Abstract
-
The clinical features of hypothermia vary among patients and core temperatures are often unreliable; therefore, prompt recognition of each stage of hypothermia is crucial in its management.
-
Gentle handling of the patient is paramount since manipulation can precipitate arrhythmias in the irritable myocardium.
-
With failure to rewarm a clinician should consider underlying sepsis or non-infectious causes of impaired thermogenesis.
-
With regard to frostbite rewarming is an essential component of therapy but should be delayed until definitive care is imminent since refreezing following rewarming results in worsening tissue damage.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Key Points-
The clinical features of hypothermia vary among patients and core temperatures are often unreliable; therefore, prompt recognition of each stage of hypothermia is crucial in its management.
-
Gentle handling of the patient is paramount since manipulation can precipitate arrhythmias in the irritable myocardium.
-
With failure to rewarm a clinician should consider underlying sepsis or non-infectious causes of impaired thermogenesis.
-
With regard to frostbite rewarming is an essential component of therapy but should be delayed until definitive care is imminent since refreezing following rewarming results in worsening tissue damage.
Introduction
Accidental hypothermia is the involuntary drop in core temperature below 35 °C [1]. Death from accidental hypothermia occurs throughout the world, and although more commonly seen in cold climates, hypothermia may develop without exposure to extreme environmental conditions [1]. In spite of current advances in rescue, prehospital and supportive care, the in-hospital mortality of patients with moderate or severe hypothermia is approximately 40 % [1].
Classification
The stage of hypothermia impacts directly on both recognition and management. The most widely used definitions in the literature are as follows [2]:
-
Mild hypothermia: Core temperature 32–35 °C
-
Moderate hypothermia: Core temperature 28–32 °C
-
Severe hypothermia: Core temperature <28 °C, although some experts regard a core temperature <24 °C as profound hypothermia [3].
Because the clinical features of hypothermia vary among patients and core temperatures are often unreliable, the appreciation of each stage is more important than the absolute temperature when managing hypothermia. Other published temperature ranges are similar.
Prehospital personnel may also refer to the clinical staging defined by the International Commission for Mountain Emergency Medicine also known as the Swiss System (Tables 21.1).
Pathophysiology
The body maintains homeostasis of normal core temperature by a balance between heat production and heat loss. Heat is generated by cellular metabolism and lost via skin and lungs via four main mechanisms [5]:
-
Evaporation: vaporisation of water through insensible losses and sweat
-
Radiation: emission of infrared electromagnetic energy
-
Conduction: direct transfer of heat to an adjacent cooler object
-
Convection: direct transfer of heat to convective currents of air and water
Convective heat loss to cold air and conductive heat loss to water are the most prevalent mechanisms of accidental hypothermia [5].
The preoptic nucleus of the anterior hypothalamus is responsible for thermoregulation at a set point core temperature of 37 ± 0.5 °C. In response to cold stress, the hypothalamus endeavours to stimulate heat production through shivering and increased thyroid, catecholamine and adrenal activity. Sympathetically mediated vasoconstriction decreases heat loss by reducing blood flow to the peripheral tissues. Peripheral blood vessels (where cooling is greatest) also vasoconstrict in direct response to cold [5].
Cooling also decreases neural activity and tissue metabolism. Initially, however, shivering in response to cooling skin produces heat and increased metabolism, cardiac output and ventilation. Once core temperature reaches 32 °C cardiac output, ventilation and shivering becomes ineffective and finally ceases as core temperature plummets [2].
The human body has therefore limited physiological capacity to maintain a narrow temperature homeostasis. Thus, behavioural responses like clothing and shelter are critical to avert hypothermia.
Clinical Features
Patients will present with:
-
Mild hypothermia: tachypnoea, tachycardia, hyperventilation, ataxia, impaired level of consciousness, shivering and cold diuresis
-
Moderate hypothermia: bradycardia, reduced cardiac output, arrhythmias, hypoventilation, CNS depression, hyporeflexia and loss of shivering
-
Severe hypothermia: pulmonary oedema, oliguria, areflexia, ventricular arrhythmias and asystole [5]
Neurological features vary widely but the level of consciousness should correlate with core temperature. An alternative diagnosis should be considered if a significant discrepancy exists.
