Abstract
Humans, like all living organisms, biosynthesize the proteins, nucleic acids, phospholipids, and many of the smaller molecules on which they depend for life functions. Their health and well-being also depend on their ability to obtain from their external chemical environments a number of compounds that they cannot synthesize, or that they cannot produce at rates sufficient to support vital functions. Thus, of the large set of bioactive compounds and metabolites called “nutrients,” some are referred to as “essential” because they must be obtained from the air (oxygen), diet and water. These include vitamins, some fatty acids, some amino acids, and several mineral elements. Foods contain essential nutrients as a result of the capacities of plants and, in some cases, food animals to synthesize and/or store them. The human body, therefore, consists of substantial amounts of mineral elements (see Table 8.1) obtained mostly from such foods. These elements ultimately come from soils and, in turn, from the parent materials from which soils are derived. Therefore, good mineral nutrition is, in part, a geologic issue.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cystic Fibrosis Transmembrane Conductance Regulator
- Mineral Element
- Phytic Acid
- Zinc Deficiency
- Enteric Absorption
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Geological Sources of Nutrients
Humans, like all living organisms, biosynthesize the proteins, nucleic acids, phospholipids, and many of the smaller molecules on which they depend for life functions. Their health and well-being also depend on their ability to obtain from their external chemical environments a number of compounds that they cannot synthesize, or that they cannot produce at rates sufficient to support vital functions. Thus, of the large set of bioactive compounds and metabolites called “nutrients,” some are referred to as “essential” because they must be obtained from the air (oxygen), diet and water. These include vitamins, some fatty acids, some amino acids, and several mineral elements.Footnote 1 Foods contain essential nutrients as a result of the capacities of plants and, in some cases, food animals to synthesize and/or store them. The human body, therefore, consists of substantial amounts of mineral elements (see Table 8.1) obtained mostly from such foods. These elements ultimately come from soils and, in turn, from the parent materials from which soils are derived. Therefore, good mineral nutrition is, in part, a geologic issue.
About 22 mineral elements are known or suspected to be essential for humans and other animals; 16 are accepted as being indispensible from diets. (see Table 8.2). Some are required in fairly large amounts, e.g., grams per kilogram of diet, and are, therefore, referred to as “macronutrients”. Others are required in much smaller amounts, e.g., microgram-to-milligrams per kilogram of diet and are referred to as “micronutrients.” At least eight mineral elements function physiologically in their simple cationic forms (Ca+2, Mg+, Na+, K+, Fe+2, Cu+2, Zn+2, and Mn+) and can, therefore, be subject to chelation by either intact proteins or a variety of small, organic molecules. Some chelates (e.g., the heme moieties of hemoglobin and myoglobin) are essential in metabolism; some (e.g., amino acids, EDTA) facilitate the absorption, transport and tissue storage of mineral ions. Others (e.g., phytic acid, oxalic acid) can interfere with the enteric absorption of certain essential mineral cations. For example, the transition metal ions (Fe+2, Cu+2 and Zn+2) form coordinate covalent bonds with ligands containing the electron-donor atoms N, S and O; Cu+2 complexes with the histidinyl imidazole-N; Zn+2 binds the cysteinyl sulfhydryl-S; and Fe+2, Cu+2 and Zn+2 can bind the aspartyl and glutamyl carboxyl-O. Three mineral elements function as anions or in anionic groupings: Cl−, PO4 −3, MoO4 −2. Unlike the other nutritionally important mineral elements, two non-metals, iodine [I] and Se, function in organic metabolites in which they are covalently bound (e.g., iodothyronine, selenocysteine). The biologic significance of these elements is a property of the particular organic species in which the element is present.
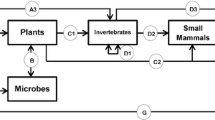
Nutritionally important mineral elements occur in soils as silicates (e.g., manganese, zinc, selenium), sulfides (e.g., zinc, selenium, copper, iron), and as the native elemental form (iron). The most abundant of these is iron, the fourth most abundant element in the Earth’s crust (see also Chap. 2, this volume). These are taken up by plants, which are consumed directly or indirectly as tissues of animals feeding of those plants. The grazing practices of many livestock allow them to harvest mineral elements over relatively large geographic areas. Nevertheless, for several mineral elements (e.g., selenium, zinc), the contents of both plant- and animal-base foods ten to reflect the mineral contents of the soils of their respective areas of production.
Water supplies are variable in their mineral contents. Most provide only small amounts of essential minerals; however, some can contribute appreciable amounts of certain mineral elements due to natural conditions (e.g., calcium, magnesium, selenium, fluoride, zinc), to intentional addition (e.g., flouride) and/or to leaching from pipes (e.g.,copper). In general, those water-borne mineral elements of greatest health import include calcium, magnesium, sodium, potassium, copper and selenium. Epidemiological studies conducted in several parts of the world have indicated an inverse relationship of water hardness and cardiovascular disease risk (WHO 2005). These benefits are thought to relate to magnesium and/or calcium, as clinical studies have found that these minerals can be effective in reducing hypertension. There is evidence that consumption of drinking water containing flouride reduces risk of dental carries, but that consumption of drinking water containing iron and copper may increase risks of heart attack.
2 Mineral Elements Needed for Good Health
Sixteen mineral elements are established as being essential for good health (Table 8.2). These, collectively, have five general physiological roles:
-
1.
Bone and membrane structure: calcium, phosphorus, magnesium, fluoride
-
2.
Water and electrolyte balance: sodium, potassium, chloride
-
3.
Metabolic catalysis: zinc, copper, selenium, magnesium, molybdenum
-
4.
Oxygen binding: iron
-
5.
