Abstract
The first successful hysteroscopy was reported by Pantaleoni in 1869. In the last two decades, technical developments led to major improvements in diagnostic hysteroscopy and hysteroscopic surgery. Diagnostic hysteroscopy is currently the “gold standard” investigation of diseases involving the uterine cavity (Fraser 1993; Nagele et al. 1996) and hysteroscopic surgery is currently the standard treatment of intrauterine pathology, such as endometrial polyps (Polena et al. 2005; Preutthipan and Herabutya 2005; Savelli et al. 2003), submucous fibroids (Rosati et al. 2008; Timmermans and Veersema 2005), uterine septa (Colacurci et al. 2002; Perino et al. 1987) and intrauterine adhesions (Al-Inany 2001). Appropriate instrumentation, together with distension media like CO2, saline and nonsaline solutions are of vital importance in hysteroscopic procedures.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
2.1 Introduction
The first successful hysteroscopy was reported by Pantaleoni in 1869. In the last two decades, technical developments led to major improvements in diagnostic hysteroscopy and hysteroscopic surgery. Diagnostic hysteroscopy is currently the “gold standard” investigation of diseases involving the uterine cavity (Fraser 1993; Nagele et al. 1996) and hysteroscopic surgery is currently the standard treatment of intrauterine pathology, such as endometrial polyps (Polena et al. 2005; Preutthipan and Herabutya 2005; Savelli et al. 2003), submucous fibroids (Rosati et al. 2008; Timmermans and Veersema 2005), uterine septa (Colacurci et al. 2002; Perino et al. 1987) and intrauterine adhesions (Al-Inany 2001). Appropriate instrumentation, together with distension media like CO2, saline and nonsaline solutions are of vital importance in hysteroscopic procedures.
2.2 Diagnostic Hysteroscopy
Diagnostic hysteroscopy can be carried out as an outpatient procedure, taking only a few minutes, with success rates up to 98 % (Wieser et al. 1998). Outpatient hysteroscopy saves the patients’ inconvenience, cost, undue stress and concern. Further advantages of outpatient hysteroscopy include its safety, expeditious performance, and high diagnostic accuracy (Glasser 2009).
An additional advantage above other diagnostic options for the uterine cavity (ultrasound, sonohysterography, MRI) is the possibility of performing therapeutic interventions in the same session in appropriate cases and situations.
2.2.1 Distension Medium in Hysteroscopy
The most commonly used distension media in hysteroscopy is saline. Saline is equal (Litta et al. 2003; Shankar et al. 2004) or better (Pellicano et al. 2003) in terms of patient discomfort and satisfaction and provides a superior view to CO2, as bubbles and bleeding impede the view more often when CO2 is used (Litta et al. 2003; Shankar et al. 2004; Pellicano et al. 2003). If the choice is made to convert to a see-and-treat procedure, saline has the advantage of compatibility with bipolar equipment allowing for immediate treatment. It is not advisable to use nonelectrolytic distension fluids (e.g. glycine 1.5 %, sorbitol-mannitol) associated with monopolar equipment, as these are limited to shorter use due to a higher risk of hyponatremia and brain edema (Istre et al. 1994).
2.2.2 Instruments for Hysteroscopy
-
1.
Rigid 3.5–5.5 mm endoscope (Agdi and Tulandi 2009)
Distension medium: saline
-
2.
Office Continuous Flow Hysteroscope (Karl Storz GmbH, Tuttlingen, Germany; Olympus Surgery Technologies Europe GmbH, Hamburg, Germany; Richard Wolf GmbH, Knittlingen, Germany, etc.). Based on 1.9–3.0 mm rod lens systems with an outer diameter of 4.0–5.5 mm.
Equipped with or without an operative 5-Fr canal (multiple 5-Fr mechanical instruments and 5-Fr bipolar electrodes are available) (Bettocchi et al. 2003).
-
3.
Versascope (Gynecare division of Johnson & Johnson). 3.5 mm endoscope with a disposable sheath containing a collapsed working channel (5–7 Fr), which is distended during introduction of an instrument.
