Abstract
Nonadherence is highly prevalent in schizophrenia. It has been estimated that nonadherence rate for prescribed antipsychotic medications is about 50 %. Nonadherence with antipsychotic medication is a major cause of relapse and it is associated with poorer functional outcomes in patients with schizophrenia. After identifying factors that may be contributing to a patient’s adherence, it is important for clinicians to initiate strategies specifically targeted to those problems. Research has increasingly focused on psychosocial and pharmacological interventions to improve outcomes in patients with schizophrenia. Systematic reviews of various psychosocial approaches to enhance adherence to medication in schizophrenia indicate that some approaches have yielded some promising results, but they are still controversial or preliminary. The aim of this chapter is to provide a comprehensive overview of the available data on nonpharmacological strategies designed to improve adherence to medication in schizophrenia. Interventions and strategies proposed and/or tested to enhance adherence to antipsychotic medication are systematically described and discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
There is wide agreement that a major problem limiting success in the treatment of patients with serious mental illnesses, including schizophrenia, is poor adherence to prescribed medication regimens [1]. Long-term adherence to antipsychotic therapy is the cornerstone of contemporary management of psychosis, and patients who stop therapy have a markedly increased risk of relapse. Nonadherence with medication treatment is common but difficult to detect in patients with schizophrenia, almost half of whom take less than 70 % of prescribed doses [2]. The consequences of nonadherence can be devastating for patients and their families in terms of personal suffering, reduced quality of life as well as for society in general due to direct costs of healthcare, and loss of income [3]. Nonadherence is associated with poorer functional outcomes, including greater risks of psychiatric hospitalizations, use of emergency psychiatric services, arrests, violence, victimization, suicide, poorer mental functioning, poorer life satisfaction, greater substance use, and more alcohol-related problems [1, 4–7].
Despite the widespread nature and serious consequences of nonadherence to antipsychotic medication regimens, there is an evidence that physicians may not be aware when their patients discontinue their medications and that they overestimate their patients’ adherence [1].
Interventions able to improve medication adherence in patients with schizophrenia would be beneficial in maximizing treatment outcomes with antipsychotics.
Studies that have specifically investigated adherence to psychiatric medications vary in the definitions of adherence and methodology used, making interpretation of results sometimes difficult. Numerous strategies have been proposed for improving adherence to treatment in patients with schizophrenia. The most successful strategies used a combination of educational, affective, and behavioral approaches. Interventions to improve adherence include encouraging acceptance of the illness, drawing analogies with treatment for chronic medical disease, and involving the patient in decision making. Clinicians must remain nonjudgmental, encouraging patients to disclose problems with adherence, and anticipating that improvement in adherence may require a prolonged effort [3, 8–11].
Factors Influencing (Non)Adherence in Schizophrenia
Medication taking is a complex health behavior that is affected by multiple factors that include treatment efficacy, side effects, clinician characteristics, treatment, illness beliefs, and sociodemographic factors [12]. Nonadherence can be viewed as either inadvertent or intentional [13]. Involuntary nonadherence occurs when signs or symptoms get in the way of taking medication (e.g., cognitive deficits), while intentional nonadherence results from a conscious decision on the part of the patient to discontinue medication. Unintentional dosage deviations and irregular adherence may further erode insight and therapeutic alliance resulting in the intentional discontinuation of antipsychotic treatment. Different interventions may be needed to address these different types of nonadherence [13].
The most common reason people do not take medication they intend to take is that they simply forget. This problem is compounded by the memory difficulties experienced by many patients with schizophrenia [14]. Furthermore, complex medication regimens are more difficult for people with schizophrenia to follow because of other cognitive problems, such as conceptual disorganization or inability to plan ahead [15, 16].
Patients with schizophrenia may not adhere to their prescribed medication regimen for several reasons (Table 1), including the following: illness awareness (lack of insight into illness, distorted, and ambiguous beliefs about treatment); psychopathology (psychotic symptoms, negative symptoms, and cognitive impairment); medication-related aspects (lack of early therapeutic response or inefficacy of antipsychotic medication, medication side effects, route of administration and dosing strategies); environmental factors (family and social support); lack of access to medications; substance abuse; therapeutic alliance [3, 10, 17–20].
Interventions to Enhance Adherence: Research and Clinical Evidence
Although antipsychotic medications are the mainstay of treatment for schizophrenia, pharmacotherapy alone produces only limited improvement in negative symptoms, cognitive functions, social functioning, and quality of life [2]. Additionally, many patients continue to suffer from persistent positive symptoms and relapses particularly when they fail to adhere to prescribed medications. This underlines the need for multimodal care including psychosocial therapies as adjuncts to antipsychotic medications to help alleviate symptoms and to improve adherence, social functioning, and quality of life [21, 22].
Despite the growing acceptance that medication nonadherence is a significant public health issue associated with financial, social, and illness costs, there is a limited amount of rigorous research on the use of specific interventions to target the problem. The available literature describes interventions of various types that have been utilized in schizophrenia. Some studies have specifically measured medication adherence as a primary outcome (primary outcome studies), while others described psychosocial interventions not used directly to address medication nonadherence, but that reported the effect of the intervention on adherence as a secondary outcome measure or as incidental finding (secondary outcome studies). Although the former provide more robust evidence, both types of study will be reviewed to give as much information as possible for translation into clinical practice [23]. Given the magnitude and importance of poor adherence to medication regimens, the WHO has published an evidence-based guide for clinicians, health care managers, and policymakers to improve strategies of medication adherence [24].
Several nonpharmacological strategies to enhance adherence in schizophrenia have been investigated. They include education sessions, memory aids, motivational interviewing, and cognitive behavioral approaches such as adherence or compliance therapy. Other suggestions such as optimizing therapy, for example by simplifying the regimen and considering side effect profiles with respect to individual patient characteristics, as well as fostering a good relationship between the patient and the healthcare professional, have been repeatedly mentioned. Studies demonstrate that no single strategy is effective for all patients and that a multidisciplinary approach customized to the patient’s individual needs results in improved adherence rates [3, 8–10, 17, 23, 25–27].
Experts’ recommendations reflect also the importance of individually tailoring medication regimens to improve adherence. It is crucial to select interventions that are likely to help eliminate the barriers that are interfering with adherence in the specific patient. Likewise, clinicians should keep in mind that the ultimate goal of any intervention is not medication adherence per se, but achieving the best possible outcomes for the patient [10, 28].
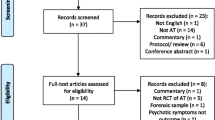
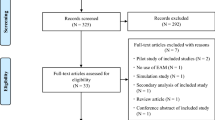
This systematic literature review focuses on studies examining psychosocial interventions to improve adherence to antipsychotic medications in patients with schizophrenia as a primary or a secondary outcome. Electronic searches were performed in the PubMed database and all studies published until April 2012 were included, without any language restriction. We found many kinds of psychosocial and programmatic interventions strategies for addressing adherence problems in schizophrenia that could have promising implications for clinical practice.
Comprehensive Review of Psychosocial and Programmatic Interventions to Enhance Adherence to Antipsychotic Medication in Schizophrenia
All the interventions and the strategies to improve adherence to antipsychotic medication in schizophrenia reviewed in this chapter are listed in Tables 2 and 3.
Psychoeducation
Psychoeducational interventions provide information to patients and family members about the disorder, its treatment, and strategies to cope with schizophrenia [2]. An extensive body of literature has accumulated regarding the efficacy of these interventions.
Meta-analyses [29–32] suggest that these interventions reduce high EE among relatives, and decrease relapse and rehospitalization rates. In general, interventions that include family members are more effective [33, 34].
-
(i)
Patient psychoeducation involves strategies (e.g., individual and group counseling, use of written or audiovisual materials) to teach patients about their illness, medication and their side effects, and relapse prevention. Studies of psychoeducation in schizophrenia have used a range of interventions, but the majority has focused primarily on dissemination of knowledge about schizophrenia and treatment options to achieve medication adherence without specific action on attitudinal and behavioral change.
Seltzer et al. [35] described a cohort study of 67 inpatients with schizophrenia (44), bipolar disorder (16), and unipolar depression (7), allocated either to a control condition or to a psychoeducation programe consisting of nine lectures about their disorder and its pharmacological treatment, combined with behavioral reinforcement for desirable medication routines. Due to the inclusion of this latter approach, Zygmunt et al. [25] suggested that this was not a purely educational intervention as it contained elements of behavior modification. At the 5-month follow-up, it was found that the intervention group had a nonadherence rate of 6 % according to urine test and 9 % according to pill counts, whereas the control group showed rates of 25 and 66 %, respectively. The study has been criticized because of a substantial dropout rate both in the intervention and in the comparison group, which raised concerns about possible attrition bias. Brown et al. [36] randomly assigned 30 patients to receive one of four interventions: verbal information about their medication but not about side effects; verbal and written information about their medication but not side effects; verbal information about medication and side effects; or verbal and written information about medication and side effects. Results showed that although patients’ knowledge about their medication improved with the interventions, this failed to translate into any change in adherence.
References [37, 38] reported that extended courses of group psychoeducation (35–75 sessions) did not significantly change adherence levels.
A further review by Dolder et al. [8] showed that only one of four educational interventions improved adherence.
Other studies found that psychoeducation used alone is not effective in improving medication adherence in schizophrenia [34].
In a randomized controlled study Maurel et al. [39] conclude that pharmacoeducation can reduce hospital stays of patients with schizophrenia and schizoaffective disorders, as well as improve their clinical and functional state, through better compliance.
In 2011 a Cochrane Database systematic review was made available, including a total of 5142 participants (mostly inpatients) from 44 trials conducted between 1988 and 2009 (median study duration ~12 weeks, risk of bias—moderate). Authors found that incidence of noncompliance was lower in the psychoeducation group in the short term; this finding holds for the medium and long term. Relapse appeared to be lower in the psychoeducation group. They concluded that psychoeducation did reduce relapse, readmission, and encourage medication compliance, as well as reduce the length of hospital stay at least in these hospital-based studies. However, they also indicated that the true size of effect is likely to be less than demonstrated in this review—but, nevertheless, some sort of psychoeducation could be clinically effective and potentially cost beneficial [40].
-
(ii)
Family psychoeducation Family psychoeducation has been shown to reduce relapse rates and facilitate recovery in persons with mental illness [41]. Psychoeducation for patients with schizophrenia that includes family members has been found to be more effective in reducing symptoms and preventing relapse than psychoeducation involving the patient alone [8, 34].
A trial by Xiang et al. [42] investigated family therapy in a rural province in China and showed significant benefits from this approach. The intervention group (n = 36) received a teaching program designed to provide family members with a basic knowledge of mental disorders and their treatment. The aim was to allow family members to understand the patient and his disorder and to understand how to care for the patient physically and psychologically. The intervention used family visits, workshops, and monthly supervision. At 4 months the rates of full adherence (patients were receiving a depot injection) were significantly improved in the intervention group (47 %) versus the control group (15 %), and the rates of full and partial adherence combined were 75 and 34 % in the intervention and control groups, respectively.
Two other studies showed positive results. In a rural area in China, Ran et al. [43] carried out a cluster randomized trial with 357 participants, in which three groups were compared. Intervention groups received depot medication, but one received in addition a monthly psychoeducational family intervention. After 9 months, 35 % of patients in the combined treatment group maintained regular treatment, in comparison with 32 % in the depot-only group and 5 % in the control group. The rates of patients who did not comply with treatment at all were 2 % in the combined group, 27 % in the depot group and 50 % in the control group, with accordingly increasing rates of relapse.
In a controlled trial, Chan et al. [44] investigated a psychoeducational program for patients and family caregivers in the urban area of Hong Kong. 73 patients were included and the intervention consisted of 10 family sessions of psychoeducation within a period of 3 months. One month after completion of the interventions, and again 6 months later, significant differences in favor of the intervention group were reported on adherence to medication, as measured by the ROMI, mental status, insight into illness in patients, self-efficacy, satisfaction, and perception of family burden in caregivers, yet these benefits were not sustained after 12 months of follow-up. They concluded that psychoeducation should be offered as an ongoing intervention.
