Abstract
Low-dose metronomic (LDM) chemotherapy, the frequent and continuous use of low doses of conventional chemotherapeutics, is an emerging alternative to conventional chemotherapy. Several pediatric preclinical solid tumor models are supporting the clinical development of this new therapeutic modality in pediatric cancer. Maintenance low dose chemotherapy has proven its benefits in increasing overall survival in several pediatric cancer. This chapter is reviewing the current knowledge of pediatric metronomic chemotherapy and potential for future development as cytotoxic agents or in combination with targeted therapy including its potential application in emerging countries.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Vascular Endothelial Growth Factor
- Zoledronic Acid
- Minimal Residual Disease
- Conventional Chemotherapy
- Malignant Peripheral Nerve Sheath Tumor
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
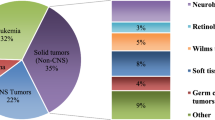
According to the WHO mortality report in 2008, cancer is the leading cause of disease-related death among children 5–14 years of age in high-income countries. Although communicable diseases remain the most common cause of death in low- and middle-income countries, because of high population density, 84 % of all children affected with cancer live in those countries [1, 2].
Conventional therapies have been effective in decreasing overall mortality rate from pediatric cancer; however, the prognosis remains poor for a subset of leukemias and lymphomas and metastatic solid tumors such as Ewing sarcoma, rhabdomyosarcoma, osteosarcoma, and neuroblastoma. Therefore, novel therapeutic approaches for these tumors should be explored, particularly in the setting of minimal residual disease that is associated with high risk of relapse and poor prognosis.
2 Conventional Chemotherapy
Cytotoxic antiproliferative agents are the mainstay of conventional chemotherapy regimens. In conventional chemotherapy, maximum tolerated dose (MTD) of cytotoxic drugs is used to kill the tumor cells. This approach has improved the cure and survival rates for different types of pediatric cancer; however, short- and long-term adverse effects of high doses of cytotoxic agents are of considerable importance, especially in young survivors of pediatric cancer. Acute adverse effects of conventional chemotherapy are mainly due to nonspecific effect of the cytotoxic drugs on the proliferating cells. Seventy percent of pediatric cancer survivors experience long-term complications of conventional chemotherapy and almost 40 % of them suffer from life-threatening or debilitating complications [3]. Eighty-seven percent of childhood cancer survivors report multiple symptom classes that impair their health-related quality of life [4]. In addition, most solid tumors are composed of heterogeneous subpopulations of cells with different cell kinetics, metastatic characteristics, and angiogenic and invasive potential [5]. Therefore, their response to conventional chemotherapy varies widely. Despite the advances in conventional therapeutic approaches, the overall survival rate of some of the pediatric solid tumors such as high-risk neuroblastoma and metastatic sarcomas has not improved since a few decades ago.
3 Minimal Residual Disease
Minimal residual disease (MRD) is characterized by the presence of a small number of cells unaffected by therapy. MRD is an independent prognostic factor of poor response and a predictor of relapse in hematologic malignancies, neuroblastoma, and rhabdomyosarcoma [6–8]. Conventional chemotherapeutic approaches fail to inhibit a group of tumor cells that either escape therapy by hiding in sites characterized by poor oxygenation or drug penetration or develop resistance to chemotherapeutic drugs [9]. Therefore, relapsed tumors respond poorly to conventional chemotherapy.
It has been postulated that tumor-initiating cells (TICs), which are known to generate the bulk of the tumor through their self-renewal and extensive proliferation capacities might present as MRD [10–12]. TICs are resistant to chemotherapy and can survive as MRD in the primary location or metastatic organs [13, 14]. Although the concept of cancer stem cells was first explored in hematologic malignancies, further studies led to the identification of TICs in solid tumors. Hsu et al. recently reported a distinct subpopulation in neuroblastoma with stem cell-like phenotype and high tumorigenic potential [15].
4 Maintenance Therapy
Maintenance therapy has been used in pediatric malignancies for many years. The wide acceptance of the concept of maintenance therapy in pediatric malignancies is reflected in the standard protocols of ALL, where maintenance regimen is continued for 2–3 years and consists of daily oral mercaptopurine, weekly methotrexate, vincristine, and corticosteroids [3]. Maintenance therapy with 13-cis-retinoic acid after myeloablative chemotherapy has improved the overall survival in neuroblastoma [16]. The goal of maintenance therapy is to prevent relapse by inhibiting the progression of MRD. Since maintenance therapy is administered in long term and usually in heavily pretreated patients, it should be minimally toxic. It is also crucial to avoid regimens, which have cross-resistance with previously administered drugs. The efficacy of maintenance therapy in improving survival rate was confirmed by a stage IV pediatric soft-tissue sarcoma trial comparing the oral maintenance regimen (consisting of trofosfamide + etoposide and trofosfamide + idarubicin) with high-dose therapy (thiotepa + cyclophosphamide and melphalan + etoposide). Patients who received maintenance therapy showed a survival rate of 57.8 % after 57.4 months versus 24.4 % in high-dose group [17].
5 Angiogenesis
Dr. Folkman first described the theory of tumor angiogenesis in 1971. He proposed that the size of the tumor is limited by its ability to develop new vasculature [18]. In addition to tumor growth, angiogenesis is required for metastatic spread and progression of tumor cells, as blood is the most common media to deliver tumor cells to other organs [19].
The mechanisms of tumor angiogenesis are varied. In sprouting angiogenesis, endothelial cells from preexisting blood vessels proliferate and migrate into tumor tissue to form the tumor vasculature. Intussusception refers to the process of the division of preexisting capillary plexus, without actual mitosis of endothelial cells [20]. In vasculogenesis endothelial progenitor cells are released from bone marrow and recruited by tumor tissue to form the new blood vessels [21]. Stromal Cell-Derived Factor-1 α and vascular endothelial growth factor (VEGF) are cytokines that facilitate the mobilization of bone marrow progenitors.
