Abstract
This chapter examines patient mobility across Italian regions using data on hospital discharges that occurred in 2008. The econometric analysis is based on Origin–Destination (OD) flow data. Since patient mobility is a crucial phenomenon in contexts of hospital competition based on quality and driven by patient choice, as is the case in Italy, it is crucial to understand its determinants. What makes the Italian case more interesting is the decentralization of the National Health Service that yields large regional variation in patient flows in favor of Centre-Northern regions, which typically are ‘net exporters’ of hospital treatments. We present results from gravity models estimated using count data estimators, for total and specific types of flows (ordinary admissions, surgical DRGs and medical DRGs). We model cross-section dependence by specifically including features other than geographical distance for OD pairs, such as past migration flows and the share of surgical DRGs. Most of the explanatory variables exhibit the expected effect, with distance and GDP per capita at origin showing a negative impact on patient outflows. Past migrations and indicators of performance at destination are effective determinants of patient mobility. Moreover, we find evidence of regional externalities due to spatial proximity effects at both origin and destination.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
JEL Classification
1 Introduction
The Italian National Health Service (NHS) is a regionally decentralized tax-funded system where patients are entitled to choose their own preferred provider of hospital and specialized care. The system is characterized by prospective payment schemes and some degree of competition between providers of health care services. Since the constitutional reform approved in 2001, Italian regions have gained a larger autonomy in the administration and organisation of the health care service. The decentralization process has also involved the funding system, which is largely based on regional budgets, and has had effects on the efficiency and effectiveness of the health care provided at the regional level, creating separate and autonomous regional health services (RHSs). Health care provision and financing have become one of the central issues in the debate on fiscal federalism in Italy, because of the consequences that they can have on universalism and equity in health care. In this context, patient mobility concerns both patients’ choices and financial resources flows across regions.
Patient decision to be hospitalised in any public or private accredited hospital is mainly determined by health needs and hospital specialization. Patients essentially move to get the best hospital treatments that the NHS can provide, or at least better services than those offered locally. They are expected to move when waiting lists are too long in the local hospitals but also when the perceived quality of their RHS is low. Since hospital in-patient services are provided free at the point of use, patient choice does not depend on treatment costs. At the same time, however, patient mobility is likely to be limited by distance from home, travel costs and the difficulties of getting informal support by the relatives and friends when admission is in an extra-regional hospital.
In this context, the importance of patient mobility is twofold. First, the geography of patient mobility yields very important indications on the actual level of the services provided. When individual preferences are not perfectly observable, “exit” mechanisms-such as patient outflows-reveal the effectiveness of public health care supply. Such information may be adequately exploited by central planners interested in correcting inefficiencies of decentralized provision as well as by local governments wishing to improve the RHSs performance. Second, flow imbalances across regions may challenge the stability of regional budgets. As a matter of fact, public hospitals are financed on the basis of the capitated prospective budget attributed to each Local Health Authority (LHA) and, similarly to private accredited hospitals, they are reimbursed for each admission according to a Diagnosis Related Groups (DRG)–tariff system. National tariffs represent the ceilings to reimbursements for hospital admissions and regional variations are allowed downwards to discourage inappropriate admissions. In the case of inter-regional patient mobility the national tariff is used for reimbursement between LHAs, with an exception for the Autonomous Provinces (P.A.) of Trento and Bolzano, while intraregional mobility is paid on the basis of regional tariffs. On the one hand, this provides a financial incentive for each RHS to attract patients from outside the region, thus reducing the unit cost associated with each admission (regions that experience high patient inflows rapidly absorb fixed costs). On the other hand, patient mobility also provides a strong financial incentive to restrain outflows of patients who seek treatments delivered also in the region of residence, particularly where the regional tariff is lower than the national one.
Typically, Centre-Northern regions in Italy are net exporters of hospital treatments. This fact translates into additional amounts of financial resources, generated by the compensation of patient flows, in favor of those regions, and exacerbates the North–South gradient in health care in the Italian NHS. Southern regions typically display the highest negative mobility balances, meaning that they pay a higher amount for hospital care services used by their enrolees outside the region than the amount received as reimbursement from the other regions. In 2008, the mobility balance in the South of Italy was between 1.3 (in Abruzzo) and 6.8 (in Calabria) % of regional public health expenditures, thus increasing the deficit of those RHSs. Only one Southern region, Molise, appears to exploit patient flows and reduce its deficit by about 40 %. The RHSs that get the greatest advantage from inter-regional mobility and transform their deficits into net gains are Lombardia and Emilia-Romagna (where the mobility balances are 2.7 and 4.3 % of regional public health expenditures). These figures reflect the effects of competition due to patient mobility on the sustainability of the RHSs. These stylized facts should also induce the regional governments and LHAs to increase investments aimed at improving the quality and the efficiency of the regional hospital sector. This would decrease the social costs associated with mobility and would also permit to attract more patients, and therefore financial resources, from outside the region. As inter-regional mobility for hospital care is becoming one important source of reallocation of financial resources between regions, identifying the main determinants of patient flows becomes a central issue.