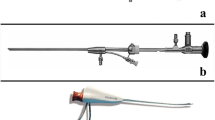
2.2.2.1 Rigid Versus Flexible Hysteroscopes
There are two different hysteroscope systems on the market: rigid and flexible hysteroscopes. The diameter of flexible hysteroscopes is smaller than that of rigid hysteroscopes and their rounded tip allows it to bend according to need, but rigid endoscopes have superior optical quality as the fiber optic pattern is clearly seen with the flexible hysteroscopes. Although more pain is associated with the “bigger” diameter rigid hysteroscopes, this is well compensated by the superior optical quality allowing for faster examination (on average 50s less (>70 %)) (Unfried et al. 2001) at higher success rates (100 % versus 87.5 %) (Unfried et al. 2001), and at a lower price than flexible endoscopes.
2.2.3 Tricks for Hysteroscopic Insertion
-
1.
Rotate the scope 90°
The internal cervical os is oval shaped with a diameter of approximately 4–5 mm. The “new” small-diameter hysteroscopes imitate this oval profile keeping the total diameter between 4 and 5 mm. Rotate the scope 90° on the endo-camera to align the longitudinal axis of the scope with the transverse axis of the internal cervical os. Doing so facilitates a painless entry (Bettocchi et al. 2003).
-
2.
Keep the cervical canal in the lower half of the screen
If you look through a hysteroscope the view is deflected by 12–30° (depending on the scope). In this way the structures in the middle of the screen are actually positioned 12–30° lower. To ensure a painless entry keep the cervical canal in the lower half of the screen during insertion. In this way the scope will be located in the middle of the canal, avoiding stimulation of the muscle fibers (Bettocchi et al. 2003).
-
3.
Use 30° lenses
For a correct examination of the uterine cavity and to reduce patient discomfort it is advisable to use 30° lenses. If the tip of the scope is placed 1–1.5 cm from the fundus, a view of the whole cavity and tubal ostiae can be gained by rotating the instrument on its axis, without any other lateral movement of the scope being required, which might cause pain to the patient (Bettocchi et al. 2003).
2.3 Hysteroscopic Surgery
Hysteroscopic surgery is now widely used to treat a variety of intrauterine diseases. In the scope of this article we discuss the instrumentation used for the following pathology: intrauterine synechiae, polyps and myoma, and the uterine septum followed by the hysteroscopic techniques used for ablation of the endometrium.
2.3.1 View Angle of the Telescope
The angle of the telescope on the resectoscope is usually 12° to always keep the loop within the viewing field (Mencaglia et al. 2009). By using a wider field of vision some companies offer resectoscopes with 0° or 30°, but care has to be taken to use these dedicated scopes that cannot be changed with just any other in order to avoid the above-mentioned viewing problems.
2.3.2 Distension Media in Hysteroscopic Surgery
The choice of the distension medium in hysteroscopic surgery depends on the type of equipment used. In the first days of hysteroscopic surgery only nonelectric/mechanical or monopolar equipment was available and mainly hypotonic, electrolyte-free solutions were used to distend the uterine cavity. These solutions, when absorbed in large volumes, potentially cause hyponatremia and hypervolemia leading to neurotoxic coma or even death. In 1999 the first bipolar resectoscope was introduced (Loffer 2000). Bipolar systems show an improved safety profile through the use of physiological saline (contains electrolytes, 0.9 % NaCl), which prevents the drop in serum sodium associated with nonelectrolytic solutions used with monopolar equipment (Berg et al. 2009). The electrical current passes through multiple tissues before its return to the generator in the monopolar technique, in the bipolar technique the electrical current is restricted between the two loops of the electrode, thereby decreasing electrical/thermal injury to adjacent tissues. The “plasma effect” makes the bipolar more effective than the monopolar system. With bipolar equipment the generator produces a high initial voltage spike that establishes a voltage gradient in a gap between the bipolar electrodes. When the activated bipolar electrode is not in contact with the tissue, the electrolyte solution in the uterus dissipates it. When the loop is sufficiently close to tissue, the high bipolar voltage spike arc between the electrodes converts the conductive sodium chloride solution into a nonequilibrium vapor layer or “plasma effect.” Once formed, this plasma effect can be maintained at lower voltages (Mencaglia et al. 2009). This suggests bipolar equipment to be superior to monopolar equipment, however current data show no differences in terms of safety and effectiveness (Garuti and Luerti 2009).
