Abstract
Diffuse neurofibrillary tangles with calcification (DNTC) is a primary and sporadic presenile dementia that is characterized by temporal and/or frontal atrophy with diffuse neurofibrillary tangles (NFTs) and Fahr-type calcification without senile plaques (SPs).
We reviewed clinical symptoms in 21 autopsy-proven DNTC cases in Japan. It is characterized by slowly progressive cortical dementia mimicking Alzheimer’s disease (AD) because of the appearance of memory disturbance and disorientation in the early stages, or simulating Pick’s disease as a result of the presence of personality changes in the early to middle clinical stages, followed by various psychiatric and neurological symptoms such as Parkinson’s symptoms, aphasia, and apraxia.
In terms of neuropathology, DNTC is characterized by the appearance of massive NFTs in the cerebral cortex and in Meynert’s nucleus and the locus ceruleus/raphe nuclei as well. These sites are similar to those with AD. Differing from AD, SPs were absent, or only a small number were detected. Ultrastructural and immunohistochemical study revealed that NFTs with DNTC were morphologically and biochemically the same with those in AD. Fahr-type calcification is also one of the most characteristic findings; it was found in the basal ganglia and the cerebellum. We conducted elementary analysis of the calcified sites. In addition to calcium and iron, a higher level of lead was detected in comparison with control groups. The etiology should be further investigated.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Diffuse neurofibrillary tangles with calcification (DNTC) is a primary and sporadic presenile dementia. Ando et al. initially reported a patient with this disorder at an annual meeting of the Japanese Society of Neuropathology in 1964 [1]. Because atrophy of the temporal lobe was marked, how to differentiate this disorder from Pick’s disease was discussed at that time. Thereafter, these cases were reported in the literature as cases of atypical Alzheimer’s disease (AD), Pick’s disease, or combined Alzheimer/Pick disease. After Shibayama et al. [2] and Kosaka [3] published their manuscripts, interest in DNTC was particularly emphasized in Japan. More than 20 autopsy cases have been reported. Pathologically, DNTC is characterized by localized temporal and/or frontal lobe atrophy, numerous neurofibrillary tangles (NFTs) without senile plaques (SPs), and calcification in the basal ganglia and dentate nucleus of the cerebellum that exceeded the normal physiological level. The term DNTC, which was proposed by Kosaka, has been used, because it represents well these pathological characteristics.
Case Presentation
Case 1. A 75-year-old woman. Her medical history included hypertension. There was no family history of dementia. At the age of 58 years, memory disturbance was noted. At the age of 62 years, she was admitted to the hospital because she was violent toward her husband. In the ward, her attitude was pleasant, but euphoric. She showed a tendency to repeat the same questions. Disorientation regarding places and persons, perseveration, and confabulation were noted. Neither apraxia nor agnosia was observed. There was no neurological sign other than severe dementia. However, hyperreflexia, tremor, and rigidity were noted at the age of 65 years. After the age of 66 years, she was usually cheerful, but became irritable frequently, and she got angry when displeased. Wandering was marked. Verbal output gradually decreased. At 72 years, she became bedridden. Brain computed tomography (CT) at the age of 74 showed cerebral atrophy of temporal and frontal lobes and calcification in the basal ganglia and cerebellum (Fig. 1). At the age of 75, she died of pneumonia. The clinical course was similar to that of AD. However, intracerebral calcification suggested DNTC. Autopsy was performed. The brain weighed 850 g. On the outer surface, there was an enlargement of the bilateral Sylvian fissures, and the temporal lobe showed marked atrophy. The right side of the temporal lobe showed more marked atrophy. The atrophic sites were brown and hard. Atrophy of the frontal, parietal, and occipital gyri was less marked. There were no marked changes in the cerebellum or brainstem. The basilar arteries showed moderate arteriosclerotic changes. Microscopically, neuronal loss and gliosis in the atrophic foci of the cortices were observed in the temporal pole in particular. The amygdala, hippocampus, and temporal lobe showed marked gliosis, and the white matter of the frontal and occipital lobed had slight to moderate gliosis. Numerous NFTs were observed in the cerebral cortex involving the frontal to occipital lobes. NFTs contained both 3 repeat and 4 repeat tau. A few SPs were detected in the temporal cortex; however, they were absent in other areas. The caudate nucleus showed atrophy, and there were only a small number of NFTs and neuropil threads. There were a few NFTs in the neurons of the substantia nigra and locus ceruleus. Calcification was present in the pallidum, putamen, granular layer, and the dentate nucleus of the cerebellum.
