Abstract
The autoimmune pancreatitis (AIP) seen in Japan occurs preferentially in older men, presents with jaundice in many cases, and is seldom associated with symptoms and signs of acute pancreatitis. Elevated serum IgG4 concentrations are noted in a high proportion of cases, and the pancreas characteristically shows a marked lymphoplasmacytic infiltrate with IgG4-positive plasma cells and fibrosis. This entity has been termed lymphoplasmacytic sclerosing pancreatitis (LPSP) and is now known also as type 1 (IgG4-related) AIP.
In contrast, data to date suggest that a different pattern (i.e., a different type) of AIP is more common in Western countries. In the West, AIP often presents at a younger age and has a balanced sex distribution. Moreover, AIP in the West is frequently complicated by inflammatory bowel disease. Most importantly, the pathological features of this other form of AIP, now termed type 2 AIP, consist of neutrophilic infiltration of the pancreatic duct epithelium: the granulocytic epithelial lesion (GEL). IgG4-positive plasma cells are generally absent from the tissue lesions of type 2 AIP, and serum IgG4 concentrations are usually normal.
In our experience in considering all cases of AIP, among patients with normal serum IgG4 concentrations, the percentage of women is high and symptoms of acute pancreatitis such as abdominal pain are common. Segmental as opposed to diffuse pancreatic swelling is common in this AIP subtype, but extrapancreatic lesions were few. In particular, salivary and lacrimal gland enlargement and dysfunction tend not to occur in this AIP subtype, and IgG4-positive plasma cells are not found on tissue specimens.
Patients with normal serum IgG4 concentrations should be classified as type 1 (IgG4-related AIP) if histopathologic examination and immunohistochemical studies of pancreatic specimens demonstrate the typical hematoxylin and eosin features of IgG4-related disease as well as increased numbers of IgG4-positive plasma cells. Type 2 AIP, which is usually associated with normal serum IgG4 concentrations and is linked to pathological findings that contrast sharply with those of type 1 (IgG4-related) AIP, is not a form of IgG4-related disease and should be regarded as a separate disease entity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introductory Remarks
Autoimmune pancreatitis (AIP), which was introduced from Japan to the rest of the world, is a distinctive type of pancreatitis. In 1995, a case was reported that showed pancreatic duct narrowing, pancreatic swelling, hypergammaglobulinemia, and positive autoantibodies, as well as marked responsiveness to steroids [1]. It subsequently became clear that in the condition now known as type 1 AIP, an elevated serum IgG4 concentration is observed in a high proportion of cases [2].
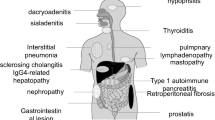
Extrapancreatic lesions are common in patients with type 1 AIP and may affect a wide range of organs with pathological features that are strikingly similar to those of the pancreas and tend to respond well to steroids. These pathological features include a marked lymphoplasmacytic infiltrate with an increased number of IgG4-positive plasma cells and a distinctive form of fibrosis that often assumes a storiform pattern. These multi-organ features are now recognized to comprise one systemic disease with the capability of affecting multiple organs in either a simultaneous fashion or, more commonly, in a metachronous manner. Thus, lymphoplasmacytic sclerosing pancreatitis (LPSP), as type 1 AIP is commonly known in the medical literature, is now regarded as the pancreatic lesion of IgG4-related disease (IgG4-RD) [3–5].
Broader experience with AIP led to the recognition of a form of this condition that is associated with normal IgG4 concentrations in the blood. In this chapter, we outline the clinical features of such cases, focusing on our own experience.
2 Autoimmune Pancreatitis: Types 1 and 2
Before the clear emergence of a second type of AIP and recognition of the need to designate the two currently recognized forms of AIP as types 1 and 2, the most common form of AIP in Japan came to be known as LPSP [6]. LPSP is characterized by extensive cellular infiltrates consisting of IgG4-positive plasma cells, T lymphocytes, fibrosis, and obliterative phlebitis. Neutrophils are typically absent in LPSP, and the inflammatory cell infiltrate tends to spare the pancreatic duct epithelium. The typical patient is an elderly man who presents with painless jaundice, i.e., minimal to no signs of acute pancreatitis. Other sclerosing extrapancreatic lesions are often present, such as in the biliary tree (IgG4-related sclerosing cholangitis) or salivary glands (IgG4-related sialadenitis, with submandibular or parotid gland involvement). In contrast to type 2 AIP, inflammatory bowel disease is almost never seen in LPSP [4, 5].
A European histopathological study detected neutrophil infiltration of the pancreatic duct epithelium (granulocytic epithelial lesion: GEL) in 24 of 53 AIP cases [7]. In these cases the mean age at onset was young compared to that of LPSP patients, the sexes were affected in equal proportions, and inflammatory bowel disease was frequently present. The patients in that European series whose pancreatic biopsies did not show GEL had clinical and pathological features similar to the type of AIP described consistently in Japan. In a recent international study, AIP patients in Italy showed similar features with regard to age at onset—approximately 20 years younger than that in Japan and no tendency to affect one sex more frequently than the other [8]. In addition, symptoms of acute pancreatitis and inflammatory bowel disease were reported in 32 % and 30 %, respectively, of the Italian patients. The contrasting experiences between Japan and Europe indicate clearly that there are at least two different conditions grouped under the common heading of “AIP.”
Histopathological studies from the Mayo Clinic of resected cases of idiopathic chronic pancreatitis with heavy inflammatory cell infiltration revealed cases with copious neutrophil infiltration, particularly in the pancreatic lobule [9]. These cases, readily separated from the pathology of LPSP, were termed “idiopathic duct-centric chronic pancreatitis” (IDCP). In IDCP, neutrophil infiltration within the pancreatic duct epithelium is a hallmark of the condition but in contrast to LPSP (type 1 AIP), but there is little inflammatory cell infiltration in the fibrotic layer, obliterative phlebitis is rare, and IgG4-positive plasma cell infiltrates are considerably less prominent than in LPSP. In these cases a clinical picture almost identical to that of the GEL-positive cases is present [9]. Some cases of juvenile-onset AIP have demonstrated similar clinical and pathological pictures [10].
Substantial clarity has been brought to the field in recent years [11, 12]. LPSP and IDCP are now recognized as type 1 and type 2 AIP, respectively [11]. In the recently proposed international consensus diagnostic criteria for AIP [13], the diagnostic criteria for types 1 and 2 AIP are listed separately. The criteria emphasize that the two types of AIP share the same pancreatic imaging findings and responsiveness to steroids, but elevated serum IgG4 values and the presence of IgG4-related extrapancreatic lesions are limited to type 1, and inflammatory bowel disease is limited to type 2. Moreover, marked periductal lymphocyte and IgG4-positive plasma cell infiltration (>10/HPF), obliterative phlebitis, and storiform fibrosis are noted in type 1 and neutrophil infiltration of the pancreatic duct wall in type 2.
3 Clinicopathologic Features of AIP with Normal Serum IgG4 Concentrations in Our Own Cases
Fifty-eight AIP patients diagnosed in our department were divided into two groups according to their serum IgG4 concentrations: a normal serum IgG4 AIP group (≦135 mg/dL; n = 13) and an elevated serum IgG4 positive group positive group (>135 mg/dL; n = 45). We then compared their clinicopathologic features [14].
3.1 Age and Sex Distribution
The proportion of women tended to be higher among the group of patients with normal serum IgG4 concentrations, although this comparison fell just short of statistical significance. The male/female ratio in the normal serum IgG4 group was 7/6, compared with 36/9 among those patients with elevated serum IgG4 concentrations (p = 0.07). There was no difference in the mean age at diagnosis between the two groups: 61.5 years (normal serum IgG4) versus 63.7 years (elevated serum IgG4).
3.2 Presenting Symptoms
Obstructive jaundice was substantially less common among the patients with normal serum IgG4 concentrations (31 % versus 78 %, p < 0.01), but abdominal symptoms suggestive of acute pancreatitis were markedly more common (38 % versus 7 %, p = 0.01).
3.3 Pancreatic Swelling
Segmental pancreatic swelling was noted more frequently in the group of patients with normal serum IgG4 concentrations (46 % versus 13 %, p < 0.05).
3.4 Extrapancreatic Lesions
Extrapancreatic lesions such as sclerosing cholangitis, sclerosing cholecystitis, sclerosing sialadenitis, and retroperitoneal fibrosis were more frequently found among the group of patients whose serum IgG4 concentration was elevated (51 % versus 8 %, p < 0.01), but acute pancreatitis was more common in the group with normal serum IgG4 values (23 % versus 4 %, p < 0.05). Ulcerative colitis was seen in one case each in both groups.
3.5 Salivary Gland and Lacrimal Gland Function
Salivary gland function determined by biochemical analysis of saliva and lacrimal gland function by Schirmer’s test. Salivary Na+ and β2-microglobulin concentrations were increased significantly in both groups as compared to the control, but they were significantly higher in the group with elevated serum IgG4 concentrations (Na+: a mean 32.6 mEq/L vs. 21.7 mEq/L, p < 0.05, and β2-microglobulin: 2.7 mg/dL vs. 1.5 mg/dL, p < 0.05).
Data of Schirmer’s test were significantly lower in the group with elevated serum IgG4 concentrations (a mean 5.4 mm vs. 11.9 mm, p < 0.05).
3.6 Responsiveness to Steroids
Both groups were initially responsive to steroids. No patients with normal serum IgG4 concentrations relapsed during a mean 57.3 (8–140) months, while five patients with elevated serum IgG4 concentrations relapsed during 50.2 (6–173) months.
3.7 Histopathological Findings of the Pancreas
The five resected and the five biopsied pancreatic specimens of patients with elevated serum IgG4 concentrations revealed LPSP in ten cases, and EUS-FNA of three patients could not confirm the diagnosis. Two resected, one biopsied, and 1 EUS-FNA pancreatic specimen of patients with normal serum IgG4 concentrations revealed LPSP, two fine needle aspirates yielded tissue that was insufficient for diagnosis, and two other biopsies showed B cell infiltrates and fibrosis. One patient whose fine needle aspirate was non-diagnostic had a high pretest likelihood of IDCP (type 2 AIP), as he presented with acute pancreatitis and had a history of inflammatory bowel disease.
In the specimens from patients with elevated serum IgG4 concentrations, dense lymphocyte and IgG4-positive plasma cell infiltrates were noted. The lymphoplasmacytic infiltrates were particularly concentrated in the pancreatic interlobular interstitium and around the pancreatic duct (Fig. 7.1a, b). In contrast, the specimens from the patients with normal IgG4 concentrations were characterized by comparatively little inflammatory cell infiltration (Fig. 7.2a, b).
Histopathological features of the pancreas in autoimmune pancreatitis cases with elevated serum IgG4 values. (a): Around the pancreatic duct marked inflammatory cell infiltration and fibrosis are seen (H&E staining ×100). (b): Numerous IgG4-positive plasma cell infiltrates are found around the pancreatic duct (IgG4 staining ×40)
Histopathological features of the pancreas in autoimmune pancreatitis cases with low serum IgG4 values. (a): Inflammatory cell infiltration and fibrosis are seen around the pancreatic duct, but the degree of cell infiltration is less than that seen in Fig. 7.1 (H&E staining ×100). (b): IgG4-positive plasma cell infiltration is also markedly less conspicuous as compared to that in Fig. 7.1 (IgG4 staining ×40)
3.8 Number of IgG4-Positive Plasma Cells in the Biopsied Gastric Tissues
The IgG4-positive plasma cells infiltrating gastric mucosal tissues obtained by biopsy numbered a mean 7.0 (0–20)/HPF in the positive group (n = 17) as compared to only 1.4 (0–3)/HPF in the negative group (n = 7, p < 0.01).
3.9 Subsets of AIP Among Patients with Normal Serum IgG4 Levels
The AIP patients with normal serum IgG4 concentrations could be divided into three groups: (a) type 1 AIP; (b) fibrosis associated with dense B lymphocyte infiltration; and (c) an undiagnosable category. The specimens from patients with type 1 AIP but normal serum IgG4 concentrations had relatively little IgG4-positive plasma cell infiltration in the pancreas, and in some cases lesions were limited to the pancreas. The histopathologically undiagnosable cases were thought to possibly include some type 2 cases. It is possible that cases exist with a histological picture that differs from either type 1 or type 2 AIP.
4 Concluding Remarks
Patients with AIP and normal IgG4 concentrations in the serum appear to have three possible diagnoses: (a) type 1 AIP that is characterized histopathologically be relatively sparse IgG4-positive plasma cell infiltration with fibrosis; (b) type 2 AIP, a condition that is not part of the IgG4-RD spectrum; and (c) other pathology not classifiable at present as either type 1 or type 2 AIP, suggesting that the spectrum of AIP may extend beyond these two currently recognized entities.
References
Yoshida K, Toki F, Takeuchi T, et al. Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci. 1997;40:1561–8.
Okazaki K, Kawa S, Kamisawa T, et al. Clinical diagnostic criteria of autoimmune pancreatitis: revised proposal. J Gastroenterol. 2006;41:626–31.
Kamisawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38:982–4.
Kamisawa T, Okamoto A. Autoimmune pancreatitis. Proposal of IgG4-related sclerosing disease. J Gastroenterol. 2006;41:613–25.
Kamisawa T, Takuma K, Egawa N, et al. Autoimmune pancreatitis and IgG4-related sclerosing disease. Nat Rev Gastroenterol Hepatol. 2010;7:401–9.
Kawaguchi K, Koike M, Tsuruta K, et al. Lymphoplasmacytic sclerosing pancreatitis with cholangitis: a variant of primary sclerosing cholangitis extensively involving pancreas. Hum Pathol. 1991;22:387–95.
Zamboni G, Luttges J, Capelli P, et al. Histopathological features of diagnostic and clinical relevance in autoimmune pancreatitis: a study on 53 resection specimens and 9 biopsy specimens. Virchow Arch. 2004;445:552–63.
Kamisawa T, Chari ST, Giday SA, et al. Clinical profile of autoimmune pancreatitis and its histological subtypes. An international multicenter study. Pancreas. 2011;40:809–14.
Notohara K, Burgart LJ, Yadav D, Chari S, Smyrk TC. Idiopathic chronic pancreatitis with periductal lymphoplasmacytic infiltration. Clinicopathologic features of 35 cases. Am J Surg Pathol. 2004;27:1119–27.
Kamisawa T, Wakabayashi T, Sawabu N. Autoimmune pancreatitis in young patients. J Clin Gastroenterol. 2006;40:847–50.
Sah RP, Chari ST, Pannala R, et al. Differences in clinical profile and relapse rate of type 1 vs type 2 autoimmune pancreatitis. Gastroenterology. 2010;139:140–8.
Kamisawa T, Notohara K, Shimosegawa T. Two clinicopathologic subtypes of autoimmune pancreatitis: LPSP and IDCP. Gastroenterology. 2010;139:22–5.
Shimosegawa T, Chari ST, Frulloni L, et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas. 2011;40: 352–8.
Kamisawa T, Takuma K, Tabata T, et al. Serum IgG4-negative autoimmune pancreatitis. J Gastroenterol. 2011;46:108–16.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Japan
About this chapter
Cite this chapter
Hara, S., Kamisawa, T., Tabata, T., Kuruma, S., Chiba, K., Koizumi, S. (2014). Autoimmune Pancreatitis with Normal Serum IgG4 Concentrations: What Is the Correct Classification for Such Patients?. In: Umehara, H., Okazaki, K., Stone, J., Kawa, S., Kawano, M. (eds) IgG4-Related Disease. Springer, Tokyo. https://doi.org/10.1007/978-4-431-54228-5_7
Download citation
DOI: https://doi.org/10.1007/978-4-431-54228-5_7
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-54227-8
Online ISBN: 978-4-431-54228-5
eBook Packages: MedicineMedicine (R0)