This chapter investigates patient mobility across Italian RHSs, in a context of regional competition driven by patient choice, using data from hospital discharge records available from the Ministry of Health for 2008. The econometric analysis is based on Origin-to-Destination (OD) flow data. We present results from a gravity model for bilateral patient flows that take into account the count nature of data. We focus on both demand and supply factors in each region and distinguish between pull factors which describe the ability of a region to attract patients from other regions, and push factors which describe the ability to restrain the outflows. We control for the well-known cross-section dependence feature of flow data by including regional pairs’ covariates. Besides geographical distance, we consider past migration flows and the share of surgical admissions, which are expected to approximate information and support networks. Externality effects from neighboring RHSs are taken into account by means of spatial lags of some specific pull and push factors.
The chapter is organised as follows. Section 2 presents a selective review of the previous studies most directly related to our contribution. In Sect. 3 we present a detailed description of the Italian regional patient flows along with a brief discussion on the main features of the explanatory variables included in the econometric analysis, which follows in Sect. 4. Section 5 concludes.
2 Related Literature
The empirical literature on patient mobility has been mainly developed in the last fifteen years, with a particular focus on modelling hospital choices and flows across different jurisdictions. A large part of the literature analyses the relationship between competition and quality in health care markets, where patient choice—and therefore patient flows—typically mirrors differences in quality among providers.Footnote 1 In an extensive review of the literature, Gaynor and Town (2012) find that the effect of competition on health care quality is generally positive in the case of price-regulated markets. Nonetheless, national health systems often impose severe restrictions on patients’ freedom of choice. Where reforms towards patient choice have been put in place, results are consistent with quality improvements, as in the English NHS reform on patient choice accomplished in 2008 (Propper 2012; Bloom et al. 2010; Cooper et al. 2011; Gaynor et al. 2010).
Other works are directly focused on patient mobility aiming at identifying the main drivers of flows occurring within and between health care systems. The related literature presents a clear dichotomy between studies where the unit of analysis is the single patient and macro-level studies where the unit of analysis is a geographical area or a political decision unit. The former have singled out a wide set of potential determinants of mobility (see Victoor et al. 2012, for a survey), referred both to patient characteristics (e.g. education, income and age), and provider characteristics, classifiable as “structure factors” (e.g. availability and accessibility of the providers; cost of treatments), “process factors” (availability of information, continuity of treatment, waiting time and quality of treatment) and “outcome factors” (e.g. mortality indicators).Footnote 2 These studies have also detected that a substantial fraction of patients does not consider choice to be very important: they simply choose the nearest provider or follow the advices of their GP, who in turn tends to refer patients to the closest hospitals (Birk and Henriksen 2012).
At the macroeconomic level, the investigation of the determinants of patient mobility has been developed along both the theoretical and empirical level. Theoretical studies often examine patient mobility within a framework of institutional competition, where sub-national levels of government (the decision units in a federal system) compete among them. Brekke et al. (2011) consider a situation where regional governments differ in their ability to provide public services (namely health care). In this context, patient mobility within a system which centrally defines the quality of services, can play a major role in improving overall welfare, though with asymmetric effects: since decentralization creates more incentives for quality improvement, all patients from “high-skill” regions are better off than in a system without mobility. Conversely, in “low-skill” regions only patients who move to a high-skill region benefit from the higher quality provided. Levaggi and Menoncin (2008, 2012) provide another explanation of the large patient flows observed in decentralized health care systems with a central government defining health targets. In the presence of a national regulator characterized by a “soft budget constraint” vis à vis the local authorities,Footnote 3 inefficient regions have an incentive to send patients to more efficient ones. This increases the probability of being bailed-out by the central authority, thus avoiding the need to finance budget deficits by increasing local taxes. Efficient regions benefit from incoming patients, and compensate the bail-out cost of the service through the soft budget constraint. Hence, part of patient mobility is induced by lack of coordination between competing constituencies in a fiscal federalism framework.
The applied macroeconomic analysis of patient mobility between “competing” constituencies has mainly been based on gravity models, more commonly encountered in the analysis of bilateral international trade and migration flows. With gravity models, flows are viewed as being positively influenced by “mass” accumulation at origin and destination, and negatively influenced by the distance between the two. Origin-specific variables reflect potential demand or repulsion effects, while destination-specific indicators should proxy the degree of attraction.Footnote 4 In the health economics literature, gravity models were originally introduced by Morrill and Earickson (1968) for modelling hospital choice, then subsequently adopted for the analysis of aggregate bilateral flows such as those studied in this chapter. The studies related to our research work estimate models for patient mobility across different regions in Italy and Spain (respectively, Levaggi and Zanola 2004; Cantarero 2006). Levaggi and Zanola investigate the determinants of net patient flows from origin regions to the rest of Italy over the period 1995–1997 and find that regions providing better or faster services are characterized by lower outflows. Cantarero, using data on net patient flows across Spanish regions over the period 1996–1999, finds that patients from the worse-off regions move more than those from regions that provide better health services (quality-driven mobility). Fabbri and Robone (2010) focus on bilateral patient flows for hospital care between LHAs in Italy. They estimate a gravity model for count data and investigate the role of scale economies and the impact of the North–South economic divide on mobility. They control for the effect of push and pull factors related to both origin and destination LHAs, geographical factors, such as measures of actual distance and contiguity between LHAs, and spatial factors based on weighted distances between LHAs. Their main findings suggest that richer LHAs tend to attract more patients, especially the most severe cases, and LHAs in the South are less able to “import” patients and restrain outflows.
