Abstract
Idiopathic pulmonary fibrosis (IPF), the most common form of idiopathic interstitial pneumonias (IIPs), is a fatal disease with a mean survival time of 2–4 years from the time of diagnosis. Therefore, the early and accurate diagnosis of IPF is important and essential for management and induction of optimal therapies. In 2002, the American Thoracic Society and European Respiratory Society (ATS/ERS) published an international statement on the diagnosis and management of IPF. The 2002 ATS/ERS statement defined IPF as a distinct clinical entity associated with the histology of usual interstitial pneumonia (UIP). The revised evidence-based guidelines for diagnosis and management of IPF were published by collaboration between the ATS, ERS, Japanese Respiratory Society (JRS), and Latin American Thoracic Association (ALAT) in 2011. In the revised 2011 criteria, high-resolution CT (HRCT) has a central role for the diagnosis of IPF. The presence of UIP patterns on HRCT is essential and definitive in the diagnosis of IPF without the need for surgical lung biopsy (SLB). The revised 2011 criteria have emphasized the importance of multidisciplinary discussion between clinicians, radiologists, and pathologists experienced in the diagnosis of IPF.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Idiopathic pulmonary fibrosis (IPF)
- High-resolution CT (HRCT)
- ATS/ERS statement
- ATS/ERS/JRS/ALAT statement
1 Introduction
The idiopathic interstitial pneumonias (IIPs) are a group of diffuse parenchymal lung diseases of unknown etiology with varying degrees of inflammation and fibrosis [1]. In 1975, Liebow first described five pathologic subgroups of chronic idiopathic interstitial pneumonia: usual interstitial pneumonia (UIP), diffuse lesions similar to UIP with superimposed bronchiolitis obliterans (termed bronchiolitis interstitial pneumonia), desquamative interstitial pneumonia (DIP), lymphocytic interstitial pneumonia (LIP), and giant cell pneumonia [2].
In 1998, Kazenstein and Myers revised the classification including five histopathologically distinct subgroups: UIP, DIP, respiratory bronchiolitis-associated interstitial lung disease (RB-ILD), acute interstitial pneumonia (AIP), and nonspecific interstitial pneumonia (NSIP). AIP and NSIP were introduced as IIPs [3].
In 2002, the American Thoracic Society (ATS)/European Respiratory Society (ERS) international multidisciplinary panel proposed a new classification of IIPs that are comprised of seven clinical-pathological entities such as IPF, NSIP, cryptogenic organizing pneumonia (COP), AIP, RB-ILD, DIP, and LIP [1]. The 2002 ATS/ERS statement emphasized the importance of interaction among clinicians, radiologists, and pathologists for the final diagnosis of IIPs. IPF was defined to a distinctive type of chronic fibrosing interstitial pneumonia of unknown cause limited to the lungs and associated with a surgical lung biopsy showing a histopathologic pattern of UIP. The definitive diagnosis of IPF required histopathologic patterns of UIP on surgical lung biopsy (SLB). In the absence of SLB, a presumptive diagnosis can be made by clinical, radiologic, and physiologic criteria (four major and three minor criteria). IPF is the most common and severe form of IIPs. The prognosis of IPF has been reported to be very poor with a mean survival of 2–4 years after the initial diagnosis. Therefore, an early and accurate diagnosis of IPF is critical, especially for the management and induction of treatment to prevent disease progression [4].
In 2011, the ATS/ERS/Japanese Respiratory Society (JRS)/Latin American Thoracic Association (ALAT) has published revised evidenced-based guidelines for diagnosis and management of IPF [5]. This chapter focuses on the definition of IPF in the revised 2011 criteria and discusses clinical application and key problems.
2 The ATS/ERS/JRS/ALAT 2011 Revised Diagnostic Criteria [5]
In the 2011 revised criteria, IPF is defined as a specific form of chronic, progressive fibrosing interstitial pneumonia of unknown cause, occurring in older adults, limited to the lungs, and associated with the histopathologic and/or radiologic pattern of UIP.
The diagnosis of IPF requires:
-
(a)
Exclusion of other causes of interstitial lung disease (ILD) (e.g., domestic and occupational environmental exposures, connective tissue diseases, and drug toxicity)
-
(b)
The presence of UIP pattern on high-resolution computed tomography (HRCT) in patients not subjected to surgical lung biopsy
-
(c)
Specific combination of HRCT and surgical lung biopsy pattern in patients subjected to surgical lung biopsy
-
The major and minor criteria proposed in the 2002 ATS/ERS consensus statement have been eliminated.
The accuracy of the diagnosis of IPF increases with multidisciplinary discussion between pulmonologists, radiologists, and pathologists experienced in the diagnosis of ILDs.
IPF is a fatal lung disease; the natural history is variable and unpredictable. Most patients with IPF demonstrate a gradual worsening of lung function over years; a minority of patients remain stable or decline rapidly. Some patients may experience episodes of acute respiratory worsening despite previous stability.
Disease progression is manifested by increasing respiratory symptoms, worsening pulmonary function test results, progressive fibrosis on HRCT, acute respiratory decline, or death.
Patients with IPF may have subclinical or overt comorbid conditions including pulmonary hypertension, gastroesophageal reflux, obstructive sleep apnea, obesity, and emphysema. The impact of these conditions on the outcome of patients with IPF is unclear.