Tumor hypoxia simulates the angiogenic mechanisms. High turnover of tumor cells and abnormal architecture of tumor vasculature compromises oxygen and nutrient delivery to cells located far from the capillaries [22]. Under the hypoxic condition, stabilized HIF1-α forms a transcriptionally active complex (HIF1) with HIF1-β in the nucleus. HIF1 is a transcription factor for number of genes, involved in angiogenesis, cellular adaptation to hypoxia, and apoptosis [23]. VEGF is the most specific and critical angiogenic factor that is induced by HIF1-α.
Angiogenesis plays an important role in majority of pediatric cancers such as leukemia, CNS tumors, neuroblastoma, and pediatric sarcomas [24–28]. Inhibition of angiogenesis is therefore an effective maintenance therapy to control the growth of tumor or MRD.
Since the concept of tumor angiogenesis was suggested, several drugs with antiangiogenic properties were studied such as endogenous antiangiogenic molecules (angiostatin, endostatin) and endothelial growth inhibitors (TNP-470, thalidomide), VEGF tyrosine kinase inhibitors and receptors, MMP inhibitors, and inhibitors of vascular adhesion molecules [29]. Antiangiogenic agents are divided into two main categories based on their mechanism of action. Direct antiangiogenic drugs exert their effect directly on the endothelial cells, while indirect agents target growth factors or receptors involved in endothelial stimulation [30–35].
VEGF signaling pathway is the major pathway in tumor angiogenesis. Therefore, inhibition of VEGF pathway is the focus of most of the antiangiogenic strategies. Bevacizumab, a VEGF-neutralizing monoclonal antibody, was approved by FDA for colorectal cancer in 2004 [36]. Although it has not been yet approved for pediatric cancer, bevacizumab has been shown to delay tumor progression in an experimental metastatic neuroblastoma mice model [37]. Later, FDA also approved small-molecule receptor tyrosine kinase inhibitors (RTKIs) such as sunitinib, sorafenib, pazopanib, and axitinib, which inhibit VEGFR autophosphorylation [36]. In studies conducted by Pediatric Preclinical Testing Program (PPTP), pazopanib delayed the tumor growth and improved the survival in mice models of rhabdomyosarcoma and Ewing sarcoma [38]. Kumar et al. showed the efficacy of LDM topotecan + pazopanib in delaying tumor growth and enhancing the survival of neuroblastoma-bearing mice [39, 40].
6 Low-Dose Metronomic Chemotherapy
Low-dose metronomic (LDM) chemotherapy refers to the chronic administration of minimally toxic doses of cytotoxic agents without prolonged drug-free breaks. In 1991, Kerbel suggested that conventional chemotherapy drugs show antiangiogenic effects at low doses [41]. Klement et al. proved the efficacy of LDM vinblastine in neuroblastoma mouse model in 2000 [42]. Browder et al. could demonstrate the effectiveness of LDM cyclophosphamide in the xenograft models of breast cancer and Lewis lung carcinoma derived from cell lines, which were resistant to the same drugs [43]. Neoangiogenesis is a target for low-dose metronomic chemotherapy. Studies have shown that low doses of antiproliferative cytotoxic drugs inhibit tumor progression by antiangiogenic mechanism [42, 43].
LDM chemotherapy as a new therapeutic strategy has been explored in pediatric malignancy.
7 Preclinical Studies of LDM in Pediatric Tumor Models
Preclinical studies have provided valuable information about the efficacy and adverse effects of LDM chemotherapy in pediatric tumor models. In 2000, Klement et al. showed that in vitro low-dose vinblastine was more toxic to human umbilical vein endothelial cells (HUVEC) than to neuroblastoma cells and in vivo it caused a significant tumor growth delay and reduction in tumor perfusion [42]. In a study on Wilms tumor, topotecan reduced the size of the tumor at doses as low as 0.36 mg/kg with no observable adverse effects [44]. McCrudden et al. demonstrated growth inhibition and antiangiogenic effects of metronomic topotecan (0.36 mg/kg IV, 5 days/week for 6 weeks) in hepatoblastoma xenograft models [45]. The combination of conventional and metronomic scheduling of cytotoxic agents was shown to reduce tumor volume in osteosarcoma-bearing rat models [46]. Preclinical studies showed the effectiveness of extended low-dose topoisomerase I inhibitors against melphalan- and vincristine-resistant pediatric solid tumor xenografts [47]. Following the positive preclinical results, pharmacokinetically guided dosing schedule of topotecan was used in clinical studies involving pediatric solid tumors [48–50]. Later, Kumar et al. showed the superior efficacy of a combination of metronomic administration of topotecan and pazopanib over a single agent in either neuroblastoma, osteosarcoma, or rhabdomyosarcoma subcutaneous xenograft models. In comparison to single agents, the combination demonstrated enhanced antitumor activity and significantly increased the survival [39].
An international phase I clinical study of low-dose metronomic topotecan and pazopanib is about to start recruiting pediatric patients with recurrent or refractory solid tumors including CNS tumors (TOPAZ study).
Marimpietri et al. conducted in vitro and in vivo studies to investigate the antiangiogenic effects of low-dose vinblastine and rapamycin on neuroblastoma. They concluded that either agent alone could inhibit the growth of endothelial cells and the combination showed a significant synergistic effect [51]. Phase I clinical trial of the combination of weekly vinblastine and daily oral sirolimus (mammalian target of rapamycin inhibitor) for pediatric recurrent or refractory solid tumors showed the safety, clinical efficacy, and antiangiogenic properties of this combination [52]. This study along with other studies combining drugs to maximize the antiangiogenic effects signifies the importance of designing LDM regimens that could inhibit different mechanisms of angiogenesis.
