 52, 1026–1030.
Florido, J. F., Delgado, P. G., de San Pedro, B. S., Quiralte, J., de Saavedra, J. M., Peralta, V., & Valenzuela, L. R. (1999). High levels of Olea europaea pollen and relation with clinical findings. International Archives of Allergy and Immunology, 119, 133–137.
Fotiou, C., Damialis, A., Krigas, N., & Vokou, D. (2011). Parietaria judaica flowering phenology, pollen production, viability and atmospheric circulation, and expansive ability in the urban environment: Impacts of environmental factors. International Journal of Biometeorology, 55(1), 35–50.
Fountain, D. W., Berggren, B., Nilsson, S., & Einarsson, R. (1992). Expression of birch pollen-specific IgE-binding activity in seeds and other plant parts of birch trees (Betula verrucosa Ehrh.). International Archives of Allergy and Immunology, 98, 370–376.
Frank, E., Leonhardt, L. G. W., & Jaeger, S. (1991). Allergenic significance of Rumex pollen. In G. D’Amato, F. Th. M. Spieksma, & S. Bonini (Eds.), Allergenic pollen and pollinosis in Europe (pp. 119–120). Oxford: Blackwell Scientific Publications.
Frei, T. (1998). The effects of climate change in Switzerland 1969–1996 on airborne pollen quantities from hazel, birch and grass. Grana, 37, 172–179.
Frei, T., & Gassner, E. (2008). Trends in prevalence of allergic rhinitis and correlation with pollen counts in Switzerland. International Journal of Biometeorology, 52, 841–847.
Galán, G., Alcázar, P., Domínguez, E., Villamandos, F., & Infante, F. (1995). Airborne pollen grains concentration at two different heights. Aerobiologia, 11, 105–109.
Galán, C., Alcázar, P., Cariñanos, P., Garcia, H., & Domínguez-Vilches, E. (2000). Meteorological factors affecting daily urticaceae pollen counts in southwest Spain. International Journal of Biometeorology, 43, 191–195.
García, J. J., Trigo, M. M., Cabezudo, B., Recio, M., Vega, J. M., Barber, D., Carmona, M. J., Cervera, J. A., Toro, F. J., & Miranda, A. (1997). Pollinosis due to Australian Pine (Casuarina): An aerobiologic and clinical study in southern Spain. Allergy, 52, 11–17.
Garty, B. Z., Kosman, E., Ganor, E., Berger, V., Garty, L., Wietzen, T., & Waisman, Y. (1998). Emergency room visits of asthmatic children, relation to air pollution, weather, and airborne allergens. Annals of Allergy, Asthma & Immunology, 81, 563–570.
Gehrig, R., & Peeters, A. (2000). Pollen distribution at elevations above 1000 m in Switzerland. Aerobiologia, 16, 69–74.
Geller-Bernstein, C., Arad, G., Keynan, N., Lahoz, C., Cardaba, B., & Waisel, Y. (1996). Hypersensitivity to pollen of Olea europaea in Israel. Allergy, 51, 356–359.
Geller-Bernstein, C., Lahoz, C., Cárdaba, B., Hassoun, G., Iancovici-Kidon, M., Kenett, R., & Waisel, Y. (2002). Is it “bad hygiene” to inhale pollen early life? Allergy, 57, 43–46.
Georgitis, J. W., Meltzer, E. O., Kaliner, M., Weiler, J., & Berkowitz, R. (2000). Onset-of-action for antihistamine and decongestant combinations during an outdoor challenge. Annals of Allergy, Asthma & Immunology, 84(4), 451–459.
Gilles, S., Fekete, A,. Zhang, X., Blume, C., Behrendt, H., Schmitt-Kopplin, P., et al. (2010). Pollen-derived adenosine modulates dendritic cell function resulting in inhibition of Th1 responses. 8th EAACI-Ga2len immunology winter school. Eibsee, Germany, 11–14 February 2010.
Gioulekas, D., Papakosta, D., Damialis, A., Spieksma, F., Giouleka, P., & Patakas, D. (2004). Allergenic pollen records (15 years) and sensitization in patients with respiratory allergy in Thessaloniki, Greece. Allergy, 59, 174–184.
Gonianakis, M., Neonakis, I., Gonianakis, I., Baritaki, M., Kypriotakis, Z., Potamias, G., Bouros, D., & Kontou-Fili, K. (2006). A 10-year aerobiological study (1994–2003) in the Mediterranean island of Crete, Greece: Grasses and other weeds, aerobiological data, and botanical and clinical correlations. Allergy and Asthma Proceedings, 27, 363–370.
Gravesen, S. (1979). Fungi as a cause of allergic disease. Allergy, 34(3), 135–154.
Greiff, L., Venge, P., Andersson, M., Enander, I., Linden, M., Myint, S., & Persson, C. G. (2002). Effects of rhinovirus-induced common colds on granulocyte activity in allergic rhinitis. Journal of Infection, 45, 227–232.
Grote, M., & Fromme, H. G. (1986). Cross-reactivity of birch anthers and leaves with birch pollen antigens and allergens. A fine-structural immunocytochemical study using the post-embedding protein-A-gold technique. Journal of Histochemistry and Cytochemistry, 34, 1459–1464.
Grote, M., Valenta, R., & Reichelt, R. (2003). Study of sensitivity of Fraxinus spp. (Oleaceae) in Córdoba, Spain. Journal of Investigational Allergology and Clinical Immunology, 5, 166–170.