Hormone effects: iodine, chromium
Although some of these functions are effected by ionic forms of minerals, many are effected by macromolecules in which minerals are bound, either covalently or otherwise. Because these are all critical life functions, the tissue levels of many nutritionally essential mineral elements tend to be regulated within certain ranges despite varying levels of intake by homeostatic control of enteric absorption and tissue storage and/or excretion. For mineral cations such as Cu+2 and Zn+2, regulation occurs primarily at the level of enteric absorption. For mineral elements that tend to be highly absorbed (e.g., selenium, boron), homeostasis is achieved by control at the level of excretion, i.e., through the urine, bile, sweat and breath. In the case of iron, access to active forms is regulated by altering the storage of the element in an inactive form, e.g., ferritin. The ability to orchestrate these physiological processes to achieve homeostatic control of cellular access to such mineral elements is an important factor in ameliorating the effects of short-term dietary deficiencies or excesses.
Calcium—The human body contains more than 1 kg of calcium 99% of which is in the skeleton where it serves as the dominant cationic component (26% of dry weight). Bone mineral consists of a complex matrix of plate-like crystals laid down by osteoblasts in or along collagen fibrils in several solid phases: hydroxyapatite (Ca10[PO4]6[OH]2), whitlockite ([Ca,Mg]3[PO4]2), amorphous Ca9(PO4)6X, octacalcium phosphate (Ca8H2[PO4]6-H2O), and brushite (CaHPO4-2[H2O]). Bone calcium is in constant turnover, with mineralization and mobilization of bone minerals occurring continually in the healthy bones of both children and adults. This “remodeling” allows the bone to serve as a source of calcium for noncalcified tissues, which mitigates against irregularities in day-to-day calcium intakes. Such homeostatic control maintains calcium in the ranges of 8.5–10.5 mgdl−1 in plasma and of 45–225 mg kg−1 intracellularly. These levels are regulated by vitamin D metabolites (e.g., 1,25-dihyroxycholecalciferol), which affect the active transport of calcium across the gut, the recovery of calcium by the renal tubule, and the remodeling of bone in processes also involving parathyroid hormone, calcitonin, and estrogen (Hollick 1994; Jones et al. 1998). Only a small fraction of intracellular calcium exists in the ionic form, Ca+2, which functions as a second messenger to signal many key cellular events, e.g., cell volume regulation, fertilization, growth-factor-induced cell proliferation, secretion, platelet activation, and muscle contraction. Therefore, a key aspect of cell regulation is the control of the release of the Ca+2 signal. In various cells, this process is thought to involve 1,4-inositoltriphosphate or nervous stimulation as triggers and protein kinase C and cyclic AMP as inhibitors (Bronner 1997). Impaired bone mineralization in young children results in deformities of the growing bones and is called rickets; in adults with formed bone it is called osteomalacia and is characterized by increase fracture risk and loss of stature. Conditions of either type can be caused by insufficient intakes of calcium, vitamin D (or exposure to sunlight which is necessary for the biosynthesis of the vitamin), phosphorus and/or magnesium. Only in very severe deficiency, when bone mineral has largely been exhausted, does calcium deficiency result in impaired nervous conduction or muscular contraction. Excessive calcium intake, which typically occurs due to the inappropriate use of calcium supplements, can lead to renal stone formation, hypercalcemia, and renal insufficiency as well as impaired utilization of iron, zinc, magnesium, and phosphorus.
Phosphorus—The human body contains approximately 700 g of phosphorus, about 85% of which is in bones where it serves a structural function in bone minerals (see also Chap. 30, this volume). Much of the nearly 14% of body phosphorus in noncalcified tissues also serves a structural function in the phospholipids that comprise plasma and subcellular membranes (Berner 1997). As phosphate, the element phosphorus is also important in metabolism because it is incorporated into nucleic acids, RNA, DNA, proteins (including transcription factors), ATP, and numerous other high-energy substrates. Intracellular phosphate serves as a regulator of glycolysis, a key pathway for rendering oxygen available to the tissues; and phosphoproteins play essential roles in the electron-transport system of mitochondria, which generates metabolically useful energy from carbohydrates and lipids. Other phosphoproteins serve as cellular growth factors and cytokines. Like calcium, phosphorus homeostasis is affected by the vitamin D hormone system. Deficiency of phosphorus (hypophosphatemia) can result in tissue hypoxia due to the loss of erythrocyte 2,3-diphosphoglucose and ATP, which leads to nervous signs (convulsions, confusion), renal dysfunction, and smooth muscle problems (e.g., dysphagia, gastric atony). Hypophosphatemia can also result in rickets and osteomalacia. Chronic, excessive intakes of phosphorus can cause hyperphosphatemia which leads to interference with calcium homeostasis, bone demineralization, and ectopic calcification of the kidney.
Magnesium—The human body typically contains 20–28 g of magnesium, which is widely distributed: 60–65% of that amount is in bone, 25–30% in muscle, and the balance is in other tissue and extracellular fluid. In fact, Mg+2 is second only to K+ as the most abundant intracellular inorganic cation. Normal plasma magnesium concentrations are in the range of 0.65–0.88 mmol L−1. Magnesium tends to be well absorbed (i.e., at rates of 67–70%) by a saturable process as well as simple diffusion. Amounts of the element not retained for tissue growth/turnover are excreted in the urine. The cation, Mg+2, functions as a cofactor in at least 300 enzymatic reactions (Shils 1997). These include virtually all kinase reactions (in which Mg+2 complexes with the negatively charged ATP−4 to form the substrate), pyrophosphotransferases, acyl-CoA synthetases, and adenylate cyclase. The cation is also involved in the regulation of ion movements within cells. Magnesium deficiency (hypomagnesemia) is characterized by neuromuscular signs (hyperactivity, muscle spasms, tremor, weakness) and gastrointestinal symptoms (anorexia, nausea, vomiting). Magnesium has a cathartic effect, but adverse effects have been identified only for magnesium ingested from non-food sources. Epidemiological studies conducted in several parts of the world have indicated an inverse relationship of water hardness and cardiovascular disease risk (WHO 2005). These benefits are thought to relate to the associated intakes of magnesium and, perhaps, calcium, which have been found in clinical studies to be effective in reducing hypertension presumably through its effects on the function of smooth muscle.
