Abstract
Cyclodextrins are water-soluble oligosaccharides that form hydrophilic complexes with many lipophilic poorly soluble drugs. Cyclodextrins and cyclodextrin complexes do not permeate intact skin, and, thus, hydrophilic cyclodextrins do not affect the skin barrier, stratum corneum. Studies have shown that, in general, cyclodextrins only enhance drug permeation into and through the skin from aqueous vehicles and only if an aqueous diffusion barrier at the skin exterior contributes to the overall skin permeation barrier. Cyclodextrins do not enhance drug penetration from lipophilic vehicles or when the skin barrier itself is the main permeation barrier. Cyclodextrins are able to prevent drug partition from an aqueous exterior into the skin. Thus, it is of uttermost importance to optimize composition of cyclodextrin-containing drug vehicles with regard to drug release and permeation. In this chapter, the effects of cyclodextrins on percutaneous drug permeation are described. Simple mathematical models are used to explain how and when cyclodextrins act as penetration enhancers and then how these models can be applied to optimize drug delivery from a topical formulation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Drugs permeate intact skin as single molecules. When drug products are applied to the skin surface, dissolved drug molecules diffuse through the vehicle to the skin where the molecules partition from the vehicle into the skin and then permeate the skin barrier, stratum corneum, into the more permeable inner skin layers. Most penetration enhancers, chemical as well as physical, enhance drug delivery by making the skin barrier more permeable. Cyclodextrins are different. They enhance drug delivery into and through the skin by increasing the availability of dissolved drug molecules right at the skin surface. However, cyclodextrins can also hamper dermal and transdermal drug delivery by preventing drug molecules from partitioning from the surface into the skin. Thus, successful employment of cyclodextrins in topical drug formulations requires good understanding of their physicochemical properties and the way they enhance topical drug bioavailability.
Numerous books and reviews have been written on cyclodextrins, their industrial applications, and usage in drug formulations (Loftsson and Brewster 1996; Dodziuk 2006; Douhal 2006; Brewster and Loftsson 2007; Loftsson and Brewster 2010; Loftsson and Duchêne 2007; Stella and He 2008; Uekama et al. 2006; Hedges 1998; Kurkov and Loftsson 2013; Bilensoy 2011). In this chapter, the effects of cyclodextrins on drug delivery through biological membranes are discussed with emphasis on dermal and transdermal drug delivery.
1.1 Cyclodextrins and Their Properties
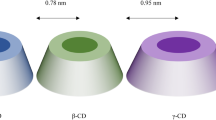
Cyclodextrins are cyclic oligosaccharides containing 6 (αCD), 7 (βCD), 8 (γCD), or more glucopyranose monomers linked via α-1,4-glycoside bonds (Table 14.1). These parent cyclodextrins are natural products formed by microbial degradation of starch. The outer surface of the doughnut-shaped cyclodextrin molecules is hydrophilic, bearing numerous hydroxyl groups, but their central cavity is somewhat lipophilic. Although the parent cyclodextrins and their complexes are hydrophilic, their aqueous solubility is somewhat limited. This is thought to be due to relative strong intermolecular binding in their crystal state. Partial random substitution of the hydroxy groups will result in significant improvements in their solubility (Table 14.1). Cyclodextrins possess many of the same physicochemical and biological properties as their corresponding linear dextrins. In their solid state, cyclodextrins are as stable as starch and can be stored for a number of years at room temperature without any detectable degradation (Szejtli 1988). In aqueous solutions, their degradation follows specific acid-catalyzed hydrolysis of the glycoside bonds to form glucose, maltose, and linear dextrins. In pure aqueous solution, the half-life for ring opening of βCD was determined to be approximately 15 h at pH 1.1 and 70 °C (Hirayama et al. 1992). αCD is somewhat more stable and γCD somewhat less than βCD (Schönberger et al. 1988). Cyclodextrins are stable towards β-amylases, but γCD is degraded by salivary α-amylase (Szejtli 1987; Munro et al. 2004). αCD, βCD, and γCD, as well as their derivatives that are currently used in pharmaceutical products, undergo bacterial digestion in the gastrointestinal tract (Irie and Uekama 1997; Kurkov and Loftsson 2013). Formation of inclusion complexes increases the stability of cyclodextrins, both towards nonenzymatic and enzymatic degradation. There are no reports of transporter-mediated permeation of cyclodextrins across biological membranes, and in general, the oral bioavailability of cyclodextrins is well below 4 % (Kurkov and Loftsson 2013). After parenteral administration, cyclodextrins are, like low-molecular-weight dextrins, mainly excreted unchanged with urine. In humans, their biological half-life is about 1.9 h and volume of distribution about 0.2 L/kg (Kurkov and Loftsson 2013). The safety and toxicology of cyclodextrins have recently been reviewed (Stella and He 2008; Arima et al. 2011).
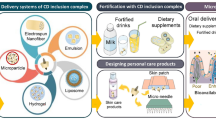
The regulatory status of cyclodextrins is slowly evolving as more and more cyclodextrin-containing products are being approved (Hincal et al. 2011). All three parent cyclodextrins and many of their derivatives can be found in US Pharmacopeia/National Formulary (USP/NF), the European Pharmacopoeia (Ph.EUR.), and the Japanese Pharmaceutical Codex (JPC). The parent cyclodextrins have been included in the “generally recognized as safe” (GRAS) list of the FDA, and they are commonly found in both food and toiletry products throughout the world. Worldwide cyclodextrins can be found in about 40 marketed pharmaceutical products (Loftsson and Brewster 2010; Hincal et al. 2011).
1.2 Cyclodextrin Complexes
Cyclodextrins are able to form drug-cyclodextrin inclusion complexes by taking up somewhat lipophilic drug moieties (or even small lipophilic molecules) into the central cavity (Fig. 14.1). No covalent bonds are formed or broken during the complex formation, and drug molecules bound in the complex are in very dynamic equilibrium with free drug molecules in solution. Thus, cyclodextrin complexes dissociate readily upon simple dilution, for example, upon injection into liquid chromatographic system or after parenteral administration.