2.4 Intrauterine Synechiae
2.4.1 Instruments for Hysteroscopic Adhesiolysis
-
1.
5-F mechanical instrument (office hysteroscope) equipped with hysteroscopic scissors (Karl Storz GmbH, Tuttlingen, Germany; Olympus Surgery Technologies Europe GmbH, Hamburg, Germany; Richard Wolf GmbH, Knittlingen, Germany; Gynecare Johnson & Johnson Versascope) (Pabuccu et al. 2008).
Distension medium: saline
-
2.
A 7–9 mm working element along with sheath and 4 mm 30° telescope (Karl Storz GmbH, Tuttlingen, Germany; Olympus Surgery Technologies Europe GmbH, Hamburg, Germany; Richard Wolf GmbH, Knittlingen, Germany; Gynecare Johnson & Johnson) equipped with a hysteroscopic monopolar or bipolar (Collin’s) knife (Roy et al. 2010). A monopolar or bipolar loop could also be used, but is less versatile due to the fact that more working space is needed.
Distension medium: glycine (1.5 %) or saline resp.
-
3.
Versapoint Twizzle bipolar electrode (Gynecare Johnson & Johnson).
Distension medium: saline.
2.4.2 Diagnosis
Hysteroscopy.
2.4.3 Discussion
The use of hysteroscopic scissors avoids the possibility of energy-related damage to the endometrium. However, several studies have reported successful outcomes of adhesiolysis by using electrosurgery, which suggests that with proper application significant damage is unlikely (Cararach et al. 1994; Chervenak and Neuwirth 1981; Decherney and Polan 1983). Electrosurgery has the advantage over scissors by achieving better hemostasis, thus providing an improved optical clarity of the operative field (Yu et al. 2008).
2.5 Uterine Septum
2.5.1 Instruments for Metroplasty
-
1.
26 F resectoscope fitted with monopolar or bipolar 90° knife electrode and with a 0–12° telescope (Karl Storz GmbH, Tuttlingen, Germany; Olympus Surgery Technologies Europe GmbH, Hamburg, Germany; Richard Wolf GmbH, Knittlingen, Germany; Ethicon Gynecare Inc., Johnson & Johnson) (Colacurci et al. 2007).
Distension medium: sorbitol, mannitol, saline
-
2.
Continuous flow small-diameter hysteroscope (maximum diameter 5 mm) (Karl Storz GmbH, Tuttlingen, Germany; Olympus Surgery Technologies Europe GmbH, Hamburg, Germany; Richard Wolf GmbH, Knittlingen, Germany; Ethicon Gynecare Inc., Johnson & Johnson) fitted with a 0–30° telescope of 1.9–2.9 mm caliber equipped with a 1.6 mm single-fiber, twizzle-tip electrode passed through the 5 F working channel of the hysteroscope and connected with an electrosurgical generator (Versapoint Bipolar System) (Colacurci et al. 2007).
Distension medium: saline
2.5.2 Background
To date, many data are available regarding the treatment of septate uterus performed by means of a traditional 26 F resectoscope fitted with a unipolar knife requiring nonelectrolytic solutions to distend the uterine cavity. Despite the excellent results, this technique was associated with serious complications such as mechanical trauma to the cervix, thermal injuries and fluid intravasation. In recent years technological improvements have led to the introduction of small-diameter hysteroscopes not exceeding 5 mm in diameter fitted with bipolar electrodes that work in saline solution, which allow simple and safe treatment of many intrauterine diseases, thus reducing the risk of severe complications.
The efficacy on reproductive outcome after metroplasty has never been proven in randomized controlled trials. A similar multicenter trial is now being performed in several centers in the Netherlands50.
2.5.3 Diagnosis
Three-dimensional ultrasound.

Uterine septum
2.5.4 Conclusion
No difference is seen with regard to reproductive outcome between both electrosurgical techniques mentioned before, so the choice of technique depends on the cost of instrumentation, operating time, and rate of complication. The resectoscopes offer that advantage of no requirement for disposable or specific equipments because the unipolar electrosurgery unit is usually available in most operating rooms and also nonexpensive and readily feasible. On the other hand, because of the shorter operating time, the easier feasibility, the lower incidence of complications, and the general improved safety, in experienced hands the small-diameter hysteroscope technique is a valuable and valid alternative to resectoscopy and should be preferred for the septate uterus class Vb (Colacurci et al. 2007).