Guerra, F., Daza, J. C., Miguel, R., Moreno, C., Galán, C., Domínguez, E., & Sanchez Guijo, P. (1996). Sensitivity to Cupressus, allergenic significance in Córdoba (Spain). Journal of Investigational Allergology and Clinical Immunology, VI(2), 117–120.
Guzman, A., Tonelli, L. H., Roberts, D., Stiller, J. W., Jackson, M. A., Soriano, J. J., Yousufi, S., Rohan, K. J., Komarow, H., & Postolache, T. T. (2007). Mood-worsening with high-pollen-counts and seasonality: A preliminary report. Journal of Affective Disorders, 101(1–3), 269–274.
Hakko, H., Räsänen, P., & Tiihonen, J. (1998). Seasonal variation in suicide occurrence in Finland. Acta Psychiatrica Scandinavica, 98(2), 92–97.
Hanigan, I. C., & Johnston, F. H. (2004). Respiratory hospital admissions were associated with ambient airborne pollen in Darwin, Australia, 2004–2005. Clinical and Experimental Allergy, 37(10), 1556–1565.
Harf, R., & Déchamp, C. (2001). Pollinosis and anti-allergic drug use: Ambrosia in the Rhône-Alpes Region. Revue des Maladies Respiratoires, 18, 517–522.
Hartl, A., Kiesslich, J., Weiss, R., Bernhaupt, A., Mostbock, S., Scheiblhofer, S., Flöckner, H., Sippl, M., Ebner, C., Ferreira, F., & Thalhamer, J. (1999). Isoforms of the major allergen of birch pollen induce different immune responses after genetic immunization. International Archives of Allergy and Immunology, 120, 17–29.
Hashimoto, M., Fukuda, T., Shimizu, T., Watanabe, S., Watanuki, S., Eto, Y., & Urashima, M. (2004). Influence of climate factors on emergency visits for childhood asthma attack. Pediatrics International, 46, 48–52.
Heinzerling, L. M., Burbach, G. J., Edenharter, G., Bachert, C., Bindslev-Jensen, C., Bonini, S., et al. (2009). GA(2)LEN skin test study I: GA(2)LEN harmonization of skin prick testing: Novel sensitization patterns for inhalant allergens in Europe. Allergy, 64, 1498–1506.
Hemmer, W., Focke, M., Wantke, F., Götz, M., Jarisch, R., & Jäger, S. (2000). Ash (Fraxinus excelsior)-pollen allergy in central Europe: Specific role of pollen panallergens and the major allergen of ash pollen, Frax e 1. Allergy, 55, 923–930.
Hernandez, P. M., Lorente, T. F., Romo, C. A., Davila, G. I., Laffond, Y. E., & Calvo, B. A. (1998). Pollen calendar of the city of Salamanca (Spain). Aeropalynological analysis for 1981–1982 and 1991–1992. Allergologia et immunopathologia, 26, 209–222.
Hidalgo, P. J., Galán, C., & Domínguez, E. (2003). Male phenology of three species of Cupressus: Correlation with airborne pollen. Trees, 17, 336–344.
Hirschwehr, R., Heppner, C., Spitzauer, S., Sperr, W. R., Valent, P., Berger, U., Horak, F., Jäger, S., Kraft, D., & Valenta, R. (1998). Identification of common allergenic structures in mugwort and ragweed pollen. Journal of Allergy and Clinical Immunology, 101, 196–206.
Hjern, A., Rasmussen, F., Johansson, M., & Aberg, N. (1999). Migration and atopic disorder in Swedish Conscripts. Pediatric Allergy and Immunology, 10, 209–215.
Hjern, A., Haglund, B., & Hedlin, G. (2000). Ethnicity, childhood environment and atopic disorder. Clinical and Experimental Allergy, 30, 521–528.
Hofman, T., Wykretowicz, G., Stach, A., Springer, E. K. B., & Ossowski, M. (1996). A multicentre analysis of a population of patients with newly-diagnosed pollinosis in Poznan, Poland, in the year 1995. Annals of Agricultural and Environmental Medicine, 3, 171–177.
Hopp, R. J., Bewtra, A., Nair, N. M., & Townley, R. G. (1985). The effect of age on methacholine response. Journal of Allergy and Clinical Immunology, 76, 609–613.
Horak, F., Hussarke, M., Jäger, S., & Skoda-Türk, R. (1979). Die Bestimmung der Aggressivität allergisierender Pollenarten. Wiener klinische Wochenschrift, 92, 161–164.
Horak, F., Stubner, P., Zieglmeyer, R., & Harris, A. G. (2003). Comparison of the effects of desloratadine 5-mg daily and placebo on nasal airflow and seasonal allergic rhinitis symptoms induced by grass pollen exposure. Allergy, 58(6), 481–485.
Italian Association of Aerobiology. (2002). An epidemiological survey of Cupressaceae pollinosis in Italy. Journal of Investigational Allergology and Clinical Immunology, 12, 287–292.
Jäger, S. (1998). Global aspects of ragweed in Europe. In F. Th. M. Spieksma (Ed.), Ragweed in Europe (6th International Congress on Aerobiology, Satellite Symposium Proceedings, Perugia 1998, pp. 11–14). Horsholm: ALK-Abello A/S.
Jensen, J., Poulsen, L. K., Mygind, K., Weeke, E. R., & Weeke, B. (1989). Immunochemical estimations of allergenic activities from outdoor aero-allergens, collected by a high-volume air sampler. Allergy, 44, 52–59.