Risk factors associated with increased mortality of accidental hypothermia include: [6]
-
Ethanol use
-
Older age
-
Psychiatric illness
-
Homelessness
-
Malnutrition
Investigations
Investigations should be guided by thorough history and clinical examination. The goal of laboratory evaluation should be to identify potential co-morbidities and complications including lactic acidosis, bleeding tendency and infection. Previously healthy patients with mild accidental hypothermia may not require investigation. The following evaluation is suggested in cases of moderate to severe hypothermia [2]:
-
Bedside glucose determination
-
ECG (Fig. 21.1)
-
Urine dipstick
-
Serum electrolytes and urea, creatinine
-
Serum haemoglobin, white cell count and platelets
-
Serum lactate
-
Creatine phosphokinase
-
Arterial blood gas (uncorrected for temperature) in ventilated patients
-
Chest radiograph
Treatment
Both general supportive measures and specific rewarming techniques remain the cornerstone in the management of hypothermia. Gentle handling of the patient is paramount since manipulation can precipitate arrhythmias in the irritable myocardium. Detection of pulses may be challenging and chest compressions may potentiate ventricular fibrillation. Inappropriate chest compressions should be avoided by examining the patient carefully for any respiratory activity, signs of life or cardiac contractility on ultrasound, suggesting a perfusing rhythm.
Management of cardiac arrest according to standard ACLS protocols is advised but electrical defibrillation is rarely successful until core temperature is greater than 30 °C. Oxygen and intravenous fluids should be warmed, and patients should have continuous monitoring of core temperature (low reading), cardiac rhythm and oxygen saturation.
Rewarming Approaches
-
1.
Passive rewarming: remove cold damp clothes and wrap with blankets in a warm room.
-
2.
Active external rewarming: apply heat to skin.
-
Heating blanket or radiant heat
-
Hot water bottles or heating pads to trunk (caution can burn skin)
-
Risk of core temperature after-drop: vasodilation with active external rewarming which causes:
-
Cold peripheral blood to return to heart
-
Decreased systemic vascular resistance and hypotension
-
Wide pulse pressure
-
-
Risk of rewarming acidosis: lactate from periphery returns to core circulation which may cause transient shock
-
-
3.
Active core rewarming:
-
Humidified air at 40 °C
-
Warm intravenous fluids at 40–45 °C
-
Warm fluid lavage of stomach, bladder, colon or pleural space
-
Cardiopulmonary bypass (CPB), haemodialysis (HD) or extracorporeal membrane oxygenation (ECMO)
-
Peritoneal dialysis with normal saline at 40–45 °C at 6–10 L/h
-
Mediastinal lavage through open thoracotomy [7]
-
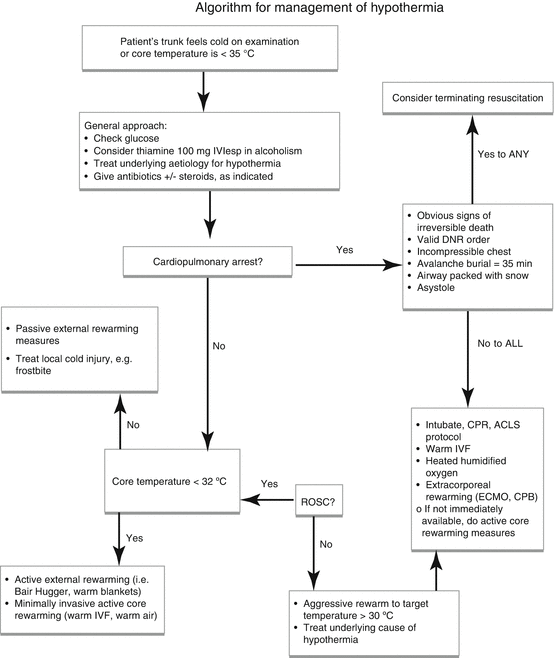
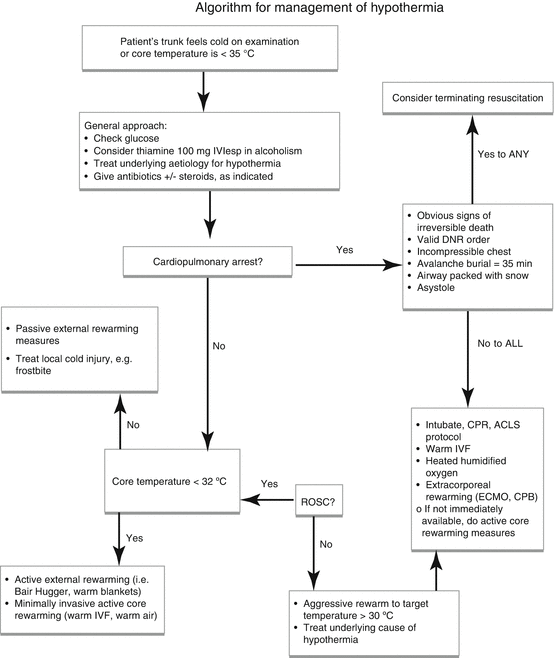
Choosing a Rewarming Approach
General approach:
-
Check glucose.
