Abstract
A detailed and accurate pretherapeutic evaluation of stage plays a crucial role in the prognosis as well as the choice and extent of the therapeutic procedure required for patients with oral cancer. For this purpose, various modern diagnostic imaging modalities are routinely used. In this section, the potential roles of conventional X-rays, computed tomography (CT), magnetic resonance imaging (MRI), ultrasonography (US), and positron emission tomography (PET)/CT in the staging of oral cancer are addressed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
5.1 Imaging Techniques
5.1.1 Conventional X-Ray in Oral Cancer
A conventional X-ray is commonly used for surveillance of oral cancer. Because of the limited viewing direction, its role in staging of oral cancer is limited. This technique renders a three-dimensional volume onto a two-dimensional plane. As a consequence, overlying and underlying tissues and structures are superimposed, which generally results in reduced conspicuity as well as subject contrast.
5.1.1.1 Dental X-Ray
The detailed shape of the margins of bone absorption in gingival carcinoma can be assessed with a dental X-ray. Small fragments of the destroyed bone can also be detected. The exact extent of the tumor involvement can hardly be evaluated because of the superimposition of adjacent structures.
5.1.1.2 Orthopantomography (Panoramic X-Ray)
Orthopantomography is a two-dimensional half-circle view of the upper and lower jaws from ear to ear obtained by panoramic X-ray scanning. Its intrinsic value is screening for malignancy in routine dental practice. Marked maxillary or mandibular bone absorption caused by gingival, floor of mouth, and tongue carcinomas can be detected by orthopantomography. However, the diagnostic sensitivity for the extent of tumor involvement is insufficient compared with modern sectional imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI), because of the limited viewing direction. From the viewpoint of treatment outcome, the Japan Society for Oral Tumors (JSOT) proposed a classification regarding the shape of the absorbed bone involved in gingival carcinoma [1]. The characteristic shape of the absorbed bone margin was classified into three types: pressure type; moth-eaten type; and intermediate type (Fig. 5.72). Moth-eaten type, which commonly shows a poorer outcome, is applied if an ill-defined permeated margin and small bone fragments within the lesion are observed.
5.1.1.3 Other Conventional X-Ray
Posteroanterior projection and Waters projection X-rays can occasionally reveal bone destruction at the lateral portion of the maxilla and mandibular bone structure, which might be overlooked by orthopantomography.
5.1.2 CT in Oral Cancer
5.1.2.1 Plain CT and CECT
CT is a fundamental cross-sectional imaging modality for evaluating oral cancer and is superior for detecting cortical bone destruction and intratumoral calcification compared with other imaging modalities [2]. As modern CT equipment can deal with isotropic voxel data, three-dimensional evaluation using multiplanar reformatted images is routinely used to define the extent of tumor involvement. Contrast-enhanced CT (CECT) using iodine contrast materials is an excellent modality for oral cancer staging, i.e., determining the tumor extent (especially depth of invasion) and size, identifying lymph node metastases, assessing response to therapy, and evaluating recurrent disease.
On CT, tumors appear as homogeneous or heterogeneous soft-tissue-attenuated lesions that are variably enhanced after intravenous administration of iodine contrast materials [3]. Commonly, the tumor is intensely enhanced compared with adjacent normal structures because of the tumor neoangiogenesis, and a central necrotic portion is frequently identified as a non-enhanced or barely enhanced hypodense area within the tumor mass. There may be early or prominent enhancement of the tumor margins, because of the higher vascularity of the tumor periphery.
Tumors located around the occlusal plane level are frequently obscured with metallic artifacts caused by dental prostheses. A CT image is also degraded by motion artifacts, but is less affected by breathing and swallowing artifacts than MRI. Good-quality imaging obtained with CT is readily reproducible. A soft-tissue window setting image with a soft-tissue algorithm at a level of 40–50 with a window width of 250–350 is recommended for discrimination of enhanced tumor tissue. In addition, a bone window setting with a bone algorithm should be used for osseous involvement of the tumor (thin slice images of less than 1 mm are preferable). For routine examination in oral cancer, contiguous scanning from the level of the nasopharynx to the level of the supraclavicular fossa is recommended.
5.1.2.2 CT Perfusion
CT Perfusion (CTP) is a technique that measures the parameters of tissue perfusion through dynamic acquisition of images after contrast material administration (Fig. 5.130) [2]. The physiologic basis of contrast enhancement on CT closely mimics the physiologic effects of tumor angiogenesis. Angiogenesis is a key factor for tumor growth and metastasis and is a complex process that includes endothelial cell breakdown, proliferation, and migration stimulated by angiogenic factors. CTP can be routinely performed on all modern CT equipment and is potentially useful to distinguish neoplasms from normal structures and posttreatment changes. The major drawback of CTP is an excessive radiation exposure dose, and therefore lower tube voltages and mAs are recommended.