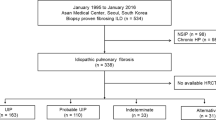
The diagnostic algorithm for adult patients with suspected IPF is shown in Fig. 1.1. HRCT has an essential role in the diagnostic pathway in IPF (Fig. 1.1 and Table 1.1). UIP is characterized on HRCT by the presence of reticular opacities, often associated with traction bronchiectasis. Honeycombing is common and critical for making a definite diagnosis of IPF. Honeycombing is manifested on HRCT as clustered cystic airspaces, typically of comparable diameters in the order rof 3–10 mm but occasionally as large as 25 mm. It is usually subpleural and is characterized by well-defined walls. Ground-glass opacities are common, but usually less extensive than the reticulation. The distribution of UIP on HRCT is characteristically basal and peripheral, though often patchy. The presence of coexistent pleural abnormalities (e.g., pleural plaques, calcifications, significant pleural effusion) suggests an alternative etiology for UIP pattern. Micronodules, air trapping, non-honeycomb cysts, extensive ground-glass opacities, consolidation, or a peribronchovascular-predominant distribution should lead to consideration of an alternative diagnosis. Mild mediastinal lymph node enlargement (usually <1.5 cm in short axis) can be seen. Possible UIP and inconsistent with UIP patterns on HRCT are presented in Table 1.1. The UIP pattern does not need to be confirmed by histopathology. In patients demonstrating radiological features that meet the criteria for “possible UIP” or “inconsistent with UIP” patterns on HRCT, SLB should be considered. Patients with a possible UIP pattern on HRCT and UIP or probable histological UIP pattern allow for the diagnosis of IPF (Table 1.2). Combinations of HRCT and SLB for the diagnosis are presented in the revised 2011 criteria (Table 1.2). The major and minor criteria for the clinical diagnosis of IPF in the 2002 ATS/ERS consensus statement have been eliminated. It is most important to make an accurate diagnosis of IPF through multidisciplinary discussion between clinicians, radiologists, and pathologists.
Diagnostic algorithm for idiopathic pulmonary fibrosis (IPF). Patients with suspected IPF should be carefully evaluated for identifiable causes of interstitial lung disease (ILD). In the absence of an identifiable cause for ILD, an HRCT demonstrating UIP pattern is diagnostic of IPF. In the absence of UIP pattern on HRCT, IPF can be diagnosed by the combination of specific HRCT and histopathologic pattern. The accuracy of the diagnosis of IPF increases with multidisciplinary discussion among ILD experts [5]
3 Clinical Application and Key Problems
To exclude other known causes of lung fibrosis represents a key factor in the diagnostic process of IPF. Careful medical history and physical examinations focusing on comorbidities, drug use, environmental exposures, and family histories are needed. It is very important to evaluate possibilities of chronic hypersensitivity pneumonitis (CHP), because such patients might mimic IPF. Patients who met the criteria for collagen vascular disease do not have the diagnosis of IPF. Even without clinical or serologic features at presentation, clinical features of collagen vascular disease may reveal thereafter. Even though surgical lung biopsy demonstrates histopathological features of UIP, a definitive diagnosis required the exclusion of other causes of ILDs, including chronic hypersensitivity pneumonitis, collagen vascular disease, drug toxicity, asbestosis, and familial interstitial pneumonia.
The identification of honeycombing is central in the diagnosis of IPF. Several studies have documented that the positive predictive value with HRCT diagnosis of UIP is more than 90 % [5]. The accuracy of trained observers in distinguishing IPF from other ILDs is approximately 80–90 % [6]. There is substantial variation in the distinction between typical and atypical HRCT findings of IPF among less experienced observers [6]. Interobserver variation is a significant problem in the diagnostic process of IPF. If honeycombing is absent, however, other HRCT features meet the criteria for IPF, the imaging features are regarded as possible UIP, and SLB is necessary to make an accurate diagnosis. Even in patients without honeycombing on HRCT, combinations of interstitial scoring and older age (over 65) have reported to be highly predictive of the diagnosis of IPF [7]. It is necessary to establish the standardization of prognostic pathway and quality assurance for the accurate diagnosis of IPF.
4 Conclusion
The 2011 ATS/ERS/JRS/ALAT evidenced-based guidelines for IPF are major improvement from the previous 2002 ATS/ERS statements. The guidelines emphasize the importance of HRCT for the diagnosis of definite IPF. In the absence of UIP patterns on HRCT, combined radiological and pathological findings are needed. It is most important to make a final diagnosis of IPF through multidisciplinary discussion between clinicians, radiologists, and pathologists. There is a need for clinician training in integrating data from clinical, radiological, and histological examinations to achieve the accurate diagnosis of IPF.
References
American Thoracic Society, European Respiratory Society. American Thoracic Society/European Respiratory Society international multidisciplinary consensus classification of the idiopathic interstitial pneumonia. Am J Respir Crit Care Med. 2002;165:277–304.
Liebow AA. Definition and classification of interstitial pneumonia in human pathology. Prog Respir Res. 1975;8:1–31.
Kazenstein AA, Myers JL. Idiopathic pulmonary fibrosis: clinical relevance of pathologic classification. Am J Respir Crit Care Med. 1998;157:1301–15.
Kim DS, Collard HR, Talmadge E, et al. Classification and natural history of the idiopathic interstitial pneumonia. Proc Am Thorac Soc. 2006;3:285–92.
Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824.
Wells AU. Managing diagnostic procedures in idiopathic pulmonary fibrosis. Eur Respir Rev. 2013;22:158–62.
Fell CD, Martinez FJ, Liu LX, et al. Clinical predictors of a diagnosis of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2010;181:832–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Japan
About this chapter
Cite this chapter
Abe, S., Gemma, A. (2016). Definition of IPF. In: Nakamura, H., Aoshiba, K. (eds) Idiopathic Pulmonary Fibrosis. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55582-7_1
Download citation
DOI: https://doi.org/10.1007/978-4-431-55582-7_1
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55581-0
Online ISBN: 978-4-431-55582-7
eBook Packages: MedicineMedicine (R0)