Abstract
The past 15 years have provided an unprecedented collection of discoveries that have increased our scientific understanding of recovery of human consciousness following severe brain damage. Differentiating between patients in “unresponsive/vegetative” and minimally conscious states still represents a major challenge with profound ethical concerns in terms of medical management. Valid diagnosis is of highest importance in chronic clinical settings, relying on standardized behavioral assessments and neuroimaging paradigms to detect subtle signs of consciousness. An improved assessment of brain function in coma and related states is not only changing nosology and medical care, but also offers a better-documented diagnosis and prognosis and helps to further identify the neural correlates of human consciousness. Recent treatment interventions aimed at accelerating the recovery of awareness show encouraging results, with improvements of behavioral signs of consciousness of severely brain-injured patients. These new insights in this field also raise new legal questions regarding treatment strategies, rehabilitation, and end-of-life decisions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Noxious Stimulation
- Minimally Conscious State
- Artificial Nutrition
- Surrogate Decision Maker
- Visual Pursuit
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
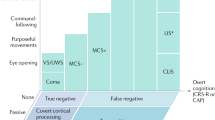
8.1 Disorders of Consciousness
Patients with disorders of consciousness (DOC) represent an important proportion of the disabled population worldwide. Severe brain injury can lead to coma where patients remain unaware with their eyes closed and do not respond to external stimulation (Plum and Posner 1983). When patients open their eyes but remain unconscious, they are diagnosed with vegetative state (VS) (The Multi-Society Task Force on PVS 1994; Laureys and Schiff 2012). The European Task Force on Disorders of Consciousness, recognizing that part of the health care, media, and lay public feels uncomfortable using the unintended denigrating “vegetable-like” connotation (seemingly intrinsic to the term VS), proposed the alternative name “unresponsive wakefulness syndrome” (UWS) (Laureys et al. 2010). UWS is a more neutral and descriptive term, pertaining to patients showing a number of clinical signs (i.e., syndrome) of unresponsiveness (i.e., without response to commands or oriented voluntary movements) in the presence of wakefulness (i.e., eye opening).
Patients who evolve from the UWS/VS condition show nonreflexive, goal-directed behaviors (e.g., visual pursuit, reproducible responses to commands or localisation to pain) and hence are considered to be in a minimally conscious state (MCS) (Giacino et al. 2002). Patients with MCS demonstrate partially preserved fluctuating levels of awareness, but they remain unable to functionally communicate. Depending on the complexity of the demonstrated behaviors, it was recently proposed to subcategorize the MCS condition into MCS- (i.e., when only showing simple nonreflex movements, such as visual pursuit, orientation to pain, or non-contingent behaviors) and MCS + (i.e., when patients recover the ability to respond to simple commands) (Bruno et al. 2011). Compared to the patients with MCS+, patients with MCS- may suffer from a significant general decrease in brain metabolism in the dominant hemisphere and particularly in regions that are functionally linked to speech comprehension and production, in motor and pre-motor areas and in sensory-motor areas (Bruno et al. 2012). Differential diagnosis for patients with MCS would therefore be mainly due to the functional recovery (or not) of speech-processing areas (Thibaut et al. 2012). Once these patients can communicate in a functional manner and/or show functional object use, they are diagnosed as having emerged from MCS (Giacino et al. 2002). These states lie between unconsciousness and awareness; the distinction between them has important therapeutic and ethical implications (Hirschberg and Giacino 2011). Patients in MCS are more likely to feel pain (Boly et al. 2008; Chatelle et al. 2014a, b) and might benefit from analgesic treatment or other interventions aimed to improve their interaction with the environment (Cruse et al. 2011; Lule et al. 2013; Thibaut et al. 2014). Patients in an MCS are also more likely to recover higher levels of consciousness than are patients with UWS/VS (Luaute et al. 2010; Hirschberg and Giacino 2011). Several countries have established the legal right of physicians to withdraw artificial life support from patients with UWS/VS (Gevers 2005; Perry et al. 2005; Ferreira 2007), but not from patients in a MCS (Manning 2012).