2.5.5 Instruments for Polypectomy and Myomectomy
-
1.
Outpatient setting: a 1.9–3 mm rigid optic with 0, 12° or 30° fore oblique lens and an outer sheath executed with a 5-french operating channel and continuous flow, with a maximum diameter of 4.5–5.5 mm. Equipped with either a graper forceps or scissors (mechanically), with bipolar electrodes (electrosurgical) (Van et al. 2009), an intrauterine morcellator (Smith & Nephew Trueclear® or Hologic Myosure® system) or with a polypsnare (Cook) (Timmermans and Veersema 2005).
-
2.
Day case setting: a continuous flow operative hysteroscope (Karl Storz GmbH, Tuttlingen, Germany; Olympus Surgery Technologies Europe GmbH, Hamburg, Germany; Richard Wolf GmbH, Knittlingen, Germany; Ethicon Gynecare Inc., Johnson & Johnson or Smith and Nephew, Andover, MA, USA) with a 7- or 9-mm operative sheath and a 0° or 12° optic. Equipped with either a mechanical device (intrauterine morcellator: Smith & Nephew or Hologic Myosure®, scissors or forceps) or electrosurgical device (monopolar or bipolar electrodes) (Van et al. 2009).
-
3.
Resectoscopes:
-
(a)
TCRis resectoscope (Olympus Surgery Technologies Europe GmbH, Hamburg), ch. 26 model WA 22061 with 12 optic 22001A with various loop sizes and types. Dedicated electrogenerator.
-
(b)
Gynecare 9 mm resectoscope with Versapoint loop (Ethicon Gynecare Inc., Johnson & Johnson), various loop sizes. Dedicated electrogenerator.
-
(c)
Storz bipolar resectoscope (Karl Storz GmbH, Tuttlingen, Germany).
-
(d)
Wolf Princess bipolar and monopolar 7 mm resectoscope or Wolf Resection Master with automatic chip aspiration (Richard Wolf GmbH, Knittlingen, Germany).
all using NaCl 0.9 % (Braun) as irrigant (Berg et al. 2009).
-
(a)
Resection of polyp with the loop resectoscope
Resection of fibroid with the loop resectoscope
2.5.6 Background
There are many different resectoscopes available for treatment of endometrial polyps and fibroids. The current standard of treatment is resectoscopic surgery under general or epidural anesthesia. Marketing of small-diameter operative hysteroscopes, uterine distention by liquid delivered at controlled pressure, visualization supported by videocamera, and the vaginoscopic approach rendered hysteroscopic polypectomy toward a one-stop diagnostic and therapeutic step, safely and effectively accomplished in an office setting (Bettocchi et al. 2002; Garuti et al. 2004; Sesti et al. 2000).
2.5.7 Diagnosis
Transvaginal ultrasound, saline infusion sonography, diagnostic hysteroscopy.
Transvagial ultrasound
2.5.8 Discussion
Mechanical or electrosurgical outpatient polypectomy is equally safe and effective and does not differ in terms of operating time or induced pelvic discomfort (Garuti et al. 2008). Bipolar electrodes appear to have a safer profile compared with monopolar electrodes because of the unchanged serum sodium (Berg et al. 2009). Small versus big loops. A smaller loop will cut more superficially and remove a smaller amount of tissue. Subsequently, it may be necessary to resect twice at the same level to remove the basal layer, and this may increase operating time (Berg et al. 2009).
The differences between the various systems for the resection of fibroids need further evaluation (efficacy, speed, safety), although the learning curve seems to be shorter for mechanical myomectomy (van Dongen et al. 2008) and therefore this technique might be more appropriate for less experienced physicians.
2.5.9 Instruments for Hysteroscopic Endometrial Ablation
-
1.
9 mm (Perez-Medina et al. 2002)/26Fr (Gupta et al. 2006) resectoscope (Karl Storz GmbH & Co., Tuttlingen, Germany) equipped with a 4 mm cutting loop.