Findings by the Munich Psychosis Information Project Study are described in the following two studies. In the first [45], the authors examined whether psychoeducational groups for patients with schizophrenia and their families could reduce rehospitalization rates and improve compliance 236 inpatients who met DSM-III-R criteria for schizophrenia or schizoaffective disorder and who had regular contact with at least one relative or other key person were randomly assigned to one of two treatment conditions. In the intervention condition, patients and their relatives were encouraged to attend psychoeducational groups over a period of 4–5 months. The patients and ‘relatives’ psychoeducational programs were separate, and each consisted of eight sessions. Outcomes were compared over 12 and 24-month follow-up periods. The rehospitalization rate after 12 and 24 months in patients who attended psychoeducational groups was significantly lower and degree of compliance higher than those obtained in patients receiving routine care (P < 0.05). The results suggest that a relatively brief intervention of 8 psychoeducational sessions with systematic family involvement in simultaneous groups can considerably improve the treatment of schizophrenia.
In the second intervention study [46], the same research group investigated the long-term effects of psychoeducation over a period of 7 years in regard to rehospitalization rates and hospital days. Of 101 patients with DSM-III-R or ICD-9 schizophrenia randomly allocated to either the intervention or the control group, 48 patients were available for follow-up after 7 years. Main outcome measures were rehospitalization rate, number of intervening hospital days, compliance, and mean number of consumed chlorpromazine (CPZ) units. Seven years after index discharge, the rate of rehospitalization was 54 % in the intervention group and 88 % in the control group. In the intervening period, the mean number of hospital days spent in a psychiatric hospital was 75 in the intervention group and 225 in the control group (P < 0.05). The mean number of consumed CPZ units was 354 in the intervention and 267 in the control group. Therefore, 7 years after psychoeducational group therapy, significant effects on the long-term course of the illness could be found.
In a more recent study [47] it has been investigated whether a culturally adapted, MFG, based on psychoeducation and skills training, would increase medication adherence and decrease psychiatric hospitalizations for Spanish-speaking Mexican-Americans with schizophrenia. There are 174 Mexican-American adults with schizophrenia-spectrum disorder with a recent exacerbation of psychotic symptoms and their key relatives were studied in a 3-arm, randomized controlled trial of MFG therapy focused on improving medication adherence. Assessments occurred at baseline and at 4, 8, 12, 18, and 24 months. Patients participated in one of two MFGs (culturally modified MFG-adherence or MFG-standard) or treatment as usual. Groups convened twice a month in 90-minute sessions for 1 year. At the end of the 1-year treatment, MFG-adherence was associated with higher medication adherence than MFG-standard or treatment as usual (P = 0.003). The MFG-adherence participants were less likely to be hospitalized than those in MFG-standard (P = 0.04) and treatment as usual alone (P < 0.001). Authors concluded that MFG therapy specifically tailored to improve medication adherence is associated with improved outcome for Mexican-American adults with schizophrenia-spectrum disorders.
On the other hand, other studies utilizing psychoeducation and family interventions failed to demonstrate an improvement in medication adherence [48, 49], as did an inpatient family intervention [50] and a family relapse prevention program [51].
A recent meta-analysis [34] has evaluated short and long-term efficacy of psychoeducation with and without inclusion of families with regard to relapse, symptom reduction, knowledge, medication adherence, and functioning. Randomized controlled trials comparing psychoeducation to standard care or nonspecific interventions were included. Independent of treatment modality, psychoeducation produced a medium effect size at post-treatment for relapse and a small effect size for knowledge. Psychoeducation had no effect on symptoms, functioning, and medication adherence. Effect sizes for relapse and rehospitalization remained significant for 12 months after treatment but failed to reach significance for longer follow-up periods. Interventions that included families were more effective in reducing symptoms and preventing relapse at 7–12 month follow-up. The most interesting finding is that psychoeducation offered solely to patients was ineffective. It was concluded that the additional effort of integrating families in psychoeducation is worthwhile, while patient-focused interventions alone need further improvement and research.
A 2010-Cochrane review estimated the effects of family psychosocial interventions in community settings for people with schizophrenia or schizophrenia-like conditions compared with standard care. Family intervention may decrease the frequency of relapse and may also reduce hospital admissions and encourage compliance with medication, but it does not consistently affect the tendency of individuals/families to drop out of care. Authors concluded that family interventions may reduce the number of relapse events and hospitalizations, but they also underlined that treatment effects of these trials may have been overestimated [52].
Behavioral and Cognitive-Behavioral Interventions
CBT seeks to help patients rationally appraise their experience of symptoms of disease and how they respond to them, thereby reducing symptoms and preventing relapse [53, 54]. Although CBT is recommended as a standard of care for persons with schizophrenia [55, 56], data from pragmatic studies suggest that its benefits are modest at best [57, 58]. We will analyze separately behavioral and cognitive-behavioral interventions (Table 4).
-
(i)
Behavioral Interventions assume that behaviors are acquired through learning and conditioning and can be modified by targeting, shaping, rewarding, or reinforcing specific behavioral patterns. Interventions include skills building, practising activities, behavioral modeling, and reinforcement strategies. Behavioral tailoring involves developing natural prompts by fitting the taking of medication into each person’s usual routine.
A number of studies have shown behavioral interventions to be successful in improving medication adherence.
Eckman et al. [59] investigated a behavioral program in improving adherence and medication management skills in 160 outpatients with schizophrenia. Patients followed a structured module in groups for about 3 h per week over 4 months. Adherence improved significantly from about 60 % preintervention to 80 % post-intervention.
Boczkowski et al. [60] randomly assigned 36 males with schizophrenia to behavioral training, didactic psychoeducation, or standard treatment. The behavioral intervention consisted of patients being told the importance of adhering to medication and each participant was helped to tailor the prescribed regimen so that it was better adapted to their personal habits and routines. This involved identifying a highly visible location for placement of medications and pairing the daily medication intake with specific routine behaviors. At a 3-month follow-up, there was a significant improvement in the behavioral intervention group compared with the other two groups. Totally, 8 out of 11 patients who had received behavioral therapy showed adherence with 80 % or more of their medication, whereas only three out of 11 in the psychoeducation intervention group showed such levels.
Cramer and Rosenheck [61] described a randomized controlled trial of 60 patients allocated to usual treatment or to the MUSE program that teaches simple techniques of how to remember daily medication doses to patients with severe mental disorders. The intervention consisted of an initial session of 15 min where the patient was taught to develop cues to remember the dose times. The intervention utilized electronic monitoring pill bottles with special caps that display the date and time of each bottle opening. Results showed significant improvement in the intervention group. The mean 1-month adherence rate was 81 % in the intervention group and 68 % in the control group, at 6 months the rate was 76 and 57 %, respectively.
Razali et al. [62] studied the effectiveness of culturally modified behavioral family therapy compared with a standard version of behavioral family therapy in 166 individuals. Post-randomization, there were 74 subjects in the culturally modified intervention group and 69 in the behavioral family therapy group. Adherence was measured globally as a percentage of the total prescribed dosages actually taken during the previous 6 months. At follow-up, 73 % in the group receiving culturally modified therapy as compared to 59 % in the control group were adherent with 90 % of their prescribed medication. At 1 year, rates were 85 and 55 %, respectively.
-
(ii)
Cognitive-Behavioral Interventions are focused on understanding patients’ perception of their problems and treatment. One of the major challenges in addressing the patient’s attitude toward medication is the degree to which patients with schizophrenia avoid acknowledging that they have an illness or need treatment in the first place. For patients who do not believe they need medication, environmental supports alone will not address the problem, but CBT may help. Because CBT focuses on changing attitudes, it may be ideally suited to addressing adherence problems in patients who do not believe they are ill. CBT include assessing patient perspective, examining evidence, and rolling with resistance. Rolling with resistance means not challenging the patient’s resistance to taking medication but exploring this resistance to better understand the patient’s viewpoint and help the patient re-evaluate beliefs about medication. CBT therapists help patients identify and modify negative automatic thoughts about medications and use guided discovery to help strengthen patients’ belief that taking medication is associated with staying well and achieving goals. The support for CBT to address lack of insight reflects findings from controlled trials showing that CBT significantly improves insight into the need for treatment and that even a brief CBT intervention can significantly improve symptomatology and insight [2, 63].
In schizophrenia, CBT to improve adherence often incorporates motivational interviewing techniques. First developed for use in addiction treatment, these techniques assess patients’ motivation to make changes in behavior related to adherence.
Lecompte and Pelc [64] tested a cognitive behavioral program targeted at changing adherence patterns through the use of five therapeutic strategies: engagement, psychoeducation, identifying prodromal symptoms, developing coping strategies and strategies for reinforcing adherence behavior, and correcting false beliefs about medication. There are 64 nonadherent patients with psychosis were randomly assigned to receive either the active intervention or a control treatment of unstructured conversation. The primary outcome measure was the duration of hospitalizations 1 year before and 1 year after the intervention, which the authors argued was a useful indirect measure of adherence. Patients receiving the cognitive behavioral intervention spent significantly less time in hospital in the year after as compared to the year before the intervention, but no significant difference was found relative to the control group. Although these findings suggest the intervention is beneficial, it is not certain that this improvement can be attributed solely to improved adherence.
Motivational Interviewing has been defined as “a directive client centered counseling style for eliciting behavior change by helping clients to explore and resolve ambivalence” [65]. Although behavioral analysis is used, motivational interviewing does not try to force the person into accepting the evidence of advantages of a new behavior but considers the value of letting persons progressively discover advantages and disadvantages of their behavior for themselves.
Hayward et al. [66] used an intervention of medication self-management based on motivational interviewing aiming to allow patients and clinicians to work collaboratively to examine medication issues. Twenty-one inpatients received three 30-min sessions of either medication self-management or nondirective discussion on any issue except medication. The pilot work showed trends in favor of the intervention group with regard to adherence and attitudes toward treatment but none reached statistical significance.
This led to the development of the longer, more structured intervention CT [67, 68] which modified motivational interviewing techniques to give particular attention to the therapeutic relationship and to make the approach useful with patients suffering from psychosis and combined this with cognitive behavioral techniques. CT is a CBT intervention that targets adherence issues and incorporates psychoeducation and motivational interviewing to help patients understand the connection between relapse and medication nonadherence to improve motivation for taking medication.
The therapy is described in detail in a treatment manual [69]. The key techniques are those of reflective listening, regular summarizing, inductive questioning, exploring ambivalence, developing discrepancy between present behavior and broader goals, and using normalizing rationales. The intervention is divided into three phases that acknowledge that readiness to change is on a continuum. Phase 1 deals with patients’ experiences of treatment by helping them review their illness history. In phase 2 the common concerns about treatment are discussed and the “good” and the “bad things” about treatment are explored. Phase 3 deals with long-term prevention and strategies for avoiding relapse. Despite its name, CT appears to fit with a concordance model, involving patients in making decisions that are right for them, rather than trying to get them to be obedient to professional advice.
In a small-scale study, Kemp et al. [68] found that CT significantly improved insight, attitudes toward treatment, and adherence in patients with schizophrenia. The same research group reported a randomized controlled trial of 74 patients with psychosis allocated to 4–6 sessions of CT versus 4–6 sessions of supportive counseling [70]. Results demonstrated a significant effect on adherence in the intervention group as compared to the control group immediately post-treatment and at an 18-month follow-up. The improvements in compliance did result in enhanced community tenure, with patients in the CT group taking longer to relapse than those receiving nonspecific counseling. CT is effective in enhancing concordance and reducing the risk of relapse. There is also emerging evidence that after training in medication management, mental health nurses are able to deliver compliance therapy to people with a diagnosis of schizophrenia [71].
In contrast to the above studies, O’Donnell et al. [72] conducted a randomized controlled trial comparing CT with nonspecific counseling in a 1-year study of 56 inpatients with schizophrenia. No effect of CT over a control group was identified. The study did show that attitudes to treatment at baseline predicted adherence at 1 year, thus suggesting early identification of attitudes toward medication may be useful in clinical practice. Noticeably, this study had a longer period of follow-up (1 year), while the two previous studies had shorter periods of follow-up assessment (3 and 6 months). Although the study by Kemp et al. had further assessments at 12 and 18 months, their booster doses of the intervention at 3, 6, and 12 months may have influenced its long-term outcome.