The main purpose for adding cyclodextrins to percutaneous drug formulations is to enhance aqueous solubility of poorly soluble drugs and, thus, increase their topical bioavailability. Higuchi and Connors’ phase-solubility method is used to study the effect of cyclodextrin concentrations on drug solubility (Fig. 14.2) (Higuchi and Connors 1965; Loftsson et al. 2005; Loftsson and Hreinsdóttir 2006). The complex formation is a reversible process:
Phase-solubility diagrams. A-type diagrams are due to formation of water-soluble complexes and are usually associated with the water-soluble cyclodextrin derivatives. B-type diagrams indicate formation of poorly soluble complexes that are usually associated with the poorly soluble parent cyclodextrins. S0 is the intrinsic drug solubility, i.e., the solubility of the drug in the complexation media when no cyclodextrin is present
where m drug molecules (D) associate with n cyclodextrin (CD) molecules to form a complex of m:n stoichiometry. K m:n is the observed stability constant of the complex, also known as the binding constant, formation constant, or association constant. The stability constant can be written as follows:
where the brackets denote the molar concentrations. Most commonly, one drug molecule forms a complex with one cyclodextrin molecule:
where, in saturated drug solutions, [D] is the intrinsic solubility of the drug (S 0), i.e., the solubility when no cyclodextrin is present in the aqueous complexation media. The total drug solubility ([D]T) in a given media is then:
assuming 1:1 D/CD complex formation according to Eq. 14.3. A plot of [D]T versus [CD]T for the formation of a 1:1 D/CD complex should give a straight line (i.e., AL-type phase-solubility diagram, Fig. 14.2) with the y-intercept representing S 0 and K 1:1 defined as (Higuchi and Connors 1965):
where Slope is the slope of the linear AL diagram. The slope is always less than unity when 1:1 complex is being formed. Complexes of other stoichiometry are less common (Brewster and Loftsson 2007; Loftsson and Brewster 2010). AP-type profile can indicate formation of a complex that is second or higher order with respect to cyclodextrin or that cyclodextrin complex aggregates (nanoparticles) are being formed. The complexation efficiency (CE) is calculated from the slope of the phase-solubility diagram. It is independent of the intercept (or S 0) and frequently used when the influence of various pharmaceutical excipients on the solubilization is investigated (Loftsson and Brewster 2010, 2012). For 1:1 D/CD complexes, the CE is calculated as follows:
The drug:CD molar ratio in a particular complexation media saturated with the drug can thus be calculated from the CE:
For a more detailed mathematical description of the complex formation, the reader is referred to recent reviews (Brewster and Loftsson 2007; Loftsson and Brewster 2010) and the original publication by Higuchi and Connors (1965). Additionally, the effects of various pharmaceutical excipients on K 1:1 and CE and how they can enhance the solubilizing effects of cyclodextrins have been reviewed (Loftsson and Brewster 2012).
2 Cyclodextrins as Permeability Enhancers
In general, chemical penetration enhancers, such as sulfoxides, fatty acids, fatty acid esters, alcohols, amides, and surfactants, enhance drug permeation into and through the skin by permeating into the skin barrier where they temporarily decrease its barrier properties. These penetration enhancers enhance membrane permeation of both hydrophilic and lipophilic drugs and, in most cases, from both nonaqueous and aqueous vehicles. Studies have shown that the permeation-enhancing properties of cyclodextrins are quite different from these chemical permeation enhancers (Masson et al. 1999; Loftsson and Masson 2001; Loftsson et al. 2004; Dahan et al. 2010; Dahan and Miller 2012; Hymas et al. 2012). For example, only negligible amounts of cyclodextrins are able to permeate intact skin and, thus, they do not directly affect the skin barrier. In one study only 0.02 % of topically applied HPβCD was absorbed into intact hairless mouse skin over 24 h period, whereas 24 % was absorbed into stripped skin where stratum corneum had been removed (Tanaka et al. 1995). Another study showed that only 0.3 % of the more lipophilic dimethyl-β-cyclodextrin was absorbed into intact rat skin after topical application (Gerlóczy et al. 1988). In addition, cyclodextrins are only able to enhance drug permeation from aqueous vehicles and in most cases they are only able to enhance permeation of lipophilic poorly water-soluble drugs (Loftsson et al. 2007b, 2008; Loftsson and Brewster 2011; Loftsson 2012).
There are numerous reports on the effects of cyclodextrins on dermal and transdermal drug delivery (Table 14.2). Depending on the experimental conditions and vehicle composition, cyclodextrins either increase or decrease drug permeation through the skin. Still more studies can be found on the effects of cyclodextrins on drug absorption from the gastrointestinal tract and the buccal cavity through the nasal mucosa as well as through other mucosal membranes, all of which can give us some insight into how cyclodextrins act as penetration enhancers (Loftsson et al. 2007b, 2008; Loftsson and Brewster 2011; Loftsson 2012).
2.1 Theoretical Background
Drugs permeate the skin via passive diffusion. The driving force for passive diffusion through an aqueous vehicle into the skin and then through the skin is the gradient of chemical potential (μ) (Higuchi 1960; Idson 1971). Likewise, the partitioning of drug molecules from the skin exterior into the outermost skin layer is controlled by the chemical potential. High chemical potential of the drug in topical vehicle is a prerequisite for its good dermal bioavailability:
and
where μ 2 is the chemical drug potential in the vehicle, μ θ2 is the chemical potential in a given standard state, a 2 is the thermodynamic drug activity, R is the gas constant, T is the temperature in Kelvin, γ 2 is the activity coefficient, and m 2 is the molality of the drug. The thermodynamic definition of the partition coefficient (K o/w) of a drug between organic (o) and aqueous (w) phases is:
Equation 14.10 states that equilibrium between the two phases is attained when the chemical potential of the drug in one phase (e.g., in water or the aqueous membrane exterior (μ w)) is equal to the chemical potential in the other phase (e.g., the oil phase or the membrane itself (μ o)). Thermodynamic activity is equal to unity in saturated solutions, and, thus, many ointments and creams consist of finely divided drug suspensions. Under such conditions, the vehicle is saturated with drug, and dissolved drug molecules are at their highest potential to leave the vehicle and partition into the skin. Addition of solubilizers, such as cyclodextrins, to an aqueous drug solution will lower the drug activity (i.e., lowers γ w in Eq. 14.10), and, thus, under normal conditions, cyclodextrins lower the potential of the drug to exit the formulation (Másson et al. 2005). However, addition of cyclodextrin to aqueous drug suspension, increasing the amount of dissolved drug while keeping the solution saturated with drug, will not lower the drug activity as long as solid drug is present in the aqueous suspension. Under such condition, the thermodynamic activity (a w in Eq. 14.10) will remain equal to unity, and, thus, dissolved drug molecules are at their highest “exiting” potential, while total amount of dissolved drug is increased. Adding too much cyclodextrin to an aqueous dermal formulation will, on the other hand, decrease the activity (a w) below unity and, consequently, result in less than optimum topical bioavailability. Although passive diffusion is driven by the gradient of chemical potential, it is common to replace it by the concentration gradient. For example, according to Fick’s first law, the driving force for steady-state drug diffusion between two points (i.e., from point 1 to point 2) in a solution is the concentration gradient:
where J is the drug flux, D is the drug diffusion constant, C 1 and C 2 are the drug concentrations at point 1 and point 2, respectively, and h is the distance between the two points.