Case 2. A 48-year-old woman. There was no family history of dementia. At the age of 45, she became unable to do housework. Memory disturbance and disorientation gradually progressed, requiring caregiving for meals and excretion. Neurologically, there were no abnormal findings other than dementia. The blood pressure was normal. Personal contacts were maintained. Euphoria was noted. Neither aggression nor negativism was observed. Wandering and yelling made keeping her at home difficult, and the patient was admitted to a psychiatric hospital. Dementia progressed, and she died of pneumonia, with a dementia follow-up of 3 years. Autopsy was performed. The brain weighed 1,000 g. The frontal lobes showed atrophy bilaterally. On the cut surface, temporal lobe atrophy was noted. In the temporal lobe, the myelin sheath was markedly lightened, and gliosis was observed at the same site. In the frontal lobe, similar changes were also noted, although the grade was lower. Numerous NFTs were observed in the amygdala, hippocampus and inferior temporal gyrus. Calcification was observed in the vascular wall and parenchyma of the basal ganglia and granular layer of the cerebellar vermian cortex. In the substantia nigra, a small number of NFTs and Lewy bodies were present. A SP-like structure was observed, but amyloid staining showed no amyloid deposition in this structure.
Epidemiology of DNTC
Clinical and pathological reports of more than 30 patients with DNTC have been reported in Japan. However, in Western countries, not much interest in this disorder has been shown. Calcification was observed in the basal ganglia, dentate nucleus of the cerebellum, and cerebral white matter in severe cases (Fahr type). Brain CT scanning facilitates detection of atrophy and calcification at these sites. In our survey using the criteria proposed by Kosaka [4] DNTC was suspected in 4 of 3,053 patients (male:female = 1:2) with dementia residing in Okayama Prefecture. All these cases were female. In one case, autopsy led to a definitive diagnosis of DNTC. The incidence of DNTC was 0.13% in patients with dementia in Okayama. However, it may be lower in the general population. In Japan, several patients have been reported in Tokyo, Nagoya, Okayama, and Kochi, suggesting regional differences. In 21 autopsied patients, the male-to-female ratio was 1:3. Familial DNTC has not been reported. The mean age at onset was 53.1 years. A presenile onset (40 69 years of age) was frequent. The mean time of illness duration was 10.5 years (range, 3 24 years). In patients without complications, the clinical course may be prolonged. Generally speaking, the longer the duration, the lower the brain weight. The brain weight had decreased to approximately 800 g in patients with a prolonged course. In some patients, however, cerebral atrophy was evident even in the early stage.
Characteristics of Clinical Symptoms
We reviewed clinical symptoms in 21 patients whose pathological findings led to a definitive diagnosis of DNTC in Japan (Fig. 2).