Byerly et al. [73] evaluated the efficacy of CT when delivered to outpatients with schizophrenia or schizoaffective disorder. Thirty patients with schizophrenia or schizoaffective disorder were recruited from urban psychiatric outpatient clinics in an open trial of CT. The primary outcome was electronically measured antipsychotic medication adherence. Adherence data were analyzed for effects during an initial treatment period (month −1 to +1) and a subsequent 5-month follow-up period. Secondary outcome measures included clinician and patient ratings of adherence, symptoms, insight, and attitudes toward medication treatment. Patient ratings of adherence improved during the month −1 to +1 period, but not in the subsequent 5-month follow-up. Authors found that CT was not associated with improvements in antipsychotic medication adherence and they concluded that outpatients with schizophrenia or schizoaffective disorder did not benefit from CT schizophrenia.
In a 2006 Cochrane review on CT, McIntosh et al. [74] assessed systematically the effects of this intervention on antipsychotic medication adherence in schizophrenia. Authors concluded that there is no clear evidence to suggest that CT is beneficial for people with schizophrenia and related syndromes, and that more randomized controlled studies were needed in order to fully examine this intervention.
CT was slightly modified into AT, a brief individual cognitive behavioral approach [75]. The AT manual (http://www.adherencetherapy.com) describes a collaborative, patient-centered phased approach to promote treatment adherence, patient choice, and shared decision-making in subjects affected by schizophrenia. Techniques derived from cognitive behavioral therapy (e.g., testing out beliefs about treatment) and motivational interviewing (e.g., exploring patient ambivalence toward treatment) are used to enhance adherence to a shared treatment plan focused on medication adherence and illness management. The key therapeutic techniques used are exchanging information, developing discrepancy, and effectively dealing with resistance. The phases of AT are engagement, assessment, rating of readiness to take medication, intervention, and evaluation working through in a flexible patient-centered way. The five key interventions from the core of the therapy phase include: (1) medication problem solving; (2) medication timeline; (3) exploring ambivalence; (4) discussing beliefs and concerns about medication; and (5) using medication in the future. The aim of the therapy process is to achieve a joint decision about medication between the patient and therapist.
A study in Thailand [76] found that AT delivered by nurses who received intensive training significantly improved psychotic symptoms and attitude toward and satisfaction with medication. Thirty two patients with schizophrenia were randomly allocated to receive eight weekly sessions of AT or continue with their TAU. Patients were assessed at baseline and after 9 weeks. The primary outcome was overall psychotic symptoms. Secondary outcomes were general functioning, attitude toward and satisfaction with antipsychotic medication, and medication side effects. The findings indicated that patients who received AT significantly improved in attitude toward and satisfaction with medication compared with TAU.
A large European 52-week, single-blind, multicentre randomized controlled trial, with a small increase in the number of sessions (two extra sessions) and a more individually tailored structure, including 409 patients in four countries, did not find any differences between AT and a control group receiving an individual intervention of health education, nor were quality of life, or rates of patient-reported medication adherence different between groups. This effectiveness trial did not confirm any effect of AT in improving treatment adherence in people affected by schizophrenia with recent clinical instability, treated in ordinary clinical settings [75].
A further pragmatic, exploratory, single-masked trial, to explore the efficacy, acceptability, and satisfaction with AT was conducted in the USA, in a sample of people with schizophrenia [77]. Twenty six patients (12 experimental and 14 controls) were randomly allocated to receive eight weekly sessions of AT or continue with TAU. Patients were assessed at baseline and after therapy completion, while the primary outcome was psychiatric symptoms and the secondary outcome medication adherence. Patients receiving AT did not significantly improve in overall psychiatric symptomatology or in medication adherence compared with the TAU group at follow-up. The results indicated no significant difference between the AT and TAU groups on measures of severity of symptomatology and subjective evaluation of treatment, including medication adherence from baseline to follow-up after the completion of the intervention.
Another adaptation of CT is called ACE, which aims at enhancing insight and at promoting treatment adherence in patients with early psychosis. In a pilot study this intervention, consisting of 14 individual sessions, was tested against supportive therapy [78]. In a sample of 19 participants, perceived need for treatment and benefits of medication appeared to be better in patients with ACE shortly after intervention, compared to controls. However, no direct adherence rates were available and follow-up results are awaited.
Staring et al. [79] developed another treatment, TAT, whose intervention modules are tailored to the reasons for an individual’s nonadherence. In a recent randomized controlled trial therapy they measured the effectiveness of TAT with regard to service engagement and medication adherence in 109 outpatients with psychotic disorders. TAT is an intervention based on an empirical–theoretical model, in which patient’s determinants of nonadherence are taken into account. According to the clusters of determinants of nonadherence, therapists choose the intervention tailored to each patient. The duration and number of sessions therefore varied according to the needs of the individual patient, in general, it took no more than 6 months. Most of the TAT therapists were trained psychiatric nurses. The study found that TAT may enhance service engagement (Cohen’s d = 0.48) and medication adherence (Cohen’s d = 0.43) more than TAU. The effects were smaller at 6-month follow-up, yet still statistically significant for medication adherence.
-
(iii)
HBM summarizes the process by which the patient weighs the cost of treatment against benefits, assuming adherence to the treatment if the benefits are seen to be greater than the costs and risks [80–82]. The HBM is one of the most known model of behavior change and it has been developed to explain why people failed to take up disease prevention measures or screening tests before the onset of symptoms [80, 83]. The original model proposed that the likelihood of someone carrying out a particular health behavior (e.g., attending for screening) was a function of their personal beliefs about the perceived threat of the disease and an assessment of the risk/benefits of the recommended course of actions. The individual weighs up the perceived benefits of an action (e.g., taking medication might ease symptoms) against the perceived barriers to the action (e.g., fear of side effects or costs of the treatment). The HBM assumes that four main beliefs contribute to the likelihood of individuals adhering to their prescribed medication:
-
perceived benefits of adherence (e.g., possibility of being symptom-free)
-
perceived barriers to adherence (e.g., stigma or problems with side effects)
-
perceived susceptibility to illness (e.g., a belief that they are likely to experience a relapse)
-
perceived severity of the outcome (e.g., a belief that relapse would have negative consequences).
-
It is proposed that individuals are more likely to adhere to medication if the perceived threat of the illness (susceptibility and severity) is high and the perceived benefits of treatment exceed the perceived barriers.
Compliant patients consider the medication to be helpful in treating their illness and have a positive attitude toward medication [84–86]. Conversely, noncompliant patients see no reason for taking medication because they may not consider themselves to be ill, or they may see taking the medication as the wrong way to solve their problems [87–91].
The beliefs described are influenced by a number of modifying factors [92] such as:
-
personality attributes (e.g., dysfunctional attitudes and health locus of control)
-
influence of significant others (e.g., family and mental health professionals)
-
cultural beliefs and context
-
general health motivations
-
general orientation toward medicine
The model also states that individuals need a prompt (a reminder either of the threat of the illness or the action that must be taken against it) before they will engage in health-related behaviors [93]. These “cues to action” may be internal, such as recognition of prodromal symptoms, alternatively, the cues may be external, such as statements made by others, or media references to illness or medication (Fig. 1).
This model emphasizes the collaboration between physician and patient in treatment decisions. The critical factor for successful management of adherence is creating an atmosphere where a nonadherent or potentially nonadherent patient does not feel disapproved and so he will be able to talk honestly about his concerns related to drug treatments and pattern of adherence [82].
The clinician needs to have a clear picture of the patient’s cognitive representation of the illness. If patients acknowledge partial or total nonadherence, it is useful to try to decide whether this is unintentional or intentional. Un-intentional nonadherers tend to identify a higher number of perceived barriers to treatment. Most of these are practical rather than psychological. Intentional nonadherers often demonstrate more ambivalence about the perceived threat of the disorder and are probably less likely to acknowledge their nonadherence without prompting. In practice, it is likely that both groups will benefit from the behavioral interventions, but that the cognitive techniques will have a more obvious role with intentional nonadherers. The primary goal with unintentional nonadherers is to enhance cues to action and to minimize any real or perceived barriers to adherence [13].
The HBM posits that health behavior is a product of an implicit and subjective assessment of the relative costs and benefits of compliance in relation to personal goals and the constraints of everyday life. HBM has proven helpful in addressing adherence in medical illness, however, it must be used cautiously in patients with schizophrenia. Disease-related symptoms such as cognitive impairment and poor reality testing may limit a patient’s ability to perceive the benefits of antipsychotic therapy. Since schizophrenia may disrupt illness perception and the capacity to plan and act, consideration of the cognitive and motivational resources available to assess risk, and formulate action should be additional elements to take into account when dealing with patients suffering from schizophrenia [13, 84–91].
Patients affected by schizophrenia weigh the benefits of antipsychotic treatment such as symptom reduction with the associated costs of antipsychotic treatment such as side effects. Benefits of antipsychotic treatment are largely dependent on the patient’s knowledge about illness and belief that the treatment may has a positive effect on the severity of their symptoms. The HBM emphasizes the patient’s as opposed to the physician’s understanding of illness and treatment [94]. Perceived benefits of treatment are largely dependent on the patient’s illness awareness and insight. Insight has been one of the most common predictors of adherence problems [94, 95] and it is not necessarily found in all patients who are adherent with antipsychotics [96]. Most patients have some ambivalence about taking antipsychotic medications, all of which can be associated with unpleasant and, rarely, dangerous side effects. On the other hand, patients with good insight into their symptoms or illness may not perceive their prescribed medication as potentially or actually helpful. Patients who do experience troublesome or serious side effects may decide that these effects outweigh the benefits of medication. If a patient stops taking medication during the stable phase, he may feel better, with less sedation or other side effects. As a result, the patient may come to the false conclusion that the medication is not necessary or does not have benefits. Finally, people significant to the patient, including family and friends, may discourage the patient from taking medication or participating in other aspects of treatment.
HBM may help clinicians to develop methods to improve adherence. To help clinicians learn how to adapt CBT for assessing adherence attitudes, Velligan et al. [97] have developed a method called the HBD. The underlying concept of this interview approach is very simple. The authors believe that attitudes or beliefs cannot be changed before the clinician understands those attitudes and beliefs. Too often patients’ perspective is interrupted by a well-meaning but ineffective lecture about the benefits of medication and the importance of adherence. In contrast, a major goal of the HBD approach is forcing the clinician to withhold any intervention or comment on adherence attitudes until those attitudes are fully understood [97].
Perkins [94] has modified the HBM in the context of schizophrenia and underlined the relevance of improving patient’s assessment of the costs and benefits of treatment. This may require targeting a diverse area of risk factors for nonadherence such as poor insight, negative attitudes toward medications, substance abuse, and alliance with therapist. When clinicians detect the presence of any of these risk factors for nonadherence, strategies to address these issues and interventions to improve adherence should be implemented. Successful aspects of the interventions reviewed can be easily incorporated by clinicians to improve adherence with antipsychotic therapy such as, providing information about the purpose and potential side effects of medications (psychoeducation); helping patients to cognitively reframe negative attitudes and learn to become more effective consumers (behavioral and affective); and simplifying regimens, teaching skills, and providing external cues such as medication reminder devices (behavioral) [8].
Perceived benefits of treatment also include the therapeutic relationship. The quality of the therapeutic relationship is related to medication adherence [98, 99]. In a cross-sectional and longitudinal adherence study with 162 patients, working alliance was most consistently related to medication adherence [100]. Patient satisfaction in the physician–patient relationship may lead to a greater willingness to follow the physician’s advice independent of the level of insight of the patient.
Costs of treatment include the patient’s perception of medication side effects. When patients perceive adverse effects as problematic or unacceptable they may lead to poor adherence. On the contrary patients will often continue to take medication despite unpleasant side effects if they perceive the benefits of medication as outweighing the disadvantages caused by side effects [101].