8.2 Behavioral Assessment
The detection of unambiguous signs of consciousness in severely brain-damaged patients is challenging and relies on disentangling automatic responses from nonreflex-oriented movements or command following. Motor responses may be ambiguous and inconsistent, potentially leading to diagnostic errors (Monti et al. 2009). A prospective study on coma survivors showed that the clinical consensus diagnosis of UWS/VS, attributed to 44 patients, was incorrect in 18 cases. Such a high rate of diagnostic error (i.e., 41 %) should prompt clinicians to use validated behavioral scales of consciousness before making the diagnosis of UWS/VS (Schnakers et al. 2009). While consensus-based diagnostic guidelines for DOC have been established (Giacino et al. 2002), there are no procedural guidelines regarding bedside assessment. Many different scales have been developed to assess patients in the chronic phase, and this last decade has particularly been focusing on the differential diagnosis between UWS/VS and MCS. Table 8.1 gives a non-exhaustive overview of the behavioral scales used in the chronic setting.
The American Congress of Rehabilitation Medicine conducted a systematic, evidence-based review of these behavioral assessment scales and provided evidence-based recommendations for clinical use (Seel et al. 2010). It was suggested to use the Coma Recovery Scale-Revised (CRS-R; Giacino et al. 2004; Schnakers et al. 2008a – summarized in Table 8.2). CRS-R has excellent content validity, and it is the only scale to address all Aspen Workgroup criteria (i.e., items used to differentiate MCS from UWS/VS). The CRS-R also offers the advantage to systematically search for signs of nonreflex behavior (e.g., visual pursuit or oriented response to noxious stimulation) and command following, in a well-defined manner. Visual pursuit, for example, should be assessed by using a moving mirror, as it has been shown that a substantial number of patients will not show eye tracking of a moving object or person but will do so when using an auto-referential stimulus such as the own face (Vanhaudenhuyse et al. 2008). Conversely, signs such as visual blinking to threat (Vanhaudenhuyse and Giacino 2008) and visual fixation (Bruno et al. 2010) were shown not to necessarily reflect conscious awareness and could hence be compatible with the diagnosis of UWS/VS. It is important that the evaluations are repeated over time and performed by trained experienced assessors (Lovstad et al. 2010). Confounding factors such as drugs with sedative side effects (e.g., against spasticity or epilepsy) or the presence of infection or other medical complications should be accounted for. This situation is even more problematical when patients have underlying deficits with communication functions, such as aphasia, agnosia, or apraxia (Majerus et al. 2005, 2009). Hence, some behaviorally unresponsive patients could, despite the best clinical assessment, be underestimated in terms of residual cognition or conscious awareness (Giacino et al. 2014). Since the venue of functional neuroimaging, this challenging issue can be addressed by measuring brain activity at rest and during sensory stimulation in these patients (Di Perri et al. 2014; Gosseries et al. 2014a)
8.3 Neuroimaging Assessment
Behavioral scales make inferences about patients’ awareness based on (the prensence/absence of) motor responsiveness. Functional neuroimaging (e.g., positron emission tomography (PET) and functional magnetic resonance imaging – fMRI) and cognitive evoked potential studies allow quantifying and noninvasively DOC patients brain activity at rest and during external activation (see Chaps. 9 and 12). fMRI activation studies in UWS/VS (Bekinschtein et al. 2005; Di et al. 2007; Fernandez-Espejo et al. 2008; Coleman et al. 2009) have confirmed previous PET studies showing preserved activation of “lower level” primary sensory cortices which are disconnected from “higher-order” associative cortical networks (i.e., frontoparietal associative cortices, cingulate gyrus, precuneus, and thalamus) (Laureys et al. 2004; Vanhaudenhuyse et al. 2010, 2011; Langsjo et al. 2012; Demertzi et al. 2013) employing auditory (Laureys et al. 2000; Boly et al. 2005), somatosensory (Boly et al. 2008), visual (Owen et al. 2002), or even emotional stimulations (Bekinschtein et al. 2004; Schiff et al. 2005).
