Abstract
A key component of the pathophysiology and subsequent treatment of meniscal tears and dysfunction is the axial alignment of the lower limb. Degenerative meniscal tears have been shown to correlate with the presence of malalignment, particularly in the medial compartment, with meniscectomy having been shown to often result in the rapid progression of osteoarthritis. This chapter will focus on the relationship of meniscus pathology and alignment and how realignment osteotomy plays an important role in off-loading the meniscus-deficient knee compartment. This can either be accomplished by correcting the alignment on either the tibial or femoral sides, depending upon where the primary deformity exists.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
11.1 Introduction
The meniscus has an important role of reinforcing and stabilizing the incongruity of the femur and tibia and is responsible for transmitting 40–60 % of stress to the knee when standing and 85 % when at 90 degrees flexion [1, 2]. Medial meniscus tears are more frequently reported since the medial structures are more firmly attached to the tibia, compared to the lateral meniscus which has a relatively free range of motion [3]. In a large-scale study targeting the middle aged or the elderly, a maximum of 35 % showed meniscus injury and the prevalence increased with age [2].
Meniscal tears are not always the result of trauma. Ferrer-Roca and Vilalta stated that it was of interest that only 35 % of their patients whose menisci had been removed had a history of trauma [4]. Therefore, it has been stated that other factors play an important role in the pathophysiology of meniscal tears [2, 5]. In this chapter, we focus on the role of axial alignment of the lower limb and its relationship with meniscal tears and degeneration. Furthermore, we will outline the biomechanical principles of realignment osteotomy, provide evidence for the role of osteotomy with meniscal pathology, and outline the surgical technique utilized at our institution.
11.2 How Does Alignment Relate to Meniscus Tears and Degeneration?
The knee joint is the largest and most complex joint in the human body and has the longest lever arms. The joint transmits muscle forces into motion, with large lever arms producing substantial load moments across the joint due to the ground reaction force acting about the center of rotation of the knee, creating adduction and abduction moments in the varus and valgus knee, respectively (Fig. 11.1). Axial load causes high mechanical stress in the respective joint compartments, with mechanical load during walking on even ground amounting to 3.4 times body weight and as much as 4.3 times when climbing stairs [6, 7].
The most frequent leg deformities occur in the coronal plane (varus–valgus deviations). Malalignment can be defined as a deviation of the mechanical axis. A significant deviation in the coronal plane is diagnosed when the weight-bearing axis of the lower extremity lies more than 15 mm medial to the center of the knee joint (varus deviation) or more than 10 mm lateral of the center (valgus deviation) [8]. To differentiate between a femoral and a tibial cause of malalignment, the mechanical lateral distal femoral angle (mLDFA, standard value 87° ± 3°) must be considered. If the mLDFA value is smaller than the standard value, the cause of the valgus deformity is femoral based. If the mechanical medial proximal tibial angle (mMPTA) is increased, the valgus malalignment is due to a tibial deviation. Conversely, an increased femoral angle (mLDFA) indicates a femoral cause of varus malalignment, whereas an mMPTA < 87° ± 3° indicates a tibial cause [8] (Fig. 11.2a).
(a, b) normal alignment indices of the distal femur and proximal tibia (c, d) preoperative correction planning for MOWHTO as per Dugdale et al. [36]
In the presence of tibial or femoral deviations in the frontal plane, forces can no longer be transferred uniformly at the knee joint. Instead, nonphysiological load distribution with mechanical stress occurs in the medial or lateral compartment. Teichtahl et al. reported that for every 1° of varus alignment, articular cartilage loss increased by 0.44 % per year, as measured on MRI [9]. It is therefore clear that mechanical overload of a joint compartment correlates with cartilage damage and either promotes the development of degenerative joint disease or accelerates its progress [10–12].