5.1.3 CBCT in Oral Cancer
As a modern cone-beam CT (CBCT) system has relatively higher spatial resolution compared with a CT system, the significance of CBCT in the evaluation of osseous involvement is almost equal or superior to the bone-algorithm CT. The major disadvantage of CBCT is poor soft-tissue contrast because of the limited radiation exposure. The tumor mass is hardly visualized clearly with CBCT, and therefore neoplastic processes are frequently overlooked. The limited field of view is another drawback of CBCT in the evaluation of tumor extent. Therefore, the role of CBCT in oral cancer staging is limited.
5.1.4 MRI in Oral Cancer
5.1.4.1 Plain MRI and Contrast-Enhanced MRI
MRI uses the magnetic properties of hydrogen and its interactions with both a large external magnetic field and radio waves to produce highly detailed images of the human body.
MRI has superior soft-tissue contrast compared with CT and may provide better delineation of soft-tissue invasion of the carcinoma [3]. The lack of ionizing radiation makes it the preferred technique in patients with iodine allergy. There is also the advantage of reduced metallic artifacts from metallic dental prostheses. However, the images are often degraded by magnetic metallic materials and unexpected oral motion. The major drawbacks of MRI are the relatively high cost and claustrophobia.
On conventional T1-weighted images obtained without fat saturation, a squamous cell carcinoma (SCC) has intermediate signal intensity and is generally isointense to muscle. On T2-weighted images, an SCC is typically heterogeneous and hyperintense to normal muscle, making it more conspicuous. However, the tumor size might be overestimated on T2-weighted images because the tumor cannot be distinguished from surrounding inflammation and edema. On gadolinium-enhanced T1-weighted images, the tumor has variable enhancement and conspicuity. Fat-saturated images are helpful in distinguishing tumors from normal surrounding structures. Axial and coronal contrast-enhanced T1-weighted images with fat saturation are superior to CT for defining the soft-tissue extent. One of the disadvantages of fat saturation is increased susceptibility to artifacts, particularly in locations near the bone or air.
MRI is the optimal modality for detection of perineural tumor spreading [3]. Direct signs of perineural tumor spreading are enlargement, irregularity, and abnormal enhancement of the major cranial nerves and their branches. Replacement of high-intensity fat-containing spaces adjacent to the major skull foramina, such as the pterygopalatine fossa, by tumor tissue is also a valuable clue to the presence of perineural tumor spreading. Although CT is generally considered superior for detection of cortical erosion, MRI is more sensitive for identification of early bone marrow invasion. Findings suggestive of marrow invasion are replacement of normal high-intensity marrow fat by tumor tissue. Dynamic contrast-enhanced MRI provides better delineation of the tumor margin.
5.1.4.2 Diffusion-Weighted MRI
Diffusion reflects the random motion of molecules, and diffusion-weighted imaging (DWI) is an MRI technique wherein images are weighted with the local characteristics of water diffusion [2]. The apparent diffusion coefficient (ADC) is a measure of the magnitude of freedom of water diffusion. Higher ADC values indicate greater magnitude of water diffusion, while lower ADC values indicate lesser magnitude of water diffusion and restricted motion. The DWI signal intensity is dependent on the magnitude of water motion. Highly cellular tissues exhibit lower ADC values than acellular or hypocellular tissues. Generally, the ADC of malignant lesions is lower than that of benign lesions (Figs. 5.54, 5.80 and 5.103). Malignant lymph nodes tend to have lower ADC values than nonmalignant lymph nodes.
5.1.5 Ultrasonography (US) in Oral Cancer
US is based on the pulse-echo principle, in which a short burst of ultrasound is emitted from a transducer and directed into a tissue, and echoes are produced as a result of the interactions of the ultrasound with the tissue, traveling back to the transducer. By timing the period that elapses between the emission of the pulse and the reception of the echo, the distance between the transducer and the echo-producing structure can be calculated. US is a real-time, multiplanar, dynamic assessment technique for oral, maxillofacial, and neck structures. The high spatial resolution of modern US equipment is superior to CT and MRI. US has limited beam penetration, with the depth inversely proportional to the frequency. Power or color Doppler sonography is useful for detection of blood flow. Elastosonography has a potential role in differentiating benign tissue from malignant tissue (Figs. 5.123 and 5.129).