8 Clinical Studies of LDM in Pediatric Malignancies
The number of clinical studies of LDM in pediatric malignancies is limited, but promising results have been achieved. Almost all pediatric studies have been conducted on metastatic or refractory tumors.
Some of the clinical trials have only used conventional cytotoxic agents with metronomic scheduling in pediatric malignancies. Fousseyni et al. showed the efficacy of a metronomic chemotherapeutic regimen consisting of vincristine, cyclophosphamide, and methotrexate in 12 children with refractory cancer (six cases of Wilms tumor, five cases of retinoblastoma, and one case of metastatic neuroblastoma). Disease stabilization was achieved in 7 patients (58 %) and 3 of them remained stable for at least 6 months posttreatment [53]. In another study on stage IV soft-tissue sarcoma, patients treated with low-dose metronomic cycles of trofosfamide, idarubicin, and etoposide showed better overall survival rate (0.52 + 0.14) compared to patients receiving high-dose chemotherapy (0.27 + 0.13) [17]. A phase II trial with metronomic thalidomide-carboplatin-vincristine-fluvastatin in pediatric brainstem tumors showed significant reduction in tumor volume after treatment. Partial response was observed in 7 out of 9 patients [54].
Minturn et al. demonstrated the efficacy of oral metronomic topotecan in recurrent childhood brain tumors. Disease stabilization and partial response were observed in 5 (20 %) and 2 (8 %) out of 25 patients, respectively [55].
Metronomic temozolomide has been used in combination with radiotherapy in children (n = 2) and adults (n = 3) with recurrent medulloblastoma. Local control was achieved in one of two pediatric patients who later developed relapse in another location under treatment with Choi protocol. Local relapse occurred in the other pediatric patient 10 months after reirradiation. The patient was reported to have stopped metronomic temozolomide earlier than planned. None of the patients showed neurological toxicity [56]. Sondhi et al. reported a case of complete remission of relapsed medulloblastoma with extensive osteosclerotic bony metastasis in a 14-year-old boy with LDM chemotherapy consisting of etoposide, cyclophosphamide, and zoledronic acid administered for 18 months. Complete response was maintained for >24 months (by the time the paper was written) with good quality of life [57].
In addition to more common cancers, metronomic chemotherapy has been associated with good results in less common pediatric malignancies. Chaudhary et al. reported the complete remission of a malignant peripheral nerve sheath tumor (MPNST) with metronomic chemotherapy. A combination of metronomic oral etoposide, cyclophosphamide, and prednisolone was administered successfully to a 10-year-old male with recurrent MPNST. Complete remission was sustained 20 months after the sessions of metronomic therapy [58]. Table 11.1 presents a summary of some of the recent LDM chemotherapy trials.
9 Combining Cytotoxic and Antiangiogenic Agents in LDM Chemotherapy
Tumor endothelial cells are susceptible to metronomic scheduling of conventional cytotoxic agents; however, upregulation of VEGF by endothelial cells can negate the antiangiogenic effects of LDM chemotherapy [62]. In addition to its growth factor effect, VEGF acts as a survival/antiapoptotic agent for endothelial cells through different mechanisms such as upregulation of antiapoptotic protein survivin, Bcl-2, and A1 in endothelial cells [63–65].
The combination of low-dose cytotoxic drugs with antiangiogenic agents has been studied in a few clinical trials in pediatric population with promising results.
A combination of temozolomide with celecoxib, 13-cis-retinoic acid, and etoposide in COMBAT (combined oral maintenance biodifferentiating and antiangiogenic therapy) protocol has been studied in 22 heavily pretreated children with relapsed solid tumors. Clinical response was observed in 9 of 14 children (64 %) with progressive disease. Patients showed good tolerance and compliance for oral medications. Side effects were minimal and responded well to dose modification or local therapy [66]. COMBAT regimen (low-dose daily temozolomide, etoposide, celecoxib, vitamin D, fenofibrate, and retinoic acid) was later used in another study achieving a 2-year overall survival in 43.1 % of patients with advanced pediatric malignancies [67].
Andrè et al. conducted a pilot study to evaluate the feasibility of a metronomic 4-drug regimen in pediatric patients with refractory or relapsing tumors. The combination consisted of vinblastine, cyclophosphamide, methotrexate, and daily celecoxib in cycles of 56 days. One objective response and 4 (25 %) disease stabilization were observed among 16 patients. Tolerability was acceptable. Interestingly, they reported reduced pain in 11 patients shortly after initiation of LDM chemotherapy [68].
Stempak et al. studied the combination of celecoxib and LDM vinblastine or cyclophosphamide in refractory pediatric solid tumors. The combination was well tolerated and 4 of 33 patients (13 %) experienced durable stable disease (28–78 weeks) [69].
In a recent phase II trial, Robison et al. evaluated the efficacy of a multi-agent metronomic therapeutic regimen consisting of celecoxib, thalidomide, and fenofibrate, with alternating 21-day cycles of low-dose cyclophosphamide and etoposide in children with recurrent or progressive disease. Favorable outcome including partial response and stable disease was reported for ependymoma and low-grade glioma. High-grade glioma and bone tumors responded poorly to treatment. The 27-week overall survival rate was 60 %. Grade 4 neutropenia (32 %) was the most common toxicity [70].
Peyrl et al. reported the therapeutic results of an antiangiogenic multidrug combination regimen consisting of bevacizumab, thalidomide, celecoxib, fenofibrate, etoposide, and cyclophosphamide and additional intraventricular therapy (etoposide and liposomal cytarabine) in children with recurrent embryonal brain tumors. Three complete and two partial responses were observed in five evaluable patients with medulloblastoma. Disease progression was seen in all patients with CNS primitive neuroectodermal tumors (CNS PNET, n = 4) and one out of seven patients with medulloblastoma. Six-month overall survival was 100 % and 75.0 ± 22 % for medulloblastoma and CNS PNET, respectively [71].