Distension medium: Glycine 1.5 % for monopolar or saline for bipolar surgery
-
2.
Rollerball electrodes, available in 2.5 and 5 mm (Chang et al. 2009).
Distension medium: Glycine 1.5 %
-
3.
Weck-Baggish hysteroscope (Weck; ER Squibb and Sons, New York, NY)
Equipped with a Neodynium:Yttrium-Aluminium Garnet (Nd-YAG)
(Surgical Laser Technology, Malvern, PA) (Garry et al. 1995; Shankar et al. 2003).
Distension medium: saline
2.5.10 Background
There are two techniques of endometrial resection/ablation: hysteroscopic guided or first-generation endometrial ablation and nonhysteroscopic second-generation endometrial ablation. The first-generation endometrial ablation techniques are considered the gold standard for endometrial ablation, these techniques include transcervical endometrial resection by resectoscope, rollerball electrocoagulation and laser ablation (Papadopoulos and Magos 2007). Second-generation endometrial techniques include thermal balloon ablation, microwave endometrial ablation, hydrotherm ablation, electrode ablation, and cryoablation (Overton et al. 1997). In experienced hands, a significant difference in efficacy between first and second-generation ablation techniques for the treatment of heavy menstrual bleeding has not been found. Second-generation techniques however are less operator-dependent, easier and appear to have a lower complication rate (van Dongen et al. 2008).
2.5.11 Description of the First-Generation Techniques
2.5.11.1 Loop Endometrial Resection
Bipolar continuous flow resectoscopes provide an effective resection of the endometrium and underlying superficial myometrium. This technique can still be used when the endometrium is not pharmacologically or mechanically prepared (Papadopoulos and Magos 2007).
2.5.11.2 Laser Ablation
The Nd-YAG laser is a fiber laser with a tissue penetration of 5–6 mm. This renders him very suitable for intrauterine surgery. The power settings for the laser generator are usually between 40 and 80 W giving a power density of 4,000–6,000 W/cm2 (Baggish and Sze 1996).
Two techniques are used for laser ablation. The first technique is described by Goldrath and is known as the dragging technique. Tissue vaporization is created by keeping the laser fiber in contact with the endometrium (Goldrath et al. 1981). The second technique is known as the blanching technique and involves no contact of the laser fiber with the endometrium. There is no consensus as to which technique is superior, but most important is to keep the distal tip of the laser fiber always in view and to move it rapidly enough to avoid excessive coagulation and resultant thermal necrosis of the full thickness of the uterine wall or extrauterine structures (Papadopoulos and Magos 2007).
2.5.11.3 Rollerball Endometrial Ablation
The rollerball electrocoagulates the endometrium to a depth of just under 4 mm (Duffy et al. 1992). The mainly used cutting current is 120 W at a setting of blend 1. To ensure deep enough tissue destruction, the rollerball should be moved slowly over the endometrium. The optimum speed is reached when a white halo of desiccated tissue appears in front of the rollerball. If you move too fast, the endometrium will not turn white. Conversely, too slow increases the risk for uterine perforation. Keep the rollerball clean, as debris adherent to it will act as an insulator resulting in suboptimal outcome (Papadopoulos and Magos 2007).
2.5.11.4 Vaporization Systems
A similar effect as described under rollerball endometrial ablation is reached by vaporization techniques, which produce tissue destruction through vaporization rather than by desiccation:
-
0° Vaporization Electrode (Versapoint generator, Johnson & Johnson Gynecare)
-
“Mushroom” bipolar vaporizing electrode (TCRis generator Olympus).
Both systems have the advantage of increased safety through bipolar electrosurgery with saline as distension medium (see Uterine septum).
2.5.11.5 Combined Cutting Loop Resection and Rollerball Ablation
Various authors use a combination of a cutting loop and a rollerball for endometrial ablation. The rollerball is used at the fundus and cornual or angular areas and the loop at the walls of the uterus (Cooper et al. 1999; Litta et al. 2006; Perino et al. 2004; Rosati et al. 2008).
2.5.12 Diagnosis
Transvaginal ultrasound, office hysteroscopy, and endometrial biopsy (Gupta et al. 2006; Litta et al. 2006; Perino et al. 2004; Rosati et al. 2008).