In many studies, the increased degree of lower limb varus is reported to be related to the progression of osteoarthritis due to medial meniscus injury and articular cartilage injury [1, 13–15]. It has been reported that the axial alignment of the lower limb in patients with isolated tears of the medial meniscus without obvious trauma is varus. The alignment is almost normal in those with obvious trauma. Therefore, it seems that a varus deformity of the knee is closely related to the occurrence of a medial meniscal tear [5]. This is not the case for the lateral meniscus, since the axial alignment of the lower limb does not appear to have a relationship with the occurrence of lateral meniscal tears, because the alignment of the lower limb was normal in these patients [5].
In summary, even without obvious trauma, the load stress to the knee produces degeneration of the medial meniscus in the varus knee, potentially leading to a later meniscal tear.
The medial meniscus is closely attached to the deep layer of the medial collateral ligament at its middle segment, resulting in relatively low mobility. In comparison with the lateral meniscus, the medial meniscus is broad and thick, particularly in the posterior segment. These conditions may explain why the medial meniscus is more prone to be influenced by load stress than the lateral meniscus [5].
11.3 Principles of Realignment Osteotomy
Osteotomies around the knee that alter the weight-bearing axis of the lower extremity have a substantial effect on the load balance and distribution of pressure at the knee joint [16]. Birmingham et al. demonstrated that valgus medial opening wedge high tibial osteotomy (MOWHTO) resulted in substantial and clinically important reductions in the load on the medial tibiofemoral compartment as measured by reductions in knee adduction moment on 3D gait analysis, with associated improvement in patient reported outcomes [17]. A similar result was found in a study by Collins et al. concerning the varus lateral opening wedge HTO [18]. Femoral and tibial osteotomies facilitate the restoration of the physiological axes of the lower limb.
To achieve the desired off-loading of the compartment, the mechanical axis is moved to a predetermined position in the knee. The most common deformity is varus malalignment in the face of medial compartment osteoarthritis. Many surgeons aim to move the axis beyond the center of the knee, to the Fujisawa point. This is 62.5 % of the medial–lateral width of the knee joint from the medial edge [19]. Fujisawa fails to provide a mechanical rationale for using this point. Rather, it appears to have been a subjective judgment based on the results of chondral biopsies in a small series of HTOs [19]. It is therefore unclear from the current literature whether Fujisawa’s desired correction is optimal for biological augmentation. Agneskirchner et al. investigated the effect on the tibiofemoral articular contact pressures by moving the resultant force vector from medial to lateral during sequential medial opening wedge osteotomy in cadavers [20]. They found that the contact pressure in the lateral compartment was already 70 % higher than that in the medial compartment when the load vector passed through the center of the knee and that it continued to increase as the valgus angulation increased [21]. Therefore, it is therefore suggested that a desired correction would be between 50 % and 62.5 % medial to lateral in order to achieve the appropriate degree of compartment unloading. The same principles may be applied to the valgus knee, where correction in alignment should aim to be either neutral or slight varus; however, no studies have determined the optimal alignment for longevity of successful treatment outcomes.
11.4 Evidence for Realignment Osteotomy with Meniscal Deficiency
The goals of treatment of patients with symptomatic meniscal deficiency are primarily to provide symptomatic relief during daily activities with subsequent improvements in patient function and quality of life; relief with higher-level activities tends to be less predictable. Ideally, treatment would prevent further progression of osteoarthritis, although the current literature has not reliably demonstrated this [22]. Surgical treatments, including meniscal allograft transplantation (MAT), synthetic segmental meniscus replacement, and realignment osteotomy, are options that attempt to decrease the loads on the articular cartilage of the meniscus-deficient compartment by replacing meniscal tissue or altering joint alignment. In this section we focus on the existing evidence concerning different types of osteotomy as a treatment option for meniscal deficiency.