Sodium—The human body contains approximately 1.3 g of sodium, 90% of which is in the extracellular space where it serves as one of the three (with K+ and Cl−) osmotically active solutes in extracellular fluid. Sodium is freely and quantitatively absorbed, but the element is homeostatically regulated within a normal range of 135–145 mmol L−1 at the level of renal reabsorption effected by renin, angiotensin, aldosterone, antidiuretic hormone, atrial natriuretic peptide, and other factors affecting renal blood flow (Harper et al. 1997). Intracellular Na+ is normally maintained at relatively low levels. The Na+ gradient is used as an energy source for the uphill transport of a variety of solutes (e.g., amino acids, Ca+2, Mg+2, H+) into the cell. The maintenance of the Na+ gradient is maintained by several transport systems including the Na+–K+ pump which effects the ATP-dependent anti-transport of Na+ (in) and K+ (out), the Na+–H+ exchanger, Na+–K+–Cl−co-transporters, the Na+–Ca+2 exchanger, Na+–Mg+2 exchangers, and the voltage-regulated Na+ channel. Sodium deficiency results in muscle cramps, headache, poor appetite, and dehydration, but the main sign is fatigue.
Potassium—Potassium is the most abundant cation in the human body, with total body stores typically in the range of 110–150 g. In contrast to Na+, K+ is found primarily (98%) in the intracellular compartment; most cells contain about 150mMK+, while the level in extracellular fluid is only about 4 mM. Potassium is freely absorbed, with homeostasis affected by rapid renal excretion. Potassium passes the plasma membrane into cells by the Na+, K+-ATPase, the H+,K+-ATPase, the Na+–2Cl−–K+ co-transporter, and K+ conductance channels. Increases in extracellular K+ concentrations can be caused by vigorous exercise leading to K+ efflux from myocytes and mediating vasodilation and increased blood flow. Such increases stimulate the release of catecholamines and insulin, which stimulates K+ uptake via the Na+, K+-ATPase (Peterson 1997). Potassium deficiency (hypokalemia) can be caused by insufficient intake and/or excessive excretion (e.g., due to diarrhea, bulimia) of the element. This is characterized by skeletal muscular weakness; smooth muscle paralysis resulting in anorexia, nausea, vomiting, and constipation; cardiac arrhythmias; carbohydrate intolerance due to diminished insulin secretion; impaired renal function due to reduced blood flow; and altered water balance involving increased water consumption secondary to elevated angiotensin II levels.
Chloride—Chloride is the major extracellular anion maintained at a concentration of 100–110 mmol L−1 in that fluid. Like Na+, there is no control over Cl−absorption, and homeostasis is affected by renal reabsorption/elimination. The transport and cellular uptake of Cl−is effected by a number of transporters including a K+–Cl−co-transporter, a Na+–K+–2Cl−co-transporter, Cl−–HCO3 exchangers, cystic fibrosis transmembrane conductance regulator (mutation of this causes cystic fibrosis), Ca+2-activated Cl−channels, voltage-regulated Cl−channels, and mechanically activated Cl−channels (Harper et al. 1997).
Iron—The human body typically contains approximately 5 g of iron, and its metabolic function is to transport oxygen and electrons. Iron serves as the redox agent in a large number of enzymatic reactions involving substrate oxidation and reduction. These include oxidoreductases (e.g., xanthine oxidase/dehydrogenase), monooxygenases (e.g., amino acid oxidases, cytochrome P-450), and dioxygenases (e.g., amino acid dioxygenases, lipoxygenases, peroxidases, fatty acid desaturases, nitric oxide synthases) (Beard and Dawson 1997). Iron homeostasis is effected at the level of enteric absorption. Dietary iron generally exists in either heme (from hemoglobin and myoglobin in animal products) or non-heme (i.e., organic and inorganic salts in plant-based and iron-fortified foods) forms, each of which is absorbed by a different mechanism. Heme iron is much better absorbed and less affected by enhancers and inhibitors of absorption than non-heme iron, which is strongly regulated by the intestinal mucosal cells in response to iron stores and blood hemoglobin status. Thus, iron-adequate men and women typically absorb about 6 and 13% of dietary iron, respectively, with non-heme iron absorption as great as 50% under conditions of severe iron-deficiency anemia. Excess absorbed iron is stored as ferritin and hemosiderin in the liver, reticuloendothelial cells, and bone marrow. The loss of iron from the body is very low, about 0.6 mg per day, and is primarily due to losses in the bile and exfoliated mucosal cells eliminated in the feces. Menstrual losses can be significant, as can nonphysiological losses resulting from parasitism, diarrhea, and enteritis, which are thought to account for half of the cases of global iron-deficiency anemia. Iron deficiency is manifested as hypochromic, normocytic anemia; lethargy; apathy; listlessness; fatigue; impaired non-shivering thermogenesis; impaired immune function; impaired cognitive development; and reduced physical performance. In pregnancy, iron-deficiency increases the risk of premature delivery, low birth weight, and infant and maternal mortality.
Epidemiologic observations have linked high dietary iron intakes or high iron stores with increased risk of coronary heart disease (Salonen et al. 1992). The toxic potential of iron arises from its pro-oxidative effects, which yield reactive oxygen species that attack polyunsaturated membrane lipids, proteins, and nucleic acids. An iron-overload disease, hereditary hemochromatosis, is caused by a defect in the regulation of iron absorption, which leads to very high circulating transferrin iron. Clinical signs appear when body iron accumulates to about tenfold excess of normal: these include hepatic cirrhosis, diabetes, heart failure, arthritis, and sexual dysfunction.