There are studies suggesting a correlation between dimensions of the HBM and adherence in schizophrenia.
Budd et al. [102] found an association between beliefs around susceptibility and adherence status, that is, those who did adhere to medication perceived themselves to be more susceptible to relapse than nonadherers. They conducted a study of the impact of the HBM in schizophrenia patients in Wales comparing 20 patients who had presented for, and accepted, depot antipsychotic medication at all scheduled appointments over the year prior to the study (compliers) with 20 patients who had failed to attend and/or accept medication for one-third or more of all scheduled appointments over the same period (noncompliers). The constructs of the HBM were evaluated using a HBQ [103, 104]. The authors found that scores on the susceptibility subscale had the greatest discriminatory power in distinguishing compliers from noncompliers. Scores on the severity and benefits subscales were significant in distinguishing between the two groups when tested in separate analyses, but were not significant when added to a model that already contained the susceptibility subscale.
Adams and Scott [105] explored the utility of the HBM in explaining medication adherence in subjects with severe and disabling mental disorders. Six well-established measuring instruments, with confirmed reliability and validity, were used to assess each component of the HBM and medication adherence in 39 hospital-treated subjects with severe mental illness. Highly adherent and partially adherent subjects differed significantly in their perception of illness severity, their beliefs about themselves and their control over the disorder, and their concerns about further hospitalization. Two components of the HBM (perceived severity of illness and perceived benefits of treatment) explained 43 % of the variance in adherence behavior. Although the study has a number of methodological limitations, the results suggest that clinical assessment of components of the HBM may improve the detection of patients at risk of medication nonadherence.
Fenton et al. [98] categorized the range of factors affecting adherence into patient-related, medication-related, environmental factors, and psychodynamic considerations. They identify patient-related factors as: demographic characteristics such as gender and ethnicity, illness characteristics such as age at onset and duration of illness, illness severity and subtype (e.g., paranoid schizophrenia), cognition or memory, insight, other health beliefs (i.e., attitudes toward medication), subjective well-being, and alcohol and drug use. The medication-related factors reviewed were side effects, dosage, agent, route, and complexity of regimen. Environment factors considered were: family and social support, practical barriers (e.g., financial burden preventing patient from filling prescription), physician–patient relationship, attitude of staff, reinforcement, education, and memory enhancement. Psychodynamic considerations include: psychological meaning (e.g., feelings about the role of authority and control in the prescribing of medications) and psychological homeostasis (e.g., relationship between delusions and self-image). The analyses would also have been improved with inclusion of a measure of patients’ attitudes toward their medication, their insight and general cognitive functioning [106], and perceptions of their quality of life. A positive view of psychiatric medications and patient insight has been shown to improve adherence [107]. These factors may be associated with the HBM, which Oehl et al. [108] suggest is a major determinant of adherence.
Although HBM may require modification in disorders like schizophrenia [109, 110], it should facilitate a shift in perspective: rather than viewing noncompliance as the patient’s problem, it is redefined as an indication that the therapeutic regimen is not assisting the individual patient to achieve his goals. Few studies have been done, but one small study demonstrated that patients with schizophrenia lack consistently coherent beliefs about their health, and beliefs may vary with mental status [111]. Persons with medical illnesses distinguish between themselves and their illness, whereas persons with schizophrenia often describe psychotic symptoms as part of themselves. Although many may not believe that they are ill, patients who acknowledge mental illness often do not view themselves as an entity separate from their mental illness. Recovery models, which address adherence, fall short because patients may not be able to conceptualize recovery or the need to recover because they cannot conceptualize their illness or a need to be well. Kinderman et al. [111] advocated more research into health beliefs in schizophrenia and speculated that assessing the patient’s concept of psychotic episodes may be more beneficial and fit better with the patient’s concept of his difficulties.
Medication Monitoring/Environmental Supports
Many studies focused on specific support for cognitive impairment, based on the assumption that nonadherence in patients with schizophrenia may be partly due to cognitive difficulties in attention or memory [17]. One approach to overcome these problems is to teach patients how to use devices to help take their medication correctly [10]. Medication monitoring and environmental supports include dispensing doses, directly observing medication taking, providing environmental supports at home as reminders to take medications and fill prescriptions, helping people deal with practical barriers to come to appointments or refilling prescriptions. A wide range of pill-organizing boxes is available for storing medications in separate compartments based on the day and time-of-day they are supposed to be taken. Pill organizers may contain the pills for a single day (which can be easily carried around in a purse or pocket), a week, or a month. When a prescription is filled, the patient, nurse, or pharmacy fills the pill organizer so that all of the pills that need to be taken at a particular time of day are stored together. Pill organizers are useful for keeping track of what medications need to be taken and when, but they often don’t address the problem of people simply forgetting to take their medication. Many patients find alarms are effective to serve this function. Some pill organizers also contain alarms or reminder chimes that can be set to prompt people to take medication. Other patients may find it more convenient to set a reminder alarm on something they frequently carry with them, such as a wrist watch, cell phone, MP3 player, or electronic scheduler. The experts considered medication monitoring/environmental supports as the first-line choice for addressing nonadherence in patients with cognitive deficits. Clinicians should note that environmental supports are not likely to be used unless they are customized for the individual patient and set up in the home environment [112, 113].
A program called CAT appears to be a promising strategy to improve adherence [114–116]. CAT is a manual-driven series of environmental supports designed to bypass problems in attention, memory, and executive functions, cue and sequence appropriate behaviors, and discourage inappropriate behavior at home. It is an intervention employing a series of compensatory strategies based on neuropsychological, behavioral, and occupational therapy principles. Training includes a neuropsychological assessment to examine the level of executive functioning, attention, and memory. Cognitive adaptation focused on medication adherence uses individually tailored environmental supports (e.g., signs, checklists, alarms, electronic cuing devices, organization of belongings) to cue adaptive behavior in the patient’s own home environment and help compensate for cognitive deficits. It also addresses logistic issues related to obtaining appointments. CAT supports are offered to the client during home visits on a weekly basis to address specific problems. An extensive intervention (full-CAT) tackling several aspects of functioning (poor hygiene, grooming, care of living quarters, leisure skills, social and role performance, and medication adherence) was compared with cognitive adaptation focusing only on adherence to medication and appointments (Pharm-CAT) and with a control group receiving TAU, in a randomized trial with 105 participants [28]. The intervention was carried out for a period of 9 months with a follow-up of 6 months. It resulted in significantly better adherence to medication for both intervention groups, as measured by unannounced pill counts. Average adherence rates were roughly 80 % in the intervention groups during the 15 months of the intervention and follow-up, compared to 60 % in the TAU group. The percentage of relapse for both intervention groups was 35 % against 81 % for the control group. This effect was maintained for 6 months after the intervention was completed. Outcomes of social and occupational functioning improved only with full-CAT, with a deterioration after the intervention stopped, suggesting that these aspects probably ask for continued intervention. The authors concluded that targeted supports can improve adherence and reduce relapse rates, but that comprehensive supports targeting multiple domains are necessary to improve functional outcomes.
In another study Velligan et al. [117] examined the short-term efficacy of CAT and GES to improve target behaviors in individuals with schizophrenia. GES include hygiene supplies, pill containers, and calendars offered to individuals at the time of their regular clinic visits. In GES, clients are expected to set up the supports on their own, supported by a tape recording of the therapist discussing where and how to use the supports in the home environment. One hundred and twenty outpatients with schizophrenia or schizoaffective disorder were randomized into one of the following three treatment groups: (1) CAT—individualized supports established on weekly visits in the clients’ homes; (2) GES—a generic group of environmental supports provided at a routine clinic visit; and (3) TAU. Global level of functional outcome and target behaviors, including medication adherence, were assessed at baseline and after 3 months. Patients in both CAT and GES had better scores on global functional outcome at 3 months than those in TAU; on the other hand, patients in CAT were more likely to improve on target behaviors, including medication adherence, than those in GES.
Another study to compensate for attention and memory problems used a Pharmacy-Based Intervention, called Meds-Help Intervention [118]. A low-complexity pharmacy-based intervention for patients with severe mental illness was developed, designed to reduce medication access barriers and to provide ‘‘cues to action’’ to help patients remember to refill prescriptions and take scheduled doses. In a randomized controlled trial with 118 participants of which 67 % had a schizophrenia-spectrum disorder, the intervention group received unit-of-dose packaging for all the medication they were taking and a packaging education session; refill reminders were mailed 2 weeks before the scheduled refill dates. Also, clinicians received notification when a patient failed to collect his antipsychotic prescriptions. Statistically significant improvements in MPR were observed in the intervention group after 6 and 12 months, compared with a control group that received care as usual. When a more stringent measure of adherence was used, by combination of a MPR of greater than 80 % with a positive subjective assessment of adherence and a blood test indicating the presence of some antipsychotics, 50 % of the intervention group fulfilled the criteria of adherence after 6 months versus 17 % in the control group. Authors conclude that this low-complexity pharmacy-based intervention is feasible in clinical practice and increased antipsychotic adherence among patients with severe mental illness.
Recent research focused on telephonic interventions and new technologies to assess and enhance adherence and treatment outcomes in persons diagnosed with schizophrenia. Reminders with SMS text messages in one study [119] did not lead to better adherence. These authors evaluated the efficacy of SMS text messages to compensate for the effects of cognitive impairments in daily life. Sixty two people with schizophrenia or related psychotic disorders were included in the study. Patients were prompted with SMS text messages to improve their everyday functioning. The overall percentage of goals achieved increased with prompting, but performance dropped to baseline level after withdrawing the prompts. Keeping appointments with mental health workers and carrying out leisure activities increased with prompting, while medication adherence and attendance at training sessions remained unchanged.
The TMM program was designed as a brief (no more than 10 min), weekly telephone-based intervention with the following goals: (1) provide verbal reinforcement for positive self-care behaviors (e.g., adhering to treatment regimen and clinic attendance); (2) encourage frank discussions about treatment- related issues; (3) validate participant’s medication and treatment experience; (4) assist problem solving on strategies to enhance self-care. TMM was an adjunctive service that ultimately aimed to enhance communication, insight into illness, attitudes and knowledge about treatment, medication adherence, treatment satisfaction, and decrease treatment side effects. A randomized demonstration study was conducted at a large, urban community mental health center to examine the feasibility and costs associated with TMM and to assess the outcomes of such an approach [120]. A total of 32 persons affected by schizophrenia-spectrum disorder were enrolled. Fourteen were randomized into the control group and 18 into the TMM condition. Results suggest that TMM was acceptable to patients and could be feasibly delivered. Although the direction of positive effects was consistently in favor of the TMM intervention, no apparent differences in treatment adherence were found, despite positive changes in other areas (e.g., insight and staff relationships) found to be associated with adherence. The results are promising enough to justify further study of this approach that requires few additional resources.
A relatively small study reports a positive effect of a Telephone-Nursing Intervention, called TIPS. This intervention comprises weekly calls by psychiatric nurses, trained to help patients with problem solving, offering reminders and coping alternatives with regard to common medication adherence barriers [121]. Overall adherence rates during the 3 months of the study were 80 % in the intervention group, versus 60, 1 % in the control group, as measured in 3-monthly pill counts in an outpatient sample of 29 participants.
Spaniel et al. [122] tested an ITAREPS that uses a mobile phone-based telemedicine strategy to remotely monitor patients with schizophrenia on a weekly basis to identify prodromal symptoms of relapse, enable early intervention, and reduce hospitalizations. ITAREPS produced a statistically significant 60 % decrease in hospitalizations over a mean of 9 months compared with the same period before entry in the program. Variables influencing number of hospitalizations after entry in ITAREPS were adherence to medication and the involvement of a family member.