Jones, A. M., & Harrison, R. M. (2004). The effects of meteorological factors on atmospheric bioaerosol concentrations: A review. Science of the Total Environment, 326, 151–189.
Jörres, R., Nowakm, D., & Magnussen, H. (1996). The effect of ozone exposure on allergen responsiveness in subjects with asthma or rhinitis. American Journal of Respiratory and Critical Care Medicine, 153(1), 56–64.
Juhász, M. (1998). History of ragweed in Europe. In F. Th. M. Spieksma (Ed.), Ragweed in Europe (6th International Congress on Aerobiology, Satellite Symposium Proceedings, Perugia 1998, pp. 11–14). Horsholm: ALK-Abello A/S.
Karrenberg, S., Kollmann, J., & Edwards, P. J. (2002). Pollen vectors and inflorescence morphology in four species of Salix. Plant Systematics and Evolution, 235(1), 181–188.
Kasprzyk, I. (2008). Aeromycology – main research fields of interest during the last 25 years. Annals of Agricultural and Environmental Medicine, 15(1), 1–7.
Kehrl, H. R., Peden, D. B., Ball, B., Folinsbee, L. J., & Horstman, D. (1999). Increased specific airway reactivity of persons with mild allergic asthma after 7.6 hours of exposure to 0.16 ppm ozone. Journal of Allergy and Clinical Immunology, 104(6), 1198–1204.
Kilpeläinen, M., Terho, E. O., Helenius, H., & Koskenvuo, M. (2002). Childhood farm environment and asthma and sensitization in young adulthood. Allergy, 57, 1130–1135.
King, T. P., Hoffman, F., Løwenstein, H., Marsh, D. G., Platts-Mills, T., & Thomas, W. (1994). Allergen nomenclature. IUIS/WHO Allergen Nomenclature Subcommittee. Bulletin of the World Health Organization, 72, 797–806.
Korsgren, M., Andersson, M., Borga, O., Larsson, L., den-Raboisson, M., Malmqvist, U., & Greiff, L. (2007). Clinical efficacy and pharmacokinetic profiles of intranasal and oral cetirizine in a repeated allergen challenge model of allergic rhinitis. Annals of Allergy, Asthma & Immunology, 98(4), 316–321.
Krug, N., Hohlfeld, J. M., Larbig, M., Buckendahl, A., Badorrek, P., Geldmacher, H., Behnke, W., Dunkhorst, W., Luettig, B., & Koch, W. (2003). Validation of an environmental exposure unit for controlled human inhalation studies with grass pollen in patients with seasonal allergic rhinitis. Clinical and Experimental Allergy, 33(12), 1667–1674.
Laurent, J., Lafay, M., Lattanzi, B., Legall, C., & Sauvaget, J. (1993). Evidence for chestnut pollinosis in Paris. Clinical and Experimental Allergy, 23, 29–43.
Lauzurica, P., Gurbindo, C., Maruri, N., Galocha, B., Diaz, R., Gonzalez, J., Garcia, R., & Lahoz, C. (1988a). Olive (Olea europea) pollen allergens-I. Immunochemical characterization by immunoblotting, CRIE and immunodetection by a monoclonal antibody. Molecular Immunology, 25, 329–335.
Lauzurica, P., Maruri, N., Galocha, B., Gonzalez, J., Diaz, R., Palomino, P., Hernandez, D., Garcia, R., & Lahoz, C. (1988b). Olive (Olea europea) pollen allergens-II. Isolation and characterization of two major antigens. Molecular Immunology, 25, 337–344.
Ledesma, A., Villalba, M., Batanero, E., & Rodríguez, R. (1998). Molecular cloning and expression of active Ole e 3, a major allergen from olive-tree pollen and member of a novel family of Ca2 + -binding proteins (polcalcins) involved in allergy. European Journal of Biochemistry, 258, 454–459.
Lee, S. K., Yoon, S. H., Kim, S. H., Choi, J. H., & Park, H. S. (2005). Chestnut as a food allergen: Identification of major allergens. Journal of Korean Medical Science, 20(4), 573–578.
Levetin, E. (2001). Effects of climate change on airborne pollen. Journal of Allergy and Clinical Immunology, 107, 172.
Lierl, M. B., & Hornung, R. W. (2003). Relationship of outdoor air quality to pediatric asthma exacerbations. Annals of Allergy, Asthma & Immunology, 90, 28–33.
Linderholm, H. W. (2006). Growing season changes in the last century. Agricultural and Forest Meteorology, 137, 1–14.
Lipiec, A., Rapiejko, P., Samolinski, B., & Krzych, E. (2005). Correlation between conjunctival provocation test results and conjunctival symptoms in pollinosis – preliminary report. Annals of Agricultural and Environmental Medicine, 12(1), 17–20.
Lombardi, C., Penagos, M., Senna, G., Canonica, G. W., & Passalacqua, G. (2008). The clinical characteristics of respiratory allergy in immigrants in Northern Italy. International Archives of Allergy and Immunology, 147, 231–234.
Low, R. B., Bielory, L., Qureshi, A. I., Dunn, V., Stuhlmiller, D. F., & Dickey, D. A. (2006). The relation of stroke admissions to recent weather, airborne allergens, air pollution, seasons, upper respiratory infections, and asthma incidence, September 11, 2001, and day of the week. Stroke, 37(4), 951–957.