Zinc—The human body contains 2–2.5 g of zinc: just over half (55%) of which is in muscle, 30% in bone, with the balance distributed in other tissues. Zinc is absorbed by both carrier-mediated and simple diffusion processes which render the element only moderately absorbed (about 30%) at nutritionally adequate intakes and more efficiently absorbed under deficient conditions (Chesters 1997). Both processes can be effected by the presence of chelating substances that may promote (e.g., meats) or impair (e.g., phytic acid) zinc absorption. Zinc homeostasis is also affected by the regulation of zinc excretion/reabsorption in and from pancreatic and intestinal secretions; urinary losses of zinc are low and not generally responsive to changes in zinc intake. Plasma zinc levels, comprising 0.1% of total body zinc, are not regulated and are therefore not indicative of overall zinc status except under conditions of marked deficiency. Zinc has been shown to function in at least 50 widely varied enzymes. In each, the element serves either in a catalytic (i.e., at the active site), a co-catalytic (i.e., near the active site), or a structural role bound most commonly to histidinyl, glutamyl, or aspartyl residues. Zinc deficiency is manifested as losses in activities of at least some zinc enzymes (e.g., some dehydrogenases, alkaline phosphatase, superoxide dismutase), although direct links between such losses and the physiologic manifestations of zinc deficiency have not been established. Zinc deficiency is characterized by poor growth and dwarfism, anorexia, parakeratotic skin lesions, diarrhea, impaired testicular development, impaired immune function (including wound healing), and impaired cognitive function. Low zinc status is also thought to increase risk to osteoporosis and susceptibility to oxidative stress. Very high intakes of zinc, which have occurred due to inappropriate use of zinc supplements, can interfere with copper metabolism and deplete the body of copper. Chronic exposure to excess zinc (>100 mg d−1) can reduce immune function and HDL cholesterol.
Copper—The human body contains approximately 120 mg of copper, which is widely distributed in many tissues and fluids at mg kg−1 or μg kg−1 concentrations. Copper serves as a cofactor for a number of oxidase enzymes including lysyl oxidase, ferroxidase (ceruloplasmin), dopamine beta-monooxygenase, tyrosinase, alpha-amidating monooxygenase, cytochrome c oxidase, and superoxide dismutase (Harris 1997). These enzymes are involved in generating oxidative energy, stabilizing connective tissue matrices, maintaining iron in the ferrous (Fe+2) state, synthesizing neurotransmitters, pigmenting hair and skin, supporting immune competence, and protecting the body from reactive oxygen species. Copper also functions non-enzymatically in angiogenesis, neurohormone release, oxygen transport, and the regulation of genetic expression. Copper homeostasis is effected at the level of enteric absorption. It is absorbed by facilitated diffusion (involving either specific transporters or nonspecific divalent metal ion transporters on the brush-border surface) and is transported to the liver where it is re-secreted into the plasma bound to ceruloplasmin. The element is excreted in the bile; only very small amounts are lost in the urine. Copper absorption/retention varies inversely with the level of copper intake, and tends to be moderate (e.g., 50–60%) even at low copper intakes. Copper deficiency is manifested as hypochromic, normocytic or macrocytic anemia; bone abnormalities resembling osteoporosis or scurvy; increased susceptibility to infection; and poor growth. The ingestion of high amounts of copper can cause nausea. Chronic high copper intake can lead to the hepatic accumulation of copper, which has been suspected in juvenile cases of hepatic cirrhosis in India. There is evidence that consumption of drinking water containing copper may increase risks of heart attack.
Iodine—The human body contains approximately 5 mg of iodine, which functions only in the iodine-containing thyroid hormones. These include the tetraiodinated protein thyroxine (T4) that is converted by a single deiodination to yield the active thyroid hormone triiodothyronine (T3). The latter functions as a regulator of growth and development by increasing energy (ATP) production and activating or inhibiting the synthesis of various proteins (Hetzel and Wellby 1997). Organic forms of iodine are converted in the upper gastrointestinal tract to the iodide anion (I−), which is rapidly and almost completely absorbed. In contrast, when T3 is ingested, about 80% is absorbed intact. Absorbed I−circulates in the plasma in the free ionic form and is rapidly removed by the thyroid and kidney. Iodine homeostasis is effected at the level of the kidney, and urinary excretion is the major route of loss (comprising 90% of iodine absorbed by iodine-adequate individuals). The deiodination of T4 occurs in the thyroid, skeletal muscles, and brain, but the thyroid gland is the only storage site for iodine where it appears mostly as mono- and diiodotyrosine and T4, with a small amount of T3. Iodine deficiency in adults is characterized as thyroid hypertrophy or goiter and in children as myxedematous cretinism. Collectively, these iodine deficiency diseases comprise a global health problem, and cretinism is the greatest source of preventable mental retardation (see also Chap. 17, this volume).
Selenium—The human body typically contains approximately 20 mg of selenium. This is widely distributed in all tissues in each of which the element present almost exclusively bound to proteins. Genomic analyses have revealed selenium to be an essential constituent of a relatively small number of proteins of which contain the element in the form of selenocysteine (Kryukov et al. 2003). That amino acid is found only in the selenproteins, as it is incorporated co-translationally by a process signaled by TGA in DNA (UGA in mRNA), which in the synthesis of other proteins functions as a stop codon. Humans have 25 selenoproteins. These include multiple isoforms of glutathione peroxidase, thioredoxin reductase and iodothyronine 5′-deiodinase; the selenium-transporter, selenoprotein P; an enzyme involved in SeCys synthesis, selenophosphate synthase; and others of uncharacterized function. In these selenoproteins, selenium functions in antioxidant protections, redox regulation, and thyroid hormone regulation. When selenium is consumed as selenomethionine (SeMet), the dominant form in plant foods, other proteins can incorporate that form nonspecifically, due to its mimicry with methionine. The non-specific presence of selenium in proteins comprises the dominant portion of tissue selenium, although apparently without physiological significance. Because foods contain both of these selenoaminoacids (selenomethionine in plant tissues; both selenocyteine and selemethionine in animal tissues), in human tissues typically contain both the specific and nonspecific selenoproteins. It is not clear whether selenium deficiency not accompanied by other deficiencies or oxidative stress results in significant physiological impairment. Severely low selenium intakes (greater than 20 μg d−1) have been associated with juvenile cardiomyopathy in China (Keshan disease); but that disease also appears to have a viral component to its etiology.