Most biological membranes are multilayer membrane barriers, and most contain various diffusion pathways and transport systems. Higuchi described passive drug transport through multilayer barriers as series of additive resistances analogous to electric circuits (Higuchi 1960). Later drug permeation through biological membranes was described mathematically as drug permeation through a lipophilic membrane sandwiched between unstirred water layers (UWLs) emphasizing that the UWL must be treated as a part of the total membrane barrier (Zwolinski et al. 1949; Flynn et al. 1972; Flynn and Yalkowsky 1972; Loftsson et al. 2007b). Here a simple two-barrier model will be used to explain how cyclodextrins affect drug permeation from an aqueous vehicle into and through the skin or other biological membranes (Fig. 14.3) (Loftsson and Brewster 2011). In this model, the drug molecules encounter two barriers on their way from the vehicle through a lipophilic membrane. The first one is the aqueous boundary layer at the membrane surface, the UWL. The second one is the lipophilic membrane itself, frequently identified as the outermost layer of the skin, stratum corneum. The total skin barrier towards drug permeation consists of the UWL and the lipophilic membrane. Assuming independent and additive resistances of the two layers, the total drug permeation resistance (R T) of this simple membrane can be defined as:
Drug permeation through a simple two-layer barrier where an unstirred water layer (UWL) forms an aqueous diffusion barrier at the vehicle – skin surface and a skin barrier (stratum corneum) that is a lipophilic membrane barrier. The vehicle contains the dissolved drug; R D, h D, R M, and h M are the resistance and the thickness of the UWL (D) and the membrane (M), respectively. C V is the drug concentration in the vehicle, C D is the drug concentration in the UWL immediate to the membrane surface, C 1 and C 2 are the drug concentrations within the membrane, and K M/D is the drug partition coefficient between the membrane and the UWL
where R D and R M are the drug permeation resistances in the UWL at the exterior and within the lipophilic membrane, respectively. Since the permeability constants (P) are the reciprocals of the resistances, the following equation is obtained assuming sink conditions (i.e., C V – C D ≈ C V and C 1 – C 2 ≈ C 1 in Fig. 14.3):
where J is the drug flux from the aqueous vehicle through the membrane, P T is the overall permeability coefficient, C V is the concentration of the compound in the aqueous vehicle, and P D and P M are the permeability coefficients in the UWL and within the membrane, respectively. Rearranging Eq. 14.13 gives:
If permeation is much slower through the membrane itself than the UWL (i.e., P D > P M), then:
In that case, stratum corneum is the main barrier, and the UWL has negligible effect on the drug permeation through the membrane and can be ignored (i.e., R M > R D). If, on the other hand, permeation through the lipophilic membrane, i.e., the skin itself, is much faster than permeation through the UWL (i.e., P M > P D), then:
In this case, the UWL is the main barrier (i.e., R D > R M), and drug permeation through the membrane becomes aqueous diffusion layer controlled. The relationship between the permeation coefficient (P) and the diffusion coefficient (D) is given by Eq. 14.17:
where h is the thickness of the UWL (h D) or the lipophilic membrane (h M) and K is either the partition coefficient between the membrane and the UWL (K M/D) or equal to unity (i.e., K = 1.00) as in the case of the UWL. Finally, D can be estimated from the Stokes-Einstein equation:
where R is the molar gas constant, T is the absolute temperature, η is the apparent viscosity within the UWL or the lipophilic membrane, r is the radius of the permeating drug molecule, and N is Avogadro’s number. Thus, the diffusion constant within the UWL (D D) will decrease with increasing viscosity of the layer as well as with increasing molecular weight of the drug.
2.2 Cyclodextrins and Biological Membranes
The effects of cyclodextrins on drug permeation through the skin, mucus membranes, and various artificial and biological membranes have been thoroughly reviewed (Matsuda and Arima 1999; Loftsson and Masson 2001; Loftsson et al. 2007b; Cal and Centkowska 2008; Loftsson and Brewster 2011). Based on these studies, some general remarks can be made on how and when cyclodextrins enhance drug delivery into and through biological membranes.
2.2.1 The Drug Molecules Have to Be Released from the Complex
Hydrophilic cyclodextrins and their complexes do not, in general, permeate lipophilic biomembranes (i.e., their K M/D ≈ 0; Fig. 14.3 and Eq. 14.17). The LogK o/w of cyclodextrins that are currently used in pharmaceutical formulations is very low (≤ −6; Table 14.1 and Eq. 14.10), and, thus, these cyclodextrins and their complexes have virtually no tendency to partition from the aqueous exterior into lipophilic membrane. There are no reports of transporter-mediated permeation of cyclodextrins across biological membranes, and in general, the oral bioavailability of cyclodextrins is well below 4 % (Kurkov and Loftsson 2013). Only about 0.02 % of topically applied HPβCD (calculated LogK o/w ≈ −11) is absorbed into intact hairless mouse skin (Tanaka et al. 1995). Consequently, the drug molecules have to be released from the complexes before they can permeate biological membranes (Loftsson and Brewster 2011). Some lipophilic cyclodextrin derivatives are, however, able to penetrate into lipophilic membranes (e.g., the nasal mucosa) and act as conventional chemical penetration enhancers, increasing drug permeation by reducing the lipophilic membrane barrier.
2.2.2 Cyclodextrins Can Prevent Drug Permeation
Cyclodextrins can prevent drug permeation through biological membranes. For example, tablets containing large amounts of αCD (calculated LogK o/w ≈ −13) are used to complex triglycerides in the gastrointestinal tract and prevent their absorption (Comerford et al. 2011; Artiss et al. 2006). Hydrophilic cyclodextrins have been added to sunscreen formulations to reduce absorption of lipophilic sunscreen agents into the skin (Felton et al. 2002, 2004; Sarveiya et al. 2004; Yang et al. 2008). Cyclodextrins, like HPβCD and γCD (calculated LogK o/w ≈ −17), have been used to reduce absorption of the mosquito repellent N,N-diethyl-3-methylbenzamide (DEET) through the skin (Proniuk et al. 2002). Cyclodextrins can likewise be used to decrease dermal and transdermal uptake of sunscreen agents (Cal and Centkowska 2008; Berbicz et al. 2011). The key factor here is to use excess amounts of cyclodextrins in the aqueous vehicle, i.e., more than what is needed to solubilize the poorly soluble lipophilic agent. This is done to reduce the amount of free agent (i.e., drug, mosquito repellent, and sunscreen agent) present in the formulation, thus reducing its partition into the skin. In other words, addition of excess cyclodextrin to the vehicle will lower the potential of the drug to exit the formulation (Eq. 14.10).
2.2.3 Cyclodextrins Only Enhance Drug Permeation from Aqueous Vehicles
In general, cyclodextrins are unable to enhance drug delivery from nonaqueous vehicles through biomembranes but enhance delivery of lipophilic drugs when an aqueous phase is in contact with the lipophilic membrane surface. Hydrophilic cyclodextrins can enhance drug release from hydrophilic creams, i.e., oil-in-water emulsions, but frequently decrease drug release and permeation from lipophilic creams, i.e., water-in-oil emulsions (Preiss et al. 1994, 1995; Loftsson and Brewster 2011). Thus, cyclodextrins can be good permeation enhancers for dermal drug delivery from hydrophilic creams, hydrophilic ointments, hydrophilic gels, aqueous lotions, foams, shampoos, and solutions, but they will most likely have no effect when included in lipophilic creams, hydrophobic ointments, and lipophilic gels. For definition of these pharmaceutical vehicles, see the European Pharmacopoeia, 8th Edition, 2014.
There are few examples where cyclodextrins can enhance drug delivery to the skin from nonaqueous vehicles. Such effects are usually related to increased chemical (e.g., prevention of drug degradation) or physical (e.g., inhabitation of crystal growth) drug stability within the vehicles (Frömming and Szejtli 1994).