A Children’s Oncology Group (COG) phase II study (NCT00061893) demonstrated the feasibility of combination of standard multi-agent chemotherapy with low-dose vinblastine and celecoxib in 35 patients with metastatic Ewing sarcoma. Patients did not show excessive neurologic complications, infections, mucositis, and GI bleeding; however, the frequency and severity of pulmonary toxicity and hemorrhagic cystitis in patients who received radiation were unexpectedly high. The 24-month event-free survival of 71 % for patients with isolated pulmonary metastasis was higher than historical controls [72].
The combination of metronomic chemotherapy with non-antiangiogenic agents has been also studied. Russell et al. studied the efficacy of zoledronic acid with metronomic cyclophosphamide in 20 patients with recurrent/refractory neuroblastoma. One partial response and 9 stable disease responses (maintained for 2–12 months) were observed. The combination was well tolerated [73].
Table 11.2 summarizes some of the recent clinical trials of LDM chemotherapy with the combination of cytotoxic and antiangiogenic drugs.
10 Advantages of LDM
Cytotoxic drugs in high doses affect both tumor cells and normal proliferating cells. Therefore, most of the acute side effects of conventional chemotherapy are related to its cytotoxic properties. Lower doses of cytotoxic drugs in LDM result in less acute toxicity effects [76, 77]. Furthermore, the main target of LDM is endothelial cells in contrast to conventional chemotherapy where killing tumor cells is the ultimate goal. In a pioneering preclinical study conducted by Klement et al., it was observed that the sensitivity of human umbilical vein endothelial cells (HUVEC) to low-dose vinblastine was significantly higher than neuroblastoma cell lines [42].
Importantly, tumors resistant to high doses of a cytotoxic agent in conventional chemotherapy might be still sensitive to LDM scheduling of the same drug [43]. Furthermore, LDM can enhance the chemosensitivity of endothelial cells contrary to MTD (where cross-resistance between paclitaxel and vinblastine has been demonstrated) [78].
Few studies focused on the feasibility of metronomic chemotherapy in low-income countries. Inexpensive anticancer drugs can be used to design metronomic chemotherapy cycles. Furthermore, less acute toxicities associated with lower doses of cytotoxic agents in LDM chemotherapy are advantageous in areas with limited medical resources. Disease stabilization achieved by a metronomic regimen consisting of vincristine, cyclophosphamide, and methotrexate in children with different types of refractory tumors in Mali confirmed the feasibility and cost-effectiveness of this approach in low-income countries [53]. In “Metro-Mali-02” study, the same combination plus valproic acid resulted in long-lasting partial response (2 years) in two out of seven children, one with metastatic neuroblastoma and the other with retinoblastoma [79].
In low-income countries where curative or novel experimental treatments are not accessible for children with progressive cancer, low-cost maintenance therapy with inexpensive cytotoxic drugs is a viable option.
11 Limitations of LDM
11.1 Biomarkers
Preclinical studies and clinical trials have increased our knowledge of LDM chemotherapy and its clinical applications. Contrary to conventional chemotherapy, LDM affects tumor indirectly through antiangiogenesis. Therefore, biomarkers required for monitoring the efficacy and progress of treatment with LDM is different from conventional chemotherapy. Response Evaluation Criteria In Solid Tumors (RECIST), which evaluates the efficacy of therapy by tumor burden, does not reflect the response of tumors to antiangiogenic effects of LDM chemotherapy accurately [80]. Hence, surrogate markers should be explored to monitor tumor’s response to cytostatic effects of LDM. Proangiogenic and antiangiogenic growth factors and cytokines such as VEGF, basic fibroblast growth factor (bFGF), soluble vascular cell adhesion protein 1 (sVCAM-1), endostatin, and thrombospondin-1 (TSP-1), which were initially thought to correlate with the clinical benefits of LDM chemotherapy, failed to show consistent results in further studies [81]. In a pilot pharmacokinetic study of celecoxib and low-dose metronomic vinblastine or cyclophosphamide for pediatric patients with recurrent solid tumors, Stempak et al. showed that VEGF, bFGF, sVCAM-1, endostatin, and TSP-1 did not correlate with disease progression or maintenance of stable disease [69]. In a phase I trial of bevacizumab in refractory pediatric solid tumors, it was shown that baseline VEGF, TSP-1, bFGF, CEC, and CEP were not correlated with clinical benefit. However, researchers observed increased levels of mature CECs with treatment [82]. In a multicenter study of metronomic temozolomide combined with radiotherapy in pediatric patients with brainstem glioma, the decreasing trend of VEGF and endoglin was observed during the first two cycles of therapy. The decreasing trend of VEGF was associated with longer event-free survival [60]. In a phase I pharmacokinetic and pharmacodynamic study of pazopanib, it was shown that therapy significantly reduces plasma soluble VEGFR-2 and endoglin. A lower baseline plasma level of VEGF and placental growth factor was associated with clinical benefit [83].
Clinical trials in adult malignancies suggested a correlation between increasing levels of circulating endothelial cells (CECs) and disease progression [84]. The utility of CEC as a biomarker to monitor the antiangiogenic effects of LDM regimens was further explored in breast cancer, lymphoma, and GI stromal tumor with promising results [74, 85–87].
Higher levels of CEP have been detected in patients with pediatric malignancies compared to healthy controls. Children with metastatic disease show higher levels of CEP in comparison to localized disease [88].