5.1.5.1 Intraoral US
A small carcinoma (T1, T2) of the mobile tongue and buccal mucosa may be visualized by intraoral US (Figs. 5.60 and 5.68) [1]. Intraoral US is performed by direct contact with the surface of the carcinoma, and therefore a small intraoperative transducer is preferable. If a thin polymer gel pad is placed as an acoustic coupling device between the probe surface and the tumor surface, three layers are clearly distinguished: (a) surface layer (hyperechoic line); (b) mucosal layer (hypoechoic line); and (c) submucosal and muscular layer (heterogeneous internal echo). Commonly, an SCC arising from the mucous membrane appears as a focal hypoechoic area continuous with the surrounding normal mucosal layer and the depth of invasion can be measured accurately (Figs. 5.60 and 5.68). Evaluation of the invasion depth of a tongue carcinoma may be useful for prediction of subsequent lymph node metastasis. In addition, Doppler US demonstrates prominent vascularity around the deep margins, arising from neoangiogenesis at the tumor invasion front. Intraoral US has a superior ability to evaluate the depth of invasion of a tumor compared with other imaging modalities.
5.1.5.2 Face and Neck US
Nodal involvement is the most important prognostic factor for oral cancer. US is the most accurate method currently available for detecting neck lymph node metastasis. Retropharyngeal and mediastinal nodes are inaccessible by US and require evaluation by CT or MRI. The US features of metastatic nodes are round shape, heterogeneity, loss of normal hilum, internal necrosis, and peripheral vascularity (Figs. 5.122 and 5.128). An ill-defined border in a metastatic node suggests extracapsular spread. With regard to internal necrosis, marked cystic degeneration is interpreted as a hypoechoic or non-echoic area with an irregular margin, whereas keratinization is demonstrated as an ill-defined hyperechoic area within a node [1]. However, diffuse-spreading tumor tissue that lacks obvious necrosis may be overlooked on a routine B-mode image only.
5.1.6 PET/CT in Oral Cancer
Positron emission tomography (PET)/CT, reflecting PET combined with CT, is the best modality for staging, monitoring, and surveillance of advanced oral cancer (Fig. 5.125) [2]. The utility of PET/CT in staging depends on the size of the primary tumor, and therefore PET/CT is not useful for a very small tumor. PET/CT is useful for identifying unsuspected additional primary tumors and/or distant metastases at the time of staging of a known primary tumor. 18F-fluorodeoxyglucose (FDG) is transported into cells like glucose by transmembrane transporters and becomes trapped, thereby accumulating in cells with high glucose metabolism. The standardized uptake value (SUV) is the quantified measure of FDG uptake. However, the SUV is highly dependent on the machine used and the patient characteristics. A small tumor size limits the detection of FDG uptake and the minimal size limit is about 5 mm. Normal physiologic uptake should be encountered. Normal salivary glands exhibit low-level FDG uptake, while lymphoid tissue uptake is highly variable, especially at the tonsils and tongue base.
5.2 Sectional Anatomy of the Oral Cavity (Figs. 5.1, 5.2, 5.3, 5.4, 5.5, 5.6, 5.7, 5.8, 5.9, 5.10, 5.11, 5.12, 5.13, 5.14, 5.15, 5.16, 5.17, 5.18, 5.19, 5.20, 5.21, 5.22, 5.23, 5.24, 5.25, 5.26, 5.27, 5.28, 5.29, 5.30, 5.31, 5.32, 5.33, 5.34, 5.35, 5.36, 5.37, 5.38, 5.39, 5.40, 5.41, 5.42, 5.43, 5.44, 5.45, 5.46 and 5.47)
5.3 Oral Cancer Staging
5.3.1 TNM (UICC Staging)
(Mainly cited from: 2010 American Joint Committee on Cancer Definitions of TNM for the Lip and Oral avity [4])
5.3.2 Primary Tumor (T)
T factor
-
TX
Primary tumor cannot be assessed
-
T0
No evidence of primary tumor
-
Tis
Carcinoma in situ
-
T1
Tumor 2 cm or less in greatest dimension
-
T2
Tumor more than 2 cm but not more than 4 cm in greatest dimension
-
T3
Tumor more than 4 cm in greatest dimension
-
T4a
Moderately advanced local disease; tumor invades adjacent structures
(according to the 2012 General Rules for Clinical and Pathological Studies on Oral Cancer by the Scientific Committee of Japan Society for Oral Tumors [5]):
-
1.
Tongue: invasion into the mandibular bone marrow, invasion into the submandibular space, and invasion into the extrinsic muscles of the tongue
-
2.
Upper gingiva: invasion into the maxillary sinus and nasal cavity and invasion into the buccal space or subcutaneous fat
-
3.