Lubitz, S., Schober, W., Pusch, G., Effner, R., Klopp, N., Behrendt, H., & Buters, J. T. (2010). Polycyclic aromatic hydrocarbons from diesel emissions exert proallergic effects in birch pollen allergic individuals through enhanced mediator release from basophils. Environmental Toxicology, 25, 188–197.
Manalai, P., Woo, J. M., & Postolache, T. T. (2009). Suicidality and montelukast. Expert Opinion on Drug Safety, 8(3), 273–282.
Mari, A., Wallner, M., & Ferreira, F. (2003). Fagales pollen sensitization in a birch-free area: A respiratory cohort survey using Fagales pollen extracts and birch recombinant allergens (rBet v 1, rBet v 2, rBet v 4). Clinical and Experimental Allergy, 33, 1419–1428.
Marsh, D., Déchamp, C., Cour, P., Bousquet, J., & Deviller, P. (1987). Study of the correlation between the atmospheric levels of the antigen Amb a 1 (Ag E) and the number of Ambrosia artemisiifolia in the Lyons area and the nearby areas. Allergie et Immunologie, 19(6), 238–243.
Matheson, E. M., Player, M. S., Mainous, A. G., King, D. E., & Everett, C. J. (2008). The association between hay fever and stroke in a cohort of middle aged and elderly adults. Journal of the American Board of Family Medicine, 21(3), 179–183.
Matthiessen, F., Ipsen, H., & Lowenstein, H. (1991). Pollen allergens. In G. D’Amato, F. Th. M. Spieksma, & S. Bonini (Eds.), Allergenic pollen and pollinosis in Europe (pp. 36–45). Oxford: Blackwell Scientific Publications.
Mitakakis, T. Z., Tovey, E. R., Xuan, W., & Marks, G. B. (2000). Personal exposure to allergenic pollen and mould spores in inland New South Wales, Australia. Clinical and Experimental Allergy, 30(12), 1733–1739.
Molfino, N. A., Wright, S. C., Katz, I., Tarlo, S., Silverman, F., McClean, P. A., Szalai, J. P., Raizenne, M., Slutsky, A. S., & Zamel, N. (1991). Effect of low concentrations of ozone on inhaled allergen responses in asthmatic subjects. The Lancet, 338(8761), 199–203.
Morgenstern, V., Zutavern, A., Cyrys, J., Brockow, I., Koletzko, S., Krämer, U., Behrendt, H., Herbarth, O., von Berg, A., Bauer, C. P., Wichmann, H.-E., Heinrich, J., Group, G. S., & Group, L. S. (2008). Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. American Journal of Respiratory and Critical Care Medicine, 177, 1331–1337.
Motta, A. C., Marliere, M., Peltre, G., Sterenberg, P. A., & Lacroix, G. (2006). Traffic-related air pollutants induce the release of allergen-containing cytoplasmic granules from grass pollen. International Archives of Allergy and Immunology, 139, 294–298.
Moverare, R., Westritschnig, K., Svensson, M., Hayek, B., Bende, M., Pauli, G., Sorva, R., Haahtela, T., Valenta, R., & Elfman, L. (2002). Different IgE reactivity profiles in birch pollen-sensitive patients from six European populations revealed by recombinant allergens: An imprint of local sensitization. International Archives of Allergy and Immunology, 128, 325–335.
Moverare, R., Kosunen, T. U., & Haahtela, T. (2006). Change in the pattern of IgE reactivity to timothy grass and birch pollen allergens over a 20-year period. Journal of Investigational Allergology and Clinical Immunology, 16, 274–278.
Namork, E., Johansen, B. V., & Lovik, M. (2006). Detection of allergens adsorbed to ambient air particles collected in four European cities. Toxicology Letters, 165, 71–78.
Negrini, A. C., Voltini, S., Troise, C., & Arobba, D. (1992). Comparison between Urticariaceae (Parietaria) pollen count and hay fever symptoms: Assessment of a “threshold-value”. Aerobiologia, 8, 325–329.
Ng, D. K., Kwok, K. I., & Chan, C. H. (2008). The association between hay fever and stroke in a cohort of middle aged and elderly adults. Journal of the American Board of Family Medicine, 21(5), 477–478.
Niederberger, V., Pauli, G., Gronlund, H., Froschl, R., Rumpold, H., Kraft, D., Valenta, R., & Spitzauer, S. (1998). Recombinant birch pollen allergens (rBet v 1 and rBet v 2) contain most of the IgE epitopes present in birch, alder, hornbeam, hazel, and oak pollen: A quantitative IgE inhibition study with sera from different populations. Journal of Allergy and Clinical Immunology, 102, 579–591.
Okuda, M., Ohkubo, K., Gotoh, M., Hiroshima, K., Ishida, Y., & Hori, K. (2005). Dynamics of airborne pollen particles from inhalation to allergic reaction in the nose. Rhinology, 43(1), 29–33.
Ostroumov, A. I. (1989). The common ragweed as a source of mass allergic diseases. Proceedings of Zoological Institute (Leningrad), 189, 230–232 (in Russian).
Papa, G., Romano, A., Quaratino, D., Di, F. M., Viola, M., Artesani, M. C., Sernia, S., Di, G. M., & Venuti, A. (2001). Prevalence of sensitization to Cupressus sempervirens: A 4-year retrospective study. Science of the Total Environment, 270, 83–87.
Pascal, L. (2009). Effets à court terme de la pollution atmosphérique sur la mortalité. Revue des Maladies Respiratoires, 26(2), 207–219.