From a methodological viewpoint, the health economic literature has been only recently enriched by approaches based on the estimation of gravity specifications augmented by spatial features. In this chapter, we thus aim to contribute to the current debate on the determinants of patient flows by focusing on the regional dimension of the phenomena, given its crucial implications on regional budgets and, ultimately, on patients utility.
3 Data
3.1 Patient Mobility in Italy
We use data on hospital discharges that occurred in 2008 in all public and private accredited hospitals of the 21 RHSs that provide health care in the country.Footnote 5 Information on in-patient care is collected by each hospital at the time of discharge and regularly transmitted through the LHA to the Ministry of Health. Each admission episode is classified using version 19 of the US DRG system, and length of stay is reported. The data at hand contain information that allow us to identify the hospital of admission, the corresponding LHA and region, as well as the LHA and the region of residence associated with each single discharge. The total number of hospitals with complete discharge data is 1,304. This corresponds to a total number of 11,701,920 admission episodes, of which 29.5 % are identified as flows because they either occur in a different region (inter-regional mobility) or in the region of residence but not in the LHA where the patient is registered (intra-regional mobility).
In this chapter we focus on inter-regional patient mobility because this represents an important source of external revenue for regions that are able to attract patients from other regions (net exporters). For the 21 Italian regions, we construct a square matrix that describes inter-regional patient flows by aggregating the number of admissions of patients from each possible region of origin (enrolees in RHS i) in public or private accredited hospitals of each possible region of destination (RHS j). For the purpose of our analysis, the main diagonal of the matrix is set to 0 in order to exclude intra-regional flows. This leaves us with 420 bilateral OD patient flows.
We concentrate our attention on potentially avoidable mobility, thus we exclude admissions that are classified in the four Major Diagnostic Categories (MDC) which most likely represent unavoidable mobility. These MDCs refer to traumatology, HIV and burns. The total number of admission episodes outside the region of origin is 863,953, which is 25.1 % of total mobility. About 47.2 % of these episodes have a surgical DRG (and hence, on average, are compensated on the basis of higher national tariffs than admissions with medical DRGs) and 64.4 % are classified as ordinary admission.Footnote 6 About 44.3 % of total OD flows are generated by Southern regions (382,682 admission episodes). About 17.2 % of total flows are from regions in the South to regions in the North (148,550 admission episodes), while only 2.8 % of flows are from the North to the South (23,831). Flows between Northern origins and destinations represent about 29.5 % of total inter-regional mobility, while this figure is only 10.9 % in the case of flows between Southern origins and destinations.
Table 1 illustrates the main differences between Italian regions in terms of their contribution to inter-regional mobility. We calculate the creation rate as the percentage ratio between enrolees of region i admitted in hospitals of other regions and the total number of patient flows in Italy, and the attraction rate as the percentage ratio between non-enrolees admitted in hospitals of region j and the total number of patient flows in Italy. Both rates show different spatial patterns. The regions that create more inter-regional mobility are the most densely populated territories in the country: Campania, in the South, generates about 10.6 % of total flows, followed by Lombardia, in the North (8.7 %), and Lazio, in the center of Italy (8.4 %). The least populated regions (P.A. Trento, Friuli Venezia-Giulia, Molise, Valle d’Aosta and P.A Bolzano) and Sardegna (probably due to insularity) generate less than 2 % of total flows. The regions that admit more non-resident patients are Lombardia, Emilia-Romagna and Lazio with attraction rates of about 19, 13.5 and 13 %, respectively. The attraction rate is largely higher in the Central-Northern regions, 81.8, than in the Southern regions, 18.2.
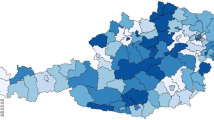
We further examine patient flows in each region using the mobility index. This index measures the ratio between the inflow rate and the outflow rate, and takes values larger than 1 when the RHS is a net importer of patients from other RHS, thus being able to offset the outflows with larger inflows.Footnote 7 The maps reported in Fig. 1 confirm the role of spatial proximity and show a clear North–South gradient. For most of the regions in the Centre-North of Italy the mobility index is larger than 1 (larger than 2 for Emilia-Romagna and Lombardia), while all Southern regions display indexes lower than 0.7. Spatial patterns in hospital admissions, which are likely due to the influence of demand and supply features of the RHSs at origin and destination, seem to reflect the well-known North–South economic divide, as richer and better equipped regions tend to attract more patients and resources.
3.2 Origin and Destination Characteristics
Inter-regional patient flows depend on characteristics of both origin and destination regions, which are related with economic and demographic aspects and features of the hospital care services. We have selected the set of variables which are expected to influence patients’ choice about the hospital where to seek care, as well as the ability of the RHS to attract inflows and restrain outflows of patients. The complete description of all variables is reported in Table 2. In this section, we distinguish between push and pull factors, which play a different role at origin and destination, respectively.
Origin Characteristics
In the following we motivate the choice of push factors used in the empirical model.
Per capita GDP. Per capita income may pick up two different effects: at the micro level, its effect can be interpreted as patients’ ability to travel and seek care outside the region of residence (richer individuals choose better hospitals regardless of travel and accommodation costs); at the macro level, the income effect can be interpreted as a greater ability of the regional health care system to provide hospital services (poorer regions experience outflows of patients towards richer regions).