These neuroimaging techniques have also been developed in order to detect “neural” (motor-independent) command following. Clinically unresponsive patients could perform mental imagery tasks, as shown by fMRI (Monti et al. 2010). Since this case report, similar “active” or “command following” paradigms have been tested in severe brain-damaged patients with different technologies such as event related potentials or electromyography (Bekinschtein et al. 2008; Schnakers et al. 2008b; Cruse et al. 2011; Habbal et al. 2014). Recently, it has been demonstrated that 18F-fluorodeoxyglucose-PET showed the highest sensitivity in identifying MCS having a good overall congruence with repeated CRS-R diagnosis, when compared to mental imagery task in fMRI (Stender et al. 2014). Complementary to these approaches, methods are developed to detect recovery of consciousness in ways that do not depend on the integrity of sensory pathways. Transcranial magnetic stimulation combined with electroencephalography can be performed at the bedside while bypassing subcortical afferent and efferent pathways and without requiring active participation of subjects or language comprehension (see Chap. 10). Hence, this complementary techinique could also permit an effective way to detect and track recovery of consciousness in patients with DOC who are unable to exchange information with the external environment (Rosanova et al. 2012, Casali AG et al. 2013 and Sarasso S et al.2014). The validation of new promising neuroimaging-based differential diagnostic markers, such as quantified metabolic markers or resting state fMRI, is of primary importance to complement the differential diagnosis.
8.4 Treatment
Although our understanding of the neural correlates of consciousness has greatly evolved over the past years, daily care has not yielded specific, evidence-based medical treatments for patients with DOC. Pharmacological treatment to promote the emergence of consciousness can be administered in the subacute and the chronic (more than 1 month) phases. Frequently prescribed pharmacological treatments include dopaminergic (e.g., amantadine, apomorphine, methylphenidate, levodopa, bromocriptine) and GABAergic agents (e.g., zolpidem, baclofen) (Chew and Zafonte 2009; Gosseries and Charland-Verville, 2014; Thonnard et al. 2014). Next, there is a long history of brain stimulation in medical science, and research has long been focused on some cortical areas and deep brain structures like the prefrontal cortex and the thalamus. Only few techniques were studied scientifically in this population of patients. Deep brain stimulation showed behavioral improvement after the implantation of an electrical stimulator in the intralaminar nuclei (Schiff et al. 2009). However, and the number of patients who can benefit from this intervention is still limited. Recently, noninvasive transcranial direct current stimulation (tDCS) studies showed encouraging results, with improvements in the behavioral signs of consciousness of severely brain-injured patients (Thibaut et al. 2014). Short-duration anodal (i.e., excitatory) tDCS of left dorsolateral prefrontal cortex induced short-term improvement in patients with MCS of acute and chronic etiologies measured by behavioral CRS-R total scores. The long-term noninvasive neuromodulatory tDCS outcome clinical improvement remains to be shown. In the years to follow, interventions should multiply, and therapeutic measures need to be more accessible, controlled, and effective.
8.5 Ethical Challenges
Early since DOC appeared in the clinical setting, clinicians, scholars, theologians, and ethicists began to wonder how it is like to be in a state of altered consciousness (e.g., Thompson 1969). First, one of the most debatable issues about this population is pain perception. Painful experience is a first-person one and classic pain assessment requires the patients’ verbal feedback (International Association of Pain Specialists (IASP 1994)). When it comes to severely brain-injured patients who are unable to communicate their feelings and possible suffering, the question of pain perception is far more complex (Chatelle et al. 2014a, b). According to survey attitudes among health-care professionals to the question “Do you think that patients in a UWS/VS can feel pain?” 68 % of the interviewed paramedical caregivers (n = 538) and 56 % of physicians (n = 1166) answered “yes.” Paramedical professionals, religious caregivers, and older caregivers reported more often that UWS/VS patients might experience pain. Following professional background, religion was the highest predictor of caregivers’ opinion: 64 % of religious (n = 1,009; 850 Christians) versus 52 % of nonreligious respondents (n = 830) answered positively. To the question “Do you think that patients with MCS can feel pain?” nearly all interviewed caregivers answered “yes” (96 % of the medical doctors and 97 % of the paramedical caregivers). Women and religious caregivers reported more often that MCS patients might experience pain (Demertzi et al. 2009). Considering these results on varying beliefs about pain perception in DOC, physicians and health-care workers’ views on analgesia and symptom management may also be affected. The presence or absence of nociception is inferred via motor responses following noxious stimulation, such as stereotypical responses, flexion withdrawal, and localization responses (Schnakers and Zasler 2007). In patients with DOC, only a clear localization to noxious stimulation is considered to be an indicator of conscious perception (Giacino et al. 2002). In order to accurately nonverbally assess nociception in this challenging population, the Nociception Coma Scale-Revised (NCS-R) (Chatelle et al. 2012) has been proposed. It assesses motor, verbal, and facial behaviors behavioral responses at rest, during daily nursing care, and during nociceptive stimulation. A cut-off score of 4 and higher suggest the need of adequate pain management (Chatelle et al. 2014a, b).