Peat, J. K., Toelle, B. G., Dermand, J., van den Berg, R., Britton, W. J., & Woolcock, A. J. (1996). Serum IgE levels, atopy, and asthma in young adults: Results from a longitudinal cohort study. Allergy, 51, 804–810.
Pehkonen, E., & Rantio-Lehtimaki, A. (1994). Variations in airborne pollen antigenic particles caused by meteorologic factors. Allergy, 49, 472–477.
Penel, V., De Clercq, G., & Déchamp, C. (2009). Is my hair a new model of pollen trap? Ambroisie, The First International Ragweed Review, 26, 60–68.
Pereira, C., Valero, A., Loureiro, C., Davila, I., Martinez-Cocera, C., Murio, C., Rico, P., & Palomino, R. (2006). Iberian study of aeroallergens sensitisation in allergic rhinitis. European Annals of Allergy and Clinical Immunology, 38, 186–194.
Perez-Badia, R., Rapp, A., Morales, C., Sardinero, S., Galán, C., & Garcia-Mozo, H. (2010). Pollen spectrum and risk of pollen allergy in central Spain. Annals of Agricultural and Environmental Medicine, 17, 139–151.
Postolache, T. T., Stiller, J. W., Herrell, R., Goldstein, M. A., Shreeram, S. S., Zebrak, R., Thrower, C. M., Volkov, J., No, M. J., Volkov, I., Rohan, K. J., Redditt, J., Parmar, M., Mohyuddin, F., Olsen, C., Moca, M., Tonelli, L. H., Merikangas, K., & Komarow, H. D. (2005). Tree pollen peaks are associated with increased nonviolent suicide in women. Molecular Psychiatry, 10(3), 232–235.
Postolache, T. T., Lapidus, M., Sander, E. R., Langenberg, P., Hamilton, R. G., Soriano, J. J., McDonald, J. S., Furst, N., Bai, J., Scrandis, D. A., Cabassa, J. A., Stiller, J. W., Balis, T., Guzman, A., Togias, A., & Tonelli, L. H. (2007). Changes in allergy symptoms and depression scores are positively correlated in patients with recurrent mood disorders exposed to seasonal peaks in aeroallergens. The Scientific World Journal, 7, 1968–1977.
Postolache, T. T., Komarow, H., & Tonelli, L. H. (2008). Allergy: A risk factor for suicide? Current Treatment Options in Neurology, 10(5), 363–376.
Pretorius, E. (2004). Asthma medication may influence the psychological functioning of children. Medical Hypotheses, 63(3), 409–413.
Prieto, L., López, M., Bertó, J. M., & Peris, A. (1994). Modification of concentration-response curves to inhaled methacholine after the pollen season in subjects with pollen induced rhinitis. Thorax, 49(7), 711–713.
Quiralte, J., Palacios, L., Rodríguez, R., Cárdaba, B., Arias de Saavedra, J. M., Villalba, M., Florido, J. F., & Lahoz, C. (2007). Modelling diseases: The allergens of Olea europaea pollen. Journal of Investigational Allergology and Clinical Immunology, 17(suppl. 1), 76–82.
Radauer, C., Bublin, M., Wagner, S., Mari, A., & Breiteneder, H. (2008). Allergens are distributed into few protein families and possess a restricted number of biochemical functions. Journal of Allergy and Clinical Immunology, 121(847–852), e7.
Rantio-Lehtimäki, A., Koivikko, A., Kupias, R., Makinen, Y., & Pohjola, A. (1991). Significance of sampling height of airborne particles for aerobiological information. Allergy, 46(1), 68–76.
Rantio-Lehtimäki, A., Viander, M., & Koivikko, A. (1994). Airborne birch pollen antigens in different particle sizes. Clinical and Experimental Allergy, 24, 23–28.
Rapiejko, P., Stanlaewicz, W., Szczygielski, K., & Jurkiewicz, D. (2007). Threshold pollen count necessary to evoke allergic symptoms. Otolaryngologia Polska, 61(4), 591–594.
Rasmussen, A. (2002). The effects of climate change on the birch pollen season in Denmark. Aerobiologia, 18, 253–265.
Raulf-Heimsoth, M., Kespohl, S., Crespo, J. F., Rodriguez, J., Feliu, A., Brüning, Th, & Rihs, H. P. (2007). Natural rubber latex and chestnut allergy: Cross-reactivity or co-sensitization? Allergy, 62(11), 1277–1281.
Reeves, G. M., Tonelli, L. H., Anthony, B. J., & Postolache, T. T. (2007). Precipitants of adolescent suicide: Possible interaction between allergic inflammation and alcohol intake. International Journal of Adolescent Medicine and Health, 19(1), 37–43.
Riccioni, G., Della Vecchia, R., Castronuovo, M., Di Pietro, V., Spoltore, R., De Benedictis, M., Di Iorio, A., Di Gioacchino, M., & Guagnano, M. T. (2002). Bronchial hyperresponsiveness in adults with seasonal and perennial rhinitis: Is there a link for asthma and rhinitis? International Journal of Immunopathology and Pharmacology, 15, 69–74.
Riedel, F., Krämer, M., Scheibenbogen, C., & Rieger, C. H. (1988). Effects of SO2 exposure on allergic sensitization in the guinea pig. Journal of Allergy and Clinical Immunology, 82(4), 527–34.