Population. Population indicates the number of enrolees to the RHS and approximates the internal demand for health care. Bigger regions have a higher internal demand of hospital care, this might induce more variety in the range of specialized health services provided in the area. Furthermore, higher populated regions may exploit economies of scale leading to cost minimization, more and better services. For this reason, highly populated regions should be able to restrain patients outflows better than small regions.
Population age 0–14 and Population over 65. This two demographic indicators allow us to capture the effect of aging on the likelihood to seek care in extra-region hospitals. Since morbidity rates among the youngest individuals are typically lower than at adult ages, we expect a negative impact on outflows. Likewise, we also expect a negative impact for the oldest individuals in the population since they are usually less prone to travel.
Technology index. The technological endowment of each RHS is captured by information on the number of high technology medical equipment. We consider ten different devices and compute a synthetic technological index on the basis of principal factor analysis, scoring the first factor, that accounts for approximately 53 % of the variance, by the regression method.Footnote 8 We expect that the higher the index, the smaller the patients’ outflows.
Hospital capacity. The number of hospital beds per 1,000 inhabitants is an indicator of hospitals supply in the region. The lower the availability of beds, the higher the waiting times for admissions and the larger the outflows. The downside of this indicator is that it does not capture the quality of care.
Organisational efficiency. An excess of beds in hospitals, however, is typically considered a signal of bad management, and can translate into a waste of resources. We propose a measure of the distance (in absolute value) between the actual number of hospital beds per 1,000 inhabitants and the national target on the optimal number of beds (4 per 1,000 inhabitants), recommended by the Italian Ministry of Health guidelines for the period 2007–2009. Although this indicator represents a single dimension of hospital organisational efficiency, we can assume that it is a fairly good approximation of organisational efficiency in the regions. Inefficient RHS are further away from the target (they can be either over- or under-endowed with respect to the target) and are expected to experience larger patients’ outflows.
HECC dummy. The “high efficiency in complex cases” dummy combines the information related to the case-mix index (CMI) and the performance index (PI), which can be used together to measure hospital efficiency at the regional level. The regional CMI is calculated as the ratio between the average weight of admissions in a region and the average weight of admissions at the national level. The DRG relative weights, which measure the amount of financial and physical resources allocated to DRGs, are used to calculate the average weights. Hence, the CMI indicates the degree of clinical complexity of hospital admissions in each region with respect to the national average and represents an index for specialization. A CMI higher (or equal) to 1 indicates a greater (or equal) clinical complexity compared to the national benchmark. The PI compares the regional performance in managing hospital length of stays and is calculated as the ratio between the case-mix standardized average length of stays in each region and the benchmark level (typically the national average).Footnote 9 A PI lower than (or equal to) 1 indicates that, assuming equal complexity, hospital stays are shorter (or have the same length) than at the national level, thus suggesting higher (or at least equal) efficiency relative to the standard. We calculate the CMI and PI on ordinary admissions only (excluding 1-day hospital stays) and we build a comprehensive variable that identifies the most efficient regions as those characterised by high complexity and high performance.Footnote 10 High efficiency regions are likely to restrain patients outflows better than other regions.
Destination Characteristics
In the following we motivate the choice of pull factors used in the empirical model.
Per capita GDP. As a pull factor, per capita GDP is expected to have a positive effect on inflows. Richer regions are more attractive because they are expected to provide more efficient and effective health care services.
Population. Bigger regions should be able to attract patients from smaller regions because of the larger variety of specialized care provided. Therefore, the size of the population is expected to be positively related to patients inflows.
Technology index. We expect that the higher the index, the higher the patients’ inflows.
Hospitals capacity. Regions with a higher number of beds, and perhaps shorter waiting lists for admissions, are more attractive.
Organisational efficiency. Less efficient regions (under- or over-endowed) should attract less patients from other regions.
HECC dummy. As explained above, efficiency calculated in terms of both clinical complexity of admissions and performance in managing hospital stays is expected to play an important role as a pull factor. High efficiency regions should attract more patients compared to other regions.
Accessibility. Attractiveness might benefit from the patients’ ability to access the destination region in an easy way. We use a five-category discrete variable that describes potential accessibility by road, train, air and time to the market. We expect a positive effect on inflows because a higher accessibility should increase the probability that individuals move to seek care in extra-regional hospitals.
Origin–Destination Flow Characteristics
Geographical distance. We include the distance for each pair of destination and origin regions as a proxy of transport costs and thus it is excepted to have a negative impact on patient movements. Within the gravity model framework the geographical distance is also expected to account for spatial correlation among the observational units.
Migration flows. Past inter-regional migration between any two OD regions is expected to have a positive impact on patient mobility. Past migration flows are a powerful source of knowledge for patients seeking health care. People who have migrated may provide their relatives and friends looking for good health care with valuable information on the medical services present in their region of residence and in the contiguous ones. Moreover, patients are more likely to seek hospital care in regions where relatives or friends of their same origin region migrated. The latter can provide informal support before, during and after the hospital stay, especially when treatments require long stays. For this reason, past migration flows allow us to account for spatial correlation in patient mobility.