2.2.4 Cyclodextrins Do Not Enhance Delivery of Hydrophilic Drugs
In general, hydrophilic water-soluble drugs have little tendency to form hydrophilic cyclodextrin complexes, and, in general, cyclodextrins do not enhance transmembrane delivery of water-soluble drugs. However, cyclodextrins can form complexes with lipophilic moieties of water-soluble drugs, and, thus, in some cases cyclodextrin can reduce topical availability of water-soluble drugs. For example, cyclodextrins form complexes with water-soluble β-blockers (Gagyi et al. 2008), and HPβCD has been shown to reduce ocular bioavailability of the water-soluble β-blocker timolol maleate in aqueous eye drop formulation (Loftsson and Stefánsson 1997). The HPβCD complexation of timolol does increase the hydrophilicity of timolol (i.e., lowers K M/D in Fig. 14.3) and increases the hydrodynamic radius (i.e., r in Eq. 14.18) of the permeating species, both of which will result in lower membrane and transmembrane diffusion of timolol. Few studies have indicated that the somewhat lipophilic methylated cyclodextrins (like RMβCD in Table 14.1) are, under certain conditions, able to act as conventional chemical penetration enhancers, that is, by penetrating into the skin, and decrease its membrane barrier towards drug penetration (Babu and Pandit 2004; Babu et al. 2008).
2.2.5 Cyclodextrins Can Enhance Transmembrane Delivery of Drugs by Increasing Their Chemical Stability
Cyclodextrins are able to increase chemical stability of drugs in aqueous solutions and prevent enzymatic degradation of drugs at aqueous membrane exterior (Loftsson 1995; Loftsson and Brewster 1996, 2010). The enzymatic activity at some mucosal membranes can be quite high, and, thus, the observed permeation enhancement is sometimes due to enhanced drug stability through complexation, especially in the case of proteins and peptides (Irie and Uekama 1997; Loftsson and Brewster 2011).
2.2.6 In Combination with Conventional Penetration Enhancers Cyclodextrins Can Have Additive Effect
Cyclodextrins and conventional penetration enhancers, like fatty acids, or mechanical enhancers, like iontophoresis, can have additive or synergistic effect on drug delivery through biological membranes (Adachi et al. 1992, 1993; Uekama et al. 1992; Loftsson et al. 1998; Sinha et al. 2003; Karandea and Mitragotri 2009). Most often the cyclodextrins increase drug availability at the skin surface, while the other enhancers decrease the membrane barrier itself. In some cases, cyclodextrins increase delivery of a lipophilic penetration enhancer to the skin surface (Adachi et al. 1993). In other cases, cyclodextrin complexation of a penetration enhancer decreases its skin-irritating effect without decreasing its penetration-enhancing property (Martini et al. 1996).
3 Formulation Optimization
In general, stratum corneum is the main barrier towards drug permeation into and across the skin, and the UWL at the skin surface is very thin. Thus, drug permeation from topically applied drug formulations through intact skin most often follows Eq. 14.15. However, under certain conditions, cyclodextrins are able to enhance dermal and transdermal drug delivery. Furthermore, since cyclodextrin complexes tend to self-assemble in aqueous solutions to form nanoparticles, they are known to target drug delivery to the sweat ducts, hair follicles, and sebaceous glands (i.e., drug delivery via shunt route penetration) (Konrádsdóttir et al. 2009).
3.1 When Can Cyclodextrin Help?
Cyclodextrins only enhance drug delivery from aqueous vehicles and only when a UWL presents a barrier towards uptake of drug molecules into the skin. Frequently, dermal formulations contain little or no water (e.g., hydrophobic ointments and lipophilic gels), and sometimes the water domains are not in contact with the skin surface (e.g., in lipophilic creams that consist of water-in-oil emulsions). Under such conditions, the UWL is very thin (h D in Fig. 14.3) and, thus, does not present a barrier (i.e., the skin permeation follows Eq. 14.15). However, many aqueous dermal formulations, such as hydrophilic creams (i.e., oil-in-water emulsions) and hydrophilic gels, increase the thickness of the UWL in which case the resistance of the UWL (R D in Eq. 14.12 and Fig. 14.3) can become comparable or greater than the resistance of stratum corneum (R M in Eq. 14.12 and Fig. 14.3). Under such conditions, cyclodextrins can enhance drug permeation from the surface into the skin. Sweat can also increase the thickness of the UWL between a water-free drug donor, such as dermal patch, and the skin surface (i.e., increasing R D).
Skin damage due to disease or injury can reduce its barrier function (i.e., R M in Eq. 14.12) and increase drug permeation through the skin (i.e., increase P M in Eqs. 14.13 and 14.14). Under such conditions, permeation through UWL might be the main barrier towards dermal and transdermal drug delivery (i.e., P M > P D) in which case the drug flux into and through the skin follows Eq. 14.16, creating conditions where cyclodextrins are known to act as penetration enhancers of lipophilic and poorly water-soluble drugs.
3.2 What Is the Desired Effect?
Most often the aim is to deliver drug molecules from the vehicle into and through the skin. In that case, it is important to include in the vehicle sufficient amount of cyclodextrin to enhance drug delivery to the skin surface and into the skin but to avoid excess amounts. For shunt delivery, the total cyclodextrin concentration, or rather the total concentration of drug-cyclodextrin complexes, has to be sufficient for formation of nanoparticles (Messner et al. 2011; Kurkov and Loftsson 2013). Still in other cases the target is the skin surface itself, and then cyclodextrins can be used to prevent drug partition into the skin adding excess amounts of cyclodextrins to the aqueous vehicle, more than what is needed to solubilize the drug (i.e., excess cyclodextrin lowers the value of K M/D in Eq. 14.17; Fig. 14.3).
3.3 How to Optimize the Formulation?
It is important to optimize cyclodextrin-containing vehicles with regard to the vehicle composition and the desired effect. Too little or too much cyclodextrin will result in less than optimum effect (Loftsson and Brewster 2011). Here we describe step by step the formulation of hydrophilic hydrocortisone gel. The hydrophilic gel (hydrogel) vehicle consists of water within a starch matrix (0.5–2 %) containing HPβCD as a solubilizer/penetration enhancer. Similar methods are used to optimize other aqueous skin preparations.
3.3.1 Phase-Solubility Study
One hydrocortisone molecule (MW 362.5 Da) forms an inclusion complex with one HPβCD molecule (MW 1400 Da). In aqueous solutions, the inclusion complexes are constantly being formed and dissociated at rates close to the diffusion-controlled limit, and, thus, the complexes are in dynamic equilibrium with free hydrocortisone and HPβCD molecules (Fig. 14.1) (Stella et al. 1999). The first step is to determine how much HPβCD is needed to dissolve given amount of hydrocortisone. This is done by determining the phase solubility of the drug in aqueous solution (Higuchi and Connors 1965; Loftsson et al. 2007a; Loftsson and Brewster 2010; Loftsson and Hreinsdóttir 2006). The aqueous solubility of hydrocortisone is determined as the function of HPβCD concentration. From the linear phase-solubility (i.e., AL-type) diagram in Fig. 14.4, we see that we will need about 7 % (w/v) HPβCD to dissolve 10 mg/ml (i.e., 1 % w/v) of hydrocortisone, about 11 % to dissolve 15 mg/ml, and about 14 % to dissolve 20 mg/ml. To calculate the stability constant (K 1:1) and the complexation efficiency (CE), we need to determine the phase-solubility diagram using molar concentrations (Fig. 14.5). From the slope (0.5432), we can determine the CE according to Eq. 14.6 (CE = 1.19) and the hydrocortisone/HPβCD molar ratio in the aqueous HPβCD solution saturated with hydrocortisone from Eq. 14.7 (about 1:2). Thus, in aqueous HPβCD solution at room temperature, at least two HPβCD molecules are needed to dissolve one molecule of hydrocortisone. Then according to Eq. 14.5, we can calculate K 1:1 from the slope and the hydrocortisone solubility in the aqueous complexation media when no HPβCD is present (1.15·10−3 M), the observed K 1:1 = 1,030 M−1.