2.5.13 Discussion
Studies showed no significant difference in menstrual improvement and patient satisfaction for the three different first-generation techniques (Papadopoulos and Magos 2007). Loop resection provides tissue for histology and is suitable even when endometrium is thick, but requires the most skill and therefore bares the greatest risk of uterine perforation. The rollerball is easier to learn and faster than the laser, but it provides no tissue for histology and fails to treat submucous fibroids. The laser can vaporize small fibroids and polyps, but is the most expensive and slowest of all three techniques (Papadopoulos and Magos 2007). Therefore, the choice of technique should depend on the operator’s preference.
Although glycine 1.5 % has been used traditionally for resectoscopic procedures, alternative-irrigating solutions should now be actively sought. Moreover, the data available motivate cautious monitoring of the inflow pressure applied and the fluid absorption during transcervical resectoscopic surgery.
New hysteroscopes and resectoscopes with continuous flow designs have greatly facilitated diagnostic and therapeutic hysteroscopy. Saline is the ideal distending medium for hysteroscopic procedures in which mechanical or bipolar instruments are used; Regardless of the medium chosen, careful fluid monitoring is essential.
References
Agdi M, Tulandi T (2009) Outpatient hysteroscopy with combined local intracervical and intrauterine anesthesia. Gynecol Obstet Invest 69:30–32
Al-Inany H (2001) Intrauterine adhesions. An update. Acta Obstet Gynecol Scand 80:986–993
Baggish MS, Sze EH (1996) Endometrial ablation: a series of 568 patients treated over an 11-year period. Am J Obstet Gynecol 174:908–913
Berg A, Sandvik L, Langebrekke A, Istre O (2009) A randomized trial comparing monopolar electrodes using glycine 1.5 % with two different types of bipolar electrodes (TCRis, Versapoint) using saline, in hysteroscopic surgery. Fertil Steril 91:1273–1278
Bettocchi S, Ceci O, Di VR, Pansini MV, Pellegrino A, Marello F, Nappi L (2002) Advanced operative office hysteroscopy without anaesthesia: analysis of 501 cases treated with a 5 Fr. bipolar electrode. Hum Reprod 17:2435–2438
Bettocchi S, Nappi L, Ceci O, Selvaggi L (2003) What does ‘diagnostic hysteroscopy’ mean today? The role of the new techniques. Curr Opin Obstet Gynecol 15:303–308
Cararach M, Penella J, Ubeda A, Labastida R (1994) Hysteroscopic incision of the septate uterus: scissors versus resectoscope. Hum Reprod 9:87–89
Chang PT, Vilos GA, Abu-Rafea B, Hollett-Caines J, Abyaneh ZN, Edris F (2009) Comparison of clinical outcomes with low-voltage (cut) versus high-voltage (coag) waveforms during hysteroscopic endometrial ablation with the rollerball: a pilot study. J Minim Invasive Gynecol 16:350–353
Chervenak FA, Neuwirth RS (1981) Hysteroscopic resection of the uterine septum. Am J Obstet Gynecol 141:351–353
Colacurci N, De FP, Fornaro F, Fortunato N, Perino A (2002) The significance of hysteroscopic treatment of congenital uterine malformations. Reprod Biomed Online 4(Suppl 3):52–54
Colacurci N, De FP, Mollo A, Litta P, Perino A, Cobellis L, De PG (2007) Small-diameter hysteroscopy with Versapoint versus resectoscopy with a unipolar knife for the treatment of septate uterus: a prospective randomized study. J Minim Invasive Gynecol 14:622–627
