Abstract
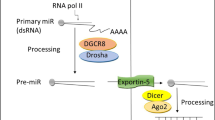
Pancreatic ductal adenocarcinoma (PDAC) is the fourth cause of death by cancer in Western countries. Its poor prognosis is primarily explained by a lack of early diagnostic markers and efficient therapeutic treatments. PDAC does not appear de novo but rather originates of an accumulation of genetic and epigenetic alterations that leads to an aberrant production of diverse molecules such as RNA and proteins. These altered expression profiles result in a multi-step progression of precursor lesions to invasive PDAC. Therefore, a better understanding of the early genetic and epigenetic alterations occurring in PDAC development is valuable for diagnostic and new therapeutic strategies. MicroRNAs (miRNAs) are small endogenous RNA molecules that function as translation inhibitors of messenger RNA by binding to their 3′ untranslated region. These molecules are tightly involved in the regulation of many physiological processes such as development, proliferation, invasion, and apoptosis among others. Their expressions are profoundly altered in PDAC and are strongly involved in PDAC carcinogenesis. In this chapter, we describe the miRNAs for which the expression is altered in PDAC and PDAC pre-neoplastic lesions. We outline the different molecular mechanisms that lead to altered miRNA expression in PDAC cells as well as the signaling pathways affected in response to altered miRNA expression. Lastly, we review the potential interests of miRNA as biological markers and therapeutic tools for PDAC.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
13.1 Introduction
Pancreatic ductal adenocarcinoma (PDAC) is the fourth cause of death by cancer in Western countries with a 5-year survival rate of ~6% (Jemal et al. 2010). This poor prognosis is frequently explained by lack of early symptoms, of early diagnostic markers and of efficient therapeutic treatments. The vast majority of patients with PDAC displays locally or advanced distant metastasis, which renders their disease surgically inoperable. Moreover, PDAC is highly resistant to cytotoxic chemotherapy and ionizing radiation (Safioleas and Moulakakis 2004).
PDAC does not develop de novo. It takes origin from an accumulation of genetic and epigenetic alterations in ductal pancreatic cells that result in altered expression of different molecules (RNA, proteins) (Torrisani and Buscail 2002). These altered expression patterns lead to a multi-step progression from pre-neoplastic lesions to invasive PDAC. Pancreatic intraepithelial neoplasia (PanIN) and intraductal papillary mucinous neoplasia (IPMN) are the most common pre-neoplastic lesions of PDAC. Both lesions affect pancreatic ducts. Therefore, a better understanding of the early genetic and epigenetic events governing PDAC development is valuable for diagnostic and new therapeutic strategies.
Many genetic and epigenetic alterations have been described in PDAC and pre-neoplastic lesions. The most frequent genetic mutations in PDAC is mutations of the oncogene K-RAS (Kirsten RAS). These activating mutations occur in 60–80% of patients with PDAC (Torrisani and Buscail 2002). Moreover, multiple molecular events (chromosomal alterations, point mutations, DNA hypermethylation, etc… ) are responsible for the inactivation of tumor suppressor genes such p16, Smad/DPC-4 (Mothers against decapentaplegic homolog 4/Deleted in pancreatic cancer 4), TP 53 (TP53), among others during PDAC development. These different alterations are also present in variable proportions in pre-neoplastic lesions (Feldmann et al. 2007).
Altered expression of microRNA (miRNA) was described in PDAC and pre-neoplastic lesions. MiRNA expression profiles were demonstrated to provide a precise classification of cancers from different origins (Lu et al. 2005; Volinia et al. 2006). In addition, expression of specific miRNAs can correlate with clinicopathological features of cancers (Lu et al. 2005).
In this chapter, we will list the miRNAs for which the expression is altered in PDAC and in PDAC pre-neoplastic lesions. We will describe the different molecular mechanisms that lead to their altered expression in PDAC cells. The functional consequences of miRNA altered expression will be also described. Finally, we will discuss the potential interests in microRNAs as biological markers and therapeutic tools for PDAC.
13.2 MiRNAs Differentially Expressed in PDAC
MiRNA expression profiles are specific for each cell types, and these profiles are profoundly altered in cancer cells (Calin and Croce 2006). Interestingly, the altered profiles are in fact specific for different tumor cell type. This specificity, therefore, allows for the classification of tumors depending on their organ of origin. qRT-PCR and the development of microarray technologies allow the simultaneous measurement of several hundred miRNAs and for the identification of miRNAs that are differentially expressed in PDAC when compared to normal pancreas or other pancreatic pathologies (Seux et al. 2008).
The first study on miRNA expression in PDAC determined the expression level of 222 miRNA precursors in 28 PDAC samples as compared to 15 adjacent benign tissues and 6 normal pancreases (Lee et al. 2007). This initial study revealed that one hundred miRNA precursors are aberrantly expressed in PDAC and that most of them display an increased expression in the tumors (Table 13.1). MiR-221, miR-100, miR-21 and miR-155 are among the most abundantly expressed in pancreatic tumors. Soon after, by use of miRNA microarray technologies, the expression of 326 miRNAs were measured in 65 microdissected PDAC samples and compared to adjacent pancreatic tissues (Bloomston et al. 2007). This analysis revealed that 30 miRNAs are over-expressed in PDAC whereas three were down-regulated (miR-148a, miR-148b and miR-375) (Table 13.1). When PDAC samples are compared with those from chronic pancreatitis, 15 miRNAs were over-expressed and 8 were under-expressed in PDAC. Meanwhile, Hahn’s group established the first pancreatic miRNAome by comparing the data from normal pancreas and a reference set of 33 human tissues. This miRNA microarray analysis revealed that most miRNAs have similar expression in both sample sets; and many miRNAs known to be highly expressed in all tissue types such as miR-16, miR-21 and let-7 family members, are also very abundant in pancreas. Nevertheless, several miRNAs such as miR-148a, miR-200a,b,c, miR-216, miR-217 and miR-375 are evidently enriched in pancreas (Szafranska et al. 2007). In parallel, the comparison of 377 miRNA expression of five normal pancreases and eight PDAC revealed that 41 miRNAs are down-regulated and 32 are up-regulated at least twofold (Table 13.1). Among them, the miR-148a, miR-148b, miR-216 and miR-217 are down-regulated more than five folds in PDAC whereas miR-155 and miR-196a are robustly enriched. Similar results were further observed from PDAC biopsy samples (Szafranska et al. 2008). Moreover, the over-expression of miR-196a in PDAC was confirmed after microdissection of PDAC, healthy ductal cells and acinar cells.