Recent interest in selenium centers around the apparent efficacy of supranutritional intakes to reduce cancer risk. A decade-long, randomized, double-blind, placebo-controlled clinical intervention trial found that supplementation of free-living American adults with 200 μg d−1 selenium (in addition to their normal diets) reduced major cancer incidence by half or more (Clark et al. 1996) if their baseline intakes did not exceed ca. 100 μg d−1. Studies with animal models have demonstrated similar protective effects of selenium intakes greater than those required to support maximal expression of selenoenzymes. Current thinking is that these effects are due to a methylated metabolite of selenium (Jackson and Combs 2011). Selenium intakes greater than 1 mg d−1 can induce dermatological changes, including brittle hair and nails. Chronic intakes approaching 5 mg has been reported to lead to skin rash, paresthesia, weakness, and diarrhea (see also Chap. 16, this volume).
Manganese—Manganese functions as a cofactor for enzymes in antioxidant defense (mitochondrial superoxide dismutase), gluconeogenesis (pyruvate carboxylase, phosphoenol–pyruvate carboxykinase), glycoprotein biosynthesis (glycosyl transferases), nitrogen metabolism (arginase, glutamine synthase), and cholesterol biosynthesis (farnesyl pyrophosphate synthetase). Little is known about the mechanisms of absorption, transport, or cellular uptake of manganese, although the element is widely distributed in noncalcified tissues with the greatest concentrations in the liver (Leach and Harris 1997). The greatest route of manganese excretion appears to be the bile in which it is released in bound form. There is little available evidence of manganese deficiency in humans, although studies in experimental animals have shown effects on fetal survival, normal skeletal development (i.e., shortened limbs, twisted legs, lameness), ataxia, glucose tolerance, and hepatic steatosis.
Molybdenum—Molybdenum functions as the active center of three enzymes that catalyze oxidative hydroxylations: sulfite oxidase (the last step in the degradation of sulfur amino acids), xanthine dehydrogenase, and aldehyde oxidase (which transfers electrons to other redox cofactors and, ultimately, to cytochrome c, molecular oxygen, or NAD+). In these enzymes, the element is found in a pterin-containing, molybdenum cofactor, the synthesis of which in eukaryotes remains poorly understood (Johnson 1997). Molybdenum appears to be efficiently absorbed at all levels of intake, apparently by a passive process. It is transported in the blood attached to proteins in erythrocytes. Whole blood molybdenum levels vary directly with dietary molybdenum intake, although plasma Mo+ levels are maintained at about 5 nmolL−1. Molybdenum is widely distributed in the body, with greatest concentrations in liver, kidney, adrenal gland, and bone. One human case of molybdenum deficiency has been described; signs (all of which responded to molybdenum therapy) included tachycardia, tachypnea, severe headache, night blindness, nausea, and vomiting.
Chromium—Chromium potentiates the action of insulin and has been shown to restore glucose tolerance in malnourished infants. Several studies have shown that chromium supplementation lowers circulating glucose levels, increases plasma insulin, and produces a favorable profile of plasma lipids (Offenbacher et al. 1997). It has been suggested that these effects may be due to a low molecular weight chromium-binding substance that may amplify insulin receptor tyrosine kinase activity in response to insulin. Chromium can also bind to one of the binding sites of transferrin, and it has been proposed that excessive iron storage in hemochromatosis may interfere with the transport of chromium to contribute to the diabetes associated with that disorder. The enteric absorption of the element, which is absorbed as Cr+3, is very low (usually no more than 2%) and appears to be regulated. Absorbed chromium accumulates in the liver, kidney, spleen, and bone.
Fluoride—Fluoride is the ionic form of fluorine. It is very highly electronegative and reacts reversibly to hydrogen to form hydrogen fluoride which freely diffuses across the intestine, dissolves in the blood, and is taken up by the tissues where its high affinity for calcium causes it to accumulate in calcified tissues. Fluoride can stimulate new bone formation; when present in oral fluids, F−exerts cariostatic effects due to enhanced remineralization of dental enamel and reduced acid production of plaque bacteria (Chow 1990; Cerklewski 1997). Prior to the widespread use of F−in dental products and water supplies, most studies showed that the incidence of dental caries (in both children and adults) was 40–60% lower in areas with drinking water F− concentrations of at least 0.7 mgL−1 when compared to communities with lower F−levels. Excessive F− intake can cause fluorosis of the enamel and bone. Although the former is a largely cosmetic effect involving the mottling of the teeth, skeletal fluorosis is associated with joint stiffness, calcification of ligaments, and some osteosclerosis of the pelvis and vertebrae (see also Chap. 13, this volume).
3 Dietary Sources of Essential Mineral Elements
Mineral elements are metabolized and, to varying degrees, stored by plants and animals, some of which constitute important sources of those elements in human diets (see Table 8.3). That the mineral elements are not homogeneously distributed among various types of foods is clear: few foods other than dairy products are rich in calcium; sea foods constitute the best sources of iodine and chloride; meats are the most important sources of iron; and protein-rich foods comprise the best sources of zinc, copper, and selenium. Therefore, optimal mineral nutrition, like optimal nutrition in general, is most likely to be obtained from mixed diets based on a diverse selection of foods. Conversely, the monotonous, non-diverse, grain-based diets accessible to the poor of the developing world are likely to provide insufficient energy, protein, and minerals, especially calcium, copper, selenium, and biologically available iron and zinc. At the same time, the increasing use in industrialized countries of non-diverse eating habits is associated with prevalent insufficient intake of such minerals as calcium.