-
Give thiamine 100 mg IVI especially in known or suspected alcoholics.
-
Treat underlying aetiology of hypothermia.
-
Give antibiotics +/− steroids as indicated only.
If patient in cardiopulmonary arrest:
-
CPR, ACLS protocol, intubate
-
Warm intravenous fluid
-
Heated humidified oxygen
-
Extracorporeal rewarming technique (e.g. CPB, ECMO)
-
If not available then, active core rewarming
-
-
Rewarm to target of >30 °C
If not in cardiopulmonary arrest and temperature <32 °C:
-
Active external rewarming (e.g. Bair Hugger or other similar external warming device)
-
Minimally invasive active core rewarming (e.g. warm air, IV fluids)
If not in cardiopulmonary arrest and temperature >32 °C
-
Passive external rewarming measures
Rewarming Pearls and Pitfalls
No prospective, randomised controlled studies comparing the various rewarming modalities have been done in humans. Therefore, firm guidelines for therapy cannot be given.
Fluid
-
Although warmed intravenous fluids are essential, they are not an effective means of treating hypothermia because of the small temperature differential or gradient and large difference in mass between body and infused fluid. Their use becomes more apparent when large volumes of fluid in a hypovolaemic patient are used for resuscitation [7].
-
One litre of crystalloid at room temperature can be heated in a microwave (1,000 W) to 40 °C for 2.5 min.
-
Glucose containing fluids and blood should not be microwaved.
Body Cavity Rewarming Techniques
-
Pleural irrigation results in cardiac rewarming and may be the technique of choice if an arrhythmia is present.
-
Direct irrigation of liver through peritoneal lavage may restore its ability to clear toxins and lactate.
-
Stomach, colon and bladder are poor sites for body cavity lavage because of their small surface area for heat exchange.
Temperature Measurement
-
A rectal probe thermometer is practical in conscious patients.
-
Rectal and bladder probes should not be used in critical patients during rewarming because a significant lag exists with core temperature.
-
Oesophageal temperature is the most accurate in rewarming.
-
An oesophageal probe placed in the lower third of the oesophagus provides near approximation of cardiac temperature.
-
The effectiveness of rewarming depends on the technique used and the clinical indication based on severity of the presenting problem (Table 21.2)
Failure to Rewarm
-
First ensure that appropriate aggressive rewarming techniques are in progress with all equipment functioning optimally.
-
Failure to rewarm may be due to the possibility of core temperature after-drop. However, its incidence, magnitude and clinical significance are unclear.
-
Consider impaired thermogenesis from underlying sepsis.
-
Consider non-infectious causes of impaired thermogenesis:
-
Toxins
-
Hypothyroidism
-
Adrenal insufficiency
-
Disposition
Provided they are asymptomatic and can return to a warm environment, patients with mild accidental hypothermia can be discharged. Most other patients require admission for treatment of hypothermia and investigation of the underlying cause.
-
The Osborn wave (J wave) is a positive deflection at the J point (negative in aVR and V1) and is usually most prominent in the precordial leads.
-
Usually seen with hypothermia <30 °C but they are not pathognomonic.
-
Hypothermia-associated ECG changes are significantly more frequent in patients with fortunate prognosis.
-
Other ECG changes may include:
-
Muscle tremor artefact
-
T wave inversion
-
PR, QRS and QT prolongation [9]
-
Dysrhythmias – sinus bradycardia, atrial fibrillation, AV block and nodal rhythms
-
Cold Injury
Introduction
The concept of localised cold injuries extends as far into history as the 1700s when the Swedish Army invaded Russia. The Swedes were defeated, with cold injury being a major contributory factor to their loss. It has also been described during Napoleon’s Franco-Russian War, nineteenth-century military conflicts and World Wars I and II.