Following these large scale miRNA analysis, other groups have focused on specific miRNAs in PDAC. Indeed, profiling analysis of 95 miRNA chosen for their potential functions related to cancer biology lead to the identification of eight miRNA that are significantly up-regulated in PDAC when compared to adjacent tissues (miR-196a, miR -190, miR-186, miR -221, miR-222, miR-200b, miR-15b and miR-95) (Zhang et al. 2009).
MiR-21, one of the most often up-regulated miRNA in human cancer is also commonly over-expressed in the vast majority of miR expression studies on PDAC samples (Dillhoff et al. 2008; Giovannetti et al. 2010; Moriyama et al. 2009; Zhu et al. 2009). Similarly, miR-155, miR-221, miR-222, miR-196a are also frequently found over-expressed in PDAC (Bloomston et al. 2007; Lee et al. 2007; Szafranska et al. 2007). Recently, an increased expression of miR-200a, b and c was reported in PDAC and PDAC derived cell lines (Li et al. 2010a; Yu et al. 2010a).
Although most deregulated miRNAs are indeed due to an over-expression in PDAC, a specific subset of miRNAs are down-regulated in tumors. Among them, miR-148a is frequently down-regulated in tumor samples (Bloomston et al. 2007; Hanoun et al. 2010; Szafranska et al. 2007). MiR-34a for which the transcription is activated by the protein TP53 was found to be down-regulated in 15/15 PDAC-derived cell lines when compared to hPNE (human Pancreatic Nestion-positive Epithelial) and hPDE (human pancreatic ductal epithelial) cell lines (Chang et al.2007). Similar results were also observed in MiaPACA-2 and BxPC-3 cell lines (Lodygin et al. 2008). Reduced expression of the let-7 miRNA family was also reported in PDAC samples (Bloomston et al. 2007; Torrisani et al. 2009). More recently, down-regulation of miR-146 was measured in PANC-1 when compared to hPDE control cell lines (Li et al. 2010b). Although microarray and qRT-PCR approaches are now usually used, miRNA expression can also be evaluated by in situ hybridization (ISH) or by Northern blot as recently reported the down-regulation of miR-20a and miR-96 in PDAC, respectively (Yan et al. 2010; Yu et al. 2010b).
Altogether, the plethora of studies emerging from numerous scientific groups show a number of miRNA that is undoubtedly deregulated in PDAC samples (Table 13.1). This collection of miRNAs could serve as the basis for future studies.
13.3 MiRNA Expression Profiles in PDAC Precursor Lesions
As described earlier, altered expression of miRNA is commonly encountered in PDAC samples. However, alteration of miRNA expression in pre-neoplastic lesions is less documented. Several precursor lesions of PDAC have been described. These include PanIN, intraductal papillary mucinous neoplasms (IPMN) and mucinous cystic neoplasms (Hruban and Adsay 2009). To date, miRNA expression patterns have been explored only in PanIN and IPMN lesions.
13.3.1 PanIN
PanIN lesions are the most common non-invasive precursor to invasive PDAC. PanINs are microscopic lesions that are categorized into three histological stages (PanIN-1A/B, PanIN-2, and PanIN-3) based on the increasing degrees of architectural and nuclear atypia. Several murine models for pancreatic carcinogenesis have been established to mimic this pancreatic cancer progression (Hingorani et al. 2003; Hruban et al. 2000; Maitra and Hruban 2008). The expression of three miRNAs, miR-21, miR-155 and miR-221 was measured in microdissected human PanIN lesions (Ryu et al.). A significant over-expression of miR-155 was measured at stage PanIN-2 when compared to non-neoplastic ductal epithelium and confirmed by ISH. Over-expression of miR-21 was only observed at stage PanIN-3. No difference in miR-221 levels was observed between normal epithelium and PanIN lesions. A similar study from our group determined the expression of seven miRNAs (miR-21, miR-221, miR-222, let-7a, miR-29c, miR-200 and miR-205) in murine and human PanIN (du Rieu et al. 2010). Globally, our study revealed that miR-21, miR-205 and miR-200 expression parallels PanIN progression in a KRAS (G12D) mouse model (Hruban et al. 2001) (Fig. 13.1). Moreover, this study further demonstrates that the expression of miR-21, miR-221 and miR-222 increases with human PanIN grade, with a peak of expression in hyperplastic PanIN-2/3 lesions. A recent study from our group demonstrated a down-regulation of the miRNA-148a in murine and human microdissected PanIN lesions (Hanoun et al. 2010) (Fig. 13.1).
13.3.2 Intraductal Papillary Mucinous Neoplasm (IPMN)
IPMN are large (usually > 1 cm) non-invasive mucin-producing epithelial neoplasms that arise in the larger pancreatic ducts (Hruban and Adsay 2009). IPMNs can be a precursor to invasive adenocarcinoma of the pancreas. So far, only one study has evaluated the expression of miRNAs in this type of lesion. Relative expression of 12 miRNAs elevated in PDAC were assessed from 15 non-invasive IPMN (miR-21, miR-155, miR-107, miR-223, miR-181a, miR-181c, miR-221, miR-210, miR-16, miR-100, miR-15a and miR-17-5p) (Habbe et al. 2009). These studies revealed that, except for miR-15a and miR-17-5p, the remaining 10 miRNAs reach a significant over-expression in IPMN. MiR-155 and miR-21 display the highest relative fold changes in these lesions. Their expression was evaluated by ISH in a panel of 64 archival IPMN. MiR-155 and miR-21 expression is elevated in 83 and 81% of IPMN compare to normal ducts, respectively.
Altogether, these studies on PDAC precursor lesions clearly demonstrate that alteration of miRNA expression is an early event in PDAC and therefore advocate a role for microRNA in PDAC initiation and progression.
13.4 Molecular Mechanisms Responsible for Altered MiRNA Expression
Several molecular mechanisms responsible for altered miRNA expression in cancers have been described. Some of which were described in PDAC or PDAC-derived cell lines.
13.4.1 Chromosomal Alterations
Chromosomal alterations (deletions, amplifications) are responsible for the loss- or gain- of miRNA expression in cancers. For example, miR-15 and miR-16 are located at chromosome 13q14, a region deleted in more than half of B cell chronic lymphocytic leukemias (Calin et al. 2002). Thus far, there are no major chromosomal alterations that lead to miRNA misexpression described in PDAC.