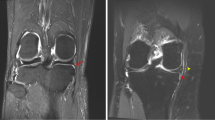
High tibial osteotomy (HTO) presents as an option for patients suffering from unicompartmental post-meniscectomy degeneration with tibial-based malalignment. This is the most common varus deformity because of a reduced medial proximal tibial angle. A medial opening wedge high tibial osteotomy (MOWHTO) (Fig. 11.3) has become the most common procedure to deal with this deformity due to the ease of angular correction and the maintenance of proximal metaphyseal bone stock. The lateral tibial closing wedge osteotomy was also common in the treatment of varus malalignment, but has fallen out of favor due to the higher risk for complications and imprecision in achieving the desired angle of correction. The dome osteotomy is not commonly performed, because it is more technically demanding to create a curved osteotomy; it is more indicated for a larger correction [22, 23].
Isolated lateral compartment osteoarthritis can occur also after meniscectomy. Due to the joint geometry and lack of congruity in the lateral compartment, resection of the lateral meniscus causes a much greater increase in contact stresses in the lateral compartment, and therefore the articular cartilage is at much greater risk of degeneration in these knees. As such, it is critical to assess the alignment of patients who have undergone lateral meniscectomy as they will be at significant risk of developing early chondrosis and subsequent OA. In this scenario, if the mechanical malalignment is femoral based, then a distal femoral varus osteotomy (DFVO) is an option to treat these patients [24] (Fig. 11.5). If, however, the valgus alignment is secondary to cartilage and meniscus loss, a tibial-based correction in the form of a lateral opening wedge HTO is a great option, because it affects the mechanical axis of the joint throughout a complete range of motion (Fig. 11.4). DFVO is only efficient in extension, whereas a tibial-based correction will also off-load the desired compartment in flexion too.
The success of HTO slowly diminishes with time. The mean range of effectiveness is more than 7 to 10 years. In this way, an HTO can win valuable time before placing a unicompartmental or total knee arthroplasty [23, 25]. Inaccurate correction of preoperative deformity is the biggest contributor to HTO failure. If inaccuracy occurs, overcorrection is more desirable than under correction [22, 26, 27]. The survival of isolated HTO gradually declines over time up to a 20-year follow-up. This was found in a review of 57 studies (4344 knees) of isolated HTO [25]. The respective survival rates were 92.4 %, 84.5 %, 77.3 %, and 72.3 % at 5, 10, 15, and 20 years of follow-up. This review also included four studies that directly compared medial opening wedge osteotomy with lateral closing wedge osteotomy, with no difference in survivorship or clinical outcomes in follow-up of more than 2 years [22, 25]. Luites et al. compared 42 patients treated with either a medial opening wedge or lateral closing wedge osteotomy in a randomized clinical trial [28]. They reported no difference in recovery period and bone healing. Song et al. similarly retrospectively compared outcomes of both medial opening and lateral closing osteotomy techniques at 3-year follow-up and found no significant difference in anterior knee pain, patellar alignment, or patellofemoral arthritis [29]. Another study observed that 90 % of patients after an HTO were engaged in sports at the same intensity as preoperatively [30].
DFO has been established for treatment of isolated lateral compartment arthritis in select patients, with a mean survivorship of 80 % at a 10-year follow-up [24].
In general, osteotomies are an effective procedure for the young patients allowing them to return to impact activities with less discomfort, with no significant differences observed between medial opening wedge and lateral closing wedge osteotomies.
11.5 Surgical Technique of Osteotomy
11.5.1 Patient Assessment
Important factors regarding osteotomy include patient comorbidities and smoking status. A study looking at the complications of HTO in our institution found that diabetics and smokers were associated with an increased risk of postoperative complications [31]. Gait assessment is important to check for a dynamic varus or valgus thrust (coronal plane movement during stance phase). An added hyperextension moment on heel strike is indicative of a further posterior soft tissue attenuation issues, usually in the opposite corner to the involved compartment.
Assessment of prior skin incisions, if present, is important, because this may dictate the surgical approach both at the current and for potential future operations. Assessment for all other pathologies that may be also addressed – either concomitantly or as a staged procedure – must be undertaken. These include stiffness, instability, malalignment, meniscal pathology, and chondral/osteochondral involvement.
