Abstract
Endometrial cancer staging has changed over time to a surgicopathologic staging system. The goal of staging is to have a clinical practice guideline which reduces inappropriate variation in clinical practice and also to have uniformity in reporting results of treatment worldwide. In addition staging intends to prognosticate disease. Presently endometrial carcinoma is surgically staged according to the joint 2010 International Federation of Gynecology and Obstetrics (FIGO)/TNM classification system [1, 2]. The revised staging eliminated cervical glandular involvement and ascitic fluid cytology from staging, grouped together both IA and IB of the previous staging as IA, and substratified Stage IIIC. This staging system for endometrial cancers has been found to be highly prognostic in the case of endometrioid tumors [3]. But size of tumor and LVSI (lymphovascular space invasion), which are also considered as prognostic factors, are not included in the current staging.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Endometrial cancer staging has changed over time to a surgicopathologic staging system. The goal of staging is to have a clinical practice guideline which reduces inappropriate variation in clinical practice and also to have uniformity in reporting results of treatment worldwide. In addition staging intends to prognosticate disease. Presently endometrial carcinoma is surgically staged according to the joint 2010 International Federation of Gynecology and Obstetrics (FIGO)/TNM classification system [1, 2] (see Table 6.3, Chap. 6). The revised staging eliminated the cervical glandular involvement and ascitic fluid cytology from the staging, grouped together both IA and IB of the previous staging as IA, and substratified Stage IIIC. This staging system for endometrial cancers has been found to be highly prognostic in the case of endometrioid tumors [3]. But size of the tumor and LVSI (lymphovascular space invasion), which are also considered as prognostic factors, are not included in the current staging.
Important notes on staging are given below [4].
Rules Related to Staging
-
1.
Corpus cancer is now surgically staged; therefore procedures previously used for determination of stages are no longer applicable (e.g., the findings of fractional curettage to differentiate between Stage I and Stage II).
-
2.
There may be a small number of women with corpus cancer who will be treated primarily with radiation therapy. In these cases, the clinical staging adopted by FIGO in 1971 would still apply, but designation of that staging system would be noted.
-
3.
Ideally, width of the myometrium should be measured along with the depth of tumor invasion.
-
4.
There should be histologic verification of grading and extent of the tumor.
Notes About the Grading
Histopathology – degree of differentiation. Cases of carcinoma of the corpus should be grouped with regard to the degree of differentiation of the adenocarcinoma as follows:
-
G1: <5 % of a nonsquamous or nonmorular solid growth pattern
-
G2: 6–50 % of a nonsquamous or nonmorular solid growth pattern
-
G3: >50 % of a nonsquamous or nonmorular solid growth pattern
Notable nuclear atypia, inappropriate for the architectural grade, raises the grade of a Grade l or Grade 2 tumor by 1:
-
In serous and clear cell adenocarcinomas, nuclear grading takes precedence.
-
Adenocarcinomas with squamous differentiation are graded according to the nuclear grade of the glandular component.
Preoperative assessment by endometrial pathology is required to differentiate between tumors at low and high risk of lymph node metastasis, and imaging can be useful in determining depth and cervical involvement and suspicion of involved nodes (Level of Evidence C).
The presence of bullous edema in the bladder is not sufficient evidence to classify a tumor as T4.
AJCC Stage Grouping [2] and FIGO Stages
Extent of the tumor, spread to lymph nodes, and distant cancer spread are combined to assign the stage of disease. This is called stage grouping. Omentectomy is also done as a part of staging procedures in Type 2 endometrial cancer.
Stage 0
Tis, N0, M0: This stage is also known as carcinoma in situ. Cancer cells are only found in the surface layer of cells of the endometrium, without growing into the layers of cells below. The cancer has not spread to nearby lymph nodes or distant sites. This is a precancerous lesion. This stage is not included in the FIGO staging system.
Stage I (Fig. 14.1)
T1, N0, M0: The cancer is confined to the body of the uterus. It may be involving the glands of the cervix but is not involving the supporting connective tissues of the cervix. The cancer has not spread to lymph nodes or distant sites.
-
Stage IA (T1a, N0, M0): In this earliest form of Stage I, the cancer is in the endometrium and/or infiltrating less than halfway through the myometrium. It has not spread to lymph nodes or distant sites.
-
Stage IB (T1b, N0, M0): The tumor involves more than half of the myometrium. The cancer has not spread beyond the body of the uterus.
Stage II (Fig. 14.2)
T2, N0, M0: The cancer has spread from the body of the uterus and infiltrates cervical stroma.
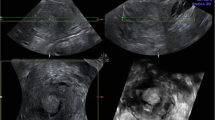
Stage III (Figs. 14.3, 14.4, 14.5, and 14.6)
T3, N0, M0: Either the cancer has spread outside of the uterus or into nearby tissues in the pelvic area.
-
Stage IIIA (T3a, N0, M0): The cancer has spread to the uterine serosa and/or to the fallopian tubes or ovaries (the adnexa).
-
Stage IIIB (T3b, N0, M0): The cancer has spread to the vagina and/or to the parametrium.