Performance on a novel, virtual reality assessment of medication management skills, the VRAMMA, was investigated in 25 patients with schizophrenia and 18 matched healthy controls [123]. The VRAMMA is a virtual 4-room apartment consisting of a living room with an interactive clock and TV, a bedroom, a kitchen, and a bathroom with an interactive medicine cabinet. After an exploratory phase, participants were given a mock prescription regimen to be taken 15 min later from pill bottles located in the medicine cabinet in the bathroom of the virtual environment. Results revealed that (1) schizophrenic patients made significantly more quantitative errors in the number of pills taken, were less accurate at taking the prescribed medications at the designated time, and checked the interactive clock less frequently than healthy controls; (2) in patients with schizophrenia, years of education and a measure of verbal learning and memory were linked to quantitative errors on the VRAMMA. This is the first study to provide evidence for the utility of VR technology in the assessment of instrumental role functioning in patients with schizophrenia.
The application of Schizophrenia Clinical Practice Guidelines in everyday health care are still described as unsatisfying. Within the project “Guideline-supported quality management in outpatient treatment”, Janssen et al. [124] investigated whether guideline adherence and quality of outcome can be improved by implementing a computer-based, guideline-oriented decision-support system. Therefore, a disease-specific decision-support system was developed interactively presenting guidelines to support the physicians’ decision-making process during the treatment of schizophrenic patients. It has been observed a strong initial but time-limited improvement with respect to the core aspects of outpatient treatment in schizophrenia in the experimental group. The findings suggest that decision-support systems can be used to enhance treatment outcome, medication compliance, and appointment adherence in schizophrenia outpatient care.
Community Interventions
Different models of community-based care have been developed to meet the diverse needs of patients with severe mental disorders. The key components of such interventions are the provision of a strong and supportive social network, close monitoring of clinical status including the medication regimen, provision of stable housing, and other supportive services [125]. Zygmunt et al. [25] noted that some community studies reported significantly greater medication adherence, although few of the studies included a rigorous assessment of such adherence.
ACT [125] and CM [126] were developed in the 1970s in response to closing of psychiatric hospitals.
ACT is an approach to provide services to patients with very severe mental illness who have difficulty accessing mental health-center-based services on their own. ACT offers an approach to integrated delivery of clinical services to patients with schizophrenia using a multidisciplinary approach, high frequency of patient contact, low patient-to-staff ratios, and outreach to patients in the community [2]. Supervision of medication follow through and close monitoring of symptoms are common activities of ACT teams. ACT, compared to routine care, has been found to significantly reduce hospitalizations and improve housing stability [127–129]. Although ACT appears to be an effective method of treatment delivery, the critical components which contribute to its benefits have not been precisely defined [25, 130].
Stein and Test [131] described a conceptual model of community treatment that encompasses six areas. These are material resources, coping skills to meet the demands of community life, motivation to persevere and remain involved with life, freedom from pathologically dependent relationships, support and education of community members who are involved with patients, and a support system that assertively helps patients with the previous requirements. They describe implementation of this programme, which they entitled ‘Training in Community Living’, and compared this with short-term hospitalization plus after care. At 8- and 12-month follow-up, adherence with antipsychotic medication in the experimental group was significantly improved compared with the control group. Following the intervention, when patients returned to traditional community programmes, these benefits were lost.
Ford et al. [132] compared intensive CM with standard CM and also showed improvement in medication adherence at 18 months.
However, other studies of enhanced care management versus standard care failed to show improvement. For example Bond et al. [133] compared ACT with standard CM and at 6 months there was no difference in adherence between the groups. Similarly, Solomon and Draine [134] compared intensive consumer CM with intensive CM and showed no difference in medication adherence between the two groups at 2 years.
Dixon et al. [135] noted that despite the uneven quality of research into the effects of community care programs on medication adherence, many programs closely monitor patients with a history of nonadherence and consider regular medication use as an important treatment goal. It is suggested that the reduction in hospitalization associated with such models of care may in part be a consequence of improved medication adherence.
About the adherence in Supported Housing Projects, a cross-sectional naturalistic survey of adults with schizophrenia living in supportive housing facilities in New York City by Grunebaum et al. [107], showed that direct supervision of medication was associated with better adherence. The main finding was that medication supervision was related to the duration of medication nonadherence. The data suggested that medication supervision is more important than medication type or regimen complexity in determining medication adherence within residential facilities. Previous studies have shown that supervision of medication by family members or friends is associated with better adherence [98] but persons living in supportive housing are often without significant others to supervise their treatment. The results of this pilot study suggest that residential staff could take over this function and improve adherence by supervising medication administration.
An Expert Consensus Guidelines on the Treatment of Schizophrenia (1999) recommended programmatic interventions (e.g., ACT, partial hospitalization, rehabilitation services), especially for severely impaired and unstable patients [136].
In a 2000 Cochrane review on these interventions, Marshall and Lockwood [125] reported that patients in ACT were more likely to stay in contact with services, were less likely to be hospitalized, and were more satisfied with care than those in standard community care; however, they found CM to be of questionable value and doubted it should be offered by community psychiatric services [125, 126]. It is noteworthy that service-based interventions implicitly target the issue of engaging the patient with their key worker or developing a strong link to a support service such as day care or supported housing. Having established a working alliance, many of the other interventions used in these programs incorporate problem-solving and behavioral strategies noted to be useful in promoting adherence in the primary outcome studies. Therefore, it is not surprising that about 50 % of studies of service-based approaches to the care and treatment of severe mental disorders also report a significant improvement in medication adherence [25].
Case managers or other members of the patient’s treatment team (e.g., nurses) can play a valuable role in helping patients follow through on overcoming barriers to taking medication [137]. Many patients are capable of learning how to organize their medications with pill boxes, but require considerable practice before they are able to safely do it on their own. A case manager can demonstrate, observe the patient, and guide him or her toward competence at this skill. Some patients may not be capable of learning how to organize their medications on their own, but can take them safely as directed once they have been organized for them by the case manager. Behavioral tailoring to natural prompts such as brushing one’s teeth is often most effectively implemented when a case manager can make one or two home visits. A home visit provides valuable information about the environment in which the patient lives, having the advantage of cueing the case manager about possible obstacles to implementing the behavioral tailoring plan.
Two studies in the last decade focused specifically on training of psychiatric nurses. In a randomized controlled cluster trial, Gray et al. [138] examined a medication management training package for Community Mental Health Nurses. Half of the 52 participating nurses received the training package, consisting of side effects management as well as training in effective treatment strategies for schizophrenia. The other half of the group of nurses received no training and delivered treatment as usual. At the 12-month follow-up, 29 patients treated by the trained nurses improved significantly in adherence rates on a clinician rating scale and on patient attitudes toward medication, as well as on symptomatology, compared with a group of 24 patients receiving care from the nontrained nurses.
In a comparable study [139] six US Department of Veteran Affairs medical centers (total participants 349) received basic guideline implementation strategies for the treatment of schizophrenia. Three of the six medical centers received an enhanced implementation strategy, in which physicians were trained to prescribe guideline-concordant. In addition, a research nurse identified barriers of adherence in patients: the nurses were trained in a protocol designed to assess medication adherence, strategies to maintain contact with the patients and provide feedback to the physician about adherence (barriers) and treatment preferences. Patients who received an enhanced guideline implementation strategy, in which a research nurse worked with them to identify and develop patient-specific strategies to overcome barriers to medication adherence, were almost twice as likely to be adherent at follow-up after 6 months. These data suggest that a patient-centered strategy to identify and overcome barriers to adherence can improve adherence to antipsychotic medications.
Psychosocial Interventions Additional to Pharmacological Treatments
Guidelines for the treatment of schizophrenia recommend the combination of pharmacologic and psychosocial interventions [2]. However, there is a lack of data on the utilization and effects of psychosocial interventions additional to neuroleptic treatment in routine care of schizophrenic patients. Linden et al. [140] investigated in 1711 schizophrenic outpatients the effectiveness of an antipsychotic treatment alone or in combination to a psychoeducation treatment. Psychosocial interventions were reported in 30 % of all patients. After 6 months of treatment with olanzapine, patients improved significantly in respect to their schizophrenic symptoms, psychosocial functioning, and quality of life. Patients receiving additional psychoeducation showed a higher degree of improvement than the other patients. They were more ill at the beginning of the study, but less ill at the end. Patients receiving psychoeducation showed also a trend to better medication compliance. The somewhat better adherence rate in psychoeducation patients (2.07 % vs. 4.60 % drop outs) raises the question of whether an optimization of drug treatment may improve the patient’s health status. In fact, the data suggest that treatment outcome can become even better, if drug treatment is combined with psychoeducation.
Guo et al. [141] evaluated the effectiveness of antipsychotic medication alone versus combined with psychosocial intervention on outcomes of early-stage schizophrenia. Patients were randomly assigned to receive antipsychotic medication treatment alone or antipsychotic medication plus 12 months of psychosocial intervention consisting of psychoeducation, family intervention, skills training, and cognitive behavior therapy administered during 48 group sessions. 1268 patients completed the baseline assessment; 633 were assigned to receive antipsychotics combined with psychosocial intervention and 635 to receive antipsychotics alone. Overall, 744 patients (60.0 %) completed the 1-year follow-up: 406 (67.2 %) in the combined intervention group and 338 (53.2 %) in the antipsychotics-alone group. The rates of treatment discontinuation or change due to any cause were 32.8 % in the combined treatment group and 46.8 % in the medication alone group. Comparisons with medication treatment alone showed lower risk of any cause discontinuation with combined treatment (P < 0.001) and lower risk of relapse with combined treatment (P < 0.001). Nonadherence was noted in 2.8 % of patients in the combined treatment group and 5.7 % of patients in the medication alone group; rates of these events were lower among patients assigned to combined treatment (P = 0.006). Compared with those receiving medication only, patients with early-stage schizophrenia receiving medication and psychosocial intervention have a lower rate of treatment discontinuation, a lower risk of relapse and hospital admission.
More Frequent and/or Longer Visits may help foster an improved therapeutic alliance [3, 8, 10, 13, 142]. Frequent and personal meetings with detailed diagnostic explanations and positive outcome possibilities will help develop a productive relationship between patients and physicians. Misdrahi et al. [142] reported that most effective therapies involve an interactional component between patients and care providers/therapists: a weak therapeutic alliance is associated with poor adherence in patients with schizophrenia who were hospitalized. Specific psychoeducational programs to improve therapeutic alliance should be implemented to achieve better therapeutic adherence and outcome alliance.
The experts stressed the importance of improving the therapeutic alliance and involving family members alliance [10, 23]. Research supports the importance of a partnership between patient and clinician and shared decision-making when treating patients with antipsychotic medications in order to improve outcomes and increase patient satisfaction and willingness to adhere to treatment [143–145]. Within the alliance, the patient and physician can work together to identify the optimal medication.
Symptom/Side Effect Monitoring is important because lack of response and side effect emergence can lead to poor adherence and discontinuation of medication against medical advice [94, 146]. It is important for clinicians to monitor symptom response on an ongoing basis (e.g., using a daily checklist) and be alert for adherence problems in patients who do not achieve an adequate response. Tacchi and Scott [23] reported that giving detailed information on how to manage specific side effects should they occur can increase the likelihood of sustained adherence.
Multifaceted/Mixed-Modality Interventions
Because adherence problems tend to be related to multiple factors, researchers often recommend multifaceted interventions. Multimodal approaches, by definition, recognize that educational, behavioral, and affective strategies are likely to improve adherence [2, 3, 10, 17]. It appears that individuaI, group and family work can all be undertaken using multimodal approaches.
Kelly and Scott [147] describe a study of 418 patients with schizophrenia or other psychotic disorders. Patients were assigned to one of three intervention groups or to a control group receiving standard treatment alone. The first intervention group received a series of up to three home visits focused on assessing the patient’s current level of adherence, devising an appropriate behavioral approach for improving it, and encouraging a positive and supportive environment. The core of the intervention was the development of an individuaI “compliance plan”. The second intervention—a clinic visit—was aimed at improving patient-provider communication designed to teach the patient to become an active health care consumer. The third active intervention was both the clinic and the home visits. 273 patients (65 %) completed follow-up at 6 months and ratings at this point demonstrated that adherence was significantly improved among the experimental groups compared with the control group. Continuous levels of adherence with medication at baseline and at 6 months between active treatments and the control treatment were significantly different. The results show that brief interventions can significantly improve medication adherence in patients with chronic psychiatric disorders.