Cooper KG, Bain C, Parkin DE (1999) Comparison of microwave endometrial ablation and transcervical resection of the endometrium for treatment of heavy menstrual loss: a randomised trial. Lancet 354: 1859–1863
Decherney A, Polan ML (1983) Hysteroscopic management of intrauterine lesions and intractable uterine bleeding. Obstet Gynecol 61:392–397
Duffy S, Reid PC, Sharp F (1992) In-vivo studies of uterine electrosurgery. Br J Obstet Gynaecol 99:579–582
Fraser IS (1993) Personal techniques and results for outpatient diagnostic hysteroscopy. Gynecol Endosc 2:29–33
Garry R, Shelley-Jones D, Mooney P, Phillips G (1995) Six hundred endometrial laser ablations. Obstet Gynecol 85:24–29
Garuti G, Luerti M (2009) Hysteroscopic bipolar surgery: a valuable progress or a technique under investigation? Curr Opin Obstet Gynecol 21:329–334
Garuti G, Cellani F, Colonnelli M, Grossi F, Luerti M (2004) Outpatient hysteroscopic polypectomy in 237 patients: feasibility of a one-stop “see-and-treat” procedure. J Am Assoc Gynecol Laparosc 11:500–504
Garuti G, Centinaio G, Luerti M (2008) Outpatient hysteroscopic polypectomy in postmenopausal women: a comparison between mechanical and electrosurgical resection. J Minim Invasive Gynecol 15:595–600
Glasser MH (2009) Practical tips for office hysteroscopy and second-generation “global” endometrial ablation. J Minim Invasive Gynecol 16:384–399
Goldrath MH, Fuller TA, Segal S (1981) Laser photovaporization of endometrium for the treatment of menorrhagia. Am J Obstet Gynecol 140:14–19
Gupta B, Mittal S, Misra R, Deka D, Dadhwal V (2006) Levonorgestrel-releasing intrauterine system vs. transcervical endometrial resection for dysfunctional uterine bleeding. Int J Gynaecol Obstet 95:261–266
Istre O, Bjoennes J, Naess R, Hornbaek K, Forman A (1994) Postoperative cerebral oedema after transcervical endometrial resection and uterine irrigation with 1.5 % glycine. Lancet 344:1187–1189
Kowalik CR, Mol BW, Veersema S, Goddijn M (2010). Critical appraisal regarding the effect on reproductive outcome of hysteroscopic metroplasty in patients with recurrent miscarriage. Arch Gynecol Obstet 282(4):465
Kowalik CR, Goddijn M, Emanuel MH, Bongers MY, Spinder T, de Kruif JH, Mol BW, Heineman MJ (2011). Metroplasty versus expectant management for women with recurrent miscarriage and a septate uterus. Cochrane Database Syst Rev 6:CD008576. Review
Litta P, Bonora M, Pozzan C, Merlin F, Sacco G, Fracas M, Capobianco G, Dessole S (2003) Carbon dioxide versus normal saline in outpatient hysteroscopy. Hum Reprod 18:2446–2449
Litta P, Merlin F, Pozzan C, Nardelli GB, Capobianco G, Dessole S, Ambrosini A (2006) Transcervical endometrial resection in women with menorrhagia: long-term follow-up. Eur J Obstet Gynecol Reprod Biol 125:99–102
Loffer FD (2000) Preliminary experience with the VersaPoint bipolar resectoscope using a vaporizing electrode in a saline distending medium. J Am Assoc Gynecol Laparosc 7:498–502
Mencaglia L, Lugo E, Consigli S, Barbosa C (2009) Bipolar resectoscope: the future perspective of hysteroscopic surgery. Gynecol Surg 6:15–20. http://springerlink.bibliotecabuap.elogim.com/search?query=mencaglia&search-within=Journal&facet-journal-id=10397.