3.3.2 The Amount of Cyclodextrin and Drug Availability
The starch (e.g., hydroxypropyl cellulose) used to form the matrix might decrease or increase the amount of HPβCD needed to solubilize hydrocortisone (Loftsson and Brewster 2012). However, it can be difficult to determine hydrocortisone solubility in a viscous gel. Alternatively, one can determine the effect of HPβCD concentration on hydrocortisone release. The phase-solubility study shows that about 11 % (w/v) HPβCD will be needed to dissolve 15 mg/ml (1.5 % w/v) hydrocortisone in the hydrophilic gel. To determine the exact amount of HPβCD needed, a series of gels are prepared, all of which contain the same amount of starch and hydrocortisone (1.5 % w/v) but different amounts (5–15 % w/v) of HPβCD, and the hydrocortisone permeation from the gels through an artificial membrane was determined (Fig. 14.6). The membrane consisted of semipermeable cellophane membrane with an octanol/nitrocellulose membrane fused to the receptor side. Only the free drug is able to permeate the octanol layer (Fig. 14.7). Permeation of hydrocortisone molecules from the gel is at its maximum when just enough HPβCD is present to dissolve all hydrocortisone. At lower HPβCD concentration, the permeation is lower, and the gel is turbid due to undissolved hydrocortisone. At higher HPβCD concentrations, the gel is clear, but excess amounts of HPβCD will decrease the concentration of free hydrocortisone at the surface of the lipophilic membrane (Fig. 14.7) resulting in decreased hydrocortisone flux through the membrane. However, to avoid drug precipitation during storage, the gel should contain a small excess of HPβCD. Maximum flux (Fig. 14.6) is obtained at 10 % (w/v) HPβCD. Increasing the concentration to 12 % (w/v) (20 % excess HPβCD) only reduces the flux from 205 to 203 mg h−1 cm−2. The final composition of the hydrophilic gel will then be 1.5 % (w/v) hydrocortisone and 12 % (w/v) HPβCD in a hydrophilic gel.
Effect of HPβCD concentration on the hydrocortisone flux from a hydrophilic gel vehicle through an artificial biomembrane at room temperature (22–23 °C). The membrane consisted of semipermeable cellophane membrane (MWCO 12,000–14,000) with an octanol/nitrocellulose membrane fused to the receptor side. The gel contained fixed amount of hydrocortisone, 1.5 % (w/v). Both free hydrocortisone and the hydrocortisone/HPβCD complex were able to permeate the cellulose membrane, but only the drug was able to permeate the octanol/nitrocellulose membrane
Permeation of hydrocortisone from a hydrophilic gel containing hydrocortisone/HPβCD complex through a cellophane-octanol membrane. HPβCD is very hydrophilic (K M/D = K O/W ≈ 10−11; see Table 14.1) and, thus, is unable to permeate into the octanol membrane, while hydrocortisone is much more lipophilic (K M/D = K O/W ≈ 40) (Másson et al. 2005) and is able to permeate the octanol membrane. The observed K 1:1 = 1,030 M−1
3.3.3 What Happens on the Skin?
The gel contains about 85 % water. The water content of the gel will decrease relatively rapidly after its application to the skin surface, due to both evaporation and water absorption into the skin. However, since hydrocortisone displays AL-type phase-solubility diagram in aqueous HPβCD solutions, decreased amount of water will not result in hydrocortisone precipitation. The gel will become stiffer, and the increased viscosity (η) might decrease hydrocortisone permeation from the gel to the skin surface (see Eq. 14.18), but increased hydrocortisone concentration could, on the other hand, result in increased hydrocortisone permeation. Hence, decreased water content might have less effect than expected.
4 Conclusions
Cyclodextrins can under certain conditions act as percutaneous penetration enhancers. In general, cyclodextrins can only enhance drug delivery through the skin from aqueous vehicles and only when an aqueous diffusion barrier at the skin exterior contributes to the overall skin permeation barrier. Cyclodextrins do not enhance drug penetration from lipophilic vehicles or when the skin barrier, i.e., stratum corneum, is the main permeation barrier. Cyclodextrins are able to prevent drug partition from an aqueous exterior into the skin. It is of uttermost importance to optimize composition of cyclodextrin-containing drug vehicles with regard to drug release and permeation.
References
Adachi H, Irie T, Uekama K, Manako T, Yano T, Saita M (1992) Inhibitory effect of prostaglandin E1 on laurate-induced peripheral vascular occlusive sequelae in rabbits; optimized topical formulation with β-cyclodextrin derivative and penetration enhancer HPE-101. J Pharm Pharmacol 44:1033–1035
Adachi H, Irie T, Uekama K, Manako T, Yano T, Saita M (1993) Combination effects of O-carboxymethyl-O-ethyl-β-cyclodextrin and penetration enhancer HPE-101 on transdermal delivery of prostaglandin-E(1) in hairless mice. Eur J Pharm Sci 1:117–123
Amdidouche D, Montassier P, Poelman MC, Duchene D (1994) Evaluation by laser-doppler velocimetry of the attenuation of tretinoin induced skin irritation by β-cyclodextrin complexation. Int J Pharm 111:111–116
Arima H, Adachi H, Kie T, Uekama K, Pitha J (1990) Enhancement of antiinflammatory effect of ethyl 4-biphenylyl acetate in ointment by β-cyclodextrin derivatives: increased absorption and localized activation of the prodrug in rats. Pharm Res 7:1152–1156
Arima H, Miyaji T, Irie T, Hirayama F, Uekama K (1996) Possible enhancing mechanism of the cutaneous permeation of 4-biphenylylacetic acid by β-cyclodextrin derivatives in hydrophilic ointment. Chem Pharm Bull 44:582–586
Arima H, Motoyama K, Irie T (2011) Recent findings on safety profiles of cyclodextrins, cyclodextrin conjugates, and polypseudorotaxanes. In: Bilensoy E (ed) Cyclodextrins in pharmaceutics, cosmetics, and biomedicine: current and future industrial applications. Wiley, Hoboken, pp 91–122
Artiss JD, Brogan K, Brucal M, Moghaddam M, Jen K-LC (2006) The effects of a new soluble dietary fiber on weight gain and selected blood parameters in rats. Metab Clin Exp 55:195–202