Hogarty et al. [148] undertook a 2-year follow-up of patients from high EE environments who had been randomly assigned to one of four treatment cells: (1) family psychoeducation; (2) social skills training; (3) both 1 and 2; or (4) supportive therapy plus medication. It was found that medication nonadherence was reduced significantly in the experimental conditions (rate = 21 %) compared with the control group (rate = 40 %).
Guimon et al. [149] studied a patient-and-family approach that involved group discussion of medication attitudes and behaviors. During group sessions patients discussed their conflicts about taking medications while a therapist and other group members provided suggestions about how to address these conflicts. Family members participated in similar groups. The intervention group showed superior medication adherence compared with standard care at 3- and 12-month follow-up.
Another study [150] included 39 such patients who were receiving case management services from a community mental health center. Patients were matched and randomly assigned to receive in a single session either (1) information regarding medication and its benefits, (2) guidelines for assuring adherence which encompassed all phases related to pill-taking including filling prescriptions, use of a pill container and self-reminders, or (3) the same guidelines as (2) but given in the presence of a family member who was enlisted in support. The results showed that adherence increased to about 94 % after the guidelines were given for both the individual and family procedure, whereas adherence remained unchanged at 73 % after the medication information procedure.
Dolder et al. [8] reviewed studies of 23 educational, behavioral, affective, or combination approaches to improve adherence in schizophrenia, 15 of which produced moderate improvements in adherence. The greatest improvement was seen with combination strategies. Reduced relapse, hospitalization, psychopathology and improved social function, gains in medication knowledge, and improved insight into need for treatment were also found. Longer interventions and a good therapeutic alliance were also important for successful outcomes.
The Danish OPUS trial [151], a large randomized clinical trial for first episode psychosis patients, investigated an integrated treatment, encompassing ACT, family involvement and social skills training and compared it to TAU. Adherence was only indirectly measured by participation in the treatment program, which showed significant differences after a follow-up of 1 year. Discontinuation of treatment for more than a month occurred in 8 % of patients in the intervention group, against 22 % in the control group. The percentage of patients stopping treatment in spite of necessity was 3 % versus 15 % in the control group, and the figure of patients making no outpatient visit was 4 % versus 15 %. At a 2-year follow-up, these differences were smaller and no longer significant for the groups stopping treatment or those discontinuing treatment for more than a month.
Masand and Narasimhan [152] recommended the following strategies to improve adherence in schizophrenia: optimizing antipsychotic therapy, minimizing adverse events, encouraging participation in psychoeducational programs, treating substance abuse, involving family members, and fostering good therapeutic relationships.
Valencia et al. [153] reported that a strategy that included psychosocial skills training, family therapy, and antipsychotic medication improved symptomatology, psychosocial, and global functioning; reduced relapse, rehospitalization, and drop-out rates; and increased adherence compared with treatment as usual after 1 year in outpatients with chronic schizophrenia.
Morken et al. [154] examined the effects on medication adherence of 2 years of integrated treatment in 50 patients with schizophrenia. Adherence to medication was examined in a randomized controlled trial of 2 years of integrated treatment versus standard treatment. The patients were clinically stable and had less than 2 years’ duration of illness. Integrated treatment consisted of ACT, family psychoeducation and involvement, social skills training, and individual cognitive behavioral therapy. Good adherence was defined as less than 1 month without medication. Outcomes were compared over 12-month and 24-month follow-up periods. No difference in adherence between the integrated treatment group and the standard treatment group (X² = 0.06, NS) was found.
Summary of Main Results and Evidences
In a 2008 Cochrane review, Haynes et al. [155] have revisited the results of RCTs of interventions to help patients follow prescriptions for medications for medical problems, including mental disorders (but not addictions). Authors concluded that improving short-term adherence is relatively successful with a variety of simple interventions. Current methods of improving adherence for chronic health problems are mostly complex and not very effective, so that the full benefits of treatment cannot be realized. High priority should be given to fundamental and applied research concerning innovations to assist patients to follow medication prescriptions for long-term medical disorders.
Early reviews [8, 25] covering interventions to improve adherence to antipsychotic medication lead to the following conclusions:
-
Psychoeducational interventions show little effect on adherence, unless they are accompanied by behavioral and cognitive interventions that aim directly at medication attitudes and adherence behavior.
-
Interventions specifically designed to improve adherence are more successful than programs intended to address a wider range of clinical problems, which suggests that a more intensive and focused approach is required to improve adherence rates.
-
Combined and integrated interventions such as cognitive behavioral techniques, family interventions and community-based interventions are associated with favorable outcomes.
-
More prolonged interventions or the use of booster sessions to reinforce and consolidate gains made during short term should be required.
In more recent reviews [3, 9, 10, 17, 23, 27], interventions that offered frequent sessions during a longer period of time, and especially those with a continuous focus on adherence, seem more likely to be successful, as well as pragmatic interventions that focus on attention and memory problems. The use of problem-solving interventions accompanied by technical aids is clearly promising. In recent years, attention was given to compensation for cognitive deficits in patients with schizophrenia, using environmental supports such as checklists, signs and electronic cueing devices. Some studies such as telephone intervention by nurses and especially CAT did show promising results, as well as a Pharmacy-Based Intervention. This suggests that all patients with chronic conditions and poor adherence could benefit from reducing access barriers with the use of Pharmacy-Based Interventions and concrete problem-solving interventions accompanied by technical aids. Possibly due to the prolonged duration of interventions, family interventions have shown positive results. Results by mixed-modality interventions suggest that a wider range of targets may be needed to promote adherence to medication, such as resuming rewarding life roles and regaining functional capacities. The positive effects of adapted forms of motivational interviewing found in earlier studies, such as CT or AT, have not been fully confirmed. Based on their comprehensive review of the literature, Julius et al. [9] recommended the following strategies for addressing adherence problems in patients with psychiatric illness: focus on strengthening the therapeutic alliance, devote time in treatment specifically to address medication adherence, assess patients’ motivation to take prescribed medication, and identify and assess potential barriers to treatment adherence.
Conclusions and Future Directions
As with pharmacologic interventions with antipsychotics, matching behavioral interventions to increase adherence with pharmacotherapy to the needs of specific patients is desirable. Different factors affecting adherence require different interventions by the clinician. For example, if a patient has an unfavorable attitude toward taking or staying on medication, it is important to: routinely assess adherence; emphasize the therapeutic alliance; use a patient-centered approach, starting with the patient’s point of view; stay symptom-focused rather than rely on the disease-model of interaction. Specific interventions include: CBT to emphasize working on problems as identified by the patient rather than the clinician; motivational interviewing to help facilitate motivation for positive change; family intervention to help educate and motivate family members in encouraging ongoing medication adherence. It is also important to appreciate the potential role of persistent symptoms as barriers to adherence and to address them not only with pharmacotherapy but also with effective behavioral interventions. Likewise, many patients have environmental barriers to adherence and interventions such as CAT may be helpful in addressing these barriers, together with good CM.
In a recent study Beck et al. [156] pointed out the importance of patients’ individual perspective and experience with treatment. The authors reported that interventions to enhance medication adherence may be more effective if they focus on treatment related attitudes rather than on global insight into illness. Clinicians may not only enhance the patients’ perceived necessity of antipsychotic treatment but also explore and address the patients’ concerns and distrust in pharmacotherapy in a more personalized way. Modification of attitudes toward pharmacotherapy in general may serve as an indirect way of enhancing medication adherence [156].
Findings of another study [157] suggest that professionals, carers, and patients do not have a shared understanding of which factors are important in patients’ medication adherence behavior. Professionals need to be aware of patients’ considerations concerning their antipsychotic medication, in particular positive aspects of medication use, in order to provide effective support and guidance. Therefore, reducing the gap between patients’ and professionals’ views on the importance of medication-related aspects seems crucial. The discrepancies between patients’ and professionals’ views on the relevance of clusters should be further explored in future research.
Rüsch et al. [158] reported that implicit attitudes toward psychiatric medication predict, independently of explicit attitudes and diagnosis, key outcome variables such as perceived need for treatment. Self-reported adherence to the currently prescribed medication, on the other hand, may be associated more with explicit than with implicit attitudes and systematically tends to overestimate adherence. Implicit measures can tap attitudes toward psychiatric medication that participants are either unwilling or unable to report explicitly. These results suggest that the measurement of implicit attitudes toward psychiatric medication is feasible and may provide important information beyond explicit, self-reported attitudes as assessed by commonly used questionnaires or interviews. Future research should investigate how implicit attitudes toward psychiatric medications may change in response to interventions designed to improve treatment adherence [158].
Nonadherence remains a challenging problem in schizophrenia. There is a great demand for more studies on this multifaceted issue, especially considering the methodological problems that researchers face when measuring the effectiveness of adherence interventions, given the heterogeneity of the population treated and the large number of possible influencing factors. This calls for large well-powered studies targeting specific interventions.
Because adherence problems in patients with schizophrenia are likely to be complex and multi-determined, the use of strategies targeted at specific types of adherence problems might be more appropriate, thereby developing an individually tailored approach to promote adherence. This appears to be a promising direction, which will require regular updates and input of ongoing initiatives to determine the relevance of targeted interventions for specific problems and for certain subgroups of patients.
More evidence and evaluation of the validity and effectiveness of specific interventions aimed at improving adherence is required to further raise the standard of care and clinical outcome of patients with schizophrenia.