However, cold-related injury is not limited to military personnel [10]. The homeless together with people who spend prolonged periods in freezing temperatures or engage in outdoor winter sports, are also at risk.
Pathophysiology
Cold exposure triggers a thermoregulatory response where the core body temperature is maintained at the expense of the extremities and skin. Freezing of the extremities is best described in four phases.
Phase 1: Cooling and Freezing
The initial response to cold temperature is vasospasm. This is followed by the ‘hunting response’ which is an alternation in vasodilation and vasoconstriction, occurring every 5–10 min. During persistently cold temperature exposure, the body attempts to maintain core body temperature by shutting off blood flow to the coldest limbs. Extracellular ice crystals form in the plasma and interstitium at a temperature of −2 °C causing stasis. The crystals produce an osmotic gradient resulting in intracellular dehydration. Intracellular crystals form and there is cellular membrane destruction.
Phase 2: Rewarming
Exposure to warmth reverses the freezing process. The crystals melt and the vulnerable endothelium of the small capillaries becomes highly permeable. Fluid extravasates with resultant oedema and blister formation.
Phase 3: Tissue Injury
This phase is similar to that of burns. An arachidonic acid cascade forms and the metabolites, prostaglandins and thromboxane are liberated. These inflammatory mediators initiate an inflammatory cascade with resultant vasoconstriction and platelet aggregation.
Phase 4: Resolution
The result of frostbite may culminate into gangrene, complete tissue recovery or later sequelae.
Clinical Features
Chilblain or pernio occurs on bare body surfaces which are chronically or repeatedly exposed to cold, but non-freezing temperatures. Acute exposure to cold may trigger symptoms of burning paraesthesiae, erythema, localised swelling and nodules on these areas. The lesions have the potential to progress to ulcerations and form bullae.
Trench foot progresses over hours to days following immersion in cold, stagnant water. Involvement of peripheral nerves causes paraesthesiae. The foot appears pale and cyanotic and is painless or extremely painful with or without a pulse. Tissue loss or permanent disability may result.
Frostnip presents as paraesthesiae that is localised and resolves with rewarming.
Frostbite most commonly occurs, but is not limited to the nose, ears, face, hands and feet. It may also present as a freezing keratitis of the cornea in skiers without eye protection.
The clinical features of frostbite is classified into first to fourth degree with first and second degrees being superficial and third and fourth degrees being deep (Table 21.3).
Investigations
The diagnosis is usually clinical. The following investigations may be used to determine the prognosis, extent of injury and associated co-morbidities.
-
Plain radiographs: To assess for fractures or growth plate destruction in children
-
Technetium scintigraphy: May be used to assess long-term tissue viability but is not superior to clinical examination
-
MRI: May demonstrate the boundaries of ischaemic and non-ischaemic tissue
Treatment
Chilblain
Therapy is mostly supportive. Affected areas should initially be rewarmed, then bandaged and elevated.
Trench Foot
Management is supportive, as with chilblain. In addition, pentoxifylline 400 mg three times a day may be considered. Wounds are to be inspected for onset of sepsis. Preventative measures should be encouraged. This includes ensuring the use of dry socks, correct boot size and keeping warm.
Frostbite
Prehospital Management
The initial aim is to treat the presenting problems and prevent further injury. All wet, constricting clothing and boots must be removed and changed to dry garments. Patients should be removed from the freezing environment as soon as possible. The affected limbs ought to be splinted, padded and elevated. Rewarming is an essential component of therapy but should be delayed until definitive care is imminent. Refreezing following rewarming results in worsening tissue damage. The use of stoves and open fires for rewarming is strongly discouraged [12].
Emergency Department Management
Hypothermia can be life threatening and should be excluded or treated, if present. Further management should focus on rewarming, analgesia, wound care and preventing complications.
-
Rewarming: Initiate only when the core body temperature is greater than or equal to 35 °C. The injured extremity should be soaked in circulating water for 10–30 min. The water temperature ought to be maintained at 40–42 °C. Successful rewarming is suggested when the tissue becomes red and pliable [13].