For many people in industrialized countries, fortified foods and nutritional supplements constitute important sources of several of the mineral elements. Various forms of copper, zinc, iron, and selenium are offered in over-the-counter formations, both as individual supplements as well as compounded in multivitamin mineral supplements. Calcium, typically as the carbonate or gluconate salts, is now commonly used to fortify orange and other fruit juices. Consumer response to such nutrient-fortified foods has been very strong, and this aspect of consumer retailing is expected to continue to grow.
Soils can contribute to the total dietary intake of mineral elements. This can occur through adherent soil particles on foods and suspended soil particles in drinking and cooking water, as well as through the direct consumption of soil. The latter practice of geophagia can be deliberate in some communities in which the eating of clays occurs (see Chap. 18 “Geophagy and the Involuntary Ingestion of Soil”, this volume). Consumption of clays with high cation-exchange capacities can provide substantial supplements of calcium, iron, copper, zinc, and manganese; other clays can interfere with the enteric absorption of iron and zinc. Consumption of iron-rich lateritic soils can provide enough iron to impair the utilization of copper and zinc.
Water supplies are variable in their mineral contents. In some areas, fresh water supplies can provide nutritionally important amounts of such minerals as calcium, magnesium, iron and manganese, and industrialized countries have used municipal water as a vehicle for providing fluoride. Municipal systems handling “soft”, i.e., low-mineral water, can have appreciable amounts of copper due to leaching from pipes. In a few locales surface runoff from selenium-rich soils has been found to contain biologically significant amounts of selenium, but such cases are rare and most water supplies are very low in that nutrient. The contributions of water-borne minerals to nutritional status depend also on the rate of water consumption, which is also highly variable, depending on behavior and environmental conditions. Individuals with the greatest intakes of water include those engaged in strenuous physical activity, residents of hot climates, and (relatively) infants.
4 Mineral Element Bioavailability
For several nutrients only a portion of the ingested amount is absorbed and utilized metabolically. Therefore, it is necessary to consider this when evaluating the nutritional adequacy of foods and diets. This concept, bioavailability, is particularly important in mineral nutrition, because some foods are less useful sources of essential minerals than might be expected from their absolute mineral content.
Mineral bioavailability depends on both physiological and exogenous factors. Physiological determinants of mineral bioavailability include:
-
1.
Age-related declines in the efficiency of enteric absorption of copper and zinc
-
2.
Early postnatal lack of regulation of absorption of iron, zinc, and chromium
-
3.
Adaptive increases in the absorptive efficiencies of iron and zinc, copper, manganese, and chromium by receptor upregulation during periods of deficiency
-
4.
Dependence on other nutrients for the physiological functions of selenium and iodine in thyroid hormone metabolism, and copper and iron in catecholamine metabolism
-
5.
Anabolic effects on tissue sequestration of zinc and selenium
-
6.
Catabolic effects on zinc, selenium, and chromium losses
The absorption and post-absorptive utilization of ingested minerals can be affected by other factors in foods and diets. For example, 25–30% of the heme iron in animal tissues can be absorbed, while only 2–5% of the iron in plant foods is absorbed. The utilization of plant sources of iron can be markedly improved by including in the diet sources of ascorbic acid (e.g., oranges) or meats, both of which promote the utilization of non-heme iron. Similarly, citrate and/or histidine can enhance the absorption of dietary zinc. Dietary ascorbate (vitamin C) can also enhance the antagonistic effect of iron on copper utilization.
Mineral bioavailability can be reduced by dietary factors that reduce enteric absorption. For example, phytate, phosphorus, and triglycerides can each reduce the luminal solubility and, hence, the absorption of calcium. Phytate and other non-fermentable fiber components can bind zinc and magnesium, reducing the absorption of each. Sulfides can reduce the absorption of copper by similar means. Minerals that share transporters can be mutually inhibitory for absorption, e.g., sulfite and selenite, cadmium and zinc, and zinc and copper.
In general, problems related to poor bioavailability are greatest for iron in plant-based containing phytates and/or polyphenols but there are few problems with promotor substances. For calcium there are problems with bioavailability when poorly soluble forms are consumed with vegetables (spinach, rhubarb, beet greens, chard) containing inhibitory oxalates without others (artichokes) containing fructose oligosaccharide promoters; for zinc in diets high in unrefined (>90% extraction), unfermented cereal grains or high-phytate soy products, especially those fortified with inorganic calcium salts; and for selenium consumed as plant foods (containing SeMet much of which is diverted to protein synthesis as a methionine analog). Accordingly, the utilization of these minerals as consumed in most diets tends to be moderate at best, though in each case it can be markedly enhanced through appropriate dietary choices.
5 Quantitative Estimates of Mineral Needs and Safe Exposures
Dietary standards have been set for several, but not all, of the nutritionally essential mineral elements. International standards have been developed for only some minerals (FAO-WHO 2002) (Table 8.4). The most current and extensive standards are the Dietary Reference Intakes (DRSs) published by the U.S. National Academy of Science (NAS) (Food and Nutrition Board 1997, 2000, 2001) (Table 8.5). It is important to note that the expert panels of the respective organizations used the same primary data, i.e., the published scientific literature. Also, each based its recommendations on estimates of individual physiological need (i.e., the World Health Organization’s “basal requirement” and the “recommended dietary allowance,” RDA, from NAS) which was then inflated to accommodate estimated inter-individual variation. This approach produced the WHO “normative requirement” and NAS “estimated average requirement” (EAR). The NAS process went further to include estimates of “average intakes” (AIs) in cases where data were not sufficient to support EARs or RDAs. Both groups also estimated safe limits of exposure: WHO created “upper limits of safe ranges of population mean intakes” (Table 8.6), and NAS created “upper tolerable limits” (ULs) (Table 8.7).
6 Clinical Assessment of Mineral Status
The status assessment of the essential minerals, which vary so much in metabolic function, homeostatic regulation, and tissue distribution, calls for a mixed approach. This approach includes elemental analyses of tissues and/or body fluids, assays of mineral-dependent enzyme activities, and measurement of functional and/or morphological indices. A battery of such tests may be feasible in research settings, but in clinical settings practicality and timeliness dictate approaches based on analyses of a single specimen of blood.
