Abstract
Aortic dilatation is constantly observed in unrepaired or repaired congenital heart diseases (CHD). Aortic dilatation might cause aortic annular enlargement that will predispose to severe aortic regurgitation (AR). In such conditions, concomitant aortic valve plasty or replacement with aortic root replacement will be required. Bentall operation is root replacement with an aortic tube graft and a mechanical valve. Coronary ostia are reimplanted to the aortic graft. Remodeling method (Yacoub) and reimplantation method (David) had been developed in order to preserve the aortic valve with the same concept as the Bentall operation. These procedures are well known as valve-sparing operations. On the other hand, in Ross procedure a pulmonary autograft is used to replace the aortic root and aortic valve. RV outflow tract and pulmonary artery are reconstructed usually with homograft or other valved conduits. Superior hemodynamics, freedom from anticoagulation, and longevity of pulmonary autografts have been substantiated in many reports.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
In various congenital heart diseases (CHD), such as Marfan syndrome, Turner syndrome, bicuspid aortic valve (BAV) syndrome, single ventricle, and repaired or unrepaired tetralogy of Fallot (TOF), aortic dilatation is constantly observed.
Marfan syndrome is frequently associated with aortic dilatation or aortic dissection. Aortic dilatation might cause aortic annular enlargement that will in turn predispose to severe aortic regurgitation (AR). In such conditions, concomitant aortic valve plasty or replacement together with replacement of the aortic root or ascending aorta will be required. Sometimes arch replacement will also be necessary in the cases associated with arch dilation or dissection.
The Bentall operation [1] was introduced first as a root replacement for annuloaortic ectasia (AAE) with a composite graft containing a mechanical valve.
The remodeling method [2] (Yacoub) and the reimplantation method [3] (David) had been developed with the same concept as the Bentall operation in order to preserve the aortic valve. Both procedures are well known as valve-sparing operations.
In contrast, in the Ross procedure [4], a pulmonary autograft is used to replace the aortic root and aortic valve. Enucleated RV outflow tract and the pulmonary artery are reconstructed usually with a homograft or other valved conduits. Superior hemodynamics, freedom from anticoagulation, and longevity of pulmonary autograft have been substantiated in many reports.
2 Aortic Root Replacement with Composite Graft – Bentall Operation
In 1968, Bentall and de Bono described the first successful complete replacement of the ascending aorta with a composite Teflon tube graft and a ball valve prosthesis (Starr valve) in a male associated with ascending aortic dilatation and aortic annular enlargement, which caused free AR. The arch vessels were not involved in the aortic dilatation.
The Bentall operation consists of aortic root and aortic valve replacement with an aortic valve conduit. The coronary arteries are reimplanted into the tube graft directly or interposing a small graft. In order to replace the ascending aorta as far distally as possible, cardiopulmonary bypass is usually established by retrograde arterial perfusion through the femoral artery. After cross-clamp of the ascending aorta, the aneurysmal ascending aorta is removed (Fig. 12.1a). The aortic valve is excised (Fig. 12.1b), and a composite tube graft prosthesis of appropriate size, including a prosthetic valve, is sutured to the aortic annulus. Usually a mechanical valve is used in this graft because of its longevity (Fig. 12.1c).
Two holes are made in the composite graft at the positions of the coronary ostia. Originally, coronary ostia were approximated to the graft and directly sutured to the holes of the graft. This method might cause significant tension to suture lines and bleeding, so that many modifications have been developed.
Nowadays, coronary ostia are detached as large buttons of the aortic wall and dissected free along their courses to ensure their mobility. The scalloped coronary buttons are sutured to the holes of the aortic graft directly (Carrel patch method) or interposing a small graft (Piehler method) (Fig. 12.1d).
The Bentall operation is usually indicated in AAE with a diseased aortic valve.
Aortic aneurysms in the patients with Marfan syndrome are also repaired with this technique. Marfan syndrome is frequently associated with aortic dissection. Depending on the location and extent of the dissection, additional reconstruction or replacement of other parts of the aorta is necessary.
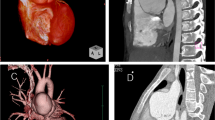
A large aorta is frequently observed in TOF, especially in the case of tetralogy of Fallot (TOF) with pulmonary atresia. Niwa [5] reported that 15 % of repaired adults with TOF had a dilated aortic root (Figs. 12.2a, 12.2b, and 12.2c).