Radiological assessment specific to osteotomy considerations includes anteroposterior, Rosenberg, lateral, and hip-to-ankle double-leg standing alignment radiographs. Varus/valgus or kneeling posterior stress views may be considered if dealing with complex instability patterns.
11.5.2 Osteotomy Planning
The following flow decision-making algorithm can be used to determine the type of osteotomy required to address the presenting pathology:
-
1.
Site of correction – tibia or femur?
-
2.
Degree of correction required – to neutral or overcorrection?
-
3.
Single or biplanar correction – is there associated anteroposterior instability?
-
4.
Opening or closing wedge – dependent upon the approach used and surgical preferences.
-
5.
Hardware choices – ensuring that the hardware is not prohibitive of further procedures.
-
6.
Concurrent vs. staged procedures – dependent upon the surgeon’s skill, the duration of the procedure, and hardware interference.
In the varus knee, a medial opening wedge HTO (MOWHTO) is the author’s first choice due to the ability to correct both coronal and sagittal planes, the ability to easily titrate the degree of correction, and the lack of disruption to the proximal tibial anatomy as seen in lateral closing wedge procedures [32]. The choice of the site of correction in the valgus knee is dependent upon the site of the deformity. If the valgus is secondary to cartilage and meniscus loss, with only a small degree of valgus, a lateral opening wedge HTO (LOWHTO) is the procedure of choice, because it addresses the problem throughout the range of flexion and extension [18]. Great care must be taken not to increase the proximal tibial joint line obliquity by more than 10°, as this has been presumed to be associated with poor outcomes [31, 33, 34].
If the deformity is primarily in the femur, i.e., if the anatomic lateral distal femoral articular angle (aLDFA) is abnormal (<80°), then a femoral-based correction is preferred. In this instance, the medial closing wedge distal femoral varus osteotomy (MCWDFVO) is our procedure of choice, due to the ease of approach, the stability of the construct, and good healing potential. A lateral opening wedge DFVO is an alternative option.
11.5.3 Degree of Correction
Fujisawa indicates that moving the mechanical axis into the opposite compartment is beneficial in isolated HTO [35]. The optimal degree of correction – whether neutral or overcorrection – is unknown. It is the authors’ preference to correct the mechanical axis of the varus knee to the downslope of the lateral tibial eminence while in the valgus knee to correct to neutral. The method of Dugdale et al. [36] is used to calculate the correction for the MOWHTO (Fig. 11.2c, d), which may be modified for the LOWHTO and the MCWDFVO.
11.5.4 MOWHTO Technique (Fig. 11.3)
-
Approach – an oblique skin incision is prepared to ensure that as much soft tissue as possible overlies the hardware in order to try and reduce the incidence of infection. A distal MCL release is performed to prevent a tension band on the medial side when opening the wedge. A blunt retractor is then placed posteriorly after elevating the posterior periosteum to protect the neurovascular structures.
-
Osteotomy and wedge opening – the desired level of the osteotomy is marked so as to ensure that there is enough room for hardware proximally in the metaphysis. A guide pin is placed from medial to lateral, making sure that the lateral hinge point is 1.5 times the distance from the lateral joint line to the lateral tibial cortex. The osteotomy is initiated with an oscillating saw and is continued with an osteotome under fluoroscopic control, with the posterior retractor in place at all times, leaving a lateral hinge. The wedge is then opened slowly, taking care not to fracture the lateral hinge. Due to the geometry of the anteromedial wall of the proximal tibia, the wedge should open approximately double the distance posteromedially as anteromedially so as to ensure that the tibial slope is not inadvertently altered.
-
Fixation – once the desired correction is achieved, based on preoperative calculations, the hardware is applied as per the manufacturer’s guidelines. The proximal screws are inserted first, followed by one distal screw. At this stage, the knee can be brought out to extension in order to attempt to close the wedge down anteriorly, thereby reducing the chance of increasing tibial slope.
-
Rehabilitation – this generally entails touch weight-bearing for 4 weeks, with range of movement limited to 0–90°. At 4 weeks, patients may weight-bear as tolerated.
