Abstract
The optimization of any contrast medium injection protocol should be aimed at achieving the best arterial and/or parenchymal enhancement according to the clinical indication. Arterial and parenchymal enhancements influence the accuracy of the MDCT examination and are generally affected by different kinetics. Arterial enhancement is determined mainly by the iodine dose delivered per unit of time and parenchymal enhancement by the total iodine dose. However, both are significantly related to patient-specific factors, such as body size, cardiac performance, gender, and age. Moreover, the goal of any MDCT examination is to achieve the best image quality using the lowest volume of contrast medium (CM), because most adverse CM reactions are a consequence of the total iodine dose administered to the patient.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
The optimization of any contrast medium injection protocol should be aimed at achieving the best arterial and/or parenchymal enhancement according to the clinical indication. Arterial and parenchymal enhancements influence the accuracy of the MDCT examination and are generally affected by different kinetics. Arterial enhancement is determined mainly by the iodine dose delivered per unit of time and parenchymal enhancement by the total iodine dose. However, both are significantly related to patient-specific factors, such as body size, cardiac performance, gender, and age. Moreover, the goal of any MDCT examination is to achieve the best image quality using the lowest volume of contrast medium (CM), because most adverse CM reactions are a consequence of the total iodine dose administered to the patient.
1 Arterial Enhancement
1.1 Body Imaging
Two important variables determine the time-course of arterial enhancement: the iodine delivery rate (IDR) and the injection duration (ID). Arterial enhancement is also influenced by patient-specific variables such as cardiovascular status (i.e., cardiac output) and individual body-size indexes (i.e., distribution volume). IDR is expressed in gI/mL, is operatorcontrolled, and determined by modifying the injection flow rate (FR) and the iodine concentration of a given CM. The required value can be obtained with virtually any concentration of CM according to the formula: {eq1} where [I] is the CM concentration (expressed in mgI/mL). If the acquisition of an arterial phase for body imaging is required, the IDR should not be < 1.2 gI/s; optimally, the value should be around 1.6 gI/s, since this provides higher conspicuity of hypervascular lesions. As an example, in order to achieve an IDR of 1.6 gI/s, CM must be injected at a concentration of 320 mgI/mL, at a FR of 5.0 mL/s, and a CM concentration of 400 mgI/mL with a flow rate of 4.0 mL/s.
Patient-specific factors contribute to the magnitude of vascular and parenchymal enhancement; the most important are patient body size and cardiac output. The latter is the most relevant factor affecting the timing of contrast enhancement and cardiovascular circulation. A reduction of cardiac output results in delayed CM arrival, higher peak arterial enhancement, and prolonged parenchymal enhancement. The slower the CM circulates, the slower its clearance and the higher its concentration. The magnitude of the aortic peak and of parenchymal enhancement increases substantially in patients with reduced cardiac output, while the magnitude of hepatic enhancement peak increases only slightly. A 60% reduction in cardiac output increases the magnitude of aortic peak enhancement by about 30% but that of hepatic enhancement by only 2% . The factors with the greatest effects on cardiac output are sex and age. It has been demonstrated that the CM bolus arrives slightly earlier in female than in male patients because of a smaller (around 5–10% ) distribution volume in the former. The demonstration of a lower cardiac output proportional to age suggests that a 10% reduction in iodine dose and injection rate in elderly patients will yield an enhancement of the same magnitude.
IDR should also be modified according to the patient’s body size. As previous studies demonstrated, IDR should be determined according to the patient’s lean body weight (LBW) as, among other body size indexes (eg. total body weight: TBW; blood volume: BV), it provides the best hepatic arterial enhancement with reduced patient-to-patient variability.
Flow rates for CM with different iodine concentrations and TBWs are suggested in Table 3.1.
1.2 CT Angiography
The delay between the intravenous injection of CM and its appearance within the arterial compartment is defined as the CM transit time (tCMT). This parameter, as discussed above, is markedly variable in different patients and is linked to the efficiency of the cardiovascular system. The bolus-tracking test and automatic monitoring techniques are used to establish the tCMT, which can then be set to determine the scan delay; this is defined as the time required for the CM to arrive in the vascular bed and to produce an enhancement of around 100 HU.
For angiographic studies, once the injection FR is chosen, the contrast volume should be set on the injector screen. If the acquisition of an arterial phase is required, the CM volume depends on the injection duration (ID) according to the formula: {eq2}
For example, if the FR is 4.0 mL/s (for CM at 400 mgI/mL) and the ID is 13 s, the total volume needed is 52 mL.
Injection duration influences vascular enhancement only in longer acquisitions (> 10 s): the longer the ID, the greater the arterial enhancement. This is due to the cumulative effects of bolus recirculation, which contributes to a 10–20% increase in peak arterial enhancement and in the magnitude of intravascular enhancement. For abdominal acquisition times (> 5 s for liver imaging) this parameter is not as important. Injection duration should be longer than the scan time and scan acquisition should be delayed until the maximum intravascular attenuation is achieved. As a ballpark rule for abdominal angiographic acquisitions, the scan delay should be 8 s after a 100-HU threshold in the aorta is reached. Injection duration is thus calculated as follows: for a 5-s acquisition, the injection duration should be 5 s + 8 s = 13 s. The scan delay s modified according to the particular clinical needs and especially according to the organ to be studied. This is discussed elsewhere in this volume.