Ascenso A, Vultos F, Ferrinho D, Salgado A, Filho SG, Ferrari V et al (2012) Effect of tretinoin inclusion in dimethyl-beta-cyclodextrins on release rate from a hydrogel formulation. J Incl Phenom Macroc Chem 73:459–465
Babu RJ, Pandit JK (2004) Effect of cyclodextrins on the complexation and transdermal delivery of bupranolol through rat skin. Int J Pharm 271:155–165
Babu RJ, Dhanasekaran M, Vaithiyalingam SR, Singh PN, Pandit JK (2008) Cardiovascular effects of transdermally delivered bupranolol in rabbits: effect of chemical penetration enhancers. Life Sci 82:273–278
Batzdorf T, Mullergoymann CC (1993) Release of ketoprofen from aqueous systems in the presence of hydrophilic β−cyclodextrin derivatives. Pharm Ind 55:857–860
Berbicz F, Nogueira AC, Neto AM, Natali MRM, Baesso ML, Matioli G (2011) Use of photoacoustic spectroscopy in the characterization of inclusion complexes of benzophenone-3-hydroxypropyl-β-cyclodextrin and ex vivo evaluation of the percutaneous penetration of sunscreen. Eur J Pharm Biopharm 79:499–57
Bilensoy E (2011) Cyclodextrins in pharmaceutics, cosmetics, and biomedicine. Current and future industrial applications. Wiley, Hoboken
Bounoure F, Lahiani-Skiba M, Barbot C, Sughir A, Mallet E, Jezequel S et al (2007) Effect of partially methylated β cyclodextrin on percutaneous absorption of metopimazine. J Incl Phenom Macroc Chem 57:191–195
Brewster ME, Loftsson T (2007) Cyclodextrins as pharmaceutical solubilizers. Adv Drug Deliv Rev 59:645–666
Cal K, Centkowska K (2008) Use of cyclodextrins in topical formulations: practical aspects. Eur J Pharm Biopharm 68:467–478
Celebi N, Kislal O, Tarimci N (1993) The effect of β-cyclodextrin and penetration additives on the release of naproxen from ointment bases. Pharmazie 48:914–917
Chang SL, Banga AK (1998) Transdermal iontophoretic delivery of hydrocortisone from cyclodextrin solutions. J Pharm Pharmacol 50:635–640
Chen C-Y, Chen F-A, Wu A-B, Hsu H-C, Kang J-J, Cheng H-W (1996) Effect of hydroxypropyl-β-cyclodextrin on the solubility, photostability and in-vitro permeability of alkannin/shikonin enantiomers. Int J Pharm 141:171–178
Comerford KB, Artiss JD, Jen KLC, Karakas SE (2011) The beneficial effects α-cyclodextrin on blood lipids and weight loss in healthy humans Obesity 19:1200–1204
Dahan A, Miller JM (2012) The solubility-permeability interplay and its implications in formulation design and development for poorly soluble drugs. AAPS J 14:244–251
Dahan A, Miller JM, Hoffman A, Amidon GE, Amidon GL (2010) The solubility–permeability interplay in using cyclodextrins as pharmaceutical solubilizers: mechanistic modeling and application to progesterone. J Pharm Sci 99:2739–2749
Dodziuk H (ed) (2006) Cyclodextrins and their complexes. Wiley-VCH Verlag, Weinheim
Doliwa A, Delgado-Charro B, Santovo S, Ygartua P, Guy RH, (eds) (2000) In vitro iontophoretic delivery of piroxicam from hydroxypropyl-β-cyclodextrin – piroxicam complexes. Proceed. 27th Int'l. Symp. Control. Rel. Bioact. Mater. 7–13 July; Paris: CRS
Doliwa A, Santoyo S, Ygartua P (2001) Influence of piroxicam:hydroxypropyl-beta-cyclodextrin complexation on the in vitro permeation and skin retention of piroxicam. Skin Pharmacol Appl Skin Physiol 14:97–107
Dollo G, Corre PL, Chevanne F, Verge RL (1998) Complexation between local anaesthetics and β-cyclodextrin derivatives – relationship between stability constants and in vitro membrane permeability of bupivacaine and lidocaine from their complexes. STP Pharma Sci 8:189–195
Douhal A (ed) (2006) Cyclodextrin materials photochemistry, photophysics and photobiology. Elsevier, Amsterdam
Felton LA, Wiley CJ, Godwin DA (2002) Influence of hydroxypropyl-β-cyclodextrin on transdermal permeation and skin accumulation of oxybenzone. Drug Devel Ind Pharm 28:1117–1124
Felton LA, Wiley CJ, Godwin DA (2004) Influence of cyclodextrin complexation on the in vivo photoprotective effects of oxybenzone. Drug Devel Ind Pharm 30:95–102
Flynn GL, Yalkowsky SH (1972) Correlation and prediction of mass transport across membranes I: influence of alkyl chain length on flux-determining properties of barrier and diffusant. J Pharm Sci 61:838–852
Flynn GL, Carpender OS, Yalkowsky SH (1972) Total mathematical resolution of diffusion layer control of barrier flux. J Pharm Sci 61:312–314
Frömming KH, Szejtli J (1994) Cyclodextrins in pharmacy. Kluwer Academic Publishers, Dordrecht
Gagyi L, Gyéresi Á, Kilár F (2008) Role of chemical structure in stereoselective recognition of β-blockers by cyclodextrins in capillary zone electrophoresis. J Biochem Biophys Methods 70:1268–1275
Gerlóczy A, Antal S, Szejtli J (1988) Percutaneous absorption of heptakis-(2,6-di-O-14C-methyl)-β-cyclodextrin in rats. In: Huber O, Szejtli J (eds) Proceedings of the fourth international symposium on cyclodextrins. Kluwer Academic Publishers, Dordrecht, pp 415–420
Hedges AR (1998) Industrial applications of cyclodextrins. Chem Rev 98:2035–2044
Hegge AB, Schüller RB, Kristensen S, Tønnesen HH (2008) In vitro release of curcumin from vehicles containing alginate and cyclodextrin. Studies of curcumin and curcuminoides. XXXIII. Pharmazie 63:585–592
Higuchi T (1960) Physical chemical analysis of percutaneous absorption process from creams and ointments. J Soc Cosmet Chem 11(2):85–97
Higuchi T, Connors KA (1965) Phase-solubility techniques. Adv Anal Chem Instrum 4:117–212
Hincal AA, Eroğlu H, Bilensoy E (2011) Regulatory status of cyclodextrins in pharmaceutical products. In: Bilensoy E (ed) Cyclodextrins in pharmaceutics, cosmetic, and biomedicine: current and future industrial applications. Wiley, Hoboken, pp 123–130
Hirayama F, Yamamoto M, Uekama K (1992) Acid-catalyzed hydrolysis of maltosyl-β-cyclodextrin. J Pharm Sci 81:913–916
Hymas RV, Ho NFH, Higuchi WI (2012) Transport of a lipophilic ionizable permeant (capric acid) across a lipophilic membrane (silicone polymer membrane) from aqueous buffered solutions in the presence of hydroxypropyl-β-cyclodextrin. J Pharm Sci 101:2340–2352