Riediker, M., Koller, T., & Monn, C. (2000). Differences in size selective aerosol sampling for pollen allergen detection using high-volume cascade impactors. Clinical and Experimental Allergy, 30, 867–873.
Riedl, M., & Diaz-Sanchez, D. (2005). Biology of diesel exhaust effects on respiratory function. Journal of Allergy and Clinical Immunology, 115, 221–228.
Rodríguez, R., Villalba, M., Monsalve, R. I., & Batanero, E. (2001). The spectrum of olive pollen allergens. International Archives of Allergy and Immunology, 125, 185–195.
Roger, L. J., Horstman, D. H., McDonnell, W., Kehrl, H., Ives, P. J., Seal, E., Chapman, R., & Massaro, E. (1990). Pulmonary function, airway responsiveness, and respiratory symptoms in asthmatics following exercise in NO2. Toxicology and Industrial Health, 6(1), 155–171.
Rogerieux, F., Godfrin, D., Senechal, H., Motta, A. C., Marliere, M., Peltre, G., & Lacroix, G. (2007). Modifications of Phleum pratense grass pollen allergens following artificial exposure to gaseous air pollutants (O(3), NO(2), SO(2)). International Archives of Allergy and Immunology, 143, 127–134.
Rogers, C. A., Wayne, P. M., Macklin, E. A., Muilenberg, M. L., Wagner, C. J., Epstein, P. R., & Bazzaz, F. A. (2006). Interaction of the onset of spring and elevated atmospheric CO2 on ragweed (Ambrosia artemisiifolia L.) pollen production. Environmental Health Perspectives, 114, 865–869.
Rottem, M., Szyper-Kravitz, M., & Shoenfeld, Y. (2005). Atopy and asthma in migrants. International Archives of Allergy and Immunology, 136, 198–204.
Rudell, B., Sandström, T., Hammarström, U., Ledin, M. L., Hörstedt, P., & Stjernberg, N. (1994). Evaluation of an exposure setup for studying effects of diesel exhaust in humans. International Archives of Occupational and Environmental Health, 66(2), 77–83.
Schäppi, G. F., Monn, C., Wuthrich, B., & Wanner, H. U. (1996). Direct determination of allergens in ambient aerosols: Methodological aspects. International Archives of Allergy and Immunology, 110, 364–370.
Schäppi, G. F., Suphioglu, C., Taylor, P. E., & Knox, R. B. (1997). Concentrations of the major birch tree allergen Bet v 1 in pollen and respirable fine particles in the atmosphere. Journal of Allergy and Clinical Immunology, 100, 656–661.
Schäppi, G. F., Taylor, P. E., Pain, M. C., Cameron, P. A., Dent, A. W., Staff, I. A., & Suphioglu, C. (1999a). Concentrations of major grass group 5 allergens in pollen grains and atmospheric particles: Implications for hay fever and allergic asthma sufferers sensitized to grass pollen allergens. Clinical and Experimental Allergy, 29, 633–641.
Schäppi, G. F., Taylor, P. E., Staff, I. A., Rolland, J. M., & Suphioglu, C. (1999b). Immunologic significance of respirable atmospheric starch granules containing major birch allergen Bet v 1. Allergy, 54, 478–483.
Schmid-Grendelmeier, P., Peeters, A. G., Wahl, R., & Wüthrich, B. (1994). Zur Bedeutung der Eschenpollenallergie. Allergologie, 17, 535–542.
Schumacher, M. J., Griffith, R. D., & O’Rourke, M. K. (1988). Recognition of pollen and other particulate aeroantigens by immunoblot microscopy. Journal of Allergy and Clinical Immunology, 82, 608–16.
Schwela, D. (2000). Air pollution and health in urban areas. Reviews on Environmental Health, 15(1–2), 13–42.
Singer, B. D., Ziska, L. H., Frenz, D. A., Gebhard, D. E., & Straka, J. G. (2005). Increasing Amb a 1 content in common ragweed (Ambrosia artemisiifolia) pollen as a function of rising atmospheric CO2 concentration. Functional Plant Biology, 32, 667–670.
Smith, M., Emberlin, J., Stach, A., Rantio-Lehtimäki, A., Caulton, E., Thibaudon, M., Sindt, C., Jäger, S., Gehrig, R., Frenguelli, G., Jato, V., Rodríguez-Rajo, F. J., Alcazar, P., & Galán, C. (2009). Influence of the North Atlantic Oscillation on grass pollen counts in Europe. Aerobiologia, 25, 321–332.
Spieksma, F. T., Emberlin, J. C., Hjelmroos, M., Jäger, S., & Leuschner, R. M. (1995a). Atmospheric birch (Betula) pollen in Europe: Trends and fluctuations in annual quantities and the starting dates of the seasons. Grana, 34, 51–57.
Spieksma, F. T., Nikkels, B. H., & Dijkman, J. H. (1995b). Seasonal appearance of grass pollen allergen in natural, pauci-micronic aerosol of various size fractions. Relationship with airborne grass pollen concentration. Clinical and Experimental Allergy, 25, 234–239.
Stach, A., Garcia-Mozo, H., Prieto-Baena, J. C., Czarnecka-Operacz, M., Jenerowicz, D., Silny, W., & Galán, C. (2007). Prevalence of Artemisia species pollinosis in western Poland: Impact of climate change on aerobiological trends, 1995–2004. Journal of Investigational Allergology and Clinical Immunology, 17, 39–47.