13.4.2 Transcription Factor Defects
Deregulated expression or function of transcription factors occurs frequently in cancers. One example is the transcription factor c-Myc which is pathologically activated in human malignancies. The predominant consequence of this activation is a widespread repression of miRNA expression (Chang et al. 2008). Although the protein TP53 was shown to activate miR-34a promoter, the loss of expression/function of this protein cannot completely explain for the loss of miR-34a expression observed in PDAC (Chang et al. 2007; Lodygin et al. 2008).
13.4.3 Epigenetic Alterations
DNA hypermethylation, a major epigenetic alteration, is responsible for silencing numerous tumor suppressor genes in cancer (Bird 1996). It was recently shown that this epigenetic alteration can affect miRNA expression (Saito et al. 2006). A number of examples for epigenetic alterations are described in PDAC samples or PDAC-derived cell lines. In fact, the miR-34 promoter is hypermethylated in 3 out 19 PDAC-derived cell lines (Lodygin et al. 2008). Moreover, the treatment of MiaPACA-2 and PANC-1 cell lines with the DNA demethylating agent 5-aza-deoxycytidine, and the histone deacetylase inhibitor, Trichostatin A, demonstrated that 14 miRNA are induced by at least two fold. Among them, miR-107, miR-103, miR-29a,b and miR-320 are up-regulated in both cell lines (Lee et al. 2009). More recently, we have shown that the DNA region encoding miR-148a is hypermethylated in 10/14 PDAC samples when compared to non-pathological adjacent tissues. We further demonstrated that this hypermethylation is inversely correlated with miR-148a expression (Fig. 13.2) (Hanoun et al. 2010).
Methylation level of miR-148a coding region in endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) biopsies from patients with chronic pancreatitis (PC) and pancreatic ductal adenocarcinoma (PDAC). DNA methylation level of miR-148a coding region as determined by quantitative methylation specific PCR (qMS-PCR) from EUS-FNA-extracted DNA of 20 patients with proven PC and 39 patients with proven PDAC (Hanoun et al. 2010)
Conversely, DNA hypomethylation of genomic sequences can be responsible for the over-expression of multiple genes in PDAC (Sato et al. 2003). Recently, Goggins and colleagues identified two members of miR-200 family, miR-200a and miR-200b that are over-expressed in PDAC, and for which the DNA coding region is hypomethylated (Li et al. 2010a).
Histone modifications are also implicated in the regulation of miRNA expression (Scott et al. 2006). In the PDAC-derived BxPC-3 cells, treatment with Trichostatin A, a potent histone deacetylase inhibitor, was shown to down-regulate 24 miRNAs and to up-regulate 5 miRNAs (Zhang et al. 2008). Among them, the miR-200c is up-regulated and miR-21 is down-regulated.
13.4.4 Exogenous Stimulation of MiRNA Expression
Several exogenous stimuli/compounds that modify miRNA expression have been reported in cancers. For example, treatment of PDAC BxPC-3 cells with curcumin (diferuloylmethane), a naturally occurring flavonoid displays anti-cancer, anti-oxidant, anti-inflammatory, anti-proliferative and pro-apoptotic activities, alters the expression profiles of miRNAs (Sun et al. 2008). Eleven miRNAs are significantly up-regulated whereas 18 are down-regulated. Among those up-regulated, miR-22 targets SP1 transcription factor and ESR1 (estrogen receptor 1) mRNAs. Another study showed that in PANC-1 cells, the isoflavones B-DIM or G2535 decrease the expression of miR-146a (Li et al. 2010b).
13.4.5 Hypoxia
Hypoxic conditions are frequently encountered in solid tumors. Recent studies demonstrate that such conditions can modify miRNA expression patterns (Crosby et al. 2009). MiR-210 is shown to be strongly induced in hypoxic conditions in several types of cancer (Mathew and Simon 2009). Therefore, it is not surprising that an induction of miR-210 expression by hypoxic condition was also described in PDAC-derived cell lines as well as in vivo (Huang et al. 2009). These findings have been complemented with analyses of miR-210 promoter sequences showing that it is controlled by HIF1alpha by a hypoxia responsive element (HRE).
13.4.6 Genetic Mutations in MiRNA Genes
Even though mutations in the genomic sequences encoding for miRNA would, in theory, not modify their expression level, such mutations were reported in both PDAC tissues and PDAC-derived cell lines (Zhu et al. 2009). Four mutations were identified in miR-155 and miR-21 genes. Although the two mutations of miR-21 did not affect the promoter activity of this gene, findings for a mutation (A-to-G at 29 nt) downstream of pre-miR-21 resulted in a conformational change of the DNA secondary structure close to the stem reaching into the pre-miR-21 that led to a relative reduction of the mature miR-21 expression in vivo.
13.5 Role of MiRNAs in Pancreatic Cancer Development and Metastasis
The consequence of altered miRNA expression in cancer cells is the deregulation of targeted mRNAs. These changes result in an aberrant translation of proteins involved in the control of several cellular processes.