Patients with chronic DOC may also pose ethical challenges requiring the mediation of legal authorities in order to regulate end-of-life decisions. When the clinical condition of a patient has been stabilized and denoted as irreversible, decisions about artificial nutrition and hydration limitation may come into play. In a European survey, the controversies around the clinical management at the end-of-life were reflected (Demertzi et al. 2011). Sixty-six percent of health-care professionals agreed to withdraw treatment in patients with UWS/VS for more than 1 year, whereas only 28 % agreed to do so for patients with MCS. In our study, we also found that end-of-life decisions are not always governed by clinical circumstances but rather, physicians’ characteristics. Geographic differences as well as religious background were the variables that consistently predicted end-of-life statements. Residents from Northern and Central Europe, as compared to Southern Europeans, were more likely to agree with medically assisted nutrition and hydration withdrawal in chronic (> 1 year) UWS/VS, whereas religious respondents, older respondents, and women were less likely to find it acceptable. From a bioethical standpoint, withdrawing artificial nutrition and hydration is comparable to withdrawing mechanical ventilation, even if emotionally these two actions may be perceived differently (Laureys 2005). Despite the controversy as to whether artificial nutrition and hydration constitutes a medical treatment (Bernat and Beresford 2006), most of the medical community would agree with its being a medical therapy which can be refused by patients and surrogate decision makers (Steinbrook and Lo 1988). Patients with DOC represent a difficult group, ethically, for surrogate decision-making. The medical community needs policies to reach better internal agreement within the professional network and effective communication with patient communities and their families (Manning 2012; Bruno et al. 2013).
8.6 Conclusion
Disentangling between patients with MCS and UWS/VS represents a major challenge that can have heavy consequences, generating ethical and legal implications (Celesia 2000; Jennett 2002). The rapidly growing scientific findings on DOC must be taking into account for patients’ future care needs and to promote adequate policies to keep up with the findings. Consciousness research leads to redefinition of recovery, clinical criterion for diagnosis, and as increasing impact on prognosis (Fins 2009). The constantly evolving neuroimaging research field is raising new questions and challenges for medical ethics. As a result, clinicians must increasingly answer requests from family members and surrogate decision makers about the new diagnostic and therapeutic procedures. Because most of these reported procedures remain investigational, clinicians must be aware of the level of evidence supporting them and of the unavoidable ethical and social issues involved in responding to such requests. Moreover, studies must be supported in order to address the sensitivity and specificity of the neuroimaging or electrophysiological tools. Multicentric studies and collaborative work seem also essential to gather comparable data for the clinical behavioral assessments and about the potential prognostic value of the neuroimaging technologies (Di et al. 2008; Coleman et al. 2009).