1.2.1 Fast CT Angiography (< 10 s)
In the case of a short scan time, as achieved by the new-generation MDCT scanners, and high FR protocols, the transit time cannot be used in a mathematical fashion. Instead, adding 8 s to the tCMT is advisable. This practical rule is applied on the basis of the technical times required for repositioning the patient tray (it is nonetheless advisable to avoid setting bolus tracking too far from the beginning of the scan). In addition, visualization of the images obtained with bolus-tracking techniques are not produced in real-time but rather as reconstruction times, which vary according to the MDCT manufacturer (around 3 s). There are also delay times associated with the change of collimation. This empirical rule enables the exact scan time to be determined, but it is also advisable to lengthen the injection duration by around 8 s, bearing in mind the delay, which needs to be adapted to the iodine concentration of the specific CM (refer to the flow-volume tables in the product information). This widens the window available for performing the scan and enables the desired iodine administration rate to be achieved. By way of example, if we wish to perform a scan of the abdominal aorta and the scan time is around 8 s, we need to position the region of interest (ROI) so as to monitor the bolus at the level of the abdominal aorta and then set a diagnostic delay of 8 s from the moment when 100 HU is reached. If the CM concentration is 350 mgI, then around 69 mL of CM should be injected at an injection FR of 4.3 mL/s for an injection duration of 16 s. With a high-concentration CM (400 mgI), the volume becomes 61 mL and the injection FR 3.8 mL/s.
1.2.2 Slow CT Angiography (> 10 s)
We have already analyzed the strategies to be implemented in order to correctly evaluate the arterial vessels when the scan times are very short. For long scan times, other factors need to be taken into consideration. The mean transit time (between the vein of the arm and the abdominal aorta) is calculated with automatic techniques, but there is evidence in the literature that even the mean transit time between the abdominal aorta and the popliteal arteries is highly variable (between 4 and 24 s). This value corresponds to a bolus FR of 29–177 mm/s. The table speed should be set at the lower limit of this range to avoid the phenomena of the bolus being overtaken by the scan. A table speed of around 30 mm/s translates into a scan time of around 40 s when we want to cover large volumes, such as in studies that include the abdominal aorta and the arterial vessels of the lower limbs.
Modern 64-slice systems allow for table speeds of around 80 mm/s in the basic configuration. The speed can be lowered by reducing the pitch; if this is not enough, the gantry rotation speed can be increased. A widely used strategy therefore consists of setting the table speed to around 30 mm/s, or simply setting the scan parameters to obtain a scan that lasts for around 40 s.
For studies with these scan durations, the CM administration strategy should involve an injection duration of around 35 s, considering that the time required for the enhancement of the abdominal aorta is excluded from the automatic techniques of bolus tracking and that the minimum scan delay is around 3 s. Accordingly, the use of a constant injection FR (5.7 mL/s for iodinated CM with a concentration of around 350 mgI/mL) requires the administration of a much higher quantity of iodine (in our case 35 × 5.7 = 199.5 mL of CM at a concentration of 350 mgI/mL). Correct enhancement of the entire vascular tree of the aorta and the lower limbs can be obtained without the need to administer < 120 mL of CM at a concentration of 350 mgI/mL, by using lower volumes of high-concentration CM with a strategy of dual-phase injection at different FRs. This strategy requires the use of an initial bolus of CM at a high FR (around 40 mL at 5 mL/s) and a maintenance bolus (around 80 mL) at a variable FR: for normal-weight patients (60–90 kg) the FR should be set at 3 mL/s, whereas for heavier patients the quantity of CM should be increased and the FR adapted to obtain a fixed injection duration of around 35 s.
2 Parenchymal Enhancement
Parenchymal enhancement is governed by the relationship between the total iodine dose (mgI) and the total volume of distribution (intravascular and interstitial spaces).
Historical studies have demonstrated that it is necessary to deliver an adequate amount of iodine, in the range of 500–600 mgI per kg TBW, to achieve optimal parenchymal enhancement of the liver (around 50–60 HU). To calculate the required volume of CM, with a concentration of 300 mgI/mL, it is necessary to deliver 2 mL/kg TBW. This value (2 mL/kg) should be adapted to the iodine concentration, thus resulting in 1.7 mL/kg for 350 mgI/mL and 1.5 mL/kg for 400 mgI/mL.