Beyond the obvious issues pertaining to sampling (i.e., number, bias, amount, homogeneity, interindividual variability, etc.), the analysis of minerals, particularly those present in only trace amounts in foods and tissues, calls for special attention to sample integrity and freedom from contamination (Milne 2000). For example, the iron and zinc contents of plasma or serum can be affected by hemolysis; rubber stoppers and borosilicate glass can contaminate blood with zinc and boron, respectively; and some anticoagulants can produce osmotic shifts that release several elements from erythrocytes. The laboratory, too, can be a significant source of contamination: poorly treated water can contaminate with iron, calcium, magnesium, manganese, zinc, or copper; stainless steel surfaces can contaminate with chromium and nickel; and dust, paper products, wood, skin, hair, and dandruff can also be sources of contamination. For these reasons, a well-monitored laboratory designed for mineral/trace element analyses is a prerequisite for the generation of useful data.
The available methods for the clinical assessment of mineral status are presented in Table 8.8, with normative values for the most practically useful of these presented in Table 8.9.
Status with respect to mineral elements that are active or highly regulated in circulating tissues can be assessed by analyzing their amounts in plasma/serum or blood cells (Sauberlich 1999). For example, knowledge of plasma/serum potassium or erythrocyte iron levels can be highly informative, because those elements exert their physiological functions in those respective compartments. This is not the case for mineral elements that function in other compartments and/or chemical forms. For example, analyses of chromium, copper, or selenium in serum/plasma have inferential value for assessing status only to the extent that those values correlate with the sizes/activities of other physiologically relevant pools. For elements that are not highly regulated in the blood, such as zinc, that parameter has limited, if any, value in assessing status in all except severely deficient individuals.
For mineral elements such as selenium, iodine, zinc, and copper, which exert their physiological functions as essential constituents of macromolecules, assessment of status calls for measurement of the levels/activities of their respective functional forms or metabolite profiles. Thus, zinc adequacy can be determined on the basis of the cytosolic superoxide dismutase, and iodine adequacy can be determined on the basis of circulating levels of triiodothyronine (T3), thyroid hormone (T4), and thyroid-stimulating hormone (TSH). Similarly, plasma selenium, because it consists of several components including nonfunctional selenium bound nonspecifically in albumin and other proteins, is best assessed in cases of subadequacy by determining the selenoproteins-extracellular glutathione peroxidase and selenoprotein P.
7 Ecological Aspects of Mineral Nutrition
Because the mineral elements are ultimately derived from soils, the mineral status of humans and other animals depends on the minerals available in the soils upon which their foods were grown and through which their drinking and cooking waters drained (see Table 8.3). Therefore, it is not surprising that mineral nutritional status can vary geographically, particularly in cases where the soil-water-plant-animal linkages are fairly direct as in the cases of grazing animals and people in highly localized food systems. Such cases have been described for iodine, copper, zinc, selenium, molybdenum, manganese, iron, boron, and cobalt (see Table 8.10). Soil mineral deficiencies can involve intrinsically low mineral contents of soils (e.g., selenium), inefficient uptake by crops (e.g., zinc deficiency in calcareous soils), and excessive leaching (e.g., iodine, zinc). In at least two general cases, Keshan disease and the iodine deficiency diseases goiter and myxedematous cretinism, endemic distributions of a disease are directly related to the geographic patterns of soil deficiencies in selenium and iodine, respectively. Interregional and international transshipment of foods can be expected to mitigate against such local soil effects, particularly in industrialized countries (see also Chap. 16, this volume).
Nutritionally important mineral elements occur in soils as silicates (e.g., manganese, zinc, selenium), sulfides (e.g., zinc, selenium, copper, iron), and as the native elemental form (iron). The most abundant of these is iron, the fourth most abundant element in the Earth’s crust (see also Chap. 2, this volume). These are taken up by plants, which are consumed directly or indirectly as tissues of animals feeding of those plants. The grazing practices of many livestock allow them to harvest mineral elements over relatively large geographic areas. Nevertheless, for several mineral elements (e.g., selenium, zinc), the contents of both plant- and animal-base foods ten to reflect the mineral contents of the soils of their respective areas of production.
Water supplies are variable in their mineral contents. Most provide only small amounts of essential minerals; however, some can contribute appreciable amounts of certain mineral elements due to natural conditions (e.g., calcium, magnesium, selenium, fluoride, zinc), to intentional addition (e.g., flouride) and/or to leaching from pipes (e.g., copper). The contributions of water-borne minerals to nutritional status depend also on the rate of water consumption, which is also highly variable, depending on behavior and environmental conditions. Individuals with the greatest intakes of water include those engaged in strenuous physical activity, residents of hot climates, and (relatively) infants. In general, those water-borne mineral elements of greatest health import include calcium, magnesium, sodium, potassium, copper and selenium. Epidemiological studies conducted in several parts of the world have indicated an inverse relationship of water hardness and cardiovascular disease risk (WHO 2005). These benefits are thought to relate to magnesium and/or calcium, as clinical studies have found that these minerals can be effective in reducing hypertension. There is evidence that consumption of drinking water containing flouride reduces risk of dental carries, but that consumption of drinking water containing iron and copper may increase risks of heart attack.
8 Summary
Minerals play essential roles in the normal metabolism and physiological functions of animals and humans. Some (calcium, phosphorus, magnesium, fluoride) are required for structural functions in bone and membranes. Some (sodium, potassium, chloride) are required for the maintenance of water and electrolyte balance in cells. Some (zinc, copper, selenium, manganese, molybdenum) are essential constituents of enzymes or serve as carriers (iron) for ligands essential in metabolism. Some serve as essential components of a hormone (iodine) or hormone-like factor (chromium).