The most common primary symptoms were memory disturbance and disorientation. In the early stage, they were observed in 80% of the 21 patients. With a slow course, personal contacts were maintained in the initial phase, and neurological symptoms were absent. Therefore, most patients were diagnosed with AD. However, personality changes such as irritability, aggression, euphoria, and disinhibition were noted in the initial phase, suggesting Pick’s disease. Some patients showed a loss of spontaneity, depression, and apathy. In the middle phase, memory disturbance was advanced. During the course, schizophrenia-like symptoms such as auditory hallucination, delusion of persecution, and hypochondriac delusion were observed in some patients. However, no patient showed “delusion of being robbed by a thief,” which is very common in patients with AD. Early DNTC did not produce any neurological symptoms, such as Parkinson’s symptoms, or focal symptoms, such as apraxia and agnosia. However, these symptoms appeared in approximately 30% to 50% of the patients during the course [5]. When the symptoms were advanced, dysphagia and primitive reflexes were noted, leading to an apallic state. Disease progression varied; memory disturbances and disorientation derived from hippocampal lesions were seen in the early stage, and personality changes derived from frontal/temporal lobe lesions were complicated by extrapyramidal symptoms and cerebrovascular diseases. In 6 of the 21 patients, a diagnosis of schizophrenia was made based on psychiatric symptoms such as hallucination and delusion during the course, and, later, cognitive impairment was observed. In the future, the course of DNTC should be investigated with a large number of cases.
Pathological Characteristics
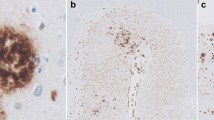
NFTs
DNTC is characterized by appearance of massive NFTs. A large number of NFTs were observed in the hippocampus and parahippocampal gyrus. They were widely distributed in the cerebral isocortex. They were also found in Meynert’s nucleus and the locus ceruleus/raphe nuclei of the brainstem. These sites were similar to those frequently observed in patients with AD. On the other hand, there were no NFTs in the basal ganglia or cerebellum. Differing from AD, SPs were absent, or only a small number were detected.
Characteristics of Degenerative Tau Protein
There are six isoforms of tau protein. Among these, tau protein involving exon-10, which exists in the microtubule-binding site, is termed “4-repeat tau protein,” and exon-10-free tau protein is called “3-repeat tau protein.” In patients with AD, all six isoforms are detected. In those with progressive supranuclear palsy or cortical basal ganglia degeneration, 4-repeat tau protein is found. In those with Pick body disease, 3-repeat tau protein is present. In patients with DNTC, 60-, 64-, and 68-kDa major and 72-kDa minor bands were recognized in the presence of various anti-tau antibodies. On Western blotting of sarkosyl-insoluble tau protein after dephosphorylation, six isoforms of tau protein were observed [6], indicating that the biochemical features of degenerative tau protein in patients with DNTC were similar to those in AD.
Electron Microscopy Findings
Electron microscopy examination was done with negative staining of sarkosyl-insoluble tau protein. A large number of paired helical filaments (PHFs) measuring 8–20 nm in diameter, with a cycle of approximately 80 nm, and a small number of straight tubules were observed [6]. These results suggest that degenerative tau protein in patients with DNTC is morphologically and biochemically identical to that in AD patients, and that PHFs are formed in the absence of β-protein [6].
Calcification
DNTC is characterized by the presence of calcification in the pallidum, putamen, and dentate nucleus of the cerebellum. Calcification was found in the capillary walls and parenchyma; this refers to false calcification with protein deposition. Calcification is also observed in the cerebral cortex, white matter, and cerebellar cortex in some cases. Neither loss of cells in the basal ganglia with calcification nor functional disturbance is noted [7]. We conducted elementary analysis of the calcified sites. In addition to calcium and iron, a higher level of lead was detected in comparison with control groups. The etiology should be further investigated [8, 9].
Cerebrovascular Lesions
The cases with DNTC have often complications of cerebrovascular disorders. Several studies have indicated the coexistence of cerebrovascular arteriolosclerosis, hypertension, Binswanger’s disease-like white matter lesions, and multiple cerebral infarctions [10].
Lewy Body Pathology
We reported that α-synuclein was accumulated in various sites in seven of eight patients with DNTC [11]. α-Synuclein was accumulated in the amygdala, hippocampus, substantia nigra, and temporal/frontal cortex. This pattern was similar to the distribution of Lewy body disease (DLB). Among other types of tauopathy, Lewy body formation has also been reported. However, this finding is the most marked in patients with DNTC [11, 12]. The accumulation of Lewy bodies/neurites may affect nerve cell function. However, it is unclear whether this finding reflected clinical symptoms in DNTC patients. Advanced DNTC cases may have deposition of α-synuclein. DNTC may also be closely associated with DLB as it is in AD patients. Hallucination and Parkinson’s symptoms, as observed in DLB patients, may appear in DNTC.