Nagele F, O’Connor H, Davies A, Badawy A, Mohamed H, Magos A (1996) 2500 Outpatient diagnostic hysteroscopies. Obstet Gynecol 88:87–92
Overton C, Hargreaves J, Maresh M (1997) A national survey of the complications of endometrial destruction for menstrual disorders: the MISTLETOE study. Minimally Invasive Surgical Techniques–Laser, EndoThermal or Endoresection. Br J Obstet Gynaecol 104:1351–1359
Pabuccu R, Onalan G, Kaya C, Selam B, Ceyhan T, Ornek T, Kuzudisli E (2008) Efficiency and pregnancy outcome of serial intrauterine device-guided hysteroscopic adhesiolysis of intrauterine synechiae. Fertil Steril 90:1973–1977
Papadopoulos NP, Magos A (2007) First-generation endometrial ablation: roller-ball vs loop vs laser. Best Pract Res Clin Obstet Gynaecol 21:915–929
Pellicano M, Guida M, Zullo F, Lavitola G, Cirillo D, Nappi C (2003) Carbon dioxide versus normal saline as a uterine distension medium for diagnostic vaginoscopic hysteroscopy in infertile patients: a prospective, randomized, multicenter study. Fertil Steril 79:418–421
Perez-Medina T, Haya J, Frutos LS, Arenas JB (2002) Factors influencing long-term outcome of loop endometrial resection. J Am Assoc Gynecol Laparosc 9:272–276
Perino A, Mencaglia L, Hamou J, Cittadini E (1987) Hysteroscopy for metroplasty of uterine septa: report of 24 cases. Fertil Steril 48:321–323
Perino A, Castelli A, Cucinella G, Biondo A, Pane A, Venezia R (2004) A randomized comparison of endometrial laser intrauterine thermotherapy and hysteroscopic endometrial resection. Fertil Steril 82:731–734
Polena V, Mergui JL, Zerat L, Darai E, Barranger E, Uzan S (2005) Long-term results of hysteroscopic resection of endometrial polyps in 367 patients. Role of associated endometrial resection. Gynecol Obstet Fertil 33:382–388
Preutthipan S, Herabutya Y (2005) Hysteroscopic polypectomy in 240 premenopausal and postmenopausal women. Fertil Steril 83:705–709
Rosati M, Vigone A, Capobianco F, Surico D, Amoruso E, Surico N (2008) Long-term outcome of hysteroscopic endometrial ablation without endometrial preparation. Eur J Obstet Gynecol Reprod Biol 138:222–225
Roy KK, Baruah J, Sharma JB, Kumar S, Kachawa G, Singh N (2010) Arch Gynecol Obstet 281(2):355–61. doi:10.1007/s00404-009-1117-x. Epub 2009 May 20.
Savelli L, De IP, Santini D, Rosati F, Ghi T, Pignotti E, Bovicelli L (2003) Histopathologic features and risk factors for benignity, hyperplasia, and cancer in endometrial polyps. Am J Obstet Gynecol 188:927–931
Sesti F, Marziali M, Santomarco N (2000) Hysteroscopic surgery for endometrial polyps using a bipolar microelectrode. Int J Gynaecol Obstet 71:283–284
Shankar M, Naftalin NJ, Taub N, Habiba M (2003) The long-term effectiveness of endometrial laser ablation: a survival analysis. Eur J Obstet Gynecol Reprod Biol 108:75–79
Shankar M, Davidson A, Taub N, Habiba M (2004) Randomised comparison of distension media for outpatient hysteroscopy. BJOG 111:57–62
Timmermans A, Veersema S (2005) Ambulatory transcervical resection of polyps with the Duckbill polyp snare: a modality for treatment of endometrial polyps. J Minim Invasive Gynecol 12(1):37–39
Unfried G, Wieser F, Albrecht A, Kaider A, Nagele F (2001) Flexible versus rigid endoscopes for outpatient hysteroscopy: a prospective randomized clinical trial. Hum Reprod 16:168–171
van Dongen H, Emanuel MH, Wolterbeek R, Trimbos JB, Jansen FW (2008) Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol 15(4):466–471, Epub 18 Apr 2008. PMID: 18588849 [PubMed – indexed for MEDLINE]
Van DH, Janssen CA, Smeets MJ, Emanuel MH, Jansen FW (2009) The clinical relevance of hysteroscopic polypectomy in premenopausal women with abnormal uterine bleeding. BJOG 116:1387–1390
Wieser F, Kurz C, Wenzl R, Albrecht A, Huber JC, Nagele F (1998) Atraumatic cervical passage at outpatient hysteroscopy. Fertil Steril 69:549–551
Yu D, Wong YM, Cheong Y, Xia E, Li TC (2008) Asherman syndrome–one century later. Fertil Steril 89:759–779
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Istre, O., Thurkow, A. (2015). Hysteroscopic Instrumentation. In: Istre, O. (eds) Minimally Invasive Gynecological Surgery. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-44059-9_2
Download citation
DOI: https://doi.org/10.1007/978-3-662-44059-9_2
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-44058-2
Online ISBN: 978-3-662-44059-9
eBook Packages: MedicineMedicine (R0)