In a preclinical study of aggressive pediatric solid tumors, it was demonstrated that the combination of metronomic oral topotecan and pazopanib significantly decreased viable CEC, viable CEP, and microvessel density [39]. In a clinical study with metronomic cyclophosphamide and celecoxib in non-Hodgkin’s lymphoma pediatric patients, CECs, CEPs, and VEGF remained low in responders after 8.4 months of follow-up [74]. Although CEC and CEP have shown promising results in adult malignancies, future preclinical and clinical studies in pediatric malignancies are required to address the utility of these cellular markers for monitoring tumor response to LDM therapy. Imaging is an alternative option to evaluate the response of tumor to antiangiogenesis. It has been demonstrated that changes in blood volume, blood flow, and vascular permeability correlate with the efficacy of antiangiogenic treatment [89].
11.2 LDM Cycles: Rationale and Design
Different drugs and drug combinations have been used in the preclinical studies and clinical trials of LDM in pediatric malignancies. The following criteria are used to choose a drug as a potential candidate for LDM chemotherapy: (a) it should be nonoverlapping and minimally toxic, (b) it could be administered orally, (c) it should have established antiangiogenic and/or immunostimulant effects, and (d) it should have low probability of developing drug resistance [90].
Pediatric patients with high-grade or refractory solid tumors are considered to benefit from LDM therapy. The type of tumor, its biological properties, and its clinical setting should be carefully considered before choosing a drug or drug combination for clinical trials of LDM chemotherapy in pediatric population. The optimal dose for the best therapeutic response is another challenge in developing LDM regimens for clinical trials. Contrary to conventional chemotherapy where maximally tolerated doses of drugs are chosen for the best clinical outcome, LDM therapy relies on the cytostatic effects of low doses of chemotherapeutic or antiangiogenic agents. Pharmacodynamic biomarkers are required to establish the optimal dose of antiangiogenic agents for LDM regimens. It has been speculated that LDM chemotherapy hinders mobilization of CEP from the bone marrow. Hence, CEP has been successfully used as a pharmacodynamic biomarker to provide information about optimum biological dose of metronomic cyclophosphamide, vinblastine, vinorelbine, and cisplatin in mice models of breast cancer, melanoma, and erythroleukemia [91].
In addition to drug and dose selection, defining clinical end points is an important step in designing and monitoring LDM therapy. Event-free survival and response rate that are commonly used in conventional chemotherapy have been employed in LDM clinical trials. Disease stabilization and good quality of life are other clinical benefits of LDM chemotherapy that could be incorporated into trials as clinical end points.
The duration of LDM chemotherapy in pediatric patients is another important question that should be answered. Sudden discontinuation versus gradual tapering of LDM chemotherapy should be compared in well-designed and closely monitored clinical trials.
Acute toxicity of LDM chemotherapy is lower than conventional chemotherapeutic approaches [76, 77, 92]. However, chronic administration of cytotoxic agents and subsequent accumulative doses might result in adverse events. Long-term side effects of LDM chemotherapy is therefore a concern that should be addressed in future studies.
Resistance to LDM chemotherapy emerged despite the initial assumptions about the genetic stability of tumor endothelial cells [62]. Resistance mechanisms are evoked in response to tumor microenvironment changes caused by antiangiogenic treatment. Upregulation of angiogenic factors [93, 94], involvement of bone marrow-derived cells [95, 96], and pericyte coverage [97] are some of the known mechanisms of resistance to LDM chemotherapy.
12 Future Direction
LDM chemotherapy is an alternative to conventional chemotherapy, which has shown promising results in preclinical and clinical studies of pediatric malignancies. However, more clinical trials are required to assess the efficacy and safety of LDM in pediatric population. Appropriate clinical end points should be defined with respect to antiangiogenic effects of LDM therapy. Studies should be conducted to validate biomarkers for evaluating the activity of treatment. Long-term side effects of LDM are of great importance and should be addressed in future studies. It should be emphasized that the goal of LDM is to be integrated into cancer maintenance therapy to control MRD and provide a good quality of life for patients living with cancer.
References
Global Health Observatory data repository—Cause-specific mortality, 2008: WHO region. http://apps.who.int/ghodata/?vid = 10012. Accessed 31 Dec 2012
Magrath I, Steliarova-Foucher E, Epelman S et al (2013) Paediatric cancer in low-income and middle-income countries. Lancet Oncol 14(3):e104–e116. doi:10.1016/S1470-2045(13)70008-1, Epub 2013 Feb 20
SEER, author. Surveillance, epidemiology, and end results (SEER) program web site. Cited 2003. Available at: http://www.seer.cancer.gov
Huang IC, Brinkman TM, Kenzik K et al (2013) Association between the prevalence of symptoms and health-related quality of life in adult survivors of childhood cancer: a report from the St Jude lifetime cohort study. J Clin Oncol 31(33):4242–4251. doi:10.1200/JCO.2012.47.8867, Epub 2013 Oct 14