However, it has been demonstrated that TBW is not the optimal body-size index for adjusting iodine dose because blood volume and liver weight are not directly proportional to TBW. For example, obese patients may have abundant body fat, which has a small vascular and interstitial space and thus contributes little to dispersing or diluting the CM in the blood. In these patients, adjusting the iodine dose so that it is proportional to TBW may lead to an overestimation of the amount of CM needed. Some experiences reported that calculating the CM dose on the basis of LBW leads to increased patient-to-patient uniformity of hepatic parenchymal and vascular enhancement. LBW can be measured using an electronic body-fat monitor, which estimates the body-fat percentage (BFP). Thus, LBW can be calculated according to the formula: {eq3}
Once the patient’s LBW is evaluated, the amount of iodine required to achieve adequate enhancement of the liver parenchyma is calculated as: {eq4} where I is the amount of iodine (g) and ΔHU represents the desired maximum hepatic enhancement (MHE), which should be around 50–60 HU. The amount of iodine needed, divided by the CM concentration (in g), results in the exact CM volume in mL.
3 Timing
Determination of the optimal temporal window for body scanning is mandatory to correctly identify and characterize focal or diffuse parenchymal disease.
The CM transit time (tCMT), as referred to above, is the time between the start of intravenous administration of a CM bolus and its arrival in the vascular region of interest. Thus, especially in patients with cardiovascular disease, scan delay should be based on the patient’s tCMT. The tCMT can be determined using a test bolus injection or by automated bolus- triggering techniques.
The use of a fixed delay time is no longer recommended, since it cannot guarantee optimal separation between dynamic phases due to inherent variability among individuals, such as patient size and cardiovascular status. Instead, a more rational use of MDCT can be accomplished using either a test bolus or bolus-tracking software.
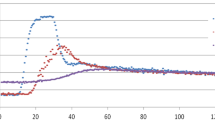
The test-bolus technique is based on the injection, at the same FR as calculated for the diagnostic injection, of a small CM bolus (15–20 mL) while acquiring multiple low-dose sequential scans at the starting level of the diagnostic scan. The time-enhancement curve obtained is a reliable method to determine the tCMT from the intravenous injection site to the arterial territory of interest. The tCMT equals the time to peak enhancement interval and is measured in a ROI placed within a reference vessel. Furthermore, time-attenuation curves obtained from one or more ROIs can be used for individual bolus-shaping techniques using set mathematical models. A test bolus is particularly useful in determining the tCMT if unusual CM injection sites must be used (e.g., lower extremities) or for very short (> 3 s) scan times when a bolus-triggering software is not suitable.
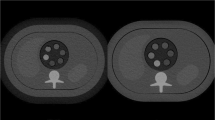
Many MDCT scanners have automatic bolus-triggering software built into their system. This allows the real-time detection of a circular ROI placed within the target vessel on a non-enhanced image. After 5–10 s from the start of the CM injection, a series of low-dose sequential scans are acquired every 1–3 s whereas the attenuation within the ROI is monitored or inspected visually. The tCMT equals the time at which a predefined enhancement threshold is reached (e.g., 100 HU), plus a diagnostic delay determined according to the specific organ to be studied. The diagnostic delay is the time between reaching a predefined enhancement threshold and the start of the MDCT acquisition; it depends on the scanner model and on the longitudinal distance between the monitoring series and the starting position of the actual MDCT series. Bolus triggering is a very robust and practical technique for routine use and has the advantage of not requiring an additional test-bolus injection.
4 Saline Flush
During fast-acquisition scans, a substantial volume of the injected CM remains in the dead space of the right heart, peripheral veins, and injection tubing. Flushing the venous system with saline immediately after CM administration pushes the CM column into the systemic circulation. Thus, a saline flush is helpful in optimizing CM volumes as it allows a reduction of the iodine dose without significant influence on the level of contrast enhancement. The reduction of CM volume is reportedly between 12 and 50 mL, with a positive effect on the risk of CM-induced nephropathy.
The most convenient technique for routine saline flush after CM injection uses the newly available programmable double-piston power injectors (one syringe for CM, one for saline).
In the field of body MDCT, there is little evidence that a saline flush influences vessel and parenchymal enhancement. A positive effect of saline flushing on aortic, portal, and hepatic enhancement has been reported, along with a significant increase in the aortic peak but no evidence of improved hepatic enhancement. However, a saline flush does not improve the magnitude of liver parenchyma enhancement in clinical imaging, whereas in time-density analyses it significantly improves the time to peak of liver, portal vein, and aortic enhancement. Furthermore, the CM left in the dead space contributes to vascular enhancement by a slow and late flowing. The clearing of this CM volume is reflected in a more rapid decline of intravascular attenuation after the peak such that scanning during this period may result in insufficient contrast enhancement.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag Italia
About this chapter
Cite this chapter
Laghi, A. (2012). Contrast-Medium Administration. In: Laghi, A. (eds) MDCT Protocols. Springer, Milano. https://doi.org/10.1007/978-88-470-2403-8_3
Download citation
DOI: https://doi.org/10.1007/978-88-470-2403-8_3
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-2402-1
Online ISBN: 978-88-470-2403-8
eBook Packages: MedicineMedicine (R0)