13.5.1 Cell Proliferation and Tumor Growth
The oncogene K-RAS is mutated in 60–80% of PDAC and; thus considered as a potential marker and target for PDAC treatment. Interestingly, let-7 miRNA family targets K-RAS protein expression in human cancer cells (Morris and McManus 2005). We showed that the restoration of let-7 level in Capan-1 PDAC cells strongly inhibit their proliferation in vitro but we failed to impede tumor growth progression following intra-tumoral gene transfer (Torrisani et al. 2009). Nevertheless, Watanabe et al. (2009) reported that the transfection of let-7 inhibitors or the let-7 clusters does not influence the proliferation rate of AsPC-1 or PANC-1 cells that endogenously express this miRNA. MiR-21 is largely implicated in the control of proliferation in various cancer cell lines. Similarly, it was reported that in PDAC cells, transfection with miR-21 precursor significantly increases their proliferation (Giovannetti et al. 2010; Moriyama et al. 2009). As mentioned earlier, miR-34 expression is reduced in PDAC cells (Chang et al. 2007; Lodygin et al. 2008). Lodygin et al. (2008) showed its involvement in the control of cell proliferation. Indeed, they demonstrated that the restoration of miR-34 in MiaPACA-2 cells suppresses colony formation and decreases the percentage of cells in S phase by directly targeting the cyclin dependent kinase 6 (CDK6). These proliferative effects induced by the restoration of miR-34 were later confirmed by other groups (Ji et al. 2009; Kent et al. 2009). Xu’s group further showed that miR-34 restoration also inhibits tumor-sphere growth in vitro and tumor formation in vivo. Similarly, it was reported that an enforced expression of miR-107 in PANC-1 and MiaPACA-2 down-regulates in vitro growth and represses the expression of a putative target CDK 6 (Lee et al. 2009). Using PDAC SU86.86 cells, the stable ectopic expression of miR-210, which is highly induced in hypoxic conditions, delays the tumor growth when subcutaneously implanted into nude mice (Huang et al. 2009). Interestingly, miR-210 expression has little consequence on angiogenesis, proliferation and apoptosis. Nonetheless, the inhibitory effect of miR-210 on tumor growth initiation is partially rescued by expressing the homeobox protein A1 (HOXA1) and fibroblast growth factor receptor-like 1 (FGFRL1) coding sequence without 3′UTR. Furthermore, lentiviral over-expression of miR-20a was recently reported to result in anti-proliferative effects in vitro and in vivo. These findings were attributed to miR-20a functions associated with an increased percentage of cells in G0/G1 phase and with an post-transcriptional regulation of the protein signal transducer and activator of transcription 3 (STAT3) (Yan et al. 2010). More recently, an ectopic over-expression of miR-200c was shown to increase PDAC cell proliferation (Yu et al. 2010a). Inversely, the transient and stable over-expression of miR-96, which directly targets the oncogene K-RAS, inhibits proliferation of MiaPCACA-2 and PANC-1 cells in vitro and in vivo (Yu et al. 2010b).
13.5.2 Epithelial-mesenchymal Transition (EMT), Invasion, and Metastatic Behavior
Invasion and metastasis of carcinoma is promoted by the activation of the embryonic EMT program, which triggers cellular mobility and subsequent dissemination of tumor cells. Several miRNAs have been involved in EMT transition, invasive capacity and metastatic behavior of PDAC cells. Burk et al. (2008) demonstrated that miR-200c and miR-141 are strong inducers of epithelial phenotype. They showed that the over-expression of both miRNAs results in the induction of the epithelial differentiation of PANC-1 cells. Watanabe et al. (2009) demonstrated that the high-mobility group A protein 2 (HMGA2), a non-histone chromatin factor, is strongly involved in EMT maintenance in PDAC cells. However, they showed that although the let-7 family directly targets the 3′UTR of HMGA1, 2 and K-RAS mRNAs, these miRNAs do not inhibit EMT in PDAC cells that have endogenous let-7 expression. MiRNA expression profiles were compared between gemcitabine-resistant and -sensitive PDAC cell lines. Interestingly, it was reported that the expression of miR-200b, miR-200c, let -7b, -7c, -7d and -7e is significantly reduced in gemcitabine-resistant cells that display EMT characteristics (Li et al. 2009). Moreover, transfection of miR-200 results in the reversal of EMT phenotype leading to epithelial morphology.
13.5.2.1 Invasion
MiR-21 is involved in invasive capacity of PDAC cells. Transfection with the pre-miR-21 markedly increases PANC-1 cell invasion by indirectly mediating matrix metalloproteinase MMP-2 and MMP-9 expression (Moriyama et al. 2009). On the other hand, restoration of miR-34 expression in PDAC cells was showed to inhibit their invasion (Ji et al. 2009). Low expression of miR-146a was reported in PDAC cells when compared with normal pancreatic duct epithelial cells (Li et al. 2010b). The same study further demonstrated that the re-expression of miR-146a inhibits the invasive capacity of PDAC cells with concomitant down-regulation of epidermal growth factor (EGFR) and the NF-κB regulatory kinase interleukin 1 receptor-associated kinase 1 (IRAK-1). In the same way, the transfection of the high invasive PANC-1 cells with the precursor of miR-29a reduces their capacity of invasion as determined by use of the Boyden chamber in vitro invasion assay (Muniyappa et al. 2009). More recently, high levels of miR-200c as measured in 15 PDAC cell lines was correlated with low invasion ability (Yu et al. 2010a). Similarly, miR-96 displays inhibitory effects of migration and invasion of PDAC cells as lately reported by Yu et al. (2010b).
13.5.2.2 Metastatic Behavior
MiRNA participate in the metastatic behavior of PDAC cells. Indeed, sixteen human PDAC cell lines were orthopically xenografted in a murine PDAC model and classified in three hierarchical groups according to their metastatic potential. CD40 was detected as a relevant target for differentially expressed miRNA in the highly metastatic group. A significant over-expression of CD40-related miR-224 and miR-486 was measured in this group, which was correlated with reduced expression of CD40 protein levels (Mees et al. 2009). Using the same approach, the authors observed a significant induction of EP300 (E1A binding protein p300) targeting miRNA in the high metastatic group (miR-194, miR-200b, miR-200c, and miR-429) (Mees et al. 2010). MiR-200 family members (miR-141, miR-200a, b and c, and miR-429) induce epithelial differentiation, thereby suppressing EMT by inhibiting translation of the EMT-activators zinc finger E-box-binding homeobox (ZEB)1 and ZEB2 transcription factor. Wellner et al. (2009) by use of PDAC cells showed that ZEB1 not only promotes tumor cell dissemination but it is also necessary for the tumor initiating capacity. The authors further showed that ZEB1 represses the expression of miR-203, known to inhibit stem-cell identity, and that candidate targets of the miR-200 family are also stem cell factors; such as sex determining region Y-box 2 (SOX 2) and Krüppel like factor 4 (KLF4). What is more, miR-200c, miR-203, and miR-183 cooperate to suppress expression of stem cell factors. MiR-10a was identified as an important mediator of metastasis formation in pancreatic tumor cells (Weiss et al. 2009). The authors observed an increased expression of miR-10a in metastatic PDAC. They also demonstrated that miR-10a promotes metastatic behavior of PDAC cells and inversely, that repression of miR-10a was sufficient to inhibit invasion and metastasis formation. These effects were presumed mediated by the inhibition of the proteins HOXB1 and HOXB3. Over-expression of miR-200a and miR-200b were shown to regulate smad interacting protein (SIP) expression, which is transcriptional repressor of E-cadherin. However, even if over-expression of miR-200a/200b induces E-cadherin in PDAC cell lines, it was incapable of reversing the EMT morphology (Yan et al. 2010). More recently, the over-expression of miR-20a in PDAC cell lines was shown to inhibit the protein STAT-3 translation and consequently reduced the invasive capacity of these cells and metastatic properties of the generated tumors (Yan et al. 2010). By targeting STAT-3, miR-20a over-expression can suppress MMP-2 and VEGF expression; two important players in EMT.