References
Ansell BJ, Keenan JE (1989) The western neuro sensory stimulation profile: a tool for assessing slow-to-recover head-injured patients. Arch Phys Med Rehabil 70(2):104–108
Bekinschtein T, Niklison J et al (2004) Emotion processing in the minimally conscious state. J Neurol Neurosurg Psychiatry 75(5):788
Bekinschtein T, Tiberti C et al (2005) Assessing level of consciousness and cognitive changes from vegetative state to full recovery. Neuropsychol Rehabil 15(3/4):307–322
Bekinschtein TA, Coleman MR et al (2008) Can electromyography objectively detect voluntary movement in disorders of consciousness? J Neurol Neurosurg Psychiatry 79(7):826–828
Bernat JL, Beresford HR (2006) The controversy over artificial hydration and nutrition. Neurology 66(11):1618–1619
Boly M, Faymonville ME et al (2005) Cerebral processing of auditory and noxious stimuli in severely brain injured patients: differences between VS and MCS. Neuropsychol Rehabil 15(3–4):283–289
Boly M, Faymonville ME et al (2008) Perception of pain in the minimally conscious state with PET activation: an observational study. Lancet Neurol 7(11):1013–1020
Bruno MA, Laureys S et al (2013) Coma and disorders of consciousness. Handb Clin Neurol 118:205–213
Bruno MA, Majerus S et al (2012) Functional neuroanatomy underlying the clinical subcategorization of minimally conscious state patients. J Neurol 259(6):1087–1098
Bruno MA, Vanhaudenhuyse A et al (2010) Visual fixation in the vegetative state: an observational case series PET study. BMC Neurol 10(1):35
Bruno MA, Vanhaudenhuyse A et al (2011) From unresponsive wakefulness to minimally conscious PLUS and functional locked-in syndromes: recent advances in our understanding of disorders of consciousness. J Neurol 258(7):1373–1384
Casali AG, Gosseries O et al (2013) A theoretically based index of consciousness independent of sensory processing and behavior. Sci Transl Med 5:198ra105
Celesia G (2000) Persistent vegetative state: clinical and ethical issues. Suppl Clin Neurophysiol 53:460–462
Chatelle C, Majerus S, Whyte J, Laureys S, Schnakers C (2012) A sensitive scale to assess nociceptive pain in patients with disorders of consciousness. J Neurol Neurosurg Psychiatry 83(12):1233–1237
Chatelle C, Thibaut A et al (2014a) Nociception coma scale-revised scores correlate with metabolism in the anterior cingulate cortex. Neurorehabil Neural Repair 28(2):149–152
Chatelle C, Thibaut A et al (2014b) Pain issues in disorders of consciousness. Brain Inj 28(9):1202–1208
Chew E, Zafonte RD (2009) Pharmacological management of neurobehavioral disorders following traumatic brain injury–a state-of-the-art review. J Rehabil Res Dev 46(6):851–879
Coleman MR, Davis MH et al (2009) Towards the routine use of brain imaging to aid the clinical diagnosis of disorders of consciousness. Brain 132(Pt 9):2541–2552
Cruse D, Chennu S et al (2011) Bedside detection of awareness in the vegetative state: a cohort study. Lancet 378(9809):2088–2094
Demertzi A, Ledoux D (2011) Attitudes towards end-of-life issues in disorders of consciousness: a European survey. J Neurol 258:1058–1065
Demertzi A, Schnakers C et al (2009) Different beliefs about pain perception in the vegetative and minimally conscious states: a European survey of medical and paramedical professionals. Prog Brain Res 177:329–338
Demertzi A, Soddu A et al (2013) Consciousness supporting networks. Curr Opin Neurobiol 23(2):239–244
Di H, Boly M et al (2008) Neuroimaging activation studies in the vegetative state: predictors of recovery? Clin Med 8(5):502–507
Di HB, Yu SM et al (2007) Cerebral response to patient’s own name in the vegetative and minimally conscious states. Neurology 68(12):895–899
Di Perri C, Thibaut A et al (2014) Measuring consciousness in coma and related states. World J Radiol 6(8):589–597
Fernandez-Espejo D, Junque C et al (2008) Cerebral response to speech in vegetative and minimally conscious states after traumatic brain injury. Brain Inj 22(11):882–890
Ferreira N (2007) Latest legal and social developments in the euthanasia debate: bad moral consciences and political unrest. Med Law 26(2):387–407