-
Analgesia: Opioids are an effective choice for analgesia. Morphine, 0.1 mg/kg, is recommended.
-
Anti-inflammatories: Ibuprofen 12 mg/kg/day dampens the arachidonic acid cascade.
-
Wound care:
-
Tetanus may be a complication. Tetanus prophylaxis is advisable.
-
Maintain sterility when examining or treating wounds.
-
Clear blisters contain thromboxane and prostaglandins. They should be aspirated and debrided.
-
Haemorrhagic blisters suggest injury to the microvasculature. They may be aspirated but not debrided.
-
Aloe vera cream is recommended as a topical application, 6 hourly. It aids in the inhibition of the arachidonic acid cascade.
-
Patients are predisposed to infection by various pathogens. Staphylococcus aureus, S. epidermidis, beta-haemolytic streptococci and anaerobes may be culprits. Prophylactic penicillin G, 500 000 units IVI 6 hourly or clindamycin 600 mg IVI, 6 hourly for 48–72 h is recommended.
-
An early surgical consult is needed, but intervention may be indicated at a later stage when there is adequate demarcation of dead tissue [14]. Early surgical intervention is indicated in the presence of a constricting eschar or very rarely a fasciotomy in the presence of compartment syndrome.
-
Various other treatment modalities are currently being researched and may prove beneficial in the treatment of cold extremity injuries in the future.
Hyperbaric oxygen therapy (HBOT) may aid in repairing vasculature and healing tissue. Anticoagulants, vasodilators, thrombolytics and sympathetic-blocking drugs are also being researched.
References
Vassal T, Benoit-Gonin B, Carrat F, et al. Severe accidental hypothermia treated in ICU: prognosis and outcome. Chest. 2001;120:1998.
Mechem CC, Zafren K, Danzl D, et al. Accidental hypothermia in adults. Available from http://www.uptodate/contents/accidental-hypothermia-in-adults. Accessed 24th Mar 2015.
Danzl D. Accidental hypothermia. In: Auerbach PS, editor. Wilderness medicine. 6th ed. Philadelphia: Elsevier; 2012.
Durrer B, Brugger H, Syme D. International Commission for Mountain Emergency Medicine. The medical onsite treatment of hypothermia: ICAR-MEDCOM recommendations. High Alt Med Biol. 2003;4:99–103. Available from http://www.ikar-cisa.org/ikar-cisa/documents/2013/ikar20131013001086.pdf. Accessed 4th Apr 2015.
Jolly BT, Ghezzi KT. Accidental hypothermia. Emerg Med Clin North Am. 1992;10:311–27.
Ranhoff AH. Accidental hypothermia in the elderly. Int J Circumpolar Health. 2000;59:255–9.
Petrone P, et al. Management of accidental hypothermia. Curr Probl Surg. 2014;51:417–31.
Brown DJA, et al. Accidental hypothermia. N Engl J Med. 2012;367:1930–8.
Mulcahy AR, Watts MR. Accidental hypothermia: an evidence based approach. Emerg Med Pract. 2009;11:1. EBMedicine.net.
Murphy JV, Bonwell PE, Roberts AH, et al. Frostbite: pathogenesis and treatment. J Trauma. 2000;48:171.
Ikaheimo TM, et al. Frostbite and other localised injuries. In: Tintinalli’s Emergency medicine: a comprehensive study guide 7e.
Mechem CC, Zafren K, Danzl D, et al. Frostbite. Available from http://www.uptodate/contents/frostbite. Accessed 24 Mar 2015.
Golant A, et al. Cold exposure injuries to the extremities. J Am Acad Orthop Surg. 2008;16:704.
Bessen A, Brian Ngo. Hypothermia. In: Tintinalli’s emergency medicine: a comprehensive study guide 7e.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer India
About this chapter
Cite this chapter
Pillay, S. (2016). Accidental Hypothermia and Cold Injury. In: David, S. (eds) Clinical Pathways in Emergency Medicine. Springer, New Delhi. https://doi.org/10.1007/978-81-322-2710-6_21
Download citation
DOI: https://doi.org/10.1007/978-81-322-2710-6_21
Published:
Publisher Name: Springer, New Delhi
Print ISBN: 978-81-322-2708-3
Online ISBN: 978-81-322-2710-6
eBook Packages: MedicineMedicine (R0)