13.5.3 Apoptosis and Sensitivity to Anti-cancer Agents
MiRNAs also play important roles in the control of apoptotic processes and in the sensitivity of PDAC cells to anti-cancer agents. Several examples for miRNA controlled apoptosis exist. For example, Chang et al. (2007) showed that miR-34 is an important component of the tumor protein 53 (TP53) transcriptional networks. Re-expression of miR-34 promotes apoptosis by repressing the expression of the anti-apoptotic protein, B cell lymphoma 2 (BCL2). These results were complemented by Xu and colleagues who showed that, in addition to inducing apoptosis, miR-34 restoration sensitizes PDAC cells to chemotherapy and radiation (Ji et al. 2009). In contrast, Dusetti’s group elegantly demonstrated that miR-155, which is up-regulated in PDAC (Bloomston et al. 2007; Lee et al. 2007; Szafranska et al. 2007), controls the expression of TP53-induced nuclear protein, a potent pro-apoptotic protein (Gironella et al. 2007). Moreover, Capan-2 cells transfected with an anti-miR-155 oligonucleotide demonstrated with a significant increase in apoptosis. In the same way, the ectopic expression of miR-96, for which expression is decreased in PDAC, induces cell death by apoptosis resulting from a decreased phosphorylation of Bcl-associated death (BAD) protein (Yu et al. 2010b). The transfection with miR-21 was shown to decrease the sensitivity to gemcitabine treatment of PANC-1 cells (Moriyama et al. 2009). These findings were recently confirmed by demonstrating that the addition of phosphoinositide 3-kinase (PI3K) inhibitors and mammalian target of rapamycin (mTOR) resulted in a decrease of phosphoprotein kinase B/Akt; and prevented miR-21-induced resistance to the pro-apoptotic effects of gemcitabine (Giovannetti et al. 2010). Inversely, the transfection of miR-200b increases the gemcitabine sensitivity of MiaPACA-2 cells (Li et al. 2009).
13.6 Potential Interests in MiRNAs as Biomarkers for PDAC
Molecular markers are still required to help alleviate PDAC prognosis. Progress must be made for the characterization of large scale diagnostic markers, and for differential markers to distinguish PDAC from other pancreatic diseases such as pseudo-tumorous pancreatitis (Bournet et al. 2009). Also, the ability to predict whether a patient will respond to therapy early in the treatment may be of particular value to stratify and individualize patient treatment strategies. In addition, a validated shorter term surrogate end point would reduce the treatment follow-up period in an attempt to prevent unnecessary disease progression, and ultimately reduce drug development costs through the more rapid completion of randomized controlled Phase III trials. A recent study effectively demonstrated the robust stability of miRNAs, even from human tissues and cell samples for which reliable mRNA analyses are commonly inapplicable (Jung et al. 2010). Therefore, this robust stability confers to miRNAs a great interest as molecular biomarkers for PDAC.
13.6.1 MiRNAs as Diagnostic Marker
Due to their robust stability, the interest in miRNAs as potential diagnostic markers for PDAC was reported in different types of biological samples (resected tumors, biopsies, blood samples).
Several attempts were made to establish a miRNA signature for PDAC. Schmittgen’s group was the first to report the expression profile of miRNA in PDAC resected tissues. In this pioneering study, the authors demonstrated that the PAM algorithm based on miRNA expression was able to correctly classified 28/28 tumors, 6/6 normal pancreas and 11 of 15 adjacent benign tissues (Lee et al. 2007). Expression profiles of miRNAs are also very informative not only to discriminate tumor type from the normal pancreas, but also for the differential diagnosis of chronic pancreatitis. Using miRNA microarrays on surgically removed PDAC, normal pancreas and chronic pancreatitis tissues, Bloomston et al. (2007) reported that 15 over-expressed and 8 under-expressed miRNAs can differentiate pancreatic cancer from chronic pancreatitis with an accuracy of 93%. In another study, Szafranska et al. (2007) showed a clear discrimination between PDAC, chronic pancreatitis and normal pancreas can be achieved by use of a subset of 20 miRNAs. These studies showed that neoplastic and non-neoplastic tissues can be secernated. As mentioned earlier, miR-21 expression is strongly increased in PDAC. It was shown that 79% of the PDAC samples demonstrated strong staining by ISH, compared to 8% of begin pancreas and to 27% of chronic pancreatitis (Dillhoff et al. 2008). Interestingly, none of the non-cancerous tissues demonstrated strong miR-21 staining. Endoscopic ultrasound (EUS) has become an essential modality in diagnosis and management of pancreatic malignancies. Gene expression analysis in EUS-guided fine needle aspirations (FNA) material is now possible on a routine basis. Szafranska (2008) reported that miRNA altered expression can be measured in PDAC FNA samples and that the combination of miR-196a and miR-217 expression can segregate PDAC samples from other pancreatic disease samples. We recently demonstrated that let-7 expression is repressed in the same type of PDAC samples. We also showed that the measurement of hypermethylation of miR-148a encoding DNA region from FNA samples can serve as a useful diagnostic tool to differentiate PDAC and pseudo-tumor forms of chronic pancreatitis (Hanoun et al. 2010) (Fig. 13.2).
Recently, the discovery of miRNAs in serum establishes the possibility of using miRNAs as biomarkers of disease. Wang et al. (2009) were the first to report the detection of miRNA in the blood of PDAC patients. Indeed, miRNA profiling in plasma can differentiate PDAC patients from healthy controls. Of importance, analyses of plasma levels revealed a 64% sensitivity and 89% specificity for a panel of four miRNAs (miR-21, miR-210, miR-196a, and miR-155). In a recent study, miRNA expression was measured by qRT-PCR in plasma of 2 different cohorts of patients with PDAC and compared to an age-matched control cohort. The authors demonstrated that circulating miR-210 level is significantly more elevated in PDAC patients and may potentially serve as a useful biomarker for PDAC diagnosis (Ho et al.). Lastly, Li et al. (2010a) demonstrated that both miR-200a and miR-200b were significantly elevated in the sera of PDAC and chronic pancreatitis patients compared with healthy controls.
13.6.2 MiRNAs as Prognostic Markers
One main reason for the poor survival rate associated to PDAC is that only a small fraction of patients (~15%) are diagnosed while they have small, surgically resectable cancers. Thus, there is considerable interest in identifying reliable prognostic markers, especially for the vast majority (85%) of patients that can undergo surgery due to a locally advanced or metastatic disease state.