Surgical technique for medial opening wedge high tibial osteotomy (MOWHTO). This is a right knee undergoing MOWHTO. A tourniquet is applied with lateral post and foot roll to support the knee held at 90° of flexion. (a) Oblique skin incision over pes anserinus allows a greater soft tissue envelope over the plate, helping to reduce wound infection and reduce risk to sartorial branch of saphenous nerve. (b) The sartorius fascia is split, and a blunt retractor is placed posteriorly protecting the neurovascular structures. The MCL is then cut at the level of the osteotomy. (c) A guide pin is placed in the line of the osteotomy, stopping at the level of the proximal tib/fib joint. The lateral hinge should be at least 1.5 times greater the distance from the lateral joint line than to the lateral cortex to help avoid intra-articular propagation of the osteotomy. (d) Following creation of the osteotomy with oscillating saw and osteotome, the wedge is opened with a spreader. (e) The osteotomy is held open with a wedge or laminar spreader and the plate is applied. (f) The screws are inserted percutaneously and the locking plate internal fixator is fixed in place as shown
11.5.5 LOWHTO Technique (Fig. 11.4)
A similar process regarding the order of HTO is followed:
-
Approach – a lateral–longitudinal skin incision is made centered between the tibial tubercle and the anterior border of the fibula head. The tibialis anterior is elevated off the bone and retracted posterolaterally, taking the nerve with it. The dissection is carried on to the anterior capsule of the proximal tibiofibular joint, which is opened and mobilized, negating the need for a fibular osteotomy. A blunt retractor is then placed posteriorly after elevating the posterior periosteum to protect the neurovascular structures.
-
Osteotomy and wedge opening – a similar process is followed as per the MOWHTO, except that the pin is placed from lateral to medial, and the wedge should have equal posterior and anterior gaps. This is again due to the proximal tibial geometry, which is more uniform on the lateral side than on the medial side.
-
Fixation – a lateral locking plate is utilized to maintain the correction.
-
Rehabilitation – similar as above.
Surgical technique for lateral opening wedge high tibial osteotomy (LOWHTO). This is a right knee undergoing LOWHTO. A tourniquet is applied with lateral post and foot roll to support knee held at 90° of flexion. (a) Curvilinear skin incision on lateral side of the knee midway between lateral border of patella and anterior border of fibula head. This may be extended if a lateral MAT is being performed and an arthrotomy is required. (b) Tibialis anterior is elevated off the proximal tibia and a blunt retractor is placed posteriorly to protect the neurovascular structures. Another blunt retractor is placed under the patella tendon to allow visualization of the anterior interval. (c, d) The osteotomy is performed with oscillating saw and osteotome under fluoroscopic guidance. (e, f) The spreader is inserted and the osteotomy is opened to the desired correction. (g) The osteotomy is held open with a wedge and the correction/alignment is checked. (h, i) The lateral plate is bent to fit the lateral cortex and applied in a standard method using locking screws
11.5.6 MCWDFVO Technique (Fig. 11.5)
-
Approach – a longitudinal paramedian skin incision is made over the distal femur and a subvastus approach is made. The distal femur is exposed, the neurovascular structures are elevated away from the posterior femur, and a blunt retractor is placed for protection throughout the procedure. A further blunt retractor is placed anteriorly under the vastus medialis.
-
Osteotomy and wedge opening – a biplanar closing wedge osteotomy is planned and measured out as per the preoperative planned correction. The biplane cut helps control coronal and sagittal displacement during wedge production and closure. A guide pin is inserted from the medial cortex to a position on the lateral side, just superior to the subchondral density of the posterior condyle. A further three pins may be inserted to mark out the size of the wedge, all culminating at a similar point on the anteroposterior fluoroscopic view, 5 mm from the cortex. The osteotomy wedge cut is then completed with an oscillating saw and an osteotome, and the wedge is removed. The wedge is then closed with a varus force applied to the leg and a medial locking plate applied.