Dexter DL, Leith JT (1986) Tumor heterogeneity and drug resistance. J Clin Oncol 4(2):244–257
Kågedal B (2009) Detecting minimal residual disease in neuroblastoma: still a ways to go. Clin Chem 55(7):1268–1270
Chertin B et al (2002) Post-chemotherapy microscopic residual prostate rhabdomyosarcoma: long-term conservative follow-up. Pediatr Surg Int 18(1):68–69
Paietta E (2002) Assessing minimal residual disease (MRD) in leukemia: a changing definition and concept? Bone Marrow Transplant 29(6):459–465
Reynolds CP (2004) Detection and treatment of minimal residual disease in high-risk neuroblastoma. Pediatr Transplant 8(Suppl 5):56–66
Nowell PC (1976) The clonal evolution of tumor cell populations. Science 194:23–28
Till JE, Mc CE (1961) A direct measurement of the radiation sensitivity of normal mouse bone marrow cells. Radiat Res 14:213–222
Luckey CJ, Bhattacharya D, Goldrath AW et al (2006) Memory T and memory B cells share a transcriptional program of self-renewal with long- term hematopoietic stem cells. Proc Natl Acad Sci U S A 103:3304–3309
Fialkow PJ, Gartler SM, Yoshida A (1967) Clonal origin of chronic myelocytic leukemia in man. Proc Natl Acad Sci U S A 58:1468–1471
Sloma I, Jiang X, Eaves AC et al (2010) Insights into the stem cells of chronic myeloid leukemia. Leukemia 24:1823–1833
Hsu DM, Agarwal S, Benham A et al (2013) G-CSF receptor positive neuroblastoma subpopulations are enriched in chemotherapy-resistant or relapsed tumors and are highly tumorigenic. Cancer Res 73(13):4134–4146
Yu AL et al (2010) Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N Engl J Med 363(14):1324–1334
Klingebiel T et al (2008) Treatment of children with metastatic soft tissue sarcoma with oral maintenance compared to high dose chemotherapy: report of the HD CWS-96 trial. Pediatr Blood Cancer 50(4):739–745
Folkman J (1971) Tumor angiogenesis: therapeutic implications. N Engl J Med 285(21):1182–1186
Folkman J (2002) Role of angiogenesis in tumor growth and metastasis. Semin Oncol 29(6 Suppl 16):15–18
Carmeliet P, Jain RK (2011) Molecular mechanisms and clinical applications of angiogenesis. Nature 473(7347):298–307
Asahara T et al (1997) Isolation of putative progenitor endothelial cells for angiogenesis. Science 275(5302):964–967
Weis SM, Cheresh DA (2011) Tumor angiogenesis: molecular pathways and therapeutic targets. Nat Med 17(11):1359–1370
Liao D, Johnson RS (2007) Hypoxia: a key regulator of angiogenesis in cancer. Cancer Metastasis Rev 26(2):281–290
Schneider P et al (2011) What role for angiogenesis in childhood acute lymphoblastic leukaemia? Adv Hematol 2011:274628
Kieran MW (2005) Anti-angiogenic therapy in pediatric neuro-oncology. J Neurooncol 75(3):327–334
Meitar D et al (1996) Tumor angiogenesis correlates with metastatic disease, N-myc amplification, and poor outcome in human neuroblastoma. J Clin Oncol 14(2):405–414
Sugiura Y et al (1998) Matrix metalloproteinases-2 and −9 are expressed in human neuroblastoma: contribution of stromal cells to their production and correlation with metastasis. Cancer Res 58(10):2209–2216
Ribatti D et al (2001) Angiogenesis extent and expression of matrix metalloproteinase-2 and −9 correlate with progression in human neuroblastoma. Life Sci 68(10):1161–1168
Gasparini G (1999) The rationale and future potential of angiogenesis inhibitors in neoplasia. Drugs 58(1):17–38
Kerbel RS (2000) Tumor angiogenesis: past, present and the near future. Carcinogenesis 21(3):505–515
Gordon MS, Mendelson DS, Kato G (2010) Tumor angiogenesis and novel antiangiogenic strategies. Int J Cancer 126(8):1777–1787
Cook KM, Figg WD (2010) Angiogenesis inhibitors: current strategies and future prospects. CA Cancer J Clin 60(4):222–243
Gately S, Li WW (2004) Multiple roles of COX-2 in tumor angiogenesis: a target for antiangiogenic therapy. Semin Oncol 31(2 Suppl 7):2–11
Oudard S et al (2009) Everolimus (RAD001): an mTOR inhibitor for the treatment of metastatic renal cell carcinoma. Expert Rev Anticancer Ther 9(6):705–717
Del Bufalo D et al (2006) Antiangiogenic potential of the Mammalian target of rapamycin inhibitor temsirolimus. Cancer Res 66(11):5549–5554
Wilson PM, LaBonte MJ, Lenz HJ (2013) Assessing the in vivo efficacy of biologic antiangiogenic therapies. Cancer Chemother Pharmacol 71(1):1–12
Sims TL et al (2008) Bevacizumab suppresses neuroblastoma progression in the setting of minimal disease. Surgery 144(2):269–275
Keir ST, Morton CL, Wu J, Kurmasheva RT, Houghton PJ, Smith MA (2012) Initial testing of the multitargeted kinase inhibitor pazopanib by the Pediatric Preclinical Testing Program. Pediatr Blood Cancer 59(3):586–588
Kumar S, Mokhtari RB, Sheikh R et al (2011) Metronomic oral topotecan with pazopanib is an active antiangiogenic regimen in mouse models of aggressive pediatric solid tumor. Clin Cancer Res 17(17):5656–5667
Kumar S, Mokhtari RB, Oliveira ID et al (2013) Tumor dynamics in response to antiangiogenic therapy with oral metronomic topotecan and pazopanib in neuroblastoma xenografts. Transl Oncol 6(4):493–503
Kerbel RS (1991) Inhibition of tumor angiogenesis as a strategy to circumvent acquired resistance to anti-cancer therapeutic agents. Bioessays 13(1):31–36
Klement G et al (2000) Continuous low-dose therapy with vinblastine and VEGF receptor-2 antibody induces sustained tumor regression without overt toxicity. J Clin Invest 105(8):R15–R24