In studies conducted from resected tissues, Bloomston et al. (2007) reported that the SAM application identified 6 miRNAs that were differentially over-expressed in patients with a longer survival rates (greater than 2 years) (miR-452, miR-105, miR-127, miR-518a-2, miR-187, and miR-30a-3p). Moreover, 2 miRNAs were of considerable interest. First, tumors with high expression of miR-196a-2 have a median survival of 14.3 months compared with 26.5 months for those with low expression. Second, the median survival in patients with high expression of miR-219 was 13.6 months compared with 23.8 for those with low expression whereas no correlation was found with increased expression of TP53 (31/54), loss of p16 expression (49/56) and lost of SMAD4/DPC4 expression (39/56). In another study, Greither et al. (2010) measured the expression of miR-155, miR-200, miR-203, and miR-205 in 56 microdissected PDAC samples and showed that elevated expression of these miRNAs is associated with poorer survival rates. Additionally, this study demonstrated that patients with tumors presenting with elevated levels of all 4 miRNAs retained a 6.2-fold increased risk of tumor-related death compared to patients whose tumors expressed a lower expression of these miRNAs. As mentioned earlier, strong expression of miR-21 in PDAC was reported in a plethora of studies. Although its strong expression in cancer does not correlate with tumor size, differentiation, nodal status or T stage, it predicts limited survival in patients with node-negative (Dillhoff et al. 2008). It is of interest that these results differ from those from Tanaka’s group, which observed no correlation between miR-21 expression and prognosis or other clinicopathologic features (Moriyama et al. 2009). More recently, by use of microdissected tissues, Giovannetti et al. (2010) found that patients with high miR-21 expression have a significantly shorter overall survival both in metastatic and adjuvant settings. Multivariate analysis confirmed the prognostic significance of miR-21 expression. The same group recently published that low miR-21 expression is associated with benefiting from adjuvant treatment in two independent cohorts of PDAC cases (Hwang et al. 2010). Lastly, Yu et al. (2010a) investigated the relationship between E-cadherin and miR-200c expression in a panel of 14 PDAC cell lines and in macrodissected formalin-fixed paraffin-embedded (FFPE) tissue samples obtained from 99 patients who underwent pancreatectomy. The authors reported that patients with high levels of miR-200c expression manifest with a significantly better survival rate as compared to those with low levels of miR-200c expression.
13.7 Potential Interests in MiRNAs as Therapeutic Tool for PDAC
It is now well established that miRNAs play pivotal roles in diverse processes involved in cancer, such as differentiation, control of cell proliferation and death, stress response and metabolism. As such, the activation of tumor-suppressive miRNAs and/or the inhibition of oncogenic miRNAs by small molecules or gene transfer may potentially provide a fundamental approach for the development of cancer therapeutics.
To date, most of the approaches used to control miRNA expression are based on the use of synthetic mimics or small interfering RNAs. Tsuda et al. (2006) reported that synthetic miRNA designed to target glioma-associated antigen 1 transcription factor inhibits division and induces late apoptosis in pancreatic tumor cells. In another study, miR-21 and miR-221 antisense oligonucleotides were demonstrated to inhibit PDAC cell proliferation (cell cycle arrest in G1) and increases their sensitivity to gemcitabine treatment (Moriyama et al. 2009; Park et al. 2009). Down-regulation of proliferation-inducing miRNA can also be triggered by external stimuli. Weiss et al. (2009) reported that miR-10a expression promotes metastatic behavior of PDAC-derived cells and that repression of miR-10a is sufficient to inhibit invasion and metastasis formation. Interestingly, the authors found that miR-10a is targeted by retinoid acid and that retinoic acid receptor antagonists effectively repress miR-10a expression and fully block metastasis. On the other hand, miR-34 enforced expression by mimics or lentiviral transduction inhibits invasion, promotes apoptosis and cell cycle arrest. As a result, treated cells are more sensitive to chemotherapy and radiation. Following a similar strategy, Li et al. (2010b) demonstrated that increasing cellular miR-146a content using mimics or the natural products 3,3′-diinodolylmethane (DIM) or isoflavone, inhibited the invasive capacity of PDAC-derived cells with concomitant down-regulation of EGFR and the NF-kappaB regulatory kinase interleukin 1 receptor-associated kinase 1 (IRAK-1). We recently demonstrated that restoring let-7 expression strongly affects the proliferation of a PDAC-derived cell line (Torrisani et al. 2009). Unfortunately, we failed to antagonize in vivo pancreatic tumors growth using the same approach by delivering let-7. Akin to our findings, Watanabe et al. (2009) suggested that ectopically expressed let-7 miRNAs may not evidently have a therapeutic role in PDAC cells that originally express let-7.
13.8 Perspectives and Challenges
MiRNAs have proven effective for PDAC classification, prognostic stratification and drug-response prediction. These small but potent molecular markers can be detected and quantified not only in frozen tissues, but also in FFPE tissues, as well as serum/plasma samples. Whether this will translate into clinical application is still highly debated. Nevertheless, circulating miRNAs are expected to be proven as specific and sensitive for PDAC as compared to current biomarkers and therefore raise promising perspectives for PDAC detection. Concerning the use of miRNA as anti-cancer targets or molecules for PDAC in vivo, the efficiency of these approaches is still to be demonstrated. In vivo use of so called antagomirs may be an opportunity to achieve significant down regulation of oncomirs in solid tumors. However, cell targeting and distribution of miRs by this approach remains challenging. This issue may be resolved by the intratumoral transduction of tumors using targeted viral vectors encoding for pro- or anti-miRNA.
References
Bird AP. The relationship of DNA methylation to cancer. Cancer Surv. 1996;28:87–101.
Bloomston M, Frankel WL, Petrocca F, et al. MicroRNA expression patterns to differentiate pancreatic adenocarcinoma from normal pancreas and chronic pancreatitis. JAMA. 2007;297:1901–8.
Bournet B, Souque A, Senesse P, et al. Endoscopic ultrasound-guided fine-needle aspiration biopsy coupled with KRAS mutation assay to distinguish pancreatic cancer from pseudotumoral chronic pancreatitis. Endoscopy. 2009;41:552–7.
Burk U, Schubert J, Wellner U, et al. A reciprocal repression between ZEB1 and members of the miR-200 family promotes EMT and invasion in cancer cells. EMBO Rep. 2008;9:582–9.