-
Fixation – the distal metaphyseal screws are inserted first, followed by a proximal non-locking screw to achieve compression at the osteotomy site. The other holes are then filled with locking screws.
-
Rehabilitation – similar as above.
Surgical technique for medial closing wedge distal femoral varus osteotomy (MCWDFVO). This is a right knee undergoing MCWDFVO. A tourniquet is applied with lateral post and foot roll to support knee held at 90° of flexion. (a, b) Medial incision to the knee followed by a subvastus approach to distal femur. (c) A guide pin is inserted in an oblique fashion, proximally on the medial cortex so that when the wedge closes, there is no step in the cortex. The pin is aimed for the medial cortex, just at the level of the radiographic “scar” of the posterior condyle. (d) A further two pins are inserted to allow for planning of a closing wedge, as well as a biplane anterior cut in the coronal plane. This adds a greater degree of stability to the construct when closing and fixing. (e, f) The corticocancellous wedge is removed. (g, h) The plate is applied and fixed with locking screws
Conclusion
While different techniques for meniscal substitution exist, it is generally accepted that they should not be performed in a knee where the mechanical axis runs through the affected compartment. The biomechanical rationale for an unloading realignment osteotomy is clear. It results in a reduction of articular contact stress and in a resultant reduction of chondral wear.
There are a number of surgical options available when realignment osteotomy is indicated. It is important that a thorough examination and radiological assessment of the patient are performed, paying close attention to the site of deformity so as to best select the most appropriate method of correction for that individual patient to result in optimal clinical outcomes.
References
Smillie IS. Injuries of the knee joint. 5th ed. Edinburgh: Churchill Livingston; 1978. p. 114–8.
Leach RE, Baumgard S, Broom J. Obesity: its relationship to osteoarthritis of the knee. Clin Orthop Relat Res. 1973;93:271–3.
Lim HC, Lee SH, Shon WY, Lee DW. A clinical study of meniscus injury. J Korean Orthop Assoc. 1989;24:27–33.
Ferrer-Roca O, Vilalta C. Lesions of the meniscus. Part I. Macroscopic and histologic findings. Clin Orthop. 1980;146:289–300.
Habata T, Ishimura M, Ohgushi H, Tamai S, Fujisawa Y. Axial alignment of the lower limb in patients with isolated meniscal tear. J Orthop Sci. 1998;3:85–9.
Morrison J. Bioengineering analysis of force actions transmitted by the knee joint. Bio Med Eng. 1968;3:164–70.
Morrison J. Function of the knee in various activities. Bio Med Eng. 1969;4:573–80.
Paley D, Pfeil J. Principles of deformity corrections around the knee. Orthopade. 2000;29:18–38.
Teichtahl AJ, Davies-Tuck ML, Wluka AE, Jones G, Cicuttini FM. Change in knee angle influences the rate of medial tibial cartilage volume loss in knee osteoarthritis. Osteoarthritis Cartilage. 2009;17:8–11.
Cicuttini F, Wluka A, Hankin J, et al. Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology. 2004;43:321–4.
Cerejo R, Dunlop DD, Cahue S, et al. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46:2632–6.
McKellop HA, Sigholm G, Redfern FC. The effect of simulated fracture-angulations of the tibia on cartilage pressures in the knee joint. J Bone Joint Surg Am. 1991;73:1382–91.
Englund M. Meniscal tear – a feature of osteoarthritis. Acta Orthop Scand. 2004;75:1–45.
Wendelboe AM, Hegmann KT, Biggs JJ, Cox CM, Portmann AJ, Gildea JH, Gren LH, Lyon JL. Relationships between body mass indices and surgical replacements of knee and hip joints. Am J Prev Med. 2003;25:290–5.
Jeong HJ, Park SJ, Shin HK, Kim EG, Choi JY, Lee JM. Analysis of the mechanical axis of the lower limb in patients with isolated meniscal tear. J Korea Knee Soc. 2009;21:286–91.