Lower gingiva: invasion reaching the mandibular canal, invasion into the buccal space or subcutaneous fat, invasion into the submandibular space, and invasion into the extrinsic muscles of the tongue
-
4.
Buccal mucosa: invasion into the subcutaneous fat, invasion into the maxillary and mandibular bone marrow, and invasion into the maxillary sinus
-
5.
Floor of the mouth: invasion into the mandibular bone marrow, invasion into the submandibular space, and invasion into the extrinsic muscles of the tongue
-
6.
Hard palate: invasion into the maxillary sinus and nasal cavity
-
1.
-
T4b
Very advanced local disease; tumor invasion into the masticator space, invasion into the pterygoid plate, invasion into the skull base, and invasion circumferentially surrounding the internal carotid artery
5.3.3 Regional Lymph Nodes (N)
The classification and range of cervical lymph nodes are the same as described in the Rules Regarding Lymph Nodes by the Japan Society of Clinical Oncology (JSCO), and lymph node metastasis is evaluated according to the UICC classification. Internationally, the level classification system by the Academy’s Committee for Head and Neck Surgery and Oncology (ACHNSO) based on the area of neck dissection is widely used, and the AAO-HNS classification, a fragmented version of the ACHNSO classification, has also been proposed [5].
N factor
-
NX
Regional lymph nodes cannot be assessed
-
N0
No regional lymph node metastasis
-
N1
Metastasis in a single ipsilateral lymph node, 3 cm or less in greatest diameter
-
N2
Metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in greatest dimension; or in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension; or in bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension
-
N2a
Metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in greatest dimension
-
N2b
Metastasis in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension
-
N2c
Metastasis in bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension
-
N3
Metastasis in a lymph node, more than 6 cm in greatest dimension
5.3.4 Distant Metastasis (M)
M Factor
-
M0
No distant metastasis
-
M1
Distant metastasis present
- 0:
-
Tis, N0, M0
- I:
-
T1, N0, M0
- II:
-
T2, N0, M0
- III:
-
T3, N0, M0
T1, T2 or T3, N1, M0
- IVA:
-
T4a, N0 or N1, M0
T1, T2, T3 or T4a, N2, M0
- IVB:
-
Any T, N3, M0
T4a and any N, M0
- IVC:
-
Any T and any N M1
- Level IA:
-
Submental lymph nodes; they lie between medial margins of the anterior bellies of the digastric muscles.
- Level IB:
-
Submandibular lymph nodes; on each side, they lie lateral to the level IA nodes and anterior to the back of each submandibular gland.
- Level IIA:
-
Superior internal jugular lymph nodes, superior deep cervical lymph nodes (jugulodigastric nodes, anterior); they lie either anterior, medial, lateral, or posterior to the internal jugular vein. If posterior to the vein, the node is inseparable from the vein.
- Level IIB:
-
Superior internal jugular lymph nodes, superior deep cervical lymph nodes (jugulodigastric nodes, posterior); they lie posterior to the internal jugular vein and have a fat plane separating it from the vein.
- Level III:
-
Middle internal jugular lymph nodes, middle deep cervical lymph nodes (jugulo-omohyoid nodes); they extend from the level of the bottom of the body of the hyoid bone to the level of the bottom of the cricoid arch. They lie anterior to the back of the sternocleidomastoid muscle.
- Level IV:
-
Inferior internal jugular lymph nodes, inferior deep cervical lymph nodes; they extend from the level of the bottom of the cricoid arch to the level of the clavicle.
- Level VA:
-
Spinal accessory lymph nodes; they extend from the skull base to the level of the bottom of the cricoid arch.
- Level VB:
-
Supraclavicular lymph nodes; they extend from the level of the bottom of the cricoid arch to the level of the clavicle.
5.4 Oral Cavity Malignancies
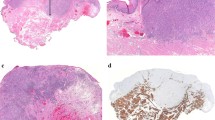
5.4.1 Tongue Carcinoma [Squamous Cell Carcinoma (SCC)]
5.4.1.1 Case 1: 82-Year-Old Female, Left-Tongue SCC T4aN0 (Figs. 5.49, 5.50, 5.51, 5.52, 5.53, 5.54, 5.55, 5.56, 5.57, 5.58 and 5.59)
5.4.1.2 Case 2: 60-Year-Old Female, Left-Tongue SCC T4aN0 (Figs. 5.60, 5.61, 5.62, 5.63, 5.64, 5.65, 5.66 and 5.67)
Intraoral ultrasonography with the acoustic coupling device between the probe surface and the tumor surface (left, fine flow Doppler; right, B-mode). Tumor is demonstrated as an ill-defined hypoechoic area (arrow) continuous with the surrounding normal mucosal layer. Note the vascularity around the deep margins arising from neoangiogenesis at the tumor invasion front (arrowheads)
5.4.1.3 Case 3: 60-Year-Old Female, Right-Tongue SCC T2N0 (Figs. 5.68, 5.69, 5.70 and 5.71)
Intraoral ultrasonography with the acoustic coupling device between the probe surface and the tumor surface (left, fine flow Doppler; right, B-mode). Tumor is demonstrated clearly as an ill-defined hypoechoic area (arrow) continuous with the surrounding normal mucosal layer. Note the prominent vascularity around the deep margins arising from neoangiogenesis at the tumor invasion front (arrowheads)
5.4.2 Gingival Carcinoma
5.4.2.1 Case 3: 62-Year-Old Male, Left-Mandibular Gingival SCC T4aN0 (Figs. 5.72, 5.73, 5.74, 5.75, 5.76, 5.77, 5.78, 5.79, 5.80, 5.81, 5.82, 5.83 and 5.84)
5.4.2.2 Case 4: 85-Year-Old Male, Right-Maxillary Gingival SCC, T4aN0 (Figs. 5.85, 5.86, 5.87, 5.88, 5.89, 5.90, 5.91, 5.92, 5.93, 5.94, 5.95 and 5.96)
5.4.3 Floor of the Mouth Carcinoma
5.4.3.1 Case 5: 64-Year-Old Male, Floor of the Mouth SCC T4aN2c (Figs. 5.97, 5.98, 5.99, 5.100, 5.101, 5.102, 5.103, 5.104 and 5.105)
5.4.4 Buccal Mucosa Carcinoma
5.4.4.1 Case 6: 78-Year-Old Male, Buccal Mucosa SCC T2N0 (Figs. 5.106, 5.107, 5.108, 5.109, 5.110, 5.111, 5.112, 5.113, 5.114 and 5.115)
5.4.5 Lymph Node Metastasis
5.4.5.1 Case 7: 64-Year-Old Male, Floor of the Mouth SCC T4aN2c (Figs. 5.116, 5.117, 5.118, 5.119, 5.120, 5.121, 5.122, 5.123, 5.124, 5.125 and 5.126)
5.4.5.2 Case 8: 61-Year-Old Male, Left-Maxillary Gingival SCC T1N2b (Figs. 5.127, 5.128, 5.129, 5.130 and 5.131)
References
Izumo T, Ariji E, Ozeki S, Okada N, Okabe S, Okazaki Y, Omura K, Kirita T, Kusama M, Sato T, Shinohara M, Shimozato K, Shintani S, Tanaka Y, Nakayama E, Hayashi T, Miyazaki A, Yagishita H, Yamane M, Working Group 1 on the ‘Guidelines for Clinical and Pathological Studies of Oral Cancer’, Scientific Committee, Japan Society for Oral Tumors (2010) General rules for clinical and pathological studies on oral cancer, 1st edn. Kaneharashuppan, Tokyo
Glastonbury CM, Harnsberger HR, Michel MA, Branstetter BF, Hudgins PA, Shatzkes D (eds) (2012) Specialty imaging: head and neck cancer: state of the art diagnosis, staging, and surveillance. Amirsys Publishing, Inc., Salt Lake City
Som PM, Curtin HD (2011) Head and neck imaging, 5th edn. Elsevier Mosby Inc., St. Louis
Edge SB, Byrd DR, Compton CC et al (eds) (2010) AJCC cancer staging manual, 7th edn. Springer, New York
Izumo T, Kirita T, Ariji E, Ozeki S, Okada N, Okabe S, Okazaki Y, Omura K, Kusama M, Sato T, Shinohara M, Shimozato K, Shintani S, Tanaka Y, Nakayama E, Hayashi T, Miyazaki A, Yagishita H, Yamane M, Working Group 1 on the "Guidelines for Clinical and Pathological Studies of Oral Cancer", Scientific Committee, Japan Society for Oral Tumors (2012) General rules for clinical and pathological studies on oral cancer: a synopsis. Jpn J Clin Oncol 42:1099–1109. doi:10.1093/jjco/hys141
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Japan
About this chapter
Cite this chapter
Hayashi, T. (2015). Imaging and Classification of Staging. In: Kirita, T., Omura, K. (eds) Oral Cancer. Springer, Tokyo. https://doi.org/10.1007/978-4-431-54938-3_5
Download citation
DOI: https://doi.org/10.1007/978-4-431-54938-3_5
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-54937-6
Online ISBN: 978-4-431-54938-3
eBook Packages: MedicineMedicine (R0)