Surgical Admissions. As another control for the flows between any two OD regions, we include an indicator of the share of patients resident in origin i and admitted with a surgical DRG in region j over the total amount of patients admitted with surgical DRG in the destination region. The national tariffs associated with surgical DRGs are typically higher compared to medical DRGs, due to complexity and effective costs. As a driver of inter-regional patient mobility, we expect a positive effect due to micro level learning (at destination) and communication (at origin) of patients sharing their experiences, within family and friends networks, on treatments received in specific destinations.
4 Empirical Analysis
4.1 Economic Framework
The empirical analysis of the determinants of inter-regional patient flows is based on the estimation of gravity models. The general model is formalized as follows:
where y ij is the number of patients resident in region i that chose to be treated in hospitals located in region j in the year 2008. The total number of possible inter-regional flows is 420. The matrix X oi comprises the variables which are supposed to represent the origin’s features, while the matrix X dj includes variables for the destinations’ characteristics. These two sets of regressors are thus expected to account for the emissiveness and attractiveness traits of each region, as detailed in the previous section. The matrix X ij includes the variables which pertain to the pair of regions involved in each patients flow, namely the geographical distance, past migration flows and the share of surgical admissions; conditional on correct model specification, the u ij term is expected to be an i.i.d. process.
Since our response variable is a count variable the natural starting point is to consider the Poisson regression model, which entails specifying the conditional mean (μ ij ) as a function of a set of covariates X. The standard parameterization of the conditional mean is E(y ij |X) = μ ij = exp(Xβ) to ensure that the non-negativity constraints are not violated. Since the Poisson distribution is characterized by the equidispersion property, the variance is equal to the mean so that the Poisson model is intrinsically heterosckedastic. The equidispersion property has often been found to be excessively restrictive in empirical applications because count data are usually characterized by overdispersion. Our sample data is no exception, our dependent variable exhibits a mean value of 2,057.03 and a standard deviation of 4,093.96.
Unobserved heterogeneity is deemed to be one of the most common causes of overdispersion (Cameron and Trivedi 2005), which can also yield an excessive number of zero observations.Footnote 11 It is common to deal with such heterogeneity by considering a continuous mixture of the Poisson distribution. This requires modifying the specification of the mean as E(y ij |X) = μ ij η ij , with μ ij defined as before and η ij a random term with E(η ij ) = 1. In this case, the Poisson mixture has the same mean as the original Poisson. When η ij follows the gamma distribution with variance α, the negative binomial model results. The first two moments are E(y ij |X) = μ ij and Var(y ij |X) = μ ij + αμ 2 ij , and α is the over-dispersion parameter to be estimated.Footnote 12 Since our flow data are characterized by over-dispersion, the preferred functional form chosen to estimate the gravity relation reported in Eq. (1) is the negative binomial model.Footnote 13
When analysing flow data, another relevant issue is the existence of spatial dependence (Griffith and Jones 1980; Le Sage and Pace 2008, 2009). Flows from a given origin are usually related to the degree of emissiveness of neighboring regions; likewise, flows towards a specific destination are enhanced or reduced according to the degree of attractiveness of nearby destination locations. In this study we deal with the spatial dependence issue by including regressors characterized by spatial features (geographical distance, regional accessibility, spatial lags of some explanatory variables) and regressors which allow us to properly account for the characteristics of the OD regional pairs. We thus include the share of surgical admissions and past migration flows.Footnote 14
4.2 Results
The main results of the analysis of the Italian inter-regional patient flows determinants are reported in Table 3. In the first column we present our baseline model, which includes—for both origin and destination regions—population, per capita GDP and hospital capacity; origin features are also accounted for by including the share of population in the groups aged 0–15 or above 65 years. In the base specification, the regional pairs’ characteristics are captured by the geographical distance. The estimated coefficients are in line with the effects expected on the basis of the arguments presented in Sect. 3. Population, acting as the “mass” variable usually included in gravity specifications, turns out to be more effective as a pull rather than a push factor (the estimated elasticity are 1.01 and 0.89 respectively). Conversely, GDP per capita is effective in restraining patient outflows; in absolute terms the estimated elasticity at origin is more than twice the one at destination (−1.88 vs. 0.79). Hence, we find evidence that the macro level effect proxied by GDP per capita described in Sect. 3.2 dominates the micro level effect. Supply factors, represented by hospital capacity, play a significant role only at destination. The additional demand side controls exhibit the expected negative sign on patients mobility because population in the “dependency” age classes are less inclined to travel. However, only the share of oldest people is statistical significant. Finally, geographical distance is highly significant and exhibits a sizeable discouraging effect (elasticity estimate of −1.57) on patient flows. It is worth noting that the estimate of the variance function parameter (α = 0.75) is highly significant, indicating that overdispersion is a relevant feature of the data. This finding is robust with respect to all the other specifications reported in Table 3.
In order to improve the understanding of the patient flows drivers we proceed by subsequently augmenting the baseline model. We first include additional variables for the regional OD pairs and then for the origin and destination regions. This estimation strategy is selected because a better characterization of the OD pairs is expected to clear any remaining cross-section dependence, not fully accounted for by the inclusion of the geographical distance. Therefore, in the regression models (2) and (3) of Table 3, we subsequently include the share of surgical admissions and past migration flows. As stated in Sect. 3, we believe that the share of surgical admission is a good proxy of hospital performance on highly complex treatments received in the destination region. Since it is measured as the share of people from a region who selected a specific destination for these treatments, it is expected to explain the proportion of patient mobility driven by the information diffused at origin by patients who were treated at specific destinations. Likewise, patient mobility should be positively affected by past migration flows given that they represent both a powerful source of knowledge and a reliable support network for arrangements, especially when treatments require long stays for patients seeking health care outside their own region.