Stahl, E., & Jork, H. (1964). Chemical Races in Medicinal Plants. I. Investigations on culture varieties originating from European parsley. Archiv der Pharmazie, 297, 273–281.
Sterk, P. J., Fabbri, L. M., Quanjer, P., Cockcroft, D. W., O’Byrne, P. M., Anderson, S. D., Juniper, E. F., & Malo, J. L. (1993). Airway responsiveness: Standardized challenge testing with pharmacological. Physical and sensitizing stimuli in adults. European Respiratory Journal, 6(Suppl. 16), 53–83.
Sunyer, J., Anto, J. M., Sabria, J., Roca, J., Morell, F., Rodriguez-Roisin, R., & Rodrigo, J. (1995). Relationship between serum IgE and airway responsiveness in adults with asthma. Journal of Allergy and Clinical Immunology, 95, 699–706.
Suphioglu, C. (1998). Thunderstorm asthma due to grass pollen. International Archives of Allergy and Immunology, 116, 253–260.
Swoboda, I., Jilek, A., Ferreiram, F., Engel, E., Hoffmann-Sommergruber, K., Scheiner, O., Kraft, D., Breiteneder, H., Pittenauer, E., Schmid, E., Vicente, O., Heberle-Bors, E., Ahorn, H., & Breitenbach, M. (1995). Isoforms of Bet v 1, the major birch pollen allergen, analyzed by liquid chromatography, mass spectrometry, and cDNA cloning. Journal of Biological Chemistry, 270, 2607–2613.
Taylor, P. E., Flagan, R. C., Miguel, A. G., Valenta, R., & Glovsky, M. M. (2004). Birch pollen rupture and the release of aerosols of respirable allergens. Clinical and Experimental Allergy, 34, 1591–1596.
Taylor, P. E., Jacobson, K. W., House, J. M., & Glovsky, M. (2007). Links between pollen, atopy and the asthma epidemic. International Archives of Allergy and Immunology, 144, 162–170.
Tejera, M. L., Villalba, M., Batanero, E., & Rodríguez, R. (1999). Identification, isolation, and characterization of Ole e 7, a new allergen of olive tree pollen. Journal of Allergy and Clinical Immunology, 104, 797–802.
Teranishi, H., Kenda, Y., Katoh, T., Kasuya, M., Oura, E., & Taira, H. (2000). Possible role of climate change in the pollen scatter of Japanese cedar Cryptomeria japonica in Japan. Climate Research, 14, 65–70.
Teuber, S. S., Comstock, S. S., Sathe, S. K., & Roux, K. H. (2003). Tree nut allergy. Current Allergy and Asthma Reports, 3, 54–61.
Thibaudon, M. (2003). Allergy risk associated with pollens in France. European Annals of Allergy and Clinical Immunology, 35, 170–172.
Thibaudon, M., & Lachasse, C. (2006). Alternaria, Cladosporium: Atmospheric dispersion, daily and seasonal rythmes. Revue Française d’Allergologie et d’Immunologie Clinique, 46, 188–196.
Thibaudon, M., & Sindt, C. (2008). Mesure des allergènes de pollens d’arbre dans l’air (bouleau, olivier). Revue Française d’Allergologie et d’Immunologie Clinique, 48(3), 179–186.
Thibaudon, M., Olliver, G., & Cheynel, A. (2008). L’index clinique: Outil d’évaluation de l’impact sanitaire du pollen. Environnement, Risques and Santé, 7, 411–416.
Traidl-Hoffmann, C., Kasche, A., Menzel, A., Jakob, T., Thiel, M., Ring, J., & Behrendt, H. (2003). Impact of pollen on human health: More than allergen carriers? International Archives of Allergy and Immunology, 131(1), 1–13.
Traidl-Hoffmann, C., Mariani, V., Hochrein, H., Karg, K., Wagner, H., Ring, J., Mueller, M. J., Jakob, T., & Behrendt, H. (2005). Pollen-associated phytoprostanes inhibit dendritic cell interleukin-12 production and augment T helper type 2 cell polarization. The Journal of Experimental Medicine, 201, 627–36.
Traidl-Hoffmann, C., Jakob, T., & Behrendt, H. (2009). Determinants of allergenicity. Journal of Allergy and Clinical Immunology, 123, 558–566.
Trigo, M. M., Recio, M., Toro, F. J., Caño, M., Dopazo, M. A., García, H., Sabariego, S., Ruiz, L., & Cabezudo, B. (1999). Annual variations of airborne Casuarina pollen in the Iberian Peninsula. Pollen, 10, 67–73.
Tunnicliffe, W. S., Burge, P. S., & Ayres, J. G. (1994). Effect of domestic concentrations of nitrogen dioxide on airway responses to inhaled allergen in asthmatic patients. The Lancet, 344(8939–8940), 1733–1736.
Vaidyanathan, V., Miguel, A. G., Taylor, P. E., Flagan, R. C., & Glovsky, M. M. (2006). Effects of electric fields on pollen rupture. Journal of Allergy and Clinical Immunology, 117, 157.
van der Heide, S., De Monchy, J., de Vries, K., Bruggink, T. M., & Kauffman, H. F. (1994). Seasonal variation in airway hyperresponsiveness and natural exposure to house dust mite allergens in patients with asthma. Journal of Allergy and Clinical Immunology, 93, 470–475.
Vandenplas, O., D’Alpaos, V., & Van, B. P. (2008). Rhinitis and its impact on work. Current Opinion in Allergy and Clinical Immunology, 8, 145–149.