-
Stage IIIC1 (T1 to T3, N1, M0): The endometrial cancer has spread to pelvic lymph nodes but not to lymph nodes around the aorta or distant sites.
-
Stage IIIC2 (T1 to T3, N2, M0): The endometrial cancer has involved para-aortic lymph nodes but not spread to distant sites.
Stage IV (Fig. 14.7)
The cancer has spread to the urinary bladder or rectum, or to inguinal lymph nodes, and/or to distant organs, such as the bones, omentum, or lungs.
-
Stage IVA (T4, any N, M0): Mucosa of the bladder or rectum is involved by the endometrial cancer.
-
Stage IVB (any T, any N, M1): The cancer has spread to distant lymph nodes, the upper abdomen, and the omentum or to organs away from the uterus, such as the bones or lungs.
Tumor Extent (T)
-
T0: No signs of a tumor in the uterus.
-
Tis: Preinvasive cancer (also called carcinoma in situ). Cancer cells are only found in the surface layer of cells of the endometrium, without growing into the layers of cells below.
-
T1: The cancer is only growing in the body of the uterus. It may also be growing into the glands of the cervix, but is not growing into the supporting connective tissue of the cervix.
-
T1a: The cancer is in the endometrium (inner lining of the uterus) and may have grown from the endometrium less than halfway through the underlying muscle layer of the uterus (the myometrium).
-
T1b: The cancer has grown from the endometrium into the myometrium, growing more than halfway through the myometrium. The cancer has not spread beyond the body of the uterus.
-
-
T2: The cancer has spread from the body of the uterus and is growing into the supporting connective tissue of the cervix (called the cervical stroma). The cancer has not spread outside of the uterus.
-
T3: The cancer has spread outside of the uterus, but has not spread to the inner lining of the rectum or urinary bladder.
-
T3a: The cancer has spread to the outer surface of the uterus (called the serosa) and/or to the fallopian tubes or ovaries (the adnexa).
-
T3b: The cancer has spread to the vagina or to the tissues around the uterus (the parametrium).
-
-
T4: The cancer has spread to the inner lining of the rectum or urinary bladder (called the mucosa).
Lymph Node Spread (N)
-
NX: Spread to nearby lymph nodes cannot be assessed.
-
N0: No spread to nearby lymph nodes.
-
N1: Cancer has spread to lymph nodes in the pelvis.
-
N2: Cancer has spread to lymph nodes along the aorta (periaortic lymph nodes).
Distant Spread (M)
-
M0: The cancer has not spread to distant lymph nodes, organs, or tissues.
-
M1: The cancer has spread to distant lymph nodes, the upper abdomen, the omentum, or other organs (such as the lungs or liver).
Conclusion
Staging is inevitable in treatment decisions and standardizing treatment. It also helps in prognostication of disease. The two systems used for staging endometrial cancer, the FIGO (International Federation of Gynecology and Obstetrics) system and the American Joint Committee on Cancer TNM staging system, are basically the same. They both classify this cancer on the basis of three factors: the extent of the tumor (T), spread to lymph nodes (N), and presence of metastasis (M). The difference between the AJCC system and the FIGO system is that the FIGO system does not include Stage 0. Both the staging systems require surgicopathologic confirmation. However, comprehensive surgical staging in low-grade endometrial cancer still remains controversial.
Key Points
-
1.
Endometrial cancer staging has changed over time to a surgicopathologic classification.
-
2.
The goal of staging is to have a good practice guideline or a clinical practice guideline.
-
3.
Staging also intends to prognosticate the disease.
-
4.
Ideally, width of the myometrium should be measured along with the depth of tumor invasion.
-
5.
There should be histologic verification of grading and extent of the tumor.
-
6.
The difference between the AJCC system and the FIGO system is that the FIGO system does not include Stage 0.
References
Creasman W. Revised FIGO staging carcinoma of the endometrium. Int J Gynaecol Obstet. 2009;105:109.
American Joint Committee on Cancer. Corpus uteri. In: AJCC staging manual. 7th ed. New York: Springer; 2010. p. 403.
Lewin SN, Herzog TJ, Barrena Medel NI, Deutsch I, Burke WM, Sun X, Wright JD. Comparative performance of the 2009 international federation of gynecology and obstetrics’ staging system for uterine corpus cancer. Obstet Gynecol. 2010;116(5):1141–9.
Benedet JL, Hacker NF, Ngan HYS. Staging classifications and clinical practice guidelines of gynaecologic cancers. Int J Gynecol Obstet. 2000;70:207–312.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer India
About this chapter
Cite this chapter
Raj, S.T.J., Chitrathara, K. (2015). Endometrial Cancer Staging. In: Rajaram, S., K, C., Maheshwari, A. (eds) Uterine Cancer. Springer, New Delhi. https://doi.org/10.1007/978-81-322-1892-0_14
Download citation
DOI: https://doi.org/10.1007/978-81-322-1892-0_14
Publisher Name: Springer, New Delhi
Print ISBN: 978-81-322-1891-3
Online ISBN: 978-81-322-1892-0
eBook Packages: MedicineMedicine (R0)