Abstract
The increasing number of suicidal victims all over the world is a major concern. There are three neurobiological systems involved in the pathophysiology of suicidal behavior: dysfunction of the serotonergic system, hyperactivity of the noradrenergic system, and increased activity of the hypothalamic–pituitary–adrenal (HPA) axis appear to be involved. Increasing evidence points to an overlap between neurobiological and cognitive psychological approaches to understanding suicidal behavior. The authors reviewed the molecular genetics of suicidal behavior. A better understanding of the neurobiology of suicide can help detect at-risk populations and help develop better treatment interventions. Because suicide continues to be a major public health problem, further studies are necessary, including research on the effects of combined medical and psychosocial approaches.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The number of suicide victims in Japan in the recent 11 years (1998–2008) is more than 30,000 a year, and in the year 2009 this number is 32,753. The suicide rate (number of suicide victims per 100,000 population) in Japan is about 25, and this number is the fourth highest in the world. Suicide is one of the most important public concerns and a major cause of death among young people throughout the world. No remarkable reduction in the number of suicide victims has yet been achieved, although there has been recent progress in the treatment and management of psychiatric disorders. During the past two decades, there has been a considerable accumulation of findings in the neurobiology of suicide [1].
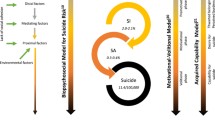
Although many factors such as biological, psychological, and social factors are involved in suicide behavior, the presence of mental disorder is thought to play an important role in suicide [2]. More than 90% of suicide victims or suicide attempters are diagnosed having mental disorders such as depression, schizophrenia, or alcohol dependence (Fig. 1). However, the underlying mental disorders are diverse, and the severity of the mental disorders does not necessarily correlate with increased risk of suicide.
Mental disorders in suicide. In completed suicide, about 30% of all suicide victims occur in relation to mood disorders, and the rest are related to various other psychiatric disorders, including substance-related disorders, such as substance abuse and alcoholism, schizophrenia and personality disorders. Source: World Health Organization: preventing suicide; a resource for general physicians. WHO/WNH/MBD/00.1, World Health Organization, Geneva, 2000
Even in the psychiatric groups at the highest risk, most patients never attempt suicide. These findings indicate the importance of a diathesis or predisposition to suicidal behavior that is independent of the main psychiatric disorder.
Molecular Genetics of Suicide
Numerous studies on neurochemical abnormalities have been done; the results obtained from those studies are summarized in Table 1. Recently, studies on the biological aspect of suicide have been shifting from neurochemical to molecular genetic approaches. Genetic studies on suicidal behavior have suggested that the heritability of such behavior is independent of psychiatric diagnosis. Adoption studies have shown a higher rate of suicide in the biological parents of adoptees who commit suicide compared with biological relatives of control adoptees, even after controlling for rates of psychosis and mood disorders (Table 2). Concordance rates for suicide and suicide attempts are higher in monozygotic than dizygotic twins, and the heritability of suicidal behavior was estimated to be approximately 55% based on twin studies in people with serious suicide attempts [3]. People who commit suicide or make suicide attempts are those with a higher rate of familial suicidal acts. These findings suggest the presence of hereditary and biological factors that determine the threshold to commit suicide and which are independent of specific psychiatric disorders. Thus, genetic factors in suicide have been a recent focus, and recognition has been growing that suicide and suicidal behaviors are highly familial and that genetics contributes to suicide and suicidal behaviors (Table 3). In addition, completed suicides are thought to be more homogeneous than suicide attempters in terms of inheritance of suicidal behavior [4].
On the basis of these findings, we have conducted genetic association analysis of completed suicides to explore the susceptible genetic variants for suicide. Up to the present date, we have found a number of associations for genetic variations with completed suicide. We have been focusing attention on several neurobiological factors including the serotonergic system, noradrenergic and hypothalamic–pituitary–adrenal (HPA) system, and the sites of action of mood stabilizers, especially the antisuicidal effects of lithium.
In addition, for the purpose of identifying new candidate systems and gaining new insight into biological mechanisms mediating suicide, we have conducted gene expression analysis in the postmortem brains of suicide victims [5–11, 13–18]. Recently, molecular genetic studies have been performed intensively to confirm disturbance of serotonergic neurotransmission in suicide. We have performed association studies of polymorphisms and mutations of genes encoding synthesizing and metabolic enzymes, receptors, and transporters involved in serotonergic neurotransmission in suicide [5–11]. However, in our studies, we have not observed any significant association between these polymorphisms and suicide (Table 4).
In addition, many other studies performed to date have not provided strong evidence supporting such an association. The relative risk was small even when association was detected by meta-analysis (Table 5).