References
Clayton CD, Veach J, Macfadden W et al (2010) Assessment of clinician awareness of non-adherence using a new structured rating scale. Psychiatr Pract 16(3):164–169
Tandon R, Nasrallah HA, Keshavan MS (2010) Schizophrenia, “just the facts” 5. Treatment and prevention. Past, present, and future. Schizophr Res 122(1–3):1–23
Goff DC, Hill M, Freudenreich O (2010) Strategies for improving treatment adherence in schizophrenia and schizoaffective disorder. J Clin Psychiatry 71(Suppl 2):20–26
Ascher-Svanum H, Faries DE, Zhu B et al (2006) Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry 67(3):453–460
Valenstein M, Copeland LA, Blow FC et al (2002) Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Med Care 40:630–639
Gilmer TP, Dolder CR, Lacro JP et al (2004) Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry 161:692–699
Weiden PJ, Olfson M (1995) Cost of relapse in schizophrenia. Schizophr Bull 21(3):419–429
Dolder CR, Lacro JP, Leckband S et al (2003) Interventions to improve antipsychotic medication adherence: review of recent literature. J Clin Psychopharmacol 23:389–399
Julius RJ, Novitsky MA Jr, Dubin WR (2009) Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract 15(1):34–44
Velligan DI, Weiden PJ, Sajatovic M et al (2009) The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. expert consensus panel on adherence problems in serious and persistent mental illness. J Clin Psychiatry 70 (Suppl 4):1–46
Hardeman SM, Harding RK, Narasimhan M (2010) Simplifying adherence in schizophrenia. Psychiatr Serv 61(4):405–408
McCann TV, Boardman G, Clark E et al (2008) Risk profiles for non-adherence to antipsychotic medications. J Psychiatr Ment Health Nurs 15(8):622–629
Scott J (1999) Cognitive and behavioural approaches to medication adherence. Adv Psych Treat 5:338–347
Saykin AJ, Gur RC, Gur RE et al (1991) Neuropsychological function in schizophrenia: selective impairment in memory and learning. Arch Gen Psychiatry 48:618–624
Liddle PF (1987) Schizophrenic syndromes, cognitive performance and neurological dysfunction. Psych Med 17:49–57
Heaton R, Paulsen JS, McAdams LA et al (1994) Neuropsychological deficits in schizophrenics: relationship to age, chronicity, and dementia. Arch Gen Psychiatry 51:469–476
Barkhof E, Meijer CJ, de Sonneville LM et al (2012) Interventions to improve adherence to antipsychotic medication in patients with schizophrenia—a review of the past decade. Eur Psychiatry 27(1):9–18
Weiden PJ, Shaw E, Mann J (1986) Causes of neuroleptic noncompliance. Psychiatr Ann 16:571–575
Rettenbacher MA, Hofer A, Eder U et al (2004) Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry 65(9):1211–1218
Lacro J (2006) Optimizing adherence to treatment in patients with schizophrenia. Behav Healthc 26(8):38–42
Kern RS, Glynn SM, Horan WP et al (2009) Psychosocial treatments to promote functional recovery in schizophrenia. Schizophr Bull 35(2):347–361
Patterson TL, Leeuwenkamp OR (2008) Adjunctive psychosocial therapies for the treatment of schizophrenia. Schizophr Res 100(1–3):108–119
Tacchi MJ, Scott J (2005) Improving adherence in schizophrenia and bipolar disorders. Wiley, Chichester
WHO (eds) (2003) Adherence to long-term therapies: evidence for action. WHO, Geneva
Zygmunt A, Olfson M, Boyer CA et al (2002) Interventions to improve medication adherence in schizophrenia. Am J Psychiatry 159(10):1653–1664
Kane JM (2011) Improving treatment adherence in patients with schizophrenia. J Clin Psychiatry 72(9):e28
Kane JM (2006) Review of treatments that can ameliorate nonadherence in patients with schizophrenia. J Clin Psychiatry 67(Suppl 5):9–14
Velligan DI, Diamond PM, Mintz J et al (2008) The use of individually tailored environmental supports to improve medication adherence and outcomes in schizophrenia. Schizophr Bull 34(3):483–493
Mari JJ, Streiner DL (1994) An overview of family interventions and relapse on schizophrenia: meta-analysis of research findings. Psychol Med 24(3):565–578
Pitschel-Walz G, Leucht S, Bäuml J et al (2001) The effect of family interventions on relapse and rehospitalization in schizophrenia—a meta-analysis. Schizophr Bull 27(1):73–92
Pilling S, Bebbington P, Kuipers E et al (2002) Psychological treatments in schizophrenia: I. meta-analysis of family intervention and cognitive behaviour therapy. Psychol Med 32(5):763–782
Girón M, Fernández-Yañez A, Mañá-Alvarenga S et al (2010) Efficacy and effectiveness of individual family intervention on social and clinical functioning and family burden in severe schizophrenia: a 2-year randomized controlled study. Psychol Med 40(1):73–84
Pharoah F, Mari J, Rathbone J et al (2006) Family intervention for schizophrenia. Cochrane Database Syst Rev 18(4):CD000088
Lincoln TM, Wilhelm K, Nestoriuc Y (2007) Effectiveness of psychoeducation for relapse, symptoms, knowledge, adherence and functioning in psychotic disorders: a meta-analysis. Schizophr Res 96(1–3):232–245
Seltzer A, Roncari I, Garfinkel P (1980) Effect of patient education on medication compliance. Can J Psychiatry 25(8):638–645
Brown CS, Wright RG, Christensen DB (1987) Association between type of medication instruction and patients’ knowledge, side effects, and compliance. Hosp Community Psychiatry 38(1):55–60
Goldman CR, Quinn FL (1988) Effects of a patient education program in the treatment of schizophrenia. Hosp Community Psychiatry 39(3):282–686
Streicker S, Amdur M, Dincin J (1986) Educating patients about psychiatric medications: failure to enhance compliance. Psychosoc Rehabil J 9:15–28
Maurel M, Drai D, Kaladjian A et al (2010) A randomized controlled study on the impact of pharmacoeducation on a French patient population with schizophrenic and schizoaffective disorders. Can J Psychiatry 55(5):329–337
Xia J, Merinder LB, Belgamwar MR (2011) Psychoeducation for schizophrenia. Cochrane Database Syst Rev 15(6):CD002831
Dixon L, McFarlane WR, Lefley H et al (2001) Evidence-based practices for services to families of people with psychiatric disabilities. Psychiatr Serv 52(7):903–910
Xiang M, Ran M, Li S (1994) A controlled evaluation of psychoeducational family intervention in a rural Chinese community. Br J Psychiatry 165(4):544–548
Ran MS, Xiang MZ, Chan CL et al (2003) Effectiveness of psychoeducational intervention for rural Chinese families experiencing schizophrenia–a randomised controlled trial. Soc Psychiatry Psychiatr Epidemiol 38(2):69–75
Chan SW, Yip B, Tso S et al (2009) Evaluation of a psychoeducation program for Chinese clients with schizophrenia and their family caregivers. Patient Educ Couns 75(1):67–76
Pitschel-Walz G, Bäuml J, Bender W et al (2006) Psychoeducation and compliance in the treatment of schizophrenia: results of the Munich psychosis information project study. J Clin Psychiatry 67(3):443–452
Bäuml J, Pitschel-Walz G, Volz A et al (2007) Psychoeducation in schizophrenia: 7-year follow-up concerning rehospitalization and days in hospital in the Munich psychosis information project study. J Clin Psychiatry 68(6):854–861
Kopelowicz A, Zarate R, Wallace CJ et al (2012) The ability of multifamily groups to improve treatment adherence in Mexican Americans with schizophrenia. Arch Gen Psychiatry 69(3):265–273
Leff J, Berkowitz R, Shavit N et al (1990) A trial of family therapy versus a relatives’ group for schizophrenia two-year follow-up. Br J Psychiatry 157:571–577
Zhang M, Wang M, Li J et al (1994) Randomised-control trial of family intervention for 78 first-episode male schizophrenic patients. An 18-month study in Suzhou Jiangsu. Br J Psychiatry 165(Suppl 24):96–102
Haas GL, Glick ID, Clarkin JF et al (1988) Inpatient family intervention: a randomized clinical trial. II. Results at hospital discharge. Arch Gen Psychiatry 45(3):217–224
Herz MI (1996) Psychosocial treatment. Psychiatr Ann 26:531–535
Pharoah F, Mari J, Rathbone J et al (2010) Family intervention for schizophrenia. Cochrane Database Syst Rev 8(12):CD000088
Turkington D, Kingdon D, Weiden PJ (2006) Cognitive behavior therapy for schizophrenia. Am J Psychiatry 163(3):365–373
Tai S, Turkington D (2009) The evolution of cognitive behavior therapy for schizophrenia: current practice and recent developments. Schizophr Bull 35(5):865–873
NICE (2009) Schizophrenia: core interventions in the treatment and management of schizophrenia in primary and secondary care (update). National Institute of Clinical Excellence, London
Dixon LB, Dickerson F, Bellack AS et al (2010) The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr Bull 36(1):48–70
Durham RC, Chambers JA, Power KG et al (2005) Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland. Health Technol Assess 9(42):1–174
Garety PA, Fowler DG, Freeman D et al (2008) Cognitive–behavioural therapy and family intervention for relapse prevention and symptom reduction in psychosis: randomised controlled trial. Br J Psychiatry 192(6):412–423
Eckman TA, Liberman RP, Phipps CC et al (1990) Teaching medication management skills to schizophrenic patients. J Clin Psychopharmacol 10(1):33–38
Boczkowski JA, Zeichner A, DeSanto NJ (1985) Neuroleptic compliance among chronic schizophrenic outpatients: an intervention outcome report. Consult Clin Psychol 53(5):666–671
Cramer JA, Rosenheck R (1999) Enhancing medication compliance for people with serious mental illness. J Nerv Ment Dis 187(1):53–55
Razali MS, Hasanach CL, Khan A et al (2000) Psychosocial interventions for schizophrenia. J Ment Health 9:283–289
Jones C, Hacker D, Cormac I et al (2012) Cognitive behaviour therapy versus other psychosocial treatments for schizophrenia. Cochrane Database Syst Rev 18(4):CD008712
Lecompte D, Pelc I (1996) A cognitive-behavioural program to improve compliance with medication in patients with schizophrenia. Int J Ment Health 25:51–56
Rollnick S, Miller WR (1995) What is motivational interviewing? Behavioural and cognitive psychotherapy. Cognit Psychother 23:325–334
Hayward P, Chan N, Kemp R et al (1995) Medication selfmanagement: a preliminary report on an intervention to improve medication compliance. J Ment Health 4:511–517
Kemp R, David A (1996) Psychological predictors of insight and compliance in psychotic patients. Br J Psychiatry 169(4):444–450
Kemp R, Hayward P, Applewhaite G et al (1996) Compliance therapy in psychotic patients: randomised controlled trial. BMJ 312(10):345–349
Kemp R, Hayward P, David A (1997) Compliance therapy manual. The Maudsley, London
Kemp R, Kirov G, Everitt B et al (1998) Randomised controlled trial of compliance therapy. 18-month follow-up. Br J Psychiatry 172:413–419
Gray R, Robson D, Bressington D (2002) Medication management for people with a diagnosis of schizophrenia. Nurs Times 98(47):38–40
O’Donnell C, Donohoe G, Sharkey L et al (2003) Compliance therapy: a randomised controlled trial in schizophrenia. BMJ 327(7419):834
Byerly MJ, Fisher R, Carmody T et al (2005) A trial of compliance therapy in outpatients with schizophrenia or schizoaffective disorder. J Clin Psychiatry 66(8):997–1001
McIntosh AM, Conlon L, Lawrie SM (2006) Compliance therapy for schizophrenia. Cochrane Database Syst Rev 19(3):CD003442
Gray R, Leese M, Bindman J et al (2006) Adherence therapy for people with schizophrenia. European multicentre randomised controlled trial. Br J Psychiatry 189:508–514
Maneesakorn S, Robson D, Gournay K et al (2007) An RCT of adherence therapy for people with schizophrenia in Chiang Mai Thailand. J Clin Nurs 16(7):1302–1312
Anderson KH, Ford S, Robson D et al (2010) An exploratory, randomized controlled trial of adherence therapy for people with schizophrenia. Int J Ment Health Nurs 19(5):340–349
Uzenoff SR, Perkins DO, Hamer RM et al (2008) A preliminary trial of adherence-coping-education (ACE) therapy for early psychosis. J Nerv Ment Dis 196(7):572–575
Staring AB, Van der Gaag M, Koopmans GT et al (2010) Treatment adherence therapy in people with psychotic disorders: randomised controlled trial. Br J Psychiatry 197(6):448–455
Becker MH, Maiman LA (1975) Sociobehavioral determinants of compliance with healthand medical care recommendations. Med Care 13:10–24
Becker MH, Maiman LA, Kirscht JP et al (1977) The health belief model and prediction of dietary compliance: a field experiment. J Health Soc Behav 18(4):348–366
Becker MH (1985) Patient adherence to prescribed therapies. Med Care 23(5):539–555
Rosenstock IM (1974) Historical origins of the health belief model. Health Educ Monogr 2:409–419
Marder SR, May PR (1986) Benefits and limitations of neuroleptics—and other forms of treatment—in schizophrenia. Am J Psychother 40(3):357–369
Albus M (1995) The problem of drug compliance in schizophrenic patients. Psychiatr Prax 22(6):221–222