Fins JJ (2009) Being conscious of their burden: severe brain injury and the two cultures challenge. Ann N Y Acad Sci 1157:131–147
Gevers S (2005) Withdrawing life support from patients in a persistent vegetative state: the law in the Netherlands. Eur J Health Law 12(4):347–355
Giacino JT, Ashwal S et al (2002) The minimally conscious state: definition and diagnostic criteria. Neurology 58(3):349–353
Giacino JT, Fins JJ et al (2014) Disorders of consciousness after acquired brain injury: the state of the science. Nat Rev Neurol 10(2):99–114
Giacino JT, Kalmar K et al (2004) The JFK coma recovery scale-revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil 85(12):2020–2029
Gill-Thwaites H (1997) The sensory modality assessment rehabilitation technique–a tool for assessment and treatment of patients with severe brain injury in a vegetative state. Brain Inj 11(10):723–734
Gill-Thwaites H, Munday R (2004) The sensory modality assessment and rehabilitation technique (SMART): a valid and reliable assessment for vegetative state and minimally conscious state patients. Brain Inj 18(12):1255–1269
Gosseries & Charland-Verville V et al (2014) Amantadine, apomorphine and zolpidem in the treatment of disorders of consciousness. Curr Pharm Des 20(26):4167–4184
Gosseries O, Zasler ND et al (2014) Recent advances in disorders of consciousness: focus on the diagnosis. Brain Inj 28(9):1141–1150
Habbal D, Gosseries O et al (2014) Volitional electromyographic responses in disorders of consciousness. Brain Inj 28(9):1171–1179
Hagen C, Malkmus D et al (1987) Levels of cognitive functioning. In: Professional Staff Association of Rancho Los Amigos Hospital (ed) Rehabilitation of the head injured adult: comprehensive physical management. Rancho Los Amigos Hospital Inc., Downey
Hirschberg R, Giacino JT (2011) The vegetative and minimally conscious states: diagnosis, prognosis and treatment. Neurol Clin 29(4):773–786
IASP (1994) Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. Task force on taxonomy. IASP Press, Seattle
Jennett B (2002) The vegetative state. Medical facts, ethical and legal dilemmas. Cambridge University Press, Cambridge
Langsjo JW, Alkire MT et al (2012) Returning from oblivion: imaging the neural core of consciousness. J Neurosci 32(14):4935–4943
Laureys S (2005) Science and society: death, unconsciousness and the brain. Nat Rev Neurosci 6(11):899–909
Laureys S, Celesia GG et al (2010) Unresponsive wakefulness syndrome: a new name for the vegetative state or apallic syndrome. BMC Med 8:68
Laureys S, Faymonville ME et al (2000) Auditory processing in the vegetative state. Brain 123(Pt 8):1589–1601
Laureys S, Owen AM et al (2004) Brain function in coma, vegetative state, and related disorders. Lancet Neurol 3(9):537–546
Laureys S, Schiff ND (2012) Coma and consciousness: paradigms (re)framed by neuroimaging. Neuroimage 61(2):478–491
Lovstad M, Froslie KF et al (2010) Reliability and diagnostic characteristics of the JFK coma recovery scale-revised: exploring the influence of rater’s level of experience. J Head Trauma Rehabil 25(5):349–356
Luaute J, Maucort-Boulch D et al (2010) Long-term outcomes of chronic minimally conscious and vegetative states. Neurology 75(3):246–252
Lule D, Noirhomme Q et al (2013) Probing command following in patients with disorders of consciousness using a brain-computer interface. Clin Neurophysiol 124(1):101–106
Majerus S, Bruno M et al (2009) The problem of aphasia in the assessment of consciousness in brain-damaged patients. Prog Brain Res 177:49–61
Majerus S, Gill-Thwaites H et al (2005) Behavioral evaluation of consciousness in severe brain damage. Prog Brain Res 150:397–413
Manning J (2012) Withdrawal of life-sustaining treatment from a patient in a minimally conscious state. J Law Med 19(3):430–435
Monti MM, Coleman MR et al (2009) Neuroimaging and the vegetative state: resolving the behavioral assessment dilemma? Ann N Y Acad Sci 1157:81–89
Monti MM, Vanhaudenhuyse A et al (2010) Willful modulation of brain activity in disorders of consciousness. N Engl J Med 362(7):579–589
Owen AM, Menon DK et al (2002) Detecting residual cognitive function in persistent vegetative state. Neurocase 8(5):394–403