Fortunately, only a small number of these patients seem to develop an aortic dissection [5]. For this reason, aortic replacement in TOF is indicated at a later stage compared to patients who developed an aortic aneurysm in other anomalies. However, when the diameter of the aortic root excesses 55 mm [6, 7], aortic replacement could be considered. If significant aortic regurgitation occurs due to annular dilatation, aortic valve replacement (AVR) combined with ascending aortic replacement or Bentall operation would be indicated.
2.1 Valve-Sparing Operation
Among patients with aortic dilatation, severe AR may occur only due to annular dilatation. When the aortic valve is not affected, it may be feasible to recover competence of the aortic valve by reducing the diameter of the aortic annulus and the suspension of cusps. Based on this concept, valve-sparing root replacement had been developed by Yacoub in 1979 (remodeling method [2]) and by David in 1992 (reimplantation method [3]).
2.1.1 Remodeling Method
Cardiopulmonary bypass is established in the same manner as in the Bentall operation. The aneurysmal ascending aorta is removed from the distal portion to the sinus of Valsalva. The coronary ostia are detached from the aortic wall as large buttons. The sinus of Valsalva is resected, whereas the aortic valve is preserved. A proper size tube graft, usually determined by the diameter of the sino-tubular junction at the time of competent approximation of the cusps, is prepared to fit the shape of the Valsalva sinuses and is sutured to the wall of the sinuses. As in the Bentall operation, two holes are made in the tube graft at the corresponding positions of the coronary ostia (Fig. 12.3). The coronary buttons are sutured to the tube graft in the same way as in the Bentall operation. Since the aortic annulus is untouched in the remodeling method, aortic root dilation may develop.
Completion of remodeling method. Aneurysmal ascending aorta is removed to Valsalva sinuses. Coronary ostia are removed as large buttons. A proper size tube graft is trimmed to fit the figure of Valsalva sinuses. The ascending aorta is replaced with this graft. Coronary ostia are reimplanted to the tube graft
2.1.2 Reimplantation Method
Preservation of the aortic valve and enucleation of coronary buttons are performed in the same manner as in the remodeling method. A tube graft of 4-5 mm larger than the diameter of the aortic annulus is selected. The first row sutures are placed inside to outside just below the aortic cusps to fix the tube graft. Commissural walls are pulled into a tube graft (Fig. 12.4a), and then first row sutures are put in the edge of the graft and tied down. Each commissural wall is suspended to the inside of the tube graft arranging competence of the aortic valve. The free edge of the Valsalva sinuses is sutured continuously to the inside of the tube graft (second row sutures) (Fig. 12.4b). Two holes are made in the tube graft at the positions of the corresponding coronary ostia. The coronary buttons are sutured to the tube graft in the same fashion as in other forms of root replacement (Fig. 12.4c). This method is particularly indicated in young female with Marfan syndrome (Fig. 12.5). Although often a straight tube graft is used for root replacement, also a new type of grafts with a bulged midportion for improvement of valve movement is utilized.
2.1.3 Differences of Various Valve-Sparing Operations
As in the remodeling method, aortic annulus and aorto-ventricular junction are left untouched, the risk of root dilatation remains in the long term. However, in the remodeling method the function of the Valsalva sinuses is preserved. Leyh et al. [8] reported that aortic root elasticity and aortic valve motion are superior in the remodeling method compared to the reimplantation method. Richardt et al. [9] reported in Marfan syndrome excellent long-term results of the reimplantation method and a superiority of this method in the prevention of aortic root dilatation.
2.2 Ross Operation
In 1967, Donald Ross [4] developed the idea of using an autologous pulmonary valve to replace the aortic valve. At first the pulmonary valve was trimmed in scallop and reimplanted at subcoronary position. Inclusion cylinder method had also been performed to simplify the procedure. Nowadays full root replacement with pulmonary autograft is most prevailed.
After establishment of the cardiopulmonary bypass, the main pulmonary artery is transected just below its branches. The pulmonary valve is satisfactorily inspected if not diseased. Then the ascending aorta is cross-clamped and transected just above the sino-tubular junction. The aortic valve is removed. Both coronary ostia are removed with a large button of the aortic wall. The pulmonary artery is separated from the ascending aorta. The RV free wall is incised a few millimeters below the pulmonary annulus. After that, the incision is extended transversally and posteriorly. The endocardium on the posterior aspect of the RV is incised below the pulmonary valve, and the pulmonary artery is enucleated (Fig. 12.6a). Great care is necessary not to injure the first septal branch of the left anterior descending coronary artery.