Browder T et al (2000) Antiangiogenic scheduling of chemotherapy improves efficacy against experimental drug-resistant cancer. Cancer Res 60(7):1878–1886
Soffer SZ et al (2001) Novel use of an established agent: Topotecan is anti- angiogenic in experimental Wilms tumor. J Pediatr Surg 36(12):1781–1784
McCrudden KW et al (2002) Topotecan is anti-angiogenic in experimental hepatoblastoma. J Pediatr Surg 37(6):857–861
Zhu XZ, Yin HM, Mei J (2010) Inhibition of tumors cell growth in osteosarcoma- bearing SD rats through a combination of conventional and metronomic scheduling of neoadjuvant chemotherapy. Acta Pharmacol Sin 31(8):970–976
Houghton PJ et al (1995) Efficacy of topoisomerase I inhibitors, topotecan and irinotecan, administered at low dose levels in protracted schedules to mice bearing xenografts of human tumors. Cancer Chemother Pharmacol 36(5):393–403
Santana VM et al (2003) A pilot study of protracted topotecan dosing using a pharmacokinetically guided dosing approach in children with solid tumors. Clin Cancer Res 9(2):633–640
Stewart CF et al (2004) Results of a phase II upfront window of pharmacokinetically guided topotecan in high-risk medulloblastoma and supratentorial primitive neuroectodermal tumor. J Clin Oncol 22(16):3357–3365
Santana VM et al (2005) Improved response in high-risk neuroblastoma with protracted topotecan administration using a pharmacokinetically guided dosing approach. J Clin Oncol 23(18):4039–4047
Marimpietri D, Nico B, Vacca A et al (2005) Synergistic inhibition of human neuroblastoma-related angiogenesis by vinblastine and rapamycin. Oncogene 24(45):6785–6795
Morgenstern DA, Marzouki M, Bartels U et al (2014) Phase I study of vinblastine and sirolimus in pediatric patients with recurrent or refractory solid tumors. Pediatr Blood Cancer 61(1):128–133
Fousseyni T, Diawara M, Pasquier E, André N (2011) Children treated with metronomic chemotherapy in a low-income country: METRO-MALI-01. J Pediatr Hematol Oncol 33(1):31–34
López-Aguilar E, Sepúlveda-Vildósola AC, Betanzos-Cabrera Y et al (2008) Phase II study of metronomic chemotherapy with thalidomide, carboplatin-vincristine-fluvastatin in the treatment of brain stem tumors in children. Arch Med Res 39(7):655–662
Minturn JE, Janss AJ, Fisher PG et al (2011) A phase II study of metronomic oral topotecan for recurrent childhood brain tumors. Pediatr Blood Cancer 56(1):39–44
Padovani L, Andre N, Gentet JC et al (2011) Reirradiation and concomitant metronomic temozolomide: an efficient combination for local control in medulloblastoma disease? J Pediatr Hematol Oncol 33(8):600–604
Sondhi V, Arun Kurkure P, Jalali R et al (2012) Complete remission and long-term survival in a child with relapsed medulloblastoma with extensive osteosclerotic bony metastasis with a novel metronomic chemobiological approach. J Pediatr Hematol Oncol 34(5):e195–e198
Chaudhary N, Borker A (2012) Metronomic therapy for malignant peripheral nerve sheath tumor in neurofibromatosis type 1. Pediatr Blood Cancer 59(7):1317–1319
Dantonello TM et al (2011) Embryonal rhabdomyosarcoma with metastases confined to the lungs: report from the CWS Study Group. Pediatr Blood Cancer 56(5):725–732
Sharp JR, Bouffet E, Stempak D (2010) A multi-centre Canadian pilot study of metronomic temozolomide combined with radiotherapy for newly diagnosed paediatric brainstem glioma. Eur J Cancer 46(18):3271–3279
Baruchel S et al (2006) Safety and pharmacokinetics of temozolomide using a dose- escalation, metronomic schedule in recurrent paediatric brain tumours. Eur J Cancer 42(14):2335–2342
Kerbel RS et al (2001) Possible mechanisms of acquired resistance to anti- angiogenic drugs: implications for the use of combination therapy approaches. Cancer Metastasis Rev 20(1–2):79–86
Tran J et al (2002) A role for survivin in chemoresistance of endothelial cells mediated by VEGF. Proc Natl Acad Sci U S A 99(7):4349–4354
Kucerová H et al (2001) Significance of P-glycoprotein expression in childhood malignant tumors. Neoplasma 48(6):472–478
Goto H et al (2000) Multidrug resistance-associated protein 1 (MRP1) expression in neuroblastoma cell lines and primary tumors. Med Pediatr Oncol 35(6):619–622
Sterba J, Valik D, Mudry P et al (2006) Combined biodifferentiating and antiangiogenic oral metronomic therapy is feasible and effective in relapsed solid tumors in children: single-center pilot study. Onkologie 29(7):308–313
Zapletalova D et al (2012) Metronomic chemotherapy with the COMBAT regimen in advanced pediatric malignancies: a multicenter experience. Oncology 82(5):249–260
André N et al (2011) Pilot study of a pediatric metronomic 4-drug regimen. Oncotarget 2(12):960–965
Stempak D, Gammon J, Halton J, Moghrabi A, Koren G, Baruchel S (2006) A pilot pharmacokinetic and antiangiogenic biomarker study of celecoxib and low-dose metronomic vinblastine or cyclophosphamide in pediatric recurrent solid tumors. J Pediatr Hematol Oncol 28(11):720–728
Robison NJ, Campigotto F, Chi SN et al (2014) A phase II trial of a multi-agent oral antiangiogenic (metronomic) regimen in children with recurrent or progressive cancer. Pediatr Blood Cancer 61(4):636–642. doi:10.1002/pbc.24794
Peyrl A, Chocholous M, Kieran MW et al (2012) Antiangiogenic metronomic therapy for children with recurrent embryonal brain tumors. Pediatr Blood Cancer 59(3):511–517