Idson B (1971) Biophysical factors in skin penetration. J Soc Cosmet Chem 22:615–634
Iervolino M, Raghavan SL, Hadgraft J (2000) Membrane penetration enhancement of ibuprofen using supersaturation. Int J Pharm 198:229–238
Irie T, Uekama K (1997) Pharmaceutical applications of cyclodextrins. III. Toxicological issues and safety evaluation. J Pharm Sci 86(2):147–162
Karandea P, Mitragotri S (2009) Enhancement of transdermal drug delivery via synergistic action of chemicals. Biochim Biophys Acta 1788:2362–2373
Kawahara K, Ueda H, Tomono K, Nagai T (1992) Effect of diethyl β-cyclodextrin on the release and absorption behaviour of indomethacin from ointment bases. STP Pharma Sci 2:506–513
Kear CL, Yang J, Godwin DA, Felton LA (2008) Investigation into the mechanism by which cyclodextrins influence transdermal drug delivery. Drug Devel Ind Pharm 34:692–697
Klang V, Matsko N, Zimmermann A-M, Vojnikovic E, Valenta C (2010) Enhancement of stability and skin permeation by sucrose stearate and cyclodextrins in progesterone nanoemulsions. Int J Pharm 393:153–161
Klang V, Haberfeld S, Hartl A, Valenta C (2012) Effect of γ-cyclodextrin on the in vitro skin permeation of a steroidal drug from nanoemulsions: impact of experimental setup. Int J Pharm 423:535–542
Konrádsdóttir F, Ogmundsdóttir H, Sigurdsson V, Loftsson T (2009) Drug targeting to the hair follicles: a cyclodextrin based drug delivery. AAPS PharmSciTech 10:266–269
Kurkov SV, Loftsson T (2013) Cyclodextrins. Int J Pharm 453:167–180
Lee BJ, Cui JH, Parrott KA, Ayres JW, Sack RL (1998) Percutaneous absorption and model membrane variations of melatonin in aqueous-based propylene glycol and 2-hydroxypropyl-β-cyclodextrin vehicles. Arch Pharm Res 21:503–507
Legendre JY, Rault I, Petit A, Luijten W, Demuynck I, Horvath S et al (1995) Effects of β-cyclodextrins on skin: implications for the transdermal delivery of piribedil and a novel cognition enhancing-drug, S-9977. Eur J Pharm Sci 3:311–322
Loftsson T (1995) Effects of cyclodextrins on chemical stability of drugs in aqueous solutions. Drug Stab 1:22–33
Loftsson T (2012) Drug permeation through biomembranes: cyclodextrins and the unstirred water layer. Pharmazie 67:363–370
Loftsson T, Bodor N (1994) The pharmacokinetics and transdermal delivery of loteprednol etabonate and related soft steroids. Adv Drug Deliv Rev 14:293–299
Loftsson T, Brewster ME (1996) Pharmaceutical applications of cyclodextrins. 1. Drug solubilization and stabilization. J Pharm Sci 85(10):1017–1025
Loftsson T, Brewster ME (2010) Pharmaceutical applications of cyclodextrins: basic science and product development. J Pharm Pharmacol 62:1607–1621
Loftsson T, Brewster ME (2011) Pharmaceutical applications of cyclodextrins: effects on drug permeation through biological membranes. J Pharm Pharmacol 63:1119–1135
Loftsson T, Brewster ME (2012) Cyclodextrins as functional excipients: methods to enhance complexation efficiency. J Pharm Sci 101:3019–3032
Loftsson T, Duchêne D (2007) Cyclodextrins and their pharmaceutical applications. Int J Pharm 329:1–11
Loftsson T, Hreinsdóttir D (2006) Determination of aqueous solubility by heating and equilibration: a technical note. AAPS PharmSciTech. 7(1): www.aapspharmscitech.org
Loftsson T, Masson M (2001) Cyclodextrins in topical drug formulations: theory and practice. Int J Pharm 225:15–30
Loftsson T, Sigurdardottir AM (1994) The effect of polyvinylpyrrolidone and hydroxypropyl methylcellulose on HPβCD complexation of hydrocortisone and its permeability through hairless mouse skin. Eur J Pharm Sci 2:297–301
Loftsson T, Sigurðardottir AM (1994) The effect of polyvinylpyrrolidone and hydroxypropyl methylcellulose on HPβCD complexation of hydrocortisone and its permeability through hairless mouse skin. Eur J Pharm Sci 2:297–301
Loftsson T, Stefánsson E (1997) Effect of cyclodextrins on topical drug delivery to the eye. Drug Devel Ind Pharm 23:473–481
Loftsson T, Ólafsdóttir BJ, Bodor N (1991) The effects of cyclodextrins on transdermal delivery of drugs. Eur J Pharm Biopharm 37:30–33
Loftsson T, Fridriksdottir H, Ingvarsdottir G, Jonsdottir B, Sigurdardottir AM (1994a) The influence of 2-hydroxypropyl-beta-cyclodextrin on diffusion rates and transdermal delivery of hydrocortisone. Drug Dev Ind Pharm 20(9):1699–1708
Loftsson T, Fridriksdottir H, Ingvarsdóttir G, Jónsdóttir B, Sigurðardottir AM (1994b) The influence of 2-hydroxypropyl-β-cyclodextrin on diffusion rates and transdermal delivery of hydrocortisone. Drug Dev Ind Pharm 20:1699–1708
Loftsson T, Sigurðardóttir AM, Ólafsson JH (1995) Improved acitretin delivery through hairless mouse skin by cyclodextrin complexation. Int J Pharm 115:255–258
Loftsson T, Masson M, Sigurdsson HH, Magnusson P, Goffic FL (1998) Cyclodextrins as co-enhancers in dermal and transdermal drug delivery. Pharmazie 53:137–139
Loftsson T, Brewster ME, Másson M (2004) Role of cyclodextrins in improving oral drug delivery. Am J Drug Deliv 2:261–275
Loftsson T, Hreinsdóttir D, Másson M (2005) Evaluation of cyclodextrin solubilization of drugs. Int J Pharm 302:18–28
Loftsson T, Hreinsdóttir D, Másson M (2007a) The complexation efficiency. J Incl Phenom Macroc Chem 57:545–552
Loftsson T, Vogensen SB, Brewster ME, Konráðsdóttir F (2007b) Effects of cyclodextrins on drug delivery through biological membranes. J Pharm Sci 96:2532–2546
Loftsson T, Sigurðsson HH, Konráðsdóttir F, Gísladóttir S, Jansook P, Stefánsson E (2008) Topical drug delivery to the posterior segment of the eye: anatomical and physiological considerations. Pharmazie 63:171–179
Lopez RFL, Collett JH, Bentley MVLB (2000) Influence of cyclodextrin complexation on the in vitro permeation and skin metabolism of dexamethasone. Int J Pharm 200:127–132
Martini A, Artico R, Civaroli P, Muggetti L, De Ponti R (1996) Critical micellar concentration shifting as a simple tool for evaluating cyclodextrin/enhancer interactions. Int J Pharm 127:239–344
Masson M, Loftsson T, Masson G, Stefansson E (1999) Cyclodextrins as permeation enhancers: some theoretical evaluations and in vitro testing. J Control Rel 59:107–118