It has been suggested that noradrenergic system abnormalities are involved in suicide [13, 14]. Recently, we have found that one promoter genetic variant (C-1291G SNP) of the a2A-adrenergic receptor (ADRA2A) gene was significantly associated with suicide in Japanese females (P = 0.043 and 0.013 for genotypic and allelic comparisons, respectively). One of the common haplotypes, CC of this polymorphism and another variant of the ADRA2A gene (rs3750625C/A), was also associated with suicide in females (P = 0.015). These associations were also significant in the female violent suicide victims (P = 0.009 and 0.009 for allelic and CC haplotypic comparisons, respectively; Table 6) [13]. In contrast, neither of these two SNPs showed any association with violent and/or nonviolent suicide in males. The noradrenergic system regulates activation of the HPA axis, dysregulation of which might be involved in the pathogenesis of suicide. Therefore, this promoter variant in the ADRA2A gene might be involved in the pathogenesis of suicide as a result of the noradrenergic dysfunction that destabilizes the HPA system.
The catechol-O-methyltransferase (COMT) gene, the catecholamine-degrading enzyme, exhibits a functional common polymorphism (158Met/Val), and this variant is considered to affect the HPA system. Individuals who are homozygous for the low-activity form of COMT (A/A, Met/Met) would exhibit greater HPA-axis activation than those who are either homozygous or heterozygous for the high-activity form of the enzyme. We found that the genotype distribution of the COMT 158Val/Met polymorphism was significantly different between male suicide completers and male controls (P = 0.036), whereas the frequency of the Val/Val genotype, a high-activity form of the enzyme, was significantly less in male suicide completers than in male controls [odds ratio (OR) = 0.52; 95% confidence interval (CI) = 0.31–0.89; P = 0.016] [14]. These findings were not the case in females. We found that this polymorphism was associated with suicide in males, and that high COMT activity could exhibit a protective effect for suicide in males (Table 7) [15].
Table 8 shows the distributions of the four polymorphisms in the μ-opioid receptor (OPRM1) gene. The OPRM1 gene is implicated in stress responses through the HPA system [16]. The substitution of A118G polymorphism in the OPRM1 gene, which results in an Asn to Asp change at amino acid 40, is suggested to influence the HPA axis response in an inhibitory manner and, possibly, decrease the HPA axis response to a social stressor. Therefore, the suicide-protective G allele would be expected to inhibit the HPA axis responses. We genotyped four single-nucleotide polymorphisms, including a common A118G SNP. The genotypic and allelic distributions of the A118G SNP were significantly different between the completed suicide and control groups (P = 0.014 and 0.039, respectively; Table 9). Moreover, the dominant model of genotype (AA vs. AG + GG) analysis showed an enhanced association with suicide (P = 0.0041, OR = 0.575). This finding means that individuals with one or two copies of the G allele of the A118G SNP of the OPRM1 gene are less vulnerable to suicide. These results raise the possibility that the A118G SNP of the OPRM1 gene is associated with suicide.
We have conducted another association study examining the functional gene polymorphisms of angiotensin-converting enzyme (insertion/deletion), prostaglandin E receptor subtype EP1 [17], and neuronal nitric oxide synthase (nNOS or NOSI), which affect the HPA system, and demonstrated significant associations with suicide. These findings have suggested that the disturbance of the HPA system plays an important role in suicide (Table 9).
Recently, we found an association between regulators of G-protein signaling (RGS) 2 gene polymorphisms and suicide and observed increased RGS2 immunoreactivity in the postmortem brains of suicide victims (Tables 10, and 11) [18]. RGSs are a family of proteins that negatively regulate intracellular signaling of G protein-coupled receptors (GPCRs), such as the serotonin receptor. RGS2 is thought to play an important role in anxiety and/or aggressive behavior.
To explore the involvement of the RGS2 gene in vulnerability to suicide, we screened Japanese suicide victims for sequence variations in the RGS2 gene and carried out an association study of RGS2 gene polymorphisms with suicide victims. In the eight identified polymorphisms that were identified by mutation screening, we genotyped four common single-nucleotide polymorphisms in the RGS2 gene and found significant differences in the distribution of the SNP3 genotypes and alleles of the SNP2 and the SNP3 between completed suicides and the controls. The distribution of the haplotype was also significantly different between the two groups (Table 11; global < 0.0001). Furthermore, RGS2 immunoreactivity significantly increased in the amygdala and the prefrontal cortex [Brodmann area 9] of the postmortem brain of the suicide subjects (Fig. 2). These findings suggest that RGS2 is genetically involved in the biological susceptibility to suicide in the Japanese population.