Maquet PG. Biomechanics of the knee: with application of the pathogenesis and the surgical treatment of osteoarthritis. 2nd ed. Heidelberg: Springer; 1984.
Birmingham TB, Giffin JR, Chesworth BM, Bryant DM, Litchfield RB, Willits K, et al. Medial opening wedge high tibial osteotomy: a prospective cohort study of gait, radiographic, and patient-reported outcomes. Arthritis Rheum. 2009;61:648–57.
Collins B, Getgood A, Alomar AZ, Giffin JR, Willits K, Fowler PJ, et al. A case series of lateral opening wedge high tibial osteotomy for valgus malalignment. Knee Surg Sports Traumatol Arthrosc. 2013;21:152–60.
Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10:585–608.
Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23:852–61.
Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg. 2004;124:575–84.
Rao AJ, Erickson BJ, Cvetanovich GL, Yanke AB, Bach Jr BR, Cole BJ. The Meniscus-deficient knee: biomechanics, evaluation and treatment options. Orthop J Sports Med. 2015;233(10):2325967115611386.
Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop. 2010;34:155–60.
Terry GC, Cimino PM. Distal femoral osteotomy for valgus deformity of the knee. Orthopedics. 1992;15:1283–9.
Harris JD, McNeilan R, Siston RA, Flanigan DC. Survival and clinical outcome of isolated high tibial osteotomy and combined biological knee reconstruction. Knee. 2013;20:154–61.
Brouwer RW, Bierma-Zeinstra SM, van Raaij TM, Verhaar JA. Osteotomy for medial compartment arthritis of the knee using a closing wedge or an opening wedge controlled by a Puddu plate. A one year randomized, controlled study. J Bone Joint Surg Br. 2006;88:1454–9.
TO S, Sexton D, Mitchell P, Hing CB. Opening- or closing wedged high tibial osteotomy: a meta-analysis of clinical and radiological outcomes. Knee. 2011;18:361–8.
Luites JW, Brinkman JM, Wymenga AB, van Heerwaarden RJ. Fixation stability of opening- versus closing-wedge high tibial osteotomy: a randomized clinical trial using radiostereometry. J Bone Joint Surg Br. 2009;91:1459–65.
Song IH, Song EK, Seo HY, Lee KB, Yim JH, Seon JK. Patellofemoral alignment and anterior knee pain after closing- and opening-wedge valgus high tibial osteotomy. Arthroscopy. 2012;28:1087–93.
Salzmann GM, Ahrens P, Naal FD, et al. Sporting activity after high tibial osteotomy for the treatment of medial compartment knee osteoarthritis. Am J Sports Med. 2009;37:312–8.
Martin R, Birmingham TB, Willits K, Litchfield R, LeBel ME, Giffin JR. Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am J Sports Med. 2014;42:1118–26.
Filho RB, Magnussen RA, Duthon V, Demey G, Servien E, Granjeiro JM, et al. Total knee arthroplasty after high tibial osteotomy: a comparison of opening and closing wedge osteotomy. Int Orthop. 2013;37(3):427–31.
Giffin JR, Vogrin TM, Zantop T, Woo S, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376–82.
El-Azab H, Glabgly P, Paul J, Imhoff AB, Hinterwimmer S. Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med. 2010;38:323–9.
Habata T, Uematsu K, Hattori K, Kasanami R, Takakura Y, Fujisawa Y. High tibial osteotomy that does not cause recurrence of varus deformity for medial gonarthrosis. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):962–7.
Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;274:248–64.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 ISAKOS
About this chapter
Cite this chapter
Dhollander, A., Getgood, A. (2017). The Role of Alignment in Meniscal Tears and the Role of Osteotomy. In: LaPrade, R., Arendt, E., Getgood, A., Faucett, S. (eds) The Menisci. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-53792-3_11
Download citation
DOI: https://doi.org/10.1007/978-3-662-53792-3_11
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-53791-6
Online ISBN: 978-3-662-53792-3
eBook Packages: MedicineMedicine (R0)