Razali MS, Yahya H (1995) Compliance with treatment in schizophrenia: a drug intervention program in a developing country. Acta Psychiatr Scand 91(5):331–335
Johnson DA, Freeman H (1973) Drug defaulting by patients on long-acting phenothiazines. Psychol Med 3(1):115–119
Johnson DA (1977) Treatment of chronic schizophrenia. Drugs 14(4):291–299
Soskis DA (1978) Schizophrenic and medical inpatients as informed drug consumers. Arch Gen Psychiatry 35(5):645–647
Marder SR, Mebane A, Chien CP et al (1983) A comparison of patients who refuse and consent to neuroleptic treatment. Am J Psychiatry 140(4):470–472
Marder SR, Swann E, Winslade WJ et al (1984) A study of medication refusal by involuntary psychiatric patients. Hosp Community Psychiatry 35(7):724–726
Horne R, Weinman J (1998) Predicting treatment adherence: an overview of theoretical models. In: Myers LB, Midence K (eds) Adherence to treatment in medical conditions. Harwood Academic Press, Amsterdam, pp 25–50
Weinstein ND (1988) The precaution adoption process. Health Psychol 7:355–386
Perkins DO (2002) Predictors of noncompliance in patients with schizophrenia. J Clin Psychiatry 63(12):1121–1128
Lacro JP, Dunn LB, Dolder CR et al (2002) Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry 63(10):892–909
Garavan J, Browne S, Gervin M et al (1998) Compliance with neuroleptic medication in outpatients with schizophrenia; relationship to subjective response to neuroleptics; attitudes to medication and insight. Compr Psychiatry 39(4):215–219
Velligan DI, Weiden PJ (2006) Interventions to improve adherence to antipsychotic medication. Psychiatric Times 23(9):1–2
Fenton WS, Blyler CR, Heinssen RK (1997) Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophr Bull 23(4):637–651
Frank AF, Gunderson JG (1990) The role of the therapeutic alliance in the treatment of schizophrenia. Relationship to course and outcome. Arch Gen Psychiatry 47(3):228–236
Weiss KA, Smith TE, Hull JW et al (2002) Predictors of risk of nonadherence in outpatients with schizophrenia and other psychotic disorders. Schizophr Bull 28(2):341–349
Fleischhacker WW, Meise U, Günther V et al (1994) Compliance with antipsychotic drug treatment: influence of side effects. Acta Psychiatr Scand Suppl 382:11–15
Budd RJ, Hughes IC, Smith JA (1996) Health beliefs and compliance with antipsychotic medication. Br J Clin Psychol 35(3):393–397
Champion VL (1984) Instrument development for health belief model constructs. ANS Adv Nurs Sci 6(3):73–85
Pan PC, Tantam D (1989) Clinical characteristics, health beliefs and compliance with maintenance treatment: a comparison between regular and irregular attenders at a depot clinic. Acta Psychiatr Scand 79(6):564–570
Adams J, Scott J (2000) Predicting medication adherence in severe mental disorders. Acta Psychiatr Scand 101(2):119–124
Robinson DG, Woerner MG, Alvir JM et al (2002) Predictors of medication discontinuation by patients with first-episode schizophrenia and schizoaffective disorder. Schizophr Res 57:209–219
Grunebaum MF, Weiden PJ, Olfson M (2001) Medication supervision and adherence of persons with psychotic disorders in residential treatment settings: a pilot study. J Clin Psychiatry 62(5):394–399
Oehl M, Hummer M, Fleischhacker WW (2000) Compliance with antipsychotic treatment. Acta Psychiatr Scand Suppl 102(407):83–86
Babiker IE (1986) Noncompliance in schizophrenia. Psychiatr Dev 4(4):329–337
Bebbington PE (1995) The content and context of compliance. Int Clin Psychopharmacol 9(Suppl 5):41–50
Kinderman P, Setzu E, Lobban F et al (2006) Illness beliefs in schizophrenia. Soc Sci Med 63(7):1900–1911
Velligan DI, Mueller J, Wang M et al (2006) Use of environmental supports among patients with schizophrenia. Psychiatr Serv 57(2):219–224
Velligan DI, Prihoda TJ, Ritch JL et al (2002) A randomized single-blind pilot study of compensatory strategies in schizophrenia outpatients. Schizophr Bull 28(2):283–292
Velligan DI, Bow-Thomas CC (2000) Two case studies of cognitive adaptation training for outpatients with schizophrenia. Psychiatr Serv 51(1):25–29
Velligan DI, Bow-Thomas CC, Huntzinger C et al (2000) Randomized controlled trial of the use of compensatory strategies to enhance adaptive functioning in outpatients with schizophrenia. Am J Psychiatry 157(8):1317–1323
Velligan DI, Mueller J, Wang M et al (2006) Use of environmental supports among patients with schizophrenia. Psychiatr Serv 57(2):219–224
Velligan DI, Diamond P, Mueller J et al (2009) The short-term impact of generic versus individualized environmental supports on functional outcomes and target behaviors in schizophrenia. Psychiatry Res 168(2):94–101
Valenstein M, Kavanagh J, Lee T et al (2011) Using a pharmacy-based intervention to improve antipsychotic adherence among patients with serious mental illness. Schizophr Bull 37(4):727–736
Pijnenborg GH, Withaar FK, Brouwer WH et al (2010) The efficacy of SMS text messages to compensate for the effects of cognitive impairments in schizophrenia. Br J Clin Psychol 49(Pt 2):259–274
Salzer MS, Tunner T, Charney NJ (2004) A low-cost, telephone intervention to enhance schizophrenia treatment: a demonstration study. Schizophr Res 66(1):75–76
Beebe LH, Smith K, Crye C et al (2008) Telenursing intervention increases psychiatric medication adherence in schizophrenia outpatients. J Am Psychiatr Nurses Assoc 14(3):217–224
Spaniel F, Vohlídka P, Hrdlicka J et al (2008) ITAREPS: information technology aided relapse prevention programme in schizophrenia. Schizophr Res 98(1–3):312–317
Kurtz MM, Baker E, Pearlson GD et al (2007) A virtual reality apartment as a measure of medication management skills in patients with schizophrenia: a pilot study. Schizophr Bull 33(5):1162–1170
Janssen B, Ludwig S, Eustermann H et al (2010) Improving outpatient treatment in schizophrenia: effects of computerized guideline implementation—results of a multicenter-study within the German research network on schizophrenia. Eur Arch Psychiatry Clin Neurosci 260(1):51–57
Marshall M, Lockwood A (2000) Assertive community treatment for people with severe mental disorders. Cochrane Database Syst Rev 2:CD001089
Marshall M, Gray A, Lockwood A et al (2000) Case management for people with severe mental disorders. Cochrane Database Syst Rev 2:CD000050
Bond GR, McGrew JH, Fekete DM (1995) Assertive outreach for frequent users of psychiatric hospitals: a meta-analysis. J Ment Health Adm 22(1):4–16
Coldwell CM, Bender WS (2007) The effectiveness of assertive community treatment for homeless populations with severe mental illness: a meta-analysis. Am J Psychiatry 164(3):393–399
Nelson G, Aubry T, Lafrance A (2007) A review of the literature on the effectiveness of housing and support, assertive community treatment, and intensive case management interventions for persons with mental illness who have been homeless. Am J Orthopsychiatry 77(3):350–361
Burns T, Catty J, Dash M et al (2007) Use of intensive case management to reduce time in hospital in people with severe mental illness: systematic review and meta-regression. BMJ:335(7615):336
Stein LI, Test MA (1980) Alternative to mental hospital treatment. I. Conceptual model, treatment program, and clinical evaluation. Arch Gen Psychiatry 37(4):392–397
Ford R, Beadsmore A, Ryan P et al (1995) Providing the safety net: case management for people with serious mental illness. J Ment Health 1:91–97
Bond GR, Miller LD, Krumwied RD et al (1988) Assertive case management in three CMHCs: a controlled study. Hosp Community Psychiatry 39(4):411–418
Solomon P, Draine J (1995) The efficacy of a consumer case management team: 2-year outcomes of a randomized trial. J Ment Health Adm 22(2):135–146
Dixon L, Weiden P, Torres M et al (1997) Assertive community treatment and medication compliance in the homeless mentally ill. Am J Psychiatry 154(9):1302–1304
McEvoy JP, Scheifler PL, Frances A et al (1999) The expert consensus guideline series: treatment of schizophrenia. J Clin Psychiatry 60(Suppl 11):3–80
Gray R, Wykes T, Gournay K (2003) The effect of medication management training on community mental health nurse’s clinical skills. Int J Nurs Stud 40(2):163–169
Gray R, Wykes T, Edmonds M et al (2004) Effect of a medication management training package for nurses on clinical outcomes for patients with schizophrenia: cluster randomised controlled trial. Br J Psychiatry 185:157–162
Hudson TJ, Owen RR, Thrush CR et al (2008) Guideline implementation and patient-tailoring strategies to improve medication adherence for schizophrenia. J Clin Psychiatry 69(1):74–80
Linden M, Pyrkosch L, Hundemer HP (2008) Frequency and effects of psychosocial interventions additional to olanzapine treatment in routine care of schizophrenic patients. Soc Psychiatry Psychiatr Epidemiol 43(5):373–379
Guo X, Zhai J, Liu Z et al (2010) Effect of antipsychotic medication alone vs combined with psychosocial intervention on outcomes of early-stage schizophrenia: a randomized, 1-year study. Arch Gen Psychiatry 67(9):895–904
Misdrahi D, Petit M, Blanc O et al (2012) The influence of therapeutic alliance and insight on medication adherence in schizophrenia. Nord J Psychiatry 66(1):49–54
Deegan PE, Drake RE (2006) Shared decision making and medication management in the recovery process. Psychiatr Serv 57(11):1636–1639
Drake RE, Deegan PE, Rapp C (2010) The promise of shared decision making in mental health. Psychiatr Rehabil J 34(1):7–13
Mistler LA, Drake RE (2008) Shared decision making in antipsychotic management. J Psychiatr Pract 14(6):333–344
Perkins DO, Gu H, Weiden PJ et al (2008) Predictors of treatment discontinuation and medication nonadherence in patients recovering from a first episode of schizophrenia, schizophreniform disorder, or schizoaffective disorder: a randomized, double-blind, flexible-dose, multicenter study. J Clin Psychiatry 69(1):106–113
Kelly GR, Scott JE, Mamon J (1990) Medication compliance and health education among outpatients with chronic mental disorders. Med Care 28(12):1181–1197
Hogarty GE, Anderson CM, Reiss DJ et al (1991) Family psychoeducation, social skills training, and maintenance chemotherapy in the aftercare treatment of schizophrenia. II. Two-year effects of a controlled study on relapse and adjustment. Environmental-Personal Indicators in the Course of Schizophrenia (EPICS) research group. Arch Gen Psychiatry 48(4):340–347
Guimon L, Eguiluz I, Bulbena A (1993) Group pharmacotherapy in schizophrenics: attitudinal and clinical changes. Eur J Psychiatry 7(3):147–154
Azrin NH, Teichner G (1998) Evaluation of an instructional program for improving medication compliance for chronically mentally ill outpatients. Behav Res Ther 36(9):849–861
Petersen L, Jeppesen P, Thorup A et al (2005) A randomised multicentre trial of integrated versus standard treatment for patients with a first episode of psychotic illness. BMJ 331(7517):602
Masand PS, Narasimhan M (2006) Improving adherence to antipsychotic pharmacotherapy. Curr Clin Pharmacol 1(1):47–56
Valencia M, Rascon ML, Juarez F et al (2007) A psychosocial skills training approach in Mexican out-patients with schizophrenia. Psychol Med 37(10):1393–1402
Morken G, Grawe RW, Widen JH (2007) Effects of integrated treatment on antipsychotic medication adherence in a randomized trial in recent-onset schizophrenia. J Clin Psychiatry 68(4):566–571
Haynes RB, Ackloo E, Sahota N et al (2008) Interventions for enhancing medication adherence. Cochrane Database Syst Rev 16(2):CD000011
Beck EM, Cavelti M, Kvrgic S et al (2011) Are we addressing the ‘right stuff’ to enhance adherence in schizophrenia? Understanding the role of insight and attitudes towards medication. Schizophr Res 132(1):42-49
Kikkert MJ, Schene AH, Koeter MW et al (2006) Medication adherence in schizophrenia: exploring patients’, carers’ and professionals’ views. Schizophr Bull 32(4):786–794
Rüsch N, Todd AR, Bodenhausen GV et al (2009) Implicit versus explicit attitudes toward psychiatric medication: Implications for insight and treatment adherence. Schizophr Res 112(1–3):119–122
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2014 Springer-Verlag Italia
About this chapter
Cite this chapter
Vita, A., Barlati, S., Sacchetti, E. (2014). Non-Pharmacological Strategies to Enhance Adherence and Continuity of Care in Schizophrenia. In: Adherence to Antipsychotics in Schizophrenia. Springer, Milano. https://doi.org/10.1007/978-88-470-2679-7_3
Download citation
DOI: https://doi.org/10.1007/978-88-470-2679-7_3
Published:
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-2678-0
Online ISBN: 978-88-470-2679-7
eBook Packages: MedicineMedicine (R0)