Varela, S., Subiza, J., Subiza, J. L., Rodríguez, R., García, B., Jerez, M., Jiménez, J. A., & Panzani, R. (1997). Platanus pollen as an important cause of pollinosis. Journal of Allergy and Clinical Immunology, 6, 748–754.
Viander, M., & Koivikko, A. (1978). The seasonal symptoms of hyposensitized and untreated hay fever patients in relation to birch pollen counts: Correlations with nasal sensitivity, prick tests and RAST. Clinical Allergy, 8(4), 387–396.
Villalba, M., Batanero, E., Monsalve, R. I., González de la Peña, M. A., Lahoz, C., & Rodríguez, R. (1994). Cloning and expression of Ole e I, the major allergen from olive tree pollen. Polymorphism analysis and tissue specificity. Journal of Biological Chemistry, 269, 15217–15222.
Vinckier, S., Cadot, P., Grote, M., Ceuppens, J. L., & Smets, E. (2006). Orbicules do not significantly contribute to the allergenic micro-aerosol emitted from birch trees. Allergy, 61, 1243–1244.
Vitányi, B., Mamkra, L., Juhasz, M., Borsos, E., Béczi, R., & Szentpéteri, M. (2003). Ragweed pollen concentration in the function of meteorological elements in the south-eastern part of Hungary. Acta Climatologica Chorologica, 36–37, 121–130.
Wahl, R., Schmid-Grendelmeier, P., Cromwell, O., & Wüthrich, B. (1996). In vitro investigation of cross-reactivity between birch and ash pollen allergen extracts. Journal of Allergy and Clinical Immunology, 98, 99–106.
Waisel, Y., Mienis, Z., Kosman, E., & Geller-Bernstein, C. (2004). The partial contribution of specific airborne pollen to pollen induced allergy. Aerobiologia, 20(4), 197–208.
Waite, K. J. (1995). Blackley and the development of hay fever as a disease of civilization in the nineteenth century. Medical History, 39, 186–196.
Watson, H. K., & Constable, D. W. (1991). Allergenic significance of Plantago pollen. In G. D’Amato, F. Th. M. Spieksma, & S. Bonini (Eds.), Allergenic pollen and pollinosos in Europe (pp. 132–134). Oxford: Blackwell Scientific Publications.
Wiltshire, P. E. (2006). Hair as a source of forensic evidence in murder investigations. Forensic Science International, 163(3), 241–248.
Winkler, H., Ostrowski, R., & Wilhelm, M. (2001). Pollenbestimmungsbuch der Stiftung Deutscher Polleninformationsdienst. Paderborn: Takt Verlag.
Wopfner, N., Gadermaier, G., Egger, M., Asero, R., Ebner, C., Jahn-Schmid, B., & Ferreira, F. (2005). The spectrum of allergens in ragweed and mugwort pollen. International Archives of Allergy and Applied Immunology, 138, 337–346.
Zeghnoun, A., Ravault, C., Fabres, B., Lecadet, J., Quénel, P., Thibaudon, M., & Caillaud, D. (2005). Short-term effects of airborne pollen on the risk of allergenic rhinoconjunctivitis. Archives of Environmental & Occupational Health, 60(3), 170–176.
Ziska, L. H., & Caulfield, F. A. (2000). Rising CO2 and pollen production of common ragweed (Ambrosia artemisiifolia), a known allergy-inducing species: Implications for public health. Australian Journal of Plant Physiology, 27, 893–898.
Ziska, L. H., & Caulfield, F. A. (2000). Rising CO2 and pollen production of common ragweed (Ambrosia artemisiifolia), a known allergy-inducing species: Implications for public health. Australian Journal of Plant Physiology, 27, 893–898.
Ziska, L. H., Gebhard, D. E., Frenz, D. A., Faulkner, S., Singer, B. D., & Straka, J. G. (2003). Cities as harbingers of climate change: Common ragweed, urbanization, and public health. Journal of Allergy and Clinical Immunology, 111, 290–295.
Zureik, M., Neukirch, C., Leynaert, B., Liard, R., Bousquet, J., & Neukirch, F. (2002). Sensitisation to airborne moulds and severity of asthma: Cross sectional study from European Community respiratory health survey. British Medical Journal, 325, 411–414.
Acknowledgements
The authors acknowledge the contributions made by these persons to this chapter:
Rui Brandao1, Andreja Seliger2, Regula Gehrig3, Jean Emberlin4, Ingrida Sauliene5
1Universidade de Evora, University of Evora, Life Sciences, Area Departamental Ciências Natureza e Ambiente Biology, Largo dos Colegiais, Centro de Estudos da Mitra, P-7000 Évora, Portugal
2Institute of public health of the republic of Slovenia, Bohoričeva 15, SI-1000 Ljubljana, Croatia
3MeteoSwiss, Kraehbuehlstrasse 58, 8044 Zurich, Switzerland
4University of Worcester, Health, Social care and Psychology, National Pollen and Aerobiology Research Unit, WR2 6AJ Worcester, UK
5Siauliai university, Environmental reseach,Vilniaus St. 88,LT-76285 Siauliai, Lithuania
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
de Weger, L.A. et al. (2013). Impact of Pollen. In: Sofiev, M., Bergmann, KC. (eds) Allergenic Pollen. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-4881-1_6
Download citation
DOI: https://doi.org/10.1007/978-94-007-4881-1_6
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-4880-4
Online ISBN: 978-94-007-4881-1
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)