According to the models reported in columns (2) and (3) of Table 3, the share of surgical admissions and past migration flows are statistically relevant in accounting for the variability of patient flows. Moreover, the previously discussed results for the baseline model are largely confirmed, although, as expected, the estimated coefficients from models (2) and (3) imply smaller effects. It is worth noting that the latter models yield higher values for the log-likelihood and that the share of the youngest population turns out to be significant in both models.
Model (4) augments model (3) by including the accessibility index at destination. The estimated coefficient (0.148) points out that easy-to-access locations are significantly more attractive to patients seeking hospital care in other regions, even when transport cost have been already accounted for by geographical distance. Note that in model (4) per capita GDP at destination is no longer significant. This is likely to be due to collinearity issues because, in general, we expect territories with a high degree of accessibility (implying for instance the existence of widespread and advanced transport infrastructures) to be located in the wealthiest regions.Footnote 15
In models (5) we include the two efficiency indicators at both origin and destination and the technology index at destination. The latter is positive (estimated coefficient 0.12) and significant at conventional levels, confirming that RHS endowed with advanced technological instruments are able to attract more patients inflows. A unit change in the overall technology index implies an increase of nearly 250 non-resident patients. This finding supports the idea that attractiveness can increase due to higher investments in advanced medical devices.
The efficiency indicators do not prove to be relevant factors in restraining patient outflows as they both turn out to be not significant at origin. However, they are highly significant at destination. This indicates that regions which have an RHS characterized by organizational inefficiency (coefficient estimate −0.78) are less attractive for potential patients, and vice versa. Organizational inefficiency at the regional level may be due both to single non-adequately-sized hospital or to a large number of small hospitals widespread in the regional territory. In general, this might generate high management costs and, due to budget constraints, crowd out resources that could be employed to enhance both quality and variety of the health treatments and technological equipment. Conversely, we found the opposite effect (coefficient estimate 0.50) for regions which are characterized by high efficiency in terms of both the case-mix complexity and the performance in hospital stays. Note that the inclusion of the additional technological and efficiency indicators leave largely unchanged the estimated effects and significance of the previously included explanatory variables.
In the final stage of our analysis we address the issue of possible externality effects produced by neighboring regions at both origin and destination.Footnote 16 We test for the existence of such effects by including the spatial lag of some specific regressors, namely the technology index and the organizational and efficiency indexes.Footnote 17 Each spatial lag is obtained as the weighted average of the corresponding regional regressors values, with weights proportional to the inverse of the geographical distance between any two regions. Focusing on the results of model (6), we find that, at destination, the spatially lagged terms of the technology index and of the two efficiency indicators are highly significant and with the expected sign, thus indicating that being located close to efficient and technological advanced RHS enhances the attractiveness of a given region. This result is likely to be driven by two different, but possibly complementary, mechanisms. The first one is related to the learning and communication processes described above: individuals who for some reason (migration, journeys, previous health treatments) happen to acquire knowledge on the reputation of hospitals in a certain area spread this information in their origin region, thus increasing the flows from that region to the destination surrounded by efficient RHSs. The other explanation may be related to a competitive market kind of mechanism: a region located close to health services efficient areas has an incentive to emulate its neighbors in providing high quality treatments, contending extra-regional patients to nearby regions.
The latter mechanism may also explain the results found for the spatially lagged terms at the origin. The more efficient the neighbors of given region, the higher the incentives for that specific region to increase its own level of efficiency in order to restrain outflows. This is reflected in the sign of the coefficients for the high efficiency dummy at the origin, although only the organizational efficiency coefficient turns out to be significant. In this case, lower efficiency of neighboring regions would not induce any special effort at origin in improving efficiency, however it would reduce the average outflows because of a reduction in flows towards closer regions. It is relevant to remark that the non-spatially lagged regressors proved robust to the inclusion of the additional geographical covariates both in terms of magnitude and statistical significance.Footnote 18
In order to test the robustness of our results, we re-estimate model (6), which is the most general specification, for a subset of specific flows, namely those related to ordinary admissions, surgical DRGs and medical DRGs. The results are reported in columns 7–9 of Table 3. Although, as expected, the magnitude of the estimated coefficient varies across the estimated models, the results previously discussed with respect to model (6) are generally confirmed. The only noticeable exception is represented by the spatial lags at destination for surgical DRGs flows, which are no longer significant. This result is in line with the intrinsic characteristics of treatment complexity, hospital specialization patterns and patient mobility motivations. For highly complex cases, patients tend to select the hospitals specialized in those cases, because they expect these to provide the highest quality treatment and thus to enhance the probability of a successful outcome. In this selection process, only very specific knowledge is applied and this is even more so when extra-regional destinations are considered. This is the reason why information on RHSs close to the selected destination becomes much less valuable yielding non-significant effects.