Unlike other essential nutrients, the mineral elements cannot be derived from the biosynthesis of food plants or animals–they must be obtained from soils and pass through food systems to humans in food forms. For this reason, local deficiencies of minerals in soils can produce deficiencies in local food systems which clinically impact the people dependent on those systems. The development of international trade and interregional transportation of foods has ameliorated the impact of such local mineral deficiencies. However, cases still occur in areas where the transshipment of food and, thus, the diversity of the diet are limited.
See Also the Following Chapters
Chapter 3 (Natural Distribution and Abundance of Elements) • Chapter 6 (Uptake of Elements from a Biological Point of View) • Chapter 9 (Biological Responses of Elements) • Chapter 16 (Selenium Deficiency and Toxicity in the Environment) • Chapter 17 (Soils and Iodine Deficiency) • Chapter 27 (Speciation of Trace Elements) • Chapter 28 (Mineralogy of Bones)
Notes
- 1.
This term refers to bioactive elements other than C, H and O that can be obtained from the earth.
Further Reading
Beard JL, Dawson HD (1997) Phosphorus. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 275–334, chap. 3
Berner YN (1997) Phosphorus. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 63–92, chap. 3
Bogden JD, Klevay LM (eds) (2000) Clinical nutrition of the essential trace elements and minerals. The guide for health professionals. Humana Press, Totowa
Bronner F (1997) Calcium. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral element. Marcel Dekker, New York, pp 13–61, chap. 2
Cerklewski FL (1997) Fluorine. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 583–602, chap. 20
Chesters JK (1997) Zinc. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 185–230, chap. 7
Chow LC (1990) Tooth-bound fluoride and dental caries. J Dent Res 69:595–600
Clark LC, Combs GF Jr, Turnbull BW, Slate E, Alberts D, Abele D, Allison R, Bradshaw R, Chalker D, Chow J, Curtis D, Dalen J, Davis L, Deal R, Dellasega M, Glover R, Graham G, Gross E, Hendrix J, Herlong J, Knight F, Krongrad A, Lesher J, Moore J, Park K, Rice J, Rogers A, Sanders B, Schurman B, Smith C, Smith E, Taylor J, Woodward J (1996) The nutritional prevention of cancer with selenium 1983–1993: a randomized clinical trial. J Am Med Assoc 276:1957–1963
Combs GF Jr (2001) Selenium in global food systems. Br J Nutr 85:517–547
FAO-WHO (2002) Human vitamin and mineral requirements: report of a joint FAO/WHO expert consultation. Food and Agricultural Organization of the United Nations, World Health Organization, Rome
Food and Nutrition Board (1989) Recommended dietary allowances, 10th edn. National Academy Press, Washington, DC
Food and Nutrition Board (1997) Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D and fluoride. National Academy Press, Washington, DC
Food and Nutrition Board (2000) Dietary reference intakes for vitamin C, vitamin E, selenium and carotenoids. National Academy Press, Washington, DC
Food and Nutrition Board (2001) Dietary reference intakes for vitamin a, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium and zinc. National Academy Press, Washington, DC
Harper ME, Willis JS, Patrick J (1997) Sodium and chloride in nutrition. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 93–116, chap. 4
Harris ED (1997) Copper. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 231–273, chap. 3
Hetzel BS, Wellby ML (1997) Iodine. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 557–581, chap. 19
Hollick MF (1994) Vitamin D–New horizons for the 21st century. Am J Clin Nutr 60:619–630
Jackson MI, Combs GF Jr (2008) Selenium and anticarcinogenesis: underlying mechanisms. Curr Opin Clin Nutr Metab Care 11:718–726
Jackson MI, Combs GF Jr (2011) Selenium as a cancer preventive agent. In: Hatfield DL, Berry MJ, Gladyshev N (eds) Selenium: its molecular biology and role in human health. Springer, New York, pp 313–324, chapter 24
Johnson JL (1997) Molybdenum. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 413–438, chap. 13
Jones G, Strugnell RA, DeLuca HF (1998) Current understanding of the molecular actions of vitamin D. Physiol Rev 78:1193–1231
Kryukov GV, Castellano S, Novoselov SV, Lobanov AV, Zehtab O, Guigo R, Gladyshev VN (2003) Characterization of mammalian selenoproteins. Science 300:1439–1443
Kubota J, Allaway WH (1972) Geographic distribution of trace element problems. In: Mortvedt JJ, Giodano PM, Lindsay WL (eds) Micronutrients in agriculture. Soil Science Society of America, Madison, pp 525–554
Leach RM Jr, Harris ED (1997) Manganese. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 335–355, chap. 10
Milne DB (2000) Laboratory assessment of trace element and mineral status. In: Clinical nutrition of the essential trace elements and minerals: the guide for health professionals. Humana Press, Totowa, pp 69–90
Offenbacher EG, Pi-Sunyer FX, Stoeker BJ (1997) Chromium. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 389–411, chap. 12
Peterson LN (1997) Potassium in nutrition. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 153–183, chap. 6
Salonen JT, Nyyssonen K, Korpela H, Tuomilehto J, Seppanen R, Salonen R (1992) High stored iron levels are associated with excess risk of myocardial infarction in eastern Finnish Men. Circulation 86:803–811
Sauberlich HE (1999) Laboratory tests for the assessment of nutritional status, 2nd edn. CRC Press, Boca Raton
Shils ME (1997) Magnesium. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 117–152, chap. 5
Sunde RA (1997) Selenium. In: O’Dell BL, Sunde RA (eds) Handbook of nutritionally essential mineral elements. Marcel Dekker, New York, pp 493–556, chap. 18
WHO (1996) Trace elements in human nutrition and health. World Health Organization, Geneva
WHO (2005) Nutrients in drinking water. World Health Organization, Geneva, 186 pp
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Combs, G.F. (2013). Geological Impacts on Nutrition. In: Selinus, O. (eds) Essentials of Medical Geology. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-4375-5_8
Download citation
DOI: https://doi.org/10.1007/978-94-007-4375-5_8
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-4374-8
Online ISBN: 978-94-007-4375-5
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)