Calin GA, Croce CM. MicroRNA signatures in human cancers. Nat Rev Cancer. 2006;6:857–66.
Calin GA, Dumitru CD, Shimizu M, et al. Frequent deletions and down-regulation of micro-RNA genes miR15 and miR16 at 13q14 in chronic lymphocytic leukemia. Proc Natl Acad Sci USA. 2002;99:15524–9.
Chang TC, Wentzel EA, Kent OA, et al. Transactivation of miR-34a by P53 broadly influences gene expression and promotes apoptosis. Mol Cell. 2007;26:745–52.
Chang TC, Yu D, Lee YS, et al. Widespread microRNA repression by myc contributes to tumorigenesis. Nat Genet. 2008;40:43–50.
Crosby ME, Devlin CM, Glazer PM, et al. Emerging roles of microRNAs in the molecular responses to hypoxia. Curr Pharm Des. 2009;15:3861–6.
Dillhoff M, Liu J, Frankel W, et al. MicroRNA-21 is overexpressed in pancreatic cancer and a potential predictor of survival. J Gastrointest Surg. 2008;12:2171–6.
du Rieu MC, Torrisani J, Selves J, et al. MicroRNA-21 is induced early in pancreatic ductal adenocarcinoma precursor lesions. Clin Chem. 2010;56:603–12.
Feldmann G, Beaty R, Hruban RH, et al. Molecular genetics of pancreatic intraepithelial neoplasia. J Hepatobiliary Pancreat Surg. 2007;14:224–32.
Giovannetti E, Funel N, Peters GJ, et al. MicroRNA-21 in pancreatic cancer: correlation with clinical outcome and pharmacologic aspects underlying its role in the modulation of gemcitabine activity. Cancer Res. 2010;70:4528–38.
Gironella M, Seux M, Xie MJ, et al. Tumor protein 53-induced nuclear protein 1 expression is repressed by miR-155, and its restoration inhibits pancreatic tumor development. Proc Natl Acad Sci USA. 2007;104:16170–5.
Greither T, Grochola LF, Udelnow A, et al. Elevated expression of microRNAs 155, 203, 210 and 222 in pancreatic tumors is associated with poorer survival. Int J Cancer. 2010;126:73–80.
Habbe N, Koorstra JB, Mendell JT, et al. MicroRNA miR-155 is a biomarker of early pancreatic neoplasia. Cancer Biol Ther. 2009;8:4.
Hanoun N, Delpu Y, Suriawinata AA, et al. The silencing of microRNA 148a production by DNA hypermethylation is an early event in pancreatic carcinogenesis. Clin Chem. 2010;56:1107–18.
Hingorani SR, Petricoin EF, Maitra A, et al. Preinvasive and invasive ductal pancreatic cancer and its early detection in the mouse. Cancer Cell. 2003;4:437–50.
Ho AS, Huang X, Cao H, et al. Circulating miR-210 as a novel hypoxia marker in pancreatic cancer. Transl Oncol. 2010;3:109–13.
Hruban RH, Adsay NV. Molecular classification of neoplasms of the pancreas. Hum Pathol. 2009;40:612–23.
Hruban RH, Adsay NV, Albores-Saavedra J, et al. Pancreatic intraepithelial neoplasia: a new nomenclature and classification system for pancreatic duct lesions. Am J Surg Pathol. 2001;25:579–86.
Hruban RH, Goggins M, Parsons J, et al. Progression model for pancreatic cancer. Clin Cancer Res. 2000;6:2969–72.
Huang X, Ding L, Bennewith KL, et al. Hypoxia-inducible miR-210 regulates normoxic gene expression involved in tumor initiation. Mol Cell. 2009;35:856–67.
Hwang JH, Voortman J, Giovannetti E, et al. Identification of microRNA-21 as a biomarker for chemoresistance and clinical outcome following adjuvant therapy in resectable pancreatic cancer. PLoS One. 2010;5:e10630.
Jemal A, Siegel R, Xu J, et al. Cancer statistics. CA Cancer J Clin. 2010; 60:277–300.
Ji Q, Hao X, Zhang M, et al. MicroRNA miR-34 inhibits human pancreatic cancer tumor-initiating cells. PLoS One. 2009;4:e6816.
Jung M, Schaefer A, Steiner I, et al. Robust microRNA stability in degraded RNA preparations from human tissue and cell samples. Clin Chem. 2010;56:998–1006.
Kent OA, Mullendore M, Wentzel EA, et al. A resource for analysis of microRNA expression and function in pancreatic ductal adenocarcinoma cells. Cancer Biol Ther. 2009;8:21.
Lee EJ, Gusev Y, Jiang J, et al. Expression profiling identifies microRNA signature in pancreatic cancer. Int J Cancer. 2007;120:1046–54.
Lee KH, Lotterman C, Karikari C, et al. Epigenetic silencing of microRNA miR-107 regulates cyclin-dependent kinase 6 expression in pancreatic cancer. Pancreatology. 2009;9:293–301.
Li A, Omura N, Hong SM, et al. Pancreatic cancers epigenetically silence SIP1 and hypomethylate and overexpress miR-200a/200b in association with elevated circulating miR-200a and miR-200b levels. Cancer Res. 2010a;70:5226–37.
Li Y, VandenBoom TG 2nd, Kong D, et al. Up-regulation of miR-200 and let-7 by natural agents leads to the reversal of epithelial-to-mesenchymal transition in gemcitabine-resistant pancreatic cancer cells. Cancer Res. 2009;69:6704–12.
Li Y, VandenBoom TG 2nd, Wang Z, et al. MiR-146a suppresses invasion of pancreatic cancer cells. Cancer Res. 2010b;70:1486–95.
Lodygin D, Tarasov V, Epanchintsev A, et al. Inactivation of miR-34a by aberrant cpg methylation in multiple types of cancer. Cell Cycle. 2008;7:2591–600.
Lu J, Getz G, Miska EA, et al. MicroRNA expression profiles classify human cancers. Nature. 2005;435:834–8.
Maitra A, Hruban RH. Pancreatic cancer. Annu Rev Pathol. 2008;3:157–88.
Mathew LK, Simon MC. MiR-210: a sensor for hypoxic stress during tumorigenesis. Mol Cell. 2009;35:737–8.
Mees ST, Mardin WA, Sielker S, et al. Involvement of CD40 targeting miR-224 and miR-486 on the progression of pancreatic ductal adenocarcinomas. Ann Surg Oncol. 2009;16:2339–50.