Felgenhauer JL, Nieder ML, Krailo MD et al (2013) A pilot study of low-dose anti-angiogenic chemotherapy in combination with standard multiagent chemotherapy for patients with newly diagnosed metastatic Ewing sarcoma family of tumors: A Children’s Oncology Group (COG) Phase II study NCT00061893. Pediatr Blood Cancer 60(3):409–414
Russell HV, Groshen SG, Ara T et al (2011) A phase I study of zoledronic acid and low-dose cyclophosphamide in recurrent/refractory neuroblastoma: a new approaches to neuroblastoma therapy (NANT) study. Pediatr Blood Cancer 57(2):275–282
Buckstein R, Kerbel RS, Shaked Y et al (2006) High-Dose celecoxib and metronomic “low-dose” cyclophosphamide is an effective and safe therapy in patients with relapsed and refractory aggressive histology non-Hodgkin’s lymphoma. Clin Cancer Res 12:5190–5198
André N, Rome A, Coze C et al (2008) Metronomic etoposide/cyclophosphamide/celecoxib regimen given to children and adolescents with refractory cancer: a preliminary monocentric study. Clin Ther 30(7):1336–1340
Kerbel RS, Kamen BA (2004) The anti-angiogenic basis of metronomic chemotherapy. Nat Rev Cancer 4:423–436
Stempak D, Seely D, Baruchel S et al (2006) Metronomic dosing of chemotherapy: applications in pediatric oncology. Cancer Invest 24(4):432–443
Pasquier E et al (2013) Concentration- and schedule-dependent effects of chemotherapy on the angiogenic potential and drug sensitivity of vascular endothelial cells. Angiogenesis 16(2):373–386
Traore F, Togo B, Pasquier E, Dembélé A, André N (2013) Preliminary evaluation of children treated with metronomic chemotherapy and valproic acid in a low-income country: Metro-Mali-02. Indian J Cancer 50(3):250–253
DePrimo SE, Bello C (2007) Surrogate biomarkers in evaluating response to anti-angiogenic agents: focus on sunitinib. Ann Oncol 18(Suppl 10):x11–x19
Lansiaux A, Salingue S, Dewitte A, Clisant S, Penel N (2012) Circulating thrombospondin 1 level as a surrogate marker in patients receiving cyclophosphamide-based metronomic chemotherapy. Invest New Drugs 30(1):403–404
Glade Bender JL, Adamson PC, Reid JM et al (2008) Phase I trial and pharmacokinetic study of bevacizumab in pediatric patients with refractory solid tumors: a Children’s Oncology Group Study. J Clin Oncol 26(3):399–405
Glade Bender JL, Lee A, Reid JM et al (2013) Phase I pharmacokinetic and pharmacodynamic study of pazopanib in children with soft tissue sarcoma and other refractory solid tumors: a children’s oncology group phase I consortium report. J Clin Oncol 31(24):3034–3043
Mancuso P, Burlini A, Pruneri G, Goldhirsch A, Martinelli G, Bertolini F (2001) Resting and activated endothelial cells are increased in the peripheral blood of cancer patients. Blood 97(11):3658–3661
Mancuso P, Colleoni M, Calleri A et al (2006) Circulating endothelial-cell kinetics and viability predict survival in breast cancer patients receiving metronomic chemotherapy. Blood 108:452–459
Fürstenberger G, von Moos R, Lucas R et al (2006) Circulating endothelial cells and angiogenic serum factors during neoadjuvant chemotherapy of primary breast cancer. Br J Cancer 4:524–531
Norden-Zfoni A, Desai J, Manola J et al (2007) Blood-based biomarkers of SU11248 activity and clinical outcome in patients with metastatic imatinib- resistant gastrointestinal stromal tumor. Clin Cancer Res 13:2643–2650
Taylor M, Rössler J, Geoerger B et al (2009) High levels of circulating VEGFR2+ Bone marrow-derived progenitor cells correlate with metastatic disease in patients with pediatric solid malignancies. Clin Cancer Res 15(14):4561–4571
Jain RK et al (2009) Biomarkers of response and resistance to antiangiogenic therapy. Nat Rev Clin Oncol 6(6):327–338
Pasquier E, Kieran MW, Sterba J et al (2011) Moving forward with metronomic chemotherapy: meeting report of the 2nd International Workshop on Metronomic and Anti-Angiogenic Chemotherapy in Paediatric Oncology. Transl Oncol 4(4):203–211
Shaked Y et al (2005) Optimal biologic dose of metronomic chemotherapy regimens is associated with maximum antiangiogenic activity. Blood 106(9):3058–3061
Baruchel S, Stempak D (2006) Low-dose metronomic chemotherapy: myth or truth? Onkologie 29(7):305–307
Mizukami Y et al (2005) Induction of interleukin-8 preserves the angiogenic response in HIF-1alpha-deficient colon cancer cells. Nat Med 11(9):992–997
Fernando NT et al (2008) Tumor escape from endogenous, extracellular matrix- associated angiogenesis inhibitors by up-regulation of multiple proangiogenic factors. Clin Cancer Res 14(5):1529–1539
Ebos JM et al (2007) Multiple circulating proangiogenic factors induced by sunitinib malate are tumor-independent and correlate with antitumor efficacy. Proc Natl Acad Sci U S A 104(43):17069–17074
Ceradini DJ et al (2004) Progenitor cell trafficking is regulated by hypoxic gradients through HIF-1 induction of SDF-1. Nat Med 10(8):858–864
Benjamin LE, Hemo I, Keshet E (1998) A plasticity window for blood vessel remodelling is defined by pericyte coverage of the preformed endothelial network and is regulated by PDGF-B and VEGF. Development 125(9):1591–1598
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Baluch, N., Kumar, S., Mokhtari, R., Baruchel, S. (2014). Metronomic Chemotherapy in Pediatric Malignancies. In: Bocci, G., Francia, G. (eds) Metronomic Chemotherapy. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-43604-2_11
Download citation
DOI: https://doi.org/10.1007/978-3-662-43604-2_11
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-43603-5
Online ISBN: 978-3-662-43604-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)