Másson M, Sigurdardóttir BV, Matthíasson K, Loftsson T (2005) Investigation of drug-cyclodextrin complexes by a phase-distribution method: some theoretical and practical considerations. Chem Pharm Bull 53:958–964
Matsuda H, Arima H (1999) Cyclodextrins in transdermal and rectal delivery. Adv Drug Deliv Rev 36:81–99
Messner M, Kurkov SV, Brewster ME, Jansook P, Loftsson T (2011) Self-assembly of cyclodextrin complexes: aggregation of hydrocortisone/cyclodextrin complexes. Int J Pharm 407:174–183
Montassier P, Duchene D, Poelman MC (1998) In vitro release study of tretinoin from tretinoin/cyclodextrin derivative complexes. J Inclus Phenom Mol 31:213–218
Munro IC, Newberne PM, Young RR, Bär A (2004) Safety assessment of γ-cyclodextrin. Regul Toxicol Pharmacol 39(Suppl 1):S3–S13
Okamoto H, Komatsu H, Hashida M, Sezaki H (1986) Effects of β-cyclodextrin and di-O-methyl-β-cyclodextrin on the percutaneous absorption of butylparaben, indomethacin and sulfanilic acid. Int J Pharm 30:35–45
Preiss A, Mehnert W, Frömming KH (1994) In-vitro hydrocortisone release from ointments in presence of cyclodextrins. Pharmazie 49:902–906
Preiss A, Mehnert W, Frömming K-H (1995) Penetration of hydrocortisone into excised human skin under the influence of cyclodextrins. Pharmazie 50:121–126
Proniuk S, Liederer BM, Dixon SE, Rein JA, Kallen MA, Blanchard J (2002) Topical formulation studies with DEET (N, N-diethyl-3-methylbenzamide) and cyclodextrins. J Pharm Sci 91:101–110
Sabadini E, Cosgrove T, Egídio FC (2006) Solubility of cyclomaltooligosaccharides (cyclodextrins) in H2O and D2O: a comparative study. Carbohydr Res 341:270–274
Sarveiya V, Templeton JF, Benson HAE (2004) Inclusion complexation of the sunscreen 2-hydroxy-4-methoxy benzophenone (oxybenzone) with hydroxypropyl-β-cyclodextrin: effect on membrane diffusion. J Incl Phenom Macroc Chem 49:275–281
Schönberger BP, Jansen ACA, Janssen LHM (eds) (1988) The acid hydrolysis of cyclodextrins and linear oligosaccharides, a comparative study. 4th Int. Symp. on Cyclodextrins. Kluwe, Munich
Shakory R, Khodabandeh M, Toliyat T, Azimzadeh S, Sadigh Z-A, Badiefar L (2010) Enhancing effect of cyclodextrins on in vitro skin permeation of hGH. Curr Trends Biotechnol Pharm 4:784–790
Sigurdardottir AM, Loftsson T (1995) The effect of polyvinylpyrrolidone on cyclodextrin complexation of hydrocortisone and its diffusion through hairless mouse skin. Int J Pharm 126:73–78
Sinha VR, Bindra S, Kumria R, Nanda A (2003) Cyclodextrin as skin-penetration enhancers. Pharm Technol 27(3):120–138
Stella VJ, He Q (2008) Cyclodextrins. Tox Pathol 36:30–42
Stella VJ, Rao VM, Zannou EA, Zia V (1999) Mechanism of drug release from cyclodextrin complexes. Adv Drug Deliv Rev 36:3–16
Szejtli J (1987) The metabolism, toxicity and biological effects of cyclodextrins. In: Duchêne D (ed) Cyclodextrins and their uses. Editions de Santé, Paris, pp 173–212
Szejtli J (1988) Cyclodextrin technology. Kluwer Academic Publisher, Dordrecht
Szeman J, Ueda H, Szejtli J, Fenyvesi E, Watanabe Y, Machida Y et al (1987) Enhanced percutaneous absorption of homogenized tolnaftate/β-cyclodextrin polymer ground mixture. Drug Design Deliv 1:325–332
Tanaka M, Iwata Y, Kouzuki Y, Taniguchi K, Matsuda H, Arima H et al (1995) Effect of 2-hydroxypropyl-β-cyclodextrin on percutaneous absorption of methyl paraben. J Pharm Pharmacol 47:897–900
Tenjarla S, Puranajoti P, Kasina R, Mandal T (1998) Preparation, characterization, and evaluation of miconazole-cyclodextrin complexes for improved oral and topical delivery. J Pharm Sci 87:425–429
Uekama K, Otagiri M, Sakai A, Irie T, Matsuo N, Matsuoka Y (1985) Improvement in the percutaneous absorption of beclomethasone dipropionate by γ-cyclodextrin complexation. J Pharm Pharmacol 37:532–535
Uekama K, Arimori K, Sakai A, Masaki K, Irie T, Otagiri M (1987) Improvement of percutaneous absorption of prednisolone by β- and γ-cyclodextrin complexations. Chem Pharm Bull 35:2910–2913
Uekama K, Adachi H, Irie T, Yano T, Saita M, Noda K (1992) Improved transdermal delivery of prostaglandin E1 through hairless mouse skin: combined use of carboxymethyl-ethyl-β-cyclodextrin and penetration enhancers. J Pharm Pharmacol 44:119–121
Uekama K, Hirayama F, Arima H (2006) Pharmaceutical applications of cyclodextrins and their derivatives. In: Dodziuk H (ed) Cyclodextrins and their complexes. Chemistry, analytical methods, applications. Wiley-VCH Verlag, Weinheim, pp 381–422
Ventura CA, Tommasini S, Falcone A, Giannone I, Paolino D, Sdrafkakis V et al (2006) Influence of modified cyclodextrins on solubility and percutaneous absorption of celecoxib through human skin. Int J Pharm 314:37–45
Vollmer V, Müller BW, Mesens J, Wilffert B, Peters T (1993) In vivo skin pharmacokinetics of liarozole: percutaneous absorption studies with different formulations of cyclodextrin derivatives in rats. Int J Pharm 99:51–58
Yang J, Wiley CJ, Godwin DA, Felton LA (2008) Influence of hydroxypropyl-β-cyclodextrin on transdermal penetration and photostability of avobenzone. Eur J Pharm Biopharm 69:605–612
Yuzuriha S, Matsuo K, Noguchi M (1999) Topical application of prostaglandin E1 ointment to cutaneous wounds in ischemic rabbit ears. Eur J Plastic Surg 22:225–229
Zi P, Yang X, Kuang H, Yang Y, Yu L (2008) Effect of HPβCD on solubility and transdermal delivery of capsaicin through rat skin. Int J Pharm 358:151–158
Zwolinski BJ, Eyring H, Reese CE (1949) Diffusion and membrane permeability. I. J Phys Coll Chem 53:1426–1453
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Loftsson, T. (2015). Formulation of Drug-Cyclodextrin Complexes. In: Dragicevic, N., Maibach, H. (eds) Percutaneous Penetration Enhancers Chemical Methods in Penetration Enhancement. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-45013-0_14
Download citation
DOI: https://doi.org/10.1007/978-3-662-45013-0_14
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-45012-3
Online ISBN: 978-3-662-45013-0
eBook Packages: MedicineMedicine (R0)