Conclusion
Although the number of patients is small, DNTC is recognized as a disease unit of tauopathy. The pathogenesis remains to be clarified. This refractory disease should be compared with other types of tauopathy to clarify its etiology. In the future, the differentiation of DNTC from Fahr’s syndrome, correlation between calcification and NFTs, and involvement of lead should be reviewed. Calcification may initiate before the onset. When Fahr’s syndrome is suspected on brain CT, DNTC must be considered. Epidemiologically, few studies have reported DNTC in other countries. Although the reason for this is unclear, an increasing number of patients may be reported in other countries in the future.
References
Ando J, Okaniwa T, Tachibana K (1965) An autopsy case of Pick’s disease. Shinkei Kenkyu-no-Shinpo 9:181–182 (In Japanese)
Shibayama H, Kobayashi H, Nagasawa MI et al (1992) Non-Alzheimer non-Pick dementia with Fahr’s syndrome. Clin Neuropathol 11:237–250
Kosaka K (1994) Diffuse neurofibrillary tangles with calcification: a new presenile dementia. J Neurol Neurosurg Psychiatry 57:594–596
Kosaka K (1997) Non-Alzheimer degenerative dementias. J Senile Dement 11:63–70 (In Japanese)
Tsuchiya K, Nakayama H, Haga C et al (2005) Distribution of cerebral cortical lesions in diffuse neurofibrillary tangles with calcification: a clinicopathological study of four autopsy cases showing prominent parietal lobe involvement. Acta Neuropathol 110:57–68
Tanabe Y, Ishizu H, Ishiguro K et al (2000) Tau pathology in diffuse neurofibrillary tangles with calcification (DNTC): biochemical and immunohistochemical investigation. Neuroreport 11:2473–2477
Ito Y, Kato T, Suzuki T et al (2003) Neuroradiologic and clinical abnormalities in dementia of diffuse neurofibrillary tangles with calcification (Kosaka-Shibayama disease). J Neurol Sci 15(209):105–109
Haraguchi T, Ishizu H, Kawai K et al (2001) Diffuse neurofibrillary tangles with calcification (a form of dementia): X-ray spectrometric evidence of lead accumulation in calcified regions. Neuroreport 12:1257–1260
Haraguchi T, Ishizu H, Takehisa Y et al (2001) Lead content of brain tissue in diffuse neurofibrillary tangles with calcification (DNTC): the possibility of lead neurotoxicity. Neuroreport 12:3887–3890
Terada S, Ishizu H, Tanabe Y et al (2001) Plaque-like structures and arteriosclerotic changes in “diffuse neurofibrillary tangles with calcification” (DNTC). Acta Neuropathol 102:597–603
Yokota O, Terada S, Ishizu H et al (2002) NACP/alpha-synuclein immunoreactivity in diffuse neurofibrillary tangles with calcification (DNTC). Acta Neuropathol 104:333–341
Hishikawa N, Hashizume Y, Ujihira N et al (2003) Alpha-synuclein-positive structures in association with diffuse neurofibrillary tangles with calcification. Neuropathol Appl Neurobiol 29:280–287
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer
About this chapter
Cite this chapter
Kuroda, S., Ishizu, H., Terada, S., Yokota, O., Tanabe, Y., Haraguchi, T. (2010). Diffuse Neurofibrillary Tangles with Calcification. In: Miyoshi, K., Morimura, Y., Maeda, K. (eds) Neuropsychiatric Disorders. Springer, Tokyo. https://doi.org/10.1007/978-4-431-53871-4_21
Download citation
DOI: https://doi.org/10.1007/978-4-431-53871-4_21
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-53870-7
Online ISBN: 978-4-431-53871-4
eBook Packages: MedicineMedicine (R0)