Perry JE, Churchill LR et al (2005) The Terri Schiavo case: legal, ethical, and medical perspectives. Ann Intern Med 143(10):744–748
Plum F, Posner JB (1983) The diagnosis of stupor and coma. F. A. Davis, Philadelphia, pp 363–364
Rappaport M (2000) The coma/near coma scale. Retrieved 21 Aug 2006, from http://www.tbims.org/combi/cnc
Rappaport M, Dougherty AM et al (1992) Evaluation of coma and vegetative states. Arch Phys Med Rehabil 73(7):628–634
Rosanova M, Gosseries O et al (2012) Recovery of cortical effective connectivity and recovery of consciousness in vegetative patients. Brain 135(Pt 4):1308–1320
Sarasso S, Rosanova M et al (2014) Quantifying cortical EEG responses to TMS in (un)consciousness. Clin EEG Neurosci 45(1):40–49
Schiff ND, Giacino JT et al (2009) Deep brain stimulation, neuroethics, and the minimally conscious state: moving beyond proof of principle. Arch Neurol 66(6):697–702
Schiff ND, Rodriguez-Moreno D et al (2005) fMRI reveals large-scale network activation in minimally conscious patients. Neurology 64(3):514–523
Schnakers C, Majerus S et al (2008a) A French validation study of the Coma Recovery Scale-Revised (CRS-R). Brain Inj 22(10):786–792
Schnakers C, Perrin F et al (2008b) Voluntary brain processing in disorders of consciousness. Neurology 71(20):1614–1620
Schnakers C, Vanhaudenhuyse A et al (2009) Diagnostic accuracy of the vegetative and minimally conscious state: clinical consensus versus standardized neurobehavioral assessment. BMC Neurol 9:35
Schnakers C, Zasler ND (2007) Pain assessment and management in disorders of consciousness. Curr Opin Neurol 20(6):620–626
Seel RT, Sherer M et al (2010) Assessment scales for disorders of consciousness: evidence-based recommendations for clinical practice and research. Arch Phys Med Rehabil 91(12):1795–1813
Shiel A, Horn SA et al (2000) The Wessex Head Injury Matrix (WHIM) main scale: a preliminary report on a scale to assess and monitor patient recovery after severe head injury. Clin Rehabil 14(4):408–416
Steinbrook R, Lo B (1988) Artificial feeding–solid ground, not a slippery slope. N Engl J Med 318(5):286–290
Stender J, Gosseries O et al (2014) Diagnostic precision of PET imaging and functional MRI in disorders of consciousness: a clinical validation study. Lancet 384(9942):514–522
The Multi-Society Task Force on PVS (1994) Medical aspects of the persistent vegetative state (2). N Engl J Med 330(22):1572–1579
Thibaut A, Bruno MA et al (2012) Metabolic activity in external and internal awareness networks in severely brain-damaged patients. J Rehabil Med 44(6):487–494
Thibaut A, Bruno MA et al (2014) tDCS in patients with disorders of consciousness: sham-controlled randomized double-blind study. Neurology 82(13):1112–1118
Thompson GT (1969) An appeal to doctors. Lancet 2:1353
Thonnard M, Gosseries O, et al (2014) Effect of zolpidem in chronic disorders of consciousness: a prospective open-label study. Funct Neurol 1–6
Vanhaudenhuyse A, Demertzi A et al (2011) Two distinct neuronal networks mediate the awareness of environment and of self. J Cogn Neurosci 23(3):570–578
Vanhaudenhuyse A, Giacino J (2008) Blink to visual threat does not herald consciousness in the vegetative state. Neurology 71:1374–1375
Vanhaudenhuyse A, Noirhomme Q et al (2010) Default network connectivity reflects the level of consciousness in non-communicative brain-damaged patients. Brain 133(Pt 1):161–171
Vanhaudenhuyse A, Schnakers C et al (2008) Assessment of visual pursuit in post-comatose states: use a mirror. J Neurol Neurosurg Psychiatry 79(2):223
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Wien
About this chapter
Cite this chapter
Charland-Verville, V., Laureys, S., Gosseries, O., Thibaut, A., Bruno, MA. (2015). The Chronic Clinical Setting. In: Rossetti, A., Laureys, S. (eds) Clinical Neurophysiology in Disorders of Consciousness. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1634-0_8
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1634-0_8
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1633-3
Online ISBN: 978-3-7091-1634-0
eBook Packages: MedicineMedicine (R0)