The pulmonary autograft is sutured to the aortic annulus with many simple interrupted sutures or a mixture of continuous running and interrupted sutures. Usually autologous pericardial strip is used to reinforce the suture line. Then incisions are made in the corresponding area of the left and right coronary artery. Large enough holes are made, and both coronary buttons are sutured to the pulmonary autograft. The distal end of the pulmonary autograft is trimmed and sutured to the distal ascending aorta. The enucleated RV outflow tract and the pulmonary artery are reconstructed, usually with a homograft or other valved conduits (Fig. 12.6c) (Fig. 12.7).
The most prevalent indication for Ross operation is aortic stenosis or a combination of stenosis and insufficiency. When the aortic annulus is too small for the pulmonary autograft, Ross-Konno operation [10] can be performed (Figs. 12.6a, 12.6b, and 12.6c).
Superior hemodynamics, freedom from anticoagulation, and longevity of the pulmonary autograft have been substantiated. Growth potential with somatic growth or merely pathological dilatation of the autograft is also expected among young patients. Elkins RC et al. [11] reviewed 487 consecutive patients with the age from 2 days to 62 years (median 24 years), who underwent Ross procedure between 1986 and 2002. Actuarial survival was 82 ± 6 % at 16 years, freedom from autograft failure was 74±5 %, and freedom from allograft reoperation or reintervention was 82±4 %. Kieverik et al. reported their 146 patients of Ross procedure, aged 4 months to 52 years (mean 22 years). The survival at 13 years was excellent as much as 94±2 %; freedom from autograft and allograft reoperation were 69.7±7 % and 87.5±5 % at 13 years, respectively. Adult patients tended to be associated with higher risk of autograft reoperation, so that the Ross operation is performed only in infants and children in their center [12]. In contrast to this study, Sievers et al. reviewed 1779 adult patients with the Ross procedure in eight centers in Germany, and the Ross procedure should be considered in young and active patients based on the excellent results in their study [13]. Since the Ross procedure requires considerable experience to obtain acceptable results, introduction of the Ross procedure to the adult patients is still controversial.
References
Bentall H, De Bono A (1968) A technique for complete replacement of the ascending aorta. Thorax 23(4):338–339
Sarsam MA, Yacoub M (1993) Remodeling of the aortic valve anulus. J Thorac Cardiovasc Surg 105(3):435–438
David TE, Feindel CM, Bos J. (1995) Repair of the aortic valve in patients with aortic insufficiency and aortic root aneurysm. J Thorac Cardiovasc Surg 109(2):345–351; discussion 51–2
Ross DN (1967) Replacement of aortic and mitral valves with a pulmonary autograft. Lancet 2(7523):956–958
Niwa K (2005) Aortic root dilatation in tetralogy of Fallot long-term after repair-histology of the aorta in tetralogy of Fallot: evidence of intrinsic aortopathy. Int J Cardiol 103:117–119
Wanes CA, William RG, Bashore TM et al (2008) ACC/AHA 2008 guidelines for the management of adults with congenital heart disease. Circulation 118:e714–e833
Gatzoulis MA, Webb GD, Daubeney PEF (2003) Diagnosis and management of adult congenital heart disease. Churchill Livingstone, Edinburgh, pp p315–p326
Leyh RG, Schmidtke C et al (1999) Opening and closing characteristics of the aortic valve after different types of valve-preserving surgery. Circulation 100(21):2153–2160
Richardt D, Stierle U, Sievers HH (2015) Long-term results after aortic valve-sparing-reimplantation operation (David) in bicuspid aortic valve. J Heart Valve Dis 24(1):4–9
Hraska V, Photiadis J, Poruban R, et al. (2008) Ross-Konno operation in children. Multimed Man Cardiothorac Surg 2008(915):mmcts 2008 003160
Elkins RC, Thompson DM, Lane MM, et al. (2008) Ross operation: 16-year experience. J Thorac Cardiovasc Surg 136(3):623–630, 30 e1–5
Klieverik LM, Takkenberg JJ, Bekkers JA et al (2007) The Ross operation: a trojan horse? Eur Heart J 28(16):1993–2000
Sievers HH, Stierle U, Charitos EI et al (2016) A multicentre evaluation of the autograft procedure for young patients undergoing aortic valve replacement: update on the German Ross Registrydagger. Eur J Cardiothorac Surg 49(1):212–218
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Japan KK
About this chapter
Cite this chapter
Matsuo, K. (2017). Surgery (Bentall, Valve Sparing, Ross Procedure, Etc.). In: Niwa, K., Kaemmerer, H. (eds) Aortopathy. Springer, Tokyo. https://doi.org/10.1007/978-4-431-56071-5_12
Download citation
DOI: https://doi.org/10.1007/978-4-431-56071-5_12
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-56069-2
Online ISBN: 978-4-431-56071-5
eBook Packages: MedicineMedicine (R0)