Mees ST, Mardin WA, Wendel C, et al. EP300 – a miRNA-regulated metastasis suppressor gene in ductal adenocarcinomas of the pancreas. Int J Cancer. 2010;126:114–24.
Moriyama T, Ohuchida K, Mizumoto K, et al. MicroRNA-21 modulates biological functions of pancreatic cancer cells including their proliferation, invasion, and chemoresistance. Mol Cancer Ther. 2009;12:12.
Morris JP 4th, McManus MT. Slowing down the Ras lane: miRNAs as tumor suppressors? Sci STKE. 2005;2005:pe41.
Muniyappa MK, Dowling P, Henry M, et al. MiRNA-29a regulates the expression of numerous proteins and reduces the invasiveness and proliferation of human carcinoma cell lines. Eur J Cancer. 2009;45:3104–18.
Park JK, Lee EJ, Esau C, et al. Antisense inhibition of microRNA-21 or -221 arrests cell cycle, induces apoptosis, and sensitizes the effects of gemcitabine in pancreatic adenocarcinoma. Pancreas. 2009;38:e190–9.
Ryu JK, Hong SM, Karikari CA, et al. Aberrant microRNA-155 expression is an early event in the multistep progression of pancreatic adenocarcinoma. Pancreatology. 2010;10:66–73.
Safioleas MC, Moulakakis KG. Pancreatic cancer today. Hepatogastroenterology. 2004;51:862–8.
Saito Y, Liang G, Egger G, et al. Specific activation of microRNA-127 with downregulation of the proto-oncogene BCL6 by chromatin-modifying drugs in human cancer cells. Cancer Cell. 2006;9:435–43.
Sato N, Maitra A, Fukushima N, et al. Frequent hypomethylation of multiple genes overexpressed in pancreatic ductal adenocarcinoma. Cancer Res. 2003;63:4158–66.
Scott GK, Mattie MD, Berger CE, et al. Rapid alteration of microRNA levels by histone deacetylase inhibition. Cancer Res. 2006;66:1277–81.
Seux M, Iovanna J, Dagorn JC, et al. MicroRNAs in pancreatic ductal adenocarcinoma: new diagnostic and therapeutic clues. Pancreatology. 2008;9:66–72.
Sun M, Estrov Z, Ji Y, et al. Curcumin (diferuloylmethane) alters the expression profiles of microRNAs in human pancreatic cancer cells. Mol Cancer Ther. 2008;7:464–73.
Szafranska AE, Davison TS, John J, et al. MicroRNA expression alterations are linked to tumorigenesis and non-neoplastic processes in pancreatic ductal adenocarcinoma. Oncogene. 2007;26:4442–52.
Szafranska AE, Doleshal M, Edmunds HS, et al. Analysis of microRNAs in pancreatic fine-needle aspirates can classify benign and malignant tissues. Clin Chem. 2008;54:1716–24.
Torrisani J, Bournet B, du Rieu MC, et al. Let-7 microRNA transfer in pancreatic cancer-derived cells inhibits in vitro cell proliferation but fails to alter tumor progression. Hum Gene Ther. 2009;20:831–41.
Torrisani J, Buscail L. Molecular pathways of pancreatic carcinogenesis. Ann Pathol. 2002;22:349–55.
Tsuda N, Ishiyama S, Li Y, et al. Synthetic microRNA designed to target glioma-associated antigen 1 transcription factor inhibits division and induces late apoptosis in pancreatic tumor cells. Clin Cancer Res. 2006;12:6557–64.
Volinia S, Calin GA, Liu CG, et al. A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci USA. 2006;103:2257–61.
Wang J, Chen J, Chang P, et al. MicroRNAs in plasma of pancreatic ductal adenocarcinoma patients as novel blood-based biomarkers of disease. Cancer Prev Res (Phila). 2009;2:807–13.
Watanabe S, Ueda Y, Akaboshi S, et al. HMGA2 maintains oncogenic RAS-induced epithelial-mesenchymal transition in human pancreatic cancer cells. Am J Pathol. 2009;174:854–68.
Weiss FU, Marques IJ, Woltering JM, et al. Retinoic acid receptor antagonists inhibit miR-10a expression and block metastatic behavior of pancreatic cancer. Gastroenterology. 2009;137:2136–45.
Wellner U, Schubert J, Burk UC, et al. The EMT-activator ZEB1 promotes tumorigenicity by repressing stemness-inhibiting microRNAs. Nat Cell Biol. 2009;11:1487–95.
Yan HJ, Wu JX, Liu WS, et al. MicroRNA-20a overexpression inhibited proliferation and metastasis of pancreatic carcinoma cells. Hum Gene Ther. 2010;21:1723–34.
Yu S, Lu Z, Liu C, et al. MiRNA-96 suppresses KRAS and functions as a tumor suppressor gene in pancreatic cancer. Cancer Res. 2010b;70:6015–25.
Yu J, Ohuchida K, Mizumoto K, et al. MicroRNA, hsa-miR-200c, is an independent prognostic factor in pancreatic cancer and its upregulation inhibits pancreatic cancer invasion but increases cell proliferation. Mol Cancer. 2010a;9:169.
Zhang S, Cai X, Huang F, et al. Effect of trichostatin a on viability and microRNA expression in human pancreatic cancer cell line BxPC-3. Exp Oncol. 2008;30:265–8.
Zhang Y, Li M, Wang H, et al. Profiling of 95 microRNAs in pancreatic cancer cell lines and surgical specimens by real-time PCR analysis. World J Surg. 2009;33:698–709.
Zhu Z, Gao W, Qian Z, et al. Genetic variation of miRNA sequence in pancreatic cancer. Acta Biochim Biophys Sin (Shanghai). 2009;41:407–13.
Acknowledgments
We thank Dr Dina Arvanitis (Centre de Biologie du Développement, Toulouse) for critical reading of the manuscript. J.T. was funded by the Ligue Nationale contre le Cancer.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Netherlands
About this chapter
Cite this chapter
Cordelier, P., Torrisani, J. (2011). MicroRNAs in Pancreatic Cancer: Potential Interests as Biomarkers and Therapeutic Tools. In: Cho, W. (eds) MicroRNAs in Cancer Translational Research. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-0298-1_13
Download citation
DOI: https://doi.org/10.1007/978-94-007-0298-1_13
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-0297-4
Online ISBN: 978-94-007-0298-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)