Overall, the results presented in this analysis provide interesting insights into the determinants of patients flows in the Italian NHS, characterized by an enhanced citizens opportunity to seek health treatments all over the national territory and framed within a persistent and growing North–South divide, that translates into differently performing RHSs. This becomes even more relevant in a context of centrally-defined targets and low variability in per capita public health expenditures across regions.
5 Conclusions
In this chapter we investigate the determinants of inter-regional patient mobility in Italy. This is a relevant issue because the Italian NHS is a regionally decentralized tax-founded system, characterized by patient choice and by a high degree of autonomy for RHSs in designing health care provision at the local level. Understanding which are the most influential drivers of patient mobility is of key importance, as mobility is increasingly determining surplus/deficit of regional budgets and thus the sustainability of the RHSs, with non-negligible consequences in terms of both universalism and equity of health care provision.
We analyze count data from hospital discharge records for inter-regional patient flows in 2008, by estimating negative binomial specifications within a gravity model framework. Our findings indicate that the most effective pull factors are hospital capacity, advanced technological endowment, high degree of efficiency and accessibility of destinations RHSs. Once we control for the demographic structure, we find that at origin patient flows are held back by high levels of per capita GDP, supposed to capture the availability of adequate local health service, and by hospital capacity. The well-known cross-section dependence feature of flow data is accounted for by including variables that characterize the unique traits of the OD pair involved in each flow, namely geographical distance (found to discourage mobility), the share of surgical admissions and past migration flows (with enhancing effects due to information and support networks), and by including spatial lags of the technology, organizational and efficiency indices. The latter detect the existence of positive externalities from proximate regions through learning and communication processes. Information on hospitals’ reputation acquired in a certain area, is likely reported at origin, thus increasing the flows from that given origin to the destination location surrounded by efficient RHSs. Evidence of positive externalities is also consistent with competitive market mechanisms because regions emulate their efficient neighbors, thus attracting extra-regional patients. Our main results are confirmed when the analysis is conducted for the sub-sample of ordinary admissions and the sub-groups of DRG (surgical and medical).
Overall, our findings provide sound evidence on what drives inter-regional patient mobility across Italian regions. Our results also call for more attention on the financial sustainability of a decentralized system with centrally defined targets in a context characterized by persistent and growing socio-economic gaps. From a policy perspective, our findings on the significant presence of externalities could suggest that a greater coordination at the central level (for example by means of “fine-tuned” reimbursement schemes) is desirable in order to design or reinforce existing patterns of regional health care specialization so that inter-regional mobility is expected to become mainly specialization-driven rather than induced by the current efficiency gap. In future research, it is worth investigating the potential welfare loss associated with excessive mobility. This is still an open question since, at least in the short run, the inefficient RHSs might benefit from “importing” hospital care from other regions. Therefore, more focused policy prescriptions cannot be directly derived from our analysis.
Notes
- 1.
- 2.
Somewhat surprisingly, process factors are found to play a major role, and outcome factors a residual one (Rademakers et al. 2011).
- 3.
In fact, health care is a public and merit good which the central regulators want to provide equitably in the whole federation.
- 4.
As remarked by Lippi Bruni et al. (2008), the importance of distance differs significantly among treatments, as demand for health services is far from homogeneous. In particular, patients generally show a greater willingness to travel for major treatments. Hence, the intensity of the distance decay effect cannot be generalized.
- 5.
Approximately 33.6 % of public hospitals are run by LHAs; 11 % are autonomous public enterprises; 4.4 % are scientific institutes for research, hospitalization and health care and 2 % are medical school hospitals. Private accredited hospitals represent about 45 % of the total number of providers but only 16 % of total admissions.
- 6.
Ordinary admissions imply at least one night spent at the hospital and exclude admissions in long-term care and rehabilitation wards, as well as admissions of healthy babies born at the hospital.
- 7.
The inflow rate is the percentage ratio between non-enrolees admitted in region j (inflows) and the total number of admissions in region j. The outflow rate is the percentage ratio between enrolees of region i admitted in other regions (outflows) and the total number of admissions of enrolees of region i.
- 8.
The devices are magnetic resonance imaging, linear accelerator in radiotherapy, computed axial tomography (CT), gamma CT, mammogram, gamma camera, positron emission tomography (PET) or CT-integrated PET, hyperbaric chamber, digital angiography, automated immunochemistry analyzer.
- 9.
The case-mix standardization controls for regional differences in the complexity of the admissions. Consequently, the indicator of regional standardized average lengths of stays assumes that each region share the same complexity of cases as the national average.
- 10.
In the yearly report on hospitals activity based on the discharges database, the Italian Ministry of Health assesses the efficiency of RHS on the basis of data on ordinary admissions with stays longer than one day. Stays are typically longer and cases can be more clinically complex in long-term and rehabilitation wards and neonatal care units.
- 11.
In our sample data we just have one pair of regions, Val d’Aosta and Basilicata, featuring a zero patient flow.
- 12.
Note that this specification is referred to as negative binomial 2 (NegBin2); the negative binomial 1 entails a linear variance function. The NegBin2 specification is typically preferred because the quadratic form has been proven to provide a very good approximation to more general variance functions. This is a remarkable advantage because the maximum likelihood estimators for negative binomial models are not consistent when the variance specification is incorrect.
- 13.
In a preliminary analysis we also estimated the Poisson model, but we found overwhelming evidence in contrast with the equidispersion assumption.
- 14.
Fabbri and Robone (2010) claim that past residential migration is one of the most relevant variable that can generate network autocorrelation in patient flows.
- 15.
In order to account for the particular morphology of the Italian territory, an undisputed factor in driving the well-known North–South divide, we also include a dummy variable to discriminate between Centre-Northern and Southern regions. The dummy turned out to be highly significant with the expected negative sign, but it makes negative the coefficient of per capita GDP. This is due to the fact that the two variables are significantly negatively correlated. For these reasons we prefer the specification that includes per capita GDP only.
- 16.
- 17.
The selection of the lagged regressors was carried out on the basis of a preliminary analysis performed on all the origin and destination covariates.
- 18.
Moreover, note that the “hospital capacity” variable turn out to be significant in model (6).
References
Birk, H. O., & Henriksen, L. O. (2012). Which factors decided general practitioners’ choice of hospital on behalf of their patients in an area with free choice of public hospital? A questionnaire study. BMC Health Services Research, 12(126), 1–10.
Bloom, N., Propper, C., Seiler, S., & Van Reenen, J. (2010). The impact of competition on management quality: evidence from public hospitals. London School of Economics CEP Discussion Paper 983.
Brekke, K. R., Levaggi, R., Siciliani, L., & Straume, O. R. (2011). Patient mobility, health care quality and welfare. Norwegian School of Economics and Business Administration Discussion Paper 13/11.
Cameron, A. C., & Trivedi, P. K. (2005). Microeconometrics: Methods and applications. New York: Cambridge University Press.
Cantarero, D. (2006) Health care and patients' migration across Spanish regions. European Journal of Health Economics, 7, 114–116.
Cookson, R., Laudicella, M., & Li Donni, P. (2013). Does hospital competition harm equity? Evidence from the English National Health Service. Journal of Health Economics, 32, 410–422.
Cooper, Z., Gibbons, S., Jones, S., & McGuire, A. (2011). Does hospital competition save lives? Evidence from the English NHS patient choice reforms. The Economic Journal, 121(554), F228–F260.
Fabbri, D., & Robone, S. (2010). The geography of hospital admission in a national health service with patient choice. Health Economics, 19, 1029–1047.
Gaynor, M., Moreno-Serra, R., & Propper, C. (2010). Death by market power: Reform, competition, and patient outcomes in the National Health Service. NBER Working Paper 16164.
Gaynor, M., & Town, R.J. (2012). Competition in Health Care Markets. In T. Mc Guire M. Pauly & P. P. Barros (Eds.), Handbook of Health Economics (Vol. 2, pp. 499–637). Amsterdam: Elsevier.
Griffith, D. A., & Jones, K. G. (1980). Explorations into the relationship between spatial structure and spatial interaction. Environment and Planning A, 12, 187–201.
Le Sage, J. P., & Pace, R. K. (2008). Spatial econometric modeling of origin-destination flows. Journal of Regional Science, 48, 941–967.
Le Sage, J. P., & Pace, R. K. (2009). Introduction to spatial econometrics. Boca Raton: CRC.
Levaggi, R., & Menoncin, F. (2008). Fiscal federalism, patient mobility and soft budget constraint in italy. Politica economica, 26, 367–386.
Levaggi, R., & Menoncin, F. (2012). Soft budget constraints in health care: Evidence from Italy. European Journal of Health Economics. doi:10.1007/s10198-012-0417-4.
Levaggi, R., & Zanola, R. (2004) Patients' migration across regions: The case of Italy. Applied Economics, 36, 1751–1757.
Lippi Bruni, M., Nobilio, L., & Ugolini, C. (2008). The analysis of a cardiological network in a regulated setting: A spatial interaction approach. Health Economics, 17, 221–233.
Morrill, R. L., & Earickson, R. J. (1968). Hospital variation and patient travel distance. Inquiry, 5, 26–34.
Propper, C. (2012) Competition, incentives and the English NHS. Health Economics, 21, 33–40.
Rademakers, J., Delnoij, D. M., & de Boer, D. (2011). Structure, process or outcome: Which contributes most to patients’ overall assessment of healthcare quality? BMJ Quality and Safety, 20(4), 326–331.
Victoor, A., Delnoij, D. M., Friele, R. D., & Rademakers, J. J. (2012). Determinants of patient choice of healthcare providers: A scoping review. BMC Health Service. Research., 12, 272.
Acknowledgments
The research leading to these results received funding from the Sardinian Region (LR7). The authors would also like to thank Daniela Moro for valuable assistance in preparing the database. We thank Lucia Lispi and Pietro Granella from the Italian Ministry of Health for offering access to the hospital discharge data.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Italia
About this chapter
Cite this chapter
Balia, S., Brau, R., Marrocu, E. (2014). What Drives Patient Mobility Across Italian Regions? Evidence from Hospital Discharge Data. In: Levaggi, R., Montefiori, M. (eds) Health Care Provision and Patient Mobility. Developments in Health Economics and Public Policy, vol 12. Springer, Milano. https://doi.org/10.1007/978-88-470-5480-6_6
Download citation
DOI: https://doi.org/10.1007/978-88-470-5480-6_6
Published:
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-5479-0
Online ISBN: 978-88-470-5480-6
eBook Packages: Business and EconomicsEconomics and Finance (R0)