Increased RGS2 immunoreactivity in suicides. RGS2 immunoreactivity significantly increased in the amygdala and the prefrontal cortex [Brodmann area 9] of the postmortem brain of the suicide subjects. These findings suggest that RGS2 is genetically involved in the biological susceptibility to suicide in the Japanese population. Cui H, Nishiguchi N, Ivleva E et al. (2008) [18]
Conclusion
Taking into consideration the presence of mental disorders as underlying suicide, it is natural that the recent trend tends to link early screening of depression to suicide prevention as a medical approach. It is inadvisable to interpret suicide solely as a symptom or outcome of disease. Expansion of the disease concept and subsequent additional medical intervention may be inappropriate. However, the biological and medical understanding of suicide, that is, interpretation as a condition that allows or requires medical intervention, may encourage people at high risk for suicide to visit psychological counselors and psychiatrists. In addition, although the processes may be indirect or secondary, medical and biological approaches could have considerable influence on individual views and social consciousness of life and death, which may contribute to the prevention of suicide.
References
Mann JJ (2003) Neurobiology of suicidal behavior. Nat Rev Neurosci 4:819–828
Brent DA, Mann JJ (2005) Family genetic studies, suicide, and suicidal behavior. Am J Med Genet C Semin Med Genet 133:13–24
Roy A, Segal NL (2001) Suicidal behavior in twins: a replication. J Affect Disord 66:71–74
Bondy B, Buettner A, Zill P (2006) Genetics of suicide. Mol Psychiatry 11:336–351
Ono H, Shirakawa O, Nishiguchi N et al (2000) Tryptophan hydroxylase gene polymorphisms are not associated with suicide. Am J Med Genet 96:861–863
Ono H, Shirakawa O, Nishiguchi N et al (2001) Serotonin 2A receptor gene polymorphism is not associated with completed suicide. J Psychiatr Res 35:173–176
Nishiguchi N, Shirakawa O, Ono H et al (2001) No evidence of an association between 5HT1B receptor gene polymorphism and suicide victims in a Japanese population. Am J Med Genet 105:343–345
Ono H, Shirakawa O, Kitamura N et al (2002) Tryptophan hydroxylase immunoreactivity is altered by the genetic variation in postmortem brain samples of both suicide victims and controls. Mol Psychiatry 7:1127–1132
Nishiguchi N, Shirakawa O, Ono H et al (2002) Lack of an association between 5-HT1A receptor gene structural polymorphisms and suicide victims. Am J Med Genet 114:423–425
Ono H, Shirakawa O, Nishiguchi N et al (2002) No evidence of an association between a functional monoamine oxidase a gene polymorphism and completed suicides. Am J Med Genet 114:340–342
Okamura K, Shirakawa O, Nishiguchi N et al (2005) Lack of an association between 5-HT6 receptor gene polymorphisms and suicide victims. Psychiatry Clin Neurosci 59:345–349
Anguelova M, Benkelfat C, Turecki G (2003) A systematic review of association studies investigating genes coding for serotonin receptors and the serotonin transporter: II. Suicidal behavior. Mol Psychiatry 8:646–653
Hattori H, Shirakawa O, Nishiguchi N et al (2006) No evidence of an association between tyrosine hydroxylase gene polymorphisms and suicide victims. Kobe J Med Sci 52:195–200
Fukutake M, Hishimoto A, Nishiguchi N et al (2008) Association of α2A-aderenergic receptor gene polymorphism with susceptibility to suicide in Japanese females. Prog Neuropsychopharmacol Biol Psychiatry 32:1428–1433
Ono H, Shirakawa O, Nushida H et al (2004) Association between catechol-O-methyltransferase functional polymorphism and male suicide completers. Neuropsychopharmacology 29:1374–1377
Hishimoto A, Cui H, Mouri K et al (2008) A functional polymorphism of the μ-opioid receptor gene is associated with completed suicides. J Neural Transm 115:531–536
Hishimoto A, Shirakawa O, Nishiguchi N et al (2006) Association between a functional polymorphism in the renin-angiotensin system and completed suicide. J Neural Transm 113:1915–1920
Cui H, Nishiguchi N, Ivleva E et al (2008) Association of RGS2 gene polymorphisms with suicide and increased RGS2 immunoreactivity in the postmortem brain of suicide victims. Neuropsychopharmacology 33:1537–1544
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer
About this chapter
Cite this chapter
Maeda, K., Shirakawa, O., Nishiguchi, N., Fukutake, M. (2010). The Molecular Genetics of Suicide. In: Miyoshi, K., Morimura, Y., Maeda, K. (eds) Neuropsychiatric Disorders. Springer, Tokyo. https://doi.org/10.1007/978-4-431-53871-4_23
Download citation
DOI: https://doi.org/10.1007/978-4-431-53871-4_23
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-53870-7
Online ISBN: 978-4-431-53871-4
eBook